Abstract
Atypical antipsychotics (AAPs) are considered to possess superior efficacy for treating both the positive and negative symptoms of schizophrenia; however, AAP use often causes excessive weight gain and metabolic abnormalities. Recently, several reports have demonstrated that AAPs activate sterol regulatory element-binding protein (SREBP). SREBP, SREBP cleavage-activating protein (SCAP) and insulin-induced gene (Insig) regulate downstream cholesterol and fatty acid biosynthesis. In this study, we explored the effects of clozapine, olanzapine and risperidone on SREBP signaling and downstream lipid biosynthesis genes in the early events of adipogenic differentiation in adipose-derived stem cells (ASCs). After the induction of adipogenic differentiation for 2 days, all AAPs, notably clozapine treatment for 3 and 7 days, enhanced the expression of SREBP-1 and its downstream lipid biosynthesis genes without dexamethasone and insulin supplementation. Simultaneously, protein level of SREBP-1 was significantly enhanced via inhibition of Insig-2 expression. By contrast, SREBP-1 activation was suppressed when Insig-2 expression was upregulated by transfection with Insig-2 plasmid DNA. In summary, our results indicate that AAP treatment, notably clozapine treatment, induces early-stage lipid biosynthesis in ASCs. Such abnormal lipogenesis can be reversed when Insig-2 expression was increased, suggesting that Insig/SCAP/SREBP signaling may be a therapeutic target for AAP-induced weight gain and metabolic abnormalities.
Introduction
Schizophrenic patients need to take antipsychotic agents for most of their lives. Atypical antipsychotics (AAPs) are considered to possess superior efficacy for treating both the positive and negative symptoms of schizophrenia compared to typical antipsychotics1, 2. However, a high prevalence of metabolic syndrome3–6 and increased mortality rate7, 8 were observed in schizophrenic patients, and were considered to be adverse effects of AAPs. AAP-induced metabolic syndrome consists of excessive weight gain, type II diabetes mellitus, hyperglycemia, dyslipidemia, insulin resistance and cardiovascular disease3–7, 9, 10. Of note, the incidence of cardiovascular mortality in the schizophrenic population is over twice that of the general population5, 11, which may also be related to AAP treatment. Consequently, it is important to monitor the metabolic function of patients with schizophrenia, who have a higher risk of metabolic disorders due to the use of AAPs.
The mechanisms underlying AAP-induced metabolic dysfunction are still elusive. Several hypotheses have been proposed, including the impact of genetic factors12, 13, stimulation of appetite by central histamine H1 blockage14, modulation of serotoninergic/noradrenergic pathways in the central nervous system and/or involvement of the hormones leptin, ghrelin and adiponectin15. Additionally, AAPs are involved not only in the regulation of critical adipose biochemical processes, including signal transduction, mitochondrial biogenesis, adipogenesis and metabolism during adipogenic differentiation, but also in the production of proinflammatory cytokines in fully differentiated adipocytes from human adipose-derived stem cells (hASCs), which may associate with AAP-induced weight gain16. Sertie et al. reported that in cultured hASCs, clozapine and olanzapine increased peroxisome proliferator-activated receptor gamma (PPAR-γ) expression and induced insulin-stimulated lipogenesis more than the typical antipsychotic drug haloperidol17.
Recent studies suggested that the sterol-regulatory element-binding proteins (SREBPs) are central in the regulation of various lipid biosynthetic pathways18. SREBPs are transcription factors that respond to nutrient levels and regulate the transcription of genes required for many aspects of lipid metabolism19, including genes that are important for downstream cholesterol and fatty acid biosynthesis20. There are three major SREBP isoforms, SREBP-1a, SREBP-1c (encoded by SREBF1 gene) and SREBP-2 (encoded by SREBF2 gene). SREBP-1 primarily controls the gene expression involved in fatty acid and triacylglycerol metabolism, whereas SREBP-2 preferentially regulates cholesterol metabolism18. SREBPs are synthesized as precursor proteins, which reside in the endoplasmic reticulum (ER), where they form a complex with SREBP chaperone proteins, an SREBP cleavage activating protein (SCAP) and an insulin-induced gene (Insig) protein21. At low sterol levels, SREBPs are released from the membrane and activated by cleavage; then, the water-soluble N-terminal domain is translocated to the nucleus21, 22 where it binds to the SRE in the promoter of numerous SREBP target genes for lipid biosynthesis22. Insigs have two isoforms; Insig-1, a target of nuclear SREBPs, whose mRNA expression depends on nuclear SREBP levels, and Insig-2, whose amount is low but constant and is negatively regulated by insulin without being influenced by SREBPs18. However, Yabe et al. reported that Insig-2 can also bind the SCAP/SREBP complex and cause its retention in the ER in a sterol dependent fashion. When sterols are present, Insig-2 causes ER retention of the SCAP/SREBP complex23. Liou et al. demonstrated that three haplotypes of the Insig-2 gene significantly increased the risk of AAP-induced metabolic syndrome. They also found that the Insig-1 gene was not associated with metabolic syndrome; however, the gene interaction between Insig-1 and Insig-2 was implicated in AAP-induced metabolic adverse effects24. Additionally, Le et al. also found a significant association between SREBP-mediated activation of lipid biosynthesis with Insig-2 blockade and weight gain during AAP treatment in patients with schizophrenia22.
The biochemical pathways involving SREBP may be altered by a variety of AAPs. AAPs, such as clozapine, olanzapine, and risperidone can elicit significant upregulation of SREBP-1 and SREBP-2 and their downstream target genes leading to increased lipid and cholesterol synthesis25–28. Several studies demonstrated that AAPs activate the SREBP which might be crucial for AAP-mediated dyslipidemia, weight gain and cardiovascular diseases22, 24, 29, 30. The work by Ferno and colleagues showed the possible of SREBP pathway activation in antipsychotic-induced metabolic disorders26. They demonstrated that the antipsychotic drugs clozapine and haloperidol both activate the SREBP pathway in cultured human glioma cells26. In other studies, clozapine induced pronounced activation of SREBP, with subsequent transcriptional activation of downstream cholesterol and fatty acid biosynthesis, in cultured hepatocytes and adipocytes31, 32. Additionally, both clozapine and olanzapine have been shown to enhance differentiation of adipose precursor cells 3T3-L1 into mature adipocytes, possibly through activation of SREBP-133. However, little is known about the effects of AAPs on SREBP signaling and lipid biosynthesis in the early events of adipogenic differentiation in ASCs. Different AAPs are associated with various degrees of metabolic adverse effects34. Therefore, this study aimed to compare the effects of clozapine, olanzapine and risperidone on Insig/SCAP/SREBP pathway and the downstream expression of lipid biosynthesis genes during adipogenic differentiation without dexamethasone and insulin supplementation in rat ASCs.
