Abstract
Excessive or risky alcohol use is a preventable cause of significant morbidity and mortality in the U.S. and worldwide. Alcohol use is a common preventable cancer risk factor among young adults; it is associated with increased risk of developing at least six types of cancer. Alcohol consumed during early adulthood may pose a higher risk of female breast cancer than alcohol consumed later in life. Reducing alcohol use may help prevent cancer. Alcohol misuse screening and brief counseling or intervention (also called alcohol screening and brief intervention among other designations) is known to reduce excessive alcohol use, and the U.S. Preventive Services Task Force recommends that it be implemented for all adults aged ≥ 18 years in primary healthcare settings. Because the prevalence of excessive alcohol use, particularly binge drinking, peaks among young adults, this time of life may present a unique window of opportunity to talk about the cancer risk associated with alcohol use and how to reduce that risk by reducing excessive drinking or misuse. This article briefly describes alcohol screening and brief intervention, including the Centers for Disease Control and Prevention’s recommended approach, and suggests a role for it in the context of cancer prevention. The article also briefly discusses how the Centers for Disease Control and Prevention is working to make alcohol screening and brief intervention a routine element of health care in all primary care settings to identify and help young adults who drink too much.
ALCOHOL USE AND CANCER
Aiming to translate science into public health practice, the Centers for Disease Control and Prevention (CDC)’s Division of Cancer Prevention and Control has examined cancer risk factors and opportunities for cancer prevention using a life course approach.1 The most recent phase of life considered by CDC was young adulthood, roughly defined as age 18–44 years.2 Evidence suggests that exposures to risk factors during young adulthood may contribute to the multistage development of cancer, underscoring the importance of interventions during this time of life to reduce exposures.3 Additionally, young adulthood may be an opportune time to establish and sustain lifelong healthy behaviors,4 which can prevent cancer, and other chronic diseases, later in life.
Alcohol use is a critical health behavior; excessive alcohol use is implicated in a wide range of acute and long-term social harms and adverse health outcomes, including cancer.5 However, the potential role of alcohol in cancer development may not be well understood, or even recognized, by many adults.6 The prevalence of past-year alcohol use and past-month binge drinking peaks among young adults (aged 18–44 years),7 presenting a window of opportunity to talk about the associated cancer risks and how to reduce a risk factor by reducing excessive drinking. Evidence indicates that excessive alcohol use can be reduced through community-level policy interventions, including increasing alcohol taxes and regulating alcohol outlet density.8 Further, alcohol misuse screening and brief counseling or intervention (also called alcohol screening and brief intervention [SBI]) is also an evidence-based and recommended9–11 clinical preventive service to reduce excessive alcohol use. This article provides a brief overview of the association between alcohol use and cancer, describes alcohol SBI’s efficacy and key components, places alcohol SBI in the context of cancer prevention, and reviews how CDC is working to make alcohol SBI a routine element of health care in all primary care settings to identify and help adults who drink too much.
Alcohol use can contribute to the development of cancers of the breast (female); liver; colon, rectum, mouth, pharynx, larynx, and esophagus, and accumulating evidence suggests causal associations with other sites such as pancreas and prostate cancer.12 Some evidence suggests that alcohol consumed during early adulthood may pose a higher risk of female breast cancer than alcohol consumed later in life.2 Alcohol use is related causally to cancer.12,13 Alcoholic drinks contain at least 15 carcinogens; the most potent are ethanol and its metabolite, acetaldehyde.12 The mechanisms by which alcohol can cause cancer are complex, not completely understood, and may differ by cancer site, but there is ample information to consider the role and impact of these mechanisms. Possible carcinogenic mechanisms include causing direct insult to tissue, promoting oxidative stress, interfering with DNA synthesis and repair, increasing estrogen concentration, thereby activating cellular proliferation, interfering with folate metabolism, and inducing cirrhosis and chronic inflammation.12,14,15 Regardless of drink type (beer, wine, or liquor), the risk of cancer increases with the number of consumed drinks, and even one alcoholic drink a day increases the risk of developing cancers of the breast (female), mouth, and esophagus.16 Reducing or discontinuing alcohol use may help to reduce the risk of cancer.17
