Abstract
Background
We examined the contribution of patient, physician, and environmental factors to demographic and health variation in colonoscopy follow-up after positive Fecal Occult Blood Test/Fecal Immunochemical Test (FOBT/FIT+) screening.
Methods
We identified 76,243 FOBT/FIT+ cases from 120 Veterans Health Administration (VHA) facilities between 8/16/09–3/20/11 and followed them for 6 months. We identified patient demographic (race/ethnicity, gender, age, marital status) and health characteristics (comorbidities); physician characteristics (training level, whether primary care provider) and behaviors (inappropriate FOBT/FIT screening); and environmental factors (geographic access, facility type) from VHA administrative records. We estimated patient behaviors (refusal, private sector colonoscopy use) with statistical text mining conducted on clinic notes. We estimated follow-up predictors and adjusted rates using hierarchical logistic regression.
Results
Roughly 50% completed a colonoscopy at a VHA facility within 6 months. Age and comorbidity score were negatively associated with follow-up. Blacks were more likely to receive follow-up than Whites. Environmental factors attenuated but did not fully account for these differences. Patient behaviors (refusal, private sector colonoscopy use), and physician behaviors (inappropriate screening) fully accounted for the small reverse race disparity, and attenuated variation by age and comorbidity score. Patient behaviors (refusal and private sector colonoscopy use) contributed more to variation in follow-up rates than physician behaviors (inappropriate screening).
Conclusions
In the VHA, Blacks are more likely to receive colonoscopy follow-up for FOBT/FIT+ results than Whites, and follow-up rates markedly decline with advancing age and comorbidity burden. Patient and physician behaviors explain race variation in follow-up rates and contribute to variation by age and comorbidity burden.
Keywords: Early Detection of Cancer, Diagnostic Services, Mass Screening, Colorectal Neoplasms, Colonoscopy, Health Services Accessibility, Veterans Health
BACKGROUND
Colorectal cancer was diagnosed in an estimated 134,490 individuals and resulted in an estimated 49,190 deaths in 2016.1 Routine screening can reduce the burden of this disease, and the United States Preventive Services Task Force recommends a number of screening modalities.2 Fecal occult blood test and fecal immunochemical test-based (FOBT/FIT) screening are common modalities in many settings, including the two largest health care systems in the United States (Kaiser Permanente and the Veterans Health Administration).3;4 However, the benefits of FOBT/FIT screening cannot be achieved unless positive results are followed by colonoscopy. Prior studies have documented gaps in colonoscopy follow-up rates among individuals with a positive FOBT/FIT (FOBT/FIT+), and in many settings less than 60% receive follow-up before they are due for repeat screening.5–10 Understanding the reasons for these gaps is essential for guiding development of effective strategies for closing them.
Prior studies have found lower rates of colonoscopy follow-up for FOBT/FIT+ associated with various demographic and health characteristics, including non-African American race,11 Hispanic ethnicity,12 female gender,12–14 increasing age,10;13;15;16 and comorbidities,10 but it is not clear whether these patterns are due to variation in patient behaviors (e.g., refusal), physician behaviors (e.g., potentially inappropriate screening among those with limited life expectancy or recent prior colonoscopy), or environmental factors such as geographic access to colonoscopy. Two studies found that 14–38% of patients lacking follow-up for FOBT/FIT+ results had documentation of refusal, comorbidity or a contraindication that would preclude follow-up testing,8;17 but one of these studies was limited to patients age 70 and older17 and neither examined demographic or health-related variation in reasons for lack of follow-up. Variation in patient refusal of treatment has been found to contribute to age and race differences in receipt of cancer therapy,18 but to our knowledge, no studies have examined whether refusal and potentially inappropriate screening contribute to demographic and health-related differences in colonoscopy follow-up for FOBT/FIT+ results.
This study addresses this gap by examining the contribution of patient behavior (refusal), physician behavior (potentially inappropriate FOBT/FIT screening), and environmental factors (access) to demographic and health variation in colonoscopy following a positive FOBT/FIT in a sample of adults age 50–85 receiving care at a VHA facility. We hypothesized that any observed differences in follow-up rates by patient age, race, and comorbidities would be explained by variation in refusal, inappropriate screening, and access.
METHODS
Setting and Participants
We identified patients receiving FOBT/FIT+ results from one of 120 eligible VHA facilities between 8/16/09–3/20/11 and followed them until 9/30/11 for colonoscopy completion or documentation of potentially valid reasons for not completing colonoscopy. As described previously,19 we identified FOBT/FIT+ results from VHA laboratory records, using the codes in Supplementary Material 1. We defined FOBT/FIT+ cases as any individual or multiple card series with one or more positive result cards. We restricted the sample to patients receiving FOBT/FIT+ results from facilities that conducted at least 1,400 FOBTs in 2009 to permit rigorous examination of facility-level variation in follow-up colonoscopy.19 We excluded patients if they were less than 50 or more than 85 years of age at the time of the FOBT/FIT+ result; had a diagnosis of colorectal cancer; or died during the follow-up interval. To minimize the number of cases with missing data, we also excluded patients that received their FOBT/FIT+ from a VHA Community Based Outpatient Clinic (CBOC) referring <70% of colonoscopies to one of the sampled facilities, or from a facility where >90% of cases were missing clinical notes data used to assess refusal and private sector colonoscopy use. Using these criteria, we identified 76,243 FOBT/FIT+ cases from 120 VHA facilities for the analysis (Figure 1).
Figure 1.
