Abstract
Background
Wii Fit was originally designed as a health and fitness interactive training experience for the general public. There are, however, many examples of Wii Fit being utilized in clinical settings. This article aims to identify the contribution of Wii Fit in the field of health promotion and rehabilitation by: (1) identifying the health-related domains for which the Wii Fit series has been tested, (2) clarifying the effect of Wii Fit in those identified health-related domains and (3) quantifying this effect.
Method
A systematic literature review was undertaken. The MEDLINE database and Games for Health Journal published content were explored using the search term “Wii-Fit.” Occurrences resulting from manual searches on Google and material suggested by experts in the field were also considered. Included articles were required to have measurements from Wii Fit activities for at least one relevant health indicator. The effect of Wii Fit interventions was assessed using meta-analyses for the following outcomes: activity-specific balance confidence score, Berg balance score (BBC) and time-up-and-go test (TUG).
Findings
A total of 115 articles highlighted that the Wii Fit has been tested in numerous healthy and pathological populations. Out of these, only a few intervention studies have focused on the prevention of chronic diseases. A large proportion of the studies focus on balance training (N = 55). This systematic review highlights several potential benefits of Wii Fit interventions and these positive observations are supported by meta-analyses data (N = 25). For example, the BBC and the TUG respond to a similar extend to Wii Fit interventions compared with traditional training.
Conclusion
Wii Fit has the potential to be used as a rehabilitation tool in different clinical situations. However, the current literature includes relatively few randomized controlled trials in each population. Further research is therefore required.
Keywords: Wii Fit, Balance training, Health and fitness, Health promotion, Active video games, Rehabilitation, Prevention of chronic diseases
Introduction
The past decade saw the emergence of home-based active video games (AVG), with the Wii (Nintendo Co. Ltd., Kyoto, Japan) being released in 2006, followed by the PlayStation Move (Sony Corp, Tokyo, Japan) and the Kinect (Microsoft, Redmond, WA, USA) in 2010. These systems take advantage of accelerometry and video camera-mediated motion detection technologies to track the player’s movements and convert them into gaming commands. The Wii offers an original game modality with the Wii Balance Board accessory, which can be used as a weighing scale or as a gamepad sensitive to body sway (Clark et al., 2010).
Among the home-based AVG, the well-known Wii Fit series (Nintendo, Japan) runs on the Wii console and consists of a combination of both serious and entertaining activities requiring body movement to fulfill gaming commands. The software displays various kinds of health metrics (body mass index, number of kilocalories burned over a given period) encouraging the players to improve their physical fitness. Whilst the Wii Fit was primarily designed to be used in homes by healthy individuals for health and fitness purposes, an overview of the literature indicates that physical therapists and physicians from different medical fields include the use of Wii Fit in their clinical practice. For instance, the National Stroke Audit: Rehabilitation Services Report recently indicated that 76% of Australian hospitals have a Wii console available to aid with the rehabilitation of stroke patients (the National Stroke Foundation, 2012 in Levac et al., 2010).
Many reviews have focused on AVG and their effects on health and describe mitigated outcomes (LeBlanc et al., 2013; Peng, Crouse & Lin, 2013). However, the distinction between Wii Fit and other AVG was not always clear, resulting in the inability to ascertain an objective picture of the contribution from the Wii Fit. The goals for this systematic review are as follows:
Goal 1: Identifying the health-related domains (i.e., populations and clinical situations) in which the Wii Fit series has already been tested or used. A scientific database search with reasoned exclusion criteria was undertaken.
Goal 2: Understanding the effect of Wii Fit in the identified populations (cf. Goal 1). A qualitative systematic review of studies including Wii Fit interventions was performed, with particular attention given to health and physical activity outcomes.
Goal 3: When possible, quantification of the effect Wii Fit has on selected health-related domains was achieved by conducting meta-analyses.
Methods
Literature search
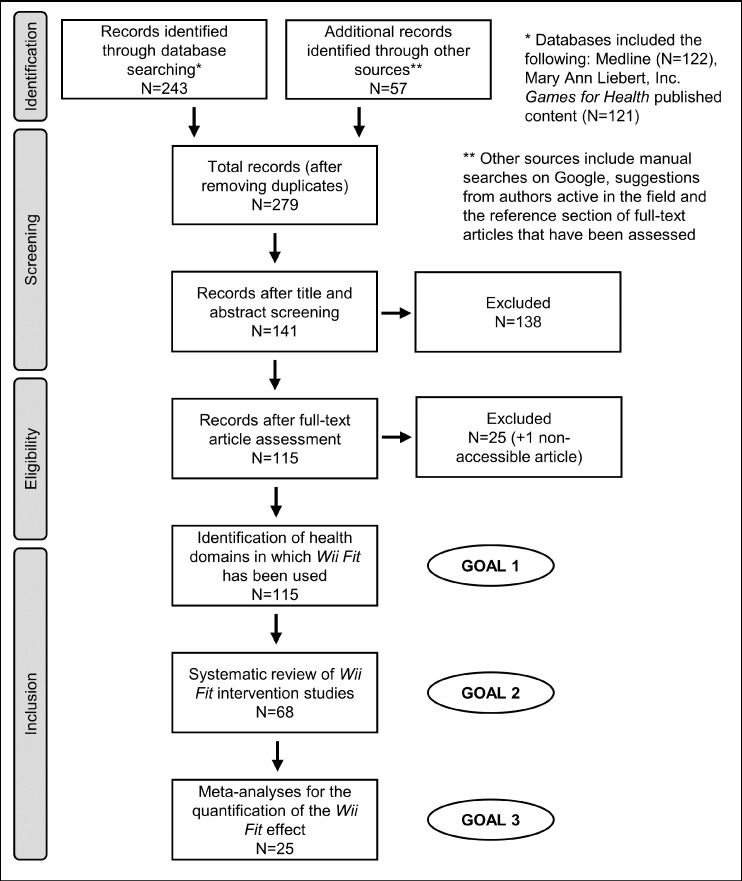
The selection process is summarized in a PRISMA flow diagram (Fig. 1). Several strategies were adopted: (1) The MEDLINE database was used to conduct a systematic search using the following keywords: “wii fit,” “wii-fit” and “wiifit” (occurrences: N = 122). (2) The same keywords were used to search for additional articles in the Mary Ann Liebert, Inc. Games and Health Journal (N = 121). (3) Additional peer-reviewed articles were identified during manual searches via Google Search (Google Inc., Mountain View, CA, USA) (N = 1). (4) Articles suggested by authors active in the field of AVG (N = 10) or identified in the reference section of eligible papers (N = 46). (5) Only papers in English, French or Japanese were eligible for this review. The search and data extraction were performed by two independent researchers (Murakami H and Tripette J) and any discrepancies were resolved by a third contributor (Miyachi M).
Figure 1. Flow diagram for the selection of studies included in the systematic review and the meta-analyses.
Details about exclusion criteria and the selection process can be found in Table 1 and the “Methods.”
The literature search was completed in June 2015. A total of 200 articles were identified. In order to meet the primary inclusion criteria, studies were required to: (1) have a primary focus on any software of the Wii Fit series, and (2) focus on a recognized health issue. A total of 279 articles were screened after the identification and removal of 21 duplicates (Fig. 1).
Goal 1: identification of health domains
The exclusion criteria applied to identify medical domains in which the Wii Fit has already been tested or used are described in Table 1. The identification process involved screening titles and abstracts. The full texts were read when the abstracts provided insufficient details (Fig. 1 and Table 1). The results are shown in Table 2.
Table 1. Summary of exclusion criteria.
| Literature review stage | Exclusion criteria |
|---|---|
| Screening |
|
| Goal 1 |
|
| Goal 2 |
|
| Goal 3 |
|
Notes:
SD, standard deviation.
Examples of excluded studies for this selection criteria are (Morone et al., 2014; Wall et al., 2015).
Examples of excluded studies for this selection criteria are (Bieryla & Dold, 2013; Janssen, Tange & Arends, 2013; Rendon et al., 2012; Bainbridge et al., 2011).
An example of an excluded study for this selection criteria is (Fung et al., 2012).
An example of an excluded study for this selection criteria is (Salem et al., 2012).
Table 2. Wii Fit studies, health domains and populations of interest.
Notes:
Not including overweight populations.
Some papers focused on various populations may appear in several fields.
Not including studies that focus on healthy adult women only.
The study included healthy subjects but targeted women with urinary incontinence.
Patients with « other neurological disorders » were included as well.
Includes both middle-age adults and seniors.
Includes subjects referred for rehabilitation, presenting a history of accidental falls, having fear of falling or described as frail or pre-frail.
Goal 2: systematic review, data extraction and synthesis
A qualitative systematic review was performed to understand the effect of Wii Fit in the previously identified health domains. This study followed the 2009 PRISMA guidelines for the conductance of systematic reviews and meta-analyses (Liberati et al., 2009) (see, Data S1). The exclusion criteria which were applied at this stage are described in Table 1.
The content of each eligible article was extracted according to the following protocol: (1) Study identification (first author’s name, year and country), (2) methodological details (study design, sample size, population characteristics, etc.), (3) activities used, (4) description of each identified primary or secondary health and physical activity outcome and (5) key findings (i.e., pre- and post-intervention as well as differences between Wii Fit and control groups) (Tables 3 and 4).
Table 3. Wii Fit interventions for health status and well-being improvement1.
| Authors (year), country | Population characteristics | Study design | Wii Fit activities (or other video games) | Outcomes and measures | Key findings and data used for the meta-analyses |
|---|---|---|---|---|---|
| Healthy population | |||||
| Nitz et al. (2010), Australia | Women (N = 10) Age range: 30–60 years Mean age: 47 ± 10 years |
Intervention One group Duration: 10 weeks (30 min, two sessions/week) Location: Home (supposedly) |
Not specified, possibly all the Wii Fit’s activities | Physical fitness (6 min walk test, lower limb strength), body composition, balance and functional mobility (TUG, TUGcog, step test, CTSIB, basic balance master test), well-being (home-made scale), adherence (attendance) | Improvement for some balance tests and lower limb strength. The overall attendance was 70%. Adverse events: No TUG (s): Wii Fit group Pre-intervention: 4.93 ± 0.76 Post-intervention: 5.00 ± 0.73 |
| Owens et al. (2011), USA | Eight families (parents and children, F/M, N = 13/8) Age range: 8–44 years |
Intervention One group (statistical analysis: children vs. adults) Duration: 13 weeks (no further specifications: naturalistic approach) Location: Home |
Not specified (subjects used the four categories of activities: yoga, strength, aerobics, balance) | PA (accelerometry), body composition, balance (SOT), physical fitness (VO2max, upper limb strength, flexibility), adherence (playing time) | No significant change was noted in most of the physical fitness outcomes. Peak VO2 increased in children only. Adherence declined over time. In realistic conditions Wii Fit may not provide sufficient stimulus for fitness improvement Adverse events: No |
| Tripette et al. (2014b), Japan | Postpartum women (N = 34) Mean age: 32 ± 5 years |
Intervention (RCT) Two groups: Wii Fit vs. passive control Duration: five weeks (30 min, daily) Location: Home |
All activities included in the Wii Fit Plus software | Body composition, physical fitness (flexibility and strength), energy intakes (questionnaire), adherence (playing time) | Women playing Wii Fit lost more weight than their passive control counterpart. They expended an average 4,700 ± 2,900 kcal playing Wii Fit and decrease their energy intakes Adverse events: lower back pain (N = 1), ankle twist (N = 1) and wrist tendinitis (N = 1) |
| Chronic diseases | |||||
| Albores et al. (2013), USA | COPD patients (F/M, N = 14/6) Mean age: 68 ± 10 years |
Intervention One group Duration: 12 weeks (30 min, daily) Location: Home |
Aerobics: Basic run, free step; Training plus: Bird’s eye Bull’s-eye, obstacle course |
Primary: physical fitness (ESWT and other tests) Secondary: health status (CRQ-SR, dyspnea assessment) |
Home-based Wii Fit training improved physical fitness and overall health status but not dyspnea in COPD patients Adverse events: No |
| Kempf & Martin (2013), Germany | T2DM patients (F/M, N = 119/101) Age range: 50–75 years Mean age: 61 ± 8 years |
Intervention (RCT) Two groups: Wii Fit-traditional care vs. traditional care-Wii Fit Duration: 12 weeks (30 min/day) Location: Home |
Not specified (supposedly, all the activities included in Wii Fit Plus) |
Primary: glycemic variations (HbA1c) and various blood markers Secondary: body composition, blood pressure, PA (questionnaire), adherence (retention), health status (SF-12, PAID) and well-being and quality of life (WHO-5, CESD) |
Subjects adhered to the Wii Fit intervention (retention rate: 80%). Playing Wii Fit on a daily basis significantly decreased HbA1c in T2DM patients (−0.3 ± 1.1). Fasting glucose, weight, BMI, PA, as well as other well-being outcomes were also improved Adverse events: No |
| Cho & Sohng (2014), Korea | Hemodialysis patients (F/M, N = 18/28) Mean age: 59 ± 8 years |
Intervention (RCT) Two groups: Wii Fit vs. passive control Duration: eight weeks (30 min, three sessions/week) Location: Hospital |
Yoga: Chair, Half Moon, Standing Knee (supposedly); strength: Torso Twist, Triceps Extension (supposedly); balance: Balance Bubble, Tightrope Walk; aerobics: Basic Steps (supposedly), Hula Hoop; training plus: Big Top Juggling, Bird’s-Eye Bulls-Eye, Rhythm Kung Fu, Rhythm Parade (+5 other activities that were not explicitly named) | Physical Fitness (back strength, handgrip, leg strength, sit-and-reach, single leg stance test), body composition (bioimpedancemetry), fatigue (analogue scale) | Significant improvements were noted for physical fitness, body composition and fatigue in the Wii Fit group but not the control group, suggesting that this software could be used for health promotion program in hemodialysis patients Adverse events: No |
| Kim et al. (2014), Korea | Middle-aged women with lower back pain (N = 30) Mean age: 47 years |
Intervention (RCT) Two groups: Wii Fit vs. traditional therapy Duration: four weeks (30 min, three sessions/week) Location: not specified |
Yoga: Chair, Deep Breathing, Half Moon, Palm Tree, Sun Salutation (supposedly), Tree, Warrior | Pain (visual analogue scale, pressure algometry), disability (ODI, RDQ, FABQ) | Both interventions induced lower pain and self-perceived disability. Wii Fit induced significantly higher improvements for all outcomes except for deep tissue mechanical pain sensitivity (pressure algometry) Adverse event: No |
| Drug dependency problems | |||||
| Cutter et al. (2014), USA | Opioid- or cocaine-dependent subjects (F/M, N = 17/12) Mean age: 43 ± 9 years |
Intervention (RCT) Two groups: Wii Fit vs. sedentary video games Duration: eight weeks (20–25 min, five sessions/week) Location: Drug rehabilitation center |
For each session, subjects were invited to choose, two aerobics activities, one yoga activity, one balance activity and one strength activity | Acceptability (attendance, four-item questionnaire), physical activity (in-session energy expenditure, IPAQ-L), substance use (diary, urine toxicology screening), well-being (PSS, BLSS, LOT) | Both interventions showed high level of acceptability, decreased substance use and increased well-being. Wii Fit participants reported high level of MVPA at the end of the intervention period Adverse events: No |
| Cancer patients (fatigue management) | |||||
| Hoffman et al. (2013)2, USA | Post-surgical non-small lung cancer patients (F/M, N = 5/2) Age range: 53–73 years Mean age: 65 ± 7 years |
Intervention (phase 1, cf. phase 2 below) One group Duration: six weeks (5–30 min “walking with the Wii” (see elsewhere) + 3–4 Wii Fit balance activities, five sessions/week) Location: Home |
Aerobics: “walking with the Wii” (might described an aerobics—Free Run—activity played by walking instead of running); balance: Ski Slalom, Soccer Heading; Training Plus: Driving Range; and “other activities” | Acceptability (questionnaire), fatigue (BFI), Fatigue management (PSEFSM), balance and functional mobility (ABC, self-efficacy for walking duration instrument, step-count) and adherence (playing time) | Patients adhered to the Wii Fit intervention, which was rated as acceptable. Perceived efficacy for balance and functional mobility increased, perceived fatigue decreased, and perceived self-efficacy for fatigue self-management increased (No statistics however). Light intensity home-based exertion delivered via a game console was effective for fatigue self-management in cancer patients Adverse events: No |
| Hoffman et al. (2014)2,USA | Same as for phase 1 (cf. above) | Intervention (phase 2, cf. phase 1 above) One group Duration: 10 weeks (30 min “walking with the Wii” (see elsewhere) + 3–4 Wii Fit balance activities, five sessions/week) Location: Home Note: phase 1 and phase 2 together: 16-week intervention |
Same as for phase 1 (cf. above) | Same as for phase 1 (cf. above) | Positive outcomes noted at the end of phase 1 (cf. the above) were maintained or reinforced at the end of the phase 2. Light intensity home-based exertion delivered via a game console was effective for fatigue self-management in cancer patients (even for those undergoing an adjuvant therapy) for a period as long as 16 weeks at least. Adverse events: No ABC (no unit): Wii Fit group Pre-intervention: 72.8 ± 20.5 Post-intervention: 88.9 ± 24.8 |
| Systemic lupus erythematosus | |||||
| Yuen et al. (2011), USA | African American women with systemic lupus erythematosus (N = 15) Age range: 25–67 years Mean age: 47 ± 14 years |
Intervention One group Duration: 10 weeks (30 min, two sessions/week) Location: Home |
Yoga, strength and aerobics activities |
Primary: fatigue (FSS) Secondary: anxiety level, pain intensity, body composition, step-count, physical fitness, adherence |
Fatigue, anxiety and pain were reduced. Body composition and physical fitness improved. Good adherence Adverse events: No |
| Seniors | |||||
| Chan et al. (2012), China | Elderly referred for rehabilitation (F/M, N = 22/8, 13 of them having acquired neurological disorders) Mean age: 80 ± 7 years |
Intervention One group (+comparison with a historic pool of 60 patients) Duration: 5–9 weeks (10 min, 1–2 sessions/week, total of eight Wii Fit sessions) Location: Geriatric center |
Aerobics: 2P Run |
Primary: feasibility (Borg scale, HR), adherence (playing time), acceptability (questionnaire) Secondary: functional ability (FIM) |
Participants completed an average of 72 ± 7 min of Wii Fit during their 5–9-week rehabilitation period (instructions: about 80 min). No difference was noted in exertion rate between the Wii Fit activity and a traditional arm ergometer exercise. Wii Fit participants exhibited a higher improvement in functional abilities compared to historic controls and wanted to continue the game at home Adverse events: No |
| Daniel (2012), USA | Pre-frail elderly (F/M, N = 14/9) Mean age: 77 ± 5 years |
Intervention (RCT) Three groups: passive control vs. seated exercise training vs. Wii Fit + weight vest Duration: 15 weeks (45 min, three sessions/weeks) Location: Laboratory |
Not specified (supposedly, all activities included in Wii Fit and Wii Sports) | Physical fitness (SFT, CHAMPS) body composition, balance and functional mobility (ABC, LLFDI, 8-feet TUG), adherence (attendance) | Authors described an improvement in physical fitness and balance confidence in the Wii Fit group, but no statistical significance was indicated. Same attendance rate (86%) in both seated exercising and Wii Fit groups. Adverse events: No |
Notes:
%, Percentage; ABC, activities-specific balance confidence scale; BFI, brief fatigue inventory; BLSS, brief life satisfaction scale; BMI, body mass index; CESD, center for epidemiologic studies depression scale; CHAMPS, community healthy activities model program for seniors; COPD, chronic obstructive pulmonary disease; CRQ-SR, chronic respiratory questionnaire; CTSIB, clinical test of sensory interaction and balance; EE, energy expenditure; ESWT, endurance shuttle walk test; FABQ, fear avoidance beliefs questionnaire; FIM, functional independence measure; FFS, fatigue severity scale; HR, hear rate (beats/min); IMI, intrinsic motivation inventory; LLFDI, late life function and disability index; IPAQ-L, physical activity questionnaire-long version; LOT, life orientation test; METs, metabolic equivalent; MVPA, moderate-to-vigorous physical activity; PSEFSM, perceived self-efficacy for fatigue self-management; RPP, rate pressure product; PAID, problem areas in diabetes scale; sec, second; SEES, subjective exercise experience scale; SFT, senior fitness test; PA, physical activity; PACES, physical activity and exercise questionnaire; ODI, Oswestry low-back pain disability index; PSS, perceived stress scale; RDQ, Roland Morris disability questionnaire; SF-12, short form-12 health survey; SOT, sensory organization test; TD2M, type 2 diabetes mellitus; TUG, time up and go; VPA, vigorous physical activity; VO2, oxygen consumption; VO2max, maximal oxygen consumption; WHO-5, five-item WHO well-being index.
