Abstract
Medial elbow pain is uncommon when compared with lateral elbow pain.
Medial epicondylitis is an uncommon diagnosis and can be confused with other sources of pain.
Overhead throwers and workers lifting heavy objects are at increased risk of medial elbow pain.
Differential diagnosis includes ulnar nerve disorders, cervical radiculopathy, injured ulnar collateral ligament, altered distal triceps anatomy or joint disorders.
Children with medial elbow pain have to be assessed for ‘Little League elbow’ and fractures of the medial epicondyle following a traumatic event.
This paper is primarily focused on the differential diagnosis of medial elbow pain with basic recommendations on treatment strategies.
Cite this article: EFORT Open Rev 2017;2:362-371. DOI: 10.1302/2058-5241.2.160006
Keywords: medial elbow pain, medial epicondylitis, ulnar collateral ligament, ulnar neuritis, elbow, sports
Introduction
Medial elbow pain is not very common in the general population. Medial epicondylitis (ME) has shown a prevalence of < 1% and has been calculated to be one-third as frequent as lateral epicondylitis.1 Certain groups of the population are at an increased risk of suffering from this condition, including carpenters, plumbers and ‘overhead’ athletes. Work-related problems generally involve repetitive movement, including a combination of pronation of the forearm and wrist flexion.2
Overhead throwers are at risk due to the valgus torque of the elbow during the acceleration phase of throwing, causing significant strain on the common flexor pronator mass.3 Some throwers may have further pathology, including medial collateral ligament (MCL) insufficiency, and, of those, some may have chronic signs of impingement, also known as ‘chronic valgus overload syndrome’. Acute medial elbow instability is usually a distinct and obvious diagnosis, but progressive attenuation and failure can be a gradual process.4
Medial elbow pain can be caused by ulnar nerve problems, which can include neuropathy and neuritis with or without nerve dislocation. The medial antebrachial cutaneous nerve (MABCN) has also been reported to be a cause of medial elbow pain.5 Other diagnoses that may produce medial elbow pain are ulno-humeral arthritis, the presence of medial osteophytes, medial epicondyle avulsion fractures or the rare presence of osteochondritis dissecans of the trochlea.
Cervical radiculopathy of C6 and C7 has been associated with weakness and dysfunction of the pronator teres, flexor carpi radialis, palmaris longus, flexor digitorum superficialis and flexor carpi ulnaris and, potentially, can lead to an imbalance of the muscles around the elbow and precipitate the onset of ME.6-8
Children may present with medial elbow pain after elbow trauma or intensive sportive activities, and due to the presence of open physes, apophysitis and ‘Little League elbow’ must be considered.9,10
Certain patient characteristics may be helpful to orientate the diagnosis (Table 1). These include age, gender, sports involvement, occupation, history of trauma or the presence of a tingling in the hand.
Table 1.
Clinical patient characteristics may orient the diagnosis of medial elbow pain. Some presentations may be complex and include more than one diagnosis
| Adult |
Children (open physes) |
||||||
|---|---|---|---|---|---|---|---|
| Trauma | Non-trauma | Trauma | Non-trauma | ||||
| Acute pain +/- instability | Pain with resisted wrist flexion +/- pronation | MVT + | Medial Snapping | Positive Tinel | Acute pain +/- instability | Insidious pain, decreased throwing velocity, Positive MVT, Anomalous Rx | Pain with abnormal imaging findings |
| Acute MCL tear | Medial epicondylitis | MCL injury | Snapping ulnar nerve +/- snapping triceps | Ulnar neuritis/neuropathy | Acute MCL injury | Little League elbow | OCD trochlea |
| Fx. sublime tubercule | Avulsion Fx. medial epicondyle | ||||||
Fx., fracture; MVT, moving valgus test; MCL, medial collateral ligament; OCD, osteochondritis dissecans
ME
Analogous to lateral epicondylitis, ME has been described as an angiofibroblastic tendinosis of the flexor-pronator mass close to the origin of the muscle in an area where the flexor carpi radialis and pronator teres coalesce.8 An inadequate healing response of microscopic tears may progress to attritional partial tearing and, occasionally, complete tearing of the origin of the flexor-pronator mass.
Patient history
Patients present with a full range of movement (ROM), tenderness just distal to the medial epicondyle and referred pain with activities that place stress on the origin of these muscles, such as golf, tennis, weight-lifting, swimming and work-related activities.
Physical examination and imaging studies
Some patients may have pain only during physically demanding activities and that may deter them from seeking prior consultation. Workers handling objects heavier than 5 kg for more than two hours per day or objects weighing > 10 kg more than ten times a day are at high risk of developing ME.11 Wrist flexion and forearm pronation may be weaker when compared with the opposite side due to pain (Fig. 1). Concomitant ulnar neuritis can be seen in 20% of patients.12 Radiographs are usually normal but may rule out other causes of medial pain.
Fig. 1.

Patients with medial epicondylitis have pain on resisted flexion and/or pronation. Those patients with more chronic symptoms may exhibit pain with resisted elbow flexion. This manoeuvre, shown in this clinical picture, includes resisted elbow and wrist flexion and resisted pronation, thus, is very sensitive. The patient is asked to take the hand as if to wash their face and the examiner places resistance on the radial border of the hand. Pain on the medial epicondyle is generally reproduced in patients with medial epicondylitis.
