Abstract
Background
Depression may contribute to increased drinking in individuals with alcohol use disorder. Although Alcoholics Anonymous (AA) attendance predicts drinking reductions, there is conflicting information regarding the intermediary role played by reductions in depression.
Objectives
We explored whether AA attendance reduces depressive symptoms, the degree to which improvement in depression results in reductions in drinking, and in which subgroups these effects occur.
Methods
253 early AA affiliates (63% male) were recruited and assessed at baseline 3, 6, 9, 12, 18, and 24 months. Depression was measured using the Beck Depression Inventory (BDI) and was administered at baseline 3, 6, 12, 18, and 24 months. AA attendance and alcohol use outcomes were obtained with the Form 90. Mediation analyses were performed at early (3, 6, and 9 months) and late (12, 18, and 24 months) follow-up to investigate the degree to which reductions in depression mediated the effect of AA attendance on drinking, controlling for concurrent drinking. In addition, a series of moderated mediation analyses were performed using baseline depression severity as a moderator.
Results
At early follow-up, reductions in depression (6 months) mediated the effects of AA attendance (3 months) on later drinking (drinks per drinking day) (9 months) (b = −0.02, boot CI [−0.055, −0.0004]), controlling for drinking at 6 months. Baseline depression severity did not moderate the degree to which BDI mediated the effects of AA attendance on alcohol use (ps > .05).
Conclusion
These findings provide further evidence that depression reduction is a mechanism by which AA attendance leads to reductions in alcohol use. Improving depression may help reduce alcohol use in individuals with AUD, and AA attendance may be an effective way to achieve that goal.
Keywords: 12-step, alcoholics anonymous, depression, alcohol use disorders, negative affect
Background
Relatively consistent evidence has accumulated, indicating that community-based Alcoholics Anonymous (AA) attendance is predictive of decreased alcohol use for many, but not all, problem drinkers (1–5). Importantly, self-selection bias does not appear to account for AA-related benefit (6–8), and the salutary effects of AA have been observed in diverse populations including urban Native Americans (9), dually diagnosed adults (10,11), and ethnic minorities (12,13). Factors that do appear to account for AA-related benefit during early AA affiliation include acquiring an AA sponsor (14–16) social support for abstinence (17,18), gains in spiritual practices (19,20), and increased abstinence self-efficacy (21–24).
Central in the core AA literature (25) is the proposition that negative affect is a leading precipitant to relapse and much of the prescribed step work in 12-step programs is therefore directed at reducing the unbridled expression of anger, depression, and selfishness. The degree to which AA attendance influences AA member depression and, in turn, how changes in depression among AA members actually explains the beneficial effect of AA on drinking, remains unclear, however. Specifically, three rigorous longitudinal studies have investigated changes in depression among AA members (26–28) (hereafter referred to as Wilcox et al. (26), Worley et al. (27) and Kelly et al. (28), respectively). Found in each of these studies, AA exposed adults reported significant reductions in depressive symptoms over time, with such pre-post reductions observed at 6-month follow-up among veterans with substance use and major depressive disorder [Worley et al. (27); Hedges g (g, Cohen’s d adjusted for small sample bias) = 0.55], at 9 months in both outpatient and aftercare treatment seeking Project MATCH samples (Kelly et al. (28); g = 0.29), and over the course of 2 years in a community-recruited sample (Wilcox et al. (26); g = 0.18). Lagged analyses in each aforementioned study showed that frequency of AA attendance was associated with later reductions in depression.
Findings diverge, however, when changes in depressive symptoms were examined after statistically controlling for concurrent drinking. In the Kelly et al. (28) study, for example, the inclusion of current drinking in the lagged models eliminated the direct and independent effect of AA attendance on levels of depression symptoms, so reductions in depressive symptoms were attributed to the direct effect of AA attendance on reducing drinking. Furthermore, Kelly et al. (28) determined that changes in depressive symptoms did not mediate that association between frequency of AA attendance and later drinking in either the aftercare or outpatient MATCH samples. A different relationship between AA attendance and changes in depression was presented in Worley et al. (27) and Wilcox et al. (26). Specifically, these studies found that the independent effect of AA on later levels of depression symptoms remained even after controlling for concurrent alcohol and substance use, suggesting that reductions in levels of depression symptoms may be attributable to the influence of AA beyond that explained by reductions in alcohol or substance use. Also noteworthily, Worley et al. (27) reported that reductions in depression significantly mediated 15% of the direct effect of AA on drinking. Wilcox et al. (26) did not examine whether reductions in depression mediated the effect of AA on drinking.
There are some possible explanations for the conflicting results between these three studies. Foremost, at baseline, the absolute severity of depressive symptoms was significantly different across the three studies, with the MATCH aftercare and outpatient samples for Kelly et al. (28) reporting significantly lower levels of depression. Combining the MATCH aftercare and outpatient samples, for example, yielded a mean Beck Depression Inventory-II (BDI) (29) score at intake of 10.16 (SD 8.25). The mean score for the community-based AA sample for Wilcox et al. (26) was 19.79 (SD 11.35), almost twice as depressed as the Kelly et al. (28) sample, and approached the BDI cutoff score of 20 for moderate depression. The most depressed sample studied was that of Worley et al. (27) which had a mean Hamilton Depression Scale score of 28.55 (SD 10.82), well above the cutoff of 17 for moderate depression (30), and all subjects had a diagnosis of major depressive disorder. We therefore suspected that adults with major depressive disorders were disproportionately represented in Worley et al. (27) and Wilcox et al. (26), and that, to some extent, the significantly lower levels of depression symptoms found in the MATCH sample from Kelly et al. (28) could have resulted in lower effects of AA on depression. Other related work, using multiple mediator analyses, has also found a stronger relationship between AA, depression, and later drinking (mediation) in individuals with more severe depression (19).
Objectives
The objective of this study was to shed light on the reasons for conflicting findings in studies of the relationship between AA exposure, changes in depression, and drinking outcomes by performing additional analyses on the dataset used in the Wilcox et al. (26) study, with a particular focus on whether or not changes in depression mediated the reductions in drinking observed AA attendance. To do so, we investigated whether changes in levels of depression could explain the effects of AA exposure on later drinking in our sample, using similar approaches to those utilized by Kelly et al. (28) and Worley et al. (27). Furthermore, we investigated whether or not the presence or absence of a clinically relevant depression score at study entry moderated the strength of these associations. We hypothesized that since our sample was more depressed than that of Kelly et al. (28), and therefore more similar to that of Worley et al. (27), changes in depression would mediate the effects of AA on drinking (Aim 1), similar to the results in Worley et al. (27), but unlike those in Kelly et al. (28). Furthermore, if differences in baseline depression levels between the Worley et al. (27) and Kelly et al. (28) studies were driving the differences in findings, we hypothesized that baseline depression would moderate the meditational effect, and that mediation would be more pronounced (larger indirect effect) in those with greater baseline depression (Aim 2).
