Abstract
Retaining participants in longitudinal studies is a unique methodological challenge in many areas of investigation, and specifically for researchers aiming to identify effective interventions for women experiencing Intimate Partner Violence (IPV). Individuals in abusive relationships are often transient and have logistical, confidentiality, and safety concerns that limit future contact. A natural experiment occurred during a large randomized clinical trial enrolling women in abusive relationships who were also heavy drinkers, which allowed for the comparison of two incentive methods to promote longitudinal retention: cash payment vs. reloadable wireless bank cards. Six-hundred patients were enrolled in the overall trial which aimed to incentivize participants using a reloadable bank card system in order to promote the completion of 11 weekly interactive voice response system (IVRS) phone surveys and 3, 6 and 12-month follow up phone or in person interviews. The first 145 participants were paid with cash as a result of logistical delays in setting up the bank card system. At 12 weeks, participants receiving the bank card incentive completed significantly more IVRS phone surveys (OR 2.4, 95% CI .01–1.69). There were no significant differences between the 2 groups related to satisfaction or safety and/or privacy. The bankcard system delivered lower administrative burden for tracking payments for study staff. Based on these and other results, our large medical research university is implementing reloadable bank card as the preferred method of subject incentive payments.
Keywords: Retention, Subject incentives, Intimate Partner Violence, Drinking Behaviors, Clinical Trials
Selected Keywords: Domestic Violence < Alcohol and Drugs, Intervention/treatment<Domestic Violence, Anything related to domestic violence<Domestic Violence
Introduction
Rigorous evaluation of healthcare interventions with women experiencing intimate partner violence (IPV) has been hampered by safety and confidentiality concerns. The lack of evidence for the effectiveness of IPV interventions compounds the problem of restricted resources available to both study and address the impact of interventions for this common social problem. With some important exceptions (Campbell et al., 2011; Clough et al., 2010; Sullivan et al., 1996), most IPV efficacy trials have experienced one or more methodological limitations, such as problems with subject engagement, adequate comparison groups, assessment reactivity, and challenges with long-term retention of this vulnerable population (Dutton et al., 2003; MacMillian et al., 2009; McFarlane, 2007; Mechanic & Pole, 2013). Optimizing recruitment and retention within clinical trials is necessary to reduce bias and disparities in patients accepting enrollment, as well as ensure the validity of clinical research results (Dunn & Gordon, 2005; Festinger et al., 2008; Grady et al., 2005; NIH, 1959; Schulz & Grimes, 2002; US FDA, 1998). This is particularly true of studies enrolling underrepresented, at risk populations (Patel, Doku, & Tennakoon, 2003; UyBico, Pavel, & Gross, 2007). Studies comparing methods to improve participant engagement and reduce clinical trial attrition have largely focused on timing and compensation amount, with the aim of maximizing recruitment and retention, while limiting the possibility of coercion (Doody et al., 2003; VanGeest, Wynia, Cummins, & Wilson, 2001). Among research subjects experiencing IPV, human subject concerns around safety and confidentiality related to completion of follow up activities must also be carefully considered (Sullivan & Cain, 2004).
As part of a large randomized clinical trial enrolling abused women who were also heavy drinkers to test a motivational intervention, we were particularly interested in the use of technologies that would allow women to complete and be reimbursed for study activities at safe and convenient times. Women in abusive relationships who are also heavy drinkers are a particularly vulnerable, transient population, with significant barriers to follow up contact, returning to the study site, and carrying cash. For our study, primary outcome measures (incidents of IPV and days of heavy drinking) were collected by interactive voice response system (IVRS), a technology that allowed women to complete weekly phone surveys for 12 weeks following enrollment at their convenience. Additional longitudinal data was also collected at 3, 6, and 12 months using frequently updated individualized safe contact information, so that, once enrolled, women would never have to return to the study enrollment site. The proposed plan was for all subject incentives to be paid via wireless reloadable bank cards, within 1–2 days of completing study activities. Beyond human subjects’ concerns, reloadable bank cards for clinical trial participants also offer the potential advantage of improving retention and recruitment, compared to traditional cash incentives. Theories of behavioral economics and response behavior support the possibility that a reloadable bank card will improve study participation by providing more immediate gratification (payment shortly after completed follow up activity) and continued engagement with study activities. Recent literature includes the use and procedures for reloadable bank or gift cards (Barber, Kusunoki, & Gatny, 2011; Blackstone, Wiebe, Mollen, Kalra, & Fein, 2009; Gatny, Couper, Axinn, & Barber, 2009; South-Paul et al., 2014; Wiebe, Carr, Datner, Elliott, & Richmond, 2008); however, to our knowledge, no previous studies have evaluated the effectiveness of a reloadable bank card when compared to more traditional incentives, such as cash payments. This quasi-experimental study compares the completion of study activities for participants paid within 1–2 days on a wirelessly reloadable bank card to participants paid with a delayed cash system (returning to the ED at their discretion).
We have previously reported on the results of our RCT with 600 women in abusive relationships who exceeded sex-specific NIAAA recommended safe drinking limits (Rhodes et al., 2015) during which we were able to achieve high rates of completion of primary data collection and good long-term subject retention. As discussed above, we specifically targeted the use of innovative asynchronous technologies to address common weaknesses in IPV studies, such as limited enrollment, high attrition and inadequate outcome data (Sullivan et al., 1996; Zink & Putnam, 2005). The current study reports on the natural experiment that allowed for the investigation of the potential retention benefits of using a reloadable payment compared to cash incentives with a vulnerable population, specifically in the collection of repeated outcome measures via weekly phone surveys. University administrative constraints setting up the reloadable bank card incentive system delayed its implementation, and the study was launched using cash incentives. After 8 months of enrollment, all new participants were only offered wirelessly reloadable bank card incentives.
The primary object of the current study is to determine the comparative effectiveness of a reloadable bank card versus a traditional cash incentive for increasing study retention among women experiencing intimate partner violence. Secondary objectives explore participant satisfaction and potential safety concerns with the use of wireless subject incentives.