Conservative treatment
Conservative management is initiated and generally includes a combination of activity modification: ice, oral analgesics, anti-inflammatories, physical therapy, iontophoresis and acupuncture. Local injections have been used including steroids, platelet-rich plasma and dry needling with blood injection, although the available evidence suggests that the outcome may not be much different from the natural history.13-15 The use of ultrasound (US) to guide the injections may improve the outcome of the injection when using autologous blood therapy.13 Conservative management may improve nine out of ten patients, although those with long-standing symptoms may be at higher risk of failure after conservative management.
Failure to improve after six months of appropriate medical care is an indication to proceed with surgical treatment. In cases of persistent symptoms unresponsive to conservative management, we favour additional imaging techniques (US or MRI) to rule out other abnormalities. The presence of intermediate to high T2 signal intensity or high T2 signal intensity within the common flexor tendon and the presence of paratendinous soft-tissue oedema are the most specific findings of ME on MRI.16
Surgical treatment
Many surgical options have been described and they include some form of debridement of the origin of the flexor-pronator mass.17 As in lateral epicondylitis, the medial epicondyle can be stimulated with perforations to promote healing and the muscle tears may be repaired back to their origin with the use of an anchor.12,18 Associated procedures to the ulnar nerve include decompression, with anterior transposition in cases of instability of the nerve after decompression (Table 2).
Table 2.
Results of surgical debridement with and without repair for chronic medial epicondylitis
| Author | Patients (n) | Procedure | Follow-up (mths) | Results | Commentary |
|---|---|---|---|---|---|
| Vangsness and Jobe (1991)22 | 35 | Debridement. | 85 | Excellent results in 25, good in nine and far in 1.86% had no limitation. | Subjective elbow function increased from 38% to 98%. Isokinetic strength showed no difference with the unoperated elbow. |
| Gabel and Morrey (1995)19 | 30 (26 patients) | Debridement of the origin of the flexor-pronator tendon mass, with decompression or transposition of the ulnar nerve. | 7 yrs (2 to 15) | 87% rate (26 elbows) of good or excellent results. | Patients without or mild ulnar neuropathy had a better outcome. Improvement was slow (> 6 mths) in 9 patients. |
| Kurvers and Verhaar (1995)20 | 40 (38 patients) | Debridement of the origin of the flexor-pronator tendon mass, with decompression of the ulnar nerve (24 patients). | 44 (24 to 67) | 25 had good subjective outcome. | Outcome was less favorable for the elbows that had had coexistent ulnar neuritis. Symptoms of ulnar neuritis persisted in 15 patients. |
| Ollivierre et al (1995)8 | 50 | Debridement and side to side repair. | 37 | No pain at rest post-operatively. 10 patients did not return to pre-operative. Activities. |
Dynamometer testing improved in all patients. |
| Vinod and Ross (2015)12 | 60 | Debridement with repair and restoration of the flexor-pronator origin, using a suture anchor. | 12 | MEPS 88 +/- 7.8 | 20% concomitant preoperative ulnar neuritis. Pronation weakness was noted in all cases pre-operatively. |
| Grawe et al (2016)18 | 31 | Debridement with repair and restoration of the flexor-pronator origin, using a suture anchor. | 40 (12 to 67) | QuickDASH 2.3 OES 45. Return to premorbid sporting activities at 4.5 mths. |
Older age at surgery predicted better DASH and OES. A shorter duration of symptoms was beneficial. 19% patients reported pre-operative symptoms of ulnar neuritis. |
MEPS, Mayo Elbow Performance Score; DASH, Disabilities of the Arm, Shoulder and Hand; OES, Oxford Elbow Score
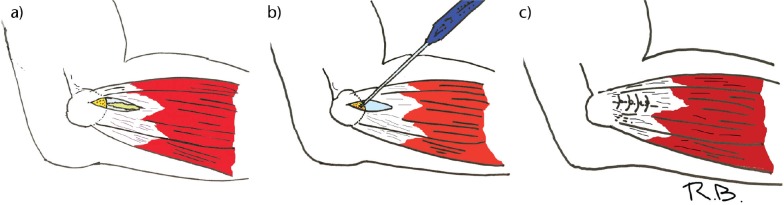
Open treatment includes a skin incision just anterior to the medial epicondyle with subcutaneous dissection and protection of the MABCN. The flexor pronator mass is divided and dissected in the interval between the flexor and pronator muscles and the pathological tissue is debrided and excised. The authors favour a slight bony decortication to promote healing and reconstruction of the flexor pronator mass with the use of a suture anchor (Fig. 2). Most of the reports focus on open techniques, and although the use of elbow arthroscopy for debridement has been described in a cadaver study, clinical studies are lacking.17,19-21 Potential dangers with this technique include damage to the MCL and the ulnar nerve.21 Post-operatively, the arm is placed in a well-padded splint for one week and there is a transition to the use of a sling with gentle ROM activities. Active wrist flexion and pronation are avoided while inflammation persists.
Fig. 2.

This picture depicts exploring the elbow with the ‘moving valgus test’ developed by O’Driscoll et al.28 The patient is seated with the shoulder locked in maximum external rotation. The examiner places the elbow through a range of movement while applying a valgus torque on the elbow throughout the exploration. Patients with medial elbow instability typically have maximum pain on the medial side of the elbow between 75° to 95º of elbow flexion. Pain in terminal extension and pronation may be used to detect valgus overload syndrome.
