Abstract
Objective
The objective of this study is to answer three questions: (1) Is perceived discrimination adversely related to self-rated stress via the social capital and health care system distrust pathways? (2) Does the relationship between perceived discrimination and self-rated stress vary across race/ethnicity groups? And (3) do the two pathways differ by one’s race/ethnicity background?
Design
Using the Philadelphia Health Management Corporation’s Southeastern Pennsylvania Household Survey, we classified 9,831 respondents into four race/ethnicity groups: non-Hispanic White (n=6,621), non-Hispanic Black (n=2,359), Hispanic (n=505), and non-Hispanic other races (n=346). Structural equation modeling was employed to simultaneously estimate five sets of equations, including the confirmatory factor analysis for both social capital and health care distrust and both direct and indirect effects from perceived discrimination to self-rated stress.
Results
The key findings drawn from the analysis include the following: (1) in general, people who experienced racial discrimination have higher distrust and weaker social capital than those without perceived discrimination and both distrust and social capital are ultimately related to self-rated stress. (2) The direct relationship between perceived discrimination and self-rated stress is found for all race/ethnicity groups (except non-Hispanic other races) and it does not vary across groups. (3) The two pathways can be applied to non-Hispanic White and Black, but for Hispanic and non-Hispanic other races, we found little evidence for the social capital pathway.
Conclusions
For non-Hispanic White, non-Hispanic Black, and Hispanic, perceived discrimination is negatively related to self-rated stress. This finding highlights the importance of reducing interpersonal discriminatory behavior even for non-Hispanic White. The health care system distrust pathway can be used to address the racial health disparity in stress as it holds true for all four race/ethnicity groups. On the other hand, the social capital pathway seems to better help non-Hispanic White and Black to mediate the adverse effect of perceived discrimination on stress.
Keywords: stress, discrimination, health care system distrust, social capital, structural equation modeling
Introduction
In the United States (US), racial disparities in health outcomes remain large and pervasive despite recent efforts to minimize the gaps across racial groups. In general, the White population enjoys the best health outcomes compared to other racial/ethnic groups (NCHS 2013). While the factors associated with socioeconomic status, such as educational attainment and income, may account for some of the racial disparities in health outcomes, the difference in socioeconomic inequality does not directly translate into a difference in health outcomes (Braveman 2012). In the past decade, perceived racial discrimination has been identified as a determinant of racial health disparities (Jones 2000, Williams and Mohammed 2009, Williams, Neighbors, and Jackson 2003) and there is a growing interest in exploring the mechanisms through which perceived racial discrimination is associated with health (Brondolo, Gallo, and Myers 2009, Brondolo et al. 2011, Benkert et al. 2006).
While several psychophysiological mechanisms (e.g., anxiety and depression) from perceived discrimination and health have been documented (Pascoe and Richman 2009, Brondolo et al. 2011), relatively few studies explore the socio-attitudinal pathways linking perceived discrimination and health. The goal of this study is to fill this gap by exploring whether social capital and health care system distrust mediate the adverse effect of perceived discrimination on self-rated stress and examining whether the pathways differ by race/ethnicity.
Perceived racial discrimination refers to the unfair treatment an individual perceives due to his/her race/ethnicity (Clark et al. 1999) and it may occur in different social encounters and levels (e.g., institutional and interpersonal discrimination). Though it may be true that White individuals may not experience institutional discrimination (Wellman 2007, Feagin 2009), they are still subject to interpersonal discrimination, which is the core of perceived discrimination particularly since the Civil Rights Era (Pager and Shepherd 2008). To thoroughly understand these mechanisms, it is necessary to include the racial/ethnic majority. Furthermore, given the institutional discrimination history in the US, discrimination in housing markets has drawn researchers’ attention (Wienk 1979, Yinger 1995). One significant/well-documented consequence of discrimination in housing markets is the forcing of minorities to live in substandard housing areas (Williams and Mohammed 2009), which may undermine interpersonal relationships and lead to health disparities. Similarly, the health care system has a legacy of mistreating minorities (Brandon, Isaac, and LaVeist 2005) and personal experiences in getting medical care may also directly influence health behaviors/outcomes and cause health disparities. Recently, the institutional performance model has suggested that when an individual has a high level of health care system distrust, s/he tends to distrust other social institutions, which in turn may create additional stress for an individual (Blendon 2007). This study situates the discriminatory experience in these two social contexts to better connect perceived discrimination to stress.
Self-rated daily stress has been found to be negatively related to mental and physical health (DeLongis, Folkman, and Lazarus 1988, Thoits 2010) and it takes psychological and social resources to adequately cope. As Brondolo and colleagues suggested (2009), perceived discrimination is a well-known stressor. It should be emphasized that the same stressor may generate different levels of stress as individuals have different access to the mediators (or resources), which makes perceived discrimination less stressful for some but more stressful for others. Should the mechanisms proposed in this study be confirmed, our findings will shed new light on mitigating the relationship of perceived discrimination in getting suitable housing and medical care with stress. The next section will elaborate on the research framework, explain why social capital and health care system distrust could serve as mediators, and propose the research hypothesis.
Research framework and literature review
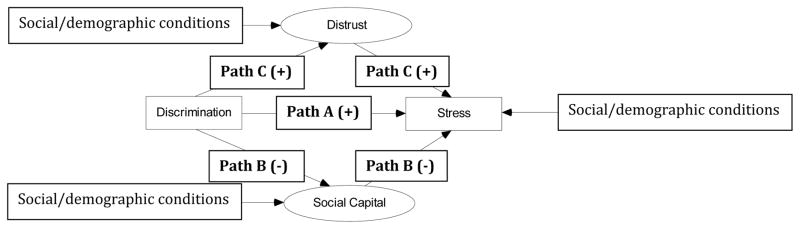
Figure 1 illustrates three social and attitudinal pathways through which perceived racial discrimination may be associated with stress in the context of getting housing and medical care. First, Path A suggests that individual discriminatory experience has a direct association with stress. As discussed previously, perceived racial discrimination may cause stress that must be mediated at the expense of social or psychological resources. Specifically, following the work by Lazarus and Folkman (1984), racial discrimination could be understood as a factor appraised by an individual that may be “taxing or exceeding his or her resources and endangering his or her well-being” (p.19). Individuals may exhibit physiological responses to the stressors and eventually take coping actions (e.g., problem-focused and emotion-focused coping) to manage perceived discrimination (Pascoe and Richman 2009). In addition, exposure to racial discrimination may leave an individual more susceptible to future stressful social situations or other stressful events (Guyll, Matthews, and Bromberger 2001), which increases overall stress levels in daily life. It has been found that recurring racial discrimination may deprive an individual of protective resources and undermine the ability to fight stress or related illness (Gee et al. 2007). Explicitly, perceived racial discrimination may directly augment daily stress due to the biological and social over- or under-reactions.
Figure 1.
The structural model linking perceived racial discrimination to self-rated stress
Note: The measurement model is not included in the figure. Rectangles and ovals denote manifest variables and latent variables respectively.
The relationship between perceived discrimination and stress has been well-documented in the literature with an emphasis on minority groups. For example, Bynum and colleagues (2007) found that high exposure to racial discrimination is associated with high psychological stress among African American adolescents. Peters (2006), who focused on the African American adult population, reported similar findings. Thoits (2010) reviewed research on the relationships between a range of social dimensions (e.g., race and socioeconomic status) and stress over the past few decades. She concluded that people belonging to minority groups experience more stress throughout their lifetime than their counterparts in the dominant racial group, even after controlling for other potential confounders. The literature provides substantial evidence to support the direct path from perceived racial discrimination to stress. Nonetheless, previous research overlooked the possibility that perceived racial discrimination may work differently across unique racial/ethnic groups as the Public Health Critical Race Praxis suggested (Thrasher et al. 2012). Despite recent efforts to explore racial differences in the effect of discrimination on health (Brondolo et al. 2011), little attention has been paid to the comparisons between the racial/ethnic majority and minority groups, and even less is known about whether there is any racial difference in the socio-attitudinal pathways between perceived discrimination and stress.
As this study situates the discriminatory experience in the housing market and health care system, both proposed pathways in our framework are closely related to these social contexts. Perceived racial discrimination is hypothesized to be related to stress through social capital and social capital may buffer the adverse association of perceived discrimination with stress (Path B). In this study, social capital refers to the social relationships that may create many forms of resources (both tangible and intangible) and the social relationships are based on interactions, reciprocity, and mutual trust among individuals (Putnam 2001, Dean et al. 2014). Discriminatory experience in the housing market may result in an individual residing in a less desirable neighborhood where his/her interaction with other residents may be constrained. Furthermore, the development of interpersonal relationships could then be undermined resulting from a weak sense of belonging and attachment and depreciation of personal connections (Burt, Simons, and Gibbons 2012). Consequently, an individual’s social relationships may be compromised, which may not buffer the adverse relationship between perceived discrimination and stress. In addition, social capital is not unlimited (Jasinskaja-Lahti et al. 2006), thus when people use it to cope with perceived discrimination (e.g., emotion-focused coping), social capital decreases consequentially and stress may ultimately be generated (Gee et al. 2007). It should also be noted that the relationship between perceived discrimination and social capital has been hypothesized to be negative but this remains empirically underexplored (Brondolo et al. 2012). This study is among the first to explicitly examine whether perceived discrimination is negatively related to social capital, even though this relationship is only a part of the research framework.
