Abstract
BACKGROUND
It is generally accepted that obesity puts patients at an increased risk for cardiovascular and respiratory complications after surgical procedures. However, in the setting of trauma, there have been mixed findings in regards to whether obesity increases the risk for additional complications.
OBJECTIVE
The aim of this study was to identify whether obese patients suffer an increased risk of cardiac and respiratory complications following traumatic injury.
METHODS
A retrospective analysis of 275,393 patients was conducted using the 2012 National Trauma Data Bank. Hierarchical regression modeling was performed to determine the probability of experiencing a cardiac or respiratory complication.
RESULTS
Patients with obesity were at a significantly higher risk of cardiac and respiratory complications compared to patients without obesity [OR:1.81; CI:1.72–1.91]. Prevalence of cardiovascular and respiratory complications for patients with obesity was 12.6% compared to 5.2% for non-obese patients.
CONCLUSIONS
Obesity is predictive of an increased risk for cardiovascular and respiratory complications following trauma.
Keywords: Obesity, complication, trauma, post-operative care
INTRODUCTION
Obesity rates have persistently increased in the United States over the last 20 years.1 Its prevalence has caused increased awareness regarding obesity’s pathophysiology and how it impacts other aspects of patients’ health. Today, nearly a third of the U.S. adult population meet the definition of obesity (body mass index > 30kg/m2) and, with that, has acquired an increased risk of developing additional comorbid conditions.1–2 Trauma is the third most prevalent cause of death in the United States and being in poor physical health can greatly increase mortality risk.3 Thus, obese trauma patients are a medically complex subset of patients with a potential for unforeseen complications, including periods of hypoxia, unplanned intubation, increased incidence of pulmonary hypertension, heart failure, and mortality.2–3
The surgical treatment of obese patients with traumatic injuries must assess both intra- and post-operative risks factors. As a patient’s BMI increases, their risk of developing a surgical complication increases as well.1–6 Obesity is associated with several respiratory abnormalities including hypercapnia and sleep apnea, as patients with obesity typically have an increased demand for ventilation.1–6 Other known obesity-related cardiovascular and respiratory comorbidities include atherosclerotic cardiovascular disease, heart failure, systemic and pulmonary hypertension, cardiac arrhythmias, deep vein thrombosis, and history of pulmonary embolism.1–6
Currently, literature examining how obesity affects health outcomes in trauma patients is generally limited to specific mechanisms of injury. Despite the growing concern for how to clinically manage patients with obesity, there are conflicting findings on how obesity impacts trauma outcomes.2–5 For example, a study utilizing the National Trauma Databank from 2007–2010 assessed the relationship between blunt trauma and outcomes for patients with morbid obesity and concluded that patients with BMI > 40k g/m2 were at an increased risk for in-hospital complications and mortality following blunt injury.9 In contrast, a study by Ferranda et. al concluded that obesity (BMI > 25k g/m2) was not a risk factor for mortality after traumatic injury of any mechanism, but patients with a higher BMI were at an increased risk for complications only following surgery.6
While it is generally accepted that obesity is associated with adverse outcomes for injured patients, this prompts further exploration.2–8 It is critical to examine the potential risk for complications in patients with an increased BMI in order to bring awareness and resources to the patient population at risk following traumatic injury. The aim of this study was to identify whether obesity is predictive of cardiovascular and respiratory complications following traumatic injury using a large national data source.
METHODS
Data Source
A retrospective study of all trauma patients ages 18–89 with an Injury Severity Score (ISS) of 9 or greater was performed using data from the 2012 National Trauma Databank (NTDB). Patients whose mechanism of injury was due to burn, drowning, poisoning, suffocation, overexertion, or natural/environmental causes were excluded. Patients who were transferred, discharged from the emergency department, died in the emergency department, or left against medical advice were also excluded. Patients treated at facilities that failed to report comorbidity status and complication status on 20% or more of cases were also excluded from the analysis. A study flow chart is provided in Figure 1.
Figure 1.
