Abstract
Background
Observational data suggest that some donors might benefit from donating while others may be harmed. The aim of this study was to investigate the prevalence and potential, routinely measured, determinants of pre- and post-donation symptoms.
Materials and methods
In Donor InSight, questionnaire data from 23,064 whole blood donors (53% female) were linked to routinely measured data on donors’ physical characteristics (haemoglobin, blood pressure, body mass index and estimated blood volume) from the Dutch donor database. Absolute and relative associations between donors’ physical donor and the presence of pre- and post-donation symptoms were studied using multivariable logistic regression.
Results
Pre-donation symptoms (lack of energy, headaches) were reported by 3% of men and 3% of women. Five percent of men and 4% of women reported positive post-donation symptoms (feeling fit, fewer headaches). Negative symptoms (fatigue, dizziness) were more common, occurring in 8% of men and 19% of women. All the studied donors’ physical characteristics were positively associated with pre- and positive post-donation symptoms and negatively associated with negative symptoms. Body mass index was most consistently and independently associated with symptoms.
Discussion
Donors’ physical characteristics, in particular body mass index, were consistently associated with pre- and post-donation symptoms. This indicates that subgroups of donors more and less tolerant to donation might be identifiable using routinely measured data. Further research is warranted to study underlying mechanisms and potential strategies to predict and prevent donor reactions.
Keywords: donor health, symptoms, body mass index, haemoglobin
Introduction
Blood donation has been performed routinely since the early 20th century and is generally considered to be a safe way to help save other people’s lives. Nonetheless, effects on the donors’ health and wellbeing may occur, although they remain understudied and knowledge about these effects is based mainly on observations made on-site1,2. Two studies to date have reported on post-donation symptoms outside the donor centre. In the USA, 1,000 donors were asked whether they had “had any general symptoms during or after their blood donation”, which was answered in the affirmative by 36%3. As many as 54% of 528 Swedish whole blood donors reported post-donation symptoms in a postdonation questionnaire, with the majority of these symptoms being positive (29%)4. Personnel at blood collection centres in the Netherlands report that, besides post-donation symptoms, many regular donors mention having pre-donation symptoms, feelings of unease indicating that “it is time to donate again”. To our knowledge, no data currently exist on the prevalence of this phenomenon, or on its concurrence with (positive) post-donation symptoms.
Observational data suggest that some donors might benefit from donating while others might be harmed by this practice4,5. With a donation of 500 mL of whole blood, approximately 200–250 mg of haem iron are lost6,7. The loss of iron and blood cells might reduce oxidative stress and blood viscosity and therefore decrease cardiovascular risk in the long run6,8,9. On the other hand, iron loss can be detrimental in the case of low iron stores, possibly leading to fatigue, anaemia and cognitive impairment10,11. Apart from iron, blood volume and lipid levels are lowered with donation. It is known from previous studies that the loss of volume and lipids are effective ways to (temporarily) reduce blood pressure and lipid levels12–14. Potential harmful effects include the increased risk of vasovagal reactions after blood donation in donors with low blood volume15. We hypothesised that the donation-related loss of substances might be beneficial for certain subgroups of donors and harmful for others, depending on their physical characteristics. More specifically, donors with high haemoglobin (Hb), high blood pressure, high body weight or a large volume of blood would be more likely to benefit from donation, and vice versa5,16. Additionally, pre- and post-menopausal status in women and smoking behaviour could modify these associations, as these factors affect Hb levels and other physical characteristics17,18.
It is well known that donors who experience negative post-donation symptoms are less likely to return to make a subsequent donation19,20. Accordingly, it is expected that donors experiencing positive post-donation symptoms, and those who report pre-donation symptoms, are more prone to return to donate. Identifying and understanding the impact of these symptoms and recognising the donors’ physical characteristics associated with them may, therefore, be helpful in blood donor management. Ideally, routinely measured data on the donors’ physical characteristics, collected for other purposes, would be used in order to avoid the need for time-consuming additional measurements. These routinely measured data would be used to identify donors who need special attention during or after their donation, in order to increase their satisfaction and the likelihood of returning to the blood bank. The aim of this study was, therefore, to investigate the prevalence of pre- and post-donation symptoms in donors donating whole blood, and to study associations of physical characteristics routinely measured in the donors with these symptoms.