Methods
Participants and procedure
This is a follow-up report to a previously published paper (26), and details about the community-based AA sample can be obtained from the original paper. In brief, participants were early AA affiliates with little previous exposure to 12-step programs (participants were excluded for more than 16 weeks of lifetime AA exposure and if they reported ever having had a period of alcohol abstinence of at least 12 months at any time in their life after their alcohol use had become a problem). Two hundred and fifty-three adults with alcohol use problems were recruited from AA groups; from outpatient substance abuse treatment facilities; and from community sources including homeless shelters, advertisement in local newspapers, and flyers (68 were recruited from community-based AA, 87 were recruited from outpatient treatment abuse treatment centers, and 98 at shelters or through advertisements and flyers). Participants were also required to have attended one or more AA meetings in the prior 3 months, to have consumed alcohol in the prior 90 days, and to meet Diagnostic and Statistical Manual of Mental Disorders (31) criteria for alcohol dependence or abuse (32). All procedures were approved by the institutional review board at the University of New Mexico (UNM Protocol No. 24028).
Breathalyzers were used to ensure that participants’ blood alcohol concentration did not exceed 0.05 prior to the consent process, or at any subsequent interview. Once consented, participants were administered a baseline interview that included 15 self-report questionnaires, 3 semi-structured interviews, and a urine toxicology screen. Follow-up interviews were conducted in 3-month increments for one year and then at 18 and 24 months. More than 85% of the original sample provided follow-up data at 24 months. No intervention was offered in this assessment-only study, although clinical referrals were made upon participant request, or when deemed warranted by clinical staff.
Measures
Alcohol use
Alcohol use data were obtained using the Form 90 (33), which is a calendar-based semi-structured interview. Two alcohol use measures from the Form 90 were computed. Proportion of days abstinent from alcohol (PDA) was defined as the number of alcohol-abstinent days in an assessment period divided by the total number of days in the period. Drinks per drinking day (DPDD) was defined as number of drinks consumed per drinking (i.e., non-abstinent) days in the assessment period.
12-step meeting attendance
A single item from the Form 90 interview documented frequency of 12-step meeting attendance during an interview period. The proportion days of 12-step attendance for each participant was calculated as a ratio of days 12-step meeting attendance divided by the number of days in an interview period.
Depression
The Beck Depression Inventory (BDI) (29), commonly used in both clinical and research settings to screen for and establish severity of depression, was used as a measure of depressive symptomatology. The BDI is composed of 21 questions each scored on a scale of 0 to 3 asking about symptoms over the past 2 weeks such as hopelessness, irritability, guilt, feelings of being punished, fatigue, weight loss, and lack of interest in sex. Total scores on the BDI of 0–13 indicate minimal depression, 14–19 mild depression, 20–28 moderate depression, and 29–63 severe depression. For mediation analyses, we used the BDI as a continuous variable to mark the degree of depressive symptomatology. When used as a moderator, we used a dichotomous moderator variable by grouping individuals with minimal or mild depression into one group, and those with moderate or severe depression into the other group as a marker of the presence or absence of clinically relevant depression.
Statistical analyses
To examine whether the effect of AA attendance on drinking (DPDD, PDA) could be partially or fully accounted for by changes in BDI scores, we conducted mediation tests using the bias-corrected bootstrap (34) as implemented in the PROCESS macro for SPSS (35), which uses ordinary least squares regression. In all models, we bootstrapped 1000 samples and significant effects were determined by 95% bias-corrected confidence intervals that do not contain zero. We conducted two single-mediation models (Aim 1: Analysis 1 for PDA, Analysis 2 for DPDD) in which we examined the total, direct, and indirect effects of AA attendance on alcohol use via BDI scores at early follow-up (3-month AA; 6-month BDI; 9-month alcohol use; n = 194). For these two models, drinking and BDI at study entry (baseline) were entered as covariates, and concurrent drinking (6 months) was entered as a mediator operating in parallel [Figure 1; Model 4 in PROCESS Macro (36)]. We then conducted two tests of moderated mediation (Aim 2: Analysis 3 for PDA, Analysis 4 for DPDD) by entering baseline categorical depression as a moderator into the two single-mediation models defined above [Figure 2; Model 58 in PROCESS Macro (36)]. Although we did not formally test for heteroskedasticity, we used the heteroskedasticity-consistent standard errors option in the process macro (37). For our post hoc late follow-up analyses, we used exactly the same methods described above, except that we used 12 month AA, 18 month BDI and 24 month alcohol use (n = 183) instead of the 3-, 6-, and 9-month time points described above (Figures 1 and 2; Analyses 5, 6, 7, 8). The outcome variables were transformed prior to the analyses using a transformation that eliminated extreme outliers (DPDD was square root transformed; PDA was arc sin of square root transformed), although this may not have been necessary, as bootstrapping (as opposed to the Sobel test for indirect effects) significantly minimizes the need for normally distributed outcome variables (38). We note for the reader that p values are appropriate for all of the reported parameters except the indirect effects. In this case, we are interested in whether the CI contains 0 or not.
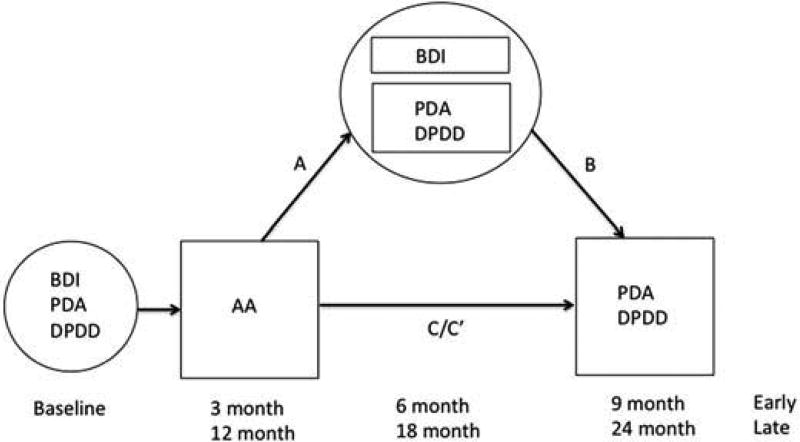
Figure 1.