For the same test, unit may vary from one paper to another.
When balance outcomes were included concomitantly with other outcomes, and were not described as a primary outcome alone, the study was only included in Table 3.
Hoffman et al. (2013, 2014) report results from two different phases of the same project.
Table 4. Wii Fit interventions for functional balance training.
| Authors (year), country | Population characteristics | Study design | Wii Fit activities (or other video games) | Outcomes and measures | Key findings and data used for the meta-analyses |
|---|---|---|---|---|---|
| Healthy young adults or middle-aged adults | |||||
| Gioftsidou et al. (2013), Greece | Healthy young adults (F/M, N = 18/22) Age range: 20–22 years Mean age: 20 ± 1 years |
Intervention (RCT) Two groups: Wii Fit vs. BOSU ball-based therapy Duration: eight weeks (14 min, two sessions/week) Location: Laboratory (supposedly) |
Balance: Balance Bubble, Penguin Slide, Snowboard Slalom, Ski Slalom, Soccer Heading, Table Tilt; Training plus: Balance Bubble Plus, Skateboard Arena, Table Tilt Plus | Balance (single leg stance tests1 and various indexes using Biodex system) | Balance improvements for both BOSU ball and Wii Fit intervention. Only one test (the balance board anterior-posterior single-limb stance test) showed greater improvement for the BOSU ball training Adverse events: No |
| Melong & Keats (2013), Canada | Healthy young adults (F/M, N = 12/8) Mean age: 20 ± 1 years |
Intervention (RCT) Two groups: Wii Fit vs. BOSU ball-based therapy Duration: four weeks (20 min, three sessions/week) Location: Laboratory |
Balance: Ski Jump, Ski Slalom, Soccer Heading, Table Tilt (+ a other activities played with the Wii Balance Board) |
Primary: adherence (attendance and playing time) Secondary: enjoyment (PACES), balance (stabilometry) |
Balance improvement were noted in both groups. While the Wii Fit group showed higher levels of enjoyment, this did not lead to a significantly higher attendance or playing time. This study may have been underpowered Adverse events: No |
| Lee, Lee & Park (2014), Korea | Healthy young adults (N = 24) Mean age: 20 ± 1 years |
Intervention (RCT) Two groups: Wii Fit vs. indoor horseback riding exercise Duration: six weeks (25 min, three sessions/week) Location: not specified (« indoor ») |
Balance: Balance Bubble, Ski Slalom, Table Tilt | Balance (dynamic tests using Biodex system: anteroposterior, mediolateral, and overall stability) | Both the Wii Fit and indoor horseback riding programs induce significant improvement in all three dynamic balance tests Adverse events: No |
| Cone, Levy & Goble (2015), USA | Healthy young adults (F/M, N = 16/24) Age range: 18–35 years Mean age: 23 ± 3 years |
Intervention (RCT) Two groups: Wii Fit vs. passive control Duration: six weeks (30–45 min, 2–4 sessions/week) Location: Laboratory (supposedly) |
Balance: Balance Bubble, Penguin Slide, Snowboard Slalom, Ski Slalom, Soccer Heading, Table Tilt, Tightrope Walk | Balance (SOT, LOF) | Significantly higher improvements in both LOS and SOT scores were noted for the Wii Fit group. Because those tests respectively focus on dynamic stability and sensory weighting, the results suggest that individuals with vestibular system alterations or dynamic balance control impairments may benefit from Wii Fit training Adverse events: No |
| Naumann et al. (2015), Germany | Healthy young adults (F/M, N = 29/8) Age range: 20–34 years Mean age: 23 ± 3 years |
Intervention (RCT) Three groups: Wii Fit vs. MFT Challenge Disc® vs. passive control Duration: four weeks (30 min, three sessions/week) + follow-up after four weeks Location: Laboratory (supposedly) |
Balance: Balance Bubble, Ski Slalom, Snowboard Slalom, Table Tilt | Balance (game scores, single- or two-leg stance COP excursion) | The performance on trained games increased in both intervention groups. No changes were noted for the COP excursion tests. Similarly, the Wii Fit group did not show any increase in MFT Challenge Disc® scores, and vice-versa. These data suggest that the training effect of Wii Fit was highly specific and may not be transferred to real life balance-related tasks Adverse events: No |
| Healthy seniors | |||||
| Williams et al. (2011), USA | Elderly (F/M, N = 18/4) Age range: 74–84 years Mean age: 84 ± 5 years |
Intervention One group Duration: four weeks (20 min, one session/week) Location: Geriatric center-based |
Balance and aerobics activities | Balance (BBS) |
Wii Fit induced improvement in balance skills. The post-intervention BBS scores (49 ± 5) were significantly higher than pre-intervention scores (39 ± 6) Adverse events: No BBS (no unit): Wii Fit group Pre-intervention: 39.41 ± 6.28 Post-intervention: 48.55 ± 4.58 |
| Bateni (2012), USA | Elderly (F/M, N = 9/8) Age range: 53–91 years Mean age: 73 ± 14 years |
Intervention (RCT) Three groups: Wii Fit vs. Wii Fit + traditional physical therapy vs. traditional physical therapy alone Duration: four weeks (15 min—estimation, three sessions/week) Location: Rehabilitation center |
Balance: Balance Bubble, Ski Jump, Ski Slalom; training plus: Table Tilt plus | Balance (BBS and Wii Fit Balance Bubble score) | Improvements in both BBS and Balance Bubble score in all three groups were observed. However, subjects who underwent traditional therapy exercises performed better at the BBS compared to subjects who only play Wii Fit alone Adverse events: No |
| Franco et al. (2012), USA | Elderly (F/M, N = 25/7) Mean age: 78 ± 6 years |
Intervention (RCT) Three groups: Wii Fit + strength training vs. traditional balance training vs. passive control Duration: three weeks (10–15 min, two sessions/week) Location: Community dwelling |
Balance: Ski Jump, Ski Slalom, Soccer Heading, Table Tilt, Tightrope Walk | Balance and gait (BBS, Tinetti test), functional health and well-being (SF-36), enjoyment (home-made questionnaire) and adherence (playing time) |
Wii Fit did not induce any balance and gait improvements. Same outcomes were observed in the traditional training group. Subjects playing Wii Fit reported high level of enjoyment. Adverse events: No BBS (no unit): Wii Fit group Pre- and post-intervention delta: 3.55 ± 5.03 Traditional therapy group Pre- and post-intervention delta: 3.45 ± 2.50 |
| Orsega-Smith et al. (2012), USA | Elderly (F/M, N = 30/4) Age range: 55–86 years Mean age: 72 ± 8 years |
Intervention (No-RCT) Three groups: playing Wii Fit for four weeks vs. playing Wii Fit for eight weeks vs. passive controls Duration: four or eight weeks (30 min, two sessions/week) Location: Community dwelling |
Yoga: Deep Breathing, Half Moon, Palm Tree; aerobics: Hula Hoop; balance: Balance Bubble, Penguin Slide, Snowboard Slalom, Ski Jumping, Ski Slalom, Table Tilt | Balance (BBS), mobility (8-feet TUG), leg strength (STST2), balance confidence (ABC, FES), autonomy (ADL) | Balance, and ability to complete activities of daily living were improved in the two Wii Fit groups. Leg strength increased in the four-week intervention group only, while balance confidence increased in the eight-week intervention group only. No change was noted in the control group Adverse events: No ABC (no unit): Wii Fit group (A: four-week) Pre- and post-intervention delta: 3.20 ± 13.88 Wii Fit group (B: eight-week) Pre- and post-intervention delta: 6.07 ± 7.04 BBS (no unit): Wii Fit group (A: four-week) Pre- and post-intervention delta: 1.44 ± 2.34 Wii Fit group (B: eight-week) Pre- and post-intervention delta: 1.22 ± 1.09 |
| Rendon et al. (2012), USA | Elderly (F/M, N = 26/14; six using an assistive devise) Age range: 60–95 years Mean age: 85 ± 5 years |
Intervention (RCT) Two groups: Wii Fit vs. passive control Duration: six weeks (35–45 min, three sessions/week) Location: Community dwelling |
Strength: Lunge, Single Leg Extension, Single Leg Twist |
Primary: balance (ABC, 8-feet up and go test) Secondary: depression (GDS) |
Wii Fit improved dynamic balance and balance confidence. No effect on depression score Adverse events: No |
| Toulotte, Toursel & Olivier (2012), France | Elderly (some had an history of falling; F/M, N = 22/14) Age range: >60 years Mean age: 75 ± 10 years |
Intervention (RCT) Four groups: passive control vs. Wii-Fit, adapted physical activities vs. Wii Fit + adapted physical activities Duration: 20 weeks (60 min, one session/week) Location: Fitness room |
Yoga activities and some balance activities (Soccer Heading, Ski Jump, Ski Slalom, Tightrope Walk, and another activity identified as “game balls”) | Balance (static tests only: a single leg stance test1 and the Wii Fit balance test; static and dynamic test: Tinetti test) |
Wii Fit significantly improved static balance but not dynamic balance. The conventional adapted PA training improved both. Combining both interventions did not induce additional benefits Adverse events: No |
| Bieryla & Dold (2013), USA | Elderly (F/M, N = 10/2) Age range: 70–92 years Mean age: 82 ± 6 years |
Intervention (RCT) Two groups: Wii Fit vs. passive control Duration: three weeks (30 min, three sessions/week) + follow-up at four-week Location: Community dwelling (supposedly: “supervised”) |
Yoga: Chair, Half Moon, Warrior; aerobics: Torso Twists; balance: Ski Jump Soccer, Heading | Balance (BBS, TUG, FAB, functional reach test) and adherence (retention rate) | In the Wii Fit group, the retention rate was 4/6 at the four-week follow-up. The Wii Fit training induced an improvement in the BBS only Adverse events: No |
| Chao et al. (2013), USA | Assisted living residents (F/M, N = 5/2, three of them having acquired neurological disorders) Age range: 80–94 years Mean age: 86 ± 5 years |
Intervention One group Duration: eight weeks (30 min, two sessions/week) Location: Assisted living dwelling |
Yoga: Chair, Deep Breathing; strength: Lunge; aerobics: Basic Run; balance: Penguin Slide, Table Tilt | Balance and mobility (BBS, TUG, 6 min walk test, FES), perceived efficacy (SSE, OEE), acceptability (questionnaire), safety | The Wii Fit intervention was acceptable and safe, and induced significant improvements in BBS. Trends only (p = 0.06) were noted for improvement in other balance and mobility indexes Adverse events: No BBS (no unit): Wii Fit group Pre-intervention: 40.9 ± 8.5 Post-intervention: 45.1 ± 8.3 TUG (sec): Wii Fit group Pre-intervention: 19.4 ± 5.5 Post-intervention: 15.8 ± 5.1 |
| Janssen, Tange & Arends (2013), The Netherlands | Home nursing residents (F/M, N = 20/9, some had a history of falling) Average age: 65–90 years Mean age: 82 ± 9 years |
Intervention (No-RCT) Three groups: Wii Fit (without history of playing) vs. Wii Fit (with an history of playing) vs. passive control Duration: 12 weeks (10–15 min, two sessions/week) Location: Assisted living dwelling |
Table Tilt Plus (Training Plus) and two other games of participants’ choice |
Primary: balance (BBS) Secondary: physical activity (LASAPAQ) |
No significant balance improvements in either Wii Fit intervention groups. However, subjects increased their volume of physical activity by about 60 min/day Adverse events: No |
| Chao et al. (2014), USA | Assisted living resident (F/M, N = 24/8) Mean age: 85 ± 6 years |
Intervention (RCT) Two groups: Wii Fit vs. “education” semi-passive control Duration: four weeks (30 min, two sessions/week) Location: Assisted living dwelling |
Yoga: Chair, Deep Breathing; strength: Lunge; balance: Penguin Slide, Table Tilt; aerobics: Basic Run | Balance and physical function (BBS, TUG, 6 min walk test, FES, SEE), depression (GDS), quality of life (SF-8) | Significant improvements in balance related-function and depression parameters were found in the Wii Fit group only. Wii Fit might be considered as a potential activity for older adults in assisted living dwellings Adverse events: No BBS (no unit): Wii Fit group Pre-intervention: 40.53 ± 6.59 Post-intervention: 43.93 ± 6.34 TUG (sec): Wii Fit group Pre-intervention: 18.52 ± 5.60 Post-intervention: 15.27 ± 4.68 |
| Cho, Hwangbo & Shin (2014), Korea | Elderly (N = 32) Mean age: 78 ± 1 years |
Intervention (RCT) Two groups: Wii Fit vs. passive control Duration: eight weeks (30 min, three sessions/week) Location: not specified |
Balance: Balance Bubble, Ski Slalom, Table Tilt | Balance (Romberg test) | Significant improvements were noted in the Wii Fit group only Adverse events: No |
| Nicholson et al. (2015), Australia | Elderly (F/M, N = 14/27) Age range: 65–84 years Mean age: 75 ± 5 years |
Intervention (RCT) Two groups: Wii Fit vs. usual exercise Duration: six weeks (30 min, three sessions/week) Location: Community dwelling |
Balance: Penguin Slide, Ski Jump, Ski Slalom, Soccer Heading, Table Tilt, Tightrope Walk; training plus: Snowball Fight, Perfect 10 | Balance and mobility (TUG, functional reach tests, single leg stance test,1 STST,2 Icon-typed FES, walking speed), enjoyment (PACES), adherence (playing frequency) | The Wii Fit group showed more improvement compared to the control group for the followings: TUG, lateral reach, left-leg single leg stance test and gait speed. Interestingly, enjoyment increased during the intervention and the adherence was very high (average attendance: 17.5 out of 18 recommended sessions) Adverse events: exacerbations of lower back pain (N = 2) TUG (sec): Wii Fit group Pre- and post-intervention delta: −0.61 ± 0.79 Traditional therapy group Pre- and post-intervention delta: −0.14 ± 0.88 |
| Roopchand-Martin et al. (2015), Jamaica | Elderly (F/M, N = 26/7) Mean age: 70 ± 7 years |
Intervention One group Duration: six weeks (30 min, two sessions/week) Location: Community dwelling |
Yoga: Tree; balance: Balance Bubble, Penguin Slide, Snowboard Slalom, Soccer Heading, Table Tilt; training plus: Obstacle Course, Skateboard | Balance and function (BBS, MCTSIB, MDRT, SEBT) | Significant balance and functional improvements were noted at the end of the Wii Fit intervention (i.e. for BBS, MDRT, SEBT, but not for MCTSIB) Adverse events: No BBS (no unit): Wii Fit group Pre- and post-intervention delta: 1.54 ± 2.60 |
| Seniors presenting balance impairments | |||||
| Williams et al. (2010), UK | Elderly with an history of falling (N = 21) Mean age: 77 ± 5 years |
Intervention (RCT) Two groups: Wii Fit vs. standard care Duration: 12 weeks (two sessions/week) Location: Rehabilitation center |
Yoga: Deep Breathing; aerobics: Basic Step, Hula Hoop, Running activities; Balance: Ski Jump, Ski Slalom, Soccer Heading, Table Tilt, | Functional balance (BBS, Tinetti test), static balance (Wii Fit age test) Balance confidence (FES), acceptability (retention, playing frequency, interviews) | The intervention met a high rate of acceptability. Balance improved in the Wii Fit group only Adverse events: fall (N = 1, no injury) BBS (no unit): Wii Fit group Pre-intervention: 43.7 ± 9.5 Post-intervention: 44.8 ± 11.8 Traditional therapy group Pre-intervention: 36.3 ± 9.9 Post-intervention: 39.0 ± 10.2 |
| Agmon et al. (2011), USA | Elderly with balance impairment (F/M, N = 4/3) Age range: 78–92 years Mean age: 84 ± 5 years |
Intervention One group Duration: 13 weeks (30 min, three sessions/week) Location: Home |
Balance: Basic Step, Ski Slalom, Soccer Heading, Table Tilt |
Primary: Balance (BBS) Secondary: mobility (4 m walk test), enjoyment (PACES), feasibility (playing time), safety (interviews) |
The Wii Fit intervention increased balance and mobility. Some activities were more enjoyable than the others. Adherence was associated with enjoyment. Adverse events: hip and neck strain (N = 1 and 2, respectively) BBS (no unit): Wii Fit group Pre-intervention: 49.0 ± 2.1 Post-intervention: 53.0 ± 1.8 |
| Bainbridge et al. (2011), USA | Elderly with perceived balance deficit (F/M, N = 7/1) Age range: 65–87 years Mean age: 75 ± 8 years |
Intervention One group Duration: six weeks (30 min, two sessions/week) Location: Community dwelling |
Yoga: Half Moon, Warrior; Balance: Penguin Slide, Ski Jump, Ski Slalom, Soccer Heading, Table Title, Tightrope Walk | Balance (BBS, ABC, MDRT), COP excursion measurements and other parameters (ankle range of motion tests…) | No statistically significant changes, but four patients (over the six who finished the intervention) demonstrated improvements on the BBS, based on established clinical guidelines Adverse events: No |
| Jorgensen et al. (2013), Denmark | Elderly with perceived balance deficit (F/M, N = 40/18) Mean age: 75 ± 6 years |
Intervention (RCT) Two groups: Wii Fit vs. passive control Duration: 10 weeks (35 min, two sessions/week) Location: Community dwelling |
Balance: Penguin Slide, Ski Slalom, Table Tilt, Tightrope Walk; training plus: Perfect 10 |
Primary: strength (maximal voluntary contraction of leg extensors (MVC), Rate of Force Development (RFD), static balance (COP velocity moment) Secondary: mobility (TUG, STST2), balance confidence (FES), motivation (questionnaire) |
