Abstract
Background:
There is evidence regarding the relationship between dietary proteins intake and blood pressure (BP), but they had inconsistent results. Therefore, this study was designed to assess the association between different kinds of protein intake (animal and plant protein) and BP.
Materials and Methods:
Data were collected from Isfahan Healthy Heart Program. We performed a cross-sectional study among 9660 randomly selected Iranian adults aged ≥19-year-old that they were selected from three large Iranian regions in 2007. A simplified validated 48-item-food frequency questionnaire was used to assess dietary intake including all kinds of protein. Systolic and diastolic BPs were measured in duplicate by trained personnel using a standard protocol. Multivariable regressions were applied to assess the relationship between protein intake and BP levels and the presence of hypertension (HTN).
Results:
More frequent consumption of animal, plant, and total protein intake were inversely associated with BP in a crude model (P < 0.001); however, after adjustment for potential confounders this relationship remained only for plant protein (P = 0.04). The risk of HTN occurrence decreased in the highest quintile of total and plant protein consumption by 19% (odds ratio [OR] = 0.81; confidence interval [CI]: [0.65–0.96]; P for trend = 0.004) and 18% (OR = 0.82; [CI: (0.67–0.94]; P for trend = 0.03), respectively.
Conclusions:
More frequent protein intake, especially plant protein consumption was inversely associated with BP and risk of HTN among Iranian adults.
Keywords: Adult, blood pressure, hypertension, Iran, protein
Introduction
Hypertension (HTN) is a common chronic disease and a major public health problem that affects nearly one billion of the adult population worldwide.[1] HTN growth is relatively large in developed countries.[2] The prevalence of HTN is 17.3% among Iranian adults.[3] Genetic and environmental factors and their interactions are related with the development of HTN.[4] Among the environmental factors, diet has a major role in regulating blood pressure (BP).[5] High BP may improve with dietary habits modifications.[6,7] Dietary approaches to stop HTN diet is an important guideline for the management of HTN and related cardiovascular diseases (CVDs).[8,9] Previous studies found that dietary protein was inversely associated with BP.[10] The antihypertensive effect of protein is related not only to the amount of dietary protein but also to the source of protein.[10] Dietary proteins have a great number of biologically active peptides with positive physiological responses in the body.[11] Moreover, it was shown that plant protein has a greater role in regulating of BP,[12] for instance soy protein is rich in arginine, cysteine, and glycine. Arginine is a semi-essential amino acid that is necessary to the production of nitric oxide (NO) that plays an important role on regulating of BP and vascular health.[13]
Several studies indicated an inverse association between protein intake and BP.[14,15,16] However, small-scale trials had inconsistent findings.[17] As the previous studies that tried to examine the association between protein intake and their sources with BP led to inconsistent results and to the best of our knowledge, there is no evidence among neither the Middle Eastern nor Iranian populations on association of different kinds of protein consumption and HTN; therefore, we examined the relationship between dietary protein intake (animal and plant protein) and BP in a large population based on study in Iranian adults.
Materials and Methods
Sampling
Data of this study were collected from Isfahan Healthy Heart Program that was conducted in 2007 and participants were enrolled from the three countries of Iran (Isfahan, Najafabad, and Arak). A total of 9960 subjects aged ≥19 years were selected based on stratified cluster random sampling method in this study. Researchers selected a number of households from each of the cluster and then individual who were in one of these five age groups (19–24, 25–34, 35–44, 45–64, and ≥65) were randomly selected from each of these households. Subjects entered the study if they had these criteria: (1) They were over 19 years of age, (2) they experienced living in one of these counties for at least 6 years, and (3) they had Iranian nationality. Subjects were excluded if (1) they were pregnant; (2) they had liver, kidney, or blood disorders; (3) they had hemorrhage diseases; and (4) they had mental and psychiatric disease. This study was approved by the Research Council of Isfahan Cardiovascular Research Center (ICRC).[18,19]
Data collection
Trained health professionals were collected the socioeconomic, demographic, nutrition, smoking, and physical activity characteristics of participants by 30 min home interviews. Information about the medical history and drug history of participants including CVD disease, diabetes, HTN, and taking medications associated with these diseases was collected by trained physicians. The anthropometric measurements were obtained by medically trained staff. Weight was measured using a scale with minimal clothing and with an accuracy of about 0.5 kg and height was measured using nonelastic meter in a standing position while subjects were without shoes and the measurements were recorded with accuracy nearest 0.5 cm. Waist circumference was measured at a level of midway between the lower rib margin and the iliac crest with the elastic meter while the subjects were in standing position. Maximum circumference over the buttocks was used for measurement of hip circumference. Fasting blood samples from the left antecubital vein of subjects were collected to assess lipid profile and blood glucose concentration. Blood samples were sent to central laboratories of the ICRC and obtained at −20°C based on the National Reference Laboratory criteria (a WHO-collaborating center). All of the parameters were measured in ICRC laboratory which is approved by a national reference laboratory (the WHO collaborating center). Special kits (Immunodiagnostic, Germany) in a Hitachi auto-analyzer (Eppendorf, Germany) were applied to the assessment of total cholesterol and triglyceride level by the standard enzymatic method. Measurement of serum high-density lipoprotein-cholesterol level was conducted with enzymatically method.[20] Serum low-density lipoprotein-cholesterol level was also measured through Friedewald equation.[21] Enzymatic reaction was also used to determine the concentration of blood glucose. A standard mercury sphygmomanometer was used for measurement of BP from the right arm of participants who had rested for at least 10 min.