Pictorial representation of statistical mediation model used for Aim 1/Analysis 1 and 2 (early follow-up for PDA and DPDD) and Analysis 5 and 6 (late follow-up for PDA and DPDD). Definitions: AA = AA attendance; PDA = percent days abstinent; DPDD = drinks per drinking day; BDI = Beck Depression Inventory; Early = early follow-up; Late = late follow-up; A = path A, B = path B, C = path C representing total effect before mediator is entered into model, C′ = path C′ representing direct effect after mediator is entered into model. Coefficients and significance values for Analysis 1 and 2 are in Table 2, and for Analysis 5 and 6 are in Table 3.
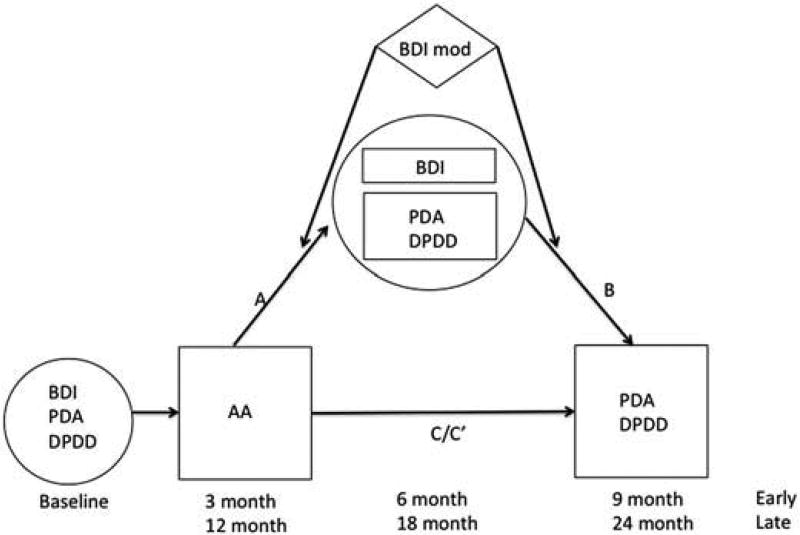
Figure 2.
Pictorial representation of statistical moderated mediation model used for Aim 2/Analysis 3 and 4 (early follow-up for PDA and DPDD) and Analysis 7 and 8 (late follow-up for PDA and DPDD). Definitions: AA = AA attendance; PDA = percent days abstinent; DPDD = drinks per drinking day; BDI = Beck Depression Inventory; Early = early follow-up; Late = late follow-up; A = path A, B = path B, C = path C representing total effect before mediator is entered into model, C′ = path C′ representing direct effect after mediator is entered into model. Coefficients and significance values for Analysis 7 and 8 are in Table 4.
Results
Participant information
Of the 253 participants, 194 participants had complete data for the planned analyses at early follow-up. Of these 194 participants, 63% of the sample was male (n=123) and the mean age of participants was 39.14 years (SD 9.84). A majority of the reduced sample had a high school degree (22.2% no degree, 12.4% GED, 38.1% high school diploma), were unemployed (63.9%), and were single or divorced (48.1%, 34.5%); 16.0% of the participants reported being homeless. Of the 194 participants, 42.9% were Hispanic, 32.1% were non-Hispanic White, 18.7% were Native American, and the remaining participants were of African, Asian, or unspecified ancestry. Finally, at study entry, participants reported that they were attending AA meetings 16.0% of the days (SD 18.5%) and had a mean BDI score of 20.1 (SD 11.3), a mean proportion of days abstinent of alcohol of 52.7 (SD 30.5) and a mean drinks per drinking day of 17.60 (12.81).
Simple correlations between primary measures [alcohol use (baseline), BDI (baseline), AA (3 month), BDI (6 month), alcohol use (9 month)] were in the expected directions such that greater AA attendance was associated with lower BDI scores and lower alcohol consumption, and lower BDI scores were associated with lower alcohol consumption (Table 1). Of note, the full sample (n = 253) and the complete data sample for the early follow-up analyses (n = 194) had very similar mean values for the key variables in our analyses (Supplementary Table 1).
Table 1.
Correlations between AA attendance, depression, and alcohol use (early).
| PDA BL | DPDD BL | BDI BL | AA 3 months | PDA 6 months | DPDD 6 months | BDI 6 months | PDA 9 months | |
|---|---|---|---|---|---|---|---|---|
| DPDD BL | −0.046, 253 | |||||||
| BDI BL | −0.247**, 227 | −0.014, 227 | ||||||
| AA 3 months | 0.196**, 239 | 0.238**, 239 | −0.201**, 215 | |||||
| PDA 6 months | 0.269**, 239 | 0.077, 239 | −0.227**, 214 | 0.438**, 236 | ||||
| DPDD 6 months | −0.113, 239 | 0.020, 239 | 0.202*, 214 | −0.282**, 236 | −0.817**, 239 | |||
| BDI 6 months | −0.097, 215 | −0.133, 215 | 0.455**, 199 | −0.235**, 215 | −0.381**, 214 | 0.327**, 214 | ||
| PDA 9 months | 0.278**, 237 | 0.072, 237 | −0.212**, 213 | 0.370**, 233 | 0.705**, 234 | −0.532**, 234 | −0.362**, 211 | |
| DPDD 9 months | −0.142*, 237 | 0.076, 237 | 0.172*, 213 | −0.258**, 233 | −0.573**, 234 | 0.575**, 234 | 0.305**, 211 | −0.837**, 237 |
p < 0.05,
p < 0.01.
All values are reported in the format: Spearman’s rho, number of participants; BL = baseline, BDI = Beck Depression Inventory, PDA = percent days abstinent, DPDD = drinks per drinking day (transformed variables for PDA and DPDD).
Mediation analyses—Aim 1/early follow-up (Analysis 1, 2)
There was a significant direct effect of AA (3 months) on drinking (6 months) for both PDA (p = 0.000, b = 0.441, t = 5.88) and DPDD (p = 0.009, b = −1.482, t = −3.388). The direct effect of AA (3 months) on drinking (9 months) was not significant, although the total effect was highly significant for both PDA (p=0.006, b = 0.102, t = 2.757) and DPDD (p = 0.008, b = −1.177, t = −2.694). Furthermore, in support of previous findings (26), there were significant effects of AA (3 months) on BDI (6 months) for PDA (p = 0.040, b = −5.043, t = −2.073) and DPDD (p = 0.050, b = −4.723, t = −1.973) (path A; Figure 1). For DPDD, but not PDA, BDI (6 month) was associated with DPDD (9 months) (p = 0.041, b = 0.023, t = 2.060) (path B; Figure 1), and the indirect effect of AA (3 months) on alcohol use at 9 months via BDI (6 months) was also significant. Not surprisingly, alcohol use at 6 months (PDA and DPDD) was a significant mediator of the effects of AA (3 months) on alcohol use (9 months) (Table 2).