Material and methods
Study population
Sanquin, by law the only blood bank in the Netherlands, each year collects about 420,000 whole blood donations and performs about 260,000 plasma apheresis procedures (2014). The active Dutch donor population consists of approximately 360,000 voluntary non-remunerated donors, all registered at Sanquin. Donor InSight (DIS) is a self-administered questionnaire study among this donor population, aimed at gaining insight into the characteristics and motivation of the Dutch donor population21. Questionnaires were sent by mail to random samples of active donors (registered as “on call”, which also includes new donors), and were completed by a representative sample of 31,338 (63% of those invited, 8% of the entire donor population) Sanquin donors participating in DIS between April 2007 and April 2009. As reported previously, the donor population is more likely to be highly educated, married and of Dutch origin in comparison to the general Dutch population of approximately 17 million21. For the purposes of this study, we included DIS participants who had donated at least once (a minimum volume of 450 mL) before participating in DIS (n=28,596), in order to exclude donors who did not have the possibility of developing symptoms. Furthermore we excluded plasma donors by selecting donors who donated whole blood at their (up to two) donations prior to participating in DIS (n=23,222). Donors with missing data on capillary haemoglobin (Hb), blood pressure, height, weight or the specific questions of interest (see also “Measurements”) were excluded (n=158, 0.7%). The Arnhem-Nijmegen Medical Ethical Committee in the Netherlands approved DIS and all participants gave their written informed consent.
Measurements
The questionnaire was self-administered, mainly multiple choice, and comprised 102 items in Dutch. The questionnaire consisted of questions regarding demographics, donation, lifestyle, family composition, health and disease. DIS data can (routinely) be linked to the donor database, with details on all donations and donor screening results including the donor health questionnaire answers, blood pressure and Hb measurements.
Pre-donation symptoms were considered by asking about physical symptoms that made donors feel that it is time to give blood. Post-donation symptoms were investigated by asking whether there were any physical symptoms in the days after donation. Categories of symptoms are listed in Table I and are ordered from most to least prevalent. Fainting and dizziness were jointly categorised as “dizzy”. Less prevalent symptoms were grouped in the category “other”. For pre-donation symptoms, the category “other” included (nose) bleeds, feeling bloated, nervousness/restlessness, and physical complaints/itches/allergies. For positive symptoms, “other” included feeling less bloated, dizzy, and/or nervous. The category “other” for negative symptoms included headaches, pain/bruises in the injected arm, and thirst/hunger.
Table I.
Characteristics of the Donor InSight (DIS) population. Data are shown as n (%), mean±standard deviation, or median (interquartile range) in the case of skewed data.
| Men (n=10,949) | Women (n=12,115) | ||
|---|---|---|---|
| Age (years) | 50±12 | 43±13 | |
|
| |||
| Smoker (current vs ex- or non-smoker) | 1,795 (16.4%) | 1,945 (16.1%) | |
|
| |||
| Haemoglobin (mmol/L) | 9.4±0.6 | 8.5±0.5 | |
|
| |||
| SBP/DBP (mmHg) | 134±14 / 81±8 | 126±14 / 78±8 | |
|
| |||
| Estimated blood volume (L) | 5.6±0.5 | 4.3±0.5 | |
|
| |||
| Body mass index (kg/m2) | 25.7±3.1 | 24.9±4.1 | |
|
| |||
| Blood typea (%) | O (+) | 50.3% (38.5%) | 49.1% (36.6%) |
| A (+) | 38.9% (31.0%) | 38.8% (30.7%) | |
| B (+) | 7.8% (6.3%) | 8.9% (7.0%) | |
| AB (+) | 3.1% (2.3%) | 3.1% (2.4%) | |
|
| |||
| Donations in the last yearb | 0 | 1,108 (10.1%) | 1,761 (14.5%) |
| 1 or 2 | 4,373 (39.9%) | 7,334 (60.5%) | |
| 3 or more | 5,468 (49.9%) | 3,020 (24.9%) | |
|
| |||
| 5 or more donations in total | 10,710 (97.8%) | 11,013 (90.9%) | |
|
| |||
| Pre-donation symptoms | 325 (3.0%) | 311 (2.6%) | |
| Lack of energy | 116 (1.1%) | 119 (1.0%) | |
| Headache | 113 (1.0%) | 125 (1.0%) | |
| Other | 96 (0.9%) | 67 (0.6%) | |
|
| |||
| Positive post-donation symptoms | 571 (5.2%) | 500 (4.1%) | |
| Feeling fit | 413 (3.8%) | 313 (2.6%) | |
| Less headache | 104 (0.9%) | 137 (1.1%) | |
| Other | 54 (0.5%) | 50 (0.4%) | |
|
| |||
| Negative post-donation symptoms | 912 (8.3%) | 2,297 (19.0%) | |
| Lack of energy | 627 (5.7%) | 1,100 (9.1%) | |
| Dizzy | 162 (1.5%) | 906 (7.5%) | |
| Other | 123 (1.1%) | 291 (2.4%) | |
SBP: systolic blood pressure; DBP: diastolic blood pressure.
Percentage of donors with the indicated ABO blood type (Rhesus D positive);
number of donors who made a certain number of donations in the year prior to DIS or 2009 (total donor population).