Results
Effects of AAP treatment on cell viability
According to the therapeutic plasma concentrations of AAPs (0.6 to 1 μM for clozapine35, 0.07 to 0.2 μM for olanzapine36 and 10 to 40 nM for risperidone37), we have treated the cells with 10 to 20-fold higher concentrations of each AAP similar to a previous study17. To explore the effects of AAPs on cell viability, ASCs were cultured with clozapine, (10 and 20 μM), olanzapine (1 and 2 μM) or risperidone (0.4 and 0.8 μM) for 48 hours. AAPs at all concentrations tested did not affect the cell viability (Fig. 1). Moreover, there is no obvious difference of lipid biosynthesis genes by AAP treatment at day 7 (Supplementary Fig. 1). Therefore, clozapine at 10 μM, olanzapine at 1 μM and risperidone at 0.4 μM were applied in subsequent experiments.
Figure 1.
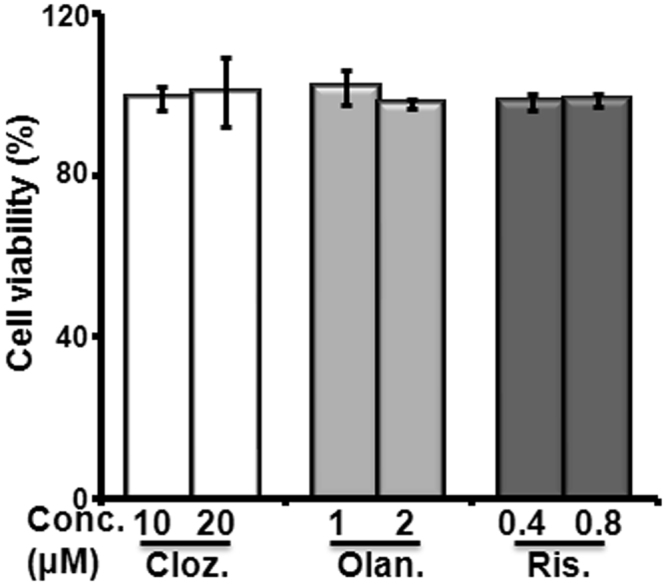
Effect of AAPs on cell viability. Cell viability was measured by CCK-8 assays. The cells were plated into 96-well microplates at a density of 5000 cells per well in complete medium and incubated at 37 °C in 5% CO2 prior to treatment. The cells were treated with clozapine (Cloz. 10 and 20 μM), olanzapine (Olan. 1 and 2 μM) and risperidone (Ris. 0.4 and 0.8 μM) for 48 hours. The data are representative of three independent experiments.
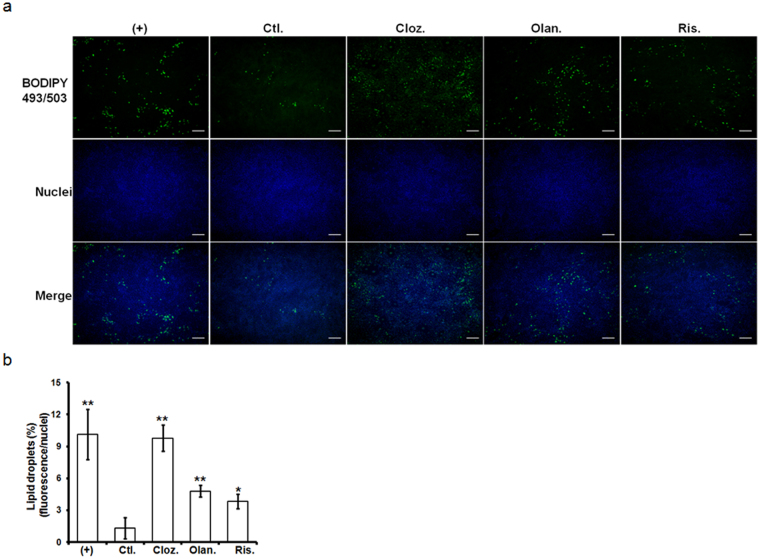
AAPs enhanced lipid droplet formation
AAPs were tested for their effects on the adipogenic differentiation of ASCs. As shown in Fig. 2, clozapine, olanzapine and risperidone significantly enhanced the number of lipid vesicles compared with the vehicle-treated control.
Figure 2.
Effect of AAPs on lipid droplet accumulation in ASCs at day 7 after treatment. (a) Lipid droplets were stained with the BODIPY fluorescence probe. Cell nuclei were stained with DAPI and fluorescent images were taken at ×40. (b) Lipid vesicles were quantified via high-content imaging and normalized to cell number. (+): treated with adipogenic media (ADM) for the indicated times; Ctl.: treated with ADM for 2 days and changed to complete media only; Cloz.: clozapine; Olan.: olanzapine; Ris.: risperidone. Results are presented as the mean of four independent experiments ± SD. Scale bar: 20 μm. *, ** denotes statistical significance: P < 0.05 and 0.01, compared with the control group, respectively.
