Abstract
Background
Cardiovascular (CV) complications are the main cause of death in end-stage renal disease (ESRD) patients. The high CV risks are attributable to the additive effects of multiple factors. Endothelin (EDN) is a potent vasoconstrictor and plays a role in regulating vascular homeostasis. However, whether variants of the EDN gene are associated with risks of CV events is not known. We conducted a study to investigate associations of variants of the EDN gene with CV events in ESRD patients.
Methods
A cohort of 190 ESRD patients was recruited, and 19 tagged single-nucleotide polymorphisms within the EDN gene family were selected for genotyping through a TaqMan assay. Data on clinical characteristics and hospitalizations for CV events were collected. Associations of genetic variants of the EDN gene with CV events were analyzed.
Results
In this cohort, 62% (n = 118) of patients were hospitalized for a CV event. The EDN1 rs4714384 (CC/TC vs. TT) polymorphism was associated with an increased risk of a CV event after multiple testing (p < 0.001). Further functional exploration showed that it was a quantitative trait locus which may significantly alter gene expression in the tibial artery.
Conclusions
EDN1 rs4714384 is very likely an important biomarker of CV events in ESRD patients.
Electronic supplementary material
The online version of this article (10.1186/s12882-017-0707-2) contains supplementary material, which is available to authorized users.
Keywords: Cardiovascular, Endothelin, Renal failure
Background
End-stage renal disease (ESRD) patients have a high risk of mortality, and 50% of these deaths are from cardiovascular (CV) complications [1]. Sudden cardiac death is observed in half of those cases, which is much more than coronary artery disease (CAD) [2]. Left ventricular hypertrophy (LVH) is considered to be one of the culprit pathophysiological expressions. It may contribute to the excess risk of sudden cardiac death and indicates poor survival in ESRD patients [3]. Besides LVH, vascular disorders, including atherosclerosis and arteriosclerosis, also account for the high risk of CV complications [4]. The exact mechanisms responsible for the excess CV risk in ESRD patients are not well understood.
Traditional and non-traditional risks factors, such as hypertension, diabetes, dyslipidemia, anemia, uremia, chronic inflammation, oxidative stress, calcium-phosphate vascular calcification, and autonomic dysfunction, contribute to a proportion of the excess risk [5, 6]. However, combining these risk factors does not fully explain the excess risk in these patients [5, 7]. Imbalances in some humoral factors and regulatory systems may also account for the excess CV risk. Activation of the renin-angiotensin-aldosterone system, and imbalanced endothelin (EDN) and nitric oxide levels were reported [8]. Demuth et al. [9] reported that an increased plasma endothelin level was associated with LVH and arterial intima-media thickening, suggesting this humoral factor may be important in cardiovascular remodeling. Whether genetic variants of candidate genes are related to the risk of CV disease (CVD) in ESRD patients is not known.
The EDN peptide family includes three isoforms (ET1, ET2, and ET3), which are coded by different genes, located on chromosomes 6p24.1 (EDN1), 1p34 (EDN2), and 20q13.2 ~ 13.3 (EDN3) [10]. Of these isoforms, ET1 is predominant. ET1 was reported to be strongly correlated with CVD, since it has a predominant vasoconstriction effect and hypertensive effect [10]. It has myocardial hypertrophic effects, [11] and its expression in endothelial tissues may be associated with instability of atherosclerotic plaque [12]. In addition, Minami et al. [13] reported that the plasma ET1 level was correlated with asymptomatic lacunar infarct and carotid plaques. ET2 was reported to be necessary for normal ovulation [14] and is associated with breast tumor invasion [15]. ET3 was identified as being abundant in the intestines and pituitary/brain tissues, which indicates it may have functions in nervous and endocrine systems [16]. Associations of genetic variants of the EDN genes with CV complications in ESRD patients are not well known. Thus, we investigated genetic variants of the EDN genes and CV events. We hypothesized that common variants of the EDN genes are associated with increased risks of hospitalizations for CV events in ESRD patients.
Methods
Study subjects
This study recruited adult patients older than 18 years, who had received chronic dialysis for at least 3 months at Taipei Medical University Hospital. 90% (n = 171) of patients received hemodialysis and the remaining received peritoneal dialysis. Demographics and clinical data of all patients were collected, including dialysis vintage, smoking, the erythropoietin resistance index (ERI), hemoglobin, albumin, iron profiles, adequacy of dialysis (Kt/V), pre-existing CV comorbidities, and cause of ESRD. ERI was calculated by the average weekly erythropoietin dose per kg body weight per average hemoglobin, which indicated a patient’s response to erythropoietin. After enrollment, patients were followed up until the development of hospitalization for a CV event. The length of time from study enrollment to the development of CV event was collected. We defined hospitalized “CV events” as including CAD, congestive heart failure (CHF), arrhythmia, aortic aneurysm, stroke, and peripheral arterial occlusive disease (PAOD). These outcomes were prespecified in our protocol. CAD was defined as patients who received coronary angiography and ≥75% stenosis of a major coronary artery was noted. Congestive heart failure was documented according to the clinical diagnostic criteria by cardiologist, either by an episode of pulmonary edema, systolic dysfunction by cardiac sonography or cardiomegaly. Arrhythmia was documented as newly onset of irregular heart beat by electrocardiogram. Aortic aneurysm was confirmed by aortic imaging via radiographic studies. Stroke was defined as focal neurologic symptoms with image evidences. Peripheral arterial occlusive disease was documented by symptoms of ischemic muscle pain and radiographic studies. This study was approved by the Institutional Review Board of Taipei Medical University (no. 201309026). Written informed consent was obtained from all patients.
Genotyping
These tagged SNPs were determined to have a minimum allele frequency of >1% in a Beijing Han Chinese population (https://www.ncbi.nlm.nih.gov/variation/news/NCBI_retiring_HapMap/). Genotyping was done using the TaqMan Allelic Discrimination Assay (Applied Biosystems, Foster City, CA). Polymerase chain reaction (PCR) was carried out with an ABI StepOnePlus Thermal Cycler (Applied Biosystems). The fluorescence from different probes was detected and analyzed via the System SDS software version 2.2.2 (Applied Biosystems).