Donors’ physical characteristics
During the study period, whole blood donations were allowed every 56 days to a maximum of three (women) or five (men) donations per year. Prior to every donation, Hb (measured using a Hb 201+ analyser, HemoCue® AB, Ängelholm, Sweden) in capillary blood obtained with a finger stick) and blood pressure (Omron HEM-907XL, Lake Forest, IL, USA) were measured to check the eligibility of the prospective donor. The same measurement devices (HemoCue and Omron) are used at every blood collection centres and all devices are calibrated yearly, according to standardised protocols. Measured data are entered into the blood bank’s computer system (e)Progesa (Mak-System International Group, Paris, France). For the present analyses, only data from the last donations prior to participation in DIS were included in the database. Each donor’s mean Hb and systolic blood pressure (SBP) were calculated from up to three instead of just one donation prior to DIS, in order to level out potential noise and fluctuations in measurements. Self-reported height (m) and weight (kg) from the DIS questionnaire were used to calculate body mass index (BMI), using the standard formula:
Blood volume was estimated as described by Nadler et al.22:
Data on age, donation frequency (the number of donations in the 12 months prior to DIS), total number of donations (>4 vs fewer), and blood types (ABO and Rhesus D) were extracted from (e)Progesa. Data on smoking (current vs ex- or non-smoker) and menopausal status of women (pre- vs post-menopausal) were assessed in the DIS questionnaire.
Statistical analyses
Descriptive statistics are presented as means±standard deviations (SD) or, in the case of a skewed distribution, as median (interquartile range), for men and women separately. Logistic regression analyses, resulting in odds ratios (OR) with 95% confidence intervals (CI), were used to assess associations of the donors’ physical characteristics with symptoms. p-values below 0.05 were considered statistically significant. All analyses were done separately for men and women and were adjusted for age, smoking, donation frequency, and total number of donations. We investigated effect modifications by adding potential effect modifiers together with interaction terms to the regression models. Tested interactions included smoking, age, total number of donations, menopausal status and blood type.
To enable direct comparisons of the strength of the associations for all physical characteristics, odds ratios are also shown graphically per one standard deviation increase of the physical characteristic under study. These regression models were derived with either one or a combination of the donor’s physical characteristics, the latter in order to investigate whether the characteristics were independently associated with symptoms. In these analyses, post-donation symptoms (categorised as positive, negative or no symptoms) were combined in one multinomial regression model. Donors who reported both negative and positive symptoms (n=91, 0.3%) were excluded from those particular analyses. The analyses were performed this way in order to investigate whether potential interdependence between negative and positive post-donation symptoms influenced associations with each separate outcome.
Results
A total of 23,064 individuals, 74% of the DIS population and 7.0% of Sanquin’s total whole blood donor population, in the age range of 18–70 years were included in the analyses, of whom 12,115 (53%) were female. The characteristics of the study population are shown in Table I. Compared to the total donor population, the included DIS participants were of similar age (50 years for men, 43 years for women) and had similar Hb levels, SBP and BMI (data not shown).
Of all participating donors, 2.8% reported having pre-donation symptoms, and 4.6% positive and 13.9% negative post-donation symptoms. The prevalences of these symptoms were similar for both sexes, except for negative symptoms, which were more prevalent in women (19.0% vs 8.3%). The majority of donors who reported pre-donation symptoms felt tired or had headaches. A lack of energy, dizziness (especially in females), and feeling fit were the most frequently reported post-donation symptoms. Donors reporting pre-donation symptoms had a higher chance of also having positive post-donation symptoms (p for χ2=0.00), while positive and negative symptoms were negatively associated (p=0.00). Pre-donation symptoms were not associated with negative post-donation symptoms (p=0.22).
Table II shows that all the physical characteristics of the donors that were studied were positively associated with pre-donation symptoms. For instance, women with Hb levels of 8.7 mmol/L had 1.42 times the odds of pre-donation symptoms of women with Hb levels of 7.7 mmol/L. These associations were statistically significant for both men and women, except for the association of Hb with pre-donation symptoms (p=0.11). Associations of donors’ physical characteristics with specific symptoms, e.g. lack of energy, headaches, or “other”, were similar but did not all reach statistical significance because of smaller numbers.
Table II.