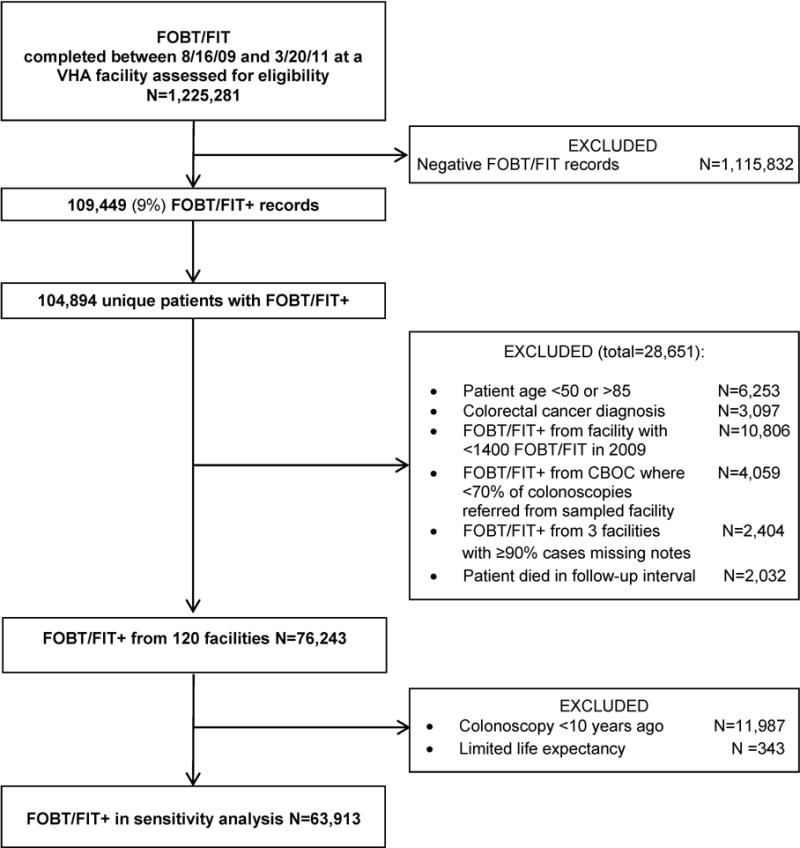
Subject Flowchart
Data sources and measures
The dependent measure for our analysis was a completed follow-up colonoscopy at a VHA facility within 6 months of the FOBT/FIT+ date. We used this follow-up window because, consistent with prior studies,10 most individuals in the VHA completing colonoscopy following FOBT/FIT+ results do so within 6 months. We identified completed colonoscopies from VHA administrative data using the codes in Supplementary Material 2.
Predictors
Guided by the Diagnostic Evaluation Model,20;21 we distinguish between patient, physician, and environmental predictors of follow-up. Patient factors examined consisted of: demographic and health characteristics, including race/ethnicity (Non-Hispanic White, Hispanic, Black, American Indian, Asian or Pacific Islander), gender, age (50–59, 60–64, 65–75, 76–85), and marital status (married, widowed, other); Charlson comorbidity score for the 1 year prior to the FOBT/FIT+ result (0, 1–2, 3 or higher); mental health diagnoses (psychiatric only, substance abuse only, dual diagnosis, or none); personal history of colorectal polyps or benign neoplasms (ICD-9 211.3–4, 569.0, v12.72); and behaviors (colonoscopy refusal, use of private sector colonoscopy for follow-up). We used Statistical Text Mining (STM) to identify documentation of refusal and private colonoscopy, using a validated algorithm, described previously.19 This algorithm searched consult, progress, primary care and clinical reminder notes entered during the follow-up interval for key phrases associated with refusal or private sector colonoscopy use, and assigned each FOBT+/FIT+ case with two continuous scores: one corresponding to the probability that their notes contain documentation of refusal, and one corresponding to the probability that their notes contained documentation of private sector colonoscopy use. We used the probabilities from STM to assign refusal and private sector colonoscopy status to each individual without VHA follow-up. The distributions for these probabilities were disparate and tended toward extreme values. Our intent was to gauge the sensitivity of the initial findings to these unobserved outcomes; so rather than performing a complex Monte Carlo simulation study, we classified notes with a refusal probability ≥0.60 as indicating the patient refused follow-up and notes with a private sector colonoscopy probability ≥0.93 as indicating the patient pursued private sector colonoscopy. We selected these thresholds based on the probability distributions (see Figures S1, S2).
Physician factors
Physician factors examined included: physician characteristics, such as FOBT/FIT ordering provider training (physician, nurse practitioner or physician assistant, resident, nurse or other staff), and whether the ordering physician was the patient’s primary care provider; and the physician behavior of potentially inappropriate screening (i.e., patient has limited life expectancy, VHA colonoscopy in prior 10 years).
Environmental factors
Environmental factors examined consisted of geographic access indicators, including residence (urban, rural) and drive time to the nearest VHA specialty care facility (<30, 30–60, >60 minutes), and FOBT/FIT ordering facility type (specialty care or CBOC). We used administrative data to identify all predictors.
Analysis
We used hierarchical regression, modeling the odds of completing follow-up colonoscopy within six months to identify individual-level predictors of follow-up. These models incorporated random effects for facility and fixed effects for the measures in Table 1. To select variables for the final model, we used a bootstrap resampling model selection algorithm.22 This involved constructing 500 bootstrap samples, using a forward selection algorithm with each individual sample to develop a bootstrapped model, and retaining predictors selected in 90% of these models for inclusion in the final model. From this final model we constructed model-based odds ratios and least square mean follow-up estimates for each measure (using the observed marginal distributions of other covariates). We did not hypothesize interactions between predictors and therefore did not include interaction terms in the model.
TABLE 1.