Statistical analysis
R 3.2.0 was used for the statistical analyses. The Chi-squared test and Student’s t-test were used for comparing demographic characteristics between groups as indicated. A multivariable logistic regression model was performed to control for possible confounding factors, including age, gender, smoking, diabetes, hypertension, pre-existing CV comorbidities, hemoglobin, albumin, ferritin, and the ERI. We analyzed the magnitude of the association between the different genotypes and hospitalization for a CV event through a likelihood ratio test. Odds ratios (OR) with 95% confidence intervals were determined. Multiple testing correction was carried out using the false discovery rate (FDR), and q-values of <0.05 were determined to indicate statistical significance.
SNP functional annotation
In order to evaluate the relationship between the SNPs and gene expression profiles, we queried the GTEx Portal (https://www.gtexportal.org/home/), which contain expression quantitative trait loci (eQTLs) across multiple tissues. The SNP function prediction web site (https://snpinfo.niehs.nih.gov/snpinfo/snpfunc.html), which provides a variety of possible downstream influence of variants, was also applied to identify potential impact of candidate SNPs.
Results
In total, 19 tSNPs of the EDN family (EDN1: rs5370, rs2070699, rs2248580, rs4714384, and rs3087459; EDN2: rs2759257, rs11210278, rs11572340, and rs11572377; and EDN3: rs742650, rs260740, rs260741, rs6064764, rs197173, rs197174, rs882345, rs926632, rs3026575, and rs11570352) were genotyped (Fig. 1a-c ). The minor allele frequencies of these tSNPs were close to those of the reference population from the Taiwan Biobank database and HapMap project (Table 1).
Fig. 1.
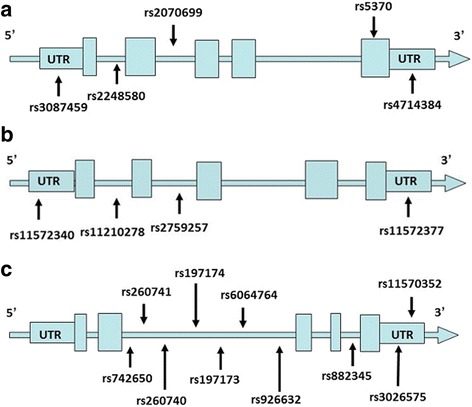
a. Graphic view of the genotyped human EDN-1 gene. b. Graphic view of the genotyped human EDN-2 gene. c. Graphic view of the genotyped human EDN-3 gene
Table 1.
Minor allele frequencies of selected tagged single-nucleotide polymorphisms (SNPs) of the endothelin (EDN) gene family
| Gene | Position | SNP | Location | Ref | Alt | AFR fre | AMR fre | ASN fre | EUR fre | TWB fre | Our fre |
|---|---|---|---|---|---|---|---|---|---|---|---|
| EDN1 | Ch6:12,289,406 | rs3087459 | 5’UTR | A | C | 0.19 | 0.14 | 0.20 | 0.20 | 0.23 | 0.17 |
| Ch6:12,291,749 | rs2248580 | Intron | C | A | 0.08 | 0.56 | 0.56 | 0.47 | 0.41 | 0.35 | |
| Ch6:12,292,539 | rs2070699 | Intron | G | T | 0.05 | 0.46 | 0.56 | 0.47 | 0.49 | 0.43 | |
| Ch6:12,296,022 | rs5370 | Missense | G | T | 0.14 | 0.17 | 0.28 | 0.21 | 0.31 | 0.23 | |
| Ch6:12,297,620 | rs4714384 | 3’UTR | T | C | 0.71 | 0.38 | 0.62 | 0.37 | 0.38 | 0.34 | |
| EDN2 | Ch1:41,485,234 | rs11572340 | 5’UTR | C | A | 0.04 | 0.16 | 0.07 | 0.21 | 0.06 | 0.02 |
| Ch1:41,484,301 | rs11210278 | Intron | C | T | 0.01 | 0.11 | 0.33 | 0.19 | 0.30 | 0.29 | |
| Ch1:41,483,957 | rs2759257 | Intron | A | C | 0.75 | 0.89 | 0.91 | 0.86 | 0.88 | 0.93 | |
| Ch1:41,478,124 | rs11572377 | 3’UTR | C | G | 0.01 | 0.01 | 0.08 | 0.02 | 0.09 | 0.05 | |
| EDN3 | Ch20:59,303,616 | rs742650 | Intron | C | T | 0.00 | 0.03 | 0.15 | 0.06 | 0.14 | 0.11 |
| Ch20:59,301,100 | rs260741 | Intron | G | A | 0.06 | 0.31 | 0.24 | 0.21 | 0.25 | 0.27 | |
| Ch20:59,305,927 | rs260740 | Intron | T | G | 0.28 | 0.25 | 0.22 | 0.28 | 0.22 | 0.15 | |
| Ch20:59,303,025 | rs197174 | Intron | T | C | 0.63 | 0.30 | 0.16 | 0.26 | 0.16 | 0.12 | |
| Ch20:59,303,536 | rs197173 | Intron | T | G | 0.96 | 0.67 | 0.72 | 0.85 | 0.74 | 0.74 | |
| Ch20:59,309,196 | rs6064764 | Intron | T | C | 0.03 | 0.20 | 0.07 | 0.32 | 0.09 | 0.10 | |
| Ch20:59,309,707 | rs926632 | Intron | C | T | 0.42 | 0.70 | 0.85 | 0.70 | 0.87 | 0.89 | |
| Ch20:59,319,323 | rs882345 | Intron | A | G | 0.10 | 0.16 | 0.15 | 0.19 | 0.13 | 0.09 | |
| Ch20:59,324,630 | rs3026575 | 3’UTR | G | A | 0.00 | 0.00 | 0.05 | 0.00 | 0.04 | 0.14 | |
| Ch20:59,324,605 | rs11570352 | 3’UTR | C | T | 0.00 | 0.00 | 0.05 | 0.00 | 0.06 | 0.06 |
Fre Alt frequency, UTR untranslated region
In total, 190 patients were recruited for this study. The length of follow-up for the entire cohort was 22.9 +/− 10.6 months. The mean age was 64 years, and 54% of them were male. Pre-existing CV events were found in 43 patients with more than 83% due to CHF (n = 16, 37%) and CAD (n = 20, 47%). After enrollment, there were 118 patients (62.1%) who experienced hospitalization for a CV event with a mean duration of 17.2 ± 8.8 months. Of these CV events, CAD and CHF remained the most commonly observed (Additional file 1: Table S1). We divided patients into study and control groups according to the development of CV events. Patients in the study group included more males, were older, and had more diabetes. Lower albumin, serum iPTH, and Kt/V levels were observed in study group patients (Table 2).