The other reason for the negative relationship between perceived discrimination and social capital is that one’s experience of racial discrimination may trigger certain behavior changes (Brondolo, Gallo, and Myers 2009). For example, coping with perceived racial discrimination costs time and effort, which makes individuals less energetic or willing to engage in social activities or interactions (Pascoe and Richman 2009), thus hindering the development of social capital. Similarly, perceived racial discrimination makes it more likely for a person to appraise routine social interactions as harassment or being unfair (Broudy et al. 2007) and reduce an individual’s investment in social capital (e.g., participation in community activities). As social capital has been found to facilitate health (Kawachi, Subramanian, and Kim 2008), people with weak social capital are expected to have high levels of stress.
Experiencing racial discrimination when obtaining medical care is hypothesized to increase an individual’s distrust of the health care system and subsequently lead to high stress (Path C).2 Distrust of the health care system is defined as an individual’s perception that the health care system does not employ key values, such as respect, honesty, dependability, and the capacity/techniques to make patients healthy (Shea et al. 2008). Why does perceived racial discrimination increase distrust? Discriminatory medical care experience may lead individuals to believe that the health care system does not serve in the patient’s best interest, hence the quality of their interaction with the medical system will be poor (Harris et al. 2012, Thrasher et al. 2008). Consequently, individuals who experienced racial discrimination see the health care system through a different lens and will develop higher distrust of the health care system than those without discriminatory experience. Armstrong and colleagues (2013) conducted a survey in 40 US metropolitan statistical areas to investigate whether the experience of racial discrimination creates distrust of the health care system. The authors found that perceived racial discrimination is positively related to distrust of the health care system and this relationship cannot be fully explained by individual sociodemogrpahic features (e.g., gender), access to health resources, and residential segregation at the metropolitan level (Armstrong et al. 2013). This suggests that perceived discrimination has an independent effect on distrust.
Recent literature has found that health care system distrust is negatively related to various health outcomes and behaviors such as self-rated health (Armstrong et al. 2006) and the use of preventive health care (Musa et al. 2009, Yang, Matthews, and Hillemeier 2011). However, relatively little is known about the association of distrust with stress. We argue that distrust of the health care system aggravates an individual’s stress for the following four reasons: (1) High distrust may prevent a person from seeking appropriate medical help in addressing health issues (Whetten et al. 2006), leading to a stressful situation. (2) Increased distrust is associated with poor evaluation of the health care system, which makes individuals skeptical about the treatment they receive (Deale and Wessely 2001). This lack of confidence in medical treatment generates even more burden on stress. (3) Patients with greater distrust will spend more time and resources on managing the issues derived from distrust (e.g., insurance bills) to the extent that one’s available resources for other stressful events may be overused. (4) According to the institutional performance model (Blendon 2007), a high level of distrust of the health care system may lead an individual to distrust other social institutions (e.g., educational system and government), which generates additional stress for an individual. Should the resources for coping with stress be reduced, an individual’s day-to-day stress will inevitably increase.
The following reasons suggest that it is necessary to explore whether he mechanisms linking perceived discrimination and stress vary by race/ethnicity. First, perceived racial discrimination is less common among non-Hispanic whites, which implies that the association of perceived discrimination with health (i.e., stress) may be different from other groups (LaVeist, Rolley, and Diala 2003). That is, the perceived discrimination experience may be qualitatively different between non-Hispanic whites and other race/ethnicity groups. Second, non-Hispanic whites, in general, have better socioeconomic profiles than other minorities and they have better access to resources that can cope with the association between perceived discrimination and health. The differences in socioeconomic status may hence make the mechanisms vary by race/ethnicity. Finally, minorities and non-Hispanic whites have different social identities and the implications of perceived discrimination for health may differ by race/ethnicity. While these reasons indicate that there may be a racial/ethnic difference in the mechanisms, a recent study did not find a significant difference in the effect of discrimination on self-rated health among minority groups (Brondolo et al. 2011). Such a finding suggests that discrimination is adversely associated with health regardless of race/ethnicity. Little attention has been paid to the difference between non-Hispanic whites and other minorities. This study will fill that gap.
To reiterate, we propose three pathways from perceived racial discrimination to stress. Path A represents the direct association between racial discrimination experience and stress. Social capital (Path B) and health care system distrust (Path C) are hypothesized to carry the indirect impacts of perceived racial discrimination on stress, representing potential changes in social behavior and attitude. We propose the following research hypotheses:
-
(H1)
After accounting for other individual socioeconomic and demographic features and the two indirect pathways, perceived racial discrimination is positively associated with stress (Path A).
-
(H2)
Assuming that all other conditions are the same, discriminatory experience is negatively related to social capital, which is also negatively related to stress (Path B).
-
(H3)
Controlling for other confounders, experiencing racial discrimination increases health care system distrust and subsequently augments stress (Path C).
-
(H4)
The direct association between perceived racial discrimination and stress could be observed across all racial/ethnic groups, though it does not vary from one group to the next.
-
(H5)
The two indirect pathways through which perceived racial discrimination exerts its influence on stress could be applied to all racial/ethnic groups; however, the effects do not vary by race/ethnicity group.
Data and methods
Data
The Public Health Management Corporation’s (PHMC) 2008 Southeastern Pennsylvania Household Health Survey provides data that can be effectively used for testing the hypotheses above. Using the computerized telephone random digit dialing technique and a stratified sampling framework, the PHMC conducted interviews in five counties of the Philadelphia metropolitan area (Bucks, Chester, Delaware, Montgomery, and Philadelphia). The target population includes residents at least 18 years old living in these counties. When needed, the interview was conducted in Spanish. The PHMC offers balancing weights that adjust for sampling bias and retain the sample size of the survey, which is designed for multivariate analysis (PHMC 2008). As such, we subsequently applied these balancing weights to our multivariate analysis. The goal of the PHMC survey was to collect information on health status, health behaviors, experience with health care, and access to health services so that researchers could conduct analysis and address public health concerns. The quality and accurate representation of the PHMC survey have been verified by comparing the PHMC data with other large surveys (Yang and Matthews 2010, Yang, Matthews, and Hillemeier 2011),3 suggesting high external validity of the 2008 PHMC survey.
The 2008 PHMC provided five exclusive race/ethnicity categories: non-Hispanic White, non-Hispanic Black, Hispanic, Asian, and other races (including multiracial and Native American). In order to have sufficient sample sizes for the race/ethnicity-specific analysis, we collapsed Asians and other races into one category to increase sample size (non-Hispanic other races). Consequently, this study has four race/ethnicity groups: non-Hispanic White (N=6,621), non-Hispanic Black (N=2,359), Hispanic (N=505), and non-Hispanic other races (N=346). The race-specific analysis is necessary for testing our last two hypotheses.
Measures
The final variable of interest, self-rated stress, was obtained by asking the respondents to assess how much day-to-day stress they experienced, with 1 indicating “no stress” and 10 representing “an extreme amount of stress.” The stress literature has suggested that evaluating stress with a satisfactory and objective inventory list is difficult, if not impossible, since whether an event is stressful is subject to an individual’s perception, interpretation, and understanding of that event (Lazarus and Folkman 1984). That said, the same event may be stressful to one person but not to another. Lazarus (1990) proposed that a subjective measure, i.e., self-rated stress, could better reflect the combination of events (or environmental demands) and an individual’s ability to manage them rather than just a set of events that may be stressful. The PHMC survey adopted this approach and subjective evaluation of day-to-day stress has been used in previous research (Yang and Matthews 2010). The single-item self-rated stress approach has been validated. For example, it has been found a 5-point Likert scale stress indicator is a useful tool to screen psychological issues (Lim, Williams, and Hagen 2005). Other scholars reached the same conclusion that a single-item stress measure is valid and reliable in health research (Elo, Leppänen, and Jahkola 2003, Littman et al. 2006).
Perceived racial discrimination was considered as a dichotomous variable. The respondents were asked if they have “ever experienced discrimination, been prevented from doing something or been hassled or made to feel inferior in events like receiving medical care or searching for housing because of their race, ethnicity, or color.” The attribution of the discrimination experience is set at “race, ethnicity, or color,” which is consistent with the approach developed by Krieger and Sidney (1996). Those who answered yes were coded 1, otherwise 0. While perceived racial discrimination may not fully reflect actual racial discrimination, the research and findings based on an individual’s perception of discriminatory behaviors are important in their own right (Pager and Shepherd 2008) and the single item self-reported discrimination has been included in other surveys administered by Federal agencies, e.g. the Behavioral Risk Factor Surveillance System and the National Longitudinal Survey of Youth.
Social capital was treated as a latent construct and measured with the following four variables: (1) Neighbor’s willingness to help. Participants answered the question of “how likely people in your neighborhood are willing to help their neighbors with routine activities such as picking up their trash cans, or helping to shovel snow.” The answers were coded from 1 (never) to 5 (always). (2) Sense of belonging. A 4-point Likert scale was used, which reflects respondent’s assessment of whether s/he feel that s/he belongs and is a part of the neighborhood. Those who strongly agreed with this statement were coded 4, whereas those who strongly disagreed were coded 1. (3) Sense of neighborhood trust. This variable was measured using a similar approach. Participants were asked if they “strongly disagree,” “disagree,” “agree,” or “strongly agree” with the notion that most people in their neighborhood can be trusted. Those who strongly agreed were coded 4 and those who strongly disagreed were coded 1. (4) Neighborhood improvement. This was a dichotomous variable based on whether a respondent agreed (coded 1) that people in his or her neighborhood worked together to improve the neighborhood, such as developing a neighborhood watch, creating a community garden, or building a community playground. Respondents who disagreed with this statement were coded 0. These variables have been included in other surveys, such as the Los Angeles Family and Neighborhood Survey (Carpiano 2007) and a recent study used similar variables to define social capital in the same study area (Dean et al. 2014). These four variables in the PHMC survey had a Cronbach’s Alpha Coefficient of 0.67.