Participant Characteristics (N=76,243)
| Characteristics | N (%) |
|---|---|
| Patient characteristics | |
|
| |
| Race/ethnicity | |
| Asian/Pacific Islander | 1,013 (1.33) |
| Black | 13,618 (17.86) |
| Native American | 644 (0.84) |
| White, Non-Hispanic | 49,692 (65.18) |
| Hispanic | 4,097 (5.37) |
| Unknown | 7,179 (9.42) |
| Gender | |
| Male | 73,487 (96.39) |
| Female | 2,756 (3.61) |
| Missing | 0 |
| Age | |
| 50–59 | 22,827 (29.94) |
| 60–64 | 22,691 (29.76) |
| 65–75 | 22,106 (28.99) |
| 76–85 | 8,619 (11.3) |
| Missing | 0 |
| Marital status | |
| Married | 40,706 (53.57) |
| Widowed | 4,313 (5.68) |
| Others | 30,964 (40.75) |
| Missing | 260 |
| Charlson score | |
| 0 | 23,260 (30.51) |
| 1 | 18,608 (24.41) |
| 2 | 13,572 (17.8) |
| 3+ | 20,803 (27.29) |
| Missing | 0 |
| Mental health diagnoses | |
| None | 24,513 (32.15) |
| Psychiatric only | 19,791 (25.96) |
| Substance abuse only | 11,875 (15.58) |
| Both | 20,064 (26.32) |
| Missing | 0 |
| Polyps diagnosis | |
| NO | 60,723 (79.64) |
| YES | 15,520 (20.36) |
| Missing | 0 |
|
| |
| Physician characteristics | |
|
| |
| FOBT ordering provider is primary care provider | |
| NO | 21,307 (27.95) |
| YES | 54,936 (72.05) |
| Missing | 0 |
| FOBT ordering provider type | |
| Physician | 54,825 (71.92) |
| Non-physician (NP, PA) | 17,408 (22.84) |
| Resident | 2,430 (3.19) |
| other | 1,563 (2.05) |
| Missing | 17 (0.02) |
|
| |
| Physician behaviors (Inappropriate screening) | |
|
| |
| Patient has limited Life Expectancy | |
| NO | 75,801 (99.42) |
| YES | 442 (0.58) |
| Missing | 0 |
| Patient had VHA Colonoscopy <10 years ago | |
| NO | 64,256 (84.28) |
| YES | 11,987 (15.72) |
| Missing | 0 |
|
| |
| Environmental factors | |
|
| |
| Residence | |
| Rural/highly rural | 38,423 (50.58) |
| Urban | 37,539 (49.42) |
| Missing | 281 |
| Drive time to specialty care facility | |
| >60 minutes | 31,756 (41.8) |
| 30–60 minutes | 17,621 (23.2) |
| <30 minutes | 26,591 (35) |
| Missing | 275 |
| Ordering facility type | |
| Specialty care facility | 33,141 (43.47) |
| CBOC | 43,102 (56.53) |
| Missing | 0 |
To assess the sensitivity of estimates to patient and physician behaviors that might explain lack of VHA follow-up, we reran our models excluding cases potentially screened inappropriately (n=343 with limited life expectancy, and n=11,987 with a prior colonoscopy), and treating those refusing (n=7,708), pursuing private sector colonoscopy (n=8,666) or both (n=2,510) as having received follow-up.
This study was reviewed and approved by the institutional review boards at the Minneapolis and Boston VA Healthcare Systems.
RESULTS
Patients were primarily non-Hispanic white (65%) men (96%) age 50–75 (89%) (Table 1). Roughly half (54%) were married, 27% had three or more comorbidities, 68% had a mental health or substance abuse diagnosis, and 20% had a personal history of polyps. The majority had their FOBT/FIT ordered by a physician (72%) who was their primary care provider (72%). Less than 1% had limited life expectancy, and 16% had a VHA colonoscopy in the prior 10 years. Roughly half (51%) lived in rural areas, 42% lived more than 60 minutes away from the nearest VHA specialty care facility, and 57% had their FOBT/FIT ordered at a CBOC.
Among the 76,243 FOBT/FIT+ cases identified, 38,005 (50%) completed a colonoscopy at a VHA facility within 6 months; 7,294 (10%) did not complete a colonoscopy but were potentially inappropriately screened, due either to limited life expectancy (0.27%) or a recent prior colonoscopy at a VHA facility (9.29%); up to 13,863 (18%) did not complete a colonoscopy but either refused a VHA colonoscopy (7%), pursued a private sector colonoscopy (8%), or both (3%); and at least 17,010 (22%) had no reason documented for not completing a colonoscopy.
With the exception of gender, residence, and provider type, all factors examined were significantly associated with follow-up rates in univariate models (Table 2). Patient factors retained in the multivariate model included: race/ethnicity, age, personal history of polyps, and comorbidity score. Age (odds ratios 2.01–3.10 for the younger versus oldest age category) was a strong independent predictor, corresponding to follow-up rate differences as large as 29 percentage points. Personal history of polyps (odds ratio 2.57) was positively associated, and the Charlson score negatively associated with follow-up. Those with a Charlson score of 3+ had follow-up rates 5 percentage points lower than those with a score of zero (46 versus 51%). We found a small reverse race disparity, with Blacks demonstrating follow-up rates 4 percentage points higher than Whites.
Table 2.
Odds ratios, 95% confidence intervals, and follow-up rate estimates from univariate and multivariate hierarchical logistic regression models.