Table 2.
Baseline characteristics of study patients according to cardiovascular disease (CVD)
| CVD (n = 118) | No CVD (n = 72) | p value | |
|---|---|---|---|
| Gender, male, n (%) | 74 (62.7%) | 29 (40.3%) | 0.003 |
| Age (years) | 67 ± 13 | 60 ± 12 | <0.001 |
| Dialysis vintage (years) | 4.3 ± 3.8 | 5.5 ± 6.7 | 0.111 |
| Current smoking (%) | 20 (16.9%) | 5 (6.9%) | 0.050 |
| Diabetes, n (%) | 73 (61.9%) | 17 (23.6%) | <0.001 |
| ERI (unit/week/kg/Hb) | 8.5 ± 6.7 | 8.0 ± 4.1 | 0.600 |
| Hemoglobin (g/dl) | 10.7 ± 1.2 | 10.7 ± 1.1 | 0.980 |
| Albumin (g/dl) | 3.9 ± 0.4 | 4.1 ± 0.4 | 0.005 |
| Ferritin (mg/dl) | 418 ± 401 | 458 ± 736 | 0.635 |
| Iron (mg/dl) | 65 ± 24 | 68 ± 33 | 0.571 |
| TIBC (mg/dl) | 236 ± 47 | 242 ± 54 | 0.441 |
| Serum i-PTH (pg/mL) | 277 ± 363 | 422 ± 354 | 0.012 |
| Kt/V | 1.44 ± 0.26 | 1.60 ± 0.31 | 0.001 |
| Cause of ESRD, n (%) | <0.001 | ||
| Hypertension | 16 (13.5%) | 18 (25.0%) | |
| Diabetes | 67 (56.8%) | 17 (23.6%) | |
| GN | 14 (11.9%) | 22 (30.6%) | |
| CHF | 8 (6.8%) | 0 (0%) | |
| Others | 13 (11.0%) | 15 (20.8%) |
CHF congestive heart failure, ERI erythropoietin resistance index, ESRD end-stage renal disease, GN glomerulonephritis, iPTH parathyroid hormone, Kt/V dialysis adequacy, TIBC total iron-binding capacity. p values of <0.05 are shown in bold
After multivariable adjustment, we found that patients carrying EDN1 rs2248580 (AA/CA vs. CC), rs2070699 (GT/TT vs. GG), rs4714384 (CC/TC vs. TT) (Table 3), EDN2 rs11210278 (TC/CC vs. TT) (Table 4) were associated with an increased risk of being hospitalized for a CV event in the recessive models. All of the EDN1 variants remained statistically significant after multiple testing correction (q values of 0.013, 0.003, and <0.001). However, none of EDN3 SNPs showed significant association with the susceptibility of developing cardiovascular disease (Table 5). In addition, we conducted functional annotation for these SNPs via several publicly available databases. The results showed that EDN1 rs4714384 is an eQTL in the tibial artery tissue (p = 6.3*10−9) (Table 6). We further analyzed the association of EDN1 rs4714384 with each CV comorbidity, which showed non-significant findings (Additional file 1: Table S2).
Table 3.
Association analysis of genetic polymorphisms of the EDN1 gene and cardiovascular disease susceptibility in end-stage renal disease patients
| Cardiovascular disease susceptibility | Recessive | |||||
|---|---|---|---|---|---|---|
| rs number | Genotype | Cases (%) | Control (%) | OR (95% CI) | p value | q-value |
| rs3087459 | CC | 3 (3%) | 3 (5.8%) | 0.06 (0.01–0.69) | 0.019 | 0.086 |
| CA | 26 (25.7%) | 13 (25%) | 1 | |||
| AA | 72 (71.3%) | 36 (69.2%) | 1 | |||
| rs2248580 | CC | 8 (7.8%) | 12 (21.8%) | 0.10 (0.02–0.47) | 0.001 | 0.013 |
| CA | 49 (48.0%) | 22 (40.0%) | 1 | |||
| AA | 45 (44.1%) | 21 (38.2%) | 1 | |||
| rs2070699 | GG | 11 (11.7%) | 16 (29.6%) | 0.09 (0.02–0.38) | <.001 | 0.003 |
| GT | 50 (53.2%) | 22 (40.7%) | 1 | |||
| TT | 33 (35.1%) | 16 (29.6%) | 1 | |||
| rs5370 | TT | 5 (2.5%) | 4 (10.0%) | 0.30 (0.04–2.08) | 0.216 | 0.388 |
| TG | 32 (40.0%) | 20 (32.2%) | 1 | |||
| GG | 61 (57.5%) | 28 (57.8%) | 1 | |||
| rs4714384 | TT | 7 (7.2%) | 14 (26.9%) | 0.05 (0.01–0.23) | <.001 | <.001 |
| TC | 42 (43.3%) | 17 (32.7%) | 1 | |||
| CC | 48 (49.5%) | 21 (40.4%) | 1 | |||
p values were adjusted for age, sex, smoking, diabetes, hypertension, pre-existing cardiovascular events, hemoglobin, albumin, ferritin, and the erythropoietin resistance index. p and q-values of <0.05 are shown in bold. q-values of <0.05 were considered statistically significant after correction for multiple testing. OR, odds ratio; CI, confidence interval
Table 4.