The distrust of the health care system was also treated as a latent construct that could be measured with a nine-item scale developed by Shea and colleagues (2008). Specifically, respondents were asked to gauge their level of agreement with a 5-point Likert scale on nine different statements about the health care system, such as “health care system makes patients’ health better” and “health care system makes too many mistakes.” We coded respondents’ answers so that higher values indicate higher distrust levels in order to capture the concept of distrust. Though the reliability and validity of the nine-item distrust scale has been discussed and reported elsewhere (Armstrong et al. 2006, Shea et al. 2008), the Alpha of this distrust scale was 0.82 and removing any of the nine statements would decrease the reliability.
Following the literature (Turner and Lloyd 1999, Turner, Wheaton, and Lloyd 1995, Yang and Matthews 2010), we consider several social and demographic variables in the analysis to be control variables. Specifically, age was measured by years and treated as a continuous variable and gender was a dichotomous variable where male was coded 1 and female coded 0. Those who were married or living with a partner were coded 1 in marital status and other statuses (e.g., single or widowed) were coded 0. These three demographic features are associated with stress because one’s ability to cope with stress changes at different life stages. For example, Turner and Lloyd (1999) found that females were found to be sensitive to stressors and marriage may bring new stressors for individuals. Similarly, one’s resources for coping with stress depend on income and education (Turner, Wheaton, and Lloyd 1995, Lazarus and Folkman 1984). In the PHMC survey, income was classified into 19 levels (1–19) with larger numbers indicating higher income and treated as an ordinal variable in the analysis. Educational attainment, categorized into five groups (i.e., four dummy variables), was included in the analysis as follows: less than high school (reference group), high school graduate, some college, college graduate, and post-college.
Beyond the social and demographic features, we considered two health outcomes that are associated with stress: depression and high blood pressure (Hicken et al. 2014, Tsai, Chi, and Wang 2013). Respondents who were clinically diagnosed with depression or high blood pressure were coded 1 in these variables, otherwise 0. The purpose of including the health-related variables in the analysis is to control for the factors that may contribute to self-rated stress. It should be noted that excluding the health-related variables in our analysis does not alter the findings and conclusions and the results without the health variables can be found in Appendices A, B, and C.
Analytic method– structural equation modeling
This study employed structural equation modeling (SEM) procedures to verify the hypothesized pathways (in the research framework) linking perceived racial discrimination to stress. Additionally, the SEM was an effective means to test whether the theoretical pathways are statistically the same across the four race/ethnicity groups. Using the program AMOS Version 22 (Byrne 2009), we used the full information maximum likelihood estimation method which takes missing values into account and gives us a well-fitted model. We followed the procedure suggested by Anderson and Gerbing (1988) to first establish valid measurement models for social capital and distrust (the two key concepts in the pathways) and then estimate the measurement models and structural equations simultaneously (the measurement modeling results are not shown but available upon request). In the third step, we revised the proposed model specifications in accordance with modification indices obtained in the second step, and estimated the model using all respondents. Multiple-group analyses were applied to the four race/ethnicity groups thereafter to appropriately test group differences.
A variety of model fit indices are available in SEM, but there is no agreement on which indices should be chosen (Byrne 2009). This study assessed the model fit (i.e., goodness-of-fit) by the Comparative Fit Index (CFI) and the Root Mean Square Error of Approximation (RMSEA) (Bentler 1990, Hatcher and O’Rourke 2013). A CFI value greater than 0.9 or a RMSEA value less than 0.05 would indicate good model fit. Due to the space constraint, we opted not to discuss how to estimate the full model and test group differences in detail but the technical details are available upon request.
Results
The descriptive statistics of the variables discussed above are presented in Table 1 where the first column demonstrated the results for all respondents, followed by race-specific findings. Overall, approximately two out of three respondents were non-Hispanic White. Among minorities, about 73 percent were non-Hispanic Black; 16 percent were Hispanic. Roughly 11 out of 100 minority respondents reported other racial groups in the PHMC survey. We further examined whether there is any significant difference between non-Hispanic White and each minority group in the variables and summarized several notable findings in Table 1 as follows. First, about 20 percent of the minorities in our data experienced racial discrimination and this figure did not change significantly by race/ethnicity. In contrast to other minority groups, only 4 percent of non-Hispanic White reported any discriminatory experience. Second, the non-Hispanic Black respondents, on average, reported the lowest day-to-day stress, which was lower than the average stress of non-Hispanic White. No significant difference in stress was found for other minority groups. Third, in comparison to non-Hispanic White respondents, the non-Hispanic Black and other race/ethnicity groups reported higher distrust. Hispanics, however, had a distrust level comparable to non-Hispanic Whites. With respect to social capital measures, the non-Hispanic White respondents tended to have stronger social capital than their minority counterparts, with the exception of neighborhood improvement. Fourth, Hispanic had the highest prevalence of depression and non-Hispanic Black respondents were the most vulnerable to high blood pressure. Finally, as for social and demographic features, non-Hispanic Black participants were less likely to both be married or living with a partner and be well-educated than non-Hispanic White. Non-Hispanic White respondents were found to have higher income and more years of schooling than other minority participants.
Table 1.
Descriptive Statistics of the variables used in this study by racial/ethnic groups
| Variable Name | Full Sample (N=9,831) | Non-Hispanic White (N=6,621) | Non-Hispanic Black (N=2,359) | Hispanic (N=505) | Other Races (N=346) | |||
|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
|
||||
| Mean (S.D.) or % | Mean (S.D.) or % | Mean (S.D.) or % | Mean (S.D.) or % | Mean (S.D.) or % | ||||
|
|
|
|
|
|
||||
| Stress (1–10) | 5.27 (2.67) | 5.30 (2.55) | 5.17 (2.91) | * | 5.39 (3.00) | 5.38 (2.73) | ||
| Discrimination (1=Yes, 0=No) | 9.39% | 4.06% | 20.28% | *** | 20.84% | *** | 18.71% | *** |
| Health care system distrust | ||||||||
| Distrust1 (1–5) | 2.77 (1.13) | 2.73 (1.12) | 2.87 (1.16) | *** | 2.68 (1.13) | 2.91 (1.16) | ** | |
| Distrust2 (1–5) | 3.56 (1.05) | 3.52 (1.05) | 3.67 (1.06) | *** | 3.50 (1.06) | 3.64 (1.04) | * | |
| Distrust3 (1–5) | 2.78 (1.07) | 2.68 (1.04) | 3.04 (1.11) | *** | 2.75 (1.06) | 2.90 (1.10) | *** | |
| Distrust4 (1–5) | 3.07 (1.08) | 3.03 (1.08) | 3.18 (1.09) | *** | 3.00 (1.05) | 3.11 (1.09) | ||
| Distrust5 (1–5) | 3.57 (1.12) | 3.51 (1.14) | 3.73 (1.08) | *** | 3.43 (1.13) | † | 3.73 (1.07) | ** |
| Distrust6 (1–5) | 2.78 (1.02) | 2.71 (1.00) | 2.96 (1.06) | *** | 2.74 (1.02) | 2.85 (1.05) | ** | |
| Distrust7 (1–5) | 3.21 (1.19) | 3.14 (1.18) | 3.44 (1.19) | *** | 3.04 (1.23) | † | 3.19 (1.26) | |
| Distrust8 (1–5) | 3.07 (1.11) | 2.95 (1.10) | 3.36 (1.08) | *** | 2.99 (1.12) | 3.26 (1.07) | *** | |
| Distrust9 (1–5) | 2.69 (1.09) | 2.47 (1.00) | 3.23 (1.10) | *** | 2.84 (1.10) | *** | 2.90 (1.13) | *** |
| Neighborhood social capital | ||||||||
| Willingness to help (1–5) | 3.60 (1.20) | 3.72 (1.14) | 3.36 (1.26) | *** | 3.27 (1.39) | *** | 3.43 (1.20) | *** |
| Neighborhood improvement (1=Yes, 0=No) | 60.84% | 57.09% | 72.71% | *** | 53.75% | 59.88% | ||
| Sense of belonging (1–4) | 3.17 (0.71) | 3.23 (0.67) | 3.07 (0.76) | *** | 3.03 (0.78) | *** | 3.07 (0.75) | *** |
| Trust (1–4) | 3.04 (0.77) | 3.20 (0.68) | 2.66 (0.84) | *** | 2.72 (0.87) | *** | 2.92 (0.79) | *** |
| Health conditions‡ | ||||||||
| Depression (1=Yes, 0=No) | 13.70% | 14.00% | 12.07% | * | 19.32% | ** | 13.29% | |
| High blood pressure (1=Yes, 0=No) | 34.59% | 31.84% | 44.59% | *** | 28.51% | 22.38% | *** | |
| Social/demographic characteristics | ||||||||
| Age | 52.38 (16.22) | 54.48 (15.74) | 49.47 (16.40) | *** | 43.08 (15.18) | *** | 44.14 (15.66) | *** |
| Gender (1=Male, 0=Female) | 32.30% | 33.71% | 27.61% | *** | 30.10% | † | 38.60% | † |
| Married or living with a partner (1=Yes, 0=No) | 54.80% | 62.11% | 36.17% | *** | 47.42% | *** | 51.45% | *** |
| Income level (1–19) | 12.14 (5.66) | 13.42 (5.14) | 9.371 (5.636) | *** | 8.442 (6.077) | *** | 12.426 (5.493) | ** |
| Educational attainment (Less than high school graduate=Reference) | ||||||||
| High school graduate (1=Yes, 0=No) | 32.22% | 29.78% | 41.58% | *** | 29.17% | 21.45% | *** | |
| Some college (1=Yes, 0=No) | 20.07% | 18.88% | 23.51% | *** | 19.44% | 20.58% | ||
| College graduate (1=Yes, 0=No) | 24.25% | 27.43% | 16.45% | *** | 15.08% | *** | 28.12% | |
| Post-college (1=Yes, 0=No) | 15.97% | 18.94% | 7.53% | *** | 10.32% | *** | 23.77% | * |
Note: significance levels were obtained by conducting two-sample t-tests for continuous or dummy variables and Mann-Whitney U-tests for ordinal variables with Non-Hispanic Black as the reference group.
p≤0.001,
p≤0.01,
p≤0.05,
p≤0.1
Please see appendices for the results without health conditions.