The success rate of open debridement is around 80% to 85%, but may be negatively affected by the presence of concomitant ulnar neuritis (Table 2).12,18,19,22 The presence of pre-operative ulnar neuritis or a longer duration of pre-operative symptoms has been associated with a less favourable outcome, including persistent pain.18,20 Surgical treatment of ME is often effective although some may have residual pain with heavy-duty activities and may have to limit recreational activities.8
MCL injury
The MCL of the elbow has three distinct bundles: anterior, posterior and transverse. The anterior bundle originates from the antero-inferior aspect of the medial epicondyle and inserts in the sublime tubercle, providing the primary resistance to valgus forces of the elbow throughout the ROM in an elbow with normal bony congruence. The anterior bundle of the MCL is mostly isometric throughout the full ROM while the posterior bundle of the MCL becomes taut in flexion. The average valgus load at which the MCL fails is 260 N and it seldom fails acutely.3,9,23,24
Injury to the MCL of the elbow is mostly an injury of throwers. The reason for this is the epidemiological feature of the high torque generated by the trunk, through the core muscles and transmitted to the upper extremity throughout the different phases of the throwing movement, which may amount to 300 N of medial shear forces for each single overhead throw.24 The repetition of the throwing movement may produce an intrinsic failure of the collagen fibres within the ligament and cause its progressive structural failure. The number of pitches has been related to an increased risk of injuries to the MCL, as well as improper technique and poor physical conditioning.25 Other injuries typical of these patients include flexor-pronator muscle injuries, radio-capitellar chondromalacia, loose bodies and posteromedial osteophyte formation.26 These late changes have been termed ‘valgus extension overload syndrome’.27
Patient history
The typical patient will present with chronic onset of symptoms over the medial elbow on late cocking and/or the acceleration phase. Some patients may report associated decreased velocity and precision. Occasionally, patients may feel a sudden pop and inability to continue throwing suggestive of acute failure of the MCL.
Physical examination and imaging studies
Patients report tenderness over the medial side of the elbow just anterior and distal to the medial epicondyle and may show symptoms of valgus instability on physical examination. The ‘moving valgus stress test’ is a very specific test for MCL injury. The test is performed with the patient sitting. The shoulder is abducted and locked in external rotation and a valgus force is applied to the elbow throughout the ROM. Insufficiency of the MCL produces pain typically in the range of 70° to 90° of elbow flexion28 (Fig. 3). The degree of instability is associated with the severity of the injury to the MCL. The ‘milking manoeuvre’ is similar to the previous test but without the dynamic component and is performed in a greater degree of flexion. As in other conditions with medial elbow pain, some patients may have associated ulnar nerve problems and this will worsen the final result.12
Fig. 3.
A medial approach at the interval between the flexor carpi radialis and pronator teres is performed with care to protect the medial antebrachial cutaneous nerve branches: a) the fascia is opened and the degenerative tissue is debrided to healthy tissue; b) the bone is slightly decorticated to promote healing and a bony anchor is inserted; c) the remnant tendinous healthy tissue is reinserted to bone with the aid of the bony anchor and the rest of the fascia is closed in a standard manner.
Radiographic examination may detect calcifications in the MCL, spurring on the medial aspect of the elbow joint, spurs in the posterior olecranon and the presence of loose bodies. An MRI scan will typically show incomplete injuries of the MCL that appear as areas of high signal intensity (Fig. 4). Other injuries can be seen in the articular cartilage, the flexor muscles and the ulnar nerve.29
Fig. 4.

In this T2 fat-saturated coronal MRI view, a partial tear of the medial collateral ligament from the medial epicondyle is observed as a high intensity signal (white arrow).
Conservative management
Conservative management is tailored according to the assessment of proper throwing technique and conditioning, the duration of symptoms, the location of pain, the presence of ulnar nerve symptoms and changes in pitch capacity and performance. An acute injury and frank instability in an ‘overhead athlete’ precludes conservative management of this injury. Conservative management generally includes stopping the aggravating activity and, after pain subsides, gradually re-introducing it while adjusting for technical errors. Proper conditioning of core muscles, scapular stabilisers and flexor-pronator muscles are crucial for proper management.
Operative treatment
Most authors favour some type of reconstruction technique although direct repair has been used occasionally. Jobe et al30 pioneered a reconstruction technique using the palmaris longus autograft that involved ulnar nerve transposition and elevation of flexor-pronator mass. Since then modifications have been introduced, most significantly a transmuscular approach that obviates the need for ulnar nerve transposition and the docking technique for proximal fixation and tensioning of the graft.31 The choice of graft material and the type of fixation is, at present, the choice of the treating surgeon.32 Fixation techniques usually involve bone tunnels around the sublime tubercle and a docking technique proximally, but an interference screw or extracortical buttons may be used to achieve proper tensioning of the graft. Associated treatment of the ulnar nerve must be performed as necessary. Associated pathologies, such as posteromedial elbow osteophytes, the presence of osteochondral injuries or loose bodies, are generally treated by arthroscopy prior to formal reconstruction of the ligament (Fig. 5).27
Fig. 5.