Dietary assessment
The common consumption of plant and animal protein among Iranian population was assessed through seven questions by a validated 48-item-food frequency questionnaire (FFQ).[22] These questionnaires were an open-ended one which no assessing serving of food consumption. Animal source of protein included meat, poultry, fish, dairy products, and egg and plant source were considered as nuts, legumes, and soy protein.
Blood pressure measurement
BP of subjects who were in sitting position for at least 10 min was measured two times by trained physicians according to standard protocol. Systolic BP (SBP) and diastolic BPs (DBPs) were obtained by calculating the average of two measures from the first and the fifth stage of Korotkoff phases, respectively. HTN was defined as an SBP ≥140 mmHg and/or a DBP ≥90 mmHg and/or use of at least one type of antihypertensive medication currently based on Joint National Committee-7 criteria.[23]
Statistical analysis
Frequencies for categorical variables and mean and standard deviations for continuous variables were used to summarize the data. Chi-squared statistics and one-way analysis of variance tests were used to compare baseline characteristics, dietary intake, and mean of SBP and DBP based on the quintiles of total dietary protein, animal and plant protein consumption. Analysis of covariance test was used to compare the mean of SBP and DBP in quintiles of total dietary protein, animal and plant protein after adjustment age (year), gender (male/female), education (illiterate/primary/high school and higher), body mass index (BMI) (kg/m2), physical activity (metabolic equivalent of tasks [METs] min/week), smoking (never/past/current), diabetes mellitus (yes/no), dyslipidemia (yes/no), dietary factor including hydrogenated vegetable oil, nonhydrogenated vegetable oil, animal fat, fast food, sweet, carbonated beverages, fruits and vegetables and cereals (time/week), and using salt at table (yes/no).
Simple logistic regression was first fitted to evaluate the crude relations between HTN and the quintiles of dietary protein sources consumption, then multiple logistic regression, to determine the adjusted associations, considering the reference category as those in the first quintile of dietary protein sources intake. The initial adjusted model was defined comprising age groups and gender as covariates. We fitted model 1 to assess the possibilities of confounding by education (illiterate/primary/high school and higher), BMI (kg/m2), physical activity (METs min/week), smoking (never/past/current), diabetes mellitus (yes/no), and dyslipidemia (yes/no). Additional adjusted for dietary factors (time/week) and using salt at the table (yes/no) were adjusted in the model 2. Statistical analyses were performed using SPSS for Windows version 15 (SPSS Inc., Chicago, IL, USA). The significance level was set at P < 0.05. The sensitivity and specificity of the logistic models were calculated for assessment of goodness of fit.