After having a basic understanding of the 2008 PHMC data, we conducted SEM analysis and demonstrated the results in Table 2, which includes unstandardized path coefficient estimates from five sets of structural equations (standardized coefficients are available upon request). The unstandardized coefficients are used to facilitate comparison across samples; whereas the standardized coefficients are important in determining the relative magnitude of different variables in a given sample (Schumacker and Lomax 2004). Before discussing the key findings, it should be emphasized that the goodness-of-fit diagnostics, CFI and RMSEA (see Table 2), suggested that the full-sample SEM and multiple-group SEM model both fit the data well. The estimated relationships in our research framework are reliable and robust.
Table 2.
Path coefficient estimates from structural equation modeling
| Equation | Dependent variable | Independent variable / Latent construct | SEM | Multiple-group SEM (Unconstrained) | |||
|---|---|---|---|---|---|---|---|
|
|
|
||||||
| Full Sample | Non-Hispanic White | Non-Hispanic Black | Hispanic | Other Races | |||
|
|
|
|
|
|
|||
| Coef. (S.E.) | Coef. (S.E.) | Coef. (S.E.) | Coef. (S.E.) | Coef. (S.E.) | |||
|
|
|
|
|
|
|
||
| (1) | Distrust1 | Distrust | 0.89 (0.02)*** | 0.85 (0.02)*** | 0.97 (0.05)*** | 0.89 (0.12)*** | 0.90 (0.11)*** |
| Distrust2 | Distrust | 0.66 (0.02)*** | 0.70 (0.02)*** | 0.57 (0.04)*** | 0.44 (0.10)*** | 0.80 (0.10)*** | |
| Distrust3 | Distrust | 0.87 (0.02)*** | 0.81 (0.02)*** | 0.94 (0.04)*** | 0.79 (0.12)*** | 1.01 (0.11)*** | |
| Distrust4 | Distrust | 0.90 (0.02)*** | 0.90 (0.02)*** | 0.92 (0.04)*** | 0.81 (0.11)*** | 1.06 (0.11)*** | |
| Distrust5 | Distrust | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | |
| Distrust6 | Distrust | 0.85 (0.02)*** | 0.80 (0.02)*** | 0.95 (0.04)*** | 0.86 (0.11)*** | 0.93 (0.10)*** | |
| Distrust7 | Distrust | 0.86 (0.02)*** | 0.76 (0.02)*** | 1.06 (0.05)*** | 1.11 (0.14)*** | 0.95 (0.12)*** | |
| Distrust8 | Distrust | 0.95 (0.02)*** | 0.90 (0.02)*** | 1.00 (0.04)*** | 1.01 (0.12)*** | 1.01 (0.10)*** | |
| Distrust9 | Distrust | 0.81 (0.02)*** | 0.69 (0.02)*** | 0.90 (0.04)*** | 0.75 (0.12)*** | 0.84 (0.11)*** | |
| (2) | Willingness to help | Neighborhood social capital | 1.48 (0.03)*** | 1.35 (0.04)*** | 1.55 (0.08)*** | 2.18 (0.24)*** | 0.97 (0.13)*** |
| Neighborhood improvement | Neighborhood social capital | 0.29 (0.01)*** | 0.31 (0.02)*** | 0.37 (0.03)*** | 0.62 (0.07)*** | 0.26 (0.05)*** | |
| Sense of belonging | Neighborhood social capital | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | |
| Trust | Neighborhood social capital | 1.09 (0.03)*** | 0.93 (0.03)*** | 1.08 (0.06)*** | 0.96 (0.13)*** | 0.99 (0.12)*** | |
| (3) | Distrust | Discrimination | 0.58 (0.03)*** | 0.54 (0.05)*** | 0.51 (0.04)*** | 0.38 (0.09)*** | 0.67 (0.11)*** |
| Distrust | Age | 0.00 (0.00)*** | 0.00 (0.00)*** | 0.00 (0.00) | 0.00 (0.00) | 0.01 (0.00)* | |
| Distrust | Male | −0.13 (0.02)*** | −0.17 (0.02)*** | −0.04 (0.04) | 0.00 (0.07) | −0.12 (0.08) | |
| Distrust | Married or living with a partner | −0.04 (0.02)* | 0.00 (0.03) | −0.03 (0.04) | −0.10 (0.07) | −0.03 (0.09) | |
| Distrust | Income level | −0.01 (0.00)*** | −0.01 (0.00)*** | 0.01 (0.00) | 0.00 (0.01) | −0.01 (0.01) | |
| Distrust | High school graduate | 0.10 (0.03)** | −0.04 (0.05) | 0.11 (0.05)* | 0.20 (0.09)* | 0.16 (0.18) | |
| Distrust | Some college | 0.18 (0.04)*** | −0.02 (0.05) | 0.27 (0.06)*** | 0.41 (0.11)*** | 0.23 (0.19) | |
| Distrust | College graduate | 0.00 (0.04) | −0.21 (0.05)*** | 0.19 (0.07)** | 0.35 (0.13)** | 0.18 (0.19) | |
| Distrust | Post-college | −0.02 (0.04) | −0.19 (0.06)*** | 0.14 (0.08)† | 0.26 (0.14)† | 0.01 (0.21) | |
| (4) | Neighborhood social capital | Discrimination | −0.21 (0.02)*** | −0.19 (0.04)*** | −0.15 (0.03)*** | −0.08 (0.07) | −0.09 (0.09) |
| Neighborhood social capital | Age | 0.01 (0.00)*** | 0.01 (0.00)*** | 0.01 (0.00)*** | 0.02 (0.01)** | 0.01 (0.01)* | |
| Neighborhood social capital | Male | −0.01 (0.01) | −0.04 (0.02)** | 0.06 (0.03)* | 0.08 (0.06) | 0.15 (0.07)* | |
| Neighborhood social capital | Married or living with a partner | 0.08 (0.01)*** | 0.09 (0.02)*** | 0.03 (0.03) | 0.05 (0.06) | 0.01 (0.08) | |
| Neighborhood social capital | Income level | 0.02 (0.00)*** | 0.02 (0.00)*** | 0.02 (0.00)*** | 0.02 (0.01)* | 0.03 (0.01)*** | |
| Neighborhood social capital | High school graduate | 0.01 (0.02) | 0.08 (0.04)* | −0.01 (0.04) | −0.02 (0.07) | 0.14 (0.16) | |
| Neighborhood social capital | Some college | 0.04 (0.03) | 0.11 (0.04)** | 0.05 (0.05) | −0.04 (0.08) | 0.11 (0.17) | |
| Neighborhood social capital | College graduate | 0.07 (0.03)** | 0.14 (0.04)*** | 0.04 (0.05) | 0.03 (0.10) | 0.14 (0.17) | |
| Neighborhood social capital | Post-college | 0.10 (0.03)*** | 0.16 (0.04)*** | 0.12 (0.06)† | −0.06 (0.11) | 0.12 (0.18) | |
| (4) | Stress | Discrimination | 0.39 (0.09)*** | 0.64 (0.15)*** | 0.59 (0.15)*** | 0.54 (0.31)† | 0.53 (0.40) |
| Stress | Health care system distrust | 0.46 (0.04)*** | 0.51 (0.05)*** | 0.45 (0.10)*** | 0.63 (0.25)* | 0.57 (0.25)* | |
| Stress | Neighborhood social capital | −0.64 (0.07)*** | −0.63 (0.07)*** | −0.63 (0.15)*** | −1.20 (0.35)*** | −0.79 (0.31)* | |
| Stress | Depression | 1.49 (0.07)*** | 1.14 (0.09)*** | 1.86 (0.17)*** | 2.20 (0.32)*** | 1.41 (0.42)*** | |
| Stress | High blood pressure | 0.37 (0.06)*** | 0.28 (0.07)*** | 0.72 (0.12)*** | 1.11 (0.29)*** | 0.43 (0.38) | |
| Stress | Age | −0.04 (0.00)*** | −0.04 (0.00)*** | −0.05 (0.00)*** | −0.05 (0.01)*** | −0.03 (0.01)** | |
| Stress | Male | −0.57 (0.05)*** | −0.52 (0.06)*** | −0.78 (0.13)*** | −0.69 (0.26)** | −0.25 (0.30) | |
| Stress | Married or living with a partner | 0.03 (0.06) | −0.12 (0.07)† | 0.22 (0.12)† | −0.03 (0.26) | −0.22 (0.32) | |
| Stress | Income level | 0.02 (0.01)* | 0.01 (0.01) | −0.02 (0.01) | 0.04 (0.03) | 0.04 (0.04) | |
| Stress | High school graduate | −0.07 (0.10) | 0.07 (0.14) | −0.29 (0.19) | −0.65 (0.34)† | −0.10 (0.66) | |
| Stress | Some college | 0.08 (0.11) | 0.14 (0.15) | 0.02 (0.22) | −0.25 (0.40) | 0.09 (0.68) | |
| Stress | College graduate | 0.17 (0.12) | 0.23 (0.15) | −0.09 (0.24) | 0.11 (0.47) | −0.15 (0.69) | |
| Stress | Post-college | 0.38 (0.13)** | 0.39 (0.16)* | 0.25 (0.29) | 0.52 (0.52) | 0.26 (0.74) | |
|
|
|
||||||
| CFI | 0.941 | 0.946 | |||||
| RMSEA (CI) | 0.042 (0.041, 0.043) | 0.020 (0.020, 0.021) | |||||
Note: A CFI value larger than 0.9 or a RMSEA value smaller than 0.05 indicate good model fit.