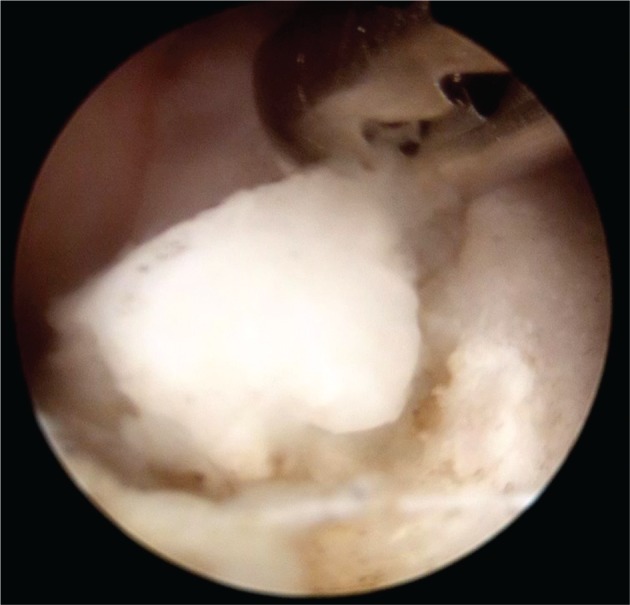
Loose bodies and osteophytes are removed arthroscopically in a patient with chronic medial collateral ligament insufficiency prior to ligament reconstruction. The image corresponds to a posterior viewing portal of a right elbow with a tissue grasper inserted through a posterolateral portal removing a posteromedial loose osteophyte.
Post-operative management includes a long arm cast for the first few days as inflammation resolves. After one week, the elbow is placed in a hinged brace and the joint is allowed to move from 40° to 90° of flexion, which is gradually increased over the next few weeks until full ROM is achieved. At week six, shoulder and forearm strengthening are initiated but valgus stress is avoided. At three months, strengthening exercises are increased, and at four months, an interval-throwing programme is initiated. Competitive throwing is usually deferred until 9 to 12 months post-operatively. Of patients treated with this protocol, 85% to 95% return to full activities (Table 3).30,32,33
Table 3.
Results of MCL repair
| Author | Patients (n) | Procedure | Follow-up | Results | Commentary |
|---|---|---|---|---|---|
| Jobe et al (1986)30 | 16 high-level throwing athletes | Free palmaris autograft. | - | 10/16 returned to same LP 1/16 lower LP 5/16 retired from pro athletics |
5/15 ulnar related problems: 3 transient sensory, 2 –late and early, required re-operation. |
| Rohrbough et al (2002)31 | 36 athletes | Free palmaris autograft with proximal docking tech. | 3.3 yrs | 92% returned to same or higher LP for at least 1 yr | All 22 professional or collegiate athletes returned to their previous competition level |
| Koh et al (2006)33 | 19 high-level throwing athletes | Muscle-splitting approach with proximal docking. Palmaris or gracilis autograft. | 41.9 mths (6.4 to 67.1) | 18 returned to same or higher LP at 13.1 mths. Conway |
Concomitant procedures included osteophyte removal (2) and loose body removal (1). 1 patient has SAT due to pre-operative ulnar neuritis. 1 patient underwent subsequent ulnar nerve SAT and returned to play. |
| Watson et al (2014)32 | 1368 patients | Included studies with the Jobe tech., Jobe modified tech. Interference screw, docking tech. and modified docking tech. |
Overall average return to play 78.9%, highest for the modified docking technique (91.3%) | Overall complication rate 18.6%: highest with original Jobe tech. and lowest with the modified docking tech. Ulnar nerve neuroapraxia in 12.9%. Re-operations in 6.7% |
LP, level of play; SAT, subcutaneous anterior transposition; tech., technique
Ulnar neuritis
Medial elbow pain may be caused by ulnar nerve entrapment with neuritis. The ulnar nerve may be entrapped in different locations from 10 cm proximal to 10 cm distal to the medial epicondyle, but most frequently by compression from Osborne’s ligament.34,35 The nerve courses proximally behind the medial epicondyle and runs close to the posterior band of the MCL and enters under the flexor carpi ulnaris fascia. Degenerative joint changes may alter the shape of the cubital tunnel and this is a cause of symptoms. Occasionally, the source of ulnar nerve symptoms may be multifocal and it can be difficult to distinguish this clinically. Snapping of the triceps, elbow instability and ME have all been related to ulnar nerve problems. This highlights the importance of exploring the ulnar nerve in patients with medial elbow pain.
Physical examination and imaging studies
Clinical examination starts with taking an appropriate history. Patients with ulnar nerve symptoms have pain on the medial side of the elbow aggravated by tapping on the nerve (neuritis) with or without sensory and/or motor symptoms distally (neuropathy). Inspection should assess for the presence of signs of trauma, deformity, masses or previous scars. A full neurological examination of the upper limb and cervical spine is required in every case presenting with medial elbow pain.7 The Tinel sign is used to address for potential sites of compression, being positive when distal tingling is elicited on percussion. If performed from distal to proximal, it may detect multiple sites of compression. Sensory testing can be performed using gross touch, two-point discrimination and Semmes-Weinstein monofilament testing. Motor testing focuses on the muscles innervated by the ulnar nerve, so a thorough understanding of the anatomy is recommended. Crossing the index and middle finger (crossover sign), Froment’s test (flexion of the thumb with a terminolateral pinch) and Wartenberg’s sign (abduction drift of the little finger) test intrinsic muscle function and can detect weakness of the first dorsal and second palmar interossei, abductor pollicis and flexor digiti quinti, respectively.
Diagnostic studies can be helpful to detect the origin and site of compression. Imaging studies, such as radiographs, may detect the presence of any deformity. US can study the cross-sectional area of the ulnar nerve and cubital tunnel and can detect soft-tissue masses and ligament injuries.36 MRI may show high signal intensity on T1 images in the surrounding muscles and increased signal intensity of the ulnar nerve on T2 images, suggesting neuritis.37 Electrodiagnostic studies can show reduced amplitude and speed at the sites of compression. The maximum drop in speed and amplitude of the electric signal detects the area of maximal compression.