Compared to controls, the Wii Fit group exhibited increased strength after 10 weeks of training. Mobility and balance confidence parameters also showed an improvement in the Wii Fit group only. Motivation for Wii Fit training was found to be high. Adverse events: No TUG (sec): Wii Fit group Pre-intervention: 10.3 ± 3.8 Post-intervention: 9.0 ± 3.2 |
| Seniors with acquired neurological alterations | |||||
| dos Santos Mendes et al. (2012), Brazil | Patients with Parkinson’s disease (stages 1 and 2 on Hoehn & Yahr scale, N = 16) Mean age: 69 ± 8 years |
Intervention Two groups: patients vs. healthy controls, N = 11) Duration: seven weeks (20–30 min, two sessions/week) + follow-up after two months Location: Rehabilitation center (supposedly: « Overseen by a physiotherapist ») |
Strength: Single Leg Extension, Torso Twists; aerobics: Basic Step; balance: Penguin Slide, Soccer Heading, Table Tilt; training plus: Basic Run Plus, Obstacle Course, Rhythm Parade, Tilt City | Stability (functional reach test) and motor learning (score performed in the selected games before and after the intervention) | Seven of the 10 tested games induced the same learning in Parkinson’s disease patients compared with healthy subjects. These patients were also able to transfer and retained (+2-months follow-up) their learning on a similar but untrained functional task Adverse events: No |
| Esculier et al. (2012)3, Canada | Patients with Parkinson’s disease (F/M, N = 5/6) Age range: 48–80 years Mean age: 62 ± 11 years |
Intervention Two groups: patients vs. healthy controls, F/M, N = 4/5) Duration: six weeks (40 min, three sessions/week) Location: Home |
Yoga: Deep Breathing; aerobics: Hula-Hoop; balance: Balance Bubble, Penguin Slide, Ski Jump, Ski Slalom, Table Tilt | Functional balance and mobility (ABC, STST,2 TUG, Tinetti test, 10 m walk test, CBM), static balance (single leg stance test,1 COP excursion) | Improvements in every outcome (except for ABC) in the two groups. A home-based Wii Fit improved static and dynamic balance, mobility and functional abilities of people affected by Parkinson’s disease Adverse events: No |
| Pompeu et al. (2012), Brazil | Patients with Parkinson’s disease (stages 1 and 2 on Hoehn & Yahr scale, F/M, N = 15/17) Age range: 60–85 years Mean age: 67 ± 8 years |
Intervention (RCT) Two groups: Wii Fit vs. traditional balance training Duration: seven weeks (30 min, two sessions/week) + follow-up 60 days after Location: Rehabilitation center |
Strength: Single Leg Extension, Torso Twist; aerobics: Basic Step, Basic Run; balance: Penguin Slide, Soccer Heading, Table Tilt; training plus: Obstacle Course, Rhythm Parade, Tilt City |
Primary: performance in daily activities Secondary: balance (static: single leg stance test,1 dynamic: BBS), cognition (Montreal cognitive assessment) |
Same improvements in Wii Fit and traditional balance training groups (maintained at 60 days follow-up). No additional advantage for the Wii Fit group Adverse events: No BBS (no unit): Wii Fit group Pre- and post-intervention delta: 1.4 ± 2.6 Traditional therapy group Pre- and post-intervention delta: 1.1 ± 2.1 |
| Padala et al. (2012), USA | Patients with an history of mild Alzheimer’s Dementia (F/M, N = 16/6) Mean age: 80 ± 7 years |
Intervention (RCT) Two groups: Wii Fit vs. walking Duration: eight weeks (30 min, five sessions/week) Location: Assisted living center |
Yoga: Chair, Half moon, Sun Salutation Warrior; strength: Lunge, Single Leg Extension, Torso Twist; balance: Balance Bubble, Penguin Slide, Ski Jump, Ski Slalom, Soccer Heading, Table Tilt |
Primary: balance (BBS, TUG, Tinetti test) Secondary: functional ability (ADL and instrumental ADL), quality of life (quality of life in Alzheimer’s disease scale), cognition (mini mental state examination) |
Significant improvements for balance outcomes in the Wii Fit group only (trends for the walking group). No significant changes in other outcomes, except for quality of life (walking group only) Adverse events: No BBS (no unit): Wii Fit group Pre-intervention: 43.4 ± 8.9 Post-intervention: 47.5 ± 5.9 Traditional therapy group Pre-intervention: 41.3 ± 7.6 Post-intervention: 46.9 ± 6.3 TUG (sec): Wii Fit group Pre-intervention: 14.7 ± 7.2 Post-intervention: 14.3 ± 6.8 Traditional therapy group Pre-intervention: 14.9 ± 4.7 Post-intervention: 12.8 ± 3.2 |
| Barcala et al. (2013), Brazil | Hemiplegic stroke patients (F/M, N = 11/9) Age range: Mean age: 64 ± 14 years |
Intervention (RCT) Two groups: conventional therapy + Wii Fit vs. conventional therapy + balance training Duration: five weeks (30 min, two sessions/week) Location: Rehabilitation center |
Balance: Penguin Slide, Table Tilt, Tightrope Walk | Functional balance (BBS), static balance (stabilometry), functional mobility, independence (TUG, functional independence test) | Both groups showed significant improvements in all parameters. No statistical differences were noted between the two groups emphasizing the efficacy of the Wii Fit therapy for functional recovery in hemiplegic stroke patient Adverse events: No BBS (no unit): Wii Fit group Pre-intervention: 39.6 ± 6.43 Post-intervention: 41.9 ± 6.91 Traditional therapy group Pre-intervention: 37.2 ± 5.22 Post-intervention: 42.2 ± 4.8 TUG (sec): Wii Fit group Pre-intervention: 27.9 ± 8.22 Post-intervention: 24.3 ± 8.64 Traditional therapy group Pre-intervention: 28.1 ± 3.10 Post-intervention: 25.2 ± 2.78 |
| Mhatre et al. (2013), USA | Patients with Parkinson’s disease (stages 2.5 or 3 on Hoehn & Yahr scale, F/M, N = 6/4) Age range: 44–91 years Mean age: 67 years |
Intervention One group Duration: eight weeks (30 min, three sessions/week) Location: Rehabilitation center |
Balance: “marble tracking,” “skiing,” “bubble rafting” (possibly: Table Tilt, Ski Slalom and Balance Bubble) |
Primary: Balance (BBS; DGI; Sharpened Romberg; Wii Balance Board-assisted postural sway tests) Secondary: Balance (ABC) and depression (GDS) |
Significant improvements in BBS (3.3) and some other balance & gait outcomes, but not in balance confidence (ABC) or mood (GDS) Adverse events: No ABC (no unit): Wii Fit group Pre-intervention: 83.5 ± 5.3 Post-intervention: 82.5 ± 3.6 BBS (no unit): Wii Fit group Pre-intervention: 48.8 ± 3.2 Post-intervention: 52.1 ± 2.3 |
| Bower et al. (2014), Australia | Stroke inpatients (F/M, N = 13/17) Mean age: 64 ± 15 years |
Intervention (RCT) Two groups: Wii Fit balance training vs. Wii Sports upper limb training Duration: 2–4 weeks (45 min, three sessions/week) Location: Rehabilitation center |
A selection of 18 activities among the 66 activities proposed in the Wii Fit Plus software (including Deep Breathing, Ski Slalom, Basic Run and others…) |
Primary: adherence (retention, attendance, playing time), acceptability (recruitment rate, questionnaire), safety (questionnaire) Secondary: Balance (Step Test, Wii Balance Board Test), Functional autonomy (functional reach test, upper limb—motor assessment scale), mobility (TUG, STREAM), balance confidence (FES) |
The recruitment rate (21%), eligibility rate (86%), retention rate (90% and 70%, respectively, at two and four weeks) and adherence rate (99% and 87%) indicated that a Wii Fit intervention would be feasible in stroke inpatients. All the patients enjoyed the intervention, which was described as safe. However, trends only were noted for improvements in some of the balance tests. Adverse events: Falls (N = 4), no subsequent injury TUG (sec): Wii Fit group Pre- and post-intervention delta: −11.2 ± 10.3 |
| Esculier, Vaudrin & Tremblay (2014)3, Canada | Patients with Parkinson’s disease (stages 3.5 or more on Hoehn & Yahr scale, F/M, N = 3/5) Mean age: 64 ± 12 years |
Intervention Two groups: patients vs. healthy controls (F/M, N = 3/5) Duration: six weeks (40 min, three sessions/week) Location: Home |
A selection of balance and strength activities involving lower limb muscles (i.e. using semi-squats Positions) | Lower limb corticomotor excitability (transcranial magnetic stimulation) |
Wii Fit training improved lower limb corticomotor excitability in Parkinson’s patients. Depending on the experimental conditions, these improvements were similar or more important when compared to healthy subjects. Home-based interventions including visual feedbacks could be beneficial for functional improvement in Parkinson’s patients Adverse events: No |
| Goncalves et al. (2014), Brazil | Patients with Parkinson’s disease (stages 2–4 on Hoehn & Yahr scale, F/M, N = 8/7) Mean age: 69 ± 10 years |
Intervention One group Duration: seven weeks (40 min, two sessions/week) Location: Hospital (supposedly, not specified) |
Balance: Ski Jump, Ski Slalom, Soccer Header; aerobics: Free Step, Rhythm Boxing; training plus: Island Cycling, Rhythm Parade (supposedly), Segway Circuit (+2 other activities that were not explicitly named) |
Functional mobility (UPDRS, SE, FIM), gait (number of steps, walking speed) | The Wii Fit program induced gait improvement, but statistical significance was not indicated. Functional mobility was significantly improved (i.e., decrease in UPDRS score, and increase in SE and FIM scores) Adverse events: No |
| Hung et al. (2014), China | Chronic stroke patients (F/M, N = 10/18) Mean age: 54 ± 10 years |
Intervention (RCT) Two groups: Wii Fit vs. traditional weight-shift training Duration: 12 weeks (30 min, Two sessions/week) + follow-up at three months Location: rehabilitation center (supposedly: according to pictures, “supervised by an occupational therapist”) |
Yoga: Warrior; balance: Balance Bubble, Penguin Slide, Ski Slalom, Soccer Heading, Table Tilt; aerobics: Basic Step | Balance (a series of COP excursion tests, FES), function (forward reach, TUG), enjoyment (PACES) | At the end of the intervention, Wii Fit induced a higher increase in some COP excursion tests compared to the traditional weigh-shift training group. However, at a three-month follow-up, these effects were not maintained, while the traditional weight-shift group showed higher improvements. Both types of intervention showed significant improvements in balance and functional outcomes, and the enjoyment was higher in the Wii Fit group Adverse events: No TUG (sec): Wii Fit group Pre-intervention: 26.06 ± 12.05 Post-intervention: 20.88 ± 7.77 Traditional therapy group Pre-intervention: 29.45 ± 16.22 Post-intervention: 26.61 ± 12.92 |
| Liao et al. (2015), China | Patients with Parkinson’s disease (stages 1 to 2 on Hoehn & Yahr scale; F/M, N = 19/17) Mean age: 66 ± 7 years |
Intervention (RCT) Three groups: Wii Fit vs. traditional therapy vs. passive control Duration: six weeks (45 min, two sessions/week + follow-up after one month Location: Rehabilitation center (supposedly: “administrated by the same physical therapist”) |
Yoga (10 min): Chair, Sun Salutation, Tree; strength (15 min); balance (20 min): Balance Bubble, Soccer Heading, Ski Slalom, Table Tilt |
Primary: mobility (obstacle crossing performance tests measured with the Liberty system), dynamic balance (LOS) Secondary: balance (SOT, FES), mobility (TUG), quality of life (PDQ-39) |
When compared with the passive control group, Wii Fit induced significant increases for the mobility, balance and quality of life outcomes. Interestingly, movement velocity evaluated with LOS test showed significantly greater improvement in the Wii Fit group compared to traditional therapy. These results should encourage the implementation of Wii Fit activities in patients with Parkinson’s disease. Adverse events: No TUG (sec): Wii Fit group Pre- and post-intervention delta: −2.9 ± 2.2 Traditional therapy group Pre- and post-intervention delta: −1.1 ± 0.1 Passive control group Pre- and post-intervention delta: +0.7 ± 1.7 |
| Morone et al. (2014), Italy | Subacute stroke patients (N = 50) Mean age: 60 ± 10 years |
Intervention (RCT) Two groups: Wii Fit + traditional therapy vs. traditional balance exercises + traditional therapy Duration: four weeks (20 min, three sessions/week) + follow-up after one month Location: Rehabilitation center |
Balance: Balance Bubble, Ski Slalom; aerobics: Hula Hoop |
Primary: balance (BBS) Secondary: mobility (10 m walk test, functional ambulatory category), independency (Barthel index) |
Wii Fit was more effective than traditional balance exercises to improve balance and independency in subacute stroke patients. No significant differences were noted between groups for mobility outcomes (increase in both groups). Interestingly, benefits in balance ability were maintained one month after the intervention Adverse events: No |
| Omiyale, Crowell & Madhavan (2015), USA | Hemiparetic stroke patients (F/M, N = 4/6) Age range: 41–73 years Mean age: 67 ± 8 years |
Intervention One group Duration: three weeks (60 min, three sessions/week) Location: not specified, but “supervised by a physical therapist” |
Balance: Balance Bubble, Penguin Slide, Ski Slalom, Table Tilt, Tightrope Walk | Neural plasticity (interhemispheric symmetry through tibialis anterior corticomotor excitability using transcranial magnetic stimulation), balance, motor response and function (COP distribution and dynamic weight shifting, Soccer Heading’s score, BBS, TUG, and dual TUG, gait speed, ABC) | Interestingly, the Wii Fit intervention significantly improved the interhemispheric symmetry. Overall, but not for all parameters, patients also improved their balance abilities, motor responsiveness, and balance related functions. These results suggest that Wii Fit rehabilitation may be able to influence positively neural plasticity and functional recovery in chronic stroke patients Adverse events: No ABC (no unit): Wii Fit group Pre-intervention: 65.9 ± 13.49 Post-intervention: 73.4 ± 13.32 BBS (no unit): Wii Fit group Pre-intervention: 51.6 ± 5.97 Post-intervention: 53.6 ± 2.95 TUG (sec): Wii Fit group Pre-intervention: 21.0 ± 12.18 Post-intervention: 19.4 ± 9.10 |
| Yatar & Yildirim (2015), Cyprus/Turkey | Chronic stroke patients (F/M, N = 13/17) Mean age: 60 ± 14 years |
Intervention (RCT) Two groups: neurodevelopmental training + Wii Fit vs. neurodevelopmental training + progressive balance training Duration: four weeks (30 min, three sessions/week) Location: Rehabilitation center (supposedly) |
Balance: Balance Bubble, Ski Slalom, Soccer Heading |
Primary: static balance (Wii Balance Board-assisted postural sway tests), dynamic balance (BBS, DGI, functional reach test, TUG) Secondary: balance confidence (ABC, ADL) |
Primary and secondary outcomes increased in both Wii Fit and progressive balance training groups. The increment was statistically higher in the Wii Fit group for: DGI. Functional reach test and ABC. Large differences in baseline values between the two groups limits the interpretation Adverse events: No BBS (no unit): Wii Fit group Pre-intervention: 45.60 ± 5.26 Post-intervention: 50.33 ± 4.09 Traditional therapy group Pre-intervention: 39.60 ± 9.31 Post-intervention: 44.80 ± 7.48 TUG (sec): Wii Fit group Pre-intervention: 17.96 ± 7.77 Post-intervention: 16.17 ± 8.23 Traditional therapy group Pre-intervention: 26.36 ± 11.60 Post-intervention: 22.11 ± 11.88 |
| Orthopedic population | |||||
| Fung et al. (2012), Canada | Adult outpatients following knee replacement (F/M, N = 33/17) Mean age: 68 ± 11 years |
Intervention (RCT) Two groups: traditional therapy + Wii Fit vs. traditional therapy + additional lower limb exercise Duration: until discharge (≈six weeks, 15 min/session) Location: Rehabilitation center |
Yoga: Deep Breathing, Half Moon; Strength: Torso Twist; Aerobics: Hula Hoop; Balance: Balance Bubble, Penguin Slide, Ski Slalom, Table tilt, Tightrope Walk | Function (range of motion), 2 min walk test, LEFS), pain (NPRS), Balance confidence (ABC) and length of rehabilitation | From baseline to discharge, the improvements were similar between the two groups for all the outcomes. The Wii Fit intervention might induce higher improvement for the LEFS. But the study was not powerful enough to obtain significance Adverse events: No |
| Baltaci et al. (2013), Turkey | Young adults with anterior cruciate ligament reconstruction (N = 30) Mean age: 29 ± 5 years |
Intervention (RCT) Two groups: Wii vs. conventional rehabilitation Duration: 12 weeks (60 min, three sessions/week) Location: Rehabilitation center (supposedly) |
Not clear. Probably a combination of Wii Sports games (Bowling, Boxing) and Wii Fit activities (“skiing games,” “football,” “balance board”) | Balance (SEBT), function (functional squat test including coordination, proprioception, time response and strength measurements) | No difference between Wii Fit and conventional physical therapy. Wii Fit may be able to address rehabilitation goals for patients with anterior cruciate ligament reconstruction Adverse events: No |
| Sims et al. (2013), USA | Young active adults with an history of lower limb injury within one year (F/M, N = 16/12) Mean age: 22 ± 2 years |
