Although important gains have been made in child survival over the past two decades, reduction in neonatal mortality (ie, deaths in the first month of life) has lagged substantially. Neonatal deaths now account for 44% of all under-5 deaths worldwide.1 Preterm birth is the leading cause of neonatal death, the second leading cause of all under-5 mortality,2 and a leading cause of severe childhood neurological disability. Despite this high global burden, little is known about how to prevent preterm birth and, in low-income and middle-income countries, how best to scale up strategies that are practical and affordable.
Preterm birth is a final common pathway for many complex pathological processes. A comprehensive research agenda is therefore needed to accelerate identification of mediators of preterm birth and innovative solutions. To forge a road map for this action agenda, the Bill & Melinda Gates Foundation (BMGF), the Global Alliance to Prevent Prematurity and Stillbirth (GAPPS), March of Dimes (MOD), the Eunice Kennedy Shriver National Institute of Child Health and Human Development, and WHO convened meetings of experts to develop a research agenda that spans the range of discovery, development, and delivery science needed to drive global change. This Comment summarises this solution pathway (figure) and the next steps toward its implementation.
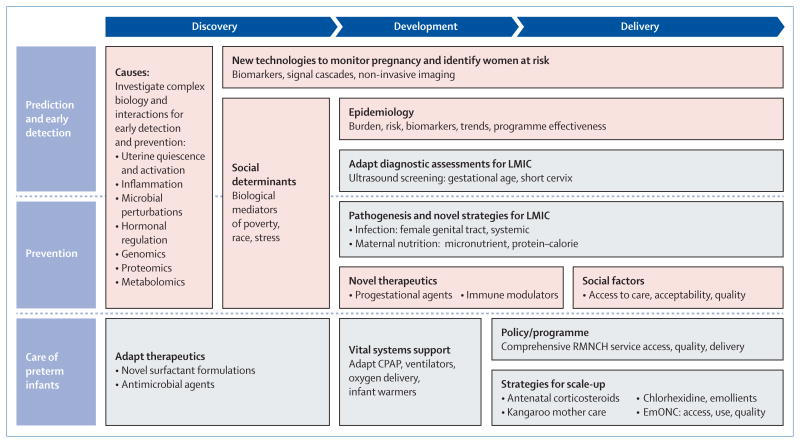
Figure. Summary of the preterm research solution pathway.
The schematic summarises key elements of the solution pathway for preterm birth research, across the range of discovery, development, and delivery science. The agenda is global in its approach; strategies more relevant to high-income countries are in pink, and low-income and middle-income countries (LMIC) in grey. CPAP = continuous positive airway pressure. EmONC = emergency obstetric and newborn care. RMNCH = reproductive, maternal, newborn, and child health.
Growing political will and new technological opportunities make this an opportune time to reinvigorate a new initiative for preterm birth research. Multiple global initiatives have gained crucial momentum to address neonatal mortality and preterm birth, including the Millennium Development Goals, Every Woman Every Child, and the Every Newborn global action plan.3–6 An essential element of these efforts is the development of new solutions to achieve health targets. Scientific advancements in the past decade have created a new opportunity for transformative research into the complex biology of pregnancy, including computational biology, genomics, informatics, microbiology, immunology, social network analysis, cell biology, imaging, nanotechnologies, and implementation science.
The first element of a solution pathway for preterm birth is an understanding of the biology of pregnancy and novel targets for preterm prevention. Most cases of preterm birth are spontaneous or follow premature rupture of membranes, usually with no identifiable cause. Multiple factors are associated with preterm birth including family history, reproductive tract and remote site infections, inflammation, nutrition, race, poverty, and emotional and physical stress.7,8 Investigation of these interrelated factors and their biological networks leading to preterm birth will be needed to advance prevention.
To understand how uterine and cervical tissues remain quiescent, sustain pregnancy, and later initiate contractility and remodelling, insights into molecular regulation of pregnancy are needed.9 Priorities include investigations of fetal–placental signalling of onset of labour and genomic, transcriptomic, proteomic, immunological, and metabolomic analyses.
The microbiome presents another important target for investigation. Female genital tract infections, altered microbiota, and associated inflammatory processes are strongly associated with preterm birth, particularly very preterm birth.10 Research is needed into microbial perturbations, immune responses, and interactions of microbiota with host and environmental factors. Investigations in low-income and middle-income countries are needed where microbial, host, and environmental milieux differ substantially.