Conservative management
Activity modification, night splinting and oral analgesics can be used in initial mild forms of the disease. Preventing high degrees of flexion may be helpful to decrease the pressure over the nerve. Patients with nerve instability may limit flexion at the point where it starts to dislocate by using a brace. Conservative management works best in cases with a short duration of symptoms and without nerve dislocation.
Surgical treatment
The options for surgical treatment include in situ decompression, transposition of the nerve or medial epicondylectomy. The clinical effect of decompression versus transposition was indistinguishable in a recent meta-analysis,38,39 while another one has shown a trend towards better outcomes with transposition (Table 4).40 Other authors have reported a lower rate of complications with decompression.41 After decompression, stability of the nerve must be carefully assessed. We favour using a subcutaneous transposition with an adipose sling if the nerve is unstable, and we only perform a submuscular transposition for revision cases or very thin patients. Post-operatively, we place the elbow in a sling and restrict heavy work of the arm for six weeks.
Table 4.
Results of surgical repair for cubital tunnel syndrome
| Author | Patients (n)/Studies | Procedure | Results | Commentary |
|---|---|---|---|---|
| Bartels et al (2005)41 | 152/RCT with 12 mths FU | SD vs AST | Excellent and good results in 49/75 in SD vs 54/77 in AST | Lower complication rate with simple decompression (9.6 vs 31%, RR, 0.32) |
| Zlowodzki et al (2006)38 | 261 / 4 RCT studies with 21 mths FU | SD vs transposition (AST – 2 studies; SMT – 2 studies) | No significant difference in clinical outcomes or motor nerve conduction tests | |
| Macadam et al (2008)40 | 449 SD, 342 AST, 115 SMT/ 10 studies | SD vs transposition (anterior/submuscular) | No significant difference in clinical outcomes | Trend toward a better outcome with transposition |
| Liu et al (2015)39 | 605 /2 RCT + 7 observational studies | Subcutaneous vs SMT | No significant differences in outcomes in either type of studies | Less adverse events in subcutaneous group. (RR, 0.54; 95% CI 0.33 to 0.87; p = 0.01) |
FU, follow-up; AST, anterior subcutaenous transposition; RCT, randomised controlled trial; SD, simple decompression; SMT, submuscular decompression; RR, risk ratio; CI, confidence interval
Snapping triceps
Snapping triceps refers to a spectrum of conditions in which the distal medial triceps subluxates over the medial epicondyle with elbow flexion, generally pushing the ulnar nerve anteriorly until it dislocates. The condition is variable in the amount of subluxation of the ulnar nerve which occurs and the triceps may be asymptomatic.42
The medial part of the distal triceps widens with elbow flexion and more so if resisted elbow extension is applied. This may push the nerve out of the groove (subluxation) or anteriorly to the medial epicondyle (dislocation) producing a snap. In certain situations, the medial border of the triceps can also subluxate, producing a second snap with increased flexion of the elbow. Conditions that may predispose this situation are a supernumerary triceps muscle, a variant tendinous insertion, a hypertrophic triceps, a hypoplastic medial epicondyle or cubitus varus.
Physical examination and imaging studies
The diagnosis is made by a good medical history and proper clinical examination. Patients report a combination of medial elbow pain, snapping and ulnar nerve symptoms. Examination should be directed towards detecting the two sources of snapping. With one’s finger in the cubital tunnel palpating the ulnar nerve, the elbow is flexed towards 90° of flexion and a first snap is palpated. Flexion is increased towards 110° to 120° and a second snap may be felt corresponding to the medial edge of the triceps dislocating over the medial epicondyle. Imaging techniques such as MR and US can help establish the relationship of these structures, however, MR must be performed in extension and in flexion to ensure appropriate evaluation. Dynamic US may be easier to perform, but requires expert evaluation.43
Other causes of snapping and medial elbow pain must be excluded clinically and include ME, posterolateral rotatory instability, isolated ulnar nerve dysfunction, MCL injury, synovial folds, loose bodies, failed ulnar nerve surgery after transposition, anconeous oedema and snapping of the medial antebrachialis cutaneous nerve.5,42
Conservative treatment
Non-operative management is warranted for a period of three to six months, except for patients presenting with severe symptoms who are recommended to have surgery earlier. Avoidance of elbow flexion during the night, sometimes using a brace, and oral analgesics or anti-inflammatories may be recommended.
Surgical treatment
If conservative management fails, surgery is warranted. The principles of surgery include treating the medial triceps and the ulnar nerve and then to evaluate and address the elbow joint (varus, instability, etc). Sequential dynamic exploration of the elbow throughout the surgery is critical to decrease the chance of persistent post-operative snapping. In general, a subcutaneous ulnar nerve transposition stabilised with an adipose or fascial sling is enough to address the ulnar neuropathy and may be enough in cases without marked triceps snapping. Revision procedures or very thin patients may require submuscular ulnar nerve transposition. Triceps snapping is addressed depending on the amount of triceps excursion over the medial epicondyle. Most frequently, a slip of the medial triceps is excised. When the triceps excursion is considered to be very large, a release and lateral transposition of the triceps is required (Fig. 6). However, it is important to rule out an associated cubitus varus.42 Post-operatively, dressings are used and active movement of wrist and fingers is encouraged. We prefer to rest the elbow in a splint for one week and in a sling after that, allowing for mild exercises for three more weeks. At six weeks, normal ROM exercises are resumed and strengthening can be started at three months post-operatively.