| Univariate | Multivariate | |||
|---|---|---|---|---|
| Odds ratio (95% CI) | Follow-up % | Odds ratio (95% CI) | Follow-up % | |
| Patient characteristics | ||||
| Race White | 1.00 | 48 | 1.00 | 49 |
| Asian/PI | 1.07 (0.94–1.22) | 49 | 1.05 (0.92–1.19) | 50 |
| Black | 1.33 (1.28–1.39) | 55 | 1.19 (1.14–1.25) | 53 |
| Hispanic | 1.17 (1.08–1.27) | 52 | 1.09 (1.00–1.19) | 51 |
| Native American | 1.18 (1.00–1.38) | 52 | 1.12 (0.95–1.32) | 51 |
| Unknown | 0.83 (0.78–0.87) | 43 | 0.81 (0.77–0.86) | 43 |
| Gender Female | 1.00 | 48 | — | — |
| Male | 1.02 (0.95–1.11) | 49 | — | — |
| Age 76–85 | 1.00 | 27 | 1.00 | 29 |
| 50–59 | 3.43 (3.24–3.62) | 56 | 3.10 (2.93–3.29) | 56 |
| 60–64 | 3.11 (2.94–3.28) | 54 | 2.89 (2.73–3.06) | 54 |
| 65–75 | 2.11 (2.0–2.24) | 44 | 2.01 (1.90–2.13) | 45 |
| Marital status Other | 1.00 | 51 | — | — |
| Married | 0.85 (0.83–0.88) | 47 | — | — |
| Widowed | 0.72 (0.67–0.76) | 43 | — | — |
| Mental Health dx - dual | 1.00 | 52 | — | — |
| None | 0.77 (0.75–0.80) | 45 | — | — |
| Psychiatric only | 0.87 (0.83–0.90) | 48 | — | — |
| Substance Abuse only | 0.99 (0.95–1.04) | 51 | — | — |
| Polyp No | 1.00 | 44 | 1.00 | 44 |
| Yes | 2.23 (2.15–2.32) | 64 | 2.57 (2.47–2.67) | 67 |
| Charlson 3+ | 1.00 | 43 | 1.00 | 46 |
| 0 | 1.50 (1.44–1.56) | 53 | 1.23 (1.18–1.28) | 51 |
| 1 | 1.35 (1.30–1.41) | 50 | 1.17 (1.12–1.22) | 50 |
| 2 | 1.24 (1.18–1.29) | 48 | 1.13 (1.08–1.19) | 49 |
| Physician characteristics | ||||
| Provider type other | 1.00 | 47 | — | — |
| Non-Physician (NP, PA) | 1.07 (0.96–1.20) | 49 | — | — |
| Physician | 1.09 (0.97–1.21) | 49 | – | — |
| Resident | 0.94 (0.82–1.08) | 45 | — | — |
| Ordering provider not PCP | 1.00 | 44 | 1.00 | 44 |
| Is PCP | 1.29 (1.24–1.33) | 50 | 1.29 (1.24–1.34) | 51 |
| Physician behaviors | ||||
| Limited life expectancy- no | 1.00 | 49 | — | — |
| Yes | 0.55 (0.45–0.68) | 34 | — | — |
| Colonoscopy <10 yrs Yes | 1.00 | 41 | 1.00 | 39 |
| No | 1.47 (1.41–1.53) | 50 | 1.66 (1.58–1.73) | 51 |
| Environmental factors | ||||
| Residence Urban | 1.00 | 49 | — | — |
| Rural | 0.97 (0.94–1.00) | 48 | — | — |
| Drive time >60 minutes | 1.00 | 46 | — | — |
| 30–60 | 1.17 (1.12–1.21) | 50 | — | — |
| <30 | 1.23 (1.19–1.30) | 51 | — | — |
| Ordering facility CBOC | 1.00 | 45 | 1.00 | 45 |
| Specialty care hospital | 1.26 (1.22–1.30) | 51 | 1.32 (1.28–1.36) | 52 |
Physician factors
Those whose FOBT/FIT was ordered by their primary care provider had follow-up rates that were 7 percentage points higher than those whose FOBT/FIT was not ordered by their primary care provider. Colonoscopy in the prior 10 years (odds ratio 1.66) was the only indicator of potentially inappropriate screening included in the multivariate model. Those with no prior colonoscopy in the past 10 years had a follow-up rate 12 percentage points higher than those with a prior colonoscopy (51 versus 39%, respectively).
Environmental factors
No geographic access measures were retained in the multivariate model, but those whose FOBT/FIT was ordered at a specialty care facility had follow-up rates that were 7 percentage points higher than those whose FOBT/FIT was ordered at a CBOC.
After excluding potentially inappropriately screened individuals and treating patients refusing colonoscopy or pursuing colonoscopy in the private sector as followed-up, the small differences by race/ethnicity attenuate further (Figure 2, Table S1), and the differences by age (Figure 3, Table S1) and Charlson score (Figure 4, Table S1) attenuate markedly. Patient behavior (refusals and private sector colonoscopy use) contributed more to the variation in follow-up rates by age, race, and Charlson score than physician behavior (inappropriate screening), although all three increased with age and Charlson score, and were more common among Whites than Blacks (Figures 2–4).
Figure 2.
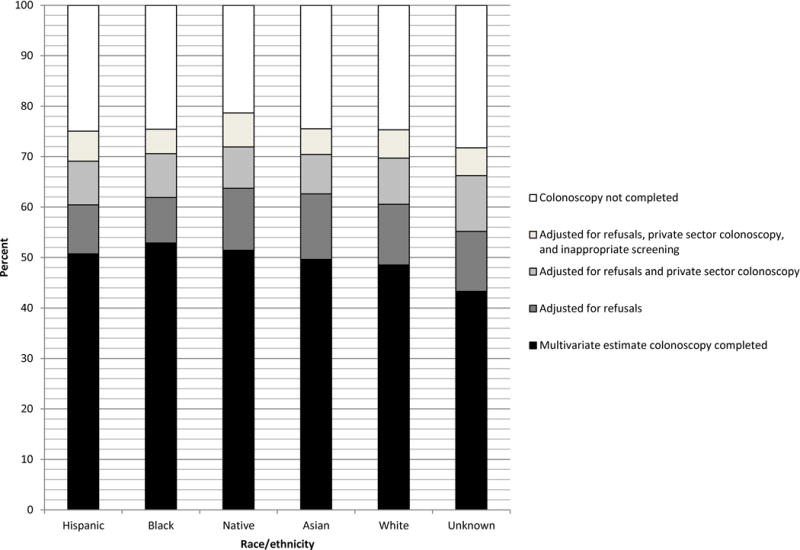
Multivariate and sensitivity-adjusted colonoscopy completion rates by race/ethnicity
Figure 3.