The expansion of the application of genomics, transcriptomics, and related technologies offers new opportunities to identify genes, pathways, and associated factors that regulate parturition and their functions,11 including epigenetic and gene–environment investigations. Large-scale studies will be needed to address these complex investigations.
Rates of preterm birth and preterm-related mortality vary significantly by race, ethnic origin, and socioeconomic strata.7, 8 Biological mediators of disparities, however, remain largely unknown. Investigations into genetic, hormonal, microbial, inflammatory, nutritional, and environmental factors, and their interactions with social, emotional, physical, and environmental stressors will elucidate causality and identify strategies for prevention and care.
Prevention of preterm birth requires the early identification of women at risk. Accelerated application of novel methods, including systems biology and network analyses, will help to identify signals that drive parturition. Genetic, inflammatory, hormonal, and growth factors based on positive and negative feedback mechanisms can identify new biomarkers. Novel biotechnologies allow non-invasive monitoring of the maternal–fetal environment, by use of imaging, nanotechnology, and assessment of metabolic activity and signal cascades. Adaptations of existing technologies for low-income and middle-income countries are needed to improve assessment of gestational age, cervical length, and pregnancy monitoring.
The second element of a solution pathway for preterm birth is to improve the survival of preterm infants in low-income and middle-income countries. Practical solutions need to be developed and moved to scale to improve care. An expanded implementation science agenda will accelerate application of effective strategies at the community and facility level, including antenatal corticosteroids, newborn resuscitation, kangaroo mother care, nutrition, intrapartum monitoring, newborn skin emollients, chlorhexidine cord care, preconception care, and strengthened commodities and essential drug programmes.12 Adaptations of interventions for newborn care are needed, including simplified continuous positive airway pressure, ventilators, high-flow nasal cannulae, antibiotic regimens, and new surfactant formulations.
Intervention trials can assess efficacy and advance understanding of the biology of pregnancy in high-income and low-income settings. Examples include screening and treatment of infectious and non-infectious proinflammatory processes and interventions that modulate immunological, microbial, and hormonal mediators.
The third element of the solution pathways is to improve the epidemiological data needed to track prevalence, risk factors, and programme effect. Accurate and standardised reporting of gestational age, preterm-related death, classification of preterm phenotypes, and health service coverage are needed in essential registries and surveys in all countries.
The final element of the solution pathway is to accelerate health gains by fostering innovation and collaboration. New approaches to research are needed that promote innovation and rapid translation of science to action. Transdisciplinary and multidimensional approaches are needed that examine interactions among complex biological mediators and health disparities. New models of funding can promote collaboration between investigators and across disciplines. Standardised databases and biorepositories will accelerate discovery, development, and delivery science.
The opportunity exists now to generate new knowledge and solutions that can move rapidly to health gains. To this end, BMGF, GAPPS, MOD, the US National Institutes of Health, and WHO have initiated efforts to forge a new coalition to advance the visibility and research needed to drive global change. The coalition is intended to be inclusive of other key stakeholders, inviting participation of governmental and multilateral organisations, foundations, and corporations that support research into maternal–newborn health and are committed to an accelerated agenda to reduce death and disability due to preterm birth. Finding solutions to the complex problem of preterm birth will not come easily, but will need an expanded strategic initiative. Time and again results have shown that investment in science yields health solutions. Now is a crucial time to effect such advancements for preterm birth.
Footnotes
Members of the Preterm Birth Research Priority Setting Group are: Shams El Arifeen, José M Belizán, Zulfiqar Bhutta, Wally Carlo, A J Challis, Jennifer F Culhane, Carolyn D Deal, Michal A Elovitz, Charles J Homer, Christopher P Howson, Joy E Lawn, James A Litch, Yvonne T Maddox, Carole R Mendelson, Sam Mesiano, David A Relman, Roberto Romero, Yoel Sadovsky, Susan B Shurin, Hyagriv N Simhan, Peter Waiswa, Peter Winch, and Paul H Wise. The views expressed in this Comment are the responsibility of the authors and do not necessarily represent the views of their institutions or organisations. We declare that we have no conflicts of interest. Funding and leadership for the preterm birth research meetings were provided by the Bill & Melinda Gates Foundation, GAPPS, March of Dimes, and NICHD.
Contributor Information
Eve M Lackritz, Global Alliance to Prevent Prematurity and Stillbirth (GAPPS), Seattle, WA 98101, USA.