Fig. 6.

When the triceps distal insertion extends medially it may predispose to elbow snapping. In this intra-operative image of a left elbow, we observe exposure of the ulnar nerve and release of the medial extension of the triceps which can be removed or flipped on its long axis and reinserted to the native triceps. This will remove the snapping generated by the triceps. The ulnar nerve usually needs an anterior subcutaneous transposition at the end of the procedure to prevent snapping from the ulnar nerve over the medial epicondyle.
The results of surgery are generally good when all components are addressed as have been reported in small series and case reports.42
Elbow pain in the skeletally immature
Patients with open physis must be examined for specific diagnoses. The secondary ossification centres at the elbow ossify, starting at the of age two years (capitellum). Every two years, another ossification centre will ossify (radial head, medial epicondyle, trochlea, olecranon and lateral epicondyle) with closure of the apophyses occurring at around 14 to 16 years of age. Elbow injuries are more frequent than shoulder injuries in this age group and are a frequent source of consultation.
‘Little League elbow’
The high torque and shear forces of the repeated throwing movement in a growing elbow may produce an array of conditions ranging from growth disturbances of the medial epicondyle, traction apophysitis with radiological fragmentation and ME.10 More rarely, there is insufficiency (acute or chronic) of the MCL. The increase in intensity, the use of breaking pitches at a younger age, longer seasons, single-sport and year-round involvement are all factors that have increased the incidence of this problem.44 Associated findings may include loose bodies and olecranon nonunion at a younger age and olecranon fractures and secondary osteophyte formation at later stages.45
Patient history
Medial elbow pain is the presenting symptom in most of the patients. In the early stages, loss of velocity and loss of precision can be signs of injury. Most patients suffer from chronic symptoms but some may present after an acute injury.
Physical examination and imaging studies
Typically, medial elbow pain is present during the cocking and acceleration phases. Posterior elbow pain during the deceleration phase is typical of valgus overload syndrome. Associated symptoms from ulnar pathology and flexor tendinitis may be present. Some patients may show a slight flexion contracture of the elbow.
Radiographs are ordered after three weeks of persistent symptoms, an acute injury or significant pain. US and MR can be used to assess the structural integrity of the different medial structures and may increase the rate of pathological findings.
Conservative management
Management involves rest until the pain subsides, ROM exercises and strengthening core exercises. Strengthening of shoulder and forearm muscles should start gradually and an interval-throwing programme is initiated four to eight weeks after the initiation of treatment. Trainers, sports physicians, parents and patients must agree on treatment guidelines for adequate compliance. Complications such as flexion contractures, growth deformities or post-traumatic arthritis may develop, so careful follow-up is required.
Fractures of the medial epicondyle in the young throwing athlete
Medial epicondylar fractures usually occur as an acute episode following a valgus torque on the elbow in association with an elbow dislocation or following an acute contraction of the flexor mass as may happen during a throwing movement.9
Patient history, physical examination and imaging studies
These fractures usually happen in patients aged 11 to 15 years. Acute pain and a sensation of giving way are usually present. Fractures may be readily seen on radiographs and treatment recommendations are based on the degree of displacement.
Treatment
Minimally displaced fractures are treated with a course of immobilisation of three weeks and then ROM exercises are started. Fractures displaced > 1 cm are best treated surgically, but initial displacement usually averages at 5 mm so a discussion with the patient and family is warranted (Fig. 7). There is controversy, however, with fractures displaced > 5 mm because good outcomes have been shown with surgical and non-surgical management.9,46,47 Successful return to sports may be achieved in less than one year.
Fig. 7.
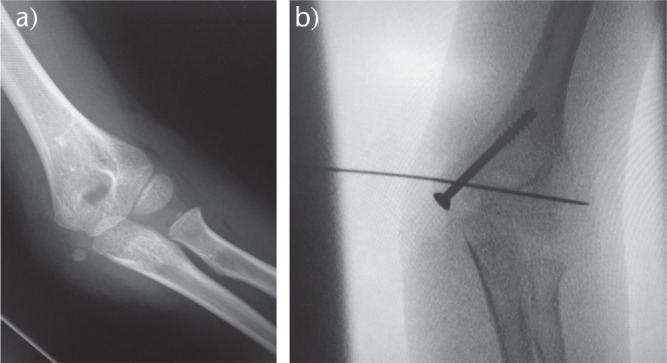
a) A displaced and comminuted medial epicondyle fracture is observed in an seven-year-old boy. b) Operative fixation of the fracture is performed with a screw. Intra-operative reduction with a Kirschner-wire assists in the reduction and is removed at the end of the procedure.
Footnotes
ICMJE Conflict of interest statement: Raul Barco is a board member of SECEC, ESSKA and SECHC, and reports consultancy and payment for lectures from Exactech, Conmed and Acumed, outside the submitted work. Samuel A. Antuña is a board member of the Journal of Shoulder and Elbow Surgery, consults for Exactech and receives payment for development of educational presentations from Zimmer Biomet and Acumed, outside the submitted work.