Methods
Overview
This is a prospective cohort study using retention and longitudinal data collected during an NIAAA-funded randomized control trial (RCT). The larger trial evaluated the effectiveness of a brief social work intervention to decrease instances of violence and heavy drinking among women seeking care at an Emergency Department (ED) (Rhodes et al., 2015). All enrollees met study eligibility criteria: female, ages 18 to 64, heavy drinking habits (defined as a score of 4 or more on the AUDIT; Babor, Higgins-Biddle, Saunders, & Monteiro, 2001), and experience with IPV in the past 3 months (a score of 1 or more on the CTS2S; Straus & Douglas, 2004). A total of 600 participants were recruited from two busy urban EDs and randomized to one of three study groups: the intervention group (n = 242), the assessed control group (n = 237) and the no contact control group (n = 121). The no contact control group was only assessed with the 3-month interview, while the other two groups completed 12 weekly phone surveys and a 3, 6, and 12-month structured interviews. The intervention group participated in a brief social work session (15–25 minutes) by counselors trained in motivational interviewing (Moyers et al., 2010). A detailed account of all study procedures including recruitment and retention can be found in the study’s protocol and primary outcome publications (Rhodes et al., 2014, 2015). Relevant to the present study, all recruitment and follow up contact with participants remained consistent throughout the study, with minor improvements over time in the procedures for updating participant contact information and identifying study participants during subsequent ED visits. The study was approved by the university’s Institutional Review Board, as meeting the ethical and safety guidelines for a population experiencing intimate partner violence.
Payment Systems
To establish the reloadable incentive system, the study team worked with the university’s administrative offices (i.e. Provost Office, Accounts Payable, Office of Research Services) to create a contract with a national bank that both protected the identities of participating subjects and allowed for adequate reconciliations of grant funds. Unanticipated administrative resources in establishing the unprecedented contract and university-approved procedures delayed the use of reloadable bank cards with the first group of enrolled participants. The study was launched using cash incentives, which is the standard approved method of paying study participants and required participant signatures with every payment. Once established, the wireless incentive structure allowed the study team to provide bank cards to participants at enrollment, track the completion of follow up activities, and load the cards online with incentive payments shortly after the completion of each study activity. Important to the protection of participant privacy, the bank administering the payment did not have any access to subject’s names or contact information.
Participants enrolled during the first 8 months of the study received in person cash incentives for the duration of their study participation, and were given two options: (1) return to the enrollment site (Emergency Department) intermittently to receive cash payments for completed calls or (2) wait to receive a lump sum payment at the completion of the 3, 6 or 12-month interview; payment choice was left at the discretion of the participant. Upon launch of the reloadable incentive system, a clean break was made to enroll all subsequent participants using reloadable bank cards, creating two distinct payment groups. These participants were provided a generic reloadable bank card (i.e. embossed with “Gift Card”, not participant name) and informed that the cards would be funded within 1 to 2 business days of completing each study activity. If a card was lost, participants contacted the study team to obtain a replacement card. The project manager could confirm the amount of funds remaining, cancel the lost card, and reissue a new card that the participant could pick up at their convenience. This change to the wireless incentive structure 8 months into data collection created a natural experiment, allowing for a comparison of retention rates between cash paid and card paid participants. The sample for this study includes participants who completed their baseline IVRS call and were enrolled in the intervention or assessed control groups; the no contact control group was excluded from this analysis because this group did not complete weekly IVRS calls and were only contacted once at 3 months to determine the impact of assessment reactivity.
Moderator Measures
The 10-item AUDIT and 16-item CTS2S assessments are collected (1) at baseline to determine eligibility and (2) weekly via IVRS and at 3, 6 and 12-month interviews to evaluate the risk reduction outcomes of the larger study. To evaluate the impact of payment method, the baseline measures are used to assess the moderating effects of severity on completion of study activities. These measures were selected because they are the most utilized in previous studies and national surveys of drinking behaviors and IPV. The AUDIT was developed by the National Institute for Alcoholism and Alcohol Abuse and its validity and reliability is established in a variety of settings worldwide, with an average Cronbach’s alpha of .80, indicating high internal consistency (de Meneses-Gaya et al., 2009). The CTS (Conflict Tactics Scale) is the most widely used tool to screen for perpetration and victimization of verbal, emotional, physical and sexual domestic violence (Straus et al., 1996; 78-items). For brevity in the screening process, the validated shorter version (CTS2S; 16-items) was selected for the larger study. Researchers have demonstrated high correlations among the five construct scores between the shortened and full version of the measure, which had high reliability ranging from .79 to .95 (Straus et al., 1996).
Outcome Measures
The outcome measures for this study include the number of completed follow up activities including potentially 11 IVRS phone surveys for the first 12 weeks of the study, and 3 follow up phone or in person interviews. We describe the procedures and compensation to provide context for participant completion of these activities. The Interactive Voice Response System (IVRS) collected the larger study’s primary outcome measures (frequency of IPV and drinking) through weekly phone survey data for 12 weeks after enrollment. Baseline calls were made in the ED at the time of enrollment, ensuring participants understood the process. Participants called a toll-free number, which was open twenty-four hours a day, seven days a week, using a subject ID number and unique password to protect confidentiality. Compensation was $10 per completed weekly call, and if the 12th week call was completed, participants received a bonus of an additional $5 for each completed call. Previous studies have used this automated telephone survey (Blackstone et al., 2009; Corkrey, & Parkinson, 2002; Johansson, Remvall, Malgerud, Lindgren, & Andersson, 2013; Searles, Perrine, Mundt, & Helzer, 2000; Wiebe, Blackstone, Mollen, Culyba, & Fein, 2011; Wiebe et al., 2008), and found IVRS to be a valuable research tool with vulnerable populations due its confidentiality, flexibility and ease of completion. Paired with reloadable bank cards, participants who were tracked for 12 months, assuming they did not lose their bank cards, never had to return to the ED after study enrollment.
The primary efficacy trial (Rhodes et al., 2015), collected additional IPV and drinking measures and other outcomes at 3, 6, and 12 months via a structured interview. Completion/non-completion of these interviews was examined as a secondary outcome in the current study. All participants were given the opportunity to complete the 20–45 minute 3, 6, and 12-month follow up measures by phone or in person. Upon completion of each interview, participants were paid $30 to $50 on the bank card or in cash, depending on when they were enrolled in the study. Cash paid participants could return to the ED (location of enrollment) any time during study hours (approximately 9am to 7pm, 6 days a week).
Retention Procedures
For the duration of the RCT, standardized retention procedures were used to ensure valid, consistent study results, and ensure the safety of the study population. On a daily basis, the project manager monitored and documented the completion of all IVRS calls. If a participant missed the first call outside the ED, or any two consecutive calls, she was contacted by phone to determine if she had the ID and password needed to complete the call. Subjects were also contacted by phone two weeks prior to schedule a 3, 6, and 12-month follow up interview. Safety concerns with a study population in abusive relationships limits the variety of methods used to for follow up; thus, all contact with study participants followed an Individualized Safe Contact Plan that was developed with participant guidance at baseline and updated at every contact. This form includes participant preferences for follow up calls and secondary contact information in the event the participant cannot be reached. Safety concerns with a study population in abusive relationships limits the variety of methods used to contact participants in other less sensitive studies (i.e. show up at their home or work; speaking at length with secondary contacts or other individuals reached via phone).
