Abstract
Background:
Medical errors are the main concerns in health systems, which considering their ascending rate in the recent years, especially in the field of midwifery, have caused a medical crisis. Considering the importance of evidence-based health services as a way to improve health systems, the aim of this study was to suggest a guideline for preventing malpractice in midwifery services.
Materials and Methods:
In this cross-sectional study that was conducted in 2013, we investigated 206 cases that were referred to the Isfahan Legal Medicine Organization and Medical Council of Forensic Medicine from 2006–2011. Data were collected by a checklist and were analyzed using SPSS-16 software. Descriptive statistical tests (mean, maximum, minimum, standard deviation, frequency, and percentage agreement) were used to describe the data. Then, we used the Delphi technique with the participation from 17 experts in midwifery, gynecology, and legal medicine to provide an evidence-based draft guideline for prevention of midwifery errors.
Results:
A total of 206 cases were reviewed. In 66 cases (32%) the verdict for malpractice in midwifery services was approved. A practical draft guideline for preventing clinical errors for midwifery in the fields of pregnancy, delivery, and postpartum period was developed.
Conclusions:
This evidence-based draft guideline can improve the attention of all the healthcare providers, especially midwives and physicians to prevent urgent problems and offer effective health services for mothers and infants.
Keywords: Complaint, guideline, Iran, malpractices, medical council, midwifery
Introduction
Medical errors are the main concerns in health systems, which considering their ascending rate in the recent years, especially in the midwifery field, have caused a medical crisis. Unique position of midwifery is the result of its great responsibility and the wide area that it covers in the health services. Midwives must be responsible for all their actions.[1] They start the treatment and care as a team and work with various specialists. In fact, this team work, in which midwives should depend on other colleagues, could cause more job responsibilities and in some cases would lead to malpractice lawsuits that may get involved the obstetricians or even anesthesiologists other than midwives. Hence, midwives would deserve commendation for fulfilling this great responsibility correctly and at the same time failure to comply the patient rights or performing illegal activities, would cause violation in the treatment process that in most cases would lead to complaints from patients.[2] The main reason of patient's complaints is not imperfect treatment; the increase in insurance coverage, patients' awareness of their rights, and lack of clear communication between gynecologists, midwives, and patients are usually the main reasons of these complaints.[3] During the recent years, high rate of patients' complaints have caused a medical crisis.[4] Legal action against gynecologists and midwives often had been a considerable concern and these specialists have paid the highest amount of compensation.[5] International reports have indicated an increase in complaints against physicians in different countries in spite of scientific progress and new diagnostic and therapeutic technologies.[3] Also, a research in Iran represented an accretion in cases referred to the Isfahan Medical Council of Forensic Medicine from 62 in 2005 to 108 in 2009. In this study, most of the complaints were against general practitioners, anesthesiologists, obstetricians and gynecologists, general surgeons, orthopedics, and nurses.[3] In Australia, midwives and gynecologists (about 2% of the medical and paramedics population) pay the highest premium for professional liability insurance (18%).[6]
Nowadays, the importance of evidence-based health services as a way to improve health systems has been noticed. In 1996, David Sackett and colleagues clarified the definition of this tributary of evidence-based medicine as “the conscientious, explicit, and judicious use of current best evidence in making decisions about the care of individual patients. It means integrating individual clinical expertise with the best available external clinical evidence from systematic research”.[7] Evidence-based medicine can help midwives to make better decisions and to improve their patient care.[7,8]
In fact, evidence-based medicine is an effort to use the results of scientific methods, especially in evaluating the evidence for advantages and disadvantages of healthcare. The evidence-based protocols can provide same medical services at different places and conditions for similar patients.[7] Therefore; we have tried to suggest a guideline to prevent malpractice in midwifery services as we investigated all midwifery cases that were referred to the Isfahan Legal Medicine Organization and Medical Council of Forensic Medicine from 2006 to 2011.