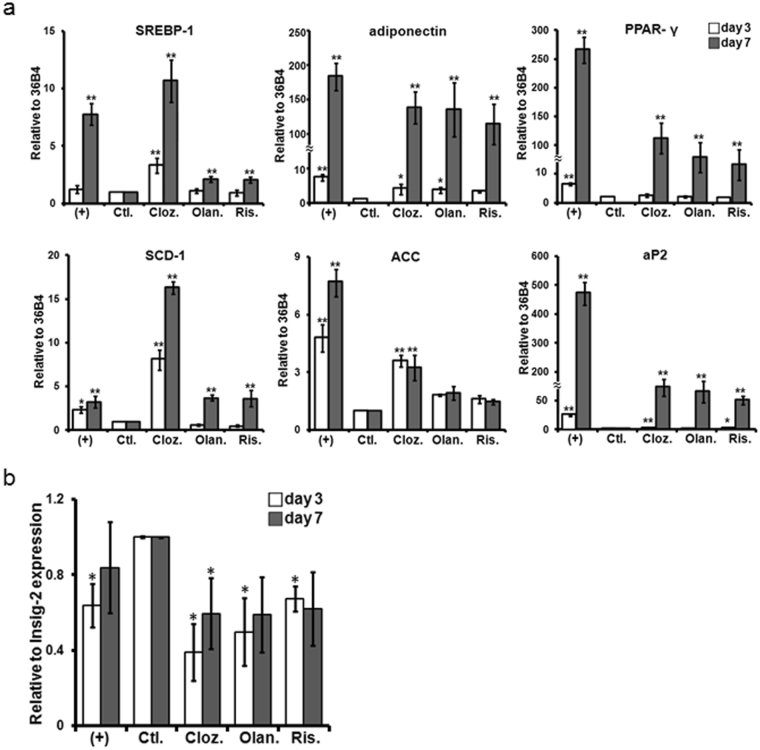
Differential modulatory effects of AAPs on SREBP signaling and lipid biosynthesis genes during adipogenesis
We next examined the effects of AAPs on the control of the adipocyte differentiation program. Enzymes that are involved in free fatty acids (FFA) regulation, such as stearoyl-CoA desaturase (SCD-1), acetyl CoA carboxylase (ACC) and adipocyte fatty acid binding protein (aP2), were increased by clozapine treatment on day 3 of the differentiation process (Fig. 3a). Interestingly, clozapine treatment strongly enhanced SREBP-1 and SCD-1 expression compared with either the vehicle-treated control or positive control on days 3 and 7. On day 7, all AAP treatments increased the expression levels of SREBP-1, adiponectin, PPAR-γ, SCD-1 and aP2 compared with the vehicle-treated control (Fig. 3a). On the other hand, the ACC level was elevated by clozapine treatment only, suggesting that clozapine is an effective inducer of SREBP-mediated lipid synthesis under these experimental conditions. SREBP is known to regulate lipid biosynthesis when it leaves the ER membrane and enters the nucleus. Additionally, Insig-2 stabilizes SREBP on the ER membrane. As shown in Fig. 3b, Insig-2 gene expression was suppressed on day 3 in all AAP treatment groups as well as positive control, while it was also suppressed on day 7 by clozapine treatment only.
Figure 3.
Effect of AAPs on lipid gene expression in ASCs at day 3 and day 7 after treatment. (a) SREBP-1 and its downstream lipid gene expression. (b) Insig-2 gene expression. ASCs were differentiated in the presence of AAPs (Cloz. 10 μM, Olan. 1 μM and Ris. 0.4 μM). At days 3 and 7, total RNA was extracted and subjected to q-PCR. The gene expressions levels were normalized to 36B4 expression. (+): treated with ADM for the indicated times; Ctl.: treated with ADM for 2 days and changed to complete media only; Cloz.: clozapine; Olan.: olanzapine; Ris.: risperidone. Results are presented as the mean of three independent experiments ± SD. *, ** denotes statistical significance: P < 0.05 and 0.01, compared with the control group, respectively.
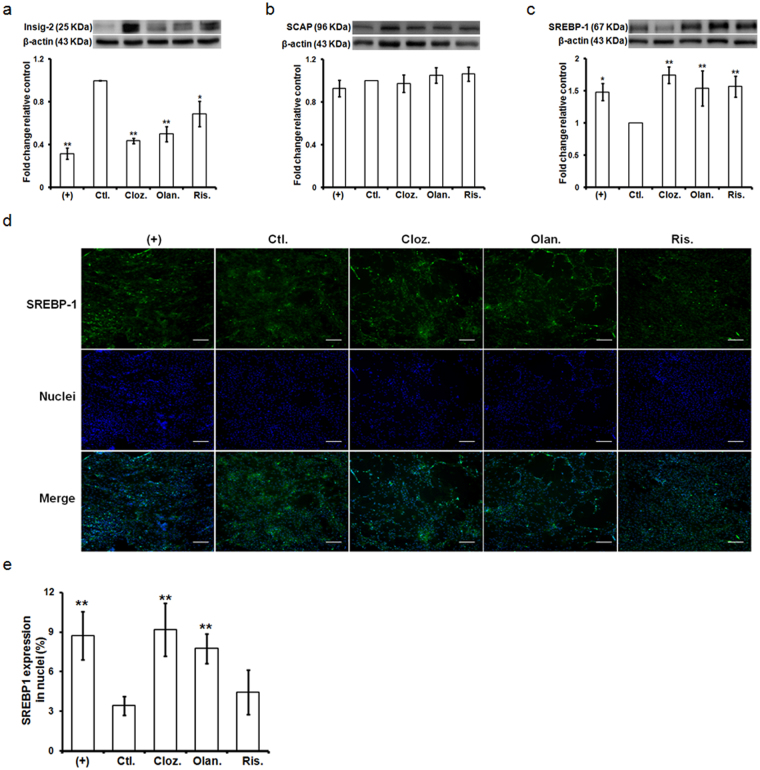
AAPs reduced Insig-2 expression and enhanced SREBP activation
SREBP is known to regulate lipid biosynthesis when it leaves the ER membrane and enters the nucleus. Additionally, Insig-2 stabilizes SREBP on the ER membrane. To verify whether AAPs regulate Insig/SCAP/SREBP signaling, we evaluated the protein levels of Insig-2, SCAP and SREBP-1 in cell lysates, as well as the nuclear level of SREBP-1, using immunoblotting and immunofluorescence microscopy. As shown in Fig. 4a–c, AAP treatment reduced Insig-2 expression but enhanced SREBP-1 expression compared with the vehicle-treated control. However, SCAP expression was not changed following AAPs treatment. The nuclear translocation of SREBP-1 was increased by clozapine and olanzapine treatment compared with the vehicle-treated control (Fig. 4d,e).
Figure 4.
Effect of AAPs on SREBP signaling during adipogenesis. The cells were treated with ADM for 2 days and supplemented with AAPs for 7 days. (a–c) The cell lysates were subjected to SDS-PAGE and immunoprobed with antibodies against Insig-2, SCAP and SREBP-1. Each protein expression was normalized to the loading control (β-actin) and the data represent the expression ratio of each protein compared to the control group. Original scans are provided in Supplementary Fig. 3. (d) The nuclear SREBP-1 level was measured by immunofluorescence using an anti-SREBP-1 antibody. Cell nuclei were stained blue with DAPI and fluorescent images were taken at ×100. (e) Nuclear fluorescence intensity was quantified via high-content imaging. (+): treated with ADM for the indicated times; Ctl.: treated with ADM for 2 days and changed to complete media only; Cloz.: clozapine; Olan.: olanzapine; Ris.: risperidone. Results are presented as the mean of three independent experiments ± SD. Scale bar: 10 μm. *, ** denotes statistical significance: P < 0.05 and 0.01, compared with the control group, respectively.