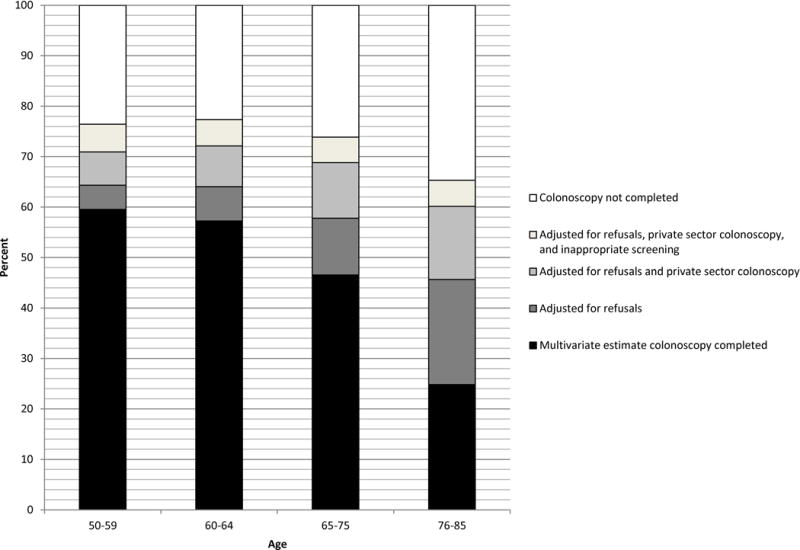
Multivariate and sensitivity-adjusted colonoscopy completion rates by age
Figure 4.
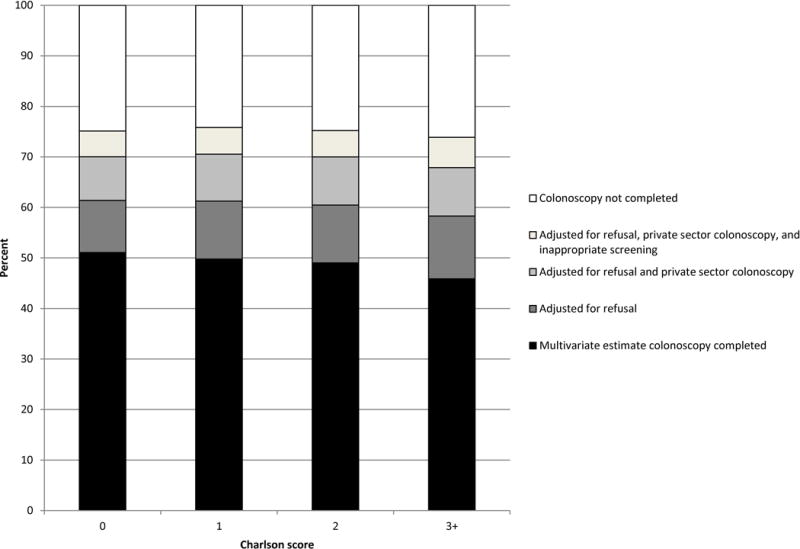
Multivariate and sensitivity-adjusted colonoscopy completion rates by Charlson score
DISCUSSION
We found that 50% of the FOBT/FIT+ cases completed a follow-up colonoscopy in the VHA within 6 months; that age and comorbidities were negatively associated with follow-up; and that Blacks were more likely to receive follow-up in the VHA than Whites. Multivariate models controlling for environmental factors, including geographic access, attenuated but did not fully account for these differences. Adjusting for patient behaviors (refusal, and private sector colonoscopy use), and physician behaviors (potentially inappropriate screening) fully accounted for the small reverse race disparity, and markedly attenuated variation by age and comorbidities.
The contribution of potentially inappropriate screening due to recent prior colonoscopy to follow-up rates we observed is consistent with findings from prior studies, including one that identified recent colonoscopy as a prevalent reason for failure to complete follow-up,12 and two that found a strong association between colonoscopy history and FOBT/FIT+ follow-up.15;16 As documented in prior studies conducted on samples age 50–75,23 potentially inappropriate screening due to limited life expectancy was relatively rare in our sample (<1%).17 The frequency of refusal among those failing to complete a colonoscopy we observed (14–21% depending on whether those who refused are combined with those who both refused and had private sector colonoscopy access) is similar to colonoscopy follow-up refusal rates reported in prior studies (range 7–26%).12;16;17;24;25
Although prior studies have documented lower rates of colorectal cancer screening26 and surveillance27 among racial and ethnic minority groups, findings regarding race/ethnic variation in colonoscopy follow-up for FOBT/FIT+ results are mixed. One prior study conducted in a community practice12 found lower follow-up rates among Hispanics, but most prior studies have either found no evidence of race/ethnic variation in follow-up,5;10;28 or higher follow-up among minorities.16;29;30 Additionally, in contrast with prior studies documenting higher refusal among Blacks for invasive procedures and treatments, including coronary angiography31–34 and revascularization,32;35 we found lower refusal rates among Blacks than Whites. This may in part reflect the fact that Blacks are more likely to rely solely on VHA care36–42, and therefore may be less likely to refuse due to access to private sector colonoscopy. The race variation in use of VHA care may be explained in part by well-documented race variation in income, education, and insurance coverage, all of which are positively associated with greater use of non-VHA care among Veterans.37;39;40
Our finding that age and comorbidities were negatively associated with follow-up is consistent with prior studies.5;10;13;16;24;43 Studies finding no significant association between follow-up and these factors either restricted the sample to the oldest age groups17 or excluded those over 75.6;12;15;44 It is not clear why the effects of age and comorbidity on follow-up were not fully explained by other patient characteristics, patient behaviors (refusal, private sector colonoscopy use), physician behaviors (inappropriate screening), or environmental factors. Possible explanations include: lower patient and provider motivation to aggressively pursue follow-up under circumstances of advanced age or severe comorbidity due to lower perceived benefits and greater perceived risks of colonoscopy; greater likelihood that those with advanced age and severe comorbidity experience acute health challenges and logistical barriers that compete with follow-up; or a failure to capture all refusal, private sector colonoscopy, and inappropriate screening with the measures employed.