Based on epidemiologic research, the 2015–2020 U.S. Dietary Guidelines for Americans state, “If alcohol is consumed, it should be consumed in moderation—up to one drink per day for women and up to two drinks per day for men—and only by adults of legal drinking age... The Dietary Guidelines does not recommend that individuals who do not drink alcohol start drinking for any reason.”18 In the U.S., a standard alcoholic drink contains 14 grams or 0.6 fluid ounces of pure alcohol, which is the equivalent of one 12-ounce can of beer (5% alcohol), one 5-ounce glass of wine (12% alcohol), or one shot (1.5 fluid ounces) of 80 proof distilled spirits (40% alcohol).18 Lower consumption limits are suggested for women than for men because given the same amount of alcohol consumption, blood alcohol concentration is proportionally higher among women because their bodies are generally smaller, have less body water, and metabolize alcohol more slowly.19 Both the U.S. Dietary Guidelines and levels of risky drinking suggested by CDC20 caution that there are circumstances in which individuals should not drink. In addition to the recommendation of abstinence for pregnant women and youth (aged <21 years), any alcohol consumption is risky for individuals who are dependent on alcohol or unable to control the amount of alcohol they drink. Further, the CDC guide recommends that individuals consider limiting or abstaining from alcohol use if they take prescription drugs that alcohol potentiates or inactivates, have medical conditions that can be made worse by alcohol (like liver disease, hypertriglyceridemia, and pancreatitis),21,22 or plan to drive or engage in other activities that require skill, coordination, or alertness.18,20
Healthcare providers can discuss alcohol use with their patients so they better understand their individual health risks. The U.S. Dietary Guidelines do not represent an absolute safe amount to drink for an individual, but are population-level suggestions that are intended to keep most people’s health risks from alcohol low. Risky alcohol use leads to increased risk of health problems and includes (1) excessive drinking in a single day (four or more drinks for women, five or more drinks for men); (2) binge drinking (exceeding the single-day limits within 2 hours); (3) high weekly consumption (eight or more drinks for women, ≥ 15 drinks for men in a week); and (4) any drinking by pregnant women or people aged <21 years.20,23
The prevalence of excessive or risky alcohol use, particularly binge drinking, peaks among young adults. 2011 data from CDC’s Behavioral Risk Factor Surveillance System (BRFSS) indicated that slightly more than half of U.S. adults report drinking at least one alcoholic drink in the past month; this prevalence was higher among younger adults <35 years of age (70% among those aged 21–25 years and 64% among those aged 26–34 years) than those aged ≥35 years (59% among those 35–54, 45% among those 55+).24 Among adults who consume alcohol, about two thirds exceeded the 2010 U. S. Dietary Guidelines for moderate alcohol use (defined as one drink a day for women; more than two drinks a day for men). The percentage was higher among younger adult drinkers <35 years of age (82% among those aged 21–25 years and 76% among those aged 26–34 years) than adults aged ≥35 years (68% among those 35–54, and 52% among those 55+).24 In 2011, about 18% of adults reported binge drinking at least once in the past month, and this percentage was highest among younger adults (Table 1).25 Although young adults (aged 25–44 years) reported binge drinking less frequently than older adults (aged ≥ 65 years), they tend to drink more during each episode (Table 1).24 These data show that excessive alcohol use is a significant problem among adults aged 18–44 years. This time of life may present a unique window of opportunity for healthcare providers to talk with their patients about the cancer risk associated with alcohol use and how to reduce that risk by reducing excessive drinking.
Table 1.
Prevalence, Frequency, and Intensity of Binge Drinkinga by Age Group—Behavioral Risk Factor Surveillance System, U.S., 2011b
| Age, years | Prevalencec of binge drinking, % | Binge drinking frequency,d episodes per month | Intensity,e number of drinks per binge drinking episode |
|---|---|---|---|
| 18–24 | 30.0 | 4.4 | 8.9 |
| 25–34 | 29.7 | 3.8 | 8.2 |
| 35–44 | 21.1 | 3.9 | 7.4 |
| 45–64 | 14.1 | 4.2 | 6.6 |
| ≥ 65 | 4.3 | 4.9 | 5.6 |
| Totals | 18.4 | 4.1 | 7.7 |
Source: Kanny D, Liu Y, Brewer RD, Liu H. Binge drinking—United States, 2011. MMWR Suppl. 2013;62(3):77–80.25
Binge drinking was defined as consuming four or more drinks on an occasion during the preceding 30 days for women and five or more drinks for men. An occasion is generally defined as 2–3 hours.
Respondents were from all 50 states and the District of Columbia.
Prevalence = total number of respondents who reported at least one binge drinking episode during the past 30 days divided by the total number of respondents.
Frequency = average number of binge drinking episodes reported by all binge drinkers during the past 30 days.
Intensity = average largest number of drinks consumed by binge drinkers on any occasion during the past 30 days.
WHAT IS ALCOHOL SCREENING AND BRIEF INTERVENTION?