Results
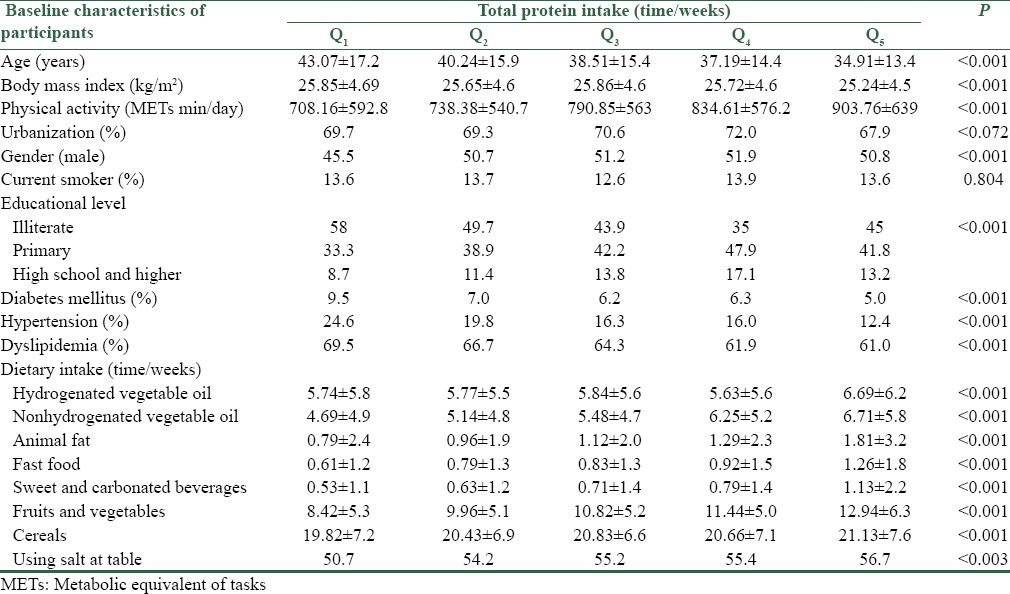
Baseline characteristics of participants by quartile of dietary protein intake are shown in Table 1. Participants with higher protein consumption were more likely to be men, younger, physically active had higher socioeconomic status and less BMI and less likely to be overweight/obese or a current smoker, hypertensive, diabetic, and dyslipidemic (P < 0.001) [Table 1]. Among dietary factors, protein consumption was positively associated with intakes of hydrogenated vegetable oil, nonhydrogenated vegetable oil, animal fat, sweet and carbonated beverages, fruits and vegetables, cereals, and salt at the table (all P < 0.01).
Table 1.
Baseline characteristics according to quintiles of dietary protein intake
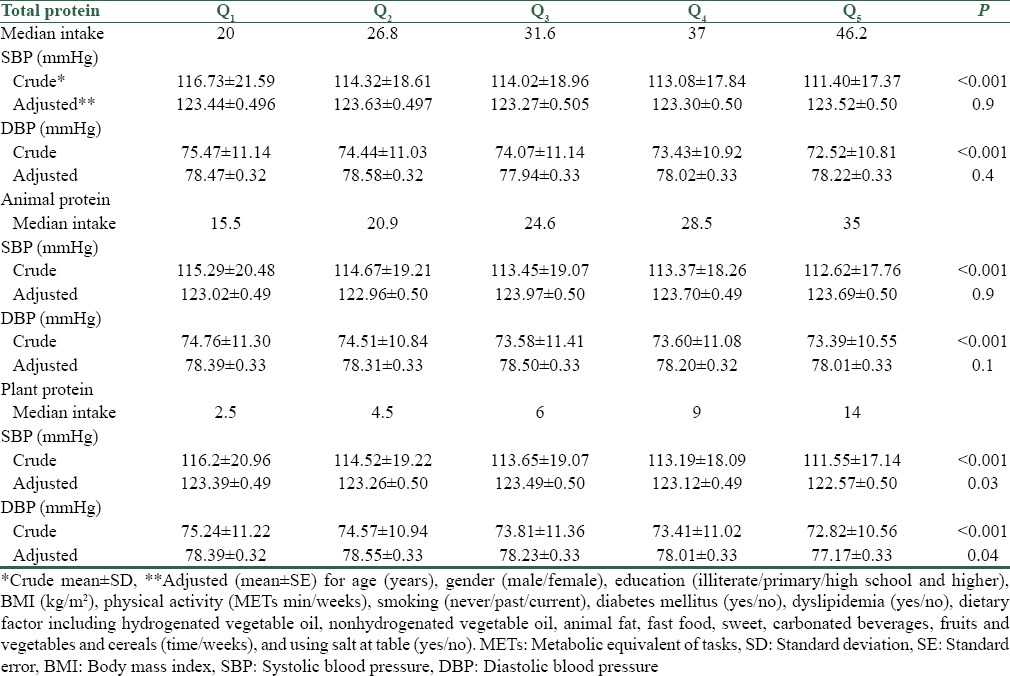
More frequent total, animal and plant protein intake was significantly related to lower SBP and DBP in a crude model (P < 0.001); however, after adjusting for potential confounders in the fully-multivariable adjusted model, only more frequent plant protein consumption was significantly associated with lower SBP and DBP (P = 0. 04) [Table 2].