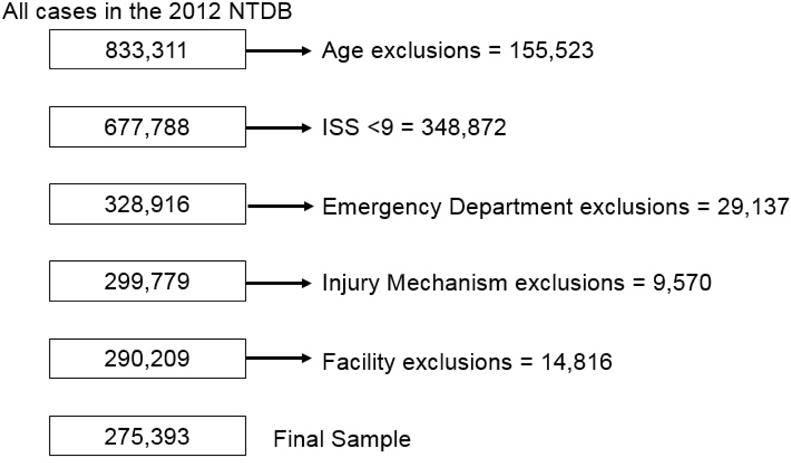
Study Sample Exclusions
Measures
The primary outcomes of interest were cardiovascular and respiratory complications. The complications examined included acute respiratory distress syndrome (ARDS), cardiac arrest, deep vein thrombosis (DVT), pulmonary embolism (PE), myocardial infarction (MI), and unplanned intubation. The independent variable of interest was obesity, which was defined by the NTDB as a BMI >30kg/m2 and included in the database’s comorbidity file. All complications and comorbidities were previously classified and coded by the NTDB. A detailed description of how complications and comorbidities are defined in the dataset is available in the 2012 National Trauma Data Bank User Manual, available publicly online (https://www.facs.org/~/media/files/quality%20programs/trauma/ntdb/ntdbmanual2012.ashx).
We also examined patient demographic and clinical data including age group (18–40, 41–60, 61–89), gender, ISS group (9–14, 15–24, 25 and higher), injury type (blunt, penetrating), Glasgow Coma Scale motor score (GCS) group (1–2, 3–4, 5–6), and whether or not the patient underwent a surgical procedure (procedure or no procedure). Comorbidity variables included alcoholism, ascites within 3 days of trauma, bleeding disorder, chemotherapy for cancer, congenital anomalies, congestive heart failure, smoking, cerebrovascular accident history, diabetes, disseminated cancer, advanced directive limiting care, esophageal varices, functionally dependent health status, history of angina within past month, history of myocardial infarction, history of peripheral vascular disease, hypertension requiring medication, impaired sensorium, prematurity, obesity (BMI ≥30kg/m2), respiratory disease, steroid use, cirrhosis, dementia, major psychiatric illness, drug abuse, prehospital cardiac arrest with CPR, and other. Comorbid conditions were grouped as: no comorbidities present, 1–2 comorbidities, 3–4 comorbidities, and ≥5 comorbidities. Diabetes and obesity were not included in the comorbidity count variable because they were analyzed independently.
Statistical Analysis
Descriptive analysis comparing characteristics between patients with obesity and patients without obesity were carried out using chi square, student’s T tests, and fisher’s exact tests. The prevalence of cardiovascular and respiratory complications in patients with obesity and patients without obesity was also calculated. Alpha was set at 0.05 and all statistical tests were two-sided.
A hierarchical regression model was used to model the probability of experiencing a cardiovascular or respiratory complication. The outcome variable in this model was a binary variable indicating whether or not the patient experienced ARDS, cardiac arrest, DVT, PE, MI, or unplanned intubation. The model controlled for age group, gender, ISS group, injury type, obesity, diabetes, comorbidity count, and GCS motor score. The hospital facility key was included as a random effect to account for clustering of patients within the same hospitals.
A second series of regression models were also ran to examine the effect of obesity on the likelihood of developing each individual cardiovascular or respiratory complications. In each of these models a single complication was used as the outcome variable. All models controlled for the same covariates as the previously described model. The SAS procedure GLIMMIX was used to carry out the hierarchical regression analyses. All statistical analysis was performed utilizing SAS 9.4 (SAS Institute Inc., Cary, NC).
RESULTS
Univariate Analyses
A total of 275,393 patients (obese: 14,210; not obese: 261,183) met the inclusion criteria for this study. There was a significant association between age, gender, mechanism of injury, GCS motor score, number of comorbidities, diabetes, and surgical procedure with obesity. Patients with obesity were more often female, older, and had a greater number of comorbidities including diabetes. Although statistically significant, there was a small absolute difference in the percentage of patients with penetrating injuries (7.42% non-obese, 5.36% obese; p<0.001) and low GCS motor score (GCS 1–2 non-obese 7.64%, obese 7.97%; p=0.024). (Table 1)
Table 1.