Alcohol SBI is an effective, quick, and inexpensive tool to identify adults across the spectrum of alcohol misuse and help them reduce the amount they drink.9–11,20,26 CDC uses the term SBI as per mid-1990s research referring to screening and brief intervention. The Substance Abuse and Mental Health Services Administration initiated a grant program to encourage SBI implementation and included “RT” for the referral to treatment aspect of addressing dependence.20 A National Academy of Medicine recommendation called for community-based screening for health risk behaviors, including substance use, which led to the development of the SBIRT model.20
Many patients who drink too much are not dependent upon alcohol.27 Data from the National Survey on Drug Use and Health (2009–2011) found that 90% of people who drink excessively did not meet criteria for dependence upon alcohol, and this percentage was similar for younger adults (88% among those aged 18–24 years and 89% among those aged 25–34 years).27 Because excessive alcohol use is a significant cause of preventable morbidity and mortality among young adults, healthcare providers can help them by implementing alcohol SBI in their practices. Healthcare providers can describe the harms associated with excessive alcohol use and explain that many of these harms occur more frequently among young adults.20 Elements of motivational interviewing (an approach that focuses on a collaborative conversation to strengthen an individual’s commitment and motivation to change their behavior) can be helpful.28 These elements include giving feedback to the patient about their consumption—listening to learn how the patient feels about the pros and cons of their drinking, and helping the patient figure out options for next steps.20 Evidence suggests that messages that highlight the benefits of engaging in a healthy behavior are effective in encouraging that behavior,29 so framing consumption of moderate or less use of alcohol as a way to reduce cancer risk may be effective in reducing excessive alcohol use. Many people respond positively to alcohol SBI and reduce their alcohol use.9,10
Alcohol SBI has been recommended as an evidence-based, cost-effective clinical preventive service since 2004 by the U.S. Preventive Services Task Force (USPSTF) for all adults aged ≥ 18 years, including pregnant women, in primary care health settings.9,10 Given that consumption of alcohol in reproductive years can result in fetal alcohol spectrum disorders (FASDs), health professionals can also address risk for unwanted reproductive outcomes associated with an alcohol-exposed pregnancy in the young adult population. Findings from the USPSTF review indicate that compared with adults who did not receive brief counseling interventions, adults who did reported reduced weekly alcohol consumption (by 3.6 drinks/week); reduced episodes of binge drinking (12% more participants); and increased compliance with recommended drinking limits (11% more participants).9 Binge drinking is also sometimes referred to as “heavy episodic drinking.”30 According to the National Commission on Prevention Priorities, alcohol SBI is ranked in the top five among clinical preventive services, even above breast and cervical cancer screening, based on the clinically preventable burden of disease and cost effectiveness of the intervention.31
Alcohol SBI involves the use of a valid screening instrument to determine if a person is drinking too much. If they are, screening is followed by assessment and counseling and treatment or referral if indicated. A variety of screening instruments are available. In 2013, the USPSTF indicated the following as screeners of choice: a single-question screener (the National Institute on Alcohol Abuse and Alcoholism single question screener is given as an example), the three-question abbreviated Alcohol Use Disorders Identification Test–Consumption (AUDIT C), and the ten-question AUDIT.10 However, the USPSTF plans to update the review of this topic and may have different recommendations in the near future. WHO recommends that the AUDIT be modified based upon the standard drink size of the country in which it is being used, which helps clinicians better identify patients who require additional assessment.32 Some well-known and validated screening tools (such as the CAGE and T-ACE, which was developed for pregnant women specifically) are often used in primary care settings to assess alcohol dependence but focus on dependence and do not assess individual patterns of alcohol consumption.10
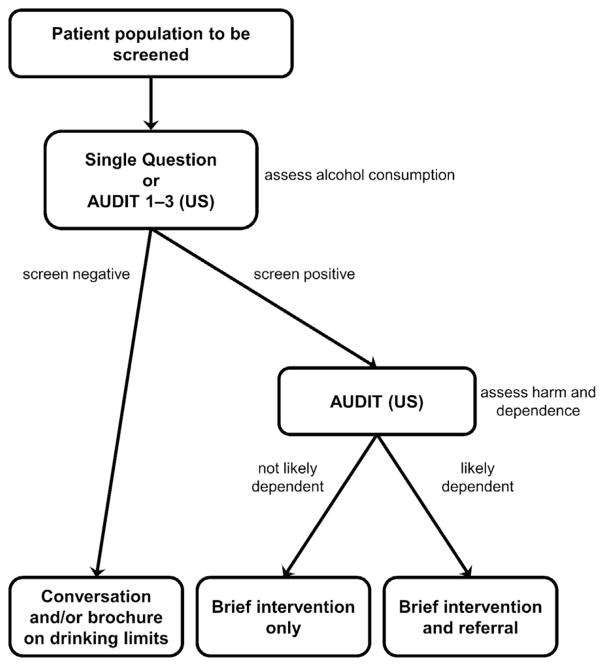
In 2014, CDC published a ten-step guide to help primary care practices conduct planning and implementation for SBI for risky alcohol use as a part of routine practice.20 These CDC guidelines include modified versions of AUDIT C and AUDIT, which include modifications based on standard U.S. drink sizes and gender differences in number of drinks consumed per binge. These versions are called AUDIT 1–3 (U.S.) and AUDIT (U.S.), respectively (Figure 1). Patients who drink too much or exceed guidelines according to screening/assessment results receive counseling and may also require treatment and referral to treatment.9,10,20 Brief counseling sessions or interventions allow a healthcare provider to discuss their patient’s alcohol use in relation to their health and help the patient reduce drinking if that is the patient’s desired goal. Patients who are found to have indications of dependence can be prescribed pharmacotherapy, referred to intensive outpatient or inpatient treatment programs, or referred to 12-step programs like Alcoholics Anonymous.9,20,26 It is important for providers to have a list of referral services and to plan to address patients who may need to utilize them.20
Figure 1.