Table 2.
Mean of blood pressure components by quintiles of dietary protein intake
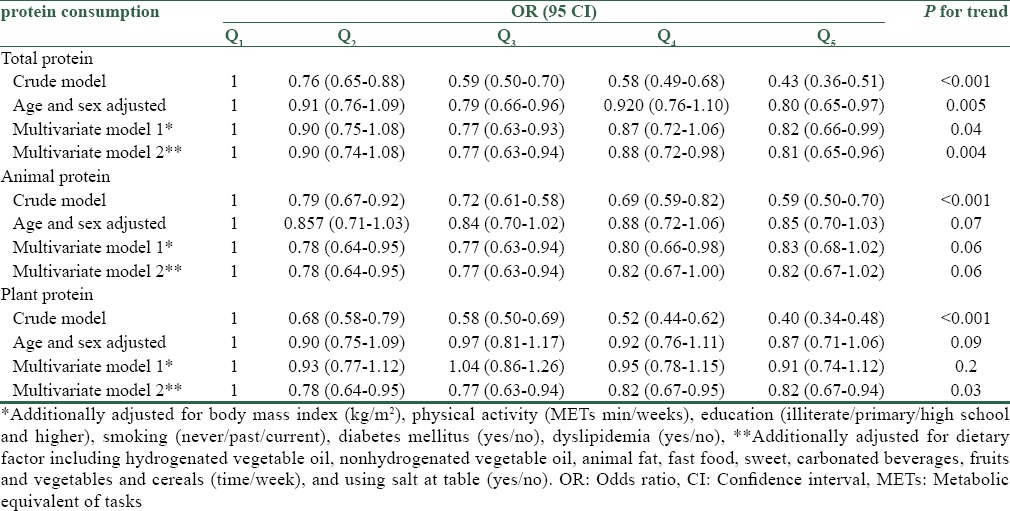
The results of logistic regression are presented in Table 3. The odds ratios (ORs) (95% confidence interval [CI]) of crude and multivariate adjusted models revealed a greater risk of HTN for participants with less frequent total protein intake (OR = 0.43; CI: 0.36–0.51; P for trend < 0.001). All multivariate adjusted models demonstrated significant inverse relationships between the higher category of total protein consumption and risk of HTN. ORs surged enormously in the higher category of total protein consumption. The risk of HTN occurrence decreased 19% in the highest quintile of total protein consumption in fully adjustment model (0.81 [0.65–0.96]; P for trend = 0.004). Only in crude model, animal protein consumption had a marked effect in lowering risk of HTN (OR = 0.59; CI: 0.50–0.70; P for trend < 0.001). As shown in Table 3, the lower risk of HTN occurrence was associated with more frequent consumption of plant protein in crude and full adjustment models. ORs demonstrated that the highest quintile of plant protein intake related to 60% reduction in the occurrence of HTN (0.40 [0.34–0.48]; P < 0.001). ORs attenuated marginally by excluding all potential confounder's effects (0.82 [0.67–0.94]; P = 0.03).
Table 3.
Multivariate odds ratios of hypertension by quintiles of protein consumption
Discussion
We found an inverse dose-response relationship between the frequency of total, animal and plant protein consumption, and the prevalence of HTN. However, after adjustment for potential confounders, these associations were diluted and significant with total and plant protein consumption. Our study demonstrated that the frequency of plant protein consumption was associated with lower means of SBP and DBP.
