To the Editor
Indoor tanning and sunburns increase the risk for skin cancer.1 We examined trends in indoor tanning among US adults during 2010–2015 and its association with sunburn.
We analyzed data from the 2010, 2013, and 2015 National Health Interview Survey (NHIS), a nationally representative sample of the US civilian noninstitutionalized population aged ≥18 years. Respondents were asked about indoor tanning and sunburns (from the sun or indoor tanning) during the preceding 12 months. We calculated the prevalence of indoor tanning and examined linear trends using regression analyses. We examined the association between indoor tanning and sunburn in 2015 using multivariable logistic regression and presented results as predictive margins. Parallel analyses were performed among nonHispanic white women aged 18–29 years, the most common users of tanning devices. Annual response rates were 55.2%–61.2%, and sample sizes were 25,233–33,912 persons. Sample weights were applied to account for the complex study design. Data were analyzed using SUDAAN 10.1 (RTI International).
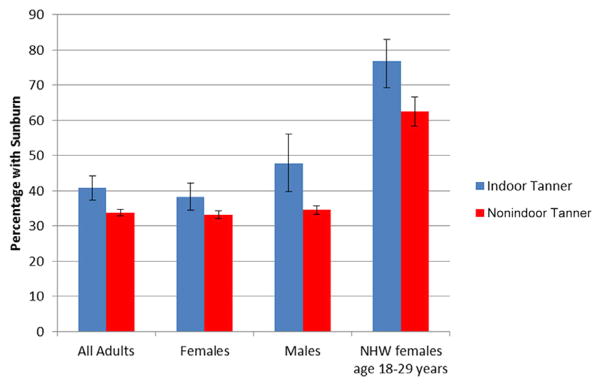
Adult indoor tanning decreased from 5.5% in 2010 to 3.5% in 2015 (P < .001), from 8.6% to 5.2% (P <.001) among women, and from 2.2% to 1.6% (P = .004) among men (Table I). Among nonHispanic white women aged 18–21 years, indoor tanning decreased from 31.8% in 2010 to 20.4% in 2015 (P = .011). In the adjusted model, indoor tanning was positively associated with sunburn; 40.8% of indoor tanners reported at least one sunburn during the preceding year compared with 33.9% of nonindoor tanners (P < .001) (Fig 1). Among nonHispanic white women aged 18–29 years, 76.9% of indoor tanners reported a sunburn compared with 62.5% of nonindoor tanners (P = .001).
Table I.
Prevalence of indoor tanning among adults, National Health Interview Survey, 2010, 2013, and 2015
| 2010
|
2013
|
2015
|
P value* | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| n = 25,233
|
n = 33,912
|
n = 31,518
|
||||||||
| % | 95% CI | % | 95% CI | % | 95% CI | |||||
| Total | 5.5 | 5.1 | 6.0 | 4.2 | 3.9 | 4.5 | 3.5 | 3.2 | 3.8 | <.001 |
| Sex | ||||||||||
| Male | 2.2 | 1.9 | 2.6 | 1.7 | 1.5 | 2.0 | 1.6 | 1.3 | 1.9 | .004 |
| Female | 8.6 | 7.9 | 9.3 | 6.5 | 6.0 | 7.0 | 5.2 | 4.8 | 5.8 | <.001 |
| Age, y | ||||||||||
| 18–29 | 11.3 | 10.1 | 12.6 | 8.6 | 7.7 | 9.5 | 6.0 | 5.1 | 6.9 | <.001 |
| 30–39 | 5.9 | 5.2 | 6.8 | 5.5 | 4.8 | 6.3 | 4.4 | 3.8 | 5.2 | .004 |
| 40–49 | 5.9 | 5.1 | 6.9 | 4.3 | 3.6 | 5.1 | 3.8 | 3.1 | 4.7 | <.001 |
| 50+ | 2.1 | 1.7 | 2.5 | 1.5 | 1.3 | 1.8 | 1.8 | 1.5 | 2.2 | .287 |
| Race/Ethnicity | ||||||||||
| NonHispanic white | 7.4 | 6.9 | 8.0 | 5.7 | 5.3 | 6.2 | 4.9 | 4.4 | 5.4 | <.001 |
| Black | 0.3† | 0.1 | 0.5 | 0.2† | 0.1 | 0.4 | 0.2† | 0.1 | 0.5 | .507 |
| Hispanic | 1.8 | 1.4 | 2.4 | 1.7 | 1.3 | 2.3 | 1.2 | 0.9 | 1.7 | .063 |
| Other | 2.0 | 1.2 | 3.3 | 1.2 | 0.8 | 1.7 | 0.8 | 0.5 | 1.3 | .033 |
| US census region‡ | ||||||||||
| Northeast | 4.1 | 3.3 | 5.1 | 3.7 | 3.1 | 4.5 | 3.1 | 2.4 | 4.0 | .080 |
| Midwest | 8.6 | 7.6 | 9.7 | 7.3 | 6.5 | 8.1 | 5.3 | 4.5 | 6.2 | <.001 |
| South | 5.4 | 4.8 | 6.2 | 3.2 | 2.8 | 3.7 | 3.4 | 3.0 | 4.0 | <.001 |
| West | 3.7 | 3.0 | 4.6 | 3.1 | 2.6 | 3.7 | 2.1 | 1.7 | 2.7 | <.001 |
| Most common users | ||||||||||
| NonHispanic white females by age, y | ||||||||||
| 18–21 | 31.8 | 25.7 | 38.7 | 21.6 | 17.4 | 26.5 | 20.4 | 15.4 | 26.5 | .011 |
| 22–25 | 29.6 | 24.6 | 35.1 | 27.0 | 22.4 | 32.2 | 13.9 | 10.7 | 18.0 | <.001 |
| 26–29 | 22.1 | 18.1 | 26.8 | 17.3 | 14.0 | 21.1 | 13.8 | 10.0 | 18.8 | .009 |
Indoor tanning is defined as using an indoor tanning device (such as a sunlamp, sunbed, or tanning booth) ≥1 times during the 12 months before the survey. Does not include getting a spray-on tan. Estimates based on weighted data. Sample sizes (n) are unweighted. Percentages and 95% CI are based on weighted population estimates.