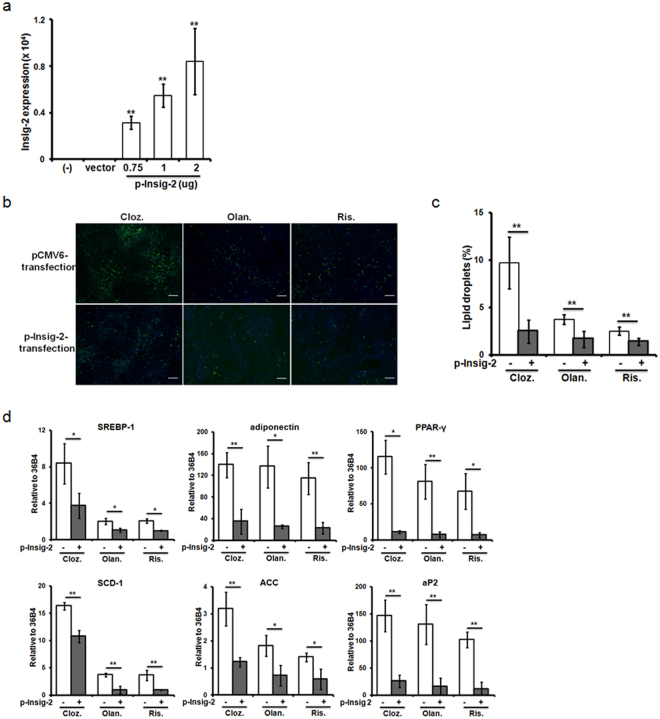
Overexpression of Insig-2 suppressed adipogenic differentiation in ASCs
The Insig-2 gene contributes to the risk of metabolic syndrome independently and in an interactive manner with Insig-1 in schizophrenic patients treated with AAPs24. Additionally, AAP-treated rats showed significantly increased hepatic expression of SREBPs and corresponding inhibition of Insig-2 expression25. Next, we determined whether Insig-2 overexpression modulates lipid biosynthesis in ASCs. To evaluate the transfection efficiency of plasmid DNA in ASCs, the expression level of Insig-2 was validated by RT-PCR. The expression of Insig-2 was significantly up-regulated by plasmid DNA transfection for 24 hours compared with empty vector transfection (Fig. 5a). To determine whether increased expression of Insig-2 could affect the efficiency of adipogenic differentiation induced by AAPs in ASCs, we evaluated the lipid droplet formation and gene expression profiles. As shown in Fig. 5b,c, increased expression of Insig-2 significantly reduced the number of lipid vesicles compared to empty vector transfection following AAP treatment for 7 days. Moreover, increased expression of Insig-2 also inhibited the expression of lipid biosynthesis genes (Fig. 5d).
Figure 5.
Overexpression of Insig-2 in ASCs during adipogenic differentiation. (a) The expression of Insig-2 in ASCs. ASCs were transfected with Insig-2 or the negative control pCMV6-Entry plasmid for 24 hours as described in the “Materials and Methods” section. (b) Lipid droplets were stained with the BODIPY fluorescence probe. Cell nuclei were stained blue with DAPI and fluorescent images were taken at ×40. (c) Lipid vesicles were quantified via high-content imaging. (d) The effects of AAPs on SREBP-1 and the downstream expression of lipid regulatory genes in Insig-2-transfected ASCs during adipogenic differentiation. The cells were switched to ADM for two days and then maintained in AAPs for 7 days. The gene expression was normalized to 36B4 and compared between the Insig-2-transfected group and the non-transfected group. Cloz.: clozapine; Olan.: olanzapine; Ris.: risperidone. Results are presented as the mean of three independent experiments ± SD. Scale bar: 20 μm. *, ** denotes statistical significance, P < 0.05 and 0.01 compared to the non-transfected group, respectively.
Discussion
Although AAPs possess superior efficacy in treating both the positive and negative symptoms of schizophrenia compared to typical antipsychotics, AAP treatment promotes metabolic disorders and cardiovascular diseases3–7. Notably, both clozapine and olanzapine treatment lead to excessive weight gain with elevated fasting plasma triglyceride (TG) and cholesterol concentrations compared with other AAPs38–40. Additionally, Lauressergues et al. reported that clozapine directs its lipogenic effects specifically on the FFA and phospholipid (PL) pathway, whereas olanzapine causes more generally effects on FFA, PL, and TG synthesis in rat hepatocytes27. Yang et al. found that olanzapine increases TG accumulation and activates SREBP-1 during 3T3-L1 preadipocyte differentiation to the mature adipocyte phenotype33. In this study, we explored the effects of AAPs on adipogenic differentiation as well as its molecular consequences in ASCs. Our results showed that lipid droplet formation was strongly enhanced in response to clozapine treatment, but olanzapine and risperidone had moderate or less effect on day 7 after AAP treatment (Fig. 2). Moreover, clozapine treatment dramatically induced SREBP-1 and SCD-1 mRNA expression in the early phase of adipogenic differentiation (day 3) and adipose induction period (day 7). All AAPs increased SREBP-1 and its downstream lipid gene expression on day 7. The differential effects of AAPs on lipid droplet formation (clozapine > olanzapine > risperidone) may depend on the nuclear translocation of SREBP-1 induced by AAPs in adipogenesis (Fig. 4). Obesity is often associated with a low-grade state of inflammation, which is attributed to the production of inflammatory cytokines in adipose tissues and causes metabolic abnormalities41. AAP treatment activated nuclear factor kappa B (NF-κB) and caused a concerted increase in the levels of proinflammatory cytokines TNF-α, IL-1β and IL-8, and the MCP-1 in hASCs after adipose differentiation for 11 days. Their results showed that clozapine causes the greatest increase in the NF-κB, IL-1β and IL-8 expression levels16. Although AAP treatment activated NF-κB similar to the positive control for adipogenic differentiation (Supplementary Fig. 2), there is no obvious difference of proinflammatory cytokine expression in this study, probably due to short treatment period with AAPs for 3 and 7 days. Adipogenic differentiation induces dynamic changes in NF-κB expression and activity42. Therefore, NF-κB activation may be associated with adipogenic differentiation rather than proinflammatory response in this culture condition. In mammalian cells, PPAR-γ, and CCAAT/enhancer binding proteins (C/EBPs) are considered the key early regulators of adipogenesis43. PPAR-γ was known to be critical both for adipogenic differentiation and for maintenance of mature adipocytes44, 45. Sertie et al. has shown that clozapine and olanzapine enhanced the early (C/EBP-β and PPAR-γ) or late (PPAR-γ and LPL) markers of adipose tissue differentiation17. Further studies are necessary to clarify the impact of AAPs on early and late events of adipogenic differentiation as well as the effect of AAPs on adipocyte hypertrophy.