Association analysis of genetic polymorphisms of the EDN2 gene and cardiovascular disease susceptibility in end-stage renal disease patients
| Cardiovascular disease susceptibility | Recessive | |||||
|---|---|---|---|---|---|---|
| rs number | Genotype | Cases (%) | Control (%) | OR (95% CI) | p value | q-value |
| rs11572340 | AA | 1 (0.9%) | 0 (0%) | 0.74 (0.14 ~ 3.85) | 0.708 | 0.796 |
| AC | 5 (4.3%) | 2 (2.9%) | 1 | |||
| CC | 109 (94.8%) | 66 (97.1%) | 1 | |||
| rs11210278 | TT | 8 (9.9%) | 7 (18.9%) | 0.17 (0.03 ~ 0.88) | 0.035 | 0.126 |
| TC | 30 (37.0%) | 9 (24.3%) | 1 | |||
| CC | 43 (53.1%) | 21 (56.8%) | 1 | |||
| rs2759257 | AA | 0 (0%) | 0 (0%) | - | NA | NA |
| AC | 17 (15.3%) | 6 (9.4%) | 1 | |||
| CC | 94 (84.7%) | 58 (90.6%) | 1 | |||
| rs11572377 | GG | 2 (1.7%) | 1 (1.4%) | 0.88 (0.07 ~ 11.11) | 0.920 | 0.953 |
| GC | 10 (8.6%) | 2 (2.8%) | 1 | |||
| CC | 104 (89.7%) | 69 (95.8%) | 1 | |||
p values were adjusted for age, sex, smoking, diabetes, hypertension, pre-existing cardiovascular events, hemoglobin, albumin, ferritin, and the erythropoietin resistance index. p and q-values of <0.05 are shown in bold. q-values of <0.05 were considered statistically significant after correction for multiple testing. OR, odds ratio; CI, confidence interval
Table 5.
Association analysis of genetic polymorphisms of the EDN3 gene and cardiovascular disease susceptibility in end-stage renal disease patients
| Cardiovascular disease susceptibility | Recessive | |||||
|---|---|---|---|---|---|---|
| rs number | Genotype | Cases (%) | Control (%) | OR (95% CI) | p value | q-value |
| rs742650 | TT | 0 (0%) | 2 (3.9%) | - | 0.087 | 0.197 |
| CT | 20 (21.5%) | 7 (13.7%) | 1 | |||
| CC | 73 (78.5%) | 42 (82.4%) | 1 | |||
| rs260741 | AA | 8 (8.4%) | 4 (9.1%) | 0.45 (0.08 ~ 2.44) | 0.356 | 0.583 |
| AG | 31 (32.6%) | 19 (43.2%) | 1 | |||
| GG | 56 (58.9%) | 21 (47.7%) | 1 | |||
| rs260740 | GG | 1 (1.0%) | 0 (0%) | - | 0.708 | 0.796 |
| GT | 27 (26.0%) | 16 (32.0%) | 1 | |||
| TT | 76 (73.1%) | 34 (68.0%) | 1 | |||
| rs197174 | GG | 1 (1.0%) | 4 (7.7%) | 0.12 (0.01 ~ 1.49) | 0.074 | 0.197 |
| GA | 19 (18.4%) | 9 (17.3%) | 1 | |||
| AA | 83 (39.0%) | 39 (75.0%) | 1 | |||
| rs197173 | TT | 9 (9.0%) | 6 (11.1%) | 1.67 (0.38 ~ 7.14) | 0.497 | 0.662 |
| GT | 33 (33.0%) | 18 (33.3%) | 1 | |||
| GG | 58 (58.0%) | 30 (55.6%) | 1 | |||
| rs6064764 | CC | 2 (1.9%) | 1 (1.6%) | 0.03 (0.01 ~ 1.59) | 0.083 | 0.197 |
| CT | 24 (22.4%) | 4 (6.3%) | 1 | |||
| TT | 81 (75.7%) | 58 (92.1%) | 1 | |||
| rs926632 | CC | 2 (1.9%) | 3 (5.2%) | 2.86 (0.97 ~ 8.33) | 0.514 | 0.662 |
| CT | 19 (17.8%) | 8 (13.8%) | 1 | |||
| TT | 86 (80.4%) | 47 (81.0%) | 1 | |||
| rs882345 | GG | 2 (1.9%) | 2 (3.7%) | 0.92 (0.05 ~ 16.67) | 0.953 | 0.953 |
| GA | 14 (13.5%) | 7 (13.0%) | 1 | |||
| AA | 88 (84.6%) | 45 (83.3%) | 1 | |||
| rs3026575 | AA | 1 (1.0%) | 0 (0%) | - | 0.515 | 0.662 |
| AG | 7 (6.8%) | 4 (7.1%) | 1 | |||
| GG | 95 (92.2%) | 52 (92.9%) | 1 | |||
| rs11570352 | TT | 3 (2.5%) | 5 (7.0%) | 0.20 (0.01 ~ 2.94) | 0.216 | 0.388 |
| TC | 4 (3.4%) | 1 (1.4%) | 1 | |||
| CC | 111 (94.1%) | 65 (91.5%) | 1 | |||
p values were adjusted for age, sex, smoking, diabetes, hypertension, pre-existing cardiovascular events, hemoglobin, albumin, ferritin, and the erythropoietin resistance index. q-values of <0.05 were considered statistically significant after correction for multiple testing. OR, odds ratio; CI, confidence interval
Table 6.