Table 2.
Results from mediation analyses to examine whether changes in depression mediate the effect of AA attendance on alcohol use outcomes at early follow-up (3, 6, 9 months; Fig.1; Aim 1; Analysis 1, 2).
| PDA early (n = 194) | Coeff | SE | t | p |
|---|---|---|---|---|
| Path A (to BDI 6 months) | ||||
| AA 3 months | −5.043 | 2.432 | −2.073 | 0.040 |
| PDA baseline | −0.009 | 2.336 | −0.004 | 0.997 |
| Path A (to PDA 6 months) | ||||
| AA 3 months | 0.441 | 0.075 | 5.875 | 0.000 |
| BDI baseline | −0.004 | 0.002 | −1.751 | 0.082 |
| Path B (to PDA 9 months) | ||||
| BDI 6 months | −0.004 | 0.003 | −1.415 | 0.159 |
| AA 3 months | −0.059 | 0.088 | −0.669 | 0.505 |
| BDI baseline | 0.001 | 0.003 | 0.526 | 0.599 |
| Total Effect (to PDA 9 months) | ||||
| AA 3 months | 0.282 | 0.102 | 2.757 | 0.006 |
| BDI baseline | −0.003 | 0.003 | −1.195 | 0.234 |
|
|
||||
| Coeff | Boot SE | Boot LLCI | Boot ULCI | |
|
|
||||
| Indirect effect (BDI 6 months is mediator) | 0.013 | 0.012 | −0.002 | 0.051 |
| Indirect Effect (PDA 6 months is mediator) | 0.221 | 0.043 | 0.141 | 0.310 |
|
| ||||
| DPDD early (n=194) | Coeff | SE | t | p |
|
| ||||
| Path A (to BDI 6 months) | ||||
| AA 3 months | −4.723 | 2.394 | −1.973 | 0.050 |
| DPDD baseline | −0.293 | 0.507 | −0.579 | 0.563 |
| Path A (to DPDD 6 months) | ||||
| AA 3 months | −1.482 | 0.437 | −3.388 | 0.001 |
| BDI baseline | 0.023 | 0.010 | 2.204 | 0.029 |
| Path B (to DPDD 9 months) | ||||
| BDI 6 months | 0.023 | 0.011 | 2.060 | 0.041 |
| AA 3 months | −0.293 | 0.347 | −0.845 | 0.399 |
| BDI baseline | −0.0001 | 0.010 | 0.008 | 0.994 |
| Total Effect (to DPDD 9 months) | ||||
| AA 3 months | −1.177 | 0.437 | −2.694 | 0.008 |
| BDI baseline | 0.022 | 0.011 | 2.023 | 0.044 |
|
|
||||
| Coeff | Boot SE | Boot LLCI | Boot ULCI | |
|
|
||||
| Indirect effect (BDI 6 months is mediator) | −0.019 | 0.013 | −0.055 | −0.0004 |
| Indirect effect (DPDD 6 months is mediator) | −0.138 | 0.043 | −0.234 | −0.065 |
PDA = percent days abstinent, DPDD = drinks per drinking day, BDI = beck depression inventory, AA = AA attendance, Coeff = coefficient, SE = standard error, LLCI = lower level of confidence interval, ULCI = upper level of confidence interval. All indirect effect values are completely standardized.
Moderated mediation—Aim 2/early follow-up (Analysis 3, 4)
We then entered a BDI categorical moderator variable (as a marker of the likely presence or absence of a depressive disorder diagnosis) into the mediation models (Figure 2). When we did so, none of the indirect effects via BDI for either category of depression and neither of the indices of moderated mediation were statistically significant for the two models tested, indicating that baseline depression severity did not moderate the degree to which BDI (6 months) mediated the relationship between AA attendance (3 months) and alcohol use (9 months). The interaction terms were not significant for either model for either path A or path B, indicating that the baseline BDI categorical variable did not moderate either the relationship between AA (3 months) and alcohol use 6 months) or BDI (6 months) or the relationship between BDI (6 months) and alcohol use (9 months), respectively (Table 4).
Table 4.
Results from moderated mediation analyses to examine whether baseline depression severity moderates the degree to which changes in depression mediate the effect of AA attendance on alcohol use outcomes at late follow-up (12, 18, 24 months; Fig. 2; Analysis 7, 8).
| PDA late with baseline depression severity moderator variable (n=194) | Coeff | SE | t | p |
|---|---|---|---|---|
| Path A (to BDI 18 months) | ||||
| BDI mod | 6.227 | 3.108 | 2.004 | 0.047 |
| BDI mod × AA 12 months | −15.811 | 7.644 | −2.068 | 0.040 |
| Path A (to PDA 18 months) | ||||
| BDI mod | −0.403 | 0.124 | −3.242 | 0.001 |
| BDI mod × AA 12 months | 0.712 | 0.284 | 2.507 | 0.013 |
| Path B (to PDA 24 months) | ||||
| BDI mod | 0.080 | 0.227 | 0.351 | 0.726 |
| BDI mod ×BDI 18 months | 0.001 | 0.006 | 0.209 | 0.835 |
| BDI mod × PDA 18 months | −0.055 | 0.139 | −0.396 | 0.692 |
|
|
||||
| Coeff | Boot SE | Boot LLCI | Boot ULCI | |
|
|
||||
| Indirect effect (BDI 18 months is mediator); minimal/mild sepression | 0.001 | 0.042 | −0.036 | 0.065 |
| Indirect effect (BDI 18 months is mediator); moderate/severe depression | −0.009 | 0.067 | −0.139 | 0.135 |
| Indirect effect (PDA 18 months is mediator); minimal/mild depression | 0.073 | 0.157 | −0.254 | 0.346 |
| Indirect effect (PDA 18 months is mediator); moderate/severe depression | 0.570 | 0.129 | 0.326 | 0.844 |
| Index of moderated mediation (BDI 18 months is mediator) | −0.009 | 0.072 | −0.155 | 0.132 |
| Index of moderated mediation (PDA 18 months is mediator) | 0.497 | 0.204 | 0.137 | 0.922 |
|
| ||||
| DPDD late with baseline depression severity moderator variable (n=183) | Coeff | SE | t | p |
|
| ||||
| Path A (to BDI 18 months) | ||||
| BDI mod | 6.157 | 3.115 | 1.977 | 0.050 |
| BDI mod ×AA 12 months | −15.868 | 7.628 | 2.080 | 0.039 |
| Path A (to DPDD 18 months) | ||||
| BDI mod | 0.447 | 0.475 | 0.942 | 0.602 |
| BDI mod × AA 12 months | −0.169 | 1.680 | −0.101 | 0.920 |
| Path B (to DPDD 24 months) | ||||
| BDI mod | 0.667 | 0.606 | 1.100 | 0.273 |
| BDI mod × BDI 18 months | 0.014 | 0.029 | 0.476 | 0.635 |
| BDI mod × DPDD 18 months | 0.117 | 0.192 | 0.610 | 0.542 |
|
|
||||
| Coeff | Boot SE | Boot LLCI | Boot ULCI | |
|
|
||||
| Indirect effect (BDI 18 months is mediator); minimal/mild depression | −0.0042 | 0.119 | −0.412 | 0.172 |
| Indirect effect (BDI 18 months is mediator); moderate/severe depression | 0.129 | 0.238 | −0.266 | 0.687 |
| Indirect effect (DPDD 18 months is mediator); minimal/mild depression | −1.094 | 0.758 | −2.806 | 0.156 |
| Indirect effect (DPDD 18 months is mediator); moderate/severe depression | −1.028 | 0.945 | −2.954 | 0.487 |
| Index of moderated mediation (BDI 18 months is mediator) | 0.133 | 0.262 | −0.301 | 0.733 |
| Index of moderated mediation (DPDD 18 months is mediator) | 0.066 | 1.180 | −2.282 | 2.389 |
BDI mod = Categorical BDI moderator variable, DPDD = drinks per drinking day, BDI = beck depression inventory, AA = AA attendance, Coeff = coefficient, SE = standard error, LLCI = lower level of confidence interval, ULCI = upper level of confidence interval; none of the paths for the analysis using percent days abstinent as the outcome were significant so these results are not reported in a table.