As to be expected with longitudinal RCTs, a few procedural adjustments and staffing changes occurred over the course of the study, which may have positively impacted retention rates. For instance, after approximately ten months of data collection, an indicator was added to the electronic medical record, seen only by the study’s certified research personnel, to identify whether an enrolled participant returned to the ED. As explained in our analyses, we attempt to control for the potential influence of the observable and unobservable study factors on our primary goal of this study: identifying the independent impact of cash payments versus card payments on study activity completion rates.
Analysis
Descriptive analyses were used to evaluate the demographic and eligibility criteria differences between the two payment groups. Weekly call and interview completion rates were analyzed by payment group. Chi-Square was used to analyze categorical variables, and Wilcoxon-Mann-Whitney test was used for the non-normally distributed continuous variables (i.e. age, CTS2S score, and AUDIT Score, weekly call completion). A negative binomial generalized linear model (GLM), which accounts for overdispersion (variance exceeds the mean) in count outcome data (Hilbe, 2011), was used to assess differences in the total number of IVRS calls completed between payment groups. The baseline call, which was completed during enrollment in the ED, was not included in the counts, meaning participants could complete a total of 0 to 11 calls. We used GLM to control for potential confounders: baseline scores of relationship violence and problem drinking, age at enrollment, the month and year of enrollment (variability with linear time trend) and treatment assignment in the larger RCT (Brief Intervention vs. Control). In addition, the interaction between the eligibility assessment scores and payment type was included to assess the potential moderating effects of IPV and drinking severity on the total number of completed calls.
In addition to including the month and year of enrollment covariates, we also conducted additional analyses to evaluate the possibility that an increase in retention rates resulted from of staff changes and improvements in follow up procedures over time. A Wilcoxon-Mann-Whitney test was used to compare the retention rates of a subset of the cash paid participants enrolled 3 months prior to the switch to card incentives to a subset of the card paid participants enrolled 3 months after implementation.
To assess the relationship between payment method and participant’s likelihood to re-engage with the study after failing to complete study activities, we defined re-engagement as missing 3 or more calls in a row (between call 2 and call 11) followed by the completion of a subsequent follow up activity. A chi-square test was used to determine if a significant relationship existed between payment type and re-engaging by completing a subsequent call or the 3-month interview.
Administrative documentation of when cash-paid participants returned to the ED to pick up incentive payments was analyzed using a Wilcoxon-Mann-Whitney test to assess for a relationship between picking up cash and completion of study activities. Reported safety indicators collected on the 3-month interview are reported and chi-square tests were used to determine significance between payment groups. Finally, summary statistics are provided for three items on satisfaction with the reloadable bank card collected from card paid participants at 3 months.
Results
Of the 479 women randomized to the intervention or control group, 10 did not complete study enrollment activities (i.e. the baseline IVRS training call in the ED), and are excluded from this analysis, leaving a sample size of 469. Of these, 111 participants received in person cash incentives and 358 participants were given a reloadable bank card for incentive payments. Demographically representative of the urban, diverse, and low to middle socioeconomic population of the recruitment site, the enrolled sample of women were primarily African-American with at least a high school education, a household income of 10,000 or more a year, and most indicated they were not married, but in a committed relationship. Approximately half were employed and half did not have any children. Table 1 presents the demographics of the two payment groups. Analyses indicate that participants were similar for all factors, with the exception of risk severity at enrollment. Cash paid participants had significantly higher scores on the baseline CTS2S (z = 3.32, p < .001) and AUDIT (z = 3.18, p = .002) assessments than those paid with the reloadable bank card. Using the recommended non-parametric effect size Cliff’s d (Cliff, 1993; Grissom & Kim, 2012), an effect size of .60 was found for both of these baseline severity differences.
Table 1.
Demographics by Incentive Type
| Cash (n =111) | Card (n=358) | p value | ||
|---|---|---|---|---|
| Age a | Median(IQR) | 27 (12) | 29 (17) | .07 |
|
| ||||
| Education, No. (%) | Less than High School | 23 (20.7) | 74 (20.7) | .99 |
| High School Education or more | 88 (79.3) | 283 (79.3) | ||
|
| ||||
| Annual Household Income, No. (%) | Less than 10,000/year | 30 (29.4) | 102 (31.7) | .67 |
| 10,000 or more/year | 72 (70.6) | 220 (68.3) | ||
|
| ||||
| Marital Status, No. (%) | Married | 17 (15.3) | 50 (14.0) | .82 |
| Single | 84 (75.7) | 280 (78.4) | ||
| Widowed/Divorced/Separated | 10 (9.0) | 27 (7.6) | ||
|
| ||||
| Employment, No. (%) | Employed outside of home | 53 (47.8) | 173 (48.3) | .92 |
| Unemployed/Retired | 58 (52.2) | 185 (51.7) | ||
|
| ||||
| Race, No. (%) | African American/Black | 75 (68.2) | 256 (71.9) | .62 |
| White | 21 (19.1) | 54 (15.2) | ||
| Other | 14 (12.7) | 46 (12.9) | ||
|
| ||||
| Children in household a (Under 18), No. (%) | 1 or more | 53 (47.8) | 101 (23.7) | .48 |
| No Children | 58 (52.2) | 351 (76.3) | ||
|
| ||||
| CTS2S Score a No. (%) | Median(IQR) | 9 (12) | 6 (9) | <.001 |
|
| ||||
| AUDIT Score a, No. (%) | Median(IQR) | 8 (6) | 6 (5) | .02 |
|
| ||||
| Assigned Study Group, No. (%) | Assessed Control Group (ACG) | 55 (49.6) | 176 (49.2) | .94 |
| Brief Intervention Group (BIG) | 56 (50.5) | 182 (50.8) | ||
Continuous variables are not normally distributed; p values calculated using the non-parametric Wilcoxon-Mann-Whitney test.