Christopher B Wilson, Bill & Melinda Gates Foundation, Seattle, WA, USA.
Alan E Guttmacher, Eunice Kennedy Shriver National Institute of Child Health and Human Development, National Institutes of Health (NIH), Bethesda, MD, USA.
Jennifer L Howse, March of Dimes Foundation, White Plains, NY, USA.
Cyril M Engmann, Bill & Melinda Gates Foundation, Seattle, WA, USA.
Craig E Rubens, Global Alliance to Prevent Prematurity and Stillbirth (GAPPS), Seattle, WA 98101, USA.
Elizabeth M Mason, Department of Maternal, Newborn, Child and Adolescent Health, World Health Organization, Geneva, Switzerland.
Louis J Muglia, Department of Pediatrics, Perinatal Institute, University of Cincinnati College of Medicine, Cincinnati, OH, USA.
Michael G Gravett, Global Alliance to Prevent Prematurity and Stillbirth (GAPPS), Seattle, WA 98101, USA; Department of Obstetrics and Gynecology, University of Washington, Seattle, WA, USA.
Robert L Goldenberg, Department of Obstetrics and Gynecology, Columbia University Medical Center, New York, NY, USA.
Jeffrey C Murray, Bill & Melinda Gates Foundation, Seattle, WA, USA; Department of Pediatrics, University of Iowa, Iowa City, IA, USA.
Catherine Y Spong, Eunice Kennedy Shriver National Institute of Child Health and Human Development, National Institutes of Health (NIH), Bethesda, MD, USA.
Joe Leigh Simpson, March of Dimes Foundation, White Plains, NY, USA.
References
- 1.UN Inter-agency Group for Child Mortality Estimation (IGME) Levels and trends in child mortality: report. [accessed Oct 11, 2013];2013 http://www.unicef.org/media/files/2013_IGME_child_mortality_Report.pdf.
- 2.Liu L, Johnson HL, Cousens S, et al. Global, regional, and national causes of child mortality: an updated systematic analysis for 2010 with time trends since 2000. Lancet. 2012;379:2151–61. doi: 10.1016/S0140-6736(12)60560-1. [DOI] [PubMed] [Google Scholar]
- 3.Countdown to 2015: accountability for maternal, newborn & child survival: the 2013 update. Geneva: World Health Organization; 2013. [Google Scholar]
- 4.UN. Global strategy for women's and children's health. [accessed Oct 11, 2013];2010 Sep; http://everywomaneverychild.org/images/content/files/global_strategy/full/20100914_gswch_en.pdf.
- 5.UNICEF and WHO. Every newborn: an action plan to end preventable deaths. [accessed Oct 11, 2013];2013 Apr; http://www.everynewborn.org.
- 6.WHO. Born too soon: the global action report on preterm birth. Geneva: World Health Organization; 2012. [Google Scholar]
- 7.Goldenberg RL, Culhane JF, Iams JD, Romero R. Epidemiology and causes of preterm birth. Lancet. 2008;371:75–84. doi: 10.1016/S0140-6736(08)60074-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Behrman RE, Butler AS. Preterm birth: causes, consequences, and prevention. Washington, DC: The National Academies Press; 2006. [PubMed] [Google Scholar]
- 9.Mendelson CR. Minireview: fetal-maternal hormonal signaling in pregnancy and labor. Mol Endocriol. 2009;23:947–54. doi: 10.1210/me.2009-0016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zhou X, Brotman RM, Gajer P, et al. Recent advances in understanding the microbiology of the female reproductive tract and the causes of premature birth. Infect Dis Obstet Gynecol. 2010 doi: 10.1155/2010/737425. published online Dec 9. http://dx.doi.org/10.1155/2010/737425. [DOI] [PMC free article] [PubMed]
- 11.Gracie S, Pennell C, Ekman-Ordeberg G, et al. BMC Pregnancy Childbirth. 2011 doi: 10.1186/1471-2393-11-71. published online Oct 12. http://dx.doi.org/10.1186/1471-2393-11-71. [DOI] [PMC free article] [PubMed]
- 12.Rubens CE, Victora CG, Gravett MG, Nunes TM, Smith GCS. Global report on preterm birth and stillbirth: the foundation for innovative solutions and improved outcomes. BMC Pregnancy Childbirth. 2010;10(suppl 1):S1–7. doi: 10.1186/1471-2393-10-S1-S7. [DOI] [PMC free article] [PubMed] [Google Scholar]