In agreement with our findings, the Shanghai woman health study assessed the relationship between soy food consumption (as a source of plant protein) and BP. This study showed that more frequent soy protein consumption was inversely associated with BP. Both SBP and DBPs were lower in subjects who consumed ≥2.5 g soy food compared with subjects who consumed <2.5 g.[24] In addition, PREMIER, INTERMAP studies and another study with cross-sectional design showed an inverse relationship between plant protein consumption and HTN risk, while animal and total protein intake had no significant association with BP.[10,25,26] Furthermore, consistent to our results, a meta-analyses study based on the findings from forty randomized-controlled trials (RCTs) demonstrated that the higher consumption of all sources of protein was associated with lower BP in healthy subjects.[27] In addition, a systematic review of 46 studies found a weak inverse association between total protein intake and BP among hypertensive participants. Most observational studies containing in this systematic review indicated an inverse association between plant protein intake and BP, while this correlation was weaker between animal protein intake and BP.[28] RCT that was conducted among pre-HTN or stage I HTN patients concluded that BP decreased with higher protein intake.[29] Although these different studies had various design and study population but they found a similar relationship between protein intake and BP. However, a prospective study that was conducted among European patients with type 1 diabetes mellitus reported that there was no significant relationship between all kinds of protein intake and incidence of HTN after 7 years follow-up. It might be due to diabetes mellitus status.[30] Umesawa et al. study demonstrated that more frequent total protein consumption was inversely associated with SBP and DBP among Japanese men and women.[31] The significant inverse association was also found between animal protein intake and SBP. It must be underlined that the protective effect of total protein on DBP was still supported by the multivariate adjusted model of linear regression. In contrast, the result of this study showed that plant protein consumption was positively correlated with SBP after adjustment for potential confounders.[31] Umesawa et al. proposed that positive association of plant protein consumption with BP derived from high sodium content of plant protein sources in the Japanese population.[31] In addition, it must be noted that the variety of nutrient content of animal protein sources including saturated fatty acid and omega-3 fatty acid that are found in red meat, fish, and poultry caused different effects on BP.[26]
There are several purported reasons, which indirectly may explain the biological plausibility of different dietary protein consumption and BP improvements. First, the amino acids content of protein including arginine, tryptophan, and tyrosine can affect the regulation of BP. L-arginine is a precursor of NO, which has a vasodilatory property so it can improve the BP.[32,33] Second, the previous study showed that increasing protein intake lead to increase renal plasma flow, rate of glomerular filtration, and exertion of sodium that they are important for regulating of BP.[34] Third, the crunchy textural property of protein promotes satiety as the mechanical act of mastication results in secretion of hormones such as cholecystokinin that is dietary compensation that finally leads to lower calorie intakes, weight management, and finally BP modulation.[35] Fourth, proteins that have low-glycemic index lead to smaller increase in insulin concentration compared with carbohydrate and thus it may play a role for management of BP.[36] In addition, plant proteins are the source of magnesium, potassium, and fiber that they are effective in regulating of BP.[37,38,39,40] The result of this study was adjusted for fruit, vegetable, and cereal that they contain high amount of fiber, but magnesium and potassium intake were not adjusted in this study so they may influence the result of our study. Soy protein that was classified as plant protein foods is containing isoflavones. The study showed that isoflavones are effective in reducing BP.[17] High intake of soy protein by the subjects of this study may be involved in a significant inverse association that was shown between plant protein intake and BP.
Strength and limitations
The strengths of this study were its large population covering three different countries with a variety of socioeconomic status, which make it unique dataset in Iran and Middle East. Limitations included the study's cross-sectional design, which is theoretically unable to clarify the effective factors resulting in dietary protein's HTN improvement properties. No adjustment for potassium, magnesium, and folate intake is another limitation, though the dietary sources of these nutrients, including fruit, vegetable, and cereal were adjusted in our analyses. Causality can therefore not be demonstrated. Furthermore, our analyses could only make associations at a particular point in time and not take into account dietary changes over time. Our data supported an association between protein consumption and lower BP, but more studies are needed to establish their individual degree of protection and effectiveness. The FFQ was qualitative; therefore, it is impossible to assess protein intake as gram or serving as well as energy intake. Our estimation may outline a missing dose responsible for protein consumption for different genders and various age groups.
Conclusions
We concluded that frequent protein consumption, particularly plant protein was inversely associated with HTN and may regulate BP and finally exert cardioprotective effects among Iranians. However, more randomized clinical trials are required to illustrate the dose-response effect of nuts on lipid profile.
Financial support and sponsorship
This program was conducted by the ICRC (the WHO Collaborating Center) in collaboration with the Isfahan Provincial Health Office. Both are affiliated with the Isfahan University of Medical Sciences. The program was supported by a grant (No. 31309304) from the Iranian Budget and Planning Organization, as well as the Deputy for Health of the Iranian Ministry of Health and Medical Education and the Iranian Heart Foundation.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
This program was conducted by the ICRC (the WHO Collaborating Center) in collaboration with the Isfahan Provincial Health Office. Both are affiliated with the Isfahan University of Medical Sciences. The program was supported by a grant (No. 31309304) from the Iranian Budget and Planning Organization, as well as the Deputy for Health of the Iranian Ministry of Health and Medical Education and the Iranian Heart Foundation. We are thankful to the large team of ICRC and Isfahan Provincial Health Office as well as collaborators from Najaf-Abad Health Office and Arak University of Medical Science.