Descriptive Characteristics of Study Cohort
| Non-Obese (n=26,1183) | Obese (n=14,210) | p value | |
|---|---|---|---|
| Gender | <.0001 | ||
| Male | 63.05% | 55.95% | |
| Female | 36.95% | 44.05% | |
| Age | <.0001 | ||
| 18–40 | 31.99% | 23.97% | |
| 41–60 | 27.47% | 35.65% | |
| 61–89 | 40.55% | 40.38% | |
| Injury Type | <.0001 | ||
| Blunt | 92.58% | 94.64% | |
| Penetrating | 7.42% | 5.36% | |
| Injury Severity Score | 0.378 | ||
| 9–14 | 63.9% | 63.7% | |
| 15–24 | 22.8% | 22.6% | |
| 25 or Greater | 13.3% | 13.7% | |
| GCS Motor Score | 0.024 | ||
| 1–2 | 7.64% | 7.97% | |
| 3–4 | 1.99% | 1.69% | |
| 5–6 | 90.37% | 90.33% | |
| Surgical Procedure | 78.62% | 82.90% | <.0001 |
| Number of Comorbidities* | <.0001 | ||
| 0 | 43.67% | 28.16% | |
| 1–2 | 48.81% | 59.68% | |
| 3–4 | 6.95% | 11.15% | |
| 5+ | 0.56% | 1.01% | |
| Diabetes | 12.27% | 30.25% | <.0001 |
| Died | 4.9% | 5.1% | 0.178 |
Obesity and diabetes not included in the number of comorbidities. GCS Motor Score = Glasgow Coma Scale Motor Score
All of the cardiovascular and respiratory complications examined in this analysis were found to be significantly associated with obesity (all p<0.001). Prevalence of cardiovascular and respiratory complications for trauma patients with obesity was 12.6% as compared to 5.2% for patients without obesity. The percentage of patients with ARDS, cardiac arrest, DVT, PE, MI, and unplanned intubation were higher in the obesity group (Figure 2).
Figure 2.
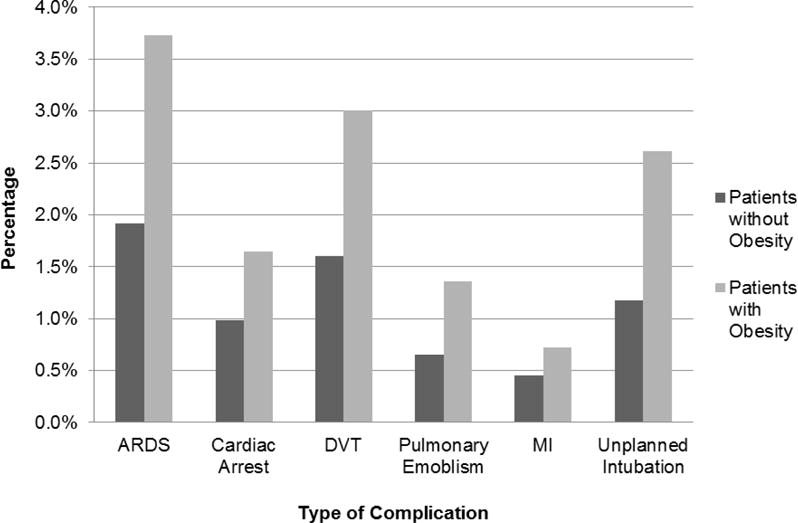
Percentage of cardiac and respiratory complications for persons with obesity versus without. ARDS = Acute Respiratory Distress Syndrome, DVT = Deep Vein Thrombosis, MI = Myocardial Infarction
Multivariable Analyses
Hierarchical regression model results demonstrated that patients with obesity were at a significantly higher risk of cardiac and respiratory complications as compared to patients without obesity. We found an approximately 80% greater risk of developing respiratory or cardiovascular complications in patients with obesity. Older adults also had a significantly increased risk of developing cardiac and respiratory compilations compared to adults aged 19–40. In particular, patients over 60 were 71% more likely to develop a cardiovascular or respiratory complication. Patients undergoing a surgical procedure were nearly five times as likely to experience cardiac and respiratory complications. Patients with comorbid conditions were also at a significantly increased risk for cardiac and respiratory complications compared to patients without comorbid conditions. Females were almost 30% less likely to develop cardiac and respiratory complications as compared with males. Blunt injuries were also associated with a 10% lower risk of respiratory and cardiac complications. (Table 2).