This study has a number of strengths, including a large, nationally representative sample of patients and facilities; rigorous methodology for assessing the impact of inappropriate screening, refusal, and private sector colonoscopy use on variation in follow-up rates by patient demographic and health characteristics; and the ability to examine the association between environmental factors and follow-up rate estimates. However, we were not able to assess patient psychosocial reasons for lack of follow-up. Understanding the contribution of patient perspectives and experiences will likely be critical to developing effective interventions to improve follow-up rates. We also might have overestimated inappropriate screening, given that some consider FOBT/FIT screening conducted more than five years after a prior colonoscopy as clinically appropriate. Additionally, because we did not link our sample with private sector medical records, our assumption that patients pursuing colonoscopy in the private sector actually completed a colonoscopy might lead to overestimates of follow-up rates. However, the fact that another study found only 2% of patients not completing a VHA colonoscopy who said they were pursuing colonoscopy in the private sector lacked a Medicare claim for a colonoscopy17 suggests this overestimate is likely small. Finally, the VHA population is unique and may not generalize to other settings. However, as the largest integrated health care system in the US, the VHA population does generalize to a substantial number of individuals, including non-VHA Medicare beneficiary populations.45
CONCLUSIONS
In the VHA setting, Blacks are more likely to receive colonoscopy follow-up for FOBT/FIT+ results than Whites, and follow-up rates significantly decline with advancing age and comorbidity burden. Patient behaviors (refusal, private sector colonoscopy use) and physician behaviors (inappropriate screening) explain race/ethnicity variation in follow-up rates and contribute to variation by age and comorbidity burden.
IMPLICATIONS FOR PRACTICE
Our finding that geographic access metrics were not significant predictors of follow-up suggest that policies such as the Veteran Choice and Accountability Act, which expand geographic access for Veterans by purchasing care from private sector providers, may not fully address existing gaps in follow-up. Inappropriate screening is an important, modifiable physician behavioral barrier to improving follow-up rates, and future efforts to optimize follow-up would benefit from implementing methods to reliably exclude those with recent colonoscopy from clinical reminders and other tools designed to prompt physicians to initiate colorectal cancer screening. The VHA has a system in place for tracking patients with positive FOBT/FIT screens at the facility-level, but the extent to which this tool is used, and whether and how well non-VHA colonoscopies are tracked at the facility level is unknown. Future improvement efforts might seek to enhance functionality of this tool by assessing whether and how accurately non-VHA colonoscopy information is included, and to encourage its use through leadership and resource support. Additional improvement efforts might evaluate approaches to reduce inappropriate screening. Implementing a centralized eligibility assessment and tracking system that incorporates information on prior colonoscopy history, age, comorbidities and/or life expectancy, is one promising strategy to explore.
Supplementary Material
Precis.
In the Veterans Health Administration, Blacks are more likely to receive colonoscopy follow-up for positive Fecal Occult Blood Test/Fecal Immunochemical Test (FOBT/FIT+) results than Whites, and follow-up rates decline with advancing age and comorbidity burden. Patient behaviors (refusal, private sector colonoscopy use), and physician behaviors (inappropriate screening) explain race variation in follow-up rates and contribute to age and comorbidity variation.
Acknowledgments
Financial support: This research was funded by the Department of Veterans Affairs Health Services Research & Development (VA HSR&D) grant #IIR 08-334-2 (Partin),VA HSR&D Research Career Scientist award #RCS 10-185 (Partin), VA HSR&D Career Development Award (CDA) #CDA 07-016 (Haggstrom), #CDA 10-022 (Sultan), VA HSR&D Associated Health Postdoctoral Fellowship (Lillie); VA Clinical Science Research & Development Career Development Award (Shaukat), and National Institute on Aging at the National Institutes of Health grant #K24AG041180 (Walter). The views expressed in this article are those of the authors and do not necessarily represent the position or policy of the Department of Veterans Affairs or the National Institutes of Health.
Footnotes
Author contributions: Partin: Conceptualization, investigation, writing original draft and editing, visualization, supervision, project administration, funding acquisition; Gravely: Methodology, software, validation, analysis, investigation, data curation, writing original draft and review, visualization; Burgess J: Conceptualization, writing review and editing; Haggstrom: Conceptualization, writing review and editing; Lillie: Conceptualization, investigation, writing review and editing; Nelson: Conceptualization, methodology, software, validation, analysis, investigation, writing original draft and review; Nugent: Methodology, software, validation, analysis, investigation, data curation, writing review and editing; Shaukat: Conceptualization, writing review and editing; Sultan: Conceptualization, writing review and editing; Walter: Conceptualization, writing review and editing; Burgess D: Conceptualization, writing review and editing.