Intervention (RCT) Three groups: Wii Fit, traditional balance training, passive control Duration: four weeks (15 min, three sessions/week) Location: Rehabilitation center |
Yoga: Chair, Half Moon, Tree; Balance: Balance bubble, Penguin Slide, Ski Slalom, Soccer Heading, Table Tilt; Strength: Lunge, Sideways Leg Lift, Single Leg Extension; Aerobics: Basic Step, Hula Hoop, Super Hula Hoop |
Primary: balance (static: Time to Boundary test, dynamic: SEBT) Secondary: function (LEFS) |
Wii Fit improved static balance to a larger extend than the traditional balance training. Dynamic balance was improved in all groups Adverse events: No |
| Punt et al. (2015), Switzerland | Adults ankle sprain patients (F/M, N = 39/51) Mean age: 34 ± 11 years |
Intervention (RCT) Three groups: Wii Fit vs. traditional balance training vs. passive control Duration: six weeks (30 min, two sessions/week) Location: Home |
Balance: Balance Bubble, Penguin Slide, Ski Slalom, Table Tilt | Function (FAAM), pain (visual analogue scale), time to return to sport, satisfaction (questionnaire) | Foot and ankle ability score increased and pain decreased in all groups. A Wii Fit intervention was as effective as traditional therapy or no therapy. In the Wii Fit group, the average time to return to sport was 27 ± 20 days and 82% of patients were satisfied Adverse events: No |
| Multiple sclerosis | |||||
| Brichetto et al. (2013), Italia | Patients with multiple sclerosis (F/M, N = 22/14) Mean age: 42 ± 11 years |
Intervention (RCT) Two groups: Wii Fit vs. traditional rehabilitation Duration: four weeks (60 min, three sessions/week) Location: Rehabilitation center |
Balance: Lotus Focus, Ski Slalom, Snowboard Slalom, Soccer Heading, Table Tilt, Tightrope Walk |
Primary: balance (BBS) Secondary: fatigue (MFIS), posture (stabilometry) |
More important balance improvements in the Wii Fit group. Fatigue was reduced and posture improved. A Wii Fit-based program might be more efficient than the standard rehabilitation procedure in multiple sclerosis patients Adverse events: No BBS (no unit): Wii Fit group Pre-intervention: 49.6 ± 4.9 Post-intervention: 54.6 ± 2.2 Traditional therapy group Pre-intervention: 48.7 ± 3.3 Post-intervention: 49.7 ± 3.9 |
| Nilsagård, Forsberg & von Koch (2013), Sweden | Patients with multiple sclerosis (F/M, N = 64/20) Mean age: 50 ± 11 years |
Intervention (RCT) Two groups: Wii Fit vs. passive control Duration: 6–7 weeks (30 min, two sessions/week) Location: Rehabilitation Center (“physical therapist supervised session”) |
Aerobics: Skateboard Arena Balance: Balance Bubble, Penguin Slide, Ski Slalom, Soccer Heading, Snowboard Slalom, Table Tilt, Tightrope Walk; Training plus: Balance Bubble plus, Perfect 10, Table Tilt Plus |
Primary: balance (TUG) Secondary: other functional tests (TUGcognitive, four square step test, 25-foot walk test, DGI, MSWS-12, ABC, STST2) |
Improvement in several balance-related outcomes for the Wii Fit group. However, same improvements were observed in the controls (because of spontaneous exercise). Wii Fit can be recommended in adults with multiple sclerosis Adverse events: No ABC (no unit): Wii Fit group Pre- and post-intervention delta: 5.0 ± 14.4 TUG (sec): Wii Fit group Pre- and post-intervention delta: −0.8 ± 2.4 |
| Prosperini et al. (2013), Italy | Patients with multiple sclerosis (F/M, N = 25/11) Mean age: 36 ± 9 years |
Intervention (cross-over RCT) Two groups: Wii Fit vs. passive control Duration: 12 weeks (30 min, five sessions/week) Location: Home |
Supposedly all balance activities included in Wii Fit Plus (for the 4 first weeks, patients were allowed to play Zazen, Table Tilt and Ski Slalom only) | Balance (COP excursion, four-step square test), mobility (25-foot walk test), self-perceived disability (MSIS-29) |
Wii Fit was effective in improving balance, mobility and self-perceived health status and quality of life Adverse events: knee pain (N = 2), lower back pain (N = 3) |
| Robinson et al. (2015), UK | Patients with multiple sclerosis (F/M, N = 38/18) Mean age: 52 ± 6 years |
Intervention (RCT) Three groups: Wii Fit vs. traditional therapy vs. passive control Duration: four weeks (40–60 min, two sessions/week) Location: Rehabilitation center |
Balance: Heading Soccer, Ski Slalom, Table Tilt, Tightrope Walk; Strength: Rowing Squats, Torso Twist; aerobics: Boxing, Hula Hoop, Advanced Steps (supposedly) |
Primary: balance (postural sway), gait (gait speed), acceptability (UTAUT, FSS) Secondary: self-perceived disability (MSWS-12, WHODAS) |
Balance but not gait was improved by both the Wii Fit and traditional therapy interventions. Wii Fit was acceptable and induced positive changes in self-perceived disability Adverse events: No |
| Spinal cord injury patients | |||||
| Wall et al. (2015), USA | Individuals with incomplete spinal cord injury (>1-year post-injury, M, N = 5) Age range: 50–64 years Mean age: 59 ± 5 years |
Intervention One group Duration: seven week (60 min, two sessions/week) + follow up after four weeks Location: Home or University (and “supervised”) |
Balance: Balance Bubble, Basic Run (or another running activity), Penguin Slide, Ski Slalom, Ski Jump, Tightrope Walk, Table Tilt; training plus: Island Bike, Obstacle Course, Segway Circuit | Walking ability (gait speed), balance (TUG, functional reach), well-being (SF-36) | Gait speed and functional reach tests score both significantly increased after the Wii Fit intervention and the effects were maintained at a four-week follow-up. However, the program failed to induce statistical improvements in wellness (SF-36) and TUG Adverse events: No |
| Children with developmental delay | |||||
| Salem et al. (2012), USA | Children with developmental delay (F/M, N = 18/22) Age range: 39–58 months Mean age: 49 ± 6 months |
Intervention (RCT) Two groups: Wii vs. passive control Duration: 10 weeks (30 min, two sessions/week) Location: Rehabilitation center |
Strength: Lunges, Single Leg Stance; aerobics: Basic Run, Basic Step, Hula Hoop; balance: Penguin Slide, Soccer Heading, Tightrope Walk; Wii Sports’ Baseball, Bowling and Boxing games were also used |
Primary: balance and gait (gait speed, TUG, single leg stance test,1 STST,2 TUDS, 2 min walk test) Secondary: grip strength (dynamometer) |
Wii Fit induced significant improvements for the single leg stance test and grip strength only Adverse events: No |
| Esposito et al. (2013), Italia | Children with migraine without aura (F/M, N = 32/39) Mean age: 9 ± 2 years |
Intervention Two groups: patients vs. healthy controls, F/M, N = 44/49) Duration: 12 weeks (30 min, three sessions/week) Location: Home |
A choice of 18 balance oriented Wii Fit Plus activities (e.g., Balance Bubble, Hula Hoop, Obstacle Course, Penguin Slide, Rhythm Activities, Segway Circuit, Snowboard Slalom, Skateboard Arena, Ski Jump, Ski Slalom, Soccer Heading, Table Tilt, Tilt City…) | Motor coordination (MABC), fine visuomotricity (Berry-VMI) | Three-month Wii Fit training in children with migraine without aura improved all parameters: motor coordination (including balance skills), and fine visuomotricity. Wii Fit could be used in this population to counterbalance associated developmental delays or other deleterious effects Adverse events: No |
| Ferguson et al. (2013), South Africa | Children with developmental coordination disorders (F/M, N = 22/24) Age range: 6–10 years Mean age: 8 ± 1 years |
Intervention Two groups: Wii Fit vs. established neuromotor task training Duration: six weeks (30 min, three sessions/week) Location: School |
A total of 18 of the Wii Fit games mimicking the act of cycling, soccer, skateboarding and skiing or played with the hand controller | Motor coordination (MABC), physical fitness (functional strength, strength measured with dynamometer, muscle power sprint test, 20 m shuttle run test, adherence | Motor performance improved in the two groups, but more important changes were noted in the traditional training group. The latter was also true for functional strength and cardiorespiratory fitness measurements. Adherence was near 100% in both groups. The choice of one or the other intervention may depend on resources and time constraints Adverse events: No |
| Hammond et al. (2014), UK | Children with developmental coordination disorders (F/M, N = 4/14) Age range: 7–10 years Mean age: 8 ± 1 years |
Intervention (cross-over RCT) Two groups: Wii Fit-regular motor training vs. regular motor training-Wii Fit Duration: four weeks (three sessions/week) Location: School |
A selection of nine Wii Fit games focusing on coordination and balance |
Childs: motor proficiency (BOT), self-perceived ability and satisfaction with motor task (coordination skills questionnaire) Parents: emotional and behavioral development (strengths and difficulties questionnaire) |
Wii Fit induced significant gains in motor proficiency and other outcomes for many, but not all the children. Including Wii Fit therapy for children with developmental disorders could be considered Adverse events: No |
| Mombarg, Jelsma & Hartman (2013), The Netherlands | Children with balance alterations (F/M, N = 6/23) Age range: 7–12 years Mean age: 10 ± 1 years |
Intervention (RCT) Two groups: Wii Fit vs. passive control Duration: six weeks (30 min, three sessions/week) Location: School |
A total of 18 activities identified as balance games (mainly from the balance and training plus categories: Ski Jump, Ski Slalom, Snowboard Slalom, Table Tilt, Obstacle Course, Segway Circuit, Skateboard Arena, Tilt City, Rhythm activities…) | Balance (MABC and BOT) | Significant improvements in the Wii Fit group. Effective intervention for children with poor motor development Adverse events: No |
| Jelsma et al. (2014), The Netherlands | Children with probable developmental coordination disorders and balance problems (F/M = 10/18) Age range: 71–136 months Mean age: 100 ± 15 months |
Intervention Two groups: Wii Fit vs. waiting period-Wii Fit Duration: six weeks (30 min, three sessions/week) Location: Laboratory (supposedly) |
A total of 18 “balancing activities” from the Wii Fit Plus software (not including Ski Slalom, which was used for test) | Motor coordination (MABC), balance (BOT, Ski Slalom), enjoyment (home-made scale) | A Wii Fit intervention significantly increased motor and balance skills in children with coordination disorders and balance problems. After six weeks of intervention, 20 children (out of 28) still rated Wii Fit as “super fun” and four as “fun” Adverse events: No |
| Children with cerebral palsy | |||||
| Ramstrand & Lygnegård (2012), Sweden | Children with hemiplegic or diplegic cerebral palsy (F/M, N = 10/8) Age range: 8–17 years Mean age: 13 ± 3 years |
Intervention (cross-over RCT) Two groups: Wii Fit-no intervention vs. no intervention-Wii Fit Duration: five weeks (>30 min, five sessions/week) Location: Home |
Balance: Balance Bubble, Ski Jump, Ski Slalom, Soccer Heading, Table Tilt, Tightrope Walk |
Primary: balance (modified SOT, reactive balance test, weight shift test) Secondary: adherence (playing time) |
No improvements after the Wii Fit intervention period. A 30 min home-based Wii Fit intervention was not effective to improve balance in children with cerebral palsy. Four children did not complete the required 30 min/day sessions Adverse events: No |
| Jelsma et al. (2013), South Africa | Children with spastic hemiplegic cerebral palsy (F/M, N = 6/8) Age range: 7–14 years Mean age: 11 ± 2 years |
Intervention (A-B) One group (cf. details in the paper) Duration: three weeks (25 min, four sessions/week) + follow-up after two months Location: Rehabilitation center |
Aerobics: Hula Hoop; balance: Balance Bubble, Penguin Slide, Snowboard Slalom, Slalom Ski, Soccer Heading | Balance (BOT), functional mobility (BOT and TUDS) | Balance score improved significantly (sustained at two months follow-up), but not the functional scores (BOT and TUDS). Ten children only preferred to play Wii Fit instead of conventional physiotherapy. Wii Fit may not be used in place of conventional therapy Adverse events: No |
| Tarakci et al. (2013), Turkey | Children with ambulatory cerebral palsy (F/M, N = 3/11) Mean age: 12 ± 3 years |
Intervention One group Duration: 12 weeks (40 min, two sessions/week) Location: Rehabilitation center |
Balance: Ski Slalom, Soccer Heading, Table Tilt, Tightrope Walk | Balance (single leg stance test,1 functional reach test, TUG, 6 min walk test) | Balance improved significantly (all outcomes) Adverse events: No TUG (sec): Wii Fit group Pre-intervention: 18.26 ± 8.95 Post-intervention: 14.57 ± 5.39 |
| Other populations with balance impairments | |||||
| Meldrum et al. (2015), Ireland | Patients with unilateral peripheral vestibular loss (F/M, N = 27/44) Mean age: 54 ± 15 years |
Intervention (RCT) Two groups: Wii Fit vs. traditional balance rehabilitation Duration: six weeks (15 min, five sessions/week) + follow-up after six months Location: Home |
Yoga: Deep Breathing, Palm Tree, Standing Knee, Tree Pose; strength: Sideways Leg Lift, Single Leg Extension; balance: Balance Bubble, Ski Slalom, Heading Soccer, Penguin Slide, Table Tilt; aerobics: Advanced Step, Basic Step, Free Step; training plus: Skateboard, Snowball Fight, Table Tilt Plus |
Primary: Gait (self-preferred gait speed) Secondary: gait parameters (various tests performed eyes open or close, including DGI), balance (ABC, SOT), dynamic visual acuity (computerized dynamic visual acuity system), self-perceived benefit (vestibular rehabilitation benefit questionnaire), mental health (Hospital Anxiety and depression Scale), adherence (diary) |
Both the Wii Fit and traditional balance training induced improvement in gait speed. No difference was noted between the two groups for gait parameters and other outcomes at the end of the intervention. Adherence was high for the two interventions but Wii Fit was described as more enjoyable Adverse events: low back pain (N = 1) ABC (no unit): Wii Fit group Pre-intervention: 64.82 ± 18.74 Post-intervention: 74.36 ± 21.25 |
Notes:
ABC, activities-specific balance confidence scale; BBS, Berg balance scale; BMI, body mass index; BOT, Bruininks-Oseretsky test; ADL, activities of daily living scale; CHAMPS, community healthy activities model program for seniors; CBM, community balance and mobility scale; COPD, chronic obstructive pulmonary disease; Beery-VMI, Beery visual-motor integration test; CRQ-SR, chronic respiratory questionnaire; CTSIB, clinical test of sensory interaction and balance; DGI, dynamic gait index; EE, energy expenditure; ESWT, endurance shuttle walk test; FAAB, foot and ankle ability measure; FAB, Fullerton advanced balance scale; FES, falls efficacy scale; FIM, functional independence measure; FSS, flow state scale; GDS, geriatric depression scale; HR, hear rate (beats/min); IMI, Intrinsic Motivation Inventory; LASAPAQ, LASA physical activity questionnaire; LEFS, lower extremity functional scale; LLFDI, late life function and disability index; LOS, limits of stability; MABC, movement assessment battery for children; MCTSIB, modified clinical test for sensory interaction in balance; MDRT, multidirectional reach test; METs, metabolic equivalent; MFIS, modified fatigue impact scale; MSIS-29, 29-item multiple sclerosis impact scale; MSWS-12, 12-items multiple sclerosis walking scale; MVC, maximal voluntary contraction of leg extensors; MVPA, moderate-to-vigorous physical activity; NPRS, numeric pain rating scale; OEE, Outcome expectations for exercise scale; PA, physical activity; PACES, physical activity and exercise questionnaire; PAID, problem areas in diabetes scale; PDQ-39, 39-question Parkinson’s disease questionnaire; RFD, rate of force development; RPP, rate pressure product; SE, Schwab & England daily living activities scales; SEE, self-efficacy exercise scale; SEES, subjective exercise experience scale; SF-8, short form-8 health survey; SF-36, short form-36 health survey; SFT, senior fitness test; SOT, sensory organization test; STREAM, stroke rehabilitation assessment of movement; STST, sit-to-stand-test; TD2M, type 2 diabetes mellitus; TUDS, time up and down stairs; TUG, time up and go; UPDRS, unified rating scale for Parkinson’s disease; UTAUT, unified theory of acceptance and use of technology questionnaire; VPA, vigorous physical activity; VO2, oxygen consumption; VO2max, maximal oxygen consumption; WHO-5, five-item WHO well-being index; WHODAS, world health organization disability assessment schedule.
For the same test, unit may vary from one paper to another.
Many different single leg stance tests were used in the Wii Fit literature for balance assessment purposes. In this table “single leg stance test” describe any test requiring subjects to stand on one leg.
Many different sit-to-stand tests (STST) were used in the Wii Fit literature for balance, strength or functional assessment purpose. In this table, “STST” describes any test that requires the subject to sit and stand repeatedly.