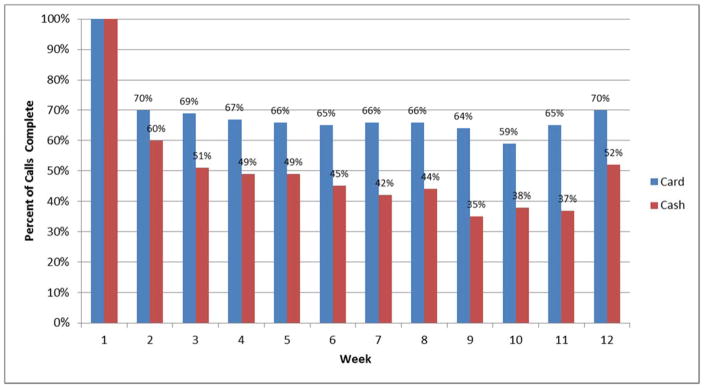
The median number of calls for the card group (9 calls) was significantly greater than the cash group median of 5 calls (z = 5.49, p < .001), with a non-parametric Cliff’s d effect size of .33. Figure 1 visually presents the higher completion of the weekly IVRS surveys for subjects receiving incentives through the reloadable bank card compared to those receiving cash incentives. In terms of the in person or phone interviews, 79% of all participants completed the 3-month women’s health interview; participants paid with the card had a completion rate of 80%, while 75% of cash paid participants completed the 3-month interviews, which is not statistically significant (χ2(1, N = 469) = 1.48, p = .22). This trend of higher retention rates among the card paid participants remains consistent for the 6-month (80% card vs. 68% cash paid) and 12-month (72% card vs. 66% cash paid) women’s health interviews, and is statistically significant at 6 months (χ2(1, N =469) = 6.27, p = .01), but not at 12 months (χ2(1, N = 469) = 1.33, p = .25).
Figure 1.
Weekly Call Participation by Payment Type.
Because there was a statistically higher level of severity of IPV and heavy drinking for those enrolled at the beginning of the study who received cash incentives (see Table 1), we assessed the influence of IPV and drinking severity on the completion of study activities. Analyses confirmed that there were no significant differences between severity of alcohol use and total number of calls completed in both the cash group (p = 0.79) and the card participants (p = .53) independently. Similarly, IPV severity was not a significant factor for call completion (Cash p = .21; Card p = .59). However, risk severity measures were still included in the GLM as a possible confounding factor.
In the negative binomial regression model predicting total number of completed calls with payment type and the aforementioned covariates, payment type and age were the only significant predictors (See Appendix A). The expected number of calls for a card paid participant is 2.3 times higher than those paid with cash (p = .047). In contrast, age had much less impact; for each year older a participant is, the expected number of total calls increased by less than 1% holding other variables constant. Similar to the bivariate analyses, severity of IPV and alcohol use, as well as the interactions between severity and payment type were not significant. A simplified model removing the non-significant predictors leaving only the age of the participant and payment type (Model 2), produced similar results with card paid participants expected to make 43% more calls than those paid with cash (p < .001).
In order to evaluate the possibility that an increase in retention may be a result of improvements in study procedures over time, we examined the retention rates of the 43 cash paid participants enrolled in the 3 months prior to switching to card incentives compared to the 48 card paid participants enrolled in the 3 month after the change in payment method. The mean number of calls for the card participants 3 months after the switch is 8.1 (SD = 3.6, Mdn = 9), which is significantly greater than the cash group (M = 5.3; SD = 3.5; Mdn = 5; z = 3.70, p < .001; Cliff’s d = .33). This is consistent with the overall findings comparing full sample of 111 cash participants versus 358 card participants, and there are no significant differences between the means of the subset and full sample for cash participants (p = .65) and card participants (p = .16) independently.
In regard to the relationship between payment and study re-engagement, a total of 172 (37%) participants missed 3 or more calls in a row and are included in our analysis of re-engagement in study activities. Only 27% of those eligible for re-engagement completed a subsequent call. While a greater percentage in the card group (30%) re-engaged than those with cash payment (22%), it is not a statistically significant difference (p = .24).
Of the 82 cash paid participants who completed at least 1 call after enrollment, 30 returned to the ED one or more times to obtain incentive payments for completing the IVRS phone surveys during the first 12 weeks of the study. The mean number of IVRS calls for the group who returned to pick up cash incentives is 7.6 (SD = 2.6; Mdn = 8), which is similar to that of the card payment group, and is significantly greater than the cash subgroup who did not return for payment (M=5.5; SD = 3.3; Mdn = 5.5; z=2.83; p = .0046; Cliff’s d = .69). There are no significant differences in completion rates of the 3-month follow up interview based on returning for payment for this subset of cash paid participants. However, the wireless payment allowed more participants to complete the 3-month follow up interview by phone; the rate of phone versus in person follow up interviews increased from 27% during cash payments to 92% once the wireless payment method was introduced.
Those participants who completed the 3-month interview (n = 369) answered questions about whether they have taken any steps to increase their safety over the past 3 months, how safe they feel in their daily life and if the study had an impact on their level of safety. Regardless of payment type, about a third of patients reported they had taken steps to increase their safety, 56% felt extremely or very safe in their daily life and 42% stated that participating in the study made them feel safer. There is no statistically significant difference in reports of any of these safety outcomes between those who were paid by card compared to cash. This finding aligns with the lack of any reports of adverse events related to study participation, even among subjects with higher severity of drinking or IPV.
At 3 months, 96% (n = 245) of participants who received wireless incentive payments on the card indicated they were satisfied or very satisfied with the process. Only 16% (n = 39) indicated that they would rather be paid by cash. A few participants (n = 28; 11%) required help to access their card payments, most of which was related to forgetting the access code or losing the card, which, unlike the loss of cash payments, could then be cancelled and replaced.
Limitations
This study has several key limitations. Because this was a natural experiment, comparative data was not collected during a concurrent time period for the two payment groups. Moreover participants enrolled during the cash payment phase of the study had greater IPV and alcohol severity at enrollment. While there is not a clear explanation for this, it is possible that participants with greater severity were both easier to identify and recruit earlier in the study and had greater difficulty completing follow up IVRS calls. However, controlling for baseline severity does not appear to impact the independent influence of the card on completion rates of study activities during the 12 weeks of IVRS calls. The addition of the electronic study enrollment alert at approximately ten months also does not appear to have influenced the rates of follow up completion of study activities. However, while procedures to re-engage participants remained otherwise consistent throughout the larger RCT, we cannot account for unobservable variation in retention methods that may have been caused by research staff experience or turnover. Although the analyses controlled for month and year of enrollment in attempt to account for this variation, we recognize that randomizing participants to different payment methods would be a more effective way to test the impact of a wireless incentive structure on subject completion of study activities. However, we did not wish to jeopardize the outcomes of the overall study by embedding an RCT within the larger RCT.