Funding
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
References
- 1. Shiri R, Viikari-Juntura E, Varonen H, Heliövaara M. Prevalence and determinants of lateral and medial epicondylitis: a population study. Am J Epidemiol 2006;164:1065-1074. [DOI] [PubMed] [Google Scholar]
- 2. Shiri R, Viikari-Juntura E. Lateral and medial epicondylitis: role of occupational factors. Best Pract Res Clin Rheumatol 2011;25:43-57. [DOI] [PubMed] [Google Scholar]
- 3. David TS. Medial elbow pain in the throwing athlete. Orthopedics 2003;26:94-105. [DOI] [PubMed] [Google Scholar]
- 4. Lynch JR, Waitayawinyu T, Hanel DP, Trumble TE. Medial collateral ligament injury in the overhand-throwing athlete. J Hand Surg Am 2008;33:430-437. [DOI] [PubMed] [Google Scholar]
- 5. Cesmebasi A, O’Driscoll SW, Smith J, Skinner JA, Spinner RJ. The snapping medial antebrachial cutaneous nerve. Clin Anat 2015;28:872-877. [DOI] [PubMed] [Google Scholar]
- 6. Nirschl RP, Ashman ES. Elbow tendinopathy: tennis elbow. Clin Sports Med 2003;22:813-836. [DOI] [PubMed] [Google Scholar]
- 7. Lee AT, Lee-Robinson AL. The prevalence of medial epicondylitis among patients with c6 and c7 radiculopathy. Sports Health 2010;2:334-336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Ollivierre CO, Nirschl RP, Pettrone FA. Resection and repair for medial tennis elbow. A prospective analysis. Am J Sports Med 1995;23:214-221. [DOI] [PubMed] [Google Scholar]
- 9. Osbahr DC, Chalmers PN, Frank JS, et al. Acute, avulsion fractures of the medial epicondyle while throwing in youth baseball players: a variant of Little League elbow. J Shoulder Elbow Surg 2010;19:951-957. [DOI] [PubMed] [Google Scholar]
- 10. Brogdon BG, Crow NE. Little leaguer’s elbow. Am J Roentgenol Radium Ther Nucl Med 1960;83:671-675. [PubMed] [Google Scholar]
- 11. van Rijn RM, Huisstede BM, Koes BW, Burdorf A. Associations between work-related factors and specific disorders at the elbow: a systematic literature review. Rheumatology (Oxford) 2009;48:528-536. [DOI] [PubMed] [Google Scholar]
- 12. Vinod AV, Ross G. An effective approach to diagnosis and surgical repair of refractory medial epicondylitis. J Shoulder Elbow Surg 2015;24:1172-1177. [DOI] [PubMed] [Google Scholar]
- 13. Suresh SPS, Ali KE, Jones H, Connell DA. Medial epicondylitis: is ultrasound guided autologous blood injection an effective treatment? Br J Sports Med 2006;40:935-939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. de Vos RJ, Windt J, Weir A. Strong evidence against platelet-rich plasma injections for chronic lateral epicondylar tendinopathy: a systematic review. Br J Sports Med 2014;48:952-956. [DOI] [PubMed] [Google Scholar]
- 15. Cardone DA, Tallia AF. Diagnostic and therapeutic injection of the elbow region. Am Fam Physician 2002;66:2097-2100. [PubMed] [Google Scholar]
- 16. Kijowski R, De Smet AA. Magnetic resonance imaging findings in patients with medial epicondylitis. Skeletal Radiol 2005;34:196-202. [DOI] [PubMed] [Google Scholar]
- 17. Amin NH, Kumar NS, Schickendantz MS. Medial epicondylitis: evaluation and management. J Am Acad Orthop Surg 2015;23:348-355. [DOI] [PubMed] [Google Scholar]
- 18. Grawe BM, Fabricant PD, Chin CS, et al. Clinical outcomes after suture anchor repair of recalcitrant medial epicondylitis. Orthopedics 2016;39:e104-e107. [DOI] [PubMed] [Google Scholar]
- 19. Gabel GT, Morrey BF. Operative treatment of medical epicondylitis. Influence of concomitant ulnar neuropathy at the elbow. J Bone Joint Surg [Am] 1995;77-A:1065-1069. [DOI] [PubMed] [Google Scholar]
- 20. Kurvers H, Verhaar J. The results of operative treatment of medial epicondylitis. J Bone Joint Surg [Am] 1995;77-A:1374-1379. [DOI] [PubMed] [Google Scholar]
- 21. Zonno A, Manuel J, Merrell G, et al. Arthroscopic technique for medial epicondylitis: technique and safety analysis. Arthroscopy 2010;26:610-616. [DOI] [PubMed] [Google Scholar]
- 22. Vangsness CT, Jr, Jobe FW. Surgical treatment of medial epicondylitis. Results in 35 elbows. J Bone Joint Surg [Br] 1991;73-B:409-411. [DOI] [PubMed] [Google Scholar]
- 23. Richard MJ, Aldridge JM, III, Wiesler ER, Ruch DS. Traumatic valgus instability of the elbow: pathoanatomy and results of direct repair. J Bone Joint Surg [Am] 2008;90-A:2416-2422. [DOI] [PubMed] [Google Scholar]
- 24. Fleisig GS, Andrews JR, Dillman CJ, Escamilla RF. Kinetics of baseball pitching with implications about injury mechanisms. Am J Sports Med 1995;23:233-239. [DOI] [PubMed] [Google Scholar]