Esculier et al. (2012) and Esculier, Vaudrin & Tremblay (2014) report results obtained with the same group of subjects during the same trial.
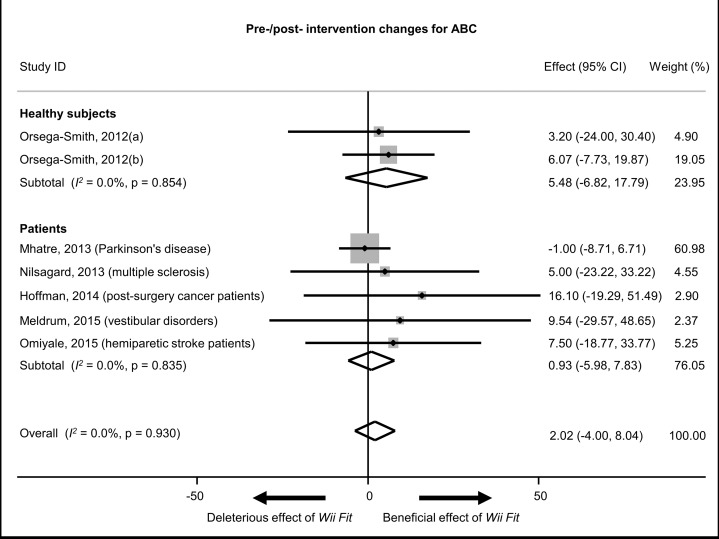
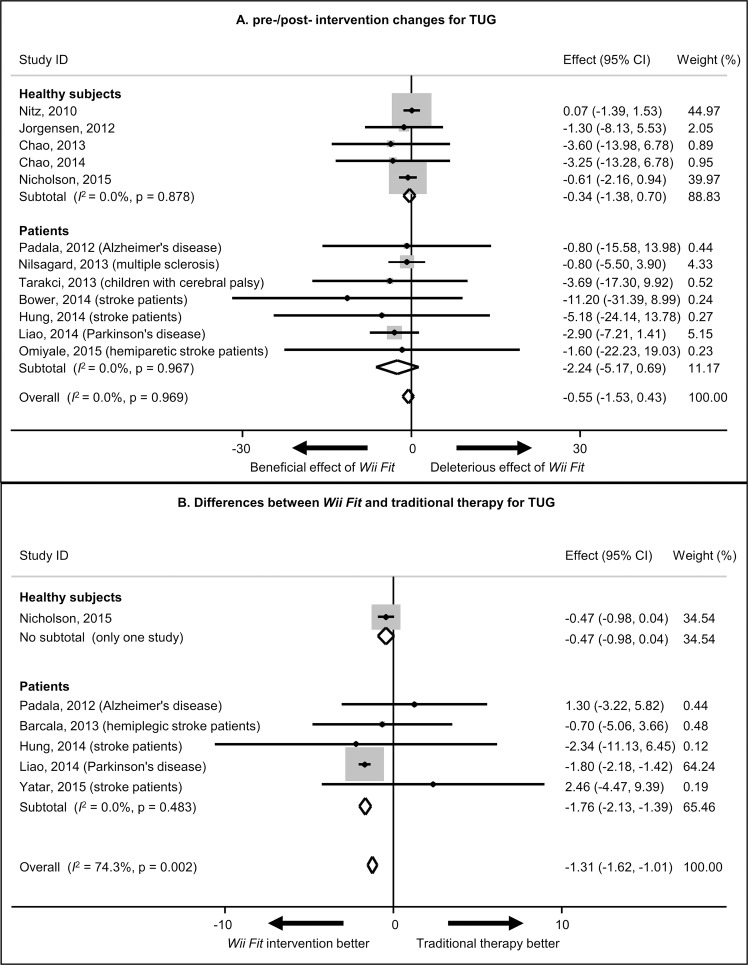
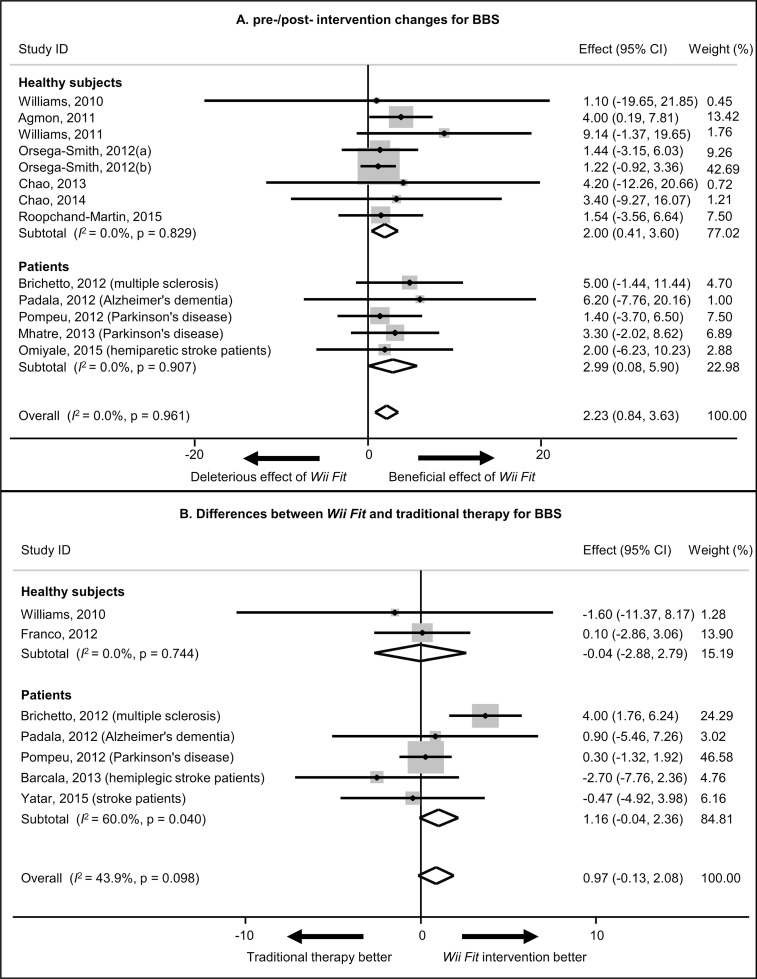
Goal 3: meta-analyses
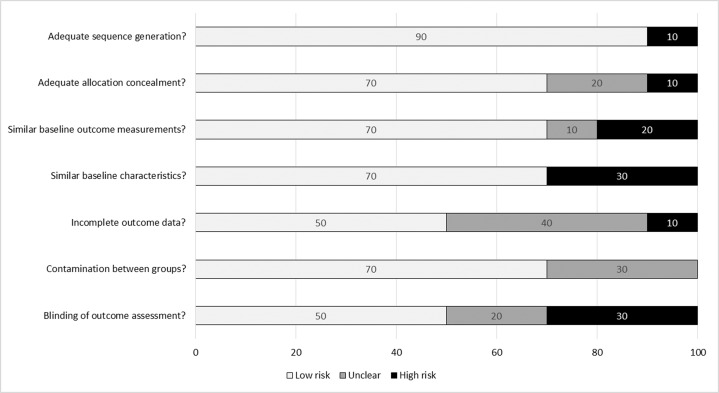
The effects of Wii Fit were quantified for selected health-related domains. The most recurrent outcomes noted were the activities-specific balance confidence test (ABC), Berg balance score (BBS) and the time-up-and-go test (TUG). These three tests are frequently used to assess patients’ balance abilities (Powell & Myers, 1995; Berg, 1989; Podsiadlo & Richardson, 1991). ABC is usually administered by a health care professional asking “How confident are you that you will not lose your balance or become unsteady when you…” for 16 different situations (e.g., “…walk around the house?,” “…walk up or down stairs”…). For each item, the participant should answer by expressing confidence in percentage (Powell & Myers, 1995). BBS is a scale able to measure balance in adults. The therapist asks participants to complete 14 different tasks (e.g., “sitting to standing,” “turning to look behind them”…) and evaluates each of them using a five-point score, ranging from 0 to 4 (Berg, 1989). TUG is a simple measure of the time taken by a subject to stand up from a chair, walk a distance of 3 m, turn, walk back to the chair, and sit down (time is expressed in seconds) (Podsiadlo & Richardson, 1991). Firstly, pre- and post-intervention meta-analyses were performed for each of these three outcomes. Secondly, Wii Fit vs. traditional therapy meta-analyses were completed, which only included results from randomized control (RCT) or two-arm trials. The exclusion criteria applied at this stage are described in Table 1. Only studies that used the 3 m version of the TUG test were included. Groups submitted to a combination of Wii Fit activities and more traditional therapy exercises were excluded from the pre- and post-intervention meta-analysis (Barcala et al., 2013; Daniel, 2012; Yatar & Yildirim, 2015). The pre- and post-intervention effect was calculated for the three selected outcomes. These meta-analyses used the mean difference between the reported pre-intervention and post-intervention values. For the Wii Fit vs. traditional therapy meta-analyses, the difference between the pre- and post-Wii Fit intervention changes and the pre- and post-traditional intervention changes were used as inputs in the meta-analysis. The variance imputation methods described by Follmann et al. (1992) were used to estimate the standard deviations of effect size when the authors did not report them. Heterogeneity between studies was assessed using the homogeneity test. A fixed-effect model was used when the I2 statistic, which is the index of heterogeneity, was under 75%. Sub-analyses were conducted in patients and healthy subjects. For ABC, because only two studies included a comparison between Wii Fit and traditional therapy (Yatar & Yildirim, 2015; Meldrum et al., 2015), only the pre- and post-intervention meta-analysis was performed. The risk of bias in each individual study included in the Wii Fit vs. traditional therapy meta-analysis was also assessed (Fig. 2). Meta-regression analyses were performed to assess the impact of intervention duration and volume (i.e., session duration × number of session) on ABC, BBS and TUG. p < 0.05 indicates statistical significance. Meta-analysis was performed using STATA 12.1 (StataCorp, College Station, TX, USA).
Figure 2. Assessment of risk of bias in individual studies included in the Wii Fit vs. traditional therapy meta-analyses.
The absence of ABC, BBS or TUG excluded de facto the studies from the meta-analyses. Therefore the usually reported “reporting bias” was not included in this assessment. No “other bias” was identified.
Results
The literature search provided a total of 279 references of interest (Fig. 1). Following the title and abstract screening process 138 studies were discarded, as they did not meet the selection criteria. One article was not accessible so was also discarded at this stage. An additional 25 references were removed after reading the full-text. Finally, 115 studies were included in the qualitative analysis, covering an approximately six-year period from July 2009 to June 2015.
Goal 1: health domains and populations of interest
The 115 selected studies focused on Wii Fit as a novel tool to improve physical function, fitness or health status. The content of the 115 articles was used to determine the different health domains in which Wii Fit may have potential benefits (Table 2).
Goal 2: systematic review of Wii-Fit interventions
From the 115 selected Wii Fit articles, 68 were intervention studies and met the selection criteria for inclusion in the systematic qualitative review. Overall, these studies involved 2,183 participants from both sexes (females: 1,161, males: 844, not specified: 178), with a wide age range (49 ± 6 months to 86 ± 6 years (Salem et al., 2012; Chao et al., 2013)), and various medical conditions. Primary and secondary outcomes, intervention content, as well as observation period vary from study to study. The intervention durations vary from 2 to 20 weeks (Bower et al., 2014; Toulotte, Toursel & Olivier, 2012), frequencies from 1 to 7 sessions per week (respectively, Toulotte, Toursel & Olivier, 2012; Chan et al., 2012 and Tripette et al., 2014b; Kempf & Martin, 2013) and session time from 10 to 60 min (respectively, Janssen, Tange & Arends, 2013; Franco et al., 2012 and Baltaci et al., 2013; Brichetto et al., 2013; Toulotte, Toursel & Olivier, 2012).
Six papers reported adverse effects: In young adults, light to moderate adverse effects (muscle soreness, pain, sprain, etc.) were observed (Tripette et al., 2014a). Among seniors, hip strain, neck strain, lower back pain as well as one fall were reported (Nicholson et al., 2015; Williams et al., 2010; Agmon et al., 2011). In multiple sclerosis patients, knee pain and lower back pain were also reported (Prosperini et al., 2013). Bower et al. (2014) observed a relatively high rate of falls in stroke patients (four events over a group of 30 patients).
Table 3 describes the characteristics and main results from studies with a primary focus on the effects of Wii Fit interventions on physical activity level, physical fitness or patients’ health status. Among 13 studies, 10 observed positive effects (Janssen, Tange & Arends, 2013; Daniel, 2012; Tripette et al., 2014b; Cutter et al., 2014; Albores et al., 2013; Kempf & Martin, 2013; Cho & Sohng, 2014; Kim et al., 2014; Hoffman et al., 2013, 2014; Chan et al., 2012) and three presented more contrasted results (Owens et al., 2011; Nitz et al., 2010; Albores et al., 2013). Interestingly, four intervention studies were conducted in patients with chronic diseases. They all reported a significant improvement in health status and well-being (chronic obstructive pulmonary disease, type two diabetes mellitus, chronic kidney disease and lower back pain) (Albores et al., 2013; Kempf & Martin, 2013; Cho & Sohng, 2014; Kim et al., 2014). Two reports described Wii Fit interventions as both feasible and effective methods for improving the overall physical fitness, mobility and independence of senior subjects (Janssen, Tange & Arends, 2013; Daniel, 2012; Chan et al., 2012).
For each population, Table 4 summarizes study characteristics and the main results for protocols with a primary focus on the effect of Wii Fit intervention on balance activities and related physical functions. Overall, the qualitative review of these studies supports a positive effect of Wii Fit interventions on balance outcomes. Among the 55 studies, 50 observed a positive effect of Wii Fit on at least one parameter (Morone et al., 2014; Wall et al., 2015; Bieryla & Dold, 2013; Rendon et al., 2012; Bainbridge et al., 2011; Fung et al., 2012; Salem et al., 2012; Barcala et al., 2013; Yatar & Yildirim, 2015; Meldrum et al., 2015; Ferguson et al., 2013; Hammond et al., 2014; Mombarg, Jelsma & Hartman, 2013; Jelsma et al., 2013, 2014; Esposito et al., 2013; Tarakci et al., 2013; Gioftsidou et al., 2013; Melong & Keats, 2013; Lee, Lee & Park, 2014; Cone, Levy & Goble, 2015; Baltaci et al., 2013; Sims et al., 2013; Punt et al., 2015; Brichetto et al., 2013; Nilsagård, Forsberg & von Koch, 2013; Prosperini et al., 2013; Robinson et al., 2015; Hung et al., 2014; Omiyale, Crowell & Madhavan, 2015; Williams et al., 2011; Bateni, 2012; Orsega-Smith et al., 2012; Toulotte, Toursel & Olivier, 2012; Chao et al., 2013, 2014; Cho, Hwangbo & Shin, 2014; Nicholson et al., 2015; Roopchand-Martin et al., 2015; Williams et al., 2010; Agmon et al., 2011; Jorgensen et al., 2013; Esculier et al., 2012; dos Santos Mendes et al., 2012; Padala et al., 2012; Pompeu et al., 2012; Mhatre et al., 2013; Esculier, Vaudrin & Tremblay, 2014; Goncalves et al., 2014; Liao et al., 2015). There were numerous examples were balance-related parameters improved to a similar or even higher extent when using Wii Fit compared to traditional therapies (Morone et al., 2014; Fung et al., 2012; Barcala et al., 2013; Daniel, 2012; Yatar & Yildirim, 2015; Meldrum et al., 2015; Gioftsidou et al., 2013; Melong & Keats, 2013; Lee, Lee & Park, 2014; Baltaci et al., 2013; Sims et al., 2013; Punt et al., 2015; Brichetto et al., 2013; Duclos et al., 2012; Hung et al., 2014; Bateni, 2012; Toulotte, Toursel & Olivier, 2012; Nicholson et al., 2015; Jorgensen et al., 2013; Pompeu et al., 2012; Liao et al., 2015). Only five papers described contrasted results or expressed some reservations about the ability of the software to induce benefits in balance skills (Janssen, Tange & Arends, 2013; Ramstrand & Lygnegård, 2012; Naumann et al., 2015; Bower et al., 2014; Franco et al., 2012), with three of these studies being conducted in healthy populations (Janssen, Tange & Arends, 2013; Naumann et al., 2015; Franco et al., 2012).
Goal 3: outcomes of meta-analyses
For the pre- and post-intervention meta-analyses, seven groups out of six studies were included for ABC, 13 groups out of 12 studies for BBS, and 12 groups out of 12 studies for TUG. For the Wii Fit vs. traditional therapy meta-analyses, 14 groups out of seven studies for BBS, and 12 groups out of six studies for TUG. Studies included in the different meta-analyses involved 595 participants from both sexes (females: 332, males: 242, not specified: 21), with a wide age range (12 ± 3 to 86 ± 5 years (Tarakci et al., 2013; Chao et al., 2013)) and various medical conditions. Whilst these papers all included a measure of ABC, BBS or TUG, the interventions content and duration vary from study to study. The assessment of individual studies revealed a low risk of bias (Fig. 2). Detailed results for ABC, BBS and TUG are presented in Figs. 3–5, and data included in the meta-analyses appears in Tables 3 and 4. Wii Fit interventions did not induce any change in ABC (2.02, 95% CI: −4.01–8.04). For BBS, significant improvements were noted in both healthy subjects and patients (2.00, 95% CI: 0.41–3.60 and 2.99, 95% CI: 0.08–5.90, respectively; 2.23, 95% CI: 0.84–3.63, overall). In addition, there was no significant difference in changes induced by traditional training and those induced by Wii Fit, suggesting that Wii Fit was as valid as traditional training. Regarding TUG, no significant reduction was noted after the Wii Fit intervention in either healthy subjects or patients (−0.34 s, 95% CI: −1.38 to 0.70 and −2.24 s, 95% CI: −5.17 to 0.69, respectively; −0.55 s, 95% CI: −1.53 to 0.43, overall). However, compared to traditional training programs, the Wii Fit did induced a more significant reduction in TUG, especially in patients (−1.76, 95% CI [−2.13 to −1.39], in patients; −1.31, 95% CI [−1.62 to −1.01], overall). The sets of studies included in both BBS and TUG pre- and post-intervention meta-analyses were statistically homogenous (I2 = 0.0%, p = 0.961 and I2 = 0.0%, p = 0.969, respectively for the overall analysis). Various levels of heterogeneity were observed in the Wii Fit vs. traditional therapy meta-analyses (I2 = 60.0%, p = 0.040 for BBS in patients and I2 = 74.3%, p = 0.002 for TUG overall (Figs. 4 and 5), indicating some inconsistencies in the literature. This was expected, however, since different populations were included in the analyses.