Odds ratios with 95% confidence intervals for associations of mean haemoglobin and systolic blood pressure (SBP, both from last 3 donations) and of body mass index (BMI) and estimated blood volume with pre-, and positive and negative post-donation symptoms.
| Pre-donation symptoms | |||||
|---|---|---|---|---|---|
|
| |||||
| Overall | Lack of energy | Headache | Other | ||
| Haemoglobin | Men | 1.17 (0.96 to 1.42) | 1.10 (0.81 to 1.50) | 0.98 (0.70 to 1.36) | 1.27 (0.92 to 1.75) |
| Women | 1.42a (1.14 to 1.78) | 1.18 (0.86 to 1.61) | 1.62a (1.12 to 2.32) | 1.85a (1.22 to 2.81) | |
|
| |||||
| SBP | Men | 1.01a (1.00 to 1.02) | 1.00 (0.99 to 1.01) | 1.01 (0.99 to 1.02) | 1.02a (1.01 to 1.04) |
| Women | 1.02a (1.01 to 1.02) | 1.02a (1.01 to 1.03) | 1.01 (1.00 to 1.03) | 1.00 (0.99 to 1.02) | |
|
| |||||
| BMI | Men | 1.09a (1.06 to 1.13) | 1.05 (1.00 to 1.11) | 1.13a (1.07 to 1.19) | 1.12a (1.06 to 1.18) |
| Women | 1.07a (1.05 to 1.10) | 1.09a (1.05 to 1.12) | 1.09a (1.05 to 1.13) | 1.03 (0.99 to 1.09) | |
|
| |||||
| Blood volume | Men | 1.35a (1.10 to 1.65) | 1.15 (0.83 to 1.60) | 1.30 (0.92 to 1.83) | 1.66a (1.19 to 2.32) |
| Women | 1.57a (1.27 to 1.94) | 1.69a (1.26 to 2.25) | 1.70a (1.22 to 2.38) | 1.48 (0.98 to 2.22) | |
|
| |||||
| Positive post-donation symptoms | |||||
|
| |||||
| Overall | Feeling fit | Less head ached | Other | ||
|
| |||||
| Haemoglobin | Men | 1.10 (0.95 to 1.28) | 1.00 (0.80 to 1.24) | 0.61 (0.17 to 2.24) | 1.19 (0.85 to 1.67) |
| Women | 1.57a (1.32 to 1.88) | 1.53a (1.17 to 1.99) | 1.55 (0.49 to 4.85) | 1.49a (1.07 to 2.09) | |
|
| |||||
| SBP | Men | 1.02a (1.01 to 1.02) | 1.02a (1.01 to 1.03) | 1.02 (0.98 to 1.07) | 1.01 (0.99 to 1.02) |
| Women | 1.01a (1.01 to 1.02) | 1.01a (1.00 to 1.02) | 1.05a (1.01 to 1.09) | 1.02a (1.01 to 1.03) | |
|
| |||||
| BMI | Men | 1.06a (1.03 to 1.08) | 1.10a (1.06 to 1.14) | 1.05 (0.85 to 1.31) | 1.02 (0.96 to 1.09) |
| Women | 1.07a (1.05 to 1.09) | 1.07a (1.04 to 1.10) | 1.11a (1.00 to 1.22) | 1.09a (1.06 to 1.13) | |
|
| |||||
| Blood volume | Men | 1.22a (1.05 to 1.43) | 1.39a (1.12 to 1.73) | 0.50 (0.12 to 2.10) | 1.14 (0.79 to 1.64) |
| Women | 1.57a (1.32 to 1.86) | 1.44a (1.12 to 1.86) | 1.66 (0.61 to 4.51) | 1.58a (1.16 to 2.17) | |
|
| |||||
| Negative post-donation symptoms | |||||
|
| |||||
| Overall | Lack of energy | Dizzy | Other | ||
|
| |||||
| Haemoglobin | Men | 0.88a (0.78 to 1.00) | 0.92 (0.78 to 1.08) | 0.97 (0.73 to 1.28) | 0.82 (0.44 to 1.55) |
| Women | 0.93 (0.85 to 1.03) | 0.91 (0.80 to 1.02) | 0.85a (0.73 to 0.97) | 1.07 (0.78 to 1.47) | |
|
| |||||
| SBP | Men | 0.99a (0.98 to 0.99) | 1.00 (0.99 to 1.00) | 0.98a (0.97 to 0.99) | 0.99 (0.97 to 1.02) |
| Women | 0.99a (0.99 to 0.99) | 0.99a (0.99 to 1.00) | 0.98a (0.98 to 0.99) | 0.99 (0.98 to 1.01) | |
|
| |||||
| BMI | Men | 0.91a (0.89 to 0.94) | 0.95a (0.92 to 0.98) | 0.88a (0.83 to 0.93) | 1.04 (0.94 to 1.16) |
| Women | 0.93a (0.92 to 0.94) | 0.93a (0.91 to 0.94) | 0.91a (0.89 to 0.93) | 0.98 (0.95 to 1.02) | |
|
| |||||
| Blood volume | Men | 0.71a (0.62 to 0.81) | 0.78a (0.66 to 0.93) | 0.65a (0.49 to 0.88) | 0.76 (0.39 to 1.45) |
| Women | 0.63a (0.57 to 0.70) | 0.61a (0.54 to 0.69) | 0.58a (0.50 to 0.67) | 1.03 (0.77 to 1.38) | |
p<0.05.