Endothelin (EDN) gene family-related expression quantitative trait loci (eQTLs)
| Gene symbol | SNP Id | GENCODE ID | p value | Effect size | Tissue |
|---|---|---|---|---|---|
| EDN1 | rs3087459 | ENSG00000078401.6 | 1.5e-5 | 0.25 | Cells - Transformed fibroblasts |
| RN7SKP293 | rs4714384 | ENSG00000223321.1 | 6.3e-9 | −0.37 | Artery - Tibial |
| EDN2 | rs11210278 | ENSG00000127129.5 | 3.1e-6 | 0.55 | Heart - Left Ventricle |
Discussion
In this study, we systemically performed genotyping of the EDN gene family, and three variants in the EDN1 gene [rs2248580 (AA/CA vs. CC), rs2070699 (GT/TT vs., GG), and rs4714384 (CC/TC vs. TT)] were associated with an increased risk of a CV event. These tSNPs were not located in the exon region, and therefore were not correlated with protein-coding functions. These genetic variants may alter disease phenotypes through other pathways, such as non-coding RNA, transcriptional regulation, or alterations in splicing [17]. Although there is no eQTL evidence between rs4714384 and EDN1 being observed in the current database due to limited available tissue specific profile, we found that rs4714384 has impact on RN7SKP293 expression in the tibial artery. The RN7SKP293 is a pseudogene, belonging to the 7SK RNA class. 7SK RNA is found in a small nuclear ribonucleoprotein (snRNP) complex, which regulates the activity of positive transcription elongation factor b (P-TEFb) [18]. P-TEFb is a kind of cyclin-dependent kinase (Cdk) which controls the elongation phase of transcription by RNA polymerase II [19]. Cdk is a cell-cycle check point regulator, and one study showed Cdk9 may have transcriptional roles in cardiac hypertrophy and mitochondrial dysfunction [20]. Another study showed overexpression of Cdk2 may promote smaller, less differentiated cardiomyocytes which have increased response to pressure overload [21]. Cdk dysregulation may be related to LVH, which may result in future CHF. Endothelial cells are the main origin of ET-1 production. Endothelial dysfunction is an important pathophysiology in ESRD patients, and is strongly associated with a risk of atherosclerosis and consequent CV events [22]. Its manifestations represent a systemic pathogenic condition, which implies an inflammatory state, prothrombotic state, and impaired vasomotor and cellular proliferation in the vascular wall [23]. Imbalances of humoral factors, including nitric oxide, oxidative stress, chemokines, angiotensin II, and EDN-1, on vascular homeostasis may contribute to this condition [22]. In addition, Ganz et al. [24] reported that the peripheral artery endothelial function has rather better prognostic predictions of CV events than coronary artery endothelial function. Our findings suggest that genetic variants of EDN1 may alter the balance of the homeostasis of peripheral vascular regulation, and affect the susceptibility to CV comorbidities.
We further investigated EDN gene expressions among different tissues through GTEx. However, low expression levels of both EDN2 and EDN3 were noted in the heart and major vessel tissues [25]. By querying the SNP function prediction web site, we found that rs11210278 (caTAATCgag) is a potential binding site for GATA6, which is a transcription factor involved in hypertrophic cardiomyopathy (Additional file 1: Table S3). This finding may be correlated with our finding, since the C allele of the rs11210278 is a predominant binding site for GATA6; therefore, patients carrying this allele may confer an increased binding affinity of the GATA6 transcription factor and consequently increased risk of hypertrophic cardiomyopathy. Cardiomyopathy is an important pathophysiology of CV events in ESRD patients [5]. Although this allele was not statistically significant after multiple testing correction, further enlarging sample sizes and functional validation studies are warranted for confirmation.
Vargas-Alarcon et al. [26] reported that an EDN1 rs3087459 polymorphism (AA allele) was associated with an increased risk of developing acute coronary syndrome. However, two other studies did not find such an association of EDN1 rs3087459 with the risk of myocardial infarction or ventricular hypertrophy [27, 28]. In our study, we also did not find a statistically significant association of higher risk of CV events with the SNP rs3087459. Rankinen et al. [29] reported that an EDN1 (Glu106Glu) polymorphism had a risk of HTN in a Caucasian population. Another study showed that genetic polymorphisms of the EDN1 rs5370 T allele and rs2070699 G allele were associated with an increased risk of ischemic stroke, [30] which is contrary to our findings. We found that rs3087459 may alter the gene expression in transformed fibroblasts according to the results of eQTL database; however, the association of fibroblasts with CV events remained elusive. Comparing the above studies to ours, different outcome measurements were noted. The small sample size may also limit our observations.
Previous studies showed dialysis vintage is a risk factor for coronary artery calcification, which may reflect the major risk of CV events [31, 32]. Therefore, the increased risk of CV events occurred with a longer duration of dialysis, which may account for the increased events during our observation period. According to the USRDS 2012 annual data report, [33] the incidence of hospitalization for CV morbidity is 4.5–5 times per 100-patient-months. Our cohort showed a relative fewer hospitalization of CV events, as compared to US database. We have a better 5-year overall survival in dialysis patients. Compared to other countries, the CV-related morbidity and mortality are much lower in Taiwan [34]. It may reflect the different epidemiology of CV events among populations. In our study, being male, being elderly, having hypoalbuminemia, and having underlying diabetes mellitus were risk factors for CV events. Being male and elderly are well known risk factors for CVDs [35, 36]. Malnutrition-inflammation complex syndrome is frequently observed in dialysis patients and is associated with an increased risk of CVD. Protein energy wasting and low albumin levels are poor outcome indicators [37]. Diabetes patients exhibit increased insulin resistance and an inflammatory status [38]. A previous study by Chang et al. [39] reported that diabetes and ESRD synergistically contribute to an increased risk of CV events.
Lower PTH and Kt/V level were associated with increased risk of CV events. Some studies showed hyperparathyroidism was associated with increased risk of CV mortality and all-cause mortality in dialysis patients [40–42]. However, a meta-analysis showed no significant association between PTH level and non-fatal cardiovascular events or CV mortality [43]. The PTH level is pulsatile in character and highly sensitive to change in ionized calcium and calcitriol levels [44]. There may be selection bias in our small sample size cohort. Therefore the association between low PTH and risk of CV events may need further investigation. In renal failure patients, there are a lot of uremic toxins leading to inflammation and subsequently CV events. Better Kt/V is associated with less uremic toxins retention, which may be related to lower risk of CV events. Đurić PS et al. [45] reported longer dialysis duration was associated with lower CV comorbidities. The FHN (Frequent Hemodialysis Network) trial group [46] also found better composite outcomes of death or change in left ventricular mass in frequent hemodialysis group as compared to conventional hemodialysis. In this view, the patients who received better dialysis clearance may have lower risk of CV events.
As we know, there were several identified risk factors contributing to cardiovascular comorbidities in renal failure patients. However, the prevalence and severity of CV events in ESRD patients is disproportionate to the identified risk profiles [47]. In the current study, we found potential genetic risk alleles and this may further improve the prediction model for CV comorbidities in these patients.