Several studies have shown a significant association between SREBP-mediated activation of lipid biosynthesis with Insig-2 blockade and AAP-induced weight gain in patients with schizophrenia22, 24. Additionally, many clinical studies have found that clozapine treatment had the highest risk for weight gain than other AAPs38, 46. The present study showed that clozapine significantly suppressed Insig-2 mRNA expression during adipogenic differentiation at early and induction phase (Fig. 3b). The results were consistent with the SREBP-1 and lipid gene expression after clozapine treatment (Fig. 3a). Additionally, AAP treatment significantly suppressed protein level of Insig-2 on day 7, which in turn enhanced SREBP-1 activity (Fig. 4). These results implicate Insig-2 in the pathogenesis of metabolic abnormalities in patients treated with AAPs. In support of our present data, Cervino et al. identified Insig-2 as a susceptibility gene for plasma cholesterol levels in mice47. In addition to the effect of Insig-2 on lipid metabolism, Herbert et al. demonstrated that a single-nucleotide polymorphism (SNP) of Insig-2 was associated with obesity48. A strong association between three Insig-2 gene SNPs (rs17587100, rs10490624 and rs17047764) and antipsychotic-related weight gain was reported22.
In this study, we demonstrated that overexpression of Insig-2 in ASCs suppresses SREBP-1 mRNA expression and subsequently inhibits AAP-induced lipid biosynthesis during adipogenic differentiation. In adult mice, deletion of the Insig genes activated SREBP-mediated lipogenesis in respiratory epithelial cells, resulting in lipotoxicity-related lung inflammation and tissue remodeling49. On the other hand, AAP treatment down-regulated Insigs and up-regulated SREBP expression in vitamin D-deficient rats. Vitamin D supplementation, in turn, increased Insig expression and abolished SREBP activation50. Interestingly, the active form vitamin D3 (1α,25(OH)2D3) directly suppresses adipogenic factors and inhibits adipocyte differentiation via strong induction of Insig-2 expression in 3T3-L1 cells51. Furthermore, 1α,25(OH)2D3, a novel response element in the promoter region of the Insig-2 gene, directs vitamin D receptor (VDR)-mediated transcriptional activation51. The above findings implicate the Insig proteins in the pathogenesis of AAP-induced adverse effects, including excessive weight gain and metabolic abnormalities; furthermore, these adverse effects were attenuated when the Insigs were modulated.
In summary, the present study demonstrates that AAP treatment significantly inhibits Insig-2 expression and, in turn, increases the expression of SREBP-1 and its downstream lipid genes during adipogenic differentiation in ASCs. Such abnormal lipogenesis was attenuated when Insig-2 expression was increased, suggesting that SREBP/Insig-2 signaling may be a therapeutic target for AAP-induced weight gain.
Materials and Methods
Drugs
AAPs including clozapine, olanzapine and risperidone, were purchased from Sigma-Aldrich (St. Louis, MO, USA). All drugs were dissolved in DMSO and stored at 4 °C until use.
Ethics statement
All animal experimentation was in compliance with the animal welfare guidelines. All protocols were approved by Animal Protection Law by the Council of Agriculture, Executive Yuan, R.O.C., and the Guide for the Care and Use of Laboratory Animals by the Institute of Laboratory Animal Resources, National Research Council, USA.
Preparation of rat ASCs
ASCs were obtained from the abdominal adipose tissue of 8-week-old Lewis rats as previously described52. Briefly, the tissue was minced, washed, and suspended in Hanks’ solution containing collagenase type II (Sigma-Aldrich). Following a 30–60 min digestion at 37 °C with agitation (50 rpm), which produced a smooth and even consistency, the cellular pellet was incubated with erythrocyte lysis buffer and resuspended in complete medium composed of DMEM supplemented with 10% fetal bovine serum (FBS, Thermo Fisher Scientific Inc. Carlsbad, CA, USA) and Penicillin-Streptomycin-Amphotericin B Solution (1%, Biological Industries, Cromwell, CT, USA). The cells were incubated for 3 to 6 days in a humidified 5% CO2 incubator until they reached approximately 80% confluence.
Adipogenic differentiation assay
The ASCs were plated into 6-well plates and allowed to come to 60% confluence in growth media. After the cells were switched to adipogenic differentiation media (ADM) (DMEM supplemented with 10% FBS, 1 μM dexamethasone and 10 μg/ml insulin (Thermo Fisher Scientific Inc.)) for 2 days, the adipogenic media were removed and the cells were cultured in complete media supplemented with clozapine (10 and 20 μM), olanzapine (1 and 2 μM) or risperidone (0.4 and 0.8 μM) or in complete media without AAPs (as a vehicle-treated control) for 3 and 7 days. As positive and negative controls, the cells were cultured in ADM and in complete media, respectively.
Cell viability assay
Cell viability was detected with the Cell Counting Kit-8 (CCK-8, Sigma-Aldrich), and the absorbance at 450 nm was measured using a Victor IV microplate reader (PerkinElmer, Waltham, MA, USA).
Lipid droplet staining
After induction of adipogenic differentiation for 2 days and following AAP treatment for 7 days, cells were fixed in phosphate-buffered formaldehyde (4%; pH 7) for 15 min and stained with a BODIPY 493/503 fluorescence lipid probe for 15 min as previously described53. The nuclei were counterstained with 4’,6-Diamidino-2-Phenylindole (DAPI; Invitrogen, Thermo Fisher Scientific Inc.). Images of lipid droplets were captured using an inverted microscope (Olympus Corporation, Tokyo, Japan) or the ImageXpress® Micro XLS Widefield High-Content Analysis System (Molecular Devices, Sunnyvale, CA, USA). The percentage of lipid droplets in each group was normalized to total number of cells determined by the DAPI counterstain. Data analysis was performed using the MetaXpress software package (Molecular Devices).
Transformation of Insig-2 expression plasmids
Transformation of Insig-2-expressing pCMV-Insig-2 plasmids, obtained from OriGene (#RN211993, Rockville, MD, USA), was carried out in Escherichia coli DH5α, and DNA was prepared using plasmid purification columns (EndoFree Plasmid Giga Kit, Qiagen, Hilden, Germany). The plasmid DNA was dissolved in milli-Q water. The purified plasmid DNA was stored at −20 °C and diluted to 1 mg/mL with phosphate-buffered saline (pH 7.4) immediately before use.
Transfection of the Insig-2 gene in ASCs
Transfection of the Insig-2 cDNA into ASCs was conducted when they reached 70% confluence. ASCs were transfected with Insig-2 or negative control pCMV6-Entry plasmids using the TurboFectin 8.0TM High Performance Transfection Reagent (OriGene), following the manufacturer’s protocol. After 24 hours, ASCs were switched to ADM for two days, followed by AAP treatment for 7 days. ADM treatment was set as the positive control.