There were no significant interaction terms nor were the indices of moderated mediation significant for PDA or DPDD at early follow-up (Analyses 3,4) and so no table was created.
Post hoc mediation Analysis—late follow-up (Analysis 5, 6)
In the aforementioned analyses looking at the 3-, 6-, and 9-month follow-up time points, we supported our findings from previous work in Wilcox et al. (26), showing that AA attendance was associated with reductions in later depression, controlling for concurrent drinking (26). Since our previous analysis included all time points (baseline to 24 months) and did not look at early and late time points separately, we wanted to explore whether or not changes in depression mediated the effect of AA on alcohol use.
As seen at early follow-up, at late follow-up, AA (12 month) was significantly associated with alcohol use (18 months) for PDA (p = 0.009, b = 0.397, t = 2.627) and at a trend level for DPDD (p = 0.064, b = −1.478, t = −1.864). In addition, AA (12 months) was significantly associated with BDI (18 months) for PDA (p = 0.047, b = −7.947, t = −2.004) and at a trend level for DPDD (p = 0.053, b = 7.801, t = −1.945) (path A; Figure 1), supporting previous findings from Wilcox et al. (26). However, BDI (18 months) was not significantly associated with alcohol use (24 months) (path B; Figure 1) for either DPDD or PDA, and the indirect effects via BDI were not significant, indicating that at late follow-up, BDI (18 months) did not mediate the effects of AA (12 month) on alcohol use (24 months) (Table 3).
Table 3.
Results from analyses to examine whether changes in depression mediate the effect of AA attendance on alcohol use outcomes at late follow-up (12, 18, 24 months; Fig. 1; Analysis 5, 6).
| PDA late (n = 183) | Coeff | SE | t | p |
|---|---|---|---|---|
| Path A (to BDI 18 months) | ||||
| AA 12 months | −7.947 | 3.966 | −2.004 | 0.047 |
| PDA baseline | 0.134 | 2.114 | 0.064 | 0.949 |
| Path A (to PDA 18 months) | ||||
| AA 12 months | 0.397 | 0.151 | 2.627 | 0.009 |
| BDI baseline | −0.004 | 0.003 | −1.779 | 0.077 |
| Path B (to PDA 24 months) | ||||
| BDI 18 months | 0.000 | 0.003 | 0.080 | 0.937 |
| AA 12 months | 0.067 | 0.097 | 0.691 | 0.490 |
| BDI baseline | 0.001 | 0.003 | 0.169 | 0.866 |
| Total effect (to PDA 24 months) | ||||
| AA 12 months | 0.351 | 0.131 | 2.680 | 0.008 |
| BDI baseline | −0.003 | 0.003 | −0.839 | 0.403 |
|
|
||||
| Coeff | Boot SE | Boot LLCI | Boot ULCI | |
|
|
||||
| Indirect Effect (BDI 18 months is mediator) | −0.006 | 0.103 | −0.293 | 0.159 |
| Indirect effect (PDA 18 months is mediator) | 0.137 | 0.050 | 0.033 | 0.234 |
|
| ||||
| DPDD late (n=183) | Coeff | SE | t | p |
|
| ||||
| Path A (to BDI 18 months) | ||||
| AA 12 months | 7.801 | 4.010 | −1.945 | 0.053 |
| DPDD baseline | −0.109 | 0.486 | −0.225 | 0.823 |
| Path A (to DPDD 18 months) | ||||
| AA 12 months | −1.478 | 0.793 | −1.864 | 0.064 |
| BDI baseline | 0.029 | 0.012 | 2.417 | 0.017 |
| Path B (to DPDD 24 months) | ||||
| BDI 18 months | −0.004 | 0.012 | −0.362 | 0.718 |
| AA 12 months | −0.356 | 0.807 | −0.441 | 0.660 |
| BDI baseline | 0.006 | 0.011 | 0.570 | 0.570 |
| Total effect (to DPDD 24 months) | ||||
| AA 12 months | −1.358 | 0.730 | −1.860 | 0.065 |
| BDI baseline | 0.024 | 0.012 | 2.021 | 0.045 |
|
|
||||
| Coeff | Boot SE | Boot LLCI | Boot ULCI | |
|
|
||||
| Indirect effect (BDI 18 months is mediator) | −0.004 | 0.012 | −0.015 | 0.034 |
| Indirect effect (DPDD 18 months is mediator | −0.122 | 0.066 | −0.257 | 0.001 |
PDA = percent days abstinent, DPDD = drinks per drinking day, BDI = beck depression inventory, AA = AA attendance, Coeff = coefficient, SE = standard error, LLCI = lower level of confidence interval, ULCI = upper level of confidence interval. All indirect effect values are completely standardized.