Materials and Methods
In this cross-sectional study, data were collected from 206 midwifery cases that referred to the Iranian Forensic Medicine Organization (IFMO) and forensic medicine commission (FMC) of Isfahan that had the required inclusion criteria. These criteria were being referred to the Isfahan IFMO and FMC from 2006–2011 and having at least one warrant issued by the outcome of the disciplinary board. In 2013, the researchers reviewed all the cases related to midwifery services that were referred to these two organizations from April 2006 to April 2011 for 8 months. Data collection was conducted by a checklist designed based on the variables under consideration such as the presence or absence of malpractice, maternal and fetal complications leading to midwifery errors, and the given verdict. Validity of checklist was confirmed by ten experts in the field of midwifery and five experts in the field of medico legal. In this study, we used the census sampling methods.
After collecting the data, the researchers categorized the midwives' and obstetricians' malpractices in the domains of prenatal care, delivery, and postpartum period care and investigated the association between these malpractices and the research variables with the help of a research counselor who was an expert of forensic medicine and a member of forensic medicine commission. Data were analyzed using SPSS-16 software; descriptive statistical tests (mean, maximum, minimum, standard deviation, frequency, and percentage agreement) were used to describe the data.
Then, a draft on common malpractice in midwifery in three domains (midwives' and obstetricians' malpractices in the domains of prenatal care, delivery, and postpartum period care) was written. Later, we used the Delphi technique with the participation of nine experts in the field of midwifery, five experts in obstetrics. and three experts in legal medicine and a practical draft guideline for preventing clinical errors of midwifery errors in the fields of prenatal care, delivery, and postpartum period was developed.
The groups of elected members from the midwifery professors, gynecologists, members of the FMC, and disciplinary board of the medical council separately discussed with each other to develop this guideline during three meetings. In the first meeting, the results of the study were reported and the first draft guideline was prepared and written. In the second session, after a conclusion and agreement between the views and opinions, the second version of the draft was adjusted, and then in the third sessions, at least, the final guideline was approved by the members. It must be noted that all the three meetings were held in all groups. Eventually data were analyzed using SPSS-16 software; descriptive statistical tests (mean, maximum, minimum, standard deviation, frequency, and percentage agreement) were used to describe the data.
Ethical considerations
The entire complainant's data and their profile and the names of the service providers who had been charged with malpractice were anonymous and were used only in the form of the research results.
Results
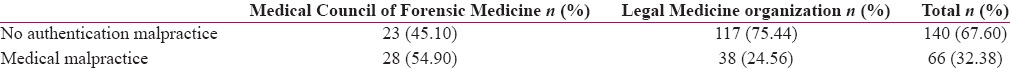
In total, 287 files from the Medical Council and 68 of the FMC were related to the field of midwifery during the studied period; of these only 206 files had the inclusion criteria and were finally reviewed and analyzed. Out of the 206 reviewed files, a total of 66 cases (32%) had at least one warrant issued by the outcome of the disciplinary board) 38 cases in FMC and 28 cases in the Medical Council of Forensic Medicine) [Table I]. Therefore, a practical draft guideline for preventing clinical errors of midwifery in the fields of prenatal care, delivery, and the postpartum period was developed as follows:
Table 1.