Participants who enrolled after the reloadable bank cards were implemented did not have the option to receive cash, the more common form of incentive payment at the enrolling institution. It is possible that this influenced some patient’s decisions not to enroll in the study, thus introducing selection bias. For instance, participants who enrolled after the launch of the bank card may have been inherently more accepting of innovative payment and data collection methods.
Participants included in this analysis were all female patients recruited from two urban EDs, who met eligibility criteria of heavy drinking (AUDIT>3) and experience with IPV in the last 3 months (CTS2S >1). While we acknowledge that this makes the results less generalizable, it also demonstrates the potential for this methodology to improve longitudinal data collection during intervention studies with vulnerable, transient populations.
Discussion
Study results indicate that the use of wireless incentives provided via generic reloadable bank cards increased subject completion rates of follow up study activities and overall retention of women drinkers in abusive relationships in a large randomized clinical intervention trial. This work adds to the literature addressing high rates of overall and/or differential attrition as significant limitations for intervention studies with abused women in acute care settings (Bair-Merrritt et al, 2010; Chermack et al, 2015; MacMillian et al., 2009). In our study, wireless payment more than tripled (from 27% to 97%) the number of participants who chose to complete follow up interviews by phone, as opposed to returning to the ED for in person follow up interviews. This supports that a reloadable subject incentive system that does not require participants to return to the study site allows for greater flexibility of collecting follow up data, particularly when paired with remote data collection methods.
A growing body of research finds that technological advances allow for new approaches to trial participant retention that can be tailored to the population being studied. Specifically, mobile technology allows for participants in sensitive social-behavioral studies to participate in the study without being physically present. For instance, recent studies with populations experiencing IPV, adolescent assault victims, and pregnant teenagers have used methods including: Interactive Voice Response Systems (IVRS) or phone surveys, online surveys, and text (SMS) messaging (Barber et al., 2011; Blackstone et al., 2009; Corkrey & Parkinson, 2002; Kew, 2010; Johansson et al., 2013; Piette et al., 2013; Searles et al., 2000; Wiebe et al, 2008, 2011). These studies also demonstrate that demographically diverse populations are willing and satisfied with these remote methods of study participation, alleviating common concerns about new technologies limiting particular socio-demographic groups from study participation (Pittle et al., 2013; Ranney, Choo, Spirito, & Mello, 2013).
With technological innovations for asynchronous communication and wireless data collection between the study team and research subjects, the administrative and transportation burdens can be lessened for study personnel and study subjects alike. New subject incentive payment systems, such as reloadable bank cards can be funded remotely upon completion of study activities. Administrative hurdles related to cash incentives, such as loss, theft, documentation, and the need for in person contact, can be mitigated using the reloadable bank cards. In recent studies, reloadable bank or store gift cards have been used to further supplement the benefits of remote data collection with sensitive, at-risk populations; as a result, potentially increasing the diversity of research participants (Barber et al., 2011; Blackstone et al., 2009; Gatny et al, 2009; South-Paul et al., 2014 Wiebe et al., 2008).
While there are valid concerns that incentives for research participation can be coercive, particularly for lower socioeconomic populations or substance abusing populations, recent studies have determined that most US clinical trials offer a pro-rated modest amount per study (median $155). Rather than introducing a threat of undue influence, incentives in this range are considered appropriate and respectful compensation, as long as the amount aligns with time contribution made by participants (Emanuel, 2005; Festinger et al., 2008; Grady, 2001; Grady et al., 2005). The maximum amount of compensation to participants described in this study was $290 for up to 15 follow ups and 12 months of participation, which was deemed suitable by the university’s IRB and comparable to other studies at the university.
While the use of reloadable cards to wirelessly pay research participants is becoming increasingly widespread, to our knowledge, this is the only study to compare wireless with cash incentives for its impact on subject retention. Prepaid card companies are now targeting the research market offering services specifically tailored to pay clinical research participants. Universities are contracting with these services or directly with banks to develop school-wide policies for paying research participants using reloadable cards, recognizing the flexibility and logistical advantages over cash or check payments (Gatny et al., 2009; University of Notre Dame, 2011). In fact, our institution recently launched a reloadable card program as the recommended method of paying research participants for all new studies, emphasizing it as a faster, safer, and easier to track alternative to checks, gift cards, and petty cash. This change was motivated by our office of research compliance’s positive experience with this study and the data reported here.
There are a few research studies that have described the use of wireless reloadable subject incentive cards with their participants. A study at University of Michigan (Gatny et al., 2009) evaluating unintended pregnancy among young women described the procedures and benefits of using reloadable cards in their study (Gatny et al., 2009). Wiebe and colleagues, whose previous work was the impetus for including this incentive payment method in the larger RCT, used reloadable convenience store gift cards to pay participants in his research with adolescents victims of violence and women experiencing IPV (Blackstone et al, 2009; Wiebe et al., 2008, 2011). Both research projects also used innovative remote data collection methods. Indeed the emerging use of asynchronous data collection in research studies is rapidly increasing. New methods of app-based, SMS or email for study data collection and tracking of health indices abound (Corkey & Parkinson, 2002; Kew, 2010; Whitford et al., 2012) allow for greater convenience for subjects to provide follow up data at times that are convenient for them. However, while the potential benefit for increasing retention and response rates seems intuitive, it has not yet been evaluated. Our study draws attention to the possibility to pair these newer methods of follow up data collection with wireless subject incentives. As such, our results address this research gap by comparing cash to reloadable bank card payment methods, and suggesting that a wireless incentive structure may help to improve retention in clinical research, particularly when a study is collecting repeated outcome measures remotely.