Post hoc moderated mediation analysis—late follow-up (Analysis 7, 8)
When the baseline BDI categorical variable was entered into the model, none of the indirect effects via BDI for either category of depression and neither of the indices of moderated mediation were statistically significant for the two models tested, indicating that baseline depression severity as a categorical variable did not moderate the degree to which BDI (18 months) mediated the relationship between AA (12 months) and alcohol use (24 months). For path A for the PDA analysis, both the BDI moderator variables and the interaction terms in the moderated mediation analysis were significant for AA (12 months) to both BDI (18 months) and PDA (18 months) (Table 4, Figure 2). For path A for the DPDD analysis, the BDI moderator variable and the interaction term for AA (12 months) to BDI (18 months) were significant (Table 4, Figure 2). Plotting slopes by group indicated that those with greater depression levels at baseline were more likely to show a decrease in BDI scores (18 months) with higher levels of AA attendance (12 months).
Discussion
This study investigated the relationship between AA attendance, depression, and alcohol consumption in individuals new to AA. In particular, our primary aim was to see whether the beneficial effects of AA attendance on drinking were mediated by effects on depression. Previous work has shown conflicting results using similar approaches at similar time points (26–28), and our findings help clarify things, somewhat. First, and most interestingly, we found that changes in depression mediated the beneficial effects of AA attendance at 3 months on drinking (DPDD) at 9 months controlling for concurrent drinking, consistent with Worley et al. (27), but in contrast to Kelly et al. (28). Our results were in support of our hypothesis, given that our sample was more similar to that of Worley et al. (27) than that of Kelly et al. (28) in terms of baseline depression levels. By contrast, in our sample, for PDA, the indirect effects were not significant, although they were still in the expected directions; changes in depression appeared to have a greater effect on the quantity consumed, rather than the decision to drink or not drink on a particular day. Other related work has also found that drinking mediated the relationship between AA and later drinking (19), and that the effect was stronger for DPDD.
We also hypothesized that baseline depression severity would moderate the indirect effect, but this hypothesis was not supported. Had it been supported, this would have indicated that differences in depression levels were driving the differences in results between the three studies. The absence of an observed effect could have resulted from the fact that BDI scores are fluid in this population and that a single time point measurement of BDI (our dichotomous moderator variable) is not a reliable marker of the presence or absence of a depressive syndrome. An alternative explanation for the differences lies in the variability in rates of AA attendance. Namely, our sample and that of Worley et al. (27) had higher AA attendance frequency than that of Kelly et al. (28); in our sample, rates were 29%, 19%, and 15% of days attending AA meetings during the preceding assessment periods at 3, 6, and 9 months, respectively (26), whereas in Kelly et al. (28) participants had minimal AA attendance. Moreover, a clear majority of the participants in Wilcox et al. (26) attended AA throughout the 24 months and, in the Worley et al. (27) study, participants reported, on average, attending more than 10 AA meetings prior to the 3-month follow-up. By contrast, in Kelly et al. (28) study, a majority of the outpatient participants did not attend AA during any follow-up and, by the 9-month follow-up, the percent of outpatient MATCH participants reporting any AA attendance had declined to 29%. The absence of mediation in the Kelly et al. (28) study may have occurred because participants had significantly less overall exposure to AA.
Although we used different methods than we had used in our previous paper (26), we still observed that AA attendance was associated with reductions in later depressive symptoms, controlling for concurrent drinking (path A; Figures 1 and 2). Moreover, we obtained further detail about the time points at which these effects were stronger (early follow-up) and in which populations (greater baseline depression levels for late follow-up). One possible reason that baseline depression severity did not moderate the relationship between AA attendance and later depression at early follow-up is that there was more room for improvement in all individuals, and due to the powerful effect of novelty, otherwise known as the “pink cloud” by AA attendees early in their AA exposure. At late follow-up, there may have been a stronger effect for those with greater depression at baseline, perhaps because they were the individuals for whom depression was not tightly linked with alcohol consumption, and who took longer to improve in their depressive symptom levels. Finally, that those with moderate or severe depression scores at baseline benefited even more at late follow-up than those with minimal or mild depression also supports findings in the literature that individuals with co-occurring psychiatric issues are just as likely to benefit from AA (11,39), and that drinking reduction improves chances of recovery from psychiatric illness.
Negative affect has long been considered a trigger for drinking and is considered a reasonable target for AUD treatment both within the AA literature (25) and treatment literature at large (40). This is supported by studies showing that compulsive alcohol use is driven by negative reinforcement (41), that people with AUD report drinking to relieve negative affect (42–44), that depression precedes relapse and is associated with greater drinking in individuals with AUD seeking treatment (45–49), and that treatments targeting negative affect and emotion regulation result in improvements in drinking (42,50). On the other hand, previous work has also shown that antidepressants in individuals with AUD but without depression are not effective at reducing drinking (51), and has shown a minimal role of depression in predicting later drinking (52). Our results supported the possibility that changes in negative affect (depression) do indeed mediate the effects of AA on later drinking, that this effect occurs above and beyond the effect of AA on drinking (for DPDD at early follow-up), and that improving negative affect is a reasonable treatment target.
One limitation of our study has to do with the fact that we only had a single measurement tool, the BDI, for negative affect. Although anger has been explored as a mediator of AA’s effect on drinking (53), to our knowledge, neither anxiety nor irritability has been. Furthermore, we had some limitations to our analysis methods. For one, we only analyzed subjects with complete data, which could have limited our power to detect effects and may have caused us to have null effects at late follow-up, for example. Second, although lagging the time points in our analyses for the independent, mediator, and dependent variables was a strength in our study in terms of being able to make inferences about causality, latent growth curve modeling would have allowed us to include all time points and may have had more sensitivity to detect effects (54). Finally, this is an observational cohort study rather than, say, a randomized trial targeting depression or assigning individuals to degrees of AA attendance frequency, and therefore, causality cannot be definitively attributed to the independent variable or mediator in such a design; associations could have been driven by unmeasured variables.
Conclusions
In conclusion, we observed that changes in depression mediated the effects of AA attendance on later drinking (DPDD) at early follow-up consistent with some but not all studies. However, baseline depression severity did not moderate the indirect effect and therefore did not provide support to the hypothesis that baseline depression differences were driving the differences between studies. Importantly, however, these findings have clinical significance by increasing support for models that ameliorating negative affect may help to reduce alcohol use in individuals with AUD and that encouraging AA attendance may be one way to achieve drinking reduction via this mechanism.
Supplementary Material
Acknowledgments
Funding
This research was supported by National Institute on Alcohol Abuse and Alcoholism (NIAAA) Grants K02-AA00326 and R01-AA014197. CEW is supported by NIA-AA Grant K23-AA021156. JST is supported by NIAAA Grant K24-AA021157. The views expressed are those of the authors and do not necessarily represent the views of the NIAAA.
Footnotes
Disclosure statement
The authors report no relevant financial conflicts.