Frequency of medical malpractice in Isfahan Iranian Legal Medicine organization and Medical Council of Forensic Medicine (2006-2011)
Proposed guidelines for improving prenatal care
According to the state protocol, integrated into maternal health care during pregnancy, the first ultrasonography is recommended during 16–18 pregnancy weeks. This has led to undiagnosed cases of obstetric complications such as ectopic pregnancy and molar pregnancy and has made pregnant mothers encounter critical issues. Ultrasonography at the first trimester (preferably between 8–11 weeks), in addition to early detection of these complications, can also be an accurate estimate of gestational age
Given the importance of early diagnosis of fetal malformations, screening of trisomy by biochemical tests and ultrasound in high-risk pregnancies in the first trimester is necessary. The high-risk mothers included those who have family marriage, mother's age of more than 35-years-old, history of recurrent abortion or intrauterine fetal death, history of child labor with congenital deformities or chromosomal abnormalities, and familial history of malformations or chromosomal abnormalities in each couple
Due to the high incidence of preeclampsia and other underlying diseases in pregnant women, training them to recognize danger signs during pregnancy and postpartum period following these disorders is recommended. In this regard, it is necessary to make sure that the necessary sensitivity has been created in mothers and their families. However, it is recommended that the risk signs training form would be attached to the mothers' medical records and at any meeting, after receiving the relevant education, women would verify them
Also, due to coagulation disorders followed by missed abortion or intrauterine fetal death in the first trimester and early second trimester, symptoms such as sudden loss of pregnancy symptoms are particularly important. Because during these gestational ages, fetal movements cannot be detected by the mothers and based on the maternal healthcare national protocol, maternity care intervals are long
Considering the numerous cases of mothers' death or disability following delayed admission or early hospital discharge by patient's relatives due to lack of their awareness or responsibility, it is recommended that husbands of pregnant women would attend training sessions that are held by gynecologists and midwives during pregnancy; so they can play a responsible role during pregnancy and delivery
According to the increasing prevalence of abnormal placenta attachment and its complications because of the high incidence of cesarean sections, we recommend Doppler ultrasound in repeated cesarean sections (especially the third pregnancy) or the presence of placenta previa from the previous cesarean sections to confirm or rule out any abnormal placental adhesion
It is recommended that the obstetricians will introduce the high-risk women to a tertiary referral hospital at the beginning of maternity care. It is also suggested that specialized healthcare teams would be created in these hospitals for taking necessary measures for these mothers. This would result in on-time reference and avoid waste of time for referring to the appropriate specialized services of these mothers.
Proposed guidelines for improving delivery time services
Due to the high prevalence of Erb's palsy among neonates, it is suggested to conduct proper prenatal care (especially for controlling blood sugar), consult an endocrinologist for diabetic mothers, and include consultation form in their pregnancy files. It could prevent fetal macrosomia or possibly predict macrosomia before birth for conducting timely cesarean section to reduce the shoulder dystocia and Erb's palsy
Since external force to the abdomen can cause many complications such as the uterus or other abdominal viscera ruptures, therefore close monitoring during delivery time and special measures to prevent this action is recommended