CI, Confidence interval.
P value based on linear contrast for trend among the estimates over the 3 years.
Estimates based on fewer than 30 observations or with a relative standard error >0.30 are considered unreliable by the standards of the National Center for Health Statistics.
Northeast: Connecticut, Maine, Massachusetts, New Jersey, New Hampshire, New York, Pennsylvania, Rhode Island, and Vermont; Midwest: Illinois, Indiana, Iowa, Kansas, Michigan, Minnesota, Missouri, Nebraska, North Dakota, Ohio, South Dakota, and Wisconsin; South: Alabama, Arkansas, Delaware, District of Columbia, Florida, Georgia, Kentucky, Louisiana, Maryland, Mississippi, North Carolina, Oklahoma, South Carolina, Tennessee, Texas, Virginia, and West Virginia; West: Alaska, Arizona, California, Colorado, Hawaii, Idaho, Montana, New Mexico, Nevada, Oregon, Utah, Washington, and Wyoming.
Fig. 1.
Association between indoor tanning and sunburn among adults, National Health Interview, 2015. Indoor tanning defined as using an indoor tanning device (such as a sunlamp, sunbed, or tanning booth) ≥1 times during the 12 months before the survey. Does not include getting a spray-on tan. Sunburns include burns from the sun and from indoor tanning. Bars represent 95% confidence intervals. Differences are statistically significant across all 4 groups (P <.05) after controlling for age, sex, and race/ethnicity among all adults; age and race/ethnicity among sex-stratified analyses; and age among nonHispanic white (NHW) women.
Indoor tanning among US adults has decreased, including among the most common users. In 2015, an estimated 7.8 million adults engaged in indoor tanning, down from 11.7 million in 2010. Increased awareness of risks,1,2 implementation of a 10% excise tax in 2010, state laws restricting minors’ access,3 new safety measures from the US Food and Drug Administration,3 and a Call to Action from the US Surgeon General promoting prevention efforts4 might explain these declines.
Indoor tanners were more likely than nonindoor tanners to report sunburns, possibly from tan-seeking behaviors and misperceptions about tanned skin. Persons with tans might overestimate the protection conferred by their tanned skin (or a base tan), possibly leading to additional overexposure to ultraviolet radiation. When asked in 2015 about problems associated with indoor tanning, 6.7% of indoor tanners (an estimated 526,000 adults) reported having been burned by an indoor tanning device in the previous year.
This study is subject to certain limitations. Results from the NHIS are generalizable only to the noninstitutionalized, civilian adult population. In addition, the use of cross-sectional data does not permit a causal inference between indoor tanning and sunburn.
Continued efforts are needed to further reduce indoor tanning. Given continued use among young women and the availability of indoor tanning in unregulated facilities near college campuses,5 colleges can adopt policies that discourage indoor tanning. Physicians can counsel young adults as recommended by the US Preventive Services Task Force.4 Reducing indoor tanning remains an important opportunity for the primary prevention of skin cancer.
Acknowledgments
Funding sources: None.
Footnotes
Conflicts of interest: None declared.
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention or the National Institutes of Health.
References
- 1.El Ghissassi F, Baan R, Straif K, et al. WHO International Agency for Research on Cancer Monograph Working Group. A review of human carcinogens, part D: radiation. Lancet Oncol. 2009;10(8):751–752. doi: 10.1016/s1470-2045(09)70213-x. [DOI] [PubMed] [Google Scholar]
- 2.Colantonio S, Bracken MB, Beecker J. The association of indoor tanning and melanoma in adults: systematic review and meta-analysis. J Am Acad Dermatol. 2014;70(5):847–857. e1–18. doi: 10.1016/j.jaad.2013.11.050. [DOI] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention. Skin Cancer Prevention Progress Report 2016. Atlanta, GA: Centers for Disease Control and Prevention, US Department of Health and Human Services; 2016. [Google Scholar]
- 4.US Department of Health and Human Services. The Surgeon General’s Call to Action to Prevent Skin Cancer. Washington, DC: US Department of Health and Human Services, Office of the Surgeon General; 2014. [Google Scholar]
- 5.Pagoto SL, Lemon SC, Oleski JL, et al. Availability of tanning beds on US college campuses. JAMA Dermatol. 2015;151(1):59–63. doi: 10.1001/jamadermatol.2014.3590. [DOI] [PubMed] [Google Scholar]