References
- 1.Tonigan JS, Toscova R, Miller WR. Meta-analysis of the literature on Alcoholics Anonymous: sample and study characteristics moderate findings. J Stud Alcohol. 1996;57:65–72. doi: 10.15288/jsa.1996.57.65. [DOI] [PubMed] [Google Scholar]
- 2.Kelly JF, Stout RL, Magill M, Tonigan JS, Pagano ME. Spirituality in recovery: a lagged mediational analysis of alcoholics anonymous’ principal theoretical mechanism of behavior change. Alcohol Clin Exp Res. 2011;35:454–463. doi: 10.1111/j.1530-0277.2010.01362.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kelly JF, Yeterian JD. The role of mutual-help groups in extending the framework of treatment. Alcohol Res Health. 2011;33:350–355. [PMC free article] [PubMed] [Google Scholar]
- 4.Magill M, Kiluk BD, McCrady BS, Tonigan JS, Longabaugh R. Active ingredients of treatment and client mechanisms of change in behavioral treatments for alcohol use disorders: progress 10 years later. Alcohol Clin Exp Res. 2015;39:1852–1862. doi: 10.1111/acer.12848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dermatis H, Galanter M. The role of twelve-step-related spirituality in addiction recovery. J Relig Health. 2015 doi: 10.1007/s10943-015-0019-4. [DOI] [PubMed] [Google Scholar]
- 6.Humphreys K, Blodgett JC, Wagner TH. Estimating the efficacy of Alcoholics Anonymous without self-selection bias: an instrumental variables re-analysis of randomized clinical trials. Alcohol Clin Exp Res. 2014;38:2688–2694. doi: 10.1111/acer.12557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Magura S, McKean J, Kosten S, Tonigan JS. A novel application of propensity score matching to estimate Alcoholics Anonymous’ effect on drinking outcomes. Drug Alcohol Depend. 2013;129:54–59. doi: 10.1016/j.drugalcdep.2012.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Humphreys K, Phibbs CS, Moos RH. Addressing self-selection effects in evaluations of mutual help groups and professional mental health services: an introduction to two-stage sample selection models. Eval Program Plann. 1996:19301–19308. [Google Scholar]
- 9.Tonigan JS, Martinez-Papponi B, Hagler KJ, Greenfield BL, Venner KL. Longitudinal study of urban American Indian 12-step attendance, attrition, and outcome. J Stud Alcohol Drugs. 2013;74:514–520. doi: 10.15288/jsad.2013.74.514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Laudet AB, Cleland CM, Magura S, Vogel HS, Knight EL. Social support mediates the effects of dual-focus mutual aid groups on abstinence from substance use. Am J Community Psychol. 2004;34:175–185. doi: 10.1007/s10464-004-7413-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bogenschutz MP. 12-step approaches for the dually diagnosed: mechanisms of change. Alcohol Clin Exp Res. 2007;31:64s–66s. doi: 10.1111/j.1530-0277.2007.00496.x. [DOI] [PubMed] [Google Scholar]
- 12.Hillhouse MP, Fiorentine R. 12-step program participation and effectiveness: do gender and ethnic differences exist? J Drug Issues. 2001;31:767–780. [Google Scholar]
- 13.Kidney CA, Alvarez J, Jason LA, Ferrari JR, Minich L. Residents of mutual help recovery homes, characteristics and outcomes: comparison of four US ethnic subgroups. Drugs. 2011;18:32–39. doi: 10.3109/09687630903440022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zemore SE, Subbaraman M, Tonigan JS. Involvement in 12-step activities and treatment outcomes. Subst Abuse. 2013;34:60–69. doi: 10.1080/08897077.2012.691452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tonigan JS, Rice SL. Is it beneficial to have an alcoholics anonymous sponsor? Psychol Addict Behav. 2010;24:397–403. doi: 10.1037/a0019013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Witbrodt J, Kaskutas LA. Does diagnosis matter? Differential effects of 12-step participation and social networks on abstinence. Am J Drug Alcohol Abuse. 2005;31:685–707. doi: 10.1081/ada-68486. [DOI] [PubMed] [Google Scholar]
- 17.Bond J, Kaskutas LA, Weisner C. The persistent influence of social networks and alcoholics anonymous on abstinence. J Stud Alcohol. 2003;64:579–588. doi: 10.15288/jsa.2003.64.579. [DOI] [PubMed] [Google Scholar]
- 18.Kelly JF, Stout RL, Magill M, Tonigan JS. The role of Alcoholics Anonymous in mobilizing adaptive social network changes: a prospective lagged mediational analysis. Drug Alcohol Depend. 2011;114:119–126. doi: 10.1016/j.drugalcdep.2010.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kelly JF, Hoeppner B, Stout RL, Pagano M. Determining the relative importance of the mechanisms of behavior change within Alcoholics Anonymous: a multiple mediator analysis. Addiction. 2012;107:289–299. doi: 10.1111/j.1360-0443.2011.03593.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tonigan JS, Rynes KN, McCrady BS. Spirituality as a change mechanism in 12-step programs: a replication, extension, and refinement. Subst Use Misuse. 2013;48:1161–1173. doi: 10.3109/10826084.2013.808540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Connors GJ, Tonigan JS, Miller WR, Group MR. A longitudinal model of intake symptomatology, AA participation and outcome: retrospective study of the project MATCH outpatient and aftercare samples. J Stud Alcohol. 2001;62:817–825. doi: 10.15288/jsa.2001.62.817. [DOI] [PubMed] [Google Scholar]
- 22.Bogenschutz MP, Tonigan JS, Miller WR. Examining the effects of alcoholism typology and AA attendance on self-efficacy as a mechanism of change. J Stud Alcohol. 2006;67:562–567. doi: 10.15288/jsa.2006.67.562. [DOI] [PubMed] [Google Scholar]
- 23.McKellar J, Ilgen M, Moos BS, Moos R. Predictors of changes in alcohol-related self-efficacy over 16 years. J Subst Abuse Treat. 2008;35:148–155. doi: 10.1016/j.jsat.2007.09.003. [DOI] [PubMed] [Google Scholar]
- 24.Moos RH. Theory-based processes that promote the remission of substance use disorders. Clin Psychol Rev. 2007;27:537–551. doi: 10.1016/j.cpr.2006.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Alcoholics Anonymous. 4. New York, NY: Alcoholics Anonymous World Services, Inc.; 2002. [Google Scholar]
- 26.Wilcox CE, Pearson MR, Tonigan JS. Effects of long-term AA attendance and spirituality on the course of depressive symptoms in individuals with alcohol use disorder. Psychol Addict Behav. 2015;29:382–391. doi: 10.1037/adb0000053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Worley MJ, Tate SR, Brown SA. Mediational relations between 12-Step attendance, depression and substance use in patients with comorbid substance dependence and major depression. Addiction. 2012;107:1974–1983. doi: 10.1111/j.1360-0443.2012.03943.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kelly JF, Stout RL, Magill M, Tonigan JS, Pagano ME. Mechanisms of behavior change in alcoholics anonymous: does Alcoholics Anonymous lead to better alcohol use outcomes by reducing depression symptoms? Addiction. 2010;105:626–636. doi: 10.1111/j.1360-0443.2009.02820.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Beck AT, Steer R, Brown GK. Manual for the Beck Depression Inventory-II. 1996 [Google Scholar]
- 30.Zimmerman M, Martinez JH, Young D, Chelminski I, Dalrymple K. Severity classification on the Hamilton Depression Rating Scale. J Affect Disord. 2013;150:384–388. doi: 10.1016/j.jad.2013.04.028. [DOI] [PubMed] [Google Scholar]
- 31.American Psychiatric Association. Diagnostic and statistical manual of mental disorders (DSM-IV-TR) 4. Washington, DC: American Psychiatric Publishing; 2000. [Google Scholar]
- 32.First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Patient Edition With Psychotic Screen (SCID-I/P W/ PSY SCREEN) 2002 [Google Scholar]
- 33.Tonigan JS, Miller WR, Brown JM. The reliability of Form 90: an instrument for assessing alcohol treatment outcome. J Stud Alcohol. 1997;58:358–364. doi: 10.15288/jsa.1997.58.358. [DOI] [PubMed] [Google Scholar]
- 34.Efron B, Tibshirani R. An introduction to the bootstrap. Boca Raton, FL: Chapman & Hall/CRC; 1993. [Google Scholar]
- 35.Hayes AF. Introduction to mediation, moderation, and conditional process analysis. The Guilford Press; New York: 2013. [Google Scholar]
- 36.Hayes AF. Model templates for PROCESS for SPSS and SAS, 2013–2015. Retrieved from http://processmacro.org/download.html.