Figure 3. Pre- and post-intervention meta-analytic effect for the activities-specific balance confidence test (ABC).
The black point shows the average change for each study. The diamonds describe the pooled values respectively for the change in healthy subjects, patients and the overall population. The vertical black line refers to no change. For each analysis (overall population) or sub-analysis (healthy subjects or patients), a significant effect is observed if the diamond does not touch the black line. The horizontal black line shows the 95% CI and the gray square shows the study weight in percentage. Four-week Wii Fit intervention group (a) and eight-week Wii Fit intervention group (b) (Orsega-Smith et al., 2012). I2: index of heterogeneity.
Figure 5. Pre- and post-intervention meta-analytic effect (A) and Wii-Fit vs. traditional therapy meta-analytic effect (B) for the time-up-and-go test (TUG).
(A) The black point shows the average change for each study. The diamonds describe the pooled values respectively for the change in healthy subjects, patients and the overall population. The vertical black line refers to no change. For each analysis (overall population) or sub-analysis (healthy subjects or patients), a significant effect is observed if the diamond does not touch the black line. (B) The black point shows the difference of effect between Wii Fit and traditional therapy for each study. The diamonds describe the pooled values respectively for the difference of effect in healthy subjects, patients and the overall population, the vertical black line refers to no difference between Wii Fit-induced change and traditional therapy-induced change. For each analysis (overall population) or sub-analysis (healthy subjects or patients), a significant difference is observed if the diamond does not touch the black line. (A and B) The horizontal black line shows the 95% CI and the gray square shows the study weight in percentage. I2: index of heterogeneity. Unlike ABC and BBS, which are scores, the TUG test results are expressed in time. A negative difference therefore indicates a higher performance.
Figure 4. Pre- and post-intervention meta-analytic effect (A) and Wii-Fit vs. traditional therapy meta-analytic effect (B) for the Berg balance score (BBS).
(A) The black point shows the average change for each study. The diamonds describe the pooled values respectively for the change in healthy subjects, patients and the overall population. The vertical black line refers to no change. For each analysis (overall population) or sub-analysis (healthy subjects or patients), a significant effect is observed if the diamond does not touch the black line. (B) The black point shows the difference of effect between Wii Fit and traditional therapy for each study. The diamonds describe the pooled values respectively for the difference of effect in healthy subjects, patients and the overall population. The vertical black line refers to no difference between Wii Fit-induced change and traditional therapy-induced change. For each analysis (overall population) or sub-analysis (healthy subjects or patients), a significant difference is observed if the diamond does not touch the black line. (A and B) The horizontal black line shows the 95% CI and the gray square shows the study weight in percentage. Four-week Wii Fit intervention group (a) and eight-week Wii Fit intervention group (b) (Orsega-Smith et al., 2012). I2: index of heterogeneity.
Meta-regression analyses revealed no significant results (not shown), suggesting no relationships between improvements in balance outcomes and intervention duration or volume.
Discussion
The three main goals set for this review were as follows:
Goal 1: Identify the health-related domains in which the Wii Fit series has been tested or used. A scientific database search was undertaken with reasoned exclusion criteria. We identified that the Wii Fit has been used for numerous health purposes and in various populations (Table 2). Balance training was identified as being the most recurrent topic in the literature and appears to be the field of predilection for the usage of the Wii Fit software. Another notable focus was the prevention of metabolic disorders as well as the improvement of health status in people with chronic disease.
Goal 2: Understand the effect of Wii Fit in the identified populations (cf. Goal 1). A qualitative systematic review of studies including Wii Fit interventions was performed, with particular attention given to health and physical activity outcomes. Wii Fit was employed to prevent falls, to induce functional improvements in seniors or in subjects presenting neurodegenerative diseases, to treat orthopedic populations, etc. (Table 4). Overall, the effects of using Wii Fit were mainly positive, with the software being recurrently described as being able to induce similar benefits to traditional therapies. In addition, Wii-Fit interventions were linked to an improvement of health status in several different patients types (diabetic subjects, cancer patients …), however its preventive effect remains to be demonstrated.
Goal 3: To conduct meta-analyses when possible to quantify the effect Wii Fit had on selected health-related domains. In regards to balance training, the results of meta-analyses revealed that Wii Fit interventions had a positive impact on BBS and TUG. Interestingly, Wii Fit interventions also appear very safe, with very low levels of injuries being reported.
Wii Fit for the prevention of metabolic disorders and health status improvement in patients
From light physical activity to moderate-to-vigorous physical activity, AVG elicit a wide range of intensities (Graves et al., 2010; O’Donovan, Roche & Hussey, 2014; Deutsch et al., 2011; Douris et al., 2012; Garn et al., 2012; Lyons et al., 2012; O’Donovan & Hussey, 2012; Tripette et al., 2014a, 2014b; Xian et al., 2014; Worley, Rogers & Kraemer, 2011; Guderian et al., 2010; Mullins et al., 2012; Peng, Lin & Crouse, 2011). However, it is difficult to state whether playing Wii Fit on a regular basis would allow one to meet the American College of Sports Medicine’s recommendations for physical activity or could induce beneficial effects on health. Intervention studies reviewed in this article indicate that playing Wii Fit is not a strategy to consider in young adults (and children) for the prevention of cardio-metabolic disease, because it does not induce any significant increase in physical activity or any improvement in physical fitness (Owens et al., 2011; Nitz et al., 2010). However, one study showed a significant and rapid weight loss during a Wii Fit intervention in postpartum women (Tripette et al., 2014b). Wii Fit may also be a promising tool to aid seniors in maintaining a healthy lifestyle. Intervention studies have reported an increase in physical activity (Janssen, Tange & Arends, 2013), physical fitness (Daniel, 2012) and functional skills (Chan et al., 2012). Playing Wii Fit also clearly appeared to be beneficial for various types of patients: Some studies have reported improvements to health status in chronic obstructive pulmonary disease, hemodialysis patients, diabetic subjects and cancer patients (Albores et al., 2013; Kempf & Martin, 2013; Cho & Sohng, 2014; Hoffman et al., 2013, 2014). While the preventive effects of Wii Fit remain to be demonstrated, the software may be of value in other clinical settings.
Wii Fit for balance training
Many of the intervention studies (55/68) were related to balance training or to the improvement of related functions, with a large majority of them (50/55, Table 4) describing a beneficial effect. The meta-analytic results supported these promising observations. Significant improvements were observed for BBS in both healthy subjects and patients, while a trend was noted for TUG improvements in patients. Interestingly, the meta-analyses also revealed no difference in improvements induced by traditional therapies and Wii Fit interventions for BBS, while TUG showed greater improvements following the Wii Fit intervention compared to after traditional therapy. Taken together, these outcomes suggest a possible therapeutic application for the software, with Wii Fit potentially being as valid as traditional training in some situations. However, a careful look at the qualitative analysis outcome (Table 4) mitigates the overall positive impression for some populations. For instance, Wii Fit intervention outcomes in children with cerebral palsy appeared somewhat contrasted, sometimes being successful (Tarakci et al., 2013), sometimes unsuccessful (Ramstrand & Lygnegård, 2012) or sometimes inducing improvements in some but not all of the parameters (Jelsma et al., 2013). In addition, BBS evaluates balance in isolated balance-related tasks, and TUG combines a limited set of very simple actions (standing-up, walking and sitting-down). Wii Fit-induced improvements were only observed in BBS score and TUG, in a clinical setting, and were not associated with improvements in self-confidence in balance abilities (no changes in ABC), therefore it is unclear whether these improvements can be transferred to activities that occur during daily-life and positively impact the quality of life. The general impressions about Wii Fit interventions are, however, currently positive. Our review should therefore encourage further research in order to assist physiotherapists and health professionals in their decision to incorporate the use of Wii Fit into their treatment regimes. Considering that contrasted observations do exist, prescribing Wii Fit should still be considered with caution.
Wii Fit therapeutic content and Wii Balance Board
It is unsurprising that Wii Fit has been the object of much attention among physical therapists. The specificities of the Wii Fit games taken together with the technical features of the Wii Balance Board tend to promote medial–lateral and anterior–posterior movements, mimicking exercises that are commonly used in physical rehabilitation programs (Levac et al., 2010; Michalski et al., 2012; Duclos et al., 2012). The board is composed of multiple pressure sensors able to work together to follow the displacement of the vertical projection of the center of gravity on the floor. Moreover, the device has been validated against the “gold standard” laboratory-grade force platform for assessing standing balance (Clark et al., 2010). In addition, high levels of adherence have frequently been reported in the reviewed studies (Tables 3 and 4). One may therefore hypothesize that key features of the Wii Fit are the ludic elements that promote adherence in individuals who are not interested in traditional training programs. However, Deutsch et al. (2011) emphasizes one limitation of the Wii Fit, which favors the “knowledge of results” rather than the “knowledge of performance” model, i.e., subjects focus on scores rather than on the quality of movements. This is an important finding, since this would limit the relevance of using Wii Fit at home without the supervision of a therapist checking the quality of movement. One difference with the traditional proprioceptive rehabilitation material is that the Wii Balance Board is unable to tilt. Medial–lateral and anterior–posterior displacements are the result of exteroceptive adaptive mechanisms triggered by visual and auditory feedback stimuli that depend on the game scenario.
Limitations
Firstly, the sub-analyses performed in patients included various pathologies. This was highlighted by the high level of heterogeneity between studies in the Wii Fit vs. traditional therapy meta-analyses (see I2 in Figs. 4B and 5B). While the overall meta-analyses described a positive effect, the results cannot be predictive of Wii Fit intervention-related changes in one specific population. This emphasizes the requirement for more research in order to determine the optimum usage of Wii Fit for each medical domain. Secondly, the attention given to AVG and other virtual reality devices for the purpose of promoting health has been constantly growing, even after the screening period of this review (July 2009 to June 2015). Therefore we encourage readers to also review the new literature on the subject.
Conclusion
Originally designed as a ludic health and fitness promotion software, the Wii Fit series grabbed the attention of physical therapists due to the panel of features favoring body movements. Initial promising observations encouraged physicians, from various medical fields, to test the Wii Fit software on numerous populations. The literature still remains contrasted on the preventive effects of Wii Fit on chronic diseases. However, Wii Fit interventions were shown to be effective for the improvement of health status in various types of patients (chronic obstructive pulmonary disease, hemodialysis, renal complications, diabetes, cancer, etc.). Our review identified that the most notable focus of Wii Fit interventions were balance training. The Wii Fit has indeed been successfully used to prevent falls or to induce functional improvements in a wide range of healthy or pathologic populations (e.g., seniors, subjects with neurodegenerative diseases, orthopedic patients, children with developmental delay, multiple sclerosis patients, etc.). Our meta-analysis supports the general positive impressions about Wii Fit, suggesting promising applications in a wide range of medical fields. The unexpected entry of a video game into the health device market could create innovative healthcare strategies, however, more research is required to validate these claims.
Supplemental Information
Funding Statement
This work was supported by the Fonds de recherche du Québec—Santé and the Japan Society for the Promotion of Science. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Additional Information and Declarations
Competing Interests
The authors declare that they have no competing interests.
Author Contributions
Julien Tripette conceived and designed the experiments, performed the experiments, analyzed the data, wrote the paper, prepared figures and/or tables, reviewed drafts of the paper.
Haruka Murakami performed the experiments, analyzed the data, prepared figures and/or tables, reviewed drafts of the paper.
Katie Rose Ryan performed the experiments, wrote the paper, reviewed drafts of the paper.
Yuji Ohta contributed reagents/materials/analysis tools, reviewed drafts of the paper.
Motohiko Miyachi conceived and designed the experiments, contributed reagents/materials/analysis tools, reviewed drafts of the paper.
Data Availability
The following information was supplied regarding data availability:
The work consists of a systematic review and a meta-analysis. No original data have been generated. The data used for the meta-analysis are reported in the tables in the manuscript.
References
- Agmon et al. (2011).Agmon M, Perry CK, Phelan E, Demiris G, Nguyen HQ. A pilot study of Wii Fit exergames to improve balance in older adults. Journal of Geriatric Physical Therapy. 2011;34(4):161–167. doi: 10.1519/jpt.0b013e3182191d98. [DOI] [PubMed] [Google Scholar]
- Albores et al. (2013).Albores J, Marolda C, Haggerty M, Gerstenhaber B, ZuWallack R. The use of a home exercise program based on a computer system in patients with chronic obstructive pulmonary disease. Journal of Cardiopulmonary Rehabilitation and Prevention. 2013;33(1):47–52. doi: 10.1097/hcr.0b013e3182724091. [DOI] [PubMed] [Google Scholar]
- Bainbridge et al. (2011).Bainbridge E, Bevans S, Keeley B, Oriel K. The effects of the Nintendo Wii Fit on community-dwelling older adults with perceived balance deficits: a pilot study. Physical & Occupational Therapy in Geriatrics. 2011;29(2):126–135. doi: 10.3109/02703181.2011.569053. [DOI] [Google Scholar]
- Ballaz et al. (2014).Ballaz L, Robert M, Parent A, Prince F, Lemay M. Impaired visually guided weight-shifting ability in children with cerebral palsy. Research in Developmental Disabilities. 2014;35(9):1970–1977. doi: 10.1016/j.ridd.2014.04.019. [DOI] [PubMed] [Google Scholar]
- Baltaci et al. (2013).Baltaci G, Harput G, Haksever B, Ulusoy B, Ozer H. Comparison between Nintendo Wii Fit and conventional rehabilitation on functional performance outcomes after hamstring anterior cruciate ligament reconstruction: prospective, randomized, controlled, double-blind clinical trial. Knee Surgery, Sports Traumatology, Arthroscopy. 2013;21(4):880–887. doi: 10.1007/s00167-012-2034-2. [DOI] [PubMed] [Google Scholar]
- Barcala et al. (2013).Barcala L, Grecco LAC, Colella F, Lucareli PRG, Salgado ASI, Oliveira CS. Visual biofeedback balance training using Wii Fit after stroke: a randomized controlled trial. Journal of Physical Therapy Science. 2013;25(8):1027–1032. doi: 10.1589/jpts.25.1027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bateni (2012).Bateni H. Changes in balance in older adults based on use of physical therapy vs the Wii Fit gaming system: a preliminary study. Physiotherapy. 2012;98(3):211–216. doi: 10.1016/j.physio.2011.02.004. [DOI] [PubMed] [Google Scholar]
- Berg (1989).Berg K. Measuring balance in the elderly: preliminary development of an instrument. Physiotherapy Canada. 1989;41(6):304–311. doi: 10.1093/gerona/50a.1.m28. [DOI] [Google Scholar]
- Bieryla & Dold (2013).Bieryla KA, Dold NM. Feasibility of Wii Fit training to improve clinical measures of balance in older adults. Clinical Interventions in Aging. 2013;8:775–781. doi: 10.2147/cia.s46164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bower et al. (2014).Bower KJ, Clark RA, McGinley JL, Martin CL, Miller KJ. Clinical feasibility of the Nintendo Wii™ for balance training post-stroke: a phase II randomized controlled trial in an inpatient setting. Clinical Rehabilitation. 2014;28:912–923. doi: 10.1177/0269215514527597. [DOI] [PubMed] [Google Scholar]