p≤0.001,
p≤0.01,
p≤0.05,
p≤0.1
The first set of equations included the associations between the latent construct of distrust in the health care system and the nine distrust items, which is comparable to the confirmatory factor analysis. Echoing the distrust literature (Armstrong et al., 2006; Shea et al., 2008), each item was significantly related to the latent construct of distrust and these results did not change across racial groups. That is, the nine-item distrust scale is robust and reliable in this study. The results in the second set of equations suggested that each social capital indicator was strongly associated with the construct of social capital, suggesting these variables captured social capital well.
The third and fourth sets of equations aimed to examine the associations of racial discrimination with distrust and social capital, respectively, after controlling for other social and demographic variables. In general, respondents who perceived racial discrimination were more likely to report high distrust of the health care system and low social capital. We also found that the magnitude of the impact of racial discrimination on distrust was larger than that on social capital. This pattern was observed within each racial group (standardized coefficients also bolster this finding). However, it should be noted that the inverse relationship between racial discrimination and social capital was not statistically significant among Hispanic and non-Hispanic other races. In addition, distrust of the health care system seemed to be associated with educational attainment more than other demographic features (particularly among non-Hispanic Black and Hispanic), whereas social capital was more closely related to age and income.
The last set of equations embraced the whole research framework using stress as the ultimate dependent variable. It first showed that perceived racial discrimination was positively and significantly associated with day-to-day stress among minorities. The analysis using samples of all respondents showed that, ceteris paribus, those who perceived discriminatory behaviors had a stress level that was roughly 0.39 units higher than the stress level reported by those who did not experience racial discrimination. It is worth noting that the direct impact of racial discrimination was not statistically significant after controlling for the distrust and social capital mechanisms for Hispanic and non-Hispanic other races.
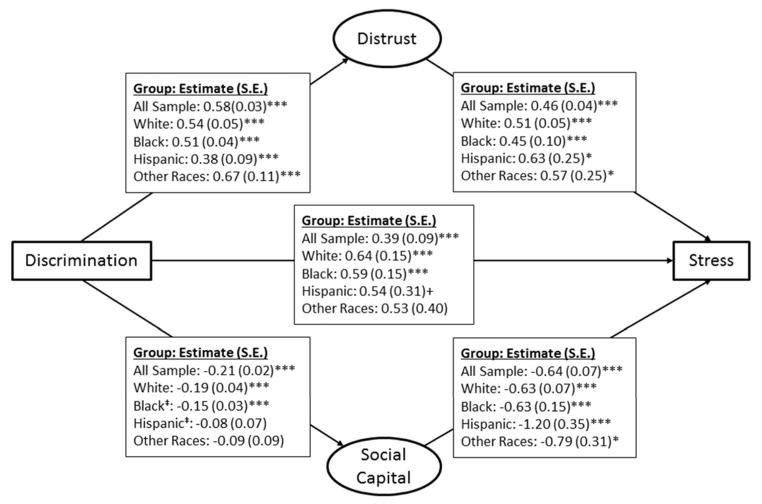
After accounting for other covariates, distrust of the health care system was found to be positively associated with stress and this positive association did not change across racial groups. According to the full sample model, a one unit increase in distrust was related to a 0.46 unit increase in stress. Social capital buffered the association between perceived discrimination and stress (−0.64 for the full sample model). The race-specific results indicated that a one unit increase in social capital was related to roughly a 0.63 (both non-Hispanic White and Black) to 1.20 (Hispanic) unit decrease in stress. The standardized coefficients suggested that social capital was a more important determinant of self-rated stress than distrust (results not shown). We incorporated these findings into our research framework (see Figure 2) to illustrate this.
Figure 2.
Summary of key estimates of both direct and indirect pathways from perceived discrimination to self-rated stress
Note: The estimates and standard errors are based on Table 2. ‡ indicates significant difference from non-Hispanic White.
In addition, we used pairwise parameter comparisons (Arbuckle 2011) to formally compare the magnitudes of coefficients from the multiple-group analysis (Table 3). Using non-Hispanic White as the reference group, we found that non-Hispanic Black demonstrated stronger relationships between the indicators and the latent constructs of distrust and social capital. Few differences were found between non-Hispanic other races and White. This finding indicates that the measurements used to capture social capital and distrust fit the non-Hispanic Black population better than non-Hispanic White. The associations between the latent construct for neighborhood social capital and various indicators were stronger for non-Hispanic Black and Hispanic, but weaker for non-Hispanic other races, all in comparison to non-Hispanic White. Among the determinants of distrust, educational attainment has a stronger association on non-Hispanic Black and Hispanic than non-Hispanic White. This pattern was observed for the association between perceived discrimination and social capital.
Table 3.
Comparison of path coefficients across racial/ethnic groups
| Equation | Dependent variable | Independent variable / Factor | Multiple-group SEM (Unconstrained) | |||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Non-Hispanic Black vs. White | Hispanic vs. White | Other Races vs. White | ||||||
|
|
|
|
||||||
| Z score | Z score | Z score | ||||||
|
|
|
|
|
|||||
| (1) | Distrust1 | Distrust | 2.43 | * | 0.26 | 0.41 | ||
| Distrust2 | Distrust | −2.89 | ** | −2.49 | * | 1.04 | ||
| Distrust3 | Distrust | 2.83 | ** | −0.16 | 1.82 | † | ||
| Distrust4 | Distrust | 0.39 | −0.81 | 1.45 | ||||
| Distrust5 | Distrust | |||||||
| Distrust6 | Distrust | 3.20 | ** | 0.51 | 1.22 | |||
| Distrust7 | Distrust | 5.84 | *** | 2.48 | * | 1.57 | ||
| Distrust8 | Distrust | 2.23 | * | 0.98 | 1.16 | |||
| Distrust9 | Distrust | 4.23 | *** | 0.45 | 1.35 | |||
| (2) | Willingness to help | Neighborhood social capital | 2.16 | * | 3.46 | *** | −2.74 | ** |
| Neighborhood improvement | Neighborhood social capital | 2.12 | * | 4.16 | *** | −0.89 | ||
| Sense of belonging | Neighborhood social capital | |||||||
| Trust | Neighborhood social capital | 2.28 | * | 0.16 | 0.49 | |||
| (3) | Distrust | Discrimination | −0.44 | −1.54 | 1.11 | |||
| Distrust | Age | 2.46 | * | 2.46 | * | 3.78 | *** | |
| Distrust | Male | 3.05 | ** | 2.28 | * | 0.56 | ||
| Distrust | Married or living with a partner | −0.70 | −1.26 | −0.28 | ||||
| Distrust | Income level | 4.25 | *** | 1.38 | 0.86 | |||
| Distrust | High school graduate | 2.04 | * | 2.24 | * | 1.01 | ||
| Distrust | Some college | 3.53 | *** | 3.47 | *** | 1.24 | ||
| Distrust | College graduate | 4.69 | *** | 4.01 | *** | 1.93 | † | |
| Distrust | Post-college | 3.41 | *** | 2.99 | ** | 0.96 | ||
| (4) | Neighborhood social capital | Discrimination | 3.41 | *** | 2.99 | ** | 0.96 | |
| Neighborhood social capital | Age | 0.87 | 1.60 | 1.09 | ||||
| Neighborhood social capital | Male | 3.29 | ** | 2.02 | * | 2.55 | * | |
| Neighborhood social capital | Married or living with a partner | −1.98 | * | −0.69 | −0.98 | |||
| Neighborhood social capital | Income level | −0.95 | −0.47 | 1.29 | ||||
| Neighborhood social capital | High school graduate | −1.63 | −1.15 | 0.35 | ||||
| Neighborhood social capital | Some college | −1.06 | −1.64 | −0.05 | ||||
| Neighborhood social capital | College graduate | −1.52 | −1.04 | −0.02 | ||||
| Neighborhood social capital | Post-college | −0.52 | −1.78 | † | −0.18 | |||
| (5) | Stress | Discrimination | −0.24 | −0.28 | −0.27 | |||
| Stress | Health care system distrust | −0.57 | 0.45 | 0.22 | ||||
| Stress | Neighborhood social capital | −0.02 | −1.63 | −0.50 | ||||
| Stress | Depression | 3.78 | *** | 3.25 | ** | 0.63 | ||
| Stress | High blood pressure | 3.16 | ** | 2.79 | ** | 0.40 | ||
| Stress | Age | −1.36 | −0.48 | 0.96 | ||||
| Stress | Male | −1.88 | † | −0.65 | 0.86 | |||
| Stress | Married or living with a partner | 2.43 | * | 0.34 | −0.29 | |||
| Stress | Income level | −1.54 | 1.08 | 0.97 | ||||
| Stress | High school graduate | −1.48 | −1.96 | † | −0.24 | |||
| Stress | Some college | −0.45 | −0.92 | −0.06 | ||||
| Stress | College graduate | −1.14 | −0.24 | −0.54 | ||||
| Stress | Post-college | -0.43 | 0.24 | −0.18 | ||||
p≤0.001,
p≤0.01,
p≤0.05,
p≤0.1
With respect to the direct impact of perceived racial discrimination on stress, we did not find statistically significant differences between any racial groups. Similarly, the associations of distrust and social capital with stress did not vary significantly by race/ethnicity. However, the effects of depression and high blood pressure on stress were stronger for non-Hispanic Black and Hispanic than for White. Moreover, the impact of marital status on stress was stronger for non-Hispanic Black than for White.