RNA isolation and reverse transcriptase polymerase chain reaction (RT-PCR)
Total RNA was extracted using NucleoSpin-RNA kits (MACHEREY-NAGEL GmbH & Co. KG, Düren, Germany), and total RNA (3 μg) was reverse-transcribed into cDNA using the High-Capacity cDNA Reverse Transcription Kit (Applied Biosystems, Foster, CA, USA) according to the manufacturer’s instructions. The quantitative RT-PCR reaction was performed on an ABI 7500 Fast Real-Time PCR System with the SDS 1.4 program (ABI 7500 Fast PCR system; Applied Biosystems) using the SYBR Green PCR Master Mix. Reverse transcriptase (RT)-negative samples were used to demonstrate that the signals obtained were RT-dependent. The 36B4 reference gene was used to normalize the data. The 2−∆CT value, which corresponds to the expression ratio of each gene compared to 36B4, and the 2−∆∆CT value, which corresponds to the expression ratio of each gene compared to the vehicle-treated control group, were calculated. The sequences of gene-specific primers were summarized in Supplementary Table 1.
Western blot analysis
The proteins were separated on 10% SDS-PAGE gels and transferred onto PVDF membranes (Bio-Rad). The membranes were blocked with 5% (w/v) skim milk/1% (v/v) Tween 20 in PBS for 30 min at room temperature and incubated overnight with the appropriate primary antibody: Insig 2 from Biorbyt (Biorbyt Llc, SF, CA, USA, 1:500 dilution); SCAP from Bioss (Bioss Inc., Woburn, MA, USA, 1:1000 dilution); SREBP1 antibody from BioVision (BioVision Inc., Milpitas, CA, USA, 1:500 dilution); NF-κB p65 (Santa Cruz Biotechnology, Santa Cruz, CA,USA, 1:1000 dilution); phospho-NF-κB p65 (Cell Signaling Technology, Inc., Danvers, MA, USA, 1:1000 dilution); anti-β-actin antibody from Millipore (Millipore Corporation, Bedford, MA, USA, 1:10000 dilution) at 4 °C. Detection was performed using an enhanced chemiluminescence (ECL) detection kit (Millipore). Images were captured using a G:BOX Image Station iChemi XL device (SYNGENE, Cambridge, UK), and the relevant bands were quantified by densitometry using GeneTools (SYNGENE).
Immunofluorescence staining
Intracellular SREBP-1 staining was performed using Image-iT® Fix Perm Kit (Thermo Fisher Scientific Inc.). Briefly, cells were fixed and permeabilized in Fixation Buffer and Permeabilization Buffer for 15 min, respectively. The cells were blocked and incubated with a primary monoclonal antibody against SREBP-1 (BioVision Inc., 1:100 dilution). After incubation with fluorophore-conjugated secondary antibodies (Thermo Fisher Scientific Inc.), cells were counterstained with DAPI (Invitrogen, Thermo Fisher Scientific Inc). After washing with PBS, cells were examined using an FV10i confocal laser microscope (Olympus) or the ImageXpress® Micro XLS Widefield High-Content Analysis System (Molecular Devices). Data analysis was performed using the MetaXpress software package (Molecular Devices).
Statistical analysis
Descriptive statistics, means, standard deviations, and ranges were used where appropriate. For comparison of groups, one-way analysis of variance (ANOVA) and Duncan’s post-hoc test were used where appropriate. Differences between the non-transfected and transfected groups were tested for statistical significance using Student’s t-test. The results are shown as the mean value ± the standard deviation (SD) of the mean. A value of p < 0.05 was considered significant.
Electronic supplementary material
Acknowledgements
This work was supported in part by grants from the Ministry of Science and Technology (MOST 104–2314-B-182A-031 and 105-2314-B-182A-058 to CC-C) and the Chang Gung Memorial Hospital (CMRPG8D0452 to CC-C and CMRPG8D1013 to CL-C) of Taiwan.
Author Contributions
C.C.C., S.G., C.L.C. and T.N. conceived of the study. S.G., C.L.C. and T.N. supervised the execution of the study. C.C.C. and L.W.H. carried out qRT-PCR, immunoblotting and immunofluorescence. C.C.C., K.T.H. and T.N. analysed the data. C.C.C., K.T.H. and T.N. drafted the manuscript. All authors critically revised the manuscript and approved it for publication.
Competing Interests
The authors declare that they have no competing interests.
Footnotes
Electronic supplementary material
Supplementary information accompanies this paper at doi:10.1038/s41598-017-11323-9
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Jann MW. Implications for atypical antipsychotics in the treatment of schizophrenia: neurocognition effects and a neuroprotective hypothesis. Pharmacotherapy. 2004;24:1759–1783. doi: 10.1592/phco.24.17.1759.52346. [DOI] [PubMed] [Google Scholar]
- 2.Bridler, R. & Umbricht, D. Atypical antipsychotics in the treatment of schizophrenia. Swiss Med Wkly133, 63–76, doi:2003/05/smw-10003 (2003). [DOI] [PubMed]
- 3.Bou Khalil R. Atypical antipsychotic drugs, schizophrenia, and metabolic syndrome in non-Euro-American societies. Clin Neuropharmacol. 2012;35:141–147. doi: 10.1097/WNF.0b013e31824d5288. [DOI] [PubMed] [Google Scholar]
- 4.Ko YK, Soh MA, Kang SH, Lee JI. The prevalence of metabolic syndrome in schizophrenic patients using antipsychotics. Clin Psychopharmacol Neurosci. 2013;11:80–88. doi: 10.9758/cpn.2013.11.2.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Said MA, et al. Metabolic syndrome and cardiovascular risk among patients with schizophrenia receiving antipsychotics in Malaysia. Singapore Med J. 2012;53:801–807. [PubMed] [Google Scholar]
- 6.Popovic I, et al. Long-Term Treatment with Olanzapine in Hospital Conditions: Prevalence and Predictors of the Metabolic Syndrome. Srp Arh Celok Lek. 2015;143:712–718. doi: 10.2298/SARH1512712P. [DOI] [PubMed] [Google Scholar]