Alcohol screening and brief intervention (Alcohol SBI): patient flow using AUDIT 1-3 (U.S.).
Source: Centers for Disease Control and Prevention. Planning and Implementing Screening and Brief Intervention for Risky Alcohol Use: A Step-by-Step Guide for Primary Care Practices. Atlanta GA: Centers for Disease Control and Prevention, National Center on Birth Defects and Developmental Disabilities, 2014.20
Note: AUDIT is the 10-question Alcohol Use Disorders Identification Test. AUDIT (U.S.) is based on U.S. drink sizes. AUDIT 1-3 (U.S.) is the three-question abbreviated AUDIT based on U.S. drink sizes.
WHAT IS THE PREVALENCE OF ALCOHOL SCREENING AND BRIEF INTERVENTION?
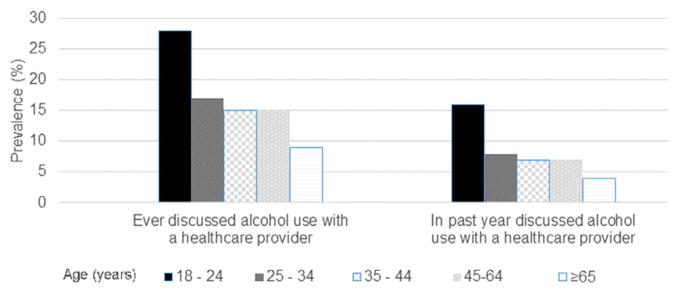
Limited surveillance data suggest that alcohol SBI is rarely used despite the fact that significant policy and public health efforts have been enacted to promote its implementation in primary care for some time.33 In 2011, only one in six U.S. adults reported ever discussing alcohol use with a doctor or healthcare professional according to a CDC report based on BRFSS data from 44 states and the District of Columbia.33 Even fewer adults discussed alcohol use with a healthcare provider in the previous year (Figure 2). Although the prevalence of ever discussing alcohol use with a healthcare provider was higher among young adults, it was still quite low, representing a significant missed opportunity to intervene with young adults to reduce their risk of cancer and other health problems (Figure 2).
Figure 2.
Prevalence of discussions of alcohol use with a healthcare provider ever and in the past year, by age group. Behavioral Risk Factor Surveillance System, 44 states and the District of Columbia, August 1–December 31, 2011.