- Brichetto et al. (2013).Brichetto G, Spallarossa P, de Carvalho MLL, Battaglia MA. The effect of Nintendo® Wii® on balance in people with multiple sclerosis: a pilot randomized control study. Multiple Sclerosis Journal. 2013;19(9):1219–1221. doi: 10.1177/1352458512472747. [DOI] [PubMed] [Google Scholar]
- Chan et al. (2012).Chan TC, Chan F, Shea YF, Lin OY, Luk JKH, Chan FHW. Interactive virtual reality Wii in geriatric day hospital: a study to assess its feasibility, acceptability and efficacy. Geriatrics & Gerontology International. 2012;12(4):714–721. doi: 10.1111/j.1447-0594.2012.00848.x. [DOI] [PubMed] [Google Scholar]
- Chao et al. (2015).Chao YY, Lucke KT, Scherer YK, Montgomery CA. Understanding the Wii exergames use: voices from assisted living residents. Rehabilitation Nursing. 2015;14(10):216. doi: 10.1002/rnj.216. [DOI] [PubMed] [Google Scholar]
- Chao et al. (2014).Chao YY, Scherer YK, Montgomery CA, Wu YW, Lucke KT. Physical and psychosocial effects of Wii Fit exergames use in assisted living residents: a pilot study. Clinical Nursing Research. 2014;24:589–603. doi: 10.1177/1054773814562880. [DOI] [PubMed] [Google Scholar]
- Chao et al. (2013).Chao Y-Y, Scherer YK, Wu Y-W, Lucke KT, Montgomery CA. The feasibility of an intervention combining self-efficacy theory and Wii Fit exergames in assisted living residents: a pilot study. Geriatric Nursing. 2013;34(5):377–382. doi: 10.1016/j.gerinurse.2013.05.006. [DOI] [PubMed] [Google Scholar]
- Cho, Hwangbo & Shin (2014).Cho GH, Hwangbo G, Shin HS. The effects of virtual reality-based balance training on balance of the elderly. Journal of Physical Therapy Science. 2014;26(4):615–617. doi: 10.1589/jpts.26.615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cho & Sohng (2014).Cho H, Sohng KY. The effect of a virtual reality exercise program on physical fitness, body composition, and fatigue in hemodialysis patients. Journal of Physical Therapy Science. 2014;26(10):1661–1665. doi: 10.1589/jpts.26.1661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark et al. (2010).Clark RA, Bryant AL, Pua Y, McCrory P, Bennell K, Hunt M. Validity and reliability of the Nintendo Wii Balance Board for assessment of standing balance. Gait & Posture. 2010;31(3):307–310. doi: 10.1016/j.gaitpost.2009.11.012. [DOI] [PubMed] [Google Scholar]
- Cone, Levy & Goble (2015).Cone BL, Levy SS, Goble DJ. Wii Fit exer-game training improves sensory weighting and dynamic balance in healthy young adults. Gait & Posture. 2015;41(2):711–715. doi: 10.1016/j.gaitpost.2015.01.030. [DOI] [PubMed] [Google Scholar]
- Cummings & Duncan (2010).Cummings J, Duncan E. Changes in affect and future exercise intentions as a result of exposure to a regular exercise programme using the Wii Fit. Sport and Exercise Psychology Review. 2010;6:31–41. [Google Scholar]
- Cutter et al. (2014).Cutter CJ, Schottenfeld RS, Moore BA, Ball SA, Beitel M, Savant JD, Stults-Kolehmainen MA, Doucette C, Barry DT. A pilot trial of a videogame-based exercise program for methadone maintained patients. Journal of Substance Abuse Treatment. 2014;47(4):299–305. doi: 10.1016/j.jsat.2014.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daniel (2012).Daniel K. Wii-Hab for pre-frail older adults. Rehabilitation Nursing. 2012;37(4):195–201. doi: 10.1002/rnj.25. [DOI] [PubMed] [Google Scholar]
- del Corral et al. (2014).del Corral T, Percegona J, Seborga M, Rabinovich RA, Vilaro J. Physiological response during activity programs using Wii-based video games in patients with cystic fibrosis (CF) Journal of Cystic Fibrosis. 2014;13(6):706–711. doi: 10.1016/j.jcf.2014.05.004. [DOI] [PubMed] [Google Scholar]
- Deutsch et al. (2011).Deutsch JE, Brettler A, Smith C, Welsh J, John R, Guarrera-Bowlby P, Kafri M. Nintendo Wii sports and Wii Fit game analysis, validation, and application to stroke rehabilitation. Topics in Stroke Rehabilitation. 2011;18(6):701–719. doi: 10.1310/tsr1806-701. [DOI] [PubMed] [Google Scholar]
- dos Santos Mendes et al. (2012).dos Santos Mendes FA, Pompeu JE, Lobo AM, da Silva KG, de Paula Oliveira T, Peterson Zomignani A, Pimentel Piemonte ME. Motor learning, retention and transfer after virtual-reality-based training in Parkinson’s disease—effect of motor and cognitive demands of games: a longitudinal, controlled clinical study. Physiotherapy. 2012;98(3):217–223. doi: 10.1016/j.physio.2012.06.001. [DOI] [PubMed] [Google Scholar]
- Douris et al. (2012).Douris PC, McDonald B, Vespi F, Kelley NC, Herman L. Comparison between Nintendo Wii Fit aerobics and traditional aerobic exercise in sedentary young adults. Journal of Strength and Conditioning Research. 2012;26(4):1052–1057. doi: 10.1519/jsc.0b013e31822e5967. [DOI] [PubMed] [Google Scholar]
- Duclos et al. (2012).Duclos C, Miéville C, Gagnon D, Leclerc C. Dynamic stability requirements during gait and standing exergames on the Wii Fit system in the elderly. Journal of NeuroEngineering and Rehabilitation. 2012;9:28. doi: 10.1186/1743-0003-9-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Esculier et al. (2012).Esculier J-F, Vaudrin J, Beriault P, Gagnon K, Tremblay LE. Home-based balance training programme using Wii Fit with balance board for Parkinson’s disease: a pilot study. Journal of Rehabilitation Medicine. 2012;44(2):144–150. doi: 10.2340/16501977-0922. [DOI] [PubMed] [Google Scholar]
- Esculier, Vaudrin & Tremblay (2014).Esculier J-F, Vaudrin J, Tremblay LE. Corticomotor excitability in Parkinson’s disease during observation, imagery and imitation of action: effects of rehabilitation using Wii Fit and comparison to healthy controls. Journal of Parkinson’s Disease. 2014;4(1):67–75. doi: 10.3233/JPD-130212. [DOI] [PubMed] [Google Scholar]
- Esposito et al. (2013).Esposito M, Ruberto M, Gimigliano F, Marotta R, Gallai B, Parisi L, Lavano SM, Roccella M, Carotenuto M. Effectiveness and safety of Nintendo Wii Fit Plus™ training in children with migraine without aura: a preliminary study. Neuropsychiatric Disease and Treatment. 2013;9:1803. doi: 10.2147/ndt.s53853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferguson et al. (2013).Ferguson G, Jelsma D, Jelsma J, Smits-Engelsman B. The efficacy of two task-orientated interventions for children with developmental coordination disorder: neuromotor task training and Nintendo Wii Fit training. Research in Developmental Disabilities. 2013;34(9):2449–2461. doi: 10.1016/j.ridd.2013.05.007. [DOI] [PubMed] [Google Scholar]
- Follmann et al. (1992).Follmann D, Elliott P, Suh I, Cutler J. Variance imputation for overviews of clinical trials with continuous response. Journal of Clinical Epidemiology. 1992;45(7):769–773. doi: 10.1016/0895-4356(92)90054-q. [DOI] [PubMed] [Google Scholar]
- Forsberg, Nilsagård & Boström (2015).Forsberg A, Nilsagård Y, Boström K. Perceptions of using videogames in rehabilitation: a dual perspective of people with multiple sclerosis and physiotherapists. Disability and Rehabilitation. 2015;37(4):338–344. doi: 10.3109/09638288.2014.918196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Franco et al. (2012).Franco JR, Jacobs K, Inzerillo C, Kluzik J. The effect of the Nintendo Wii Fit and exercise in improving balance and quality of life in community dwelling elders. Technology and Health Care. 2012;20(2):95–115. doi: 10.3233/THC-2011-0661. [DOI] [PubMed] [Google Scholar]
- Fung et al. (2012).Fung V, Ho A, Shaffer J, Chung E, Gomez M. Use of Nintendo Wii Fit™ in the rehabilitation of outpatients following total knee replacement: a preliminary randomised controlled trial. Physiotherapy. 2012;98(3):183–188. doi: 10.1016/j.physio.2012.04.001. [DOI] [PubMed] [Google Scholar]
- Garn et al. (2012).Garn AC, Baker BL, Beasley EK, Solmon MA. What are the benefits of a commercial exergaming platform for college students? Examining physical activity, enjoyment, and future intentions. Journal of Physical Activity and Health. 2012;9(2):311–318. doi: 10.1123/jpah.9.2.311. [DOI] [PubMed] [Google Scholar]
- Getchell et al. (2012).Getchell N, Miccinello D, Blom M, Morris L, Szaroleta M. Comparing energy expenditure in adolescents with and without autism while playing Nintendo® Wii™ games. Games for Health Journal. 2012;1(1):58–61. doi: 10.1089/g4h.2011.0019. [DOI] [PubMed] [Google Scholar]
- Gioftsidou et al. (2013).Gioftsidou A, Vernadakis N, Malliou P, Batzios S, Sofokleous P, Antoniou P, Kouli O, Tsapralis K, Godolias G. Typical balance exercises or exergames for balance improvement? Journal of Back and Musculoskeletal Rehabilitation. 2013;26(3):299–305. doi: 10.3233/bmr-130384. [DOI] [PubMed] [Google Scholar]
- Goncalves et al. (2014).Goncalves GB, Leite MA, Orsini M, Pereira JS. Effects of using the Nintendo Wii Fit plus platform in the sensorimotor training of gait disorders in Parkinson’s disease. Neurology International. 2014;6(1):5048. doi: 10.4081/ni.2014.5048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gras, Hummer & Hine (2009).Gras LZ, Hummer AD, Hine ER. Reliability and validity of the Nintendo Wii Fit. Journal of CyberTherapy & Rehabilitation. 2009;2(4):329–336. [Google Scholar]
- Graves et al. (2010).Graves LE, Ridgers ND, Williams K, Stratton G, Atkinson GT. The physiological cost and enjoyment of Wii Fit in adolescents, young adults, and older adults. Journal of Physical Activity and Health. 2010;7(3):393–401. doi: 10.1123/jpah.7.3.393. [DOI] [PubMed] [Google Scholar]
- Griffin et al. (2013).Griffin M, Shawis T, Impson R, Shanks J, Taylor MJ. Comparing the energy expenditure of Wii Fit™-based therapy versus traditional physiotherapy. Games for Health Journal. 2013;2(4):229–234. doi: 10.1089/g4h.2012.0078. [DOI] [PubMed] [Google Scholar]
- Guderian et al. (2010).Guderian B, Borreson L, Sletten L, Cable K, Stecker T, Probst M, Dalleck LC. The cardiovascular and metabolic responses to Wii Fit video game playing in middle-aged and older adults. Journal of Sports Medicine and Physical Fitness. 2010;50(4):436–442. [PubMed] [Google Scholar]
- Hakim et al. (2015).Hakim RM, Salvo CJ, Balent A, Keyasko M, McGlynn D. Case report: a balance training program using the Nintendo Wii Fit to reduce fall risk in an older adult with bilateral peripheral neuropathy. Physiotherapy Theory and Practice. 2015;31(2):130–139. doi: 10.3109/09593985.2014.971923. [DOI] [PubMed] [Google Scholar]
- Hammond et al. (2014).Hammond J, Jones V, Hill EL, Green D, Male I. An investigation of the impact of regular use of the Wii Fit to improve motor and psychosocial outcomes in children with movement difficulties: a pilot study. Child: Care, Health and Development. 2014;40(2):165–175. doi: 10.1111/cch.12029. [DOI] [PubMed] [Google Scholar]
- Hoffman et al. (2013).Hoffman AJ, Brintnall RA, Brown JK, von Eye A, Jones LW, Alderink G, Ritz-Holland D, Enter M, Patzelt LH, VanOtteren GM. Too sick not to exercise: using a 6-week, home-based exercise intervention for cancer-related fatigue self-management for postsurgical non-small cell lung cancer patients. Cancer Nursing. 2013;36(3):175–188. doi: 10.1097/ncc.0b013e31826c7763. [DOI] [PubMed] [Google Scholar]
- Hoffman et al. (2014).Hoffman AJ, Brintnall RA, Brown JK, von Eye A, Jones LW, Alderink G, Ritz-Holland D, Enter M, Patzelt LH, VanOtteren GM. Virtual reality bringing a new reality to postthoracotomy lung cancer patients via a home-based exercise intervention targeting fatigue while undergoing adjuvant treatment. Cancer Nursing. 2014;37(1):23–33. doi: 10.1097/ncc.0b013e318278d52f. [DOI] [PubMed] [Google Scholar]
- Hung et al. (2014).Hung JW, Chou CX, Hsieh YW, Wu WC, Yu MY, Chen PC, Chang HF, Ding SE. Randomized comparison trial of balance training by using exergaming and conventional weight-shift therapy in patients with chronic stroke. Archives of Physical Medicine and Rehabilitation. 2014;95(9):1629–1637. doi: 10.1016/j.apmr.2014.04.029. [DOI] [PubMed] [Google Scholar]
- Jacobs et al. (2011).Jacobs K, Zhu L, Dawes M, Franco J, Huggins A, Igari C, Ranta B, Umez-Eronini A. Wii health: a preliminary study of the health and wellness benefits of Wii Fit on university students. British Journal of Occupational Therapy. 2011;74(6):262–268. doi: 10.4276/030802211x13074383957823. [DOI] [Google Scholar]
- Janssen, Tange & Arends (2013).Janssen S, Tange H, Arends R. A preliminary study on the effectiveness of exergame Nintendo “Wii Fit Plus” on the balance of nursing home residents. Games for Health Journal. 2013;2(2):89–95. doi: 10.1089/g4h.2012.0074z. [DOI] [PubMed] [Google Scholar]
- Jelsma et al. (2014).Jelsma D, Geuze RH, Mombarg R, Smits-Engelsman BC. The impact of Wii Fit intervention on dynamic balance control in children with probable developmental coordination disorder and balance problems. Human Movement Science. 2014;33:404–418. doi: 10.1016/j.humov.2013.12.007. [DOI] [PubMed] [Google Scholar]
- Jelsma et al. (2013).Jelsma J, Pronk M, Ferguson G, Jelsma-Smit D. The effect of the Nintendo Wii Fit on balance control and gross motor function of children with spastic hemiplegic cerebral palsy. Developmental Neurorehabilitation. 2013;16(1):27–37. doi: 10.3109/17518423.2012.711781. [DOI] [PubMed] [Google Scholar]
- Jorgensen et al. (2013).Jorgensen MG, Laessoe U, Hendriksen C, Nielsen OBF, Aagaard P. Efficacy of Nintendo Wii training on mechanical leg muscle function and postural balance in community-dwelling older adults: a randomized controlled trial. Journals of Gerontology Series A: Biological Sciences and Medical Sciences. 2013;68(7):845–852. doi: 10.1093/gerona/gls222. [DOI] [PubMed] [Google Scholar]
- Kempf & Martin (2013).Kempf K, Martin S. Autonomous exercise game use improves metabolic control and quality of life in type 2 diabetes patients-a randomized controlled trial. BMC Endocrine Disorders. 2013;13(1):57. doi: 10.1186/1472-6823-13-57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khan, Parvaiz & Vassallo (2012).Khan O, Parvaiz A, Vassallo D. Acute hernial strangulation following Wii Fit exercises. Acta Chirurgica Belgica. 2012;113(1):58–59. doi: 10.1080/00015458.2013.11680888. [DOI] [PubMed] [Google Scholar]
- Kim et al. (2014).Kim SS, Min WK, Kim JH, Lee BH. The effects of VR-based Wii Fit yoga on physical function in middle-aged female LBP patients. Journal of Physical Therapy Science. 2014;26(4):549–552. doi: 10.1589/jpts.26.549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laver et al. (2011).Laver K, Ratcliffe J, George S, Burgess L, Crotty M. Is the Nintendo Wii Fit really acceptable to older people?: A discrete choice experiment. BMC Geriatrics. 2011;11(1):64. doi: 10.1186/1471-2318-11-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LeBlanc et al. (2013).LeBlanc AG, Chaput JP, McFarlane A, Colley RC, Thivel D, Biddle SJ, Maddison R, Leatherdale ST, Tremblay MS. Active video games and health indicators in children and youth: a systematic review. PLOS ONE. 2013;8(6):e65351. doi: 10.1371/journal.pone.0065351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee, Lee & Park (2014).Lee D, Lee S, Park J. Effects of indoor horseback riding and virtual reality exercises on the dynamic balance ability of normal healthy adults. Journal of Physical Therapy Science. 2014;26(12):1903–1905. doi: 10.1589/jpts.26.1903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levac et al. (2010).Levac D, Pierrynowski MR, Canestraro M, Gurr L, Leonard L, Neeley C. Exploring children’s movement characteristics during virtual reality video game play. Human Movement Science. 2010;29(6):1023–1038. doi: 10.1016/j.humov.2010.06.006. [DOI] [PubMed] [Google Scholar]
- Liao et al. (2015).Liao YY, Yang YR, Cheng SJ, Wu YR, Fuh JL, Wang RY. Virtual reality-based training to improve obstacle-crossing performance and dynamic balance in patients with Parkinson’s disease. Neurorehabilitation and Neural Repair. 2015;29(7):658–667. doi: 10.1177/1545968314562111. [DOI] [PubMed] [Google Scholar]
- Liberati et al. (2009).Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JPA, Clarke M, Devereaux PJ, Kleijnen J, Moher D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLOS Medicine. 2009;6(7):e1000100. doi: 10.1371/journal.pmed.1000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lyons et al. (2012).Lyons EJ, Tate DF, Ward DS, Wang X. Energy intake and expenditure during sedentary screen time and motion-controlled video gaming. American Journal of Clinical Nutrition. 2012;96(2):234–239. doi: 10.3945/ajcn.111.028423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meldrum et al. (2012).Meldrum D, Glennon A, Herdman S, Murray D, McConn-Walsh R. Virtual reality rehabilitation of balance: assessment of the usability of the Nintendo Wii® Fit Plus. Disability and Rehabilitation: Assistive Technology. 2012;7(3):205–210. doi: 10.3109/17483107.2011.616922. [DOI] [PubMed] [Google Scholar]
- Meldrum et al. (2015).Meldrum D, Herdman S, Vance R, Murray D, Malone K, Duffy D, Glennon A, McConn-Walsh R. Effectiveness of conventional versus virtual reality-based balance exercises in vestibular rehabilitation for unilateral peripheral vestibular loss: results of a randomized controlled trial. Archives of Physical Medicine and Rehabilitation. 2015;96(7):1319–1328.e1. doi: 10.1016/j.apmr.2015.02.032. [DOI] [PubMed] [Google Scholar]
- Melong & Keats (2013).Melong C, Keats MR. Comparing the effects of a novel and a traditional proprioceptive balance training program on activity adherence and balance control in a healthy university population: a preliminary study. Games for Health Journal. 2013;2(5):308–312. doi: 10.1089/g4h.2013.0042. [DOI] [PubMed] [Google Scholar]