- 25. Fleisig GS, Andrews JR, Cutter GR, et al. Risk of serious injury for young baseball pitchers: a 10-year prospective study. Am J Sports Med 2011;39:253-257. [DOI] [PubMed] [Google Scholar]
- 26. Grace SP, Field LD. Chronic medial elbow instability. Orthop Clin North Am 2008;39:213-219, vi. [DOI] [PubMed] [Google Scholar]
- 27. O’Holleran JD, Altchek DW. The thrower’s elbow: arthroscopic treatment of valgus extension overload syndrome. HSS J 2006;2:83-93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. O’Driscoll SW, Lawton RL, Smith AM. The “moving valgus stress test” for medial collateral ligament tears of the elbow. Am J Sports Med 2005;33:231-239. [DOI] [PubMed] [Google Scholar]
- 29. Cohen SB, Valko C, Zoga A, Dodson CC, Ciccotti MG. Posteromedial elbow impingement: magnetic resonance imaging findings in overhead throwing athletes and results of arthroscopic treatment. Arthroscopy 2011;27:1364-1370. [DOI] [PubMed] [Google Scholar]
- 30. Jobe FW, Stark H, Lombardo SJ. Reconstruction of the ulnar collateral ligament in athletes. J Bone Joint Surg [Am] 1986;68-A:1158-1163. [PubMed] [Google Scholar]
- 31. Rohrbough JT, Altchek DW, Hyman J, Williams RJ, III, Botts JD. Medial collateral ligament reconstruction of the elbow using the docking technique. Am J Sports Med 2002;30:541-548. [DOI] [PubMed] [Google Scholar]
- 32. Watson JN, McQueen P, Hutchinson MR. A systematic review of ulnar collateral ligament reconstruction techniques. Am J Sports Med 2014;42:2510-2516. [DOI] [PubMed] [Google Scholar]
- 33. Koh JL, Schafer MF, Keuter G, Hsu JE. Ulnar collateral ligament reconstruction in elite throwing athletes. Arthroscopy 2006;22:1187-1191. [DOI] [PubMed] [Google Scholar]
- 34. Karatas A, Apaydin N, Uz A, et al. Regional anatomic structures of the elbow that may potentially compress the ulnar nerve. J Shoulder Elbow Surg 2009;18:627-631. [DOI] [PubMed] [Google Scholar]
- 35. Khoo D, Carmichael SW, Spinner RJ. Ulnar nerve anatomy and compression. Orthop Clin North Am 1996;27:317-338. [PubMed] [Google Scholar]
- 36. van Den Berg PJ, Pompe SM, Beekman R, Visser LH. Sonographic incidence of ulnar nerve (sub)luxation and its associated clinical and electrodiagnostic characteristics. Muscle Nerve 2013;47:849-855. [DOI] [PubMed] [Google Scholar]
- 37. Dewan AK, Chhabra AB, Khanna AJ, Anderson MW, Brunton LM. MRI of the elbow: techniques and spectrum of disease: AAOS exhibit selection. J Bone Joint Surg [Am] 2013;95:1-13. [DOI] [PubMed] [Google Scholar]
- 38. Zlowodzki M, Chan S, Bhandari M, Kalliainen L, Schubert W. Anterior transposition compared with simple decompression for treatment of cubital tunnel syndrome. A meta-analysis of randomized, controlled trials. J Bone Joint Surg [Am] 2007;89-A:2591-2598. [DOI] [PubMed] [Google Scholar]
- 39. Liu CH, Wu SQ, Ke XB, et al. Subcutaneous versus submuscular anterior transposition of the ulnar nerve for cubital tunnel syndrome: a systematic review and meta-analysis of randomized controlled trials and observational studies. Medicine (Baltimore) 2015;94:e1207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Macadam SA, Gandhi R, Bezuhly M, Lefaivre KA. Simple decompression versus anterior subcutaneous and submuscular transposition of the ulnar nerve for cubital tunnel syndrome: a meta-analysis. J Hand Surg Am 2008;33:e1311-e1314. [DOI] [PubMed] [Google Scholar]
- 41. Bartels RH, Verhagen WI, van der Wilt GJ, et al. Prospective randomized controlled study comparing simple decompression versus anterior subcutaneous transposition for idiopathic neuropathy of the ulnar nerve at the elbow: Part 1. Neurosurgery 2005;56:522-530. [DOI] [PubMed] [Google Scholar]
- 42. Spinner RJ, Gabel GT. Latrogenic snapping of the medial head of the triceps after ulnar nerve transposition. J South Orthop Assoc 2001;10:236-240. [PubMed] [Google Scholar]
- 43. Spinner RJ, Hayden FR, Jr, Hipps CT, Goldner RD. Imaging the snapping triceps. AJR Am J Roentgenol 1996;167:1550-1551. [DOI] [PubMed] [Google Scholar]
- 44. Wei AS, Khana S, Limpisvasti O, et al. Clinical and magnetic resonance imaging findings associated with Little League elbow. J Pediatr Orthop 2010;30:715-719. [DOI] [PubMed] [Google Scholar]
- 45. Benjamin HJ, Briner WW., Jr. Little league elbow. Clin J Sport Med 2005;15:37-40. [DOI] [PubMed] [Google Scholar]
- 46. Josefsson PO, Danielsson LG. Epicondylar elbow fracture in children. 35-year follow-up of 56 unreduced cases. Acta Orthop Scand 1986;57:313-315. [DOI] [PubMed] [Google Scholar]
- 47. Hines RF, Herndon WA, Evans JP. Operative treatment of medial epicondyle fractures in children. Clin Orthop Relat Res 1987;223:170-174. [PubMed] [Google Scholar]