- 37.Hayes AF, Cai L. Using heteroskedasticity-consistent standard error estimators in OLS regression: an introduction and software implementation. Behav Res Methods. 2007;39:709–722. doi: 10.3758/bf03192961. [DOI] [PubMed] [Google Scholar]
- 38.Preacher KJ, Hayes AF. SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behav Res Methods Instrum Comput. 2004;36:717–731. doi: 10.3758/bf03206553. [DOI] [PubMed] [Google Scholar]
- 39.Bergman BG, Greene MC, Hoeppner BB, Slaymaker V, Kelly JF. Psychiatric comorbidity and 12-step participation: a longitudinal investigation of treated young adults. Alcohol Clin Exp Res. 2014;38:501–510. doi: 10.1111/acer.12249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Marlatt GA, George WH. Relapse prevention: introduction and overview of the model. Br J Addict. 1984;79:261–273. doi: 10.1111/j.1360-0443.1984.tb00274.x. [DOI] [PubMed] [Google Scholar]
- 41.Koob G. A role for brain stress systems in addiction. Neuron. 2008;59:11–34. doi: 10.1016/j.neuron.2008.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Stasiewicz PR, Bradizza CM, Schlauch RC, Coffey SF, Gulliver SB, Gudleski GD, Bole CW. Affect regulation training (ART) for alcohol use disorders: Development of a novel intervention for negative affect drinkers. J Subst Abuse Treat. 2013;45:433–443. doi: 10.1016/j.jsat.2013.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wilcox CE, Pommy JM, Adinoff B. Neural circuitry of impaired emotion regulation in substance use disorders. Am J Psychiatry. 2016;173(4):344–361. doi: 10.1176/appi.ajp.2015.15060710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Bradizza CM, Stasiewicz PR. Qualitative analysis of high-risk drug and alcohol use situations among severely mentally ill substance abusers. Addict Behav. 2003;28:157–169. doi: 10.1016/s0306-4603(01)00272-6. [DOI] [PubMed] [Google Scholar]
- 45.Worley MJ, Trim RS, Roesch SC, Mrnak-Meyer J, Tate SR, Brown SA. Comorbid depression and substance use disorder: longitudinal associations between symptoms in a controlled trial. J Subst Abuse Treat. 2012;43:291–302. doi: 10.1016/j.jsat.2011.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ilgen M, Moos R. Deterioration following alcohol-use disorder treatment in project MATCH. J Stud Alcohol. 2005;66:517–525. doi: 10.15288/jsa.2005.66.517. [DOI] [PubMed] [Google Scholar]
- 47.Gamble SA, Conner KR, Talbot NL, Yu Q, Tu XM, Connors GJ. Effects of pretreatment and posttreatment depressive symptoms on alcohol consumption following treatment in Project MATCH. J Stud Alcohol Drugs. 2010;71:71–77. doi: 10.15288/jsad.2010.71.71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kodl MM, Fu SS, Willenbring ML, Gravely A, Nelson DB, Joseph AM. The impact of depressive symptoms on alcohol and cigarette consumption following treatment for alcohol and nicotine dependence. Alcohol Clin Exp Res. 2008;32:92–99. doi: 10.1111/j.1530-0277.2007.00556.x. [DOI] [PubMed] [Google Scholar]
- 49.Curran GM, Flynn HA, Kirchner J, Booth BM. Depression after alcohol treatment as a risk factor for relapse among male veterans. J Subst Abuse Treat. 2000;19:259–265. doi: 10.1016/s0740-5472(00)00107-0. [DOI] [PubMed] [Google Scholar]
- 50.Berking M, Margraf M, Ebert D, Wupperman P, Hofmann SG, Junghanns K. Deficits in emotion-regulation skills predict alcohol use during and after cognitive-behavioral therapy for alcohol dependence. J Consult Clin Psychol. 2011;79:307–318. doi: 10.1037/a0023421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wilcox CE, Bogenschutz MB. Psychopharmacology for addictions. In: McCrady BS, Epstein EE, editors. Addictions: a comprehensive guidebook. New York, NY: Oxford University Press; 2013. pp. 526–550. [Google Scholar]
- 52.Janowsky DS, Boone A, Morter S, Howe L. Personality and alcohol/substance-use disorder patient relapse and attendance at self-help group meetings. Alcohol Alcohol. 1999;34:359–369. doi: 10.1093/alcalc/34.3.359. [DOI] [PubMed] [Google Scholar]
- 53.Kelly JF, Stout RL, Tonigan JS, Magill M, Pagano ME. Negative affect, relapse, and Alcoholics Anonymous (AA): does AA work by reducing anger? J Stud Alcohol Drugs. 2010;71:434–444. doi: 10.15288/jsad.2010.71.434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Selig JP, Preacher KJ. Mediation models for longitudinal data in developmental research. Res Hum Dev. 2009;6:144–164. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.