Adjusted for age, smoking, donation frequency, total number of donations, and donation type.
As shown in Table II, higher levels of all donors’ physical characteristics were also associated with higher odds of positive post-donation symptoms and lower odds of negative post-donation symptoms. Associations of donors’ physical characteristics with positive post-donation symptoms were mainly driven by their significant associations with feeling fit, which was also the most frequently reported positive symptom. Statistically significant associations were also found with specific negative symptoms: a lack of energy or dizziness were most commonly reported and also most strongly associated with donors’ physical characteristics.
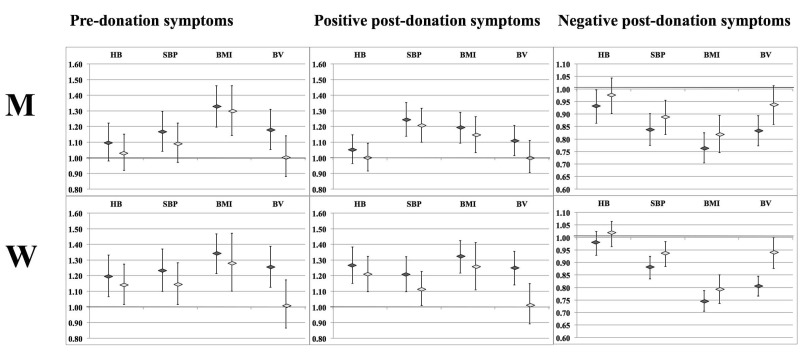
Figure 1 shows that, when looking at odds ratio per standard deviation increase, the relative strength of the associations of each donor characteristic with pre-donation symptoms were comparable, yet stronger for BMI, particularly in men. In men, BMI was the only characteristic that was associated with pre-donation symptoms independently of the other physical characteristics (Hb, SBP and estimated blood volume). In women, Hb and SBP were also strongly and independently associated with pre-donation symptoms. The associations of donors’ physical characteristics with positive post-donation symptoms were similar in strength as well, except for Hb in men (not significant). Furthermore, associations of estimated blood volume with positive symptoms disappeared after additional adjustment for Hb, SBP and BMI. Associations with negative post-donation symptoms were present for SBP, somewhat stronger, particularly in women, for estimated blood volume and strongest for BMI. The association with this last characteristic remained statistically significant after additional adjustment for the other physical characteristics (Hb, SBP and estimated blood volume).
Figure 1.
Relative associations between donors’ physical characteristics and symptoms.
Odds ratios with 95% confidence intervals for associations of Z-scores of mean haemoglobin (Hb), systolic blood pressure (SBP, both from last 3 donations), body mass index (BMI) and estimated blood volume (BV) with pre-donation symptoms (left), positive post-donation symptoms (middle) and negative post-donation symptoms (right) for men (M, upper graphs) and women (W, lower graphs). Dark grey diamonds are values adjusted for age, donation frequency, total number of donations, and donation type. Light grey diamonds are additionally adjusted for the other physical characteristics (the association for Hb is adjusted for SBP, BMI and BV).
Additional analyses
We did not find any consistently significant effect modifiers (p-values for interactions were mostly >0.05, exceptions are described in the Online Supplement), which implies that associations between donors’ physical characteristics and symptoms were not different for smokers vs non-smokers, different age categories, donors who had made more or fewer donations, pre- vs post-menopausal women, or donors with different blood types. We, therefore, removed the interaction terms from the final models and did not stratify the analyses for anything but sex (as was pre-specified). Results from multinomial regression analyses on positive and negative post-donation symptoms did not differ from results from separate logistic regression analyses. This indicates that the interdependence between negative and positive postdonation symptoms did not influence associations with each separate outcome.
Discussion
This study is the first to establish the presence and prevalence of pre-donation symptoms, and it reports on the prevalence of post-donation symptoms in the Dutch whole blood donor population. Higher levels of routinely measured Hb, SBP, BMI and estimated blood volume were significantly associated with higher odds of both pre-donation and positive post-donation symptoms, and with lower odds of negative post-donation symptoms. BMI was most consistently and independently associated with pre- and post-donation symptoms.
The strengths of the study include its large population (n>23,000) and the linkage of questionnaire data with objectively measured data from the blood bank information system. This enabled detailed assessments of how many donors have symptoms around donation, and how their routinely measured physical characteristics are associated with these symptoms. Although the DIS population is representative of the total donor population in the Netherlands, donors leaving the donor population because of negative symptoms will be underrepresented, while donors with positive symptoms will be overrepresented in both DIS and the donor population19. Extrapolation to, for instance, a population of potential donors should therefore be done with great care and would probably lead to an underestimation of negative symptoms and overestimation of positive ones.