Due to numerous reports on fetal distress following incorrect induction, correct, timely, and in accordance induction according to the medical indications with a written order from gynecologist and her/his direct supervision are recommended. In this regard, documents' registrations are necessary as an induction form for recording the intensity and frequency of uterine contractions and fetal heart (continuous monitoring) on mother's bedside while providing care
Delay in performing cesarean section may result in several deaths or injuries in fetus and numerous cases of death or disability in mothers during labor, so continuing the labor while vaginal delivery is not possible or has lingered is not indicated and it is recommended to perform emergency cesarean section without wasting time to save the mother and infant's lives
According to numerous reports of serious injury or death due to non-systematic use of forceps or vacuum, the vacuum and forceps training courses for obstetricians is recommended. Also, it should be noted that detailed examination of the vagina, cervix, and fornix under direct light and with perfect vision for checking the presence of rupture after use of these devices is necessary
According to numerous reports on delays in making the decision to terminate pregnancy in mothers with underlying diseases by gynecologists, gynecologists' training needs to pay more attention to consultation with specialists of internal diseases for early termination pregnancy in these cases
Following the risk of uterus atony, and therefore, maternal death or hysterectomy, the proper management of labor such as lack of long-term induction is essential in the perinatal care. Also, use of vasoconstrictors, bimanual massage (instead of a manual massage), and blood and body fluids correction under the supervision of internal specialist or anesthesiologist is recommended
Since lack of proper administration of serums especially in patients with heart diseases, severe preeclampsia, and chronic hypertension can cause cardiopulmonary disorders, it is recommended that the patient would immediately be advised by the internists and anesthesiologists
To prevent intestinal obstruction or paralysis following caesarean section, it is recommended to provide proper medical care including the reliability of defecation in patients before discharge. Also, it is recommended that, in the postpartum checkup forms, the “defecation” item would be added
Considering that delays in emergency hysterectomy leads to death or severe complications in some pregnant women, it is recommended that emergency cesarean section or hysterectomy would be conducted without the consent from their spouses or other relatives to prevent any waste of time for obtaining consent
Getting an exact medical history and examination on mothers' admission time and also attaching older medical files of the patients to the new records is recommended
Creating a forensic unit in all treatment centers for obtaining patients' informed consent, monitoring patients' death (death within 24 hours), transferring the corpses, if necessary, and prevention of complaints without evidence against medical staffs is recommended
To provide proper care for mothers, it is suggested to enlist expert midwives instead of the nursing staff in the recovery room and obstetrics and gynecology wards
Physiological changes resulting from pregnancy could make any surgery risky for the patient. It is recommended that all the anesthesia care in pregnant women would be performed only by anesthesiologists, not technicians
Discharge of high-risk pregnant women with a personal or family consent before completing the diagnostic and therapeutic process is dangerous. It is also recommended that the necessary arrangements would be done to monitor the mothers' situation until the end of the postpartum period with a maternal health center
Accurate documentation of all the treatment process is necessary. It is recommended that all the staff and physicians will be trained for recording and documenting of all the events accurately and honestly (even medical errors) and the Clinical Governance Office in hospital should be controlling these records, frequently.