References
- 1.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jr, et al. Seventh report of the Joint National Committee on prevention, detection, evaluation, and treatment of high blood pressure. Hypertension. 2003;42:1206–52. doi: 10.1161/01.HYP.0000107251.49515.c2. [DOI] [PubMed] [Google Scholar]
- 2.Kearney PM, Whelton M, Reynolds K, Muntner P, Whelton PK, He J. Global burden of hypertension: Analysis of worldwide data. Lancet. 2005;365:217–23. doi: 10.1016/S0140-6736(05)17741-1. [DOI] [PubMed] [Google Scholar]
- 3.Shirani S, Kelishadi R, Sarrafzadegan N, Khosravi A, Sadri G, Amani A, et al. Awareness, treatment and control of hypertension, dyslipidaemia and diabetes mellitus in an Iranian population: The IHHP study. East Mediterr Health J. 2009;15:1455–63. [PubMed] [Google Scholar]
- 4.Vasdev S, Stuckless J, Richardson V. Role of the immune system in hypertension: Modulation by dietary antioxidants. Int J Angiol. 2011;20:189–212. doi: 10.1055/s-0031-1288941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Appel LJ, Brands MW, Daniels SR, Karanja N, Elmer PJ, Sacks FM American Heart Association. Dietary approaches to prevent and treat hypertension: A scientific statement from the American Heart Association. Hypertension. 2006;47:296–308. doi: 10.1161/01.HYP.0000202568.01167.B6. [DOI] [PubMed] [Google Scholar]
- 6.Dickinson HO, Mason JM, Nicolson DJ, Campbell F, Beyer FR, Cook JV, et al. Lifestyle interventions to reduce raised blood pressure: A systematic review of randomized controlled trials. J Hypertens. 2006;24:215–33. doi: 10.1097/01.hjh.0000199800.72563.26. [DOI] [PubMed] [Google Scholar]
- 7.Ferrara LA, Raimondi AS, d’Episcopo L, Guida L, Dello Russo A, Marotta T. Olive oil and reduced need for antihypertensive medications. Arch Intern Med. 2000;160:837–42. doi: 10.1001/archinte.160.6.837. [DOI] [PubMed] [Google Scholar]
- 8.Salehi-Abargouei A, Maghsoudi Z, Shirani F, Azadbakht L. Effects of dietary approaches to stop hypertension (DASH)-style diet on fatal or nonfatal cardiovascular diseases – Incidence: A systematic review and meta-analysis on observational prospective studies. Nutrition. 2013;29:611–8. doi: 10.1016/j.nut.2012.12.018. [DOI] [PubMed] [Google Scholar]
- 9.Sacks FM, Svetkey LP, Vollmer WM, Appel LJ, Bray GA, Harsha D, et al. Effects on blood pressure of reduced dietary sodium and the dietary approaches to stop hypertension (DASH) diet. DASH-Sodium Collaborative Research Group. N Engl J Med. 2001;344:3–10. doi: 10.1056/NEJM200101043440101. [DOI] [PubMed] [Google Scholar]
- 10.Elliott P, Stamler J, Dyer AR, Appel L, Dennis B, Kesteloot H, et al. Association between protein intake and blood pressure: The INTERMAP study. Arch Intern Med. 2006;166:79–87. doi: 10.1001/archinte.166.1.79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Murray BA, FitzGerald RJ. Angiotensin converting enzyme inhibitory peptides derived from food proteins: Biochemistry, bioactivity and production. Curr Pharm Des. 2007;13:773–91. doi: 10.2174/138161207780363068. [DOI] [PubMed] [Google Scholar]
- 12.He J, Gu D, Wu X, Chen J, Duan X, Chen J, et al. Effect of soybean protein on blood pressure: A randomized, controlled trial. Ann Intern Med. 2005;143:1–9. doi: 10.7326/0003-4819-143-1-200507050-00004. [DOI] [PubMed] [Google Scholar]