- Mhatre et al. (2013).Mhatre PV, Vilares I, Stibb SM, Albert MV, Pickering L, Marciniak CM, Kording K, Toledo S. Wii Fit Balance Board playing improves balance and gait in Parkinson disease. PM&R. 2013;5(9):769–777. doi: 10.1016/j.pmrj.2013.05.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michalski et al. (2012).Michalski A, Glazebrook C, Martin A, Wong W, Kim A, Moody K, Salbach NM, Steinnagel B, Andrysek J, Torres-Moreno R, Zabjek KF. Assessment of the postural control strategies used to play two Wii Fit™ videogames. Gait & Posture. 2012;36(3):449–453. doi: 10.1016/j.gaitpost.2012.04.005. [DOI] [PubMed] [Google Scholar]
- Miller et al. (2012).Miller CA, Hayes DM, Dye K, Johnson C, Meyers J. Using the Nintendo Wii Fit and body weight support to improve aerobic capacity, balance, gait ability, and fear of falling: two case reports. Journal of Geriatric Physical Therapy. 2012;35(2):95–104. doi: 10.1519/jpt.0b013e318224aa38. [DOI] [PubMed] [Google Scholar]
- Miyachi et al. (2010).Miyachi M, Yamamoto K, Ohkawara K, Tanaka S. METs in adults while playing active video games: a metabolic chamber study. Medicine & Science in Sports & Exercise. 2010;42(6):1149–1153. doi: 10.1249/MSS.0b013e3181c51c78. [DOI] [PubMed] [Google Scholar]
- Mombarg, Jelsma & Hartman (2013).Mombarg R, Jelsma D, Hartman E. Effect of Wii-intervention on balance of children with poor motor performance. Research in Developmental Disabilities. 2013;34(9):2996–3003. doi: 10.1016/j.ridd.2013.06.008. [DOI] [PubMed] [Google Scholar]
- Monteiro-Junior et al. (2014).Monteiro-Junior RS, Figueiredo LF, Conceicao I, Carvalho C, Lattari E, Mura G, Machado S, da Silva EB. Hemodynamic responses of unfit healthy women at a training session with Nintendo Wii: a possible impact on the general well-being. Clinical Practice and Epidemiology in Mental Health. 2014;10:172–175. doi: 10.2174/1745017901410010172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morone et al. (2014).Morone G, Tramontano M, Iosa M, Shofany J, Iemma A, Musicco M, Paolucci S, Caltagirone C. The efficacy of balance training with video game-based therapy in subacute stroke patients: a randomized controlled trial. BioMed Research International. 2014;2014:1–6. doi: 10.1155/2014/580861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mullins et al. (2012).Mullins NM, Tessmer KA, McCarroll ML, Peppel BP. Physiological and perceptual responses to Nintendo® Wii Fit™ in young and older adults. International Journal of Exercise Science. 2012;5(1):9. [PMC free article] [PubMed] [Google Scholar]
- Naumann et al. (2015).Naumann T, Kindermann S, Joch M, Munzert J, Reiser M. No transfer between conditions in balance training regimes relying on tasks with different postural demands: specificity effects of two different serious games. Gait & Posture. 2015;41(3):774–779. doi: 10.1016/j.gaitpost.2015.02.003. [DOI] [PubMed] [Google Scholar]
- Nicholson et al. (2015).Nicholson VP, McKean M, Lowe J, Fawcett C, Burkett B. Six weeks of unsupervised Nintendo Wii Fit gaming is effective at improving balance in independent older adults. Journal of Aging and Physical Activity. 2015;23(1):153–158. doi: 10.1123/japa.2013-0148. [DOI] [PubMed] [Google Scholar]
- Nilsagård, Forsberg & von Koch (2013).Nilsagård YE, Forsberg AS, von Koch L. Balance exercise for persons with multiple sclerosis using Wii games: a randomised, controlled multi-centre study. Multiple Sclerosis Journal. 2013;19(2):209–216. doi: 10.1177/1352458512450088. [DOI] [PubMed] [Google Scholar]
- Nitz et al. (2010).Nitz J, Kuys S, Isles R, Fu S. Is the Wii Fit™ a new-generation tool for improving balance, health and well-being? A pilot study. Climacteric. 2010;13(5):487–491. doi: 10.3109/13697130903395193. [DOI] [PubMed] [Google Scholar]
- O’Donovan et al. (2014).O’Donovan C, Greally P, Canny G, McNally P, Hussey J. Active video games as an exercise tool for children with cystic fibrosis. Journal of Cystic Fibrosis. 2014;13(3):341–346. doi: 10.1016/j.jcf.2013.10.008. [DOI] [PubMed] [Google Scholar]
- O’Donovan & Hussey (2012).O’Donovan C, Hussey J. Active video games as a form of exercise and the effect of gaming experience: a preliminary study in healthy young adults. Physiotherapy. 2012;98(3):205–210. doi: 10.1016/j.physio.2012.05.001. [DOI] [PubMed] [Google Scholar]
- O’Donovan, Roche & Hussey (2014).O’Donovan C, Roche E, Hussey J. The energy cost of playing active video games in children with obesity and children of a healthy weight. Pediatric Obesity. 2014;9(4):310–317. doi: 10.1111/j.2047-6310.2013.00172.x. [DOI] [PubMed] [Google Scholar]
- Omiyale, Crowell & Madhavan (2015).Omiyale O, Crowell CR, Madhavan S. Effect of Wii-based balance training on corticomotor excitability post stroke. Journal of Motor Behavior. 2015;47(3):190–200. doi: 10.1080/00222895.2014.971699. [DOI] [PubMed] [Google Scholar]
- Orsega-Smith et al. (2012).Orsega-Smith E, Davis J, Slavish K, Gimbutas L. Wii Fit balance intervention in community-dwelling older adults. Games for Health Journal. 2012;1(6):431–435. doi: 10.1089/g4h.2012.0043. [DOI] [PubMed] [Google Scholar]
- Owens et al. (2011).Owens SG, Garner JC, III, Loftin JM, van Blerk N, Ermin K. Changes in physical activity and fitness after 3 months of home Wii Fit™ use. Journal of Strength and Conditioning Research. 2011;25(11):3191–3197. doi: 10.1519/jsc.0b013e3182132d55. [DOI] [PubMed] [Google Scholar]
- Padala, Padala & Burke (2011).Padala KP, Padala PR, Burke WJ. WII‐FIT as an adjunct for mild cognitive impairment: clinical perspectives. Journal of the American Geriatrics Society. 2011;59(5):932–933. doi: 10.1111/j.1532-5415.2011.03395.x. [DOI] [PubMed] [Google Scholar]
- Padala et al. (2012).Padala KP, Padala PR, Malloy TR, Geske JA, Dubbert PM, Dennis RA, Garner KK, Bopp MM, Burke WJ, Sullivan DH. Wii-Fit for improving gait and balance in an assisted living facility: a pilot study. Journal of Aging Research. 2012;2012:1–6. doi: 10.1155/2012/597573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park, Lee & Lee (2014).Park J, Lee D, Lee S. Effect of virtual reality exercise using the nintendo Wii Fit on muscle activities of the trunk and lower extremities of normal adults. Journal of Physical Therapy Science. 2014;26(2):271–273. doi: 10.1589/jpts.26.271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peng, Crouse & Lin (2013).Peng W, Crouse JC, Lin JH. Using active video games for physical activity promotion: a systematic review of the current state of research. Health Education & Behavior. 2013;40(2):171–192. doi: 10.1177/1090198112444956. [DOI] [PubMed] [Google Scholar]
- Peng, Lin & Crouse (2011).Peng W, Lin JH, Crouse J. Is playing exergames really exercising? A meta-analysis of energy expenditure in active video games. Cyberpsychology, Behavior, and Social Networking. 2011;14(11):681–688. doi: 10.1089/cyber.2010.0578. [DOI] [PubMed] [Google Scholar]
- Pigford & Andrews (2010).Pigford T, Andrews AW. Feasibility and benefit of using the Nintendo Wii Fit for balance rehabilitation in an elderly patient experiencing recurrent falls. Journal of Student Physical Therapy Research. 2010;2(1):12–20. [Google Scholar]
- Plow & Finlayson (2014).Plow M, Finlayson M. A qualitative study exploring the usability of Nintendo Wii Fit among persons with multiple sclerosis. Occupational Therapy International. 2014;21(1):21–32. doi: 10.1002/oti.1345. [DOI] [PubMed] [Google Scholar]
- Podsiadlo & Richardson (1991).Podsiadlo D, Richardson S. The timed “Up & Go”: a test of basic functional mobility for frail elderly persons. Journal of the American Geriatrics Society. 1991;39(2):142–148. doi: 10.1111/j.1532-5415.1991.tb01616.x. [DOI] [PubMed] [Google Scholar]
- Pompeu et al. (2012).Pompeu JE, dos Santos Mendes FA, da Silva KG, Lobo AM, de Paula Oliveira T, Peterson Zomignani A, Pimentel Piemonte ME. Effect of Nintendo Wii™-based motor and cognitive training on activities of daily living in patients with Parkinson’s disease: a randomised clinical trial. Physiotherapy. 2012;98(3):196–204. doi: 10.1016/j.physio.2012.06.004. [DOI] [PubMed] [Google Scholar]
- Powell & Myers (1995).Powell LE, Myers AM. The activities-specific balance confidence (ABC) scale. Journals of Gerontology Series A: Biological Sciences and Medical Sciences. 1995;50A(1):M28–M34. doi: 10.1093/gerona/50a.1.m28. [DOI] [PubMed] [Google Scholar]
- Prosperini et al. (2013).Prosperini L, Fortuna D, Gianni C, Leonardi L, Marchetti MR, Pozzilli C. Home-based balance training using the Wii Balance Board: a randomized, crossover pilot study in multiple sclerosis. Neurorehabilitation and Neural Repair. 2013;27(6):516–525. doi: 10.1177/1545968313478484. [DOI] [PubMed] [Google Scholar]
- Punt et al. (2015).Punt IM, Ziltener JL, Monnin D, Allet L. Wii Fit exercise therapy for the rehabilitation of ankle sprains: its effect compared with physical therapy or no functional exercises at all. Scandinavian Journal of Medicine & Science in Sports. 2015;26:816–823. doi: 10.1111/sms.12509. [DOI] [PubMed] [Google Scholar]
- Qualls et al. (2013).Qualls KK, Arnold SH, McEwen IR, Jeffries LM. Exercise using the Wii Fit plus with a child with primary Raynaud’s disease and obesity: a case report. Physical & Occupational Therapy in Pediatrics. 2013;33(3):327–341. doi: 10.3109/01942638.2012.747583. [DOI] [PubMed] [Google Scholar]
- Ramstrand & Lygnegård (2012).Ramstrand N, Lygnegård F. Can balance in children with cerebral palsy improve through use of an activity promoting computer game? Technology and Health Care. 2012;20(6):531–540. doi: 10.3233/THC-2012-0696. [DOI] [PubMed] [Google Scholar]
- Reger et al. (2012).Reger GM, Holloway KM, Edwards J, Edwards-Stewart A. Importance of patient culture and exergaming design for clinical populations: a case series on exercise adherence in soldiers with depression. Games for Health Journal. 2012;1(4):312–318. doi: 10.1089/g4h.2012.0014. [DOI] [PubMed] [Google Scholar]
- Rendon et al. (2012).Rendon AA, Lohman EB, Thorpe D, Johnson EG, Medina E, Bradley B. The effect of virtual reality gaming on dynamic balance in older adults. Age and Ageing. 2012;41(4):549–552. doi: 10.1093/ageing/afs053. [DOI] [PubMed] [Google Scholar]
- Robinson et al. (2015).Robinson J, Dixon J, Macsween A, van Schaik P, Martin D. The effects of exergaming on balance, gait, technology acceptance and flow experience in people with multiple sclerosis: a randomized controlled trial. BMC Sports Science, Medicine and Rehabilitation. 2015;7:8. doi: 10.1186/s13102-015-0001-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roopchand-Martin et al. (2015).Roopchand-Martin S, McLean R, Gordon C, Nelson G. Balance training with Wii Fit plus for community-dwelling persons 60 years and older. Games for Health Journal. 2015;4(3):247–252. doi: 10.1089/g4h.2014.0070. [DOI] [PubMed] [Google Scholar]
- Salem et al. (2012).Salem Y, Gropack SJ, Coffin D, Godwin EM. Effectiveness of a low-cost virtual reality system for children with developmental delay: a preliminary randomised single-blind controlled trial. Physiotherapy. 2012;98(3):189–195. doi: 10.1016/j.physio.2012.06.003. [DOI] [PubMed] [Google Scholar]
- Sims et al. (2013).Sims J, Cosby N, Saliba EN, Hertel J, Saliba SA. Exergaming and static postural control in individuals with a history of lower limb injury. Journal of Athletic Training. 2013;48(3):314. doi: 10.4085/1062-6050-48.2.04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steenstrup et al. (2014).Steenstrup B, Giralte F, Bakker E, Grise P. Evaluation of the electromyography activity of pelvic floor muscle during postural exercises using the Wii Fit Plus(©) [Analysis and perspectives in rehabilitation] Progres en Urologie. 2014;24(17):1099–1105. doi: 10.1016/j.purol.2014.09.046. [DOI] [PubMed] [Google Scholar]
- Subramaniam, Wan-Ying Hui-Chan & Bhatt (2014).Subramaniam S, Wan-Ying Hui-Chan C, Bhatt T. A cognitive-balance control training paradigm using Wii Fit to reduce fall risk in chronic stroke survivors. Journal of Neurologic Physical Therapy. 2014;38(4):216–225. doi: 10.1097/npt.0000000000000056. [DOI] [PubMed] [Google Scholar]
- Tarakci et al. (2013).Tarakci D, Ozdincler AR, Tarakci E, Tutuncuoglu F, Ozmen M. Wii-based balance therapy to improve balance function of children with cerebral palsy: a pilot study. Journal of Physical Therapy Science. 2013;25(9):1123–1127. doi: 10.1589/jpts.25.1123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor et al. (2014).Taylor MJ, Lindsverk H, Nygaard M, Hunt J, Shanks J, Griffin M, Shawis T, Impson R. Comparing the energy expenditure of Wii-Fit-based therapy with that of traditional physiotherapy in an older adult population. Journal of the American Geriatrics Society. 2014;62(1):203–205. doi: 10.1111/jgs.12624. [DOI] [PubMed] [Google Scholar]
- Tietäväinen et al. (2013).Tietäväinen A, Gates FK, Meriläinen A, Mandel JE, Hæggström E. Nintendo® Wii Fit based sleepiness tester detects impairment of postural steadiness due to 24h of wakefulness. Medical Engineering & Physics. 2013;35(12):1850–1853. doi: 10.1016/j.medengphy.2013.08.007. [DOI] [PubMed] [Google Scholar]
- Toulotte, Toursel & Olivier (2012).Toulotte C, Toursel C, Olivier N. Wii Fit® training vs. adapted physical activities: which one is the most appropriate to improve the balance of independent senior subjects? A randomized controlled study. Clinical Rehabilitation. 2012;26(9):827–835. doi: 10.1177/0269215511434996. [DOI] [PubMed] [Google Scholar]
- Tripette et al. (2014a).Tripette J, Murakami H, Ando T, Kawakami R, Tanaka N, Tanaka S, Miyachi M. Wii Fit U intensity and enjoyment in adults. BMC Research Notes. 2014a;7(1):567. doi: 10.1186/1756-0500-7-567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tripette et al. (2014b).Tripette J, Murakami H, Gando Y, Kawakami R, Sasaki A, Hanawa S, Hirosako A, Miyachi M. Home-based active video games to promote weight loss during the postpartum period. Medicine & Science in Sports & Exercise. 2014b;46(3):472–478. doi: 10.1249/mss.0000000000000136. [DOI] [PubMed] [Google Scholar]
- Wall et al. (2015).Wall T, Feinn R, Chui K, Cheng MS. The effects of the Nintendo Wii Fit on gait, balance, and quality of life in individuals with incomplete spinal cord injury. Journal of Spinal Cord Medicine. 2015;38:778–783. doi: 10.1179/2045772314y.0000000296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White, Schofield & Kilding (2011).White K, Schofield G, Kilding AE. Energy expended by boys playing active video games. Journal of Science and Medicine in Sport. 2011;14(2):130–134. doi: 10.1016/j.jsams.2010.07.005. [DOI] [PubMed] [Google Scholar]
- Wikstrom (2012).Wikstrom EA. Validity and reliability of Nintendo Wii Fit balance scores. Journal of Athletic Training. 2012;47(3):306–313. doi: 10.4085/1062-6050-47.3.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams et al. (2011).Williams B, Doherty NL, Bender A, Mattox H, Tibbs JR. The effect of Nintendo Wii on balance: a pilot study supporting the use of the Wii in occupational therapy for the well elderly. Occupational Therapy in Health Care. 2011;25(2–3):131–139. doi: 10.3109/07380577.2011.560627. [DOI] [PubMed] [Google Scholar]
- Williams et al. (2010).Williams MA, Soiza RL, Jenkinson AM, Stewart A. EXercising with computers in later life (EXCELL)-pilot and feasibility study of the acceptability of the Nintendo® Wii Fit in community-dwelling fallers. BMC Research Notes. 2010;3(1):238. doi: 10.1186/1756-0500-3-238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Worley, Rogers & Kraemer (2011).Worley JR, Rogers SN, Kraemer RR. Metabolic responses to Wii Fit™ video games at different game levels. Journal of Strength and Conditioning Research. 2011;25(3):689–693. doi: 10.1519/jsc.0b013e318207eae9. [DOI] [PubMed] [Google Scholar]
- Xian et al. (2014).Xian Y, Kakinami L, Peterson ED, Mustian KM, Fernandez ID. Will Nintendo “Wii Fit” get you fit? An evaluation of the energy expenditure from active-play videogames. Games for Health Journal. 2014;3(2):86–91. doi: 10.1089/g4h.2013.0078. [DOI] [PubMed] [Google Scholar]
- Yamada et al. (2011).Yamada M, Aoyama T, Nakamura M, Tanaka B, Nagai K, Tatematsu N, Uemura K, Nakamura T, Tsuboyama T, Ichihashi N. The reliability and preliminary validity of game-based fall risk assessment in community-dwelling older adults. Geriatric Nursing. 2011;32(3):188–194. doi: 10.1016/j.gerinurse.2011.02.002. [DOI] [PubMed] [Google Scholar]
- Yatar & Yildirim (2015).Yatar GI, Yildirim SA. Wii Fit balance training or progressive balance training in patients with chronic stroke: a randomised controlled trial. Journal of Physical Therapy Science. 2015;27(4):1145–1151. doi: 10.1589/jpts.27.1145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yuen et al. (2013).Yuen HK, Breland HL, Vogtle LK, Holthaus K, Kamen DL, Sword D. The process associated with motivation of a home-based Wii Fit exercise program among sedentary African American women with systemic lupus erythematosus. Disability and Health Journal. 2013;6(1):63–68. doi: 10.1016/j.dhjo.2012.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yuen et al. (2011).Yuen HK, Holthaus K, Kamen DL, Sword D, Breland HL. Using Wii Fit to reduce fatigue among African American women with systemic lupus erythematosus: a pilot study. Lupus. 2011;20(12):1293–1299. doi: 10.1177/0961203311412098. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The following information was supplied regarding data availability:
The work consists of a systematic review and a meta-analysis. No original data have been generated. The data used for the meta-analysis are reported in the tables in the manuscript.