Retention issues in clinical intervention studies are particularly important when working with vulnerable populations such as patients with mental health and substance abuse problems and those who are economically disadvantaged and difficult-to-reach due to the unstable nature of their housing. Women experiencing IPV overlap with many of these populations, and have the additional issue related to limited methods of safe contact. The study protocol for the larger RCT was designed to meet the ethical, confidentiality, and safety guidelines for a population experiencing intimate partner violence, while utilizing innovative technologies to address common IPV study challenges including recruitment, retention, and missing outcome data (Clough et al., 2010; Sullivan et al., 1996; Uybico et al., 2007; Zink & Putnam, 2005). The 2009 large RCT of IPV screening by MacMillian et al. (2009) experienced attrition rates exceeding 40% in both groups, and the women who were at higher risk and had greater abuse at baseline were more likely to be lost to follow up. Despite previous successes and suggested approaches of other longitudinal IPV studies (Clough et al., 2010; Sullivan et al., 1996; Zink & Putnam, 2005), this low retention rate led the authors to speculate that it might be impossible to obtain adequate long-term follow up with abused women (MacMillian et al., 2009). Furthermore, low rates of participation and nonresponse bias in IPV studies are often linked to concerns about safety. A recent study described the population in the 2006 Behavioral Risk Factor Surveillance System (BRFSS) that declined participation in an IPV survey due to safety concerns in relation to those who screened positive for IPV and associated demographic variables (i.e. age, race/ethnicity, education, and presence of children) (Ranney, Madsen, & Gjelsvik, 2012). Findings reinforce the notion that little is known about why participants indicate safety as a reason for declining participation in IPV studies, which undoubtedly influences both nonresponse bias and subject retention in study participation. Our study provides a potential procedural remedy for at least one aspect of this methodological problem – implementing flexible, confidential asynchronous data collection methods paired with more immediate, remote subject compensation.
Conclusions
The results of this study indicate that use of wireless subject incentives provided via reloadable bank cards improved completion rates compared to cash incentives for repetitive, longitudinal data collection and long-term retention in a randomized clinical trial among abused women drinkers. Future studies should continue to refine and assess the impact of asynchronous measures of both data collection and provision of wireless subject incentives on both study retention and the safety of women in abusive relationships and other vulnerable populations.
Acknowledgments
The authors wish to acknowledge the following individuals: Co-Investigators - Marilyn Sommers, Andrea Doyle, Elizabeth Datner; Statistical support - Alexandra Hanlon, and Jesse Chittams; Research Staff - Salem Wolk Valentino, Marissa Sherman, Erica Dobbins, Catherine Buttner, Kate Watson, Katherine Carroll, Cjloe Vinoya, Julie Tennille, Casey Bohrman, Alyssa Goodin, Hannah Jones-Lewis, Megan Schutt, Catherine Monsky; Reloadable Bank Card Administration - Katie Koller, Maria Rugarber, and Hannah Adkins.
Funding: This project is funded by the National Institute on Alcohol Abuse and Alcoholism (NIAAA) Award R01-AA018705. The funding source had no role in the design, execution and will not have any role during analyses and interpretation of the data or decision to submit results.
Biographies
Melissa A. Rodgers, M.Ed. is a graduate student at The University of Texas at Austin studying Quantitative Methods in Educational Psychology. Her recent research interests include research design and analytic methods to address attrition in longitudinal research. For this study, she functioned as the project manager for the large randomized control trial and oversaw the implementation of the reloadable bank card incentive system.
Zachary F. Meisel, MD MPH MSHP is co-director of the Center for Emergency Care Policy Research and Assistant Professor of Emergency Medicine at the Perelman School of Medicine at the University of Pennsylvania. He is senior fellow at the Leonard Davis Institute of Health Economics and Medical Editor of The Health Economist: A Policy Journal from the Leonard Davis Institute of Health Economics. Dr. Meisel is associate editor at Academic Emergency Medicine, the official journal for the Society for Academic Emergency Medicine. Dr. Meisel’s research interests cover emergency care access and utilization, patient safety, emergency medical services, implementation science, comparative effectiveness research.
Douglas Wiebe, PhD is an Associate Professor of Epidemiology in Biostatistics and Epidemiology at the Perelman School of Medicine, University of Pennsylvania. His research interests include environmental risk factors for injury, alcohol use and alcohol availability, the methodologic challenges of exposure measurement, and the impact of daily routines on health-related behavior. A number of his studies examine how keeping a firearm at home relates to homicide, suicide, and unintentional shootings of household members.
Paul Crits-Christoph, PhD is a Professor of Psychology in Psychiatry and Director of the Center for Psychotherapy Research in the Department of Psychiatry, University of Pennsylvania. His research has focused on psychosocial treatments for depressive, anxiety, and substance use disorders. Most recently his work has examined the effectiveness of psychosocial treatments in community settings.
Karin V. Rhodes, MD MS is Vice President for Care Management Design & Evaluation and Professor of Emergency Medicine and Psychiatry at Northwell Health System/Hofstra School of Medicine. Prior to this role she was a Senior Fellow in the Leonard Davis Institute of Health Economics and founding director of the Center of Emergency Care Policy Research Perelman School of Medicine, with appointments in Departments of Emergency Medicine, Psychiatry, and the School of Social Policy & Practice at the University of Pennsylvania. A former Robert Wood Johnson Clinical Scholar, her research focuses on developing effective patient-centered responses to health-related social problems impacting individual and public health.
Appendix A
Table A.1.
Negative Binomial Regression Models of Total Call Completed with significant predictors
| Model 1 | Model 2 | |||||||
|---|---|---|---|---|---|---|---|---|
| B | SE | 95% CI | Exp B | B | SE | 95% CI | Exp B | |
| Payment (Card Paid) | .850* | .428 | .011 – 1.689 | 2.340 | .357* | .076 | .207 – .507 | 1.429 |
| Group | .044 | .061 | −.075 – .163 | 1.045 | ||||
| Month | --** | -- | -- | -- | ||||
| AUDIT Score | −.004 | .012 | −.028 – .019 | .996 | ||||
| CTS2S Score | −.001 | .006 | −.013 – .011 | .999 | ||||
| Age | .008* | .003 | .002 – .014 | 1.008 | .008* | .003 | .002 – .013 | 1.008 |
| AUDIT Score* Payment type | −.001 | .014 | −.028 – .026 | .999 | ||||
| CTS2S Score* Payment type | .007 | .007 | −.008 – .021 | 1.007 | ||||
| Constant | .969 | .507 | −.025 – 1.963 | 2.635 | 1.378* | .113 | 1.157 – 1.599 | 3.967 |
| −2 Log Likelihood | 3049.621 | 3032.966 | ||||||
| Chi-square | 16.655 | |||||||
Model 2 includes only significant predictors detected in Model 1, and there is no significant differences in model fit.
p < .05
Month is included in the model and only 3 months detected significant results.