One advantage of the SEM approach is that it allows researchers to decompose the total effect of one variable on another into direct and indirect effects by pathway (Li 2011). As the goal of this study is to examine the pathways from perceived racial discrimination to stress, we summarized the direct and indirect effects into Table 4 (based on the coefficients in Table 2). The results drawn from the full sample demonstrated that the direct effect of perceived racial discrimination on stress accounts for almost 50 percent of the total effect. The pathway from perceived racial discrimination to stress through health care system distrust explained another 33 percent of the total effect, whereas the remaining 17 percent can be understood through the social capital mechanism. The race-specific model suggested that the direct effect of perceived discrimination on stress ranged between 54 percent (non-Hispanic other races) and 65 percent (non-Hispanic Black). As for the indirect effect, the pathway through health care system distrust (25~39 percent) remained more important than that through social capital (7~12 percent).
Table 4.
Decomposing the unstandardized effects of discrimination on stress
| SEM | Multiple-group SEM (Unconstrained) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
||||||||||
| Full Sample | Non-Hispanic White | Non-Hispanic Black | Hispanic | Other races | |||||||
|
|
|
|
|
|
|||||||
| Total effect | 0.792 | 100.00% | 1.036 | 100.00% | 0.909 | 100.00% | 0.873 | 100.00% | 0.977 | 100.00% | |
| Direct effect | 0.394 | 49.76% | 0.641 | 61.87% | 0.589 | 64.81% | 0.544 | 62.32% | 0.527 | 53.92% | |
| Indirect effect through | Health care system distrust | 0.264 | 33.30% | 0.273 | 26.38% | 0.228 | 25.05% | 0.239 | 27.35% | 0.381 | 38.97% |
| Neighborhood social capital | 0.134 | 16.94% | 0.122 | 11.74% | 0.092 | 10.14% | 0.090 | 10.33% | 0.069 | 7.10% | |
We would like to note that all the analyses above have been duplicated with the data excluding non-Hispanic White. The multi-group comparisons used non-Hispanic Black as the reference group and, similar to the findings above, we did not find significant racial/ethnic differences in the relationships between perceived discrimination and stress. Other key findings were not changed and these results are available upon request.
Discussion and conclusion
The data in Philadelphia suggested that roughly 20 percent of minority members have perceived racial discrimination when getting medical care or housing, in contrast to just 4 percent of non-Hispanic White reporting discriminatory experience. While the figures were slightly lower than those reported in earlier studies (Kessler, Mickelson, and Williams 1999, LaVeist, Rolley, and Diala 2003), the difference may be attributed to the decreasing trend in discrimination and regional variation. Using the SEM results above, we revisited the research hypotheses accordingly. We first hypothesized that, after controlling for other covariates and indirect pathways, perceived racial discrimination is positively associated with stress (H1). The SEM results in Table 2 generally provided evidence to support this hypothesis but the race-specific analysis further suggested that among Hispanic and non-Hispanic other races, taking both indirect mechanisms into consideration may fully explain the association between racial discrimination and stress. Our empirical findings not only echoed previous research (Bynum, Burton, and Best 2007, Peters 2006, Thoits 2010) where it was found that African Americans are more likely to suffer from perceived racial discrimination than others, but also suggested that the two proposed social and attitudinal pathways may account for the adverse impact of racial discrimination on stress among Hispanic and other minority groups.
Second, we proposed that discriminatory experience is indirectly associated with stress through the social capital (H2) and distrust (H3) mechanisms. We found evidence to bolster both hypotheses (model with full samples). Results for equations (3) and (4) in Table 2 first confirmed that paths from perceived racial discrimination to both social capital and health care system distrust, and the results for equation (5) shed light on the research framework of this study. More specifically, in contrast to those without discriminatory experience, people who perceived racial discrimination were found to have poorer social capital, which in turn increases stress. This indirect mechanism from perceived racial discrimination to stress echoed the literature on social capital and health. As Brondolo and colleagues (2009) suggested, perceived racial discrimination may trigger unhealthy behaviors and consume resources for coping with stress. Consequently, this can prevent an individual from participating in social activities or cause a person to evaluate social interaction negatively (Pascoe and Richman 2009, Broudy et al. 2007), thus undermining the development of social capital. As such, the beneficial effects of social capital on health (Gee et al. 2007) are minimized and the stress level increases. It should also be noted that the relationship between perceived discrimination and social capital was not significant for Hispanic and non-Hispanic other races.
In regard to the pathway through distrust, we found strong evidence to support the idea that perceived racial discrimination increases one’s level of health care system distrust. Discriminatory behaviors hinder an individual’s belief in the quality of patient care and the effectiveness of treatment, contributing to an increased level of distrust (Armstrong et al. 2013, Thrasher et al. 2008). The resulting elevated distrust may discourage certain healthy behaviors, such as the use of preventive health care (Musa et al. 2009, Yang, Matthews, and Hillemeier 2011, Yang, Matthews, and Anderson 2013). In turn, this effect may increase the fear of illness and exacerbate stress. In addition, distrust itself may cost an individual additional time and effort managing his/her health-related issues, leading to an increase in stress (Lazarus and Folkman 1984).
Third, we contended that the direct association between perceived racial discrimination and stress could be observed for all racial/ethnic groups and not vary across groups (H4), which was partially supported. Specifically, the relationship between racial discrimination and stress was observed for all racial/ethnic groups (except non-Hispanic other races) in Table 2 and the multi-group comparisons indicated that this association did not vary (Table 3) between non-Hispanic White and other minority groups. This finding echoes a recent study (Brondolo et al. 2011) and demonstrates that discrimination is detrimental to health regardless of one’s race/ethnicity. The adverse effect of discrimination on stress was not significant for non-Hispanic other races. Our last hypothesis (H5) stated that both indirect pathways through which perceived racial discrimination exerts its influence on stress could be observed in all racial groups, which was not fully supported by the multiple-group analysis in Table 2. We found strong evidence for the two pathways for non-Hispanic White and non-Hispanic Black. However, the relationship between discrimination and social capital was not significant for Hispanic and non-Hispanic other races, indicating that the social capital pathway may not hold for these two race/ethnicity groups. This non-significant finding for Hispanics implied that there may be some factors buffering the effect of perceived discrimination on social capital and these factors may contribute to our understanding of the Hispanic health paradox (Ruiz, Steffen, and Smith 2013). Due to the limitations of our data, we are unable to examine this path in this study.
This study has several limitations. First, the PHMC survey is cross-sectional and focuses on the population in the Philadelphia metropolitan area. The causality between stress and perceived racial discrimination should be understood as tentative and one should be cautious in generalizing our findings to give insight on other populations or areas. Second, there is no agreement on how to measure the two latent constructs (i.e., distrust and social capital) in this study and using different measures may alter the findings and conclusions. In addition, our measurements of perceived discrimination and stress are single-item and this study situates perceived discrimination in medical system and housing market, which does not allow us to further understand whether (and how contexts matter). Though some studies found the single-item discrimination and stress measurements to be valid and reliable (Elo, Leppänen, and Jahkola 2003, Littman et al. 2006, Hausmann et al. 2008), future studies should address these limitations.
Third, racial discrimination may occur in other social domains that are not covered by this study, such as seeking employment, and attaining education (Pager and Shepherd 2008, Quillian 2006, Benner and Graham 2011). Discrimination may also develop over time and occur with different frequency and periodicity. However, this study is not able to consider all of these factors due to data limitations. Future research should investigate whether (and how) different measures of racial discrimination (e.g., job discrimination) and/or different levels (or frequencies) of exposure to discriminatory behaviors are related to stress (Sternthal, Slopen, and Williams 2011). Fourth, while this study confirms two mechanisms from perceived racial discrimination to stress via distrust and social capital, these pathways are not exhaustive. That said, researchers should explore other mechanisms to provide a better understanding of how perceived racial discrimination gets under the skin. Finally, in the Philadelphia metropolitan area, the non-Hispanic Asian or Pacific Islander population is relatively small and the heterogeneity within each race/ethnicity group (e.g., Mexicans and Cubans) cannot be considered in our analysis. Future efforts are warranted to explore whether the mechanisms work for other minority groups.