- 7.Ventriglio A, Gentile A, Stella E, Bellomo A. Metabolic issues in patients affected by schizophrenia: clinical characteristics and medical management. Front Neurosci. 2015;9:297. doi: 10.3389/fnins.2015.00297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Luijendijk HJ, de Bruin NC, Hulshof TA, Koolman X. Terminal illness and the increased mortality risk of conventional antipsychotics in observational studies: a systematic review. Pharmacoepidemiol Drug Saf. 2016;25:113–122. doi: 10.1002/pds.3912. [DOI] [PubMed] [Google Scholar]
- 9.Malhotra N, Grover S, Chakrabarti S, Kulhara P. Metabolic syndrome in schizophrenia. Indian J Psychol Med. 2013;35:227–240. doi: 10.4103/0253-7176.119471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Laursen TM, Munk-Olsen T, Nordentoft M, Mortensen PB. Increased mortality among patients admitted with major psychiatric disorders: a register-based study comparing mortality in unipolar depressive disorder, bipolar affective disorder, schizoaffective disorder, and schizophrenia. J Clin Psychiatry. 2007;68:899–907. doi: 10.4088/JCP.v68n0612. [DOI] [PubMed] [Google Scholar]
- 11.Choure BK, Gosavi D, Nanotkar S. Comparative cardiovascular safety of risperidone and olanzapine, based on electrocardiographic parameters and blood pressure: a prospective open label observational study. Indian J Pharmacol. 2014;46:493–497. doi: 10.4103/0253-7613.140579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nussbaum LA, et al. Molecular study of weight gain related to atypical antipsychotics: clinical implications of the CYP2D6 genotype. Rom J Morphol Embryol. 2014;55:877–884. [PubMed] [Google Scholar]
- 13.Gregoor JG, et al. Polymorphisms of the LEP, LEPR and HTR2C gene: obesity and BMI change in patients using antipsychotic medication in a naturalistic setting. Pharmacogenomics. 2011;12:919–923. doi: 10.2217/pgs.11.40. [DOI] [PubMed] [Google Scholar]
- 14.Kim SF, Huang AS, Snowman AM, Teuscher C, Snyder SH. From the Cover: Antipsychotic drug-induced weight gain mediated by histamine H1 receptor-linked activation of hypothalamic AMP-kinase. Proc Natl Acad Sci USA. 2007;104:3456–3459. doi: 10.1073/pnas.0611417104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jin H, Meyer JM, Mudaliar S, Jeste DV. Impact of atypical antipsychotic therapy on leptin, ghrelin, and adiponectin. Schizophr Res. 2008;100:70–85. doi: 10.1016/j.schres.2007.11.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sarvari AK, Vereb Z, Uray IP, Fesus L, Balajthy Z. Atypical antipsychotics induce both proinflammatory and adipogenic gene expression in human adipocytes. In vitro. Biochem Biophys Res Commun. 2014;450:1383–1389. doi: 10.1016/j.bbrc.2014.07.005. [DOI] [PubMed] [Google Scholar]
- 17.Sertie AL, et al. Effects of antipsychotics with different weight gain liabilities on human in vitro models of adipose tissue differentiation and metabolism. Prog Neuropsychopharmacol Biol Psychiatry. 2011;35:1884–1890. doi: 10.1016/j.pnpbp.2011.07.017. [DOI] [PubMed] [Google Scholar]
- 18.Ye, J. & DeBose-Boyd, R. A. Regulation of cholesterol and fatty acid synthesis. Cold Spring Harb Perspect Biol3, doi:10.1101/cshperspect.a004754 (2011). [DOI] [PMC free article] [PubMed]
- 19.Osborne TF, Espenshade PJ. Evolutionary conservation and adaptation in the mechanism that regulates SREBP action: what a long, strange tRIP it’s been. Genes Dev. 2009;23:2578–2591. doi: 10.1101/gad.1854309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Horton JD, Goldstein JL, Brown MS. SREBPs: activators of the complete program of cholesterol and fatty acid synthesis in the liver. J Clin Invest. 2002;109:1125–1131. doi: 10.1172/JCI0215593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Walker AK, et al. A conserved SREBP-1/phosphatidylcholine feedback circuit regulates lipogenesis in metazoans. Cell. 2011;147:840–852. doi: 10.1016/j.cell.2011.09.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Le Hellard S, et al. Association between the insulin-induced gene 2 (INSIG2) and weight gain in a German sample of antipsychotic-treated schizophrenic patients: perturbation of SREBP-controlled lipogenesis in drug-related metabolic adverse effects? Mol Psychiatry. 2009;14:308–317. doi: 10.1038/sj.mp.4002133. [DOI] [PubMed] [Google Scholar]
- 23.Yabe D, Brown MS, Goldstein JL. Insig-2, a second endoplasmic reticulum protein that binds SCAP and blocks export of sterol regulatory element-binding proteins. Proc Natl Acad Sci USA. 2002;99:12753–12758. doi: 10.1073/pnas.162488899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Liou YJ, et al. Gene-gene interactions of the INSIG1 and INSIG2 in metabolic syndrome in schizophrenic patients treated with atypical antipsychotics. Pharmacogenomics J. 2012;12:54–61. doi: 10.1038/tpj.2010.74. [DOI] [PubMed] [Google Scholar]
- 25.Cai HL, et al. A potential mechanism underlying atypical antipsychotics-induced lipid disturbances. Transl Psychiatry. 2015;5:e661. doi: 10.1038/tp.2015.161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ferno J, et al. Antipsychotic drugs activate SREBP-regulated expression of lipid biosynthetic genes in cultured human glioma cells: a novel mechanism of action? Pharmacogenomics J. 2005;5:298–304. doi: 10.1038/sj.tpj.6500323. [DOI] [PubMed] [Google Scholar]
- 27.Lauressergues E, et al. Antipsychotic drug action on SREBPs-related lipogenesis and cholesterogenesis in primary rat hepatocytes. Naunyn Schmiedebergs Arch Pharmacol. 2010;381:427–439. doi: 10.1007/s00210-010-0499-4. [DOI] [PubMed] [Google Scholar]
- 28.Lauressergues E, et al. Overweight induced by chronic risperidone exposure is correlated with overexpression of the SREBP-1c and FAS genes in mouse liver. Naunyn Schmiedebergs Arch Pharmacol. 2011;383:423–436. doi: 10.1007/s00210-010-0597-3. [DOI] [PubMed] [Google Scholar]