Several limitations of this study should be noted. First, the sample size was not large, and thus the statistical power may be limited. Second, we did not check the plasma ET-1 level to prove associations of genetic variants with its expression, as it was reported to be associated with several phenotypes in previous studies [13]. Third, we did not find the association between the SNPs of EDN and pre-existing CV events. It may be due to different composition of pre-existing CV events and different dialysis stage of these patients.
Conclusions
We found three genetic variants of the EDN1 gene to be associated with increased risk of hospitalization for a CV event, and rs4714384 was responsible as an eQTL in the peripheral artery. It may influence the EDN1 gene expression and alter vascular homeostasis in the peripheral artery. A further validation study is required to confirm the roles of these polymorphisms in the risk of CV events.
Acknowledgements
C.C.K. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. All the authors of this work have read and approved the final version of the manuscript.
Funding
The study was supported by grants from the Ministry of Health and Welfare (MOHW104-TDU-B-212-113,001) and Taipei Medical University Hospital (103TMUH-NE-04).
Availability of data and materials
All data related to this article are shown in the manuscript or available upon request from the corresponding authors.
Abbreviations
- CAD
Coronary artery disease
- Cdk
Cyclin-dependent kinase
- CHF
Congestive heart failure
- CV
Cardiovascular
- EDN
Endothelin
- eQTL
expression quantitative trait locus
- ERI
Erythropoietin resistance index
- ESRD
End stage renal disease
- ET1
Endothelin 1
- FDR
False discovery rate
- GTEx
Genotype-Tissue Expression
- Kt/V
Adequacy of dialysis
- LVH
Left ventricular hypertrophy
- OR
Odds ratios
- PAOD
Peripheral arterial occlusive disease
- PCR
Polymerase chain reaction
- P-TEFb
Positive transcription elongation factor b
- snRNP
small nuclear ribonucleoprotein
Additional file
Demographic characteristic of the study patients. Table S2. Association of EDN1_rs4714384 and cardiovascular disease in ESRD patients. Table S3. Potential function prediction of SNP in transcription factor binding site in EDN gene family. (DOCX 21 kb)
Authors’ contributions
CCK: study concept and design; researched data; analysis and interpretation of data; drafting of the manuscript. SYC: the molecular genetic studies; researched data. MYW: researched data; analysis and interpretation of data. SCC: study concept and design; researched data. HFL: statistical analysis and interpretation of data. YWH: analysis and interpretation of data. YFZ: statistical analysis and interpretation of data. MSW: study concept and design; final approval of the version to be published. WCC: study concept and design; final approval of the version to be published.
Ethics approval and consent to participate
This study was approved by the Institutional Review Board of Taipei Medical University (no. 201309026). Written informed consent was obtained from all patients.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Footnotes
Electronic supplementary material
The online version of this article (10.1186/s12882-017-0707-2) contains supplementary material, which is available to authorized users.
Contributor Information
Chih-Chin Kao, Email: salmonkao@gmail.com.
Shih-Ying Cheng, Email: whitementha@gmail.com.
Mei-Yi Wu, Email: e220121@gmail.com.
Shu-Chen Chien, Email: sophia@tmu.edu.tw.
Hsing-Fang Lu, Email: shefunlu@gmail.com.
Yu-Wen Hsu, Email: fish770426@hotmail.com.
Yan-Feng Zhang, Email: youngorchuang@hotmail.com.
Mai-Szu Wu, Phone: 886-2-22490088, Email: maiszuwu@gmail.com.
Wei-Chiao Chang, Phone: 886-2-27361661, Email: wcc@tmu.edu.tw.
References
- 1.Collins AJ, Foley RN, Herzog C, Chavers BM, Gilbertson D, Ishani A, et al. Excerpts from the US Renal Data System 2009 Annual Data Report. Am J Kidney Dis. 2010;55(1 Suppl 1):S1–420. doi: 10.1053/j.ajkd.2009.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Genovesi S, Valsecchi MG, Rossi E, Pogliani D, Acquistapace I, De Cristofaro V, et al. Sudden death and associated factors in a historical cohort of chronic haemodialysis patients. Nephrol Dial Transplant. 2009;24(8):2529–2536. doi: 10.1093/ndt/gfp104. [DOI] [PubMed] [Google Scholar]
- 3.Silberberg JS, Barre PE, Prichard SS, Sniderman AD. Impact of left ventricular hypertrophy on survival in end-stage renal disease. Kidney Int. 1989;36(2):286–290. doi: 10.1038/ki.1989.192. [DOI] [PubMed] [Google Scholar]
- 4.London GM. Cardiovascular disease in chronic renal failure: pathophysiologic aspects. Semin Dial. 2003;16(2):85–94. doi: 10.1046/j.1525-139X.2003.16023.x. [DOI] [PubMed] [Google Scholar]
- 5.Ghanta M, Kozicky M, Jim B. Pathophysiologic and treatment strategies for cardiovascular disease in end-stage renal disease and kidney transplantations. Cardiol Rev. 2015;23(3):109–118. doi: 10.1097/CRD.0000000000000044. [DOI] [PubMed] [Google Scholar]
- 6.Anderson S, Halter JB, Hazzard WR, Himmelfarb J, Horne FM, Kaysen GA, et al. Prediction, progression, and outcomes of chronic kidney disease in older adults. J Am Soc Nephrol. 2009;20(6):1199–1209. doi: 10.1681/ASN.2008080860. [DOI] [PubMed] [Google Scholar]