Some policy implications can be drawn from this study. First and foremost, the fact that the undesirable effects of perceived discrimination on stress do not vary by race/ethnicity underscores the importance of reducing discrimination. Health professions and people working in the housing market should receive training in cultural competency techniques, such as language and cultural immersion (Brach and Fraserirector 2000). Doing so will also reduce the detrimental impact of distrust on stress. Furthermore, as social capital mediates the relationship between perceived discrimination and stress, facilitating mutual trust and reciprocity within a neighborhood will ultimately promote population health. For example, the promotion of neighborhood walks or community gardens can provide opportunities for residents to interact and build trust, which is an essential component of the social capital that reduces stress.
In sum, using data from the Philadelphia metropolitan area, this study confirmed that perceived racial discrimination (in acquiring medical care or housing) has an adverse and direct impact on stress, even after adjusting for other confounders. Beyond this direct pathway, this study provided evidence to support that perceived racial discrimination exerts its influence on stress via elevated distrust and reduced social capital. These effects were particularly strong for non-Hispanic White and Black populations.
Supplementary Material
Footnotes
Acknowledgment: We acknowledge assistance provided by the Center for Social and Demographic Analysis at the University at Albany, State University of New York, which receives core funding from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD; R24-HD04494309).
Distrust of health care system is not directly related to one’s health care providers so it does not fit the definition of social capital in this study and should be treated as an independent mechanism.
PHMC accounts for cell phone samples and the balancing weights adjust for cell phone samples as well. The response rate of the 2008 PHMC was 25% according to the criterion 3 of the American Association for Public Opinion Research
Contributor Information
Tse-Chuan Yang, Department of Sociology, Center for Social and Demographic Analysis, University at Albany, SUNY, Address: 315 Arts and Sciences Building, 1400 Washington Ave., Albany, NY 12222
Danhong Chen, Department of Agricultural Economics and Agribusiness, University of Arkansas
References
- Anderson James C, Gerbing David W. Structural equation modeling in practice: A review and recommended two-step approach. Psychological bulletin. 1988;103(3):411. [Google Scholar]
- Arbuckle James L. IBM SPSS Amos 20 user’s guide. Armonk, NY: IBM; 2011. [Google Scholar]
- Armstrong Katrina, Putt Mary, Halbert Chanita H, Grande David, Schwartz Jerome Sanford, Liao Kaijun, Marcus Noora, Demeter Mirar B, Shea Judy A. Prior experiences of racial discrimination and racial differences in health care system distrust. Medical Care. 2013;51(2):144–150. doi: 10.1097/MLR.0b013e31827310a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Armstrong Katrina, Rose Abigail, Peters Nikki, Long Judith A, McMurphy Suzanne, Shea Judy A. Distrust of the health care system and self-reported health in the United States. Journal of General Internal Medicine. 2006;21(4):292–297. doi: 10.1111/j.1525-1497.2006.00396.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benkert Ramona, Peters Rosalind M, Clark Rodney, Keves-Foster Kathryn. Effects of perceived racism, cultural mistrust and trust in providers on satisfaction with care. Journal of the National Medical Association. 2006;98(9):1532. [PMC free article] [PubMed] [Google Scholar]
- Benner Aprile D, Graham Sandra. Latino adolescents’ experiences of discrimination across the first 2 years of high school: Correlates and influences on educational outcomes. Child Development. 2011;82(2):508–519. doi: 10.1111/j.1467-8624.2010.01524.x. [DOI] [PubMed] [Google Scholar]
- Bentler Peter M. Comparative fit indexes in structural models. Psychological bulletin. 1990;107(2):238. doi: 10.1037/0033-2909.107.2.238. [DOI] [PubMed] [Google Scholar]
- Blendon RJ. Why Americans don’t trust the government and don’t trust healthcare. In: Shore DA, editor. The Trust Crisis in Healthcare: Causes, Consequences, and Cures. New York: Oxford University Press; 2007. pp. 21–31. [Google Scholar]
- Brach Cindy, Fraserirector Irene. Can cultural competency reduce racial and ethnic health disparities? A review and conceptual model. Medical Care Research and Review. 2000;57(4 suppl):181–217. doi: 10.1177/1077558700057001S09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brandon Dwayne T, Isaac Lydia A, LaVeist Thomas A. The legacy of Tuskegee and trust in medical care: is Tuskegee responsible for race differences in mistrust of medical care? Journal of the National Medical Association. 2005;97(7):951. [PMC free article] [PubMed] [Google Scholar]
- Braveman Paula. Health inequalities by class and race in the US: What can we learn from the patterns? Social Science & Medicine. 2012;74(5):665–667. doi: 10.1016/j.socscimed.2011.12.009. doi: http://dx.doi.org/10.1016/j.socscimed.2011.12.009. [DOI] [PubMed] [Google Scholar]
- Brondolo Elizabeth, Gallo Linda C, Myers Hector F. Race, racism and health: disparities, mechanisms, and interventions. Journal of Behavioral Medicine. 2009;32(1):1–8. doi: 10.1007/s10865-008-9190-3. [DOI] [PubMed] [Google Scholar]
- Brondolo Elizabeth, Hausmann Leslie RM, Jhalani Juhee, Pencille Melissa, Atencio-Bacayon Jennifer, Kumar Asha, Kwok Jasmin, Ullah Jahanara, Roth Alan, Chen Daniel. Dimensions of perceived racism and self-reported health: examination of racial/ethnic differences and potential mediators. Annals of behavioral medicine. 2011;42(1):14–28. doi: 10.1007/s12160-011-9265-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brondolo Elizabeth, Libretti Madeline, Rivera Luis, Walsemann Katrina M. Racism and Social Capital: The Implications for Social and Physical Well-Being. Journal of Social Issues. 2012;68(2):358–384. [Google Scholar]
- Brondolo Elizabeth, ver Halen Nisha Brady, Pencille Melissa, Beatty Danielle, Contrada Richard J. Coping with racism: A selective review of the literature and a theoretical and methodological critique. Journal of behavioral medicine. 2009;32(1):64–88. doi: 10.1007/s10865-008-9193-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Broudy Risa, Brondolo Elizabeth, Coakley Vonetta, Brady Nisha, Cassells Andrea, Tobin Jonathan N, Sweeney Monica. Perceived ethnic discrimination in relation to daily moods and negative social interactions. Journal of Behavioral Medicine. 2007;30(1):31–43. doi: 10.1007/s10865-006-9081-4. [DOI] [PubMed] [Google Scholar]
- Burt Callie Harbin, Simons Ronald L, Gibbons Frederick X. Racial Discrimination, Ethnic-Racial Socialization, and Crime A Micro-sociological Model of Risk and Resilience. American sociological review. 2012;77(4):648–677. doi: 10.1177/0003122412448648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bynum Mia Smith, Thomaseo Burton E, Best Candace. Racism experiences and psychological functioning in African American college freshmen: Is racial socialization a buffer? Cultural Diversity and Ethnic Minority Psychology. 2007;13(1):64–71. doi: 10.1037/1099-9809.13.1.64. [DOI] [PubMed] [Google Scholar]
- Byrne BM. Structural Equation Modeling With AMOS: Basic Concepts, Applications, and Programming. 2. Taylor & Francis; 2009. [Google Scholar]
- Carpiano Richard M. Neighborhood social capital and adult health: an empirical test of a Bourdieu-based model. Health & Place. 2007;13(3):639–655. doi: 10.1016/j.healthplace.2006.09.001. [DOI] [PubMed] [Google Scholar]
- Clark Rodney, Anderson Norman B, Clark Vernessa R, Williams David R. Racism as a stressor for African Americans: A biopsychosocial model. American psychologist. 1999;54(10):805. doi: 10.1037//0003-066x.54.10.805. [DOI] [PubMed] [Google Scholar]
- Deale Alicia, Wessely Simon. Patients’ perceptions of medical care in chronic fatigue syndrome. Social Science & Medicine. 2001;52(12):1859–1864. doi: 10.1016/s0277-9536(00)00302-6. [DOI] [PubMed] [Google Scholar]
- Dean Lorraine, Subramanian SV, Williams David R, Armstrong Katrina, Charles Camille Zubrinsky, Kawachi Ichiro. The role of social capital in African–American women’s use of mammography. Social Science & Medicine. 2014;104:148–156. doi: 10.1016/j.socscimed.2013.11.057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeLongis Anita, Folkman Susan, Lazarus Richard S. The impact of daily stress on health and mood: psychological and social resources as mediators. Journal of personality and social psychology. 1988;54(3):486. doi: 10.1037//0022-3514.54.3.486. [DOI] [PubMed] [Google Scholar]
- Elo Anna-Liisa, Leppänen Anneli, Jahkola Antti. Validity of a single-item measure of stress symptoms. Scandinavian journal of work, environment & health. 2003:444–451. doi: 10.5271/sjweh.752. [DOI] [PubMed] [Google Scholar]
- Feagin Joe R. The white racial frame: Centuries of racial framing and counter-framing. Routledge; 2009. [Google Scholar]
- Gee Gilbert C, Spencer Michael S, Chen Juan, Takeuchi David. A nationwide study of discrimination and chronic health conditions among Asian Americans. American Journal of Public Health. 2007;97(7):1275–1282. doi: 10.2105/AJPH.2006.091827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guyll Max, Matthews Karen A, Bromberger Joyce T. Discrimination and unfair treatment: relationship to cardiovascular reactivity among African American and European American women. Health Psychology. 2001;20(5):315. doi: 10.1037//0278-6133.20.5.315. [DOI] [PubMed] [Google Scholar]