- 29.Vassas TJ, Burghardt KJ, Ellingrod VL. Pharmacogenomics of sterol synthesis and statin use in schizophrenia subjects treated with antipsychotics. Pharmacogenomics. 2014;15:61–67. doi: 10.2217/pgs.13.157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ferno J, et al. Lipogenic effects of psychotropic drugs: focus on the SREBP system. Front Biosci (Landmark Ed) 2011;16:49–60. doi: 10.2741/3675. [DOI] [PubMed] [Google Scholar]
- 31.Ferno J, et al. Acute clozapine exposure in vivo induces lipid accumulation and marked sequential changes in the expression of SREBP, PPAR, and LXR target genes in rat liver. Psychopharmacology (Berl) 2009;203:73–84. doi: 10.1007/s00213-008-1370-x. [DOI] [PubMed] [Google Scholar]
- 32.Raeder MB, Ferno J, Vik-Mo AO, Steen VM. SREBP activation by antipsychotic- and antidepressant-drugs in cultured human liver cells: relevance for metabolic side-effects? Mol Cell Biochem. 2006;289:167–173. doi: 10.1007/s11010-006-9160-4. [DOI] [PubMed] [Google Scholar]
- 33.Yang LH, Chen TM, Yu ST, Chen YH. Olanzapine induces SREBP-1-related adipogenesis in 3T3-L1 cells. Pharmacol Res. 2007;56:202–208. doi: 10.1016/j.phrs.2007.05.007. [DOI] [PubMed] [Google Scholar]
- 34.Orsolini L, et al. An update of safety of clinically used atypical antipsychotics. Expert Opin Drug Saf. 2016;15:1329–1347. doi: 10.1080/14740338.2016.1201475. [DOI] [PubMed] [Google Scholar]
- 35.Broich K, Heinrich S, Marneros A. Acute clozapine overdose: plasma concentration and outcome. Pharmacopsychiatry. 1998;31:149–151. doi: 10.1055/s-2007-979318. [DOI] [PubMed] [Google Scholar]
- 36.Bergemann N, Frick A, Parzer P, Kopitz J. Olanzapine plasma concentration, average daily dose, and interaction with co-medication in schizophrenic patients. Pharmacopsychiatry. 2004;37:63–68. doi: 10.1055/s-2004-815527. [DOI] [PubMed] [Google Scholar]
- 37.Wang L, et al. Serum prolactin levels, plasma risperidone levels, polymorphism of cytochrome P450 2D6 and clinical response in patients with schizophrenia. J Psychopharmacol. 2007;21:837–842. doi: 10.1177/0269881107077357. [DOI] [PubMed] [Google Scholar]
- 38.Newcomer JW. Second-generation (atypical) antipsychotics and metabolic effects: a comprehensive literature review. CNS Drugs. 2005;19(Suppl 1):1–93. doi: 10.2165/00023210-200519001-00001. [DOI] [PubMed] [Google Scholar]
- 39.Wirshing DA, et al. The effects of novel antipsychotics on glucose and lipid levels. J Clin Psychiatry. 2002;63:856–865. doi: 10.4088/JCP.v63n1002. [DOI] [PubMed] [Google Scholar]
- 40.Baymiller SP, Ball P, McMahon RP, Buchanan RW. Serum glucose and lipid changes during the course of clozapine treatment: the effect of concurrent beta-adrenergic antagonist treatment. Schizophr Res. 2003;59:49–57. doi: 10.1016/S0920-9964(02)00158-5. [DOI] [PubMed] [Google Scholar]
- 41.Johnson AR, Milner JJ, Makowski L. The inflammation highway: metabolism accelerates inflammatory traffic in obesity. Immunol Rev. 2012;249:218–238. doi: 10.1111/j.1600-065X.2012.01151.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Berg AH, Lin Y, Lisanti MP, Scherer PE. Adipocyte differentiation induces dynamic changes in NF-kappaB expression and activity. Am J Physiol Endocrinol Metab. 2004;287:E1178–1188. doi: 10.1152/ajpendo.00002.2004. [DOI] [PubMed] [Google Scholar]
- 43.Moseti, D., Regassa, A. & Kim, W. K. Molecular Regulation of Adipogenesis and Potential Anti-Adipogenic Bioactive Molecules. Int J Mol Sci17, doi:10.3390/ijms17010124 (2016). [DOI] [PMC free article] [PubMed]
- 44.Imai T, et al. Peroxisome proliferator-activated receptor gamma is required in mature white and brown adipocytes for their survival in the mouse. Proc Natl Acad Sci USA. 2004;101:4543–4547. doi: 10.1073/pnas.0400356101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Tontonoz P, Spiegelman BM. Fat and beyond: the diverse biology of PPARgamma. Annu Rev Biochem. 2008;77:289–312. doi: 10.1146/annurev.biochem.77.061307.091829. [DOI] [PubMed] [Google Scholar]
- 46.Allison DB, et al. Antipsychotic-induced weight gain: a comprehensive research synthesis. Am J Psychiatry. 1999;156:1686–1696. doi: 10.1176/ajp.156.11.1686. [DOI] [PubMed] [Google Scholar]
- 47.Cervino AC, et al. Integrating QTL and high-density SNP analyses in mice to identify Insig2 as a susceptibility gene for plasma cholesterol levels. Genomics. 2005;86:505–517. doi: 10.1016/j.ygeno.2005.07.010. [DOI] [PubMed] [Google Scholar]
- 48.Herbert A, et al. A common genetic variant is associated with adult and childhood obesity. Science. 2006;312:279–283. doi: 10.1126/science.1124779. [DOI] [PubMed] [Google Scholar]
- 49.Plantier L, et al. Activation of sterol-response element-binding proteins (SREBP) in alveolar type II cells enhances lipogenesis causing pulmonary lipotoxicity. J Biol Chem. 2012;287:10099–10114. doi: 10.1074/jbc.M111.303669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Dang R, et al. Vitamin D deficiency exacerbates atypical antipsychotic-induced metabolic side effects in rats: involvement of the INSIG/SREBP pathway. Eur Neuropsychopharmacol. 2015;25:1239–1247. doi: 10.1016/j.euroneuro.2015.04.028. [DOI] [PubMed] [Google Scholar]
- 51.Lee S, Lee DK, Choi E, Lee JW. Identification of a functional vitamin D response element in the murine Insig-2 promoter and its potential role in the differentiation of 3T3-L1 preadipocytes. Mol Endocrinol. 2005;19:399–408. doi: 10.1210/me.2004-0324. [DOI] [PubMed] [Google Scholar]
- 52.Hsu LW, et al. The effect of exogenous histone H1 on rat adipose-derived stem cell proliferation, migration, and osteogenic differentiation in vitro. J Cell Physiol. 2012;227:3417–3425. doi: 10.1002/jcp.24042. [DOI] [PubMed] [Google Scholar]
- 53.Chen CC, et al. DHL-HisZn, a novel antioxidant, enhances adipogenic differentiation and antioxidative response in adipose-derived stem cells. Biomed Pharmacother. 2016;84:1601–1609. doi: 10.1016/j.biopha.2016.10.066. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.