The prevalences of both positive and negative symptoms after blood donation were relatively low compared to those found in previous studies in blood donors3,4. To a large extent this can be explained by differences in questionnaire phrasing. For instance, in the Swedish study by Nilsson-Sojka et al., donors were asked “How does blood donation affect you?”. This will more likely trigger a positive response than our phrasing “Are there any physical symptoms…?”. Furthermore, the Swedish study also included psychological and sociological effects, while we focused on physical effects only. Indeed we found that 13.9 and 4.6% of all donors reported negative and positive symptoms, respectively, vs 26 and 35% (with 23% reporting “a feeling of satisfaction”) in Sweden. In a study in the USA by Newman et al., donors were asked “Did you have any general symptoms during or after your blood donation?”. This phrasing, which is quite similar to ours, resulted in the reporting of fatigue and dizziness in 7.8 and 5.3% of the donors, indeed very similar to our 7.5 and 4.6%. Differences and similarities between men and women were comparable in all three studies: women were on average twice as likely to report negative symptoms, while positive symptoms were reported equally in men and women.
Higher levels of Hb, SBP, BMI and estimated blood volume can be indicators of greater reserves or even overloads of volume, iron or blood viscosity that are lost in donation. The hypothesised mechanisms underlying our results all relate to that principle, although we cannot rule out that parts of the effects are psychological rather than physical15. It is well known that Hb is needed for oxygen supply and that low levels are associated with fatigue23. Our findings that lower levels of Hb are associated with fatigue (in men) and dizziness (in women) after donation do, therefore, seem plausible. Beneficial effects of blood donation, in particular in female donors with high Hb, may be due to donation-induced decreased blood viscosity which might improve blood flow24. Although haematocrit was not measured in the present study, it is well-known to be associated with Hb levels. Another explanation for the association between Hb and both pre- and positive post-donation symptoms may be that high levels of iron and Hb are associated with fatigue, as in the case of patients with haemochromatosis who also benefit from repeated phlebotomies25.
Similar results were found for SBP: the loss of fluids and fluid retaining minerals may decrease blood pressure after donation13. This may result in a relief of complaints such as headaches in cases of fluid overload, and in dizziness or fatigue due to hypotension in cases of low blood pressure prior to donating15,26. Additional analyses on diastolic blood pressure, pulse pressure and mean arterial pressure (data not shown) showed comparable yet slightly weaker associations compared to SBP. This indicates that both the average pressure and pulsatility might contribute to pre- and post-donation symptoms.
The mechanisms behind negative symptoms in donors with low BMI or estimated blood volume are probably related to the relatively large amount of blood that is drawn from these individuals. This loss of fluids and substances will cause a greater imbalance in these donors, causing more physical problems. Indeed, a study by Newman et al. showed that the probability of an adverse event after blood donation significantly decreases with greater body weight27. Furthermore, it was shown that blood pressure, weight and, most strongly, estimated blood volume were important predictors of vasovagal reactions15,28. We confirmed that estimated blood volume is one of the most important predictors of dizziness and fainting, but BMI showed a stronger association with negative symptoms in general and with pre- and positive post-donation symptoms. Associations of estimated blood volume with pre- and post-donation symptoms largely disappeared after adjustment for Hb, SBP and BMI. This can entirely be attributed to the BMI, which is quite strongly correlated with estimated blood volume (Pearson’s correlation: 0.49 in men and 0.67 in women). Associations of BMI with pre- and post-donation symptoms were independent of Hb, SBP and estimated blood volume.
Apart from Hb, SBP, BMI and blood volume, other characteristics of the donor, including ethnicity, a lack of sleep, and time since eating, have also been linked to adverse events after donation27,29. Since the focus of the present study was to identify donors’ routinely measured physical characteristics that are associated with pre- and post-donation symptoms, most of these alternative determinants were outside the scope of this study. Regarding ethnicity, a very large proportion (98%) of our whole blood donor population is of Dutch origin, and ethnicity is not commonly registered in the blood bank information system21.
To better understand mechanisms behind donation-related symptoms, further research into non-routinely measured determinants, such as blood viscosity and volume reductions, is warranted. Our findings will also need to be confirmed and, if confirmed, interventions acting upon them need to be developed and evaluated. Ideally, our findings should be replicated in donors who are followed from their first donation, to minimise selection bias. A potential implication for donor care and research might be to apply interventions to prevent negative symptoms or reactions, such as water drinking, increasing donation intervals or increasing the amount of rest to be advised, to specific donors only, instead of targeting the entire donor population. Similarly, studies on positive effects of blood donation may benefit from a focus on donors with, for instance, a high BMI or blood pressure. In summary, donor care could be improved with a more personalised approach, acknowledging that blood donation might not always be a selfless act, and that some donors need more attention than others.