- Harris Ricci, Cormack Donna, Tobias Martin, Yeh Li-Chia, Talamaivao Natalie, Minster Joanna, Timutimu Roimata. Self-reported experience of racial discrimination and health care use in New Zealand: results from the 2006/07 New Zealand Health Survey. American Journal of Public Health. 2012;102(5):1012–1019. doi: 10.2105/AJPH.2011.300626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatcher L, O’Rourke N. A Step-by-step Approach to Using SAS® for Factor Analysis and Structural Equation Modeling. SAS Institute; 2013. [Google Scholar]
- Hausmann Leslie RM, Jeong Kwonho, Bost James E, Ibrahim Said A. Perceived discrimination in health care and use of preventive health services. Journal of general internal medicine. 2008;23(10):1679–1684. doi: 10.1007/s11606-008-0730-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hicken Margaret T, Lee Hedwig, Morenoff Jeffrey, House James S, Williams David R. Racial/ethnic disparities in hypertension prevalence: reconsidering the role of chronic stress. American journal of public health. 2014;104(1):117–123. doi: 10.2105/AJPH.2013.301395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jasinskaja-Lahti Inga, Liebkind Karmela, Jaakkola Magdalena, Reuter Anni. Perceived discrimination, social support networks, and psychological well-being among three immigrant groups. Journal of Cross-Cultural Psychology. 2006;37(3):293–311. [Google Scholar]
- Jones Camara Phyllis. Levels of racism: a theoretic framework and a gardener’s tale. American Journal of Public Health. 2000;90(8):1212–1215. doi: 10.2105/ajph.90.8.1212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kawachi Ichiro, Subramanian Sankaran Venkata, Kim Daniel. Social capital and health. Springer; 2008. [Google Scholar]
- Kessler Ronald C, Mickelson Kristin D, Williams David R. The prevalence, distribution, and mental health correlates of perceived discrimination in the United States. Journal of Health and Social Behavior. 1999;40:208–230. [PubMed] [Google Scholar]
- Krieger Nancy, Sidney Stephen. Racial discrimination and blood pressure: the CARDIA Study of young black and white adults. American Journal of Public Health. 1996;86(10):1370–1378. doi: 10.2105/ajph.86.10.1370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LaVeist Thomas A, Rolley Nicole C, Diala Chamberlain. Prevalence and patterns of discrimination among US health care consumers. International Journal of Health Services. 2003;33(2):331–344. doi: 10.2190/TCAC-P90F-ATM5-B5U0. [DOI] [PubMed] [Google Scholar]
- Lazarus Richard S. Theory-based stress measurement. Psychological Inquiry. 1990;1(1):3–13. [Google Scholar]
- Lazarus Richard Stanley, Folkman Susan. Stress, Appraisal, and Coping. Springer Publishing Company; 1984. [Google Scholar]
- Li Spencer D. Testing Mediation Using Multiple Regression and Structural Equation Modeling Analyses in Secondary Data. Evaluation review. 2011;35(3):240–268. doi: 10.1177/0193841X11412069. [DOI] [PubMed] [Google Scholar]
- Lim Lionel S, Williams Donald E, Hagen Philip T. Validation of a five-point self-rated stress score. American Journal of Health Promotion. 2005;19(6):438–441. doi: 10.4278/0890-1171-19.6.438. [DOI] [PubMed] [Google Scholar]
- Littman Alyson J, White Emily, Satia Jessie A, Bowen Deborah J, Kristal Alan R. Reliability and validity of 2 single-item measures of psychosocial stress. Epidemiology. 2006;17(4):398–403. doi: 10.1097/01.ede.0000219721.89552.51. [DOI] [PubMed] [Google Scholar]
- Musa Donald, Schulz Richard, Harris Roderick, Silverman Myrna, Thomas Stephen B. Trust in the health care system and the use of preventive health services by older black and white adults. American Journal of Public Health. 2009;99(7):1293–1299. doi: 10.2105/AJPH.2007.123927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NCHS. Health, United States, 2012: With Special Feature on Emergency Care. Hyattsville, MD: 2013. [PubMed] [Google Scholar]
- Pager Devah, Shepherd Hana. The sociology of discrimination: Racial discrimination in employment, housing, credit, and consumer markets. Annual Review of Sociology. 2008;34:181–209. doi: 10.1146/annurev.soc.33.040406.131740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pascoe Elizabeth A, Richman Laura Smart. Perceived discrimination and health: a meta-analytic review. Psychological Bulletin. 2009;135(4):531–554. doi: 10.1037/a0016059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peters Rosalind M. The relationship of racism, chronic stress emotions, and blood pressure. Journal of Nursing Scholarship. 2006;38(3):234–240. doi: 10.1111/j.1547-5069.2006.00108.x. [DOI] [PubMed] [Google Scholar]
- PHMC. Household Health Survey Documentation, 2008. Philadelphia, PA: Philadelphia Health Management Corporation; 2008. [Google Scholar]
- Putnam Robert D. Bowling alone: The collapse and revival of American community. Simon and Schuster; 2001. [Google Scholar]
- Quillian Lincoln. New approaches to understanding racial prejudice and discrimination. Annual Review of Sociology. 2006:299–328. [Google Scholar]
- Ruiz John M, Steffen Patrick, Smith Timothy B. Hispanic mortality paradox: a systematic review and meta-analysis of the longitudinal literature. American Journal of Public Health. 2013;103(3):e52–e60. doi: 10.2105/AJPH.2012.301103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schumacker Randall E, Lomax Richard G. A beginner’s guide to structural equation modeling. Psychology Press; 2004. [Google Scholar]
- Shea Judy A, Micco Ellyn, Dean Lorraine T, McMurphy Suzanne, Sanford Schwartz J, Armstrong Katrina. Development of a revised health care system distrust scale. Journal of General Internal Medicine. 2008;23(6):727–732. doi: 10.1007/s11606-008-0575-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sternthal M, Slopen N, Williams DR. Racial Disparities in Health: How Much Does Stress Really Matter? Du Bois Review. 2011;8(1):95–113. doi: 10.1017/S1742058X11000087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thoits Peggy A. Stress and health major findings and policy implications. Journal of Health and Social Behavior. 2010;51(1 suppl):S41–S53. doi: 10.1177/0022146510383499. [DOI] [PubMed] [Google Scholar]
- Thrasher Angela D, Clay Olivio J, Ford Chandra L, Stewart Anita L. Theory-guided selection of discrimination measures for racial/ethnic health disparities research among older adults. Journal of aging and health. 2012;24(6):1018–1043. doi: 10.1177/0898264312440322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thrasher Angela D, Earp Jo Anne L, Golin Carol E, Zimmer Catherine R. Discrimination, distrust, and racial/ethnic disparities in antiretroviral therapy adherence among a national sample of HIV-infected patients. Journal of Acquired Immune Deficiency Syndromes. 2008;49(1):84–93. doi: 10.1097/QAI.0b013e3181845589. [DOI] [PubMed] [Google Scholar]
- Tsai Alan C, Chi Shu-Huang, Wang Jiun-Yi. The association of perceived stress with depressive symptoms in older Taiwanese—Result of a longitudinal national cohort study. Preventive medicine. 2013;57(5):646–651. doi: 10.1016/j.ypmed.2013.08.019. [DOI] [PubMed] [Google Scholar]
- Turner R Jay, Lloyd Donald A. The stress process and the social distribution of depression. Journal of Health and Social Behavior. 1999;40:374–404. [PubMed] [Google Scholar]
- Turner R Jay, Wheaton Blair, Lloyd Donald A. The epidemiology of social stress. American Sociological Review. 1995:104–125. [Google Scholar]
- Wellman D. Unconscious racism, social congnition theory, and the intent doctrine: The neuron fires next time. In: Vera H, Feagin JR, editors. Handbook of the Sociology of Racial and Ethnic Relations. New York: Springer; 2007. pp. 39–66. [Google Scholar]
- Whetten Kathryn, Leserman Jane, Whetten Rachel, Ostermann Jan, Thielman Nathan, Swartz Marvin, Stangl Dalene. Exploring lack of trust in care providers and the government as a barrier to health service use. American Journal of Public Health. 2006;96(4):716–721. doi: 10.2105/AJPH.2005.063255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wienk Ronald E. Measuring Racial Discrimination in American Housing Markets: The Housing Market Practices Survey 1979 [Google Scholar]
- Williams David R, Mohammed Selina A. Discrimination and racial disparities in health: evidence and needed research. Journal of Behavioral Medicine. 2009;32(1):20–47. doi: 10.1007/s10865-008-9185-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams David R, Neighbors Harold W, Jackson James S. Racial/ethnic discrimination and health: findings from community studies. American Journal of Public Health. 2003;93(2):200–208. doi: 10.2105/ajph.93.2.200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang Tse-Chuan, Matthews Stephen A. The role of social and built environments in predicting self-rated stress: a multilevel analysis in Philadelphia. Health & Place. 2010;16(5):803–810. doi: 10.1016/j.healthplace.2010.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang Tse-Chuan, Matthews Stephen A, Anderson Roger T. Prostate Cancer Screening and Health Care System Distrust in Philadelphia. Journal of aging and health. 2013;25(5):737–757. doi: 10.1177/0898264313490199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang Tse-Chuan, Matthews Stephen A, Hillemeier Marianne M. Is health care system distrust a barrier to breast and cervical cancer screening? Evidence from Philadelphia. American Journal of Public Health. 2011;101(7):1297–1305. doi: 10.2105/AJPH.2010.300061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yinger John. Closed doors, opportunities lost: The continuing costs of housing discrimination. Russell Sage Foundation; 1995. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.