Table 2.
Predictors for Cardiovascular and Respiratory Complications
| Odds Ratio | Lower CL | Upper CL | |
|---|---|---|---|
| Obesity | |||
| No Obesity | Reference | ||
| Obesity | 1.81 | 1.72 | 1.91 |
| Gender | |||
| Female | Reference | ||
| Male | 0.71 | 0.69 | 0.73 |
| Age Group | |||
| 18–40 | Reference | ||
| 41–60 | 1.43 | 1.38 | 1.48 |
| 61–89 | 1.71 | 1.64 | 1.77 |
| Injury Severity Score | |||
| 9 to 14 | Reference | ||
| 15 to 24 | 2.48 | 2.40 | 2.57 |
| 25 and greater | 4.60 | 4.43 | 4.76 |
| Injury Type | |||
| Penetrating | Reference | ||
| Blunt | 0.90 | 0.85 | 0.94 |
| Diabetes Status | |||
| No Diabetes | Reference | ||
| Diabetes Status | 1.15 | 1.11 | 1.20 |
| Number of Other Comorbidities | |||
| None | Reference | ||
| 1 to 2 | 1.21 | 1.17 | 1.25 |
| 3 to 4 | 1.87 | 1.74 | 2.02 |
| 5 or greater | 2.01 | 1.28 | 3.17 |
| GCS Motor Score | |||
| 1 to 2 | Reference | ||
| 3 to 4 | 0.86 | 0.80 | 0.92 |
| 5 to 6 | 0.35 | 0.34 | 0.37 |
| Surgical Procedure | |||
| No Procedure | Reference | ||
| Surgical Procedure | 4.84 | 4.56 | 5.13 |
Obesity and diabetes not included in the number of comorbid conditions. GCS Motor Score = Glasgow Coma Scale Motor Score
Analyses of individual cardiac and respiratory complications showed that patients with obesity were at an 82% increased risk for ARDS, 69% increased risk for cardiac arrest, 83% increased risk for DVT, 63% increased risk for unplanned intubation, and over twice as likely to develop a pulmonary embolism (Table 3).
Table 3.
Adjusted Odds Ratios with 95% Confidence Intervals for Cardiovascular and Respiratory Complications Associated with Obesity
| Odds Ratio | Lower CL | Upper CL | |
|---|---|---|---|
| ARDS | 1.82 | 1.68 | 1.98 |
| Cardiac Arrest | 1.69 | 1.50 | 1.89 |
| DVT | 1.83 | 1.67 | 2.00 |
| Pulmonary Embolism | 2.09 | 1.84 | 2.37 |
| Unplanned Intubation | 1.63 | 1.48 | 1.81 |
Each model controlled for patient age, gender, ISS, mechanism of injury, GCS motor score, surgical procedure, number of comorbidities, and diabetes. ARDS = Acute Respiratory Distress Syndrome, DVT = Deep Vein Thrombosis
DISCUSSION
The growing prevalence of obesity has initiated more research in determining how best to care for patients with obesity following injury. Our results suggest that patients with obesity are at a significantly increased risk of experiencing cardiovascular and respiratory complications including ARDS, cardiac arrest, DVT, PE, and unplanned intubation after trauma. Several other studies have found that BMI influences post-operative cardiac and respiratory complications as excess body mass is known to cause changes in the cardiovascular system.13–19,21 Obesity is also a factor known to affect pulmonary physiology and consequently patients often experience reduced lung volume, which can result in pickwickian syndrome.8,13 Varon and Marik reported that obesity is known to cause changes in pulmonary function, including a total reduction in the respiratory system and increased airway resistance.13 Ditillo et al. reported that ARDS was one of the most common complications experienced by morbidly obese patients.9 Several studies have also reported that patients with obesity are at an increased risk for the occurrence of pulmonary complications following surgery.13–17 Rose et al. found that patients with obesity were twice as likely to experience acute postoperative respiratory events.18 Many of the adverse effects of obesity on post-surgical respiratory complications are likely exacerbated in the trauma setting due to their inability to physiologically compensate in response to their injury.8,13 Furthermore, obese blunt trauma patients may experience poorer survival outcomes due to their frequency of respiratory failure.13,19
With the increasing prevalence of obesity, the clinical implications of our findings stress the need for specialized treatment strategies for managing the obese trauma population. Studies examining factors that may affect outcomes for this patient population and minimize the risk of complications after surgical interventions are particularly needed. Our results indicate that obese patients are predisposed to complications associated with high mortality rates and that a need for additional surveillance and postoperative care may exist. Adequate care may include essential equipment, longer hospital stays and rehabilitation time, and need for increased staff.12 Often, patients with obesity must remain in the hospital rather than be transferred to a care facility due to the restraints of their BMI and the lack of appropriate facilities outside of a hospital. Thus, our study seeks to provide further insight into the complication risks of obese trauma patients and provide a foundation for further studies into their postoperative needs and care management.