Conclusions
Pre-donation symptoms are a new aspect of donor reactions, and different responses to blood donation appear to be dependent on routinely measured physical characteristics of the donors. Higher values of some physical parameters, in particular BMI, were consistently associated with more favourable outcomes, while lower levels were related to negative symptoms. Further research on underlying mechanisms and on strategies to predict and prevent donor reactions is warranted.
Acknowledgements
We are very grateful to all participants for their contribution to the study and for their voluntary donation of blood (components) for patients in need. We thank all the researchers, research assistants and blood bank personnel for their on-going commitment to DIS and the donor database.
Footnotes
Funding and resources
Donor InSight (DIS) was initiated by the Unit Donor Services, Division Blood Bank and the Department of Donor Studies, Division Research, of Sanquin and was funded by the Sanquin Blood Supply Foundation, the Netherlands.
Authorship contributions
KP, KH, FA, PCMPdJ, PAHvN, IJTV, and WLAMdK made substantial contributions to the conception and design of DIS and acquisition of data. KP, KH, FA, PCMPdJ, PAHvN, IJTV, and WLAMdK revised the data critically for important intellectual content. KvdH analysed and interpreted the data, and drafted the article. All listed Authors approved the final version of the manuscript.
The Authors declare no conflicts of interest.
References
- 1.Williamson LM, Devine DV. Challenges in the management of the blood supply. Lancet. 2013;381:1866–75. doi: 10.1016/S0140-6736(13)60631-5. [DOI] [PubMed] [Google Scholar]
- 2.Amrein K, Valentin A, Lanzer G, Drexler C. Adverse events and safety issues in blood donation--a comprehensive review. Blood Rev. 2012;26:33–42. doi: 10.1016/j.blre.2011.09.003. [DOI] [PubMed] [Google Scholar]
- 3.Newman BH, Pichette S, Pichette D, Dzaka E. Adverse effects in blood donors after whole-blood donation: a study of 1000 blood donors interviewed 3 weeks after whole-blood donation. Transfusion. 2003;43:598–603. doi: 10.1046/j.1537-2995.2003.00368.x. [DOI] [PubMed] [Google Scholar]
- 4.Nilsson Sojka B, Sojka P. The blood-donation experience: perceived physical, psychological and social impact of blood donation on the donor. Vox Sang. 2003;84:120–8. doi: 10.1046/j.1423-0410.2003.00271.x. [DOI] [PubMed] [Google Scholar]
- 5.Mast AE, Schlumpf KS, Wright DJ, et al. Demographic correlates of low hemoglobin deferral among prospective whole blood donors. Transfusion. 2010;50:1794–802. doi: 10.1111/j.1537-2995.2010.02649.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Holsworth RE, Jr, Cho YI, Weidman JJ, et al. Cardiovascular benefits of phlebotomy: relationship to changes in hemorheological variables. Perfusion. 2014;29:102–16. doi: 10.1177/0267659113505637. [DOI] [PubMed] [Google Scholar]
- 7.Finch CA, Cook JD, Labbe RF, Culala M. Effect of blood donation on iron stores as evaluated by serum ferritin. Blood. 1977;50:441–7. [PubMed] [Google Scholar]
- 8.Fernandez-Real JM, Manco M. Effects of iron overload on chronic metabolic diseases. Lancet Diabetes Endocrinol. 2014;2:513–26. doi: 10.1016/S2213-8587(13)70174-8. [DOI] [PubMed] [Google Scholar]
- 9.Hoydonck van PG, Schouten EG, Hoppenbrouwers KP, Temme EH. Is blood donation induced low iron status associated with favourable levels of OxLDL, s-ICAM-1, sVCAM-1 and vWF-antigen in healthy men. Atherosclerosis. 2004;172:321–7. doi: 10.1016/j.atherosclerosis.2003.11.006. [DOI] [PubMed] [Google Scholar]
- 10.Baart AM, van Noord PA, Vergouwe Y, et al. High prevalence of subclinical iron deficiency in whole blood donors not deferred for low hemoglobin. Transfusion. 2013;53:1670–7. doi: 10.1111/j.1537-2995.2012.03956.x. [DOI] [PubMed] [Google Scholar]
- 11.Blanton CA, Green MW, Kretsch MJ. Body iron is associated with cognitive executive planning function in college women. Br J Nutr. 2013;109:906–13. doi: 10.1017/S0007114512002620. [DOI] [PubMed] [Google Scholar]