- 13.Vasdev S, Gill V. The antihypertensive effect of arginine. Int J Angiol. 2008;17:7–22. doi: 10.1055/s-0031-1278274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Blumenthal JA, Babyak MA, Hinderliter A, Watkins LL, Craighead L, Lin PH, et al. Effects of the DASH diet alone and in combination with exercise and weight loss on blood pressure and cardiovascular biomarkers in men and women with high blood pressure: The ENCORE study. Arch Intern Med. 2010;170:126–35. doi: 10.1001/archinternmed.2009.470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Iseki K, Iseki C, Itoh K, Sanefuji M, Uezono K, Ikemiya Y, et al. Estimated protein intake and blood pressure in a screened cohort in Okinawa, Japan. Hypertens Res. 2003;26:289–94. doi: 10.1291/hypres.26.289. [DOI] [PubMed] [Google Scholar]
- 16.Liu L, Ikeda K, Sullivan DH, Ling W, Yamori Y. Epidemiological evidence of the association between dietary protein intake and blood pressure: A meta-analysis of published data. Hypertens Res. 2002;25:689–95. doi: 10.1291/hypres.25.689. [DOI] [PubMed] [Google Scholar]
- 17.Liu ZM, Ho SC, Chen YM, Woo J. Effect of soy protein and isoflavones on blood pressure and endothelial cytokines: A 6-month randomized controlled trial among postmenopausal women. J Hypertens. 2013;31:384–92. doi: 10.1097/HJH.0b013e32835c0905. [DOI] [PubMed] [Google Scholar]
- 18.Sarrafzadegan N, Kelishadi R, Sadri G, Malekafzali H, Pourmoghaddas M, Heidari K, et al. Outcomes of a comprehensive healthy lifestyle program on cardiometabolic risk factors in a developing country: The Isfahan Healthy Heart Program. Arch Iran Med. 2013;16:4–11. [PubMed] [Google Scholar]
- 19.Mohammadifard N, Kelishadi R, Safavi M, Sarrafzadegan N, Sajadi F, Sadri GH, et al. Effect of a community-based intervention on nutritional behaviour in a developing country setting: The Isfahan Healthy Heart Programme. Public Health Nutr. 2009;12:1422–30. doi: 10.1017/S1368980008004230. [DOI] [PubMed] [Google Scholar]
- 20.Warnick GR, Benderson J, Albers JJ. Dextran sulfate-Mg2+precipitation procedure for quantitation of high-density-lipoprotein cholesterol. Clin Chem. 1982;28:1379–88. [PubMed] [Google Scholar]
- 21.Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. 1972;18:499–502. [PubMed] [Google Scholar]
- 22.Mohammadifard N, Sarrafzadegan N, Nouri F, Sajjadi F, Alikhasi H, Maghroun M, et al. Using factor analysis to identify dietary patterns in Iranian adults: Isfahan Healthy Heart Program. Int J Public Health. 2012;57:235–41. doi: 10.1007/s00038-011-0260-x. [DOI] [PubMed] [Google Scholar]
- 23.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jr, et al. The seventh report of the Joint National Committee on prevention, detection, evaluation, and treatment of high blood pressure: The JNC 7 report. JAMA. 2003;289:2560–72. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- 24.Yang G, Shu XO, Jin F, Zhang X, Li HL, Li Q, et al. Longitudinal study of soy food intake and blood pressure among middle-aged and elderly Chinese women. Am J Clin Nutr. 2005;81:1012–7. doi: 10.1093/ajcn/81.5.1012. [DOI] [PubMed] [Google Scholar]
- 25.Altorf-van der Kuil W, Engberink MF, Vedder MM, Boer JM, Verschuren WM, Geleijnse JM. Sources of dietary protein in relation to blood pressure in a general Dutch population. PLoS One. 2012;7:e30582. doi: 10.1371/journal.pone.0030582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wang YF, Yancy WS, Jr, Yu D, Champagne C, Appel LJ, Lin PH. The relationship between dietary protein intake and blood pressure: Results from the PREMIER study. J Hum Hypertens. 2008;22:745–54. doi: 10.1038/jhh.2008.64. [DOI] [PubMed] [Google Scholar]
- 27.Rebholz CM, Friedman EE, Powers LJ, Arroyave WD, He J, Kelly TN. Dietary protein intake and blood pressure: A meta-analysis of randomized controlled trials. Am J Epidemiol. 2012;176(Suppl 7):S27–43. doi: 10.1093/aje/kws245. [DOI] [PubMed] [Google Scholar]