- 7.Sarnak MJ, Levey AS, Schoolwerth AC, Coresh J, Culleton B, Hamm LL, et al. Kidney disease as a risk factor for development of cardiovascular disease: a statement from the American Heart Association Councils on Kidney in Cardiovascular Disease, High Blood Pressure Research, Clinical Cardiology, and Epidemiology and Prevention. Circulation. 2003;108(17):2154–2169. doi: 10.1161/01.CIR.0000095676.90936.80. [DOI] [PubMed] [Google Scholar]
- 8.Schlaich MP, Socratous F, Hennebry S, Eikelis N, Lambert EA, Straznicky N, et al. Sympathetic activation in chronic renal failure. J Am Soc Nephrol. 2009;20(5):933–939. doi: 10.1681/ASN.2008040402. [DOI] [PubMed] [Google Scholar]
- 9.Demuth K, Blacher J, Guerin AP, Benoit MO, Moatti N, Safar ME, et al. Endothelin and cardiovascular remodelling in end-stage renal disease. Nephrol Dial Transplant. 1998;13(2):375–383. doi: 10.1093/oxfordjournals.ndt.a027833. [DOI] [PubMed] [Google Scholar]
- 10.Inoue A, Yanagisawa M, Kimura S, Kasuya Y, Miyauchi T, Goto K, et al. The human endothelin family: three structurally and pharmacologically distinct isopeptides predicted by three separate genes. Proc Natl Acad Sci U S A. 1989;86(8):2863–2867. doi: 10.1073/pnas.86.8.2863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Schiffrin EL, Thibault G. Plasma endothelin in human essential hypertension. Am J Hypertens. 1991;4(4 Pt 1):303–308. doi: 10.1093/ajh/4.4.303. [DOI] [PubMed] [Google Scholar]
- 12.Fukuchi M, Giaid A. Endothelial expression of endothelial nitric oxide synthase and endothelin-1 in human coronary artery disease. Specific reference to underlying lesion. Lab Investig. 1999;79(6):659–670. [PubMed] [Google Scholar]
- 13.Minami S, Yamano S, Yamamoto Y, Sasaki R, Nakashima T, Takaoka M, et al. Associations of plasma endothelin concentration with carotid atherosclerosis and asymptomatic cerebrovascular lesions in patients with essential hypertension. Hypertens Res. 2001;24(6):663–670. doi: 10.1291/hypres.24.663. [DOI] [PubMed] [Google Scholar]
- 14.Cacioppo JA, Oh SW, Kim HY, Cho J, Lin PC, Yanagisawa M, et al. Loss of function of endothelin-2 leads to reduced ovulation and CL formation. PLoS One. 2014;9(4):e96115. doi: 10.1371/journal.pone.0096115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Grimshaw MJ, Hagemann T, Ayhan A, Gillett CE, Binder C, Balkwill FR. A role for endothelin-2 and its receptors in breast tumor cell invasion. Cancer Res. 2004;64(7):2461–2468. doi: 10.1158/0008-5472.CAN-03-1069. [DOI] [PubMed] [Google Scholar]
- 16.Matsumoto H, Suzuki N, Onda H, Fujino M. Abundance of endothelin-3 in rat intestine, pituitary gland and brain. Biochem Biophys Res Commun. 1989;164(1):74–80. doi: 10.1016/0006-291X(89)91684-7. [DOI] [PubMed] [Google Scholar]
- 17.Keller BJ, Martini S, Sedor JR, Kretzler M. A systems view of genetics in chronic kidney disease. Kidney Int. 2012;81(1):14–21. doi: 10.1038/ki.2011.359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Diribarne G, Bensaude O. 7SK RNA, a non-coding RNA regulating P-TEFb, a general transcription factor. RNA Biol. 2009;6(2):122–128. doi: 10.4161/rna.6.2.8115. [DOI] [PubMed] [Google Scholar]
- 19.Peterlin BM, Price DH. Controlling the elongation phase of transcription with P-TEFb. Mol Cell. 2006;23(3):297–305. doi: 10.1016/j.molcel.2006.06.014. [DOI] [PubMed] [Google Scholar]
- 20.Sano M, Schneider MD. Cyclin-dependent kinase-9: an RNAPII kinase at the nexus of cardiac growth and death cascades. Circ Res. 2004;95(9):867–876. doi: 10.1161/01.RES.0000146675.88354.04. [DOI] [PubMed] [Google Scholar]
- 21.Liao HS, Kang PM, Nagashima H, Yamasaki N, Usheva A, Ding B, et al. Cardiac-specific overexpression of cyclin-dependent kinase 2 increases smaller mononuclear cardiomyocytes. Circ Res. 2001;88(4):443–450. doi: 10.1161/01.RES.88.4.443. [DOI] [PubMed] [Google Scholar]
- 22.Dhaun N, Goddard J, Webb DJ. The endothelin system and its antagonism in chronic kidney disease. J Am Soc Nephrol. 2006;17(4):943–955. doi: 10.1681/ASN.2005121256. [DOI] [PubMed] [Google Scholar]
- 23.Widlansky ME, Gokce N, Keaney JF, Jr, Vita JA. The clinical implications of endothelial dysfunction. J Am Coll Cardiol. 2003;42(7):1149–1160. doi: 10.1016/S0735-1097(03)00994-X. [DOI] [PubMed] [Google Scholar]
- 24.Ganz P, Vita JA. Testing endothelial vasomotor function: nitric oxide, a multipotent molecule. Circulation. 2003;108(17):2049–2053. doi: 10.1161/01.CIR.0000089507.19675.F9. [DOI] [PubMed] [Google Scholar]
- 25.Lonsdale J, Thomas J, Salvatore M, Phillips R, Lo E, Shad S, et al. The Genotype-Tissue Expression (GTEx) project. Nat Genet. 2013;45(6):580–5. Epub 2013/05/30 [DOI] [PMC free article] [PubMed]
- 26.Vargas-Alarcon G, Vallejo M, Posadas-Romero C, Juarez-Rojas JG, Martinez-Rios MA, Pena-Duque MA, et al. The -974C>A (rs3087459) gene polymorphism in the endothelin gene (EDN1) is associated with risk of developing acute coronary syndrome in Mexican patients. Gene. 2014;542(2):258–262. doi: 10.1016/j.gene.2013.09.003. [DOI] [PubMed] [Google Scholar]
- 27.Castro MG, Rodriguez-Pascual F, Magan-Marchal N, Reguero JR, Alonso-Montes C, Moris C, et al. Screening of the endothelin1 gene (EDN1) in a cohort of patients with essential left ventricular hypertrophy. Ann Hum Genet. 2007;71(Pt 5):601–610. doi: 10.1111/j.1469-1809.2007.00351.x. [DOI] [PubMed] [Google Scholar]