Potential competing interests: None
Reference List
- 1.American Cancer Society. Cancer Facts and Figures, 2016. Atlanta: American Cancer Society; 2016. [Google Scholar]
- 2.US Preventive Services Task Force. Screening for Colorectal Cancer: US Preventive Services Task Force Recommendation Statement. JAMA. 2016;315:2564–2575. doi: 10.1001/jama.2016.5989. [DOI] [PubMed] [Google Scholar]
- 3.Levin TR, Jamieson L, Burley DA, Reyes J, Oehrli M, Caldwell C. Organized colorectal cancer screening in integrated health care systems. Epidemiol Rev. 2011;33:101–110. doi: 10.1093/epirev/mxr007. [DOI] [PubMed] [Google Scholar]
- 4.El Serag HB, Petersen L, Hampel H, Richardson P, Cooper G. The use of screening colonoscopy for patients cared for by the Department of Veterans Affairs. Arch Intern Med. 2006;166:2202–2208. doi: 10.1001/archinte.166.20.2202. [DOI] [PubMed] [Google Scholar]
- 5.Fisher DA, Jeffreys A, Coffman CJ, Fasanella K. Barriers to full colon evaluation for a positive fecal occult blood test. Cancer Epidemiol Biomarkers Prev. 2006;15:1232–1235. doi: 10.1158/1055-9965.EPI-05-0916. [DOI] [PubMed] [Google Scholar]
- 6.Garman KS, Jeffreys A, Coffman C, Fisher DA. Colorectal cancer screening, comorbidity, and follow-up in elderly patients. Am J Med Sci. 2006;332:159–163. doi: 10.1097/00000441-200610000-00001. [DOI] [PubMed] [Google Scholar]
- 7.Paszat L, Rabeneck L, Kiefer L, Mai V, Ritvo P, Sullivan T. Endoscopic follow-up of positive fecal occult blood testing in the Ontario FOBT Project. The Canadian Journal of Gastroenterology. 2007;21:379–382. doi: 10.1155/2007/569689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jimbo M, Myers RE, Meyer B, et al. Reasons patients with a positive fecal occult blood test result do not undergo complete diagnostic evaluation. Ann Fam Med. 2009;7:11–16. doi: 10.1370/afm.906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Powell AA, Nugent S, Ordin DL, Noorbaloochi S, Partin MR. Evaluation of a VHA Collaborative to Improve Follow-up After a Positive Colorectal Cancer Screening Test. Medical Care. 2011;49:897–903. doi: 10.1097/MLR.0b013e3182204944. [DOI] [PubMed] [Google Scholar]
- 10.Chubak J, Garcia MP, Burnett-Hartman AN, et al. Time to colonoscopy after positive fecal blood test in four U.S. health care systems Cancer Epidemiol Biomarkers Prev. 2016;25:344–350. doi: 10.1158/1055-9965.EPI-15-0470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cooper GS, Koroukian SM. Racial disparities in the use of and indications for colorectal procedures in Medicare beneficiaries. Cancer. 2004;100:418–24. doi: 10.1002/cncr.20014. [DOI] [PubMed] [Google Scholar]
- 12.Oluloro A, Petrik AF, Turner A, et al. Timeliness of colonoscopy after abnormal fecal test results in a safety net practice. J Community Health. 2016;41:864–870. doi: 10.1007/s10900-016-0165-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Choi KS, Lee HY, Jun JK, Shin A, Park EC. Adherence to follow-up after a positive fecal occult blood test in an organized colorectal cancer screening program in Korea, 2004–2008. J Gastroenterol Hepatol. 2012;27:1070–1077. doi: 10.1111/j.1440-1746.2011.06944.x. [DOI] [PubMed] [Google Scholar]
- 14.Turner B, Myers RE, Hyslop T, et al. Physician and patient factors associated with ordering a colon evaluation after a positive fecal occult blood test. J Gen Intern Med. 2003;18:357–363. doi: 10.1046/j.1525-1497.2003.20525.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Correia A, Rabeneck L, Baxter NN, et al. Lack of follow-up colonoscopy after positive FOBT in an organized colorectal cancer screening program is associated with modifiable health care practices. Preventive Medicine. 2015;76:115–122. doi: 10.1016/j.ypmed.2015.03.028. [DOI] [PubMed] [Google Scholar]
- 16.Rao SK, Schilling TF, Sequist TD. Challenges in the management of positive fecal occult blood tests. J Gen Intern Med. 2009;24:356–360. doi: 10.1007/s11606-008-0893-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Carlson CM, Kirby KA, Casadei MA, Partin MR, Kistler CE, Walter LC. Lack of Follow-up After Fecal Occult Blood Testing in Older Adults: Inappropriate Screening or Failure to Follow Up? Arch Intern Med. 2011;171:249–256. doi: 10.1001/archinternmed.2010.372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Landrum MB, Keating NL, Lamont EB, Bozeman SR, McNeil BJ. Reasons for underuse of recommended therapies for colorectal and lung cancer in the Veterans Health Administration. Cancer. 2012;118:3345–3355. doi: 10.1002/cncr.26628. [DOI] [PubMed] [Google Scholar]
- 19.Partin MR, Burgess DJ, Burgess JF, Jr, et al. Organizational Predictors of Colonoscopy Follow-up for Positive Fecal Occult Blood Test Results: An Observational Study. Cancer Epidemiol Biomarkers Prev. 2015;24:422–434. doi: 10.1158/1055-9965.EPI-14-1170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Myers RE, Hyslop T, Gerrity M, et al. Physician intention to recommend complete diagnostic evaluation in colorectal cancer screening. Cancer Epidemiol Biomarkers Prev. 1999;8:587–593. [PubMed] [Google Scholar]
- 21.Myers RE, Turner B, Weinberg D, et al. Complete diagnostic evaluation in colorectal cancer screening: research design and baseline findings. Prev Med. 2001;33:249–260. doi: 10.1006/pmed.2001.0878. [DOI] [PubMed] [Google Scholar]
- 22.Austin PC, Tu JV. Boostrap methods for developing predictive models. The American Statistician. 2004;58:131–137. [Google Scholar]