References
- Bair-Merritt MH, Jennings JM, Chen R, Burrell L, McFarlane E, Fuddy L, Duggan AK. Reducing maternal intimate partner violence after the birth of a child: a randomized controlled trial of the Hawaii Healthy Start Home Visitation Program. Archives of Pediatrics & Adolescent Medicine. 2010;164(1):16–23. doi: 10.1001/archpediatrics.2009.237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barber JS, Kusunoki Y, Gatny HH. Design and implementation of an online weekly journal to study unintended pregnancies. Vienna Yearbook of Population research/Vienna Institute of Demography, Austrian Academy of Sciences. 2011;9:327. doi: 10.1553/populationyearbook2011s327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Babor TF, Higgins-Biddle JC, Saunders JB, Monteiro MG. AUDIT, the Alcohol Use Disorders Identification Test: guidelines for use in primary health care. 2. Geneva: Substance Abuse Department, World Health Organization, WHO/MSD/MSB/01.6a; 2001. pp. 1–38. [Google Scholar]
- Blackstone MM, Wiebe DJ, Mollen CJ, Kalra A, Fein JA. Feasibility of an interactive voice response tool for adolescent assault victims. Academic Emergency Medicine. 2009;16(10):956–962. doi: 10.1111/j.1553-2712.2009.00519.x. [DOI] [PubMed] [Google Scholar]
- Chermack ST, Bonar EE, Ilgen MA, Walton MA, Cunningham RM, Booth BM, Blow FC. Developing an integrated violence prevention for men and women in treatment for substance use disorders. Journal of Interpersonal Violence. 2015 doi: 10.1177/0886260515586369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell R, Sprague HB, Cottrill S, Sullivan CM. Longitudinal research with sexual assault survivors: A methodological review. Journal of interpersonal violence. 2011;26(3):433–461. doi: 10.1177/0886260510363424. [DOI] [PubMed] [Google Scholar]
- Cliff N. Dominance statistics: Ordinal analyses to answer ordinal questions. Psychological Bulletin. 1993;114:494–509. [Google Scholar]
- Clough A, Wagman J, Rollins C, Barnes J, Connor-Smith J, Holditch-Niolon P, … Glass N. The SHARE Project: maximizing participant retention in a longitudinal study with victims of intimate partner violence. Field Methods. 2011;23(1):86–101. doi: 10.1177/1525822X10384446. [DOI] [Google Scholar]
- Corkrey R, Parkinson L. A comparison of four computer-based telephone interviewing methods: getting answers to sensitive questions. Behavior Research Methods, Instruments, & Computers. 2002;34(3):354–363. doi: 10.3758/bf03195463. [DOI] [PubMed] [Google Scholar]
- de Meneses-Gaya C, Zuardi AW, Loureiro SR, Crippa JAS. Alcohol Use Disorders Identification Test (AUDIT): An updated systematic review of psychometric properties. Psychology & Neuroscience. 2009;2(1):83. [Google Scholar]
- Doody MM, Sigurdson AS, Kampa D, Chimes K, Alexander BH, Ron E, Tarone RE, Linet MS. Randomized trial of financial incentives and delivery methods for improving response to a mailed questionnaire. American Journal of Epidemiology. 2003;157(7):643–51. doi: 10.1093/aje/kwg033. [DOI] [PubMed] [Google Scholar]
- Dunn LB, Gordon NE. Improving informed consent and enhancing recruitment for research by understanding economic behavior. JAMA: The Journal of the American Medical Association. 2005;293(5):609–612. doi: 10.1001/jama.293.5.609. [DOI] [PubMed] [Google Scholar]
- Dutton MA, Holtzworth-Murone A, Jouriles E, McDonarld R, Krishnan S, McFarlane J, Sullivan C. Recruitment and retention in intimate partner violence research. Washington, D.C: U.S. Department of Justice, National Institute of Justice; 2003. [Google Scholar]
- Emanuel EJ. Undue inducement: nonsense on stilts? The American Journal of Bioethics. 2005;5(5):9–13. doi: 10.1080/15265160500244959. [DOI] [PubMed] [Google Scholar]
- Festinger DS, Marlowe DB, Dugosh KL, Croft JR, Arabia PL. Higher magnitude cash payments improve research follow-up rates without increasing drug use or perceived coercion. Drug and Alcohol Dependence. 2008;96(1–2):128–135. doi: 10.1016/j.drugalcdep.2008.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gatny HH, Couper MP, Axinn WG, Barber JS. Using debit cards for incentive payments: experiences of a weekly survey study. Survey Practice. 2009;2(7):1–5. [Google Scholar]
- Grady C. Money for research participation: does it jeopardize informed consent? American Journal of Bioethics. 2001;1(2):40–44. doi: 10.1162/152651601300169031. [DOI] [PubMed] [Google Scholar]
- Grady C, Dickert N, Jawetz T, Gensler G, Emanuel E. An analysis of U.S. practices of paying research participants. Contemporary Clinical Trials. 2005;26:365–375. doi: 10.1016/j.cct.2005.02.003. [DOI] [PubMed] [Google Scholar]
- Grissom RJ, Kim JJ. Effect sizes for research: Univariate and multivariate applications. 2. New York, NY: Taylor & Francis; 2012. [Google Scholar]
- Hilbe JM. Negative binomial regression. Cambridge University Press; Chicago: 2011. [Google Scholar]
- Johansson BA, Remvall S, Malgerud R, Lindgren A, Andersson C. Interactive voice response-an automated follow-up technique for adolescents discharged from acute psychiatric inpatient care: a randomised controlled trial. SpringerPlus. 2013;2(1):146. doi: 10.1186/2193-1801-2-146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kew S. Text messaging: an innovative method of data collection in medical research. BMC Research Notes. 2010;3:342. doi: 10.1186/1756-0500-3-342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McFarlane J. Strategies for successful recruitment and retention of abused women for longitudinal studies. Issues in Mental Health Nursing. 2007;28:883–97. doi: 10.1080/01612840701493527. [DOI] [PubMed] [Google Scholar]
- MacMillan HL, Wathen CN, Jamieson E, Boyle MH, Shannon HS, Ford-Gilboe M, … McMaster Violence Against Women Research Group. Screening for intimate partner violence in health care settings: a randomized trial. JAMA: Journal of American Medical Association. 2009;302(5):493–501. doi: 10.1001/jama.2009.1089. [DOI] [PubMed] [Google Scholar]
- Mechanic MB, Pole N. Methodological considerations in conducting ethnoculturally sensitive research on intimate partner abuse and its multidimensional consequences. Sex Roles. 2013;69(3–4):205–225. doi: 10.1007/s11199-012-0246-z. [DOI] [Google Scholar]
- Moyers T, Martin T, Manuel JK, Miller WR, Ernst D. [Accessed July 13, 2015];Revised Global Scales: Motivational Interviewing Treatment Integrity 3.1.1 (MITI 3.1.1) 2010 at http://casaa.unm.edu/download/miti3_1.pdf.