Proposed guidelines for improving care after delivery
Duo to the importance of physical examination, observation of nursing and paraclinic reports as well as postpartum training by a physician it is recommended that mothers would not be discharged through physician's telephone order
Exact medical history taking and examinations for detecting obstetric complications such as thrombosis, breast problems (mastitis, congestion, ulcers, or fissures), episiotomy-related complications(infection, fistula), vaginal bleeding, and abdominal tenderness are recommended during the postpartum period.
Discussion
After investigating all the midwifery cases that were referred to the Isfahan Iranian Forensic Medicine Organization (IFMO) and forensic medicine commission (FMC) from 2006–2011 that had at least one warrant issued by the outcome of the disciplinary board in a cross-sectional study and using the Delphi technique with experts in the field of midwifery, a practical draft guideline for preventing clinical errors of midwifery in the fields of pregnancy, delivery, and postpartum period was developed. The results of this review showed the records of maternal and fetal death or disability due to obvious preventable medical errors by service providers. It seems that clinical guidelines based on the type of medical malpractice can control or reduce the incidence of fraud in the scope of midwifery.
Pregnancy items in this guideline include an ultrasound control suggestion during the first trimester of pregnancy, early diagnosis of fetal malformations in high-risk pregnancies, training the warning signs to pregnant women, and allowing the patients' spouses to visit the physician's office. Several studies emphasized on the need for developing a guideline and its role in improving prenatal healthcare.[9–15] The creation of evidence-based clinical guidelines can prevent a large number of medical errors that are repeated daily and promote the services to patients.[10] Bruguera et al. also reported that compliance with evidence-based clinical guidelines can make a more solid legal defense and prevent inconsistencies in their condemnation. They also recommended that possible side effects of treatments and provided services should be explained to the patients based on clinical guidelines.[11] The most important item in the field of pregnancy care of the proposed draft gridline is about early diagnosis of fetal malformation in pregnancy and the necessity of screening by biochemical tests and ultrasound in high risk pregnancies during the first trimester. Several studies emphasized on this issue in their research such as Halder et al (2016) that recommended to perform diagnostic tests during the first trimester of pregnancy (especially in high risk women). Also they stated that, when a major malformation is identified in pregnancy, parents should be referred to a tertiary ultrasound unit for repeated assessment and attempt to detect other anomalies, and if required then should be offered all other imaging techniques such as fetal echocardiography, ultrafast fetal MRI, etc. Every parental and fetal testing should be ensured for prenatal diagnosis, even if it involves invasive procedures (chromosomal, specific molecular, etc).[12]
Delivery items are proper induction of labor, preventing delayed decision-making and proper use of forceps and vacuum. In a study about challenges for the adoption of evidence-based maternity care, it was identified that social pressure for complying with recommended practices by supervisors and peers, as well as the belief that our resources are limited would affect maternity care providers and opportunities to perform evidence-based procedures. An underlying problem was failure in involving women in decision-making regarding their own maternity care. In addition to informing providers about the evidence, it seems necessary to develop standard protocols, improve physical conditions, and implement behavioral interventions that take into account provider attitudes, social pressures, and beliefs.[13] Ngongo et al. expressed that the labor centers must be managed with explicit clinical decision-making guidelines to promote the staffs' accountability.[15] The most important items in the field of delivery care in the proposed draft gridline is about correct, timely, and in accordance induction according to the medical indications with a written order from gynecologist and her/his direct supervision. Selecting appropriate candidates and long waits for labor to progress into the active phase would make an impact on decreasing the national caesarean section delivery rate.[16] Also in a research about “Labor Induction” it was expressed that medical staff education and the development and enforcement of induction guidelines were contributed to a decrease in inappropriate inductions, a lower caesarean section birth rate for electively induced nulliparas, and a lower elective and overall induction rate.[17] Postpartum period's item is not accepting telephone order from physicians for mothers discharge. Before discharge, mothers should be examined by their gynecologist. Professionals and health services managers have a crucial role in producing the best quality obstetric and neonatal care through implementing the listed evidence-based interventions and make them accessible to all pregnant women and their newborns without delay, even in poor settings. Reasons for which progress is slow should be addressed. One of these reasons is lack of access to scientific knowledge on professionals' part in developing countries. Hereby, we would provide the key references and also websites which are freely accessible through the Internet.[14] Henry et al. in their study about “Decision-Making for Postpartum Discharge” expressed that mothers, pediatricians, and obstetricians must make decisions about postpartum discharge jointly, because perceptions of unpreparedness often differ. Sensitivity toward specific maternal vulnerabilities and an emphasis on perinatal education to insure individualized discharge plans may increase readiness and determine optimal timing for discharge and follow-up care.[18] Nipte et al. mentioned that there is an urgent need to create awareness regarding a minimum period of stay of 48 hours in the hospital after delivery among various stakeholders, especially in young mothers delivering in Governmental hospitals. Standard protocols must be followed by healthcare workers regarding adherence to this recommendation. There should be a uniform practice regarding discharge of mothers after delivery across various healthcare facilities. This might help to improve the maternal and fetal outcomes.[19]
The limitation of this research was different experts'opinions and the method of surveying the malpractice claim in the two organizations.
Conclusion
All the recommendations that were contained in the guideline may not reflect the opinion of all reviewers. This issue after identifying the types of malpractice suggests integrated methods to deal with infractions and improve deficiencies. It can also improve the attention of all the healthcare providers especially midwives and physicians to prevent urgent problems and offer effective health services for mothers and infants.
Financial support and sponsorship
Department of Midwifery in Isfahan University of Medical Sciences.
Conflicts of interest
There are no conflicts of interest.
Acknowledgement
This article was derived from a master thesis of Leila Asadi with project number 392257, Isfahan University of Medical Sciences, Isfahan, Iran.