Limitations
Limitations of this study arise from the use of national secondary data. Our study examined national trauma data that coded obesity as a comorbidity rather than listing a BMI, height, or weight. Furthermore, obesity, as indicated by the NTDB, was noted as a BMI greater than 30 kg/m2, which is inclusive of patients with morbid obesity. Therefore, our study was not able to assess the linearity of the relationship between BMI and risk of cardiopulmonary complications. Also, this analysis did not account for specific surgical site which could have implications on the type of complications experienced. Further analysis examining surgical site with respect to postoperative complications is warranted. We were also unable to determine how emergent the procedures performed on patients were, which would have provided some insight into patients’ risk of complication.
CONCLUSIONS
Our findings indicate that obesity is independently predictive of increased risk for cardiovascular and respiratory complications following trauma. Obesity was found to be a risk factor for cardiac arrest, acute respiratory distress syndrome, pulmonary embolism, deep vein thrombosis, and unplanned intubation following trauma. Obese trauma patients have an increased risk of complications that predispose them to need additional postoperative care, potentially including essential equipment, longer hospital stays and rehabilitation time, and increased staffing. This study hopes to provide further insight into the specific risks obese patients experience after trauma and provide a foundation for further studies into improving their inpatient care. Recently, hospitals have focused on preoperative conditioning as a means to reduce complications in the elective surgical population. However, future studies regarding specific interventions to prevent respiratory and cardiovascular complications in patients with obesity who require emergent care are needed.
Acknowledgments
This publication was made possible with support from Grant Numbers, KL2TR001106, and UL1TR001108 (A. Shekhar, PI) from the National Institutes of Health, National Center for Advancing Translational Sciences, Clinical and Translational Sciences Award, and with support from the John M. Templeton, Jr., MD Injury Prevention Research Scholarship from The Eastern Association for the Surgery of Trauma.
Footnotes
There was no conflict of interest for this study.
References
- 1.Poirier P, Alpert MA, Fleisher LA, Thompson PD, Sugerman HJ, Burke LE, Marceau P, Franklin BA. Cardiovascular Evaluation and Management of Severely Obese Patients Undergoing Surgery. Circulation. 2009;120:86–95. doi: 10.1161/CIRCULATIONAHA.109.192575. [DOI] [PubMed] [Google Scholar]
- 2.Brown CVR, Velmahos GC. The consequences of obesity on trauma, emergency surgery, and surgical critical care. World J Emerg Surg. 2006;1:27. doi: 10.1186/1749-7922-1-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Diaz JJ, Jr, Norris PR, Collier BR, Berkes MB, Ozdas A, May AK, Miller RS, Morris JA. Morbid obesity is not a risk factor for mortality in critically ill trauma patients. J Trauma. 2009;66(1):226–31. doi: 10.1097/TA.0b013e31815eb776. [DOI] [PubMed] [Google Scholar]
- 4.Wigfield CH, Lindsey JD, Muñoz A, Chopra PS, Edwards NM, Love RB. Is extreme obesity a risk factor for cardiac surgery? An analysis of patients with a BMI > or = 40. Eur J Cardiothorac Surg. 2006;29(4):434–40. doi: 10.1016/j.ejcts.2006.01.016. [DOI] [PubMed] [Google Scholar]