- 28.Palacin M, Rodriguez-Pascual F, Reguero JR, Rodriguez I, Avanzas P, Lozano I, et al. Lack of association between endothelin-1 gene variants and myocardial infarction. J Atheroscler Thromb. 2009;16(4):388–395. doi: 10.5551/jat.No1149. [DOI] [PubMed] [Google Scholar]
- 29.Rankinen T, Church T, Rice T, Markward N, Leon AS, Rao DC, et al. Effect of endothelin 1 genotype on blood pressure is dependent on physical activity or fitness levels. Hypertension. 2007;50(6):1120–1125. doi: 10.1161/HYPERTENSIONAHA.107.093609. [DOI] [PubMed] [Google Scholar]
- 30.Zhang L, Sui R. Effect of SNP polymorphisms of EDN1, EDNRA, and EDNRB gene on ischemic stroke. Cell Biochem Biophys. 2014;70(1):233–239. doi: 10.1007/s12013-014-9887-6. [DOI] [PubMed] [Google Scholar]
- 31.McCullough PA, Sandberg KR, Dumler F, Yanez JE. Determinants of coronary vascular calcification in patients with chronic kidney disease and end-stage renal disease: a systematic review. Journal of nephrology. 2004;17(2):205–215. [PubMed] [Google Scholar]
- 32.Rosas SE, Mensah K, Weinstein RB, Bellamy SL, Rader DJ. Coronary artery calcification in renal transplant recipients. Am J Transplant. 2005;5(8):1942–1947. doi: 10.1111/j.1600-6143.2005.00955.x. [DOI] [PubMed] [Google Scholar]
- 33.2012 USRDS, annual data report (ADR). https://www.usrds.org/atlas12.aspx
- 34.Yang WC, Hwang SJ. Incidence, prevalence and mortality trends of dialysis end-stage renal disease in Taiwan from 1990 to 2001: the impact of national health insurance. Nephrol Dial Transplant. 2008;23(12):3977–3982. doi: 10.1093/ndt/gfn406. [DOI] [PubMed] [Google Scholar]
- 35.D'Agostino RB, Sr, Grundy S, Sullivan LM, Wilson P. Validation of the Framingham coronary heart disease prediction scores: results of a multiple ethnic groups investigation. JAMA. 2001;286(2):180–187. doi: 10.1001/jama.286.2.180. [DOI] [PubMed] [Google Scholar]
- 36.Wilson PW, D'Agostino RB, Levy D, Belanger AM, Silbershatz H, Kannel WB. Prediction of coronary heart disease using risk factor categories. Circulation. 1998;97(18):1837–1847. doi: 10.1161/01.CIR.97.18.1837. [DOI] [PubMed] [Google Scholar]
- 37.Kalantar-Zadeh K, Ikizler TA, Block G, Avram MM, Kopple JD. Malnutrition-inflammation complex syndrome in dialysis patients: causes and consequences. Am J Kidney Dis. 2003;42(5):864–881. doi: 10.1016/j.ajkd.2003.07.016. [DOI] [PubMed] [Google Scholar]
- 38.Cefalu WT. Inflammation, insulin resistance, and type 2 diabetes: back to the future? Diabetes. 2009;58(2):307–308. doi: 10.2337/db08-1656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Chang YT, Wu JL, Hsu CC, Wang JD, Sung JM. Diabetes and end-stage renal disease synergistically contribute to increased incidence of cardiovascular events: a nationwide follow-up study during 1998-2009. Diabetes Care. 2014;37(1):277–285. doi: 10.2337/dc13-0781. [DOI] [PubMed] [Google Scholar]
- 40.Slinin Y, Foley RN, Collins AJ. Calcium, phosphorus, parathyroid hormone, and cardiovascular disease in hemodialysis patients: the USRDS waves 1, 3, and 4 study. J Am Soc Nephrol. 2005;16(6):1788–1793. doi: 10.1681/ASN.2004040275. [DOI] [PubMed] [Google Scholar]
- 41.Tentori F, Blayney MJ, Albert JM, Gillespie BW, Kerr PG, Bommer J, et al. Mortality risk for dialysis patients with different levels of serum calcium, phosphorus, and PTH: the Dialysis Outcomes and Practice Patterns Study (DOPPS) Am J Kidney Dis. 2008;52(3):519–530. doi: 10.1053/j.ajkd.2008.03.020. [DOI] [PubMed] [Google Scholar]
- 42.Kimata N, Albert JM, Akiba T, Yamazaki S, Kawaguchi T, Fukuhara S, et al. Association of mineral metabolism factors with all-cause and cardiovascular mortality in hemodialysis patients: the Japan dialysis outcomes and practice patterns study. Hemodial Int. 2007;11(3):340–348. doi: 10.1111/j.1542-4758.2007.00190.x. [DOI] [PubMed] [Google Scholar]
- 43.Palmer SC, Hayen A, Macaskill P, Pellegrini F, Craig JC, Elder GJ, et al. Serum levels of phosphorus, parathyroid hormone, and calcium and risks of death and cardiovascular disease in individuals with chronic kidney disease: a systematic review and meta-analysis. JAMA. 2011;305(11):1119–1127. doi: 10.1001/jama.2011.308. [DOI] [PubMed] [Google Scholar]
- 44.Chiavistelli S, Giustina A, Mazziotti G. Parathyroid hormone pulsatility: physiological and clinical aspects. Bone research. 2015;3:14049. doi: 10.1038/boneres.2014.49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Duric PS, Duric Z, Jankovic A, Tosic J, Popovic J, Dimkovic N. Influence of hemodialysis duration per week on parameters of dialysis adequacy and cardiovascular morbidity. Med Pregl. 2014;67(11–12):385–391. doi: 10.2298/MPNS1412385D. [DOI] [PubMed] [Google Scholar]
- 46.Chertow GM, Levin NW, Beck GJ, Depner TA, Eggers PW, Gassman JJ, et al. In-center hemodialysis six times per week versus three times per week. N Engl J Med. 2010;363(24):2287–2300. doi: 10.1056/NEJMoa1001593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Zoccali C, Mallamaci F, Tripepi G. Novel cardiovascular risk factors in end-stage renal disease. J Am Soc Nephrol. 2004;15(Suppl 1):S77–S80. doi: 10.1097/01.ASN.0000093240.84097.FE. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data related to this article are shown in the manuscript or available upon request from the corresponding authors.