- 28.Altorf-van der Kuil W, Engberink MF, Brink EJ, van Baak MA, Bakker SJ, Navis G, et al. Dietary protein and blood pressure: A systematic review. PLoS One. 2010;5:e12102. doi: 10.1371/journal.pone.0012102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Appel LJ, Sacks FM, Carey VJ, Obarzanek E, Swain JF, Miller ER, 3rd, et al. Effects of protein, monounsaturated fat, and carbohydrate intake on blood pressure and serum lipids: Results of the OmniHeart randomized trial. JAMA. 2005;294:2455–64. doi: 10.1001/jama.294.19.2455. [DOI] [PubMed] [Google Scholar]
- 30.Altorf-van der Kuil W, Engberink MF, Ijpma I, Verberne LD, Toeller M, Chaturvedi N, et al. Protein intake in relation to risk of hypertension and microalbuminuria in patients with type 1 diabetes: The EURODIAB prospective complications study. J Hypertens. 2013;31:1151–9. doi: 10.1097/HJH.0b013e328360418e. [DOI] [PubMed] [Google Scholar]
- 31.Umesawa M, Sato S, Imano H, Kitamura A, Shimamoto T, Yamagishi K, et al. Relations between protein intake and blood pressure in Japanese men and women: The circulatory risk in communities study (CIRCS) Am J Clin Nutr. 2009;90:377–84. doi: 10.3945/ajcn.2008.27109. [DOI] [PubMed] [Google Scholar]
- 32.Stamler J, Elliott P, Kesteloot H, Nichols R, Claeys G, Dyer AR, et al. Inverse relation of dietary protein markers with blood pressure. Findings for 10,020 men and women in the INTERSALT study. INTERSALT Cooperative Research Group. INTERnational study of SALT and blood pressure. Circulation. 1996;94:1629–34. doi: 10.1161/01.cir.94.7.1629. [DOI] [PubMed] [Google Scholar]
- 33.Anderson GH. Proteins and amino acids: Effects on the sympathetic nervous system and blood pressure regulation. Can J Physiol Pharmacol. 1986;64:863–70. doi: 10.1139/y86-149. [DOI] [PubMed] [Google Scholar]
- 34.Sved AF, Fernstrom JD, Wurtman RJ. Tyrosine administration reduces blood pressure and enhances brain norepinephrine release in spontaneously hypertensive rats. Proc Natl Acad Sci U S A. 1979;76:3511–4. doi: 10.1073/pnas.76.7.3511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Stamler J, Caggiula A, Grandits GA, Kjelsberg M, Cutler JA. Relationship to blood pressure of combinations of dietary macronutrients. Findings of the multiple risk factor intervention trial (MRFIT) Circulation. 1996;94:2417–23. doi: 10.1161/01.cir.94.10.2417. [DOI] [PubMed] [Google Scholar]
- 36.Paddon-Jones D, Westman E, Mattes RD, Wolfe RR, Astrup A, Westerterp-Plantenga M. Protein, weight management, and satiety. Am J Clin Nutr. 2008;87:1558S–61S. doi: 10.1093/ajcn/87.5.1558S. [DOI] [PubMed] [Google Scholar]
- 37.Makris AP, Borradaile KE, Oliver TL, Cassim NG, Rosenbaum DL, Boden GH, et al. The individual and combined effects of glycemic index and protein on glycemic response, hunger, and energy intake. Obesity (Silver Spring) 2011;19:2365–73. doi: 10.1038/oby.2011.145. [DOI] [PubMed] [Google Scholar]
- 38.Zhou B, Zhang X, Zhu A, Zhao L, Zhu S, Ruan L, et al. The relationship of dietary animal protein and electrolytes to blood pressure: A study on three Chinese populations. Int J Epidemiol. 1994;23:716–22. doi: 10.1093/ije/23.4.716. [DOI] [PubMed] [Google Scholar]
- 39.Streppel MT, Arends LR, van’t Veer P, Grobbee DE, Geleijnse JM. Dietary fiber and blood pressure: A meta-analysis of randomized placebo-controlled trials. Arch Intern Med. 2005;165:150–6. doi: 10.1001/archinte.165.2.150. [DOI] [PubMed] [Google Scholar]
- 40.Cunha AR, Umbelino B, Correia ML, Neves MF. Magnesium and vascular changes in hypertension. Int J Hypertens. 2012;2012:754250. doi: 10.1155/2012/754250. [DOI] [PMC free article] [PubMed] [Google Scholar]