References
- 1.Fraser D, Cooper A, Myles F. Myles' Textbook for Midwives. 15th ed. Edinburgh; New York: Churchill Livingstone English; 2014. p. 7. [Google Scholar]
- 2.Jafarian A, Parsapour A, Yalda AR, Haj-Tarkhani AH, Asghari F, Emami Razavi SH. A Survey of the Complaints Entering the Medical Council Organization of Tehran in Three Time Periods. J Med Ethics Hist Med. 2009;2:9. [PMC free article] [PubMed] [Google Scholar]
- 3.Mahmoodabadi HB, Setareh M, Nejadnick M, Niknamian M, Ayoobian A. The frequency and reasons of medical errors in cases referred to Isfahan Legal Medicine Center. Health Info Manag. 2012;9:101–9. [Google Scholar]
- 4.Haghshenas MR, Vahidshahi K, Amiri A, Rezaee M, Rahmani N, Pourhossen M, et al. Study the frequency of malpractice lawsuits referred to forensic medicine department and medical council, Sari, 2006-2011. Journal of Mazandaran University of Medical Sciences. 2012;21:253–60. [Google Scholar]
- 5.Mertens R, Wrigley J. The Role of the Legal Nurse Consultant in Brachial Plexus Injury: A Case Study. Newborn and Infant Nursing Reviews. 2010;10:138–42. [Google Scholar]
- 6.Johnson AL, Jung L, Song Y, Brown KC, Weaver MT, Richards KC. Sleep Deprivation and Error in Nurses who Work the Night Shift. J Nurs Adm. 2014;44:17–22. doi: 10.1097/NNA.0000000000000016. [DOI] [PubMed] [Google Scholar]
- 7.Sackett DL, Rosenberg WM, Gray JA, Haynes RB, Richardson WS. “Evidence based medicine: What it is and what it isn't”. BMJ. 1996;312:71–2. doi: 10.1136/bmj.312.7023.71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mostafazadeh F. Benefits application of evidence based care in midwifery education. Journal of Obstetrics and Gynecology. 2011;6:26–32. [Google Scholar]
- 9.Lamei A. evidence- based medicin. 1st ed. Tehran: Ministry of health and education of Iran pub; 2011. pp. 6–8. [Google Scholar]
- 10.Grando A, Peleg M, Glasspool D. A goal-oriented framework for specifying clinical guidelines and handling medical errors. J Biomed Inform. 2010;43:287–99. doi: 10.1016/j.jbi.2009.11.006. [DOI] [PubMed] [Google Scholar]
- 11.Bruguera M, Arimany J, Bruguera R, Barberia E, Ferrer F, Sala J, et al. Guideline to prevent claims due to medical malpractice, on how to act when they do occur and how to defend oneself through the courts. Rev Clin Esp. 2012;212:198–205. doi: 10.1016/j.rce.2011.12.018. [DOI] [PubMed] [Google Scholar]
- 12.Halder A. Approach to Prenatal Fetal Malformations. EC Gynecology. 2016;3:294–307. [Google Scholar]
- 13.Turan JM, Bulut A, Nalbant H, Ortayli N, Erbaydar T. Challenges for the adoption of evidence-based maternity care in Turkey. Soc Sci Med. 2006;62:2196–204. doi: 10.1016/j.socscimed.2005.10.005. [DOI] [PubMed] [Google Scholar]
- 14.Fauveau V, de Bernis. L. “Good obstetrics” revisited: Too many evidence-based practices and devices are not used. Int J Gyanecol Obstet. 2006;94:179–84. doi: 10.1016/j.ijgo.2006.05.020. [DOI] [PubMed] [Google Scholar]
- 15.Ngongo C, Christie K, Holden J, Ford C, Pett C. Striving for excellence: Nurturing midwives' skills in Freetown, Sierra Leone. Midwifery. 2013;29:1230–4. doi: 10.1016/j.midw.2013.01.013. [DOI] [PubMed] [Google Scholar]
- 16.Laughon SK, Zhang J, Grewal J, Sundaram R, Beaver J, Reddy UM. Induction of labor in a contemporary obstetric cohort. Am J Obstet Gyanecol. 2012;206:486. doi: 10.1016/j.ajog.2012.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fisch JM, English D, Pedaline S, Brooks K, Simhan NH. Labor Induction Process Improvement: A Patient Quality-of-Care Initiative. Obstet Gynecol. 2009;113:797–803. doi: 10.1097/AOG.0b013e31819c9e3d. [DOI] [PubMed] [Google Scholar]
- 18.Bernstein HH, Spino C, Finch S, Wasserman R, Slora E, Lalama C, et al. Decision-Making for Postpartum Discharge of 4300 Mothers and Their Healthy Infants: The Life around Newborn Discharge Study. Pediatrics. 2007;120:e391–400. doi: 10.1542/peds.2006-3389. [DOI] [PubMed] [Google Scholar]
- 19.Nipte D, Dhayarkar S, Pawar S, Venkatsubramanian S, Mehendale S. Determinants of early discharge of mothers from hospitals after delivery in Beed block of Beed District, Maharashtra, India 2014. Clinical Epidemiology and Global Health. 2015;3:S26–33. [Google Scholar]