- National Institutes of Health (NIH) Healthy volunteers help scientists conquer disease. U.S. Department of Health, Education and Welfare, Public Health Service, NIH; Bethesda, Maryland, USA: 1959. [Google Scholar]
- Patel MX, Doku V, Tennakoon L. Challenges in recruitment of research participants. Advances in Psychiatric Treatment. 2003;9(3):229–238. doi: 10.1007/s11199-012-0246-z. [DOI] [Google Scholar]
- Piette JD, Rosland AM, Marinec NS, Striplin D, Bernstein SJ, Silveira MJ. Engagement with automated patient monitoring and self-management support calls: experience with a thousand chronically ill patients. Medical Care. 2013;51(3):216–223. doi: 10.1097/MLR.0b013e318277ebf8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ranney ML, Choo EK, Spirito A, Mello MJ. Adolescents’ preference for technology-based emergency department behavioral interventions: does it depend on risky behaviors? Pediatric Emergency Care. 2013;29(4):475–481. doi: 10.1097/PEC.0b013e31828a322f. [DOI] [PubMed] [Google Scholar]
- Ranney ML, Madsen T, Gjelsvik A. Predictors of being unsafe: participation in the Behavioral Risk Factor Surveillance System 2006 intimate partner violence module. Journal of Interpersonal Violence. 2012;27(1):84–102. doi: 10.1177/0886260511416470. [DOI] [PubMed] [Google Scholar]
- Rhodes KV, Rodgers M, Sommers M, Hanlon A, Chittams J, Doyle A, Datner E, Crits-Christoph P. Brief motivational intervention for intimate partner violence and heavy drinking in the emergency department: a randomized clinical trial. JAMA: Journal of American Medical Association. 2015;314(5):466–477. doi: 10.1001/jama.2015.8369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rhodes KV, Rodgers MA, Sommers M, Hanlon A, Crits-Christoph P. The Social Health Intervention Project (SHIP): Protocol for a randomized controlled clinical trial assessing the effectiveness of a brief motivational intervention for problem drinking and intimate partner violence in an urban emergency department. BMC Emergency Medicine. 2014 doi: 10.1186/1471-227X-14-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Searles JS, Perrine MW, Mundt JC, Helzer JE. Self-report of drinking using touch-tone telephone: extending the limits of reliable daily contact. Journal of Studies on Alcohol. 1995;56:375–382. doi: 10.15288/jsa.1995.56.375. [DOI] [PubMed] [Google Scholar]
- Scott CK, Sonis J, Creamer M, Dennis ML. Maximizing follow-up in longitudinal studies of traumatized populations. Journal of Traumatic Stress. 2006;19(6):757–770. doi: 10.1002/jts.20186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schulz KF, Grimes DA. Sample size slippages in randomised trials: exclusions and the lost and wayward. Lancet. 2002;359:781–85. doi: 10.1016/S0140-6736(02)07882-0. [DOI] [PubMed] [Google Scholar]
- South-Paul JE, Ncube CN, Lin CJ, Nowalk MP, Kagwima RN, Wheeler EA, … Adeyeye A. Strategies for recruitment and retention of teen mothers in a program to prevent repeat pregnancy. Journal of Adolescent and Family Health. 2014;6(2):1. [Google Scholar]
- Straus MA, Douglas EM. A short form of the Revised Conflict Tactics Scales, and typologies for severity and mutuality. Violence and Victims. 2004;19(5):507–520. doi: 10.1891/vivi.19.5.507.63686. [DOI] [PubMed] [Google Scholar]
- Sullivan CM, Cain D. Ethical and safety considerations when obtaining information from or about battered women for research purposes. Journal of Interpersonal Violence. 2004;19(5):603–618. doi: 10.1177/0886260504263249. [DOI] [PubMed] [Google Scholar]
- Sullivan CM, Rumptz MH, Campbell R, Eby KK, Davidson WS. Retaining participants in longitudinal community research: a comprehensive protocol. The Journal of Applied Behavioral Science. 1996;32(3):262–276. [Google Scholar]
- United States Food & Drug Administration (US FDA) Guidance for institutional review boards and clinical investigators: payment to research subjects. 1998 http://www.fda.gov/oc/ohrt/irbs/default.htm.
- University of Notre Dame Comptroller. Prepaid Card for Research Participants Flier. 2011 Retrieved August 30, 2015, from http://controller.nd.edu/assets/91728/flier.pdf.
- UyBico SJ, Pavel S, Gross CP. Recruiting vulnerable populations into research: a systematic review of recruitment interventions. Journal of General Internal Medicine. 2007;22(6):852–863. doi: 10.1007/s11606-007-0126-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- VanGeest J, Wynia M, Cummins D, Wilson B. Effects of different monetary incentives on the return rate of a national mail survey of physicians. Medical Care. 2001;39:197–201. doi: 10.1097/00005650-200102000-00010. [DOI] [PubMed] [Google Scholar]
- Whitford HM, Donnan PT, Symon AG, Kellett G, Monteith-Hodge E, Rauchhaus P, Wyatt JC. Evaluating the reliability, validity, acceptability, and practicality of SMS text messaging as a tool to collect research data: results from the Feeding Your Baby project. Journal of the American Medical Informatics Association. 2012;19(5):744–749. doi: 10.1136/amiajnl-2011-000785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wiebe DJ, Carr BG, Datner EM, Elliott MR, Richmond TS. Feasibility of an automated telephone survey to enable prospective monitoring of subjects whose confidentiality is paramount: a four-week cohort study of partner violence recurrence after Emergency Department discharge. Epidemiologic Perspectives & Innovations. 2008;5(1):1. doi: 10.1186/1742-5573-5-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wiebe DJ, Blackstone MM, Mollen CJ, Culyba AJ, Fein JA. Self-reported violence-related outcomes for adolescents within eight weeks of emergency department treatment for assault injury. Journal of Adolescent Health. 2011;49(4):440–442. doi: 10.1016/j.jadohealth.2011.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zink T, Putnam F. Intimate partner violence research in the health care setting: what are appropriate and feasible methodological standards? Journal of Interpersonal Violence. 2005;20(4):365–372. doi: 10.1177/0886260504267548. Author Bios. [DOI] [PubMed] [Google Scholar]