- 23.Powell AA, Saini SD, Breitenstein MK, et al. Rates and correlates of potentially inappropriate colorectal cancer screening in the Veterans Health Administration. Journal of General Internal Medicine. 2015;30:732–741. doi: 10.1007/s11606-014-3163-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Miglioretti DL, Rutter CM, Bradford SC, et al. Improvement in the diagnostic evaluation of a positive fecal occult blood test in an integrated health care organization. Med Care. 2008;46:S91–S96. doi: 10.1097/MLR.0b013e31817946c8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Plumb AA, Ghanouni A, Rainbow S, et al. Patient factors associated with non-attendance at colonoscopy after a positive screening faecal occult blood test. Journal of Medical Screening. 2016 doi: 10.1177/0969141316645629. Online ahead of print. [DOI] [PubMed] [Google Scholar]
- 26.Jackson CS, Oman M, Patel AM, Vega KJ. Health disparities in colorectal cancer among racial and ethnic minorities in the United States. J Gastrointest Oncol. 2016;7:S32–S43. doi: 10.3978/j.issn.2078-6891.2015.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lafata JE, Williams LK, Ben Menachem T, Moon C, Divine G. Colorectal carcinoma screening procedure use among primary care patients. Cancer. 2005;104:1356–1361. doi: 10.1002/cncr.21333. [DOI] [PubMed] [Google Scholar]
- 28.Etzioni DA, Yano EM, Rubenstein LV, et al. Measuring the quality of colorectal cancer screening: the importance of follow-up. Dis Colon Rectum. 2006;49:1002–1010. doi: 10.1007/s10350-006-0533-2. [DOI] [PubMed] [Google Scholar]
- 29.Cooper LA, Roter DL, Johnson RL, Ford DE, Steinwachs DM, Powe NR. Patient-centered communication, ratings of care, and concordance of patient and physician race [see comment] Annals of Internal Medicine. 2003;139:907–915. doi: 10.7326/0003-4819-139-11-200312020-00009. [DOI] [PubMed] [Google Scholar]
- 30.Liss DT, Brown T, Lee JY, et al. Diagnostic colonoscopy following a positive fecal occult blood test in community health center patients. Cancer Causes Control. 2016;27:881–887. doi: 10.1007/s10552-016-0763-0. [DOI] [PubMed] [Google Scholar]
- 31.Heidenreich PA, Shlipak MG, Geppert J, McClellan M. Racial and sex differences in refusal of coronary angiography. Am J Med. 2002;113:200–207. doi: 10.1016/s0002-9343(02)01221-4. [DOI] [PubMed] [Google Scholar]
- 32.Sedlis SP, Fisher VP, Tice D, Esposito R, Madmon L, Steinberg EH. Racial differences in performance of invasive cardiac procedures in a Department of Veterans Affairs Medical Center. J Clin Epidemiol. 1997;50:899–901. doi: 10.1016/s0895-4356(97)00089-9. [DOI] [PubMed] [Google Scholar]
- 33.Oddone EZ, Horner RD, Diers T, et al. Understanding racial variation in the use of carotid endarterectomy: The role of aversion to surgery. J Natl Med Assoc. 1998;90:25–33. [PMC free article] [PubMed] [Google Scholar]
- 34.Ayanian JZ, Cleary PD, Weissman JS, Epstein AM. The effect of patients' preferences on racial differences in access to renal transplantation. New England Journal of Medicine. 1999;341:1661–1669. doi: 10.1056/NEJM199911253412206. [DOI] [PubMed] [Google Scholar]
- 35.Whittle J, Conigliaro J, Good CB, Joswiak M. Do Patient Preferences Contribute to Racial Differences in Cardiovascular Procedure Use? Journal of General Internal Medicine. 1997;12:267–273. doi: 10.1046/j.1525-1497.1997.012005267.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zhu CW, Livote EE, Ross JS, Penrod JD. A random effects multinomial logit analysis of using medicare and VA healthcare among veterans with dementia. Health Care Services Quarterly. 2016;29:91–104. doi: 10.1080/01621424.2010.493771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ross JS, Keyhani S, Keenan PS, et al. Dual use of Veterans Affairs Services and Use of Recommended Ambulatory Care. Med Care. 2008;46:309–316. doi: 10.1097/MLR.0b013e31815b9db3. [DOI] [PubMed] [Google Scholar]
- 38.Petersen LA, Byrne MM, Daw CN, Hasche J, Reis B, Pietz K. Relationship between clinical conditions and use of Veterans Affairs health care among Medicare-enrolled veterans. Health Serv Res. 2010;45:762–791. doi: 10.1111/j.1475-6773.2010.01107.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hynes DM, Koelling K, Stroupe K, et al. Veterans’ access to and use of Medicare and veterans affairs health care. Medical Care. 2007;45:214–223. doi: 10.1097/01.mlr.0000244657.90074.b7. [DOI] [PubMed] [Google Scholar]
- 40.Humensky J, Carretta H, de Groot K, Brown MM, Tarlov E, Hynes DM. Service utilization of veterans dually eligible for VA and Medicare fee-for-service: 1999–2004. Medicare & Medicaid Research Review. 2012;2:E1–E22. doi: 10.5600/mmrr.002.03.a06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Berke EM, West AN, Weeks WB. Practical and policy implications of using different rural-urban classification systems: A case study of inpatient service. The Journal of Rural Health. 2016;25:259–266. doi: 10.1111/j.1748-0361.2009.00228.x. [DOI] [PubMed] [Google Scholar]
- 42.Maciejewski ML, Birken S, Perkins M, Burgess JF, Jr, Sharp N, Liu CF. Medicare Managed Care Enrollment by Disability-Eligible and Age-Eligible Veterans. Med Care. 2009;47:1180–1185. doi: 10.1097/MLR.0b013e3181b58e17. [DOI] [PubMed] [Google Scholar]
- 43.Morris AL, Vito AA, Bomba MR, Bentley JM. The impact of a quality assessment program on the practice behavior of general practitioners: a follow-up study. Journal of the American Dental Association. 1989;119:705–709. doi: 10.14219/jada.archive.1989.0249. [DOI] [PubMed] [Google Scholar]
- 44.Ferrat E, Breton JL, Veerabudun K, et al. Colorectal cancer screening: Factors associated with colonoscopy after a positive faecal occult blood test. British Journal of Cancer. 2013;109:1437–1444. doi: 10.1038/bjc.2013.476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Wong ES, Wang V, Liu F, Herbert PL, Maciejewski ML. Do Veterans Health Administration Enrollees Generalize to Other Populations? Medical Care Research & Review. 2016;73:493–507. doi: 10.1177/1077558715617382. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