- 12.Ewald N, Kloer HU. Treatment options for severe hypertriglyceridemia (SHTG): the role of apheresis. Clin Res Cardiol Suppl. 2012;7( Suppl 1):31–5. doi: 10.1007/s11789-012-0042-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rosa-Bray M, Wisdom C, Marier JF, et al. The effect of plasmapheresis on blood pressure in voluntary plasma donors. Vox Sang. 2015;108:11–7. doi: 10.1111/vox.12188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kamhieh-Milz S, Kamhieh-Milz J, Tauchmann Y, et al. Regular blood donation may help in the management of hypertension: an observational study on 292 blood donors. Transfusion. 2016;56:637–44. doi: 10.1111/trf.13428. [DOI] [PubMed] [Google Scholar]
- 15.Wiltbank TB, Giordano GF, Kamel H, et al. Faint and prefaint reactions in whole-blood donors: an analysis of predonation measurements and their predictive value. Transfusion. 2008;48:1799–808. doi: 10.1111/j.1537-2995.2008.01745.x. [DOI] [PubMed] [Google Scholar]
- 16.Salvin HE, Pasricha SR, Marks DC, Speedy J. Iron deficiency in blood donors: a national cross-sectional study. Transfusion. 2014;54:2434–44. doi: 10.1111/trf.12647. [DOI] [PubMed] [Google Scholar]
- 17.Leifert JA. Anaemia and cigarette smoking. Int J Lab Hematol. 2008;30:177–84. doi: 10.1111/j.1751-553X.2008.01067.x. [DOI] [PubMed] [Google Scholar]
- 18.Murphy WG. The sex difference in haemoglobin levels in adults - mechanisms, causes, and consequences. Blood Rev. 2014;28:41–7. doi: 10.1016/j.blre.2013.12.003. [DOI] [PubMed] [Google Scholar]
- 19.France CR, Rader A, Carlson B. Donors who react may not come back: analysis of repeat donation as a function of phlebotomist ratings of vasovagal reactions. Transfus Apher Sci. 2005;33:99–106. doi: 10.1016/j.transci.2005.02.005. [DOI] [PubMed] [Google Scholar]
- 20.Van Dongen A, Abraham C, Ruiter RA, Veldhuizen IJ. The influence of adverse reactions, subjective distress, and anxiety on retention of first-time blood donors. Transfusion. 2012;53:337–43. doi: 10.1111/j.1537-2995.2012.03810.x. [DOI] [PubMed] [Google Scholar]
- 21.Atsma F, Veldhuizen IJT, de Vegt F, et al. Cardiovascular and demographic characteristics of whole blood and plasma donors: Results from the Donor InSight study. Transfusion. 2011;51:412–20. doi: 10.1111/j.1537-2995.2010.02867.x. [DOI] [PubMed] [Google Scholar]
- 22.Nadler SB, Hidalgo JU, Bloch T. Prediction of blood volume in normal human adults. Surgery. 1962;51:224–32. [PubMed] [Google Scholar]
- 23.Lasocki S, Chudeau N, Papet T, et al. Prevalence of iron deficiency on ICU discharge and its relation with fatigue: a multicenter prospective study. Crit Care. 2014;18:542. doi: 10.1186/s13054-014-0542-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Van der Veen PH, Muller M, Vincken KL, et al. Hemoglobin, hematocrit, and changes in cerebral blood flow: the Second Manifestations of ARTerial disease-Magnetic Resonance study. Neurobiol Aging. 2015;36:1417–23. doi: 10.1016/j.neurobiolaging.2014.12.019. [DOI] [PubMed] [Google Scholar]
- 25.Mast AE, Lee TH, Schlumpf KS, et al. The impact of HFE mutations on haemoglobin and iron status in individuals experiencing repeated iron loss through blood donation. Br J Haematol. 2012;156:388–401. doi: 10.1111/j.1365-2141.2011.08952.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Law M, Morris JK, Jordan R, Wald N. Headaches and the treatment of blood pressure: results from a meta-analysis of 94 randomized placebo-controlled trials with 24,000 participants. Circulation. 2005;112:2301–6. doi: 10.1161/CIRCULATIONAHA.104.529628. [DOI] [PubMed] [Google Scholar]
- 27.Newman BH, Roth AJ. Estimating the probability of a blood donation adverse event based on 1000 interviewed whole-blood donors. Transfusion. 2005;45:1715–21. doi: 10.1111/j.1537-2995.2005.00595.x. [DOI] [PubMed] [Google Scholar]
- 28.Trouern-Trend JJ, Cable RG, Badon SJ, et al. A case-controlled multicenter study of vasovagal reactions in blood donors: influence of sex, age, donation status, weight, blood pressure, and pulse. Transfusion. 1999;39:316–20. doi: 10.1046/j.1537-2995.1999.39399219291.x. [DOI] [PubMed] [Google Scholar]
- 29.Takanashi M, Odajima T, Aota S, et al. Risk factor analysis of vasovagal reaction from blood donation. Transfus Apher Sci. 2012;47:319–25. doi: 10.1016/j.transci.2012.04.002. [DOI] [PubMed] [Google Scholar]