- 5.Dossett LA, Heffernan D, Lightfoot M, Collier B, Diaz JJ, Sawyer RG, et al. Obesity and pulmonary complications in critically injured adults. Chest. 2008;134(5):974–980. doi: 10.1378/chest.08-0079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ferrada P, Anand RJ, Malhotra A, Aboutanos M. Obesity Does Not Increase Mortality after Emergency Surgery. Journal of Obesity. 2014:1–3. doi: 10.1155/2014/492127. Article ID 492127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Choban PS, Weireter LJ, Jr, Maynes C. Obesity and increased mortality in blunt trauma. J Trauma. 1991;31(9):1253–7. doi: 10.1097/00005373-199109000-00009. [DOI] [PubMed] [Google Scholar]
- 8.Liu T, Chen JJ, Bai XJ, Zheng GS, Gao W. The effect of obesity on outcomes in trauma patients: a meta-analysis. Injury. 2013;44(9):1145–52. doi: 10.1016/j.injury.2012.10.038. [DOI] [PubMed] [Google Scholar]
- 9.Ditillo M1, Pandit V, Rhee P, Aziz H, Hadeed S, Bhattacharya B, Friese RS, Davis K, Joseph B. Morbid obesity predisposes trauma patients to worse outcomes: a National Trauma Data Bank analysis. J Trauma Acute Care Surg. 2014;76(1):176–9. doi: 10.1097/TA.0b013e3182ab0d7c. [DOI] [PubMed] [Google Scholar]
- 10.Boulanger BR, Milzman D, Mitchell K, Rodriguez A. Body habitus as a predictor of injury pattern after blunt trauma. J Trauma. 1992;33(2):228–32. doi: 10.1097/00005373-199208000-00011. [DOI] [PubMed] [Google Scholar]
- 11.Gebregziabher M, Egedz L, Gilbert GE, Hunt K, Nietert PJ, Mauldin P. Fitting parametric random effects models in very large data sets with application to VHA national data. BMC Medical Research Methodology. 2012;163(12):1–14. doi: 10.1186/1471-2288-12-163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Newell MA, Bard MR, Goettler CE, Toschlog E, Schenarts P, Sagraves S, et al. Body Mass Index and Outcomes in Critically Injured Blunt Trauma Patients: Weighing the Impact. J Am Coll Surg. 2007;5(204):1056–1061. doi: 10.1016/j.jamcollsurg.2006.12.042. [DOI] [PubMed] [Google Scholar]
- 13.Varon J, Marik P. Management of the obese critically ill patient. Critical Care Clinics. 2001;(17):187–200. doi: 10.1016/s0749-0704(05)70159-7. [DOI] [PubMed] [Google Scholar]
- 14.Aganval N, Shibutani K, San Filippo JA. Hemodynamic and respiratory changes in surgery of the morbidly obese. Surgery. 1982;92(2):226–34. [PubMed] [Google Scholar]
- 15.Pasulka PS, Bistrian BR, Benotti PN. The risks of surgery in obese patients. Ann Intern Med. 1986:104540–546. doi: 10.7326/0003-4819-104-4-540. [DOI] [PubMed] [Google Scholar]
- 16.Strauss RJ, Wise L. Operative risks of obesity. Surg Gynecol Obstet. 1978;(146):286–291. [PubMed] [Google Scholar]
- 17.Vaughan RW, Wise L. Postoperative arterial blood gas measurement in obese patients: Effects of position on gas exchange. Ann Surg. 1975;(182):705–709. doi: 10.1097/00000658-197512000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rose DK, Cohen MM, Wigglesworth DF, et al. Critical respiratory events in the postanesthesia care unit: Patient, surgical and anesthetic factors. Anesthesiology. 1994;81:410–418. doi: 10.1097/00000542-199408000-00020. [DOI] [PubMed] [Google Scholar]
- 19.Smith-Choban P, Weireter LJ, Maynes C. Obesity and increased mortality in blunt trauma. J Trauma. 1991;(31):1253–1257. doi: 10.1097/00005373-199109000-00009. [DOI] [PubMed] [Google Scholar]
- 20.Christmas AB, Reynolds J, Wilson AK, Franklin GA, Miller FB, Richardson JD, Rodriguez JL. Morbid Obesity Impacts Mortality in Blunt Trauma. The American Surgeon. 2007;11(73):1122–1125. [PubMed] [Google Scholar]
- 21.Ortiz VE, Kwo J. Obesity: physiologic changes and implications for preoperative management. BMC Anesthesiol. 2015;15:97. doi: 10.1186/s12871-015-0079-8. [DOI] [PMC free article] [PubMed] [Google Scholar]