Source: McKnight-Eily LR, Liu Y, Brewer RD, et al. Vital signs: communication between health professionals and their patients about alcohol use—44 states and the District of Columbia, 2011. MMWR Morb Mortal Wkly Rep. 2014;63:16–22.33
In 2011, even among people who reported binge drinking, only one in four reported ever discussing alcohol use with a health professional.33 This represents a missed opportunity to intervene on behalf of the patient’s health.34,35 In a representative sample of young adults (some in college and others not) from the NEXT Generation Health Study, three in four (71%) reported seeing a physician in the previous year. Of those who saw a physician, most reported being asked about alcohol use (77%), although only one in three (36%) of those who reported drinking or being drunk six or more times in a month were asked to reduce their drinking.34,35 Among young adults aged 18–39 years who responded to an Internet panel, many (67%) reported seeing a doctor in the past year; however, of those who exceeded National Institute on Alcohol Abuse and Alcoholism drinking guidelines, only 14% were asked and advised about risky drinking patterns and 7% advised to cut down on drinking.35 A lower percentage of those aged 18–25 years were asked about drinking compared with other young adults, even though this age group was more likely to exceed drinking guidelines.35
EFFORTS TO INCREASE USE OF ALCOHOL SCREENING AND BRIEF INTERVENTION
Multiple policy and public health efforts have been enacted to increase the provision of alcohol SBI. As a grade B USPSTF-recommended clinical preventive service, alcohol SBI is covered by most health insurance plans under the Affordable Care Act without additional cost-sharing by the patient.36 Further, a variety of providers in a primary care practice can successfully conduct and bill for alcohol SBI, including physicians, nurses, clinical social workers, and psychologists, so that it is not incumbent on only one type of provider to ensure that screening is conducted as a part of usual care.37
Although the USPSTF recommendation is based on the effectiveness of alcohol SBI for adults in primary care settings, some organizations have recommended its use in healthcare settings other than primary care. The American College of Obstetricians and Gynecologists recommends that all women seeking obstetric–gynecologic care be screened for alcohol use at least yearly and within the first trimester of pregnancy.38 The American College of Surgeons Committee on Trauma requires that all Level I and Level II trauma centers screen patients for risky alcohol use and provide a brief intervention to those who screen positive.39
Despite policy and broad-level public health efforts to increase the provision of alcohol SBI, data suggest that it is not routinely done in primary care. Implementation barriers expressed by health professionals include lack of time, training, and self-efficacy; discomfort discussing the topic with the populations at risk because of the provider’s alcohol use; perceptions of difficulty with working with people who have substance use issues; and lack of insurance coverage. The CDC guide, “Planning and Implementing Screening and Brief Intervention for Risky Alcohol Use,”20 was designed to help providers address many of the aforementioned issues, but a multilevel approach at provider, practice, and varying health systems levels is needed.
Further, some question the effectiveness of alcohol SBI in clinical settings despite significant evidence-based research, a USPSTF recommendation since 2004, and studies of efficacy.40 It has been suggested that the use of electronic SBI for alcohol SBI delivery, which received the recommendation of the Community Preventive Services Task Force in 2012,41 could be effective in increasing alcohol SBI implementation as a “stand-alone” measure or in conjunction with traditional methods. E-SBI tools and approaches represent areas of further research and development that could potentially increase provision of the service to young adults if the tools are readily available, user-friendly for the majority of the population, and focus on drinking standards consistent with U.S. guidelines for overall health. Further, linking alcohol SBI to preventive services for other risky behaviors and mental health problems is also suggested for future consideration/research to increase the implementation of this clinical preventive service.40
WHAT IS CDC DOING TO PROMOTE ALCOHOL SCREENING AND BRIEF INTERVENTION?
Multiple federal agencies, including CDC, have worked for some time to increase the implementation of alcohol SBI in primary care settings. CDC has partnered with national health organizations and academic institutions to focus on changes at the systems level to implement alcohol SBI in primary care as a means of preventing FASDs.42 Since 2014, CDC has funded FASD Practice and Implementation Centers to promote alcohol SBI at the health systems level as a means of preventing FASDs.42 This work continued as CDC efforts begun in 1991 to address FASDs. CDC also developed a five-question module to assess the prevalence of alcohol SBI as reported by U.S. adults who had a checkup in the previous 2 years, and these questions were added to several state BRFSS surveys in 2014.43 Findings indicate that although most U.S. adults (76.6%) report being asked about alcohol use, only a third (32.9%) are screened as recommended by the USPSTF guidelines (which includes an assessment of binge drinking). Even among binge drinkers who were asked if they drink, only one in three were offered advice about what level of drinking is harmful or risky to their health, and only one in six were advised to reduce their drinking.43 It is important that providers find out the patterns of consumption of their patients using validated instruments and not just find out if they drink or if they are dependent upon alcohol.20
TYING ALCOHOL SCREENING AND BRIEF INTERVENTION TO CANCER PREVENTION IN A CLINICAL SETTING
Alcohol use was estimated to contribute to 18,200–21,300 deaths from cancers of the oral cavity, pharynx, larynx, esophagus, liver, colon, rectum, and female breast in 2010, accounting for about 3%–4% of all cancer deaths in the U.S.44 Because alcohol use is a common risk factor for cancer among young adults, reducing or discontinuing alcohol use may help to reduce their risk of cancer.
There are studies that suggest that physician advice is effective in helping cancer patients reduce their alcohol consumption and limited studies also suggest that SBI is effective at reducing consumption in patients with chronic diseases including hypertension where diastolic blood pressure was also reduced.45–49
Data from the 2003 Health Information National Trends Survey found that only 11% of U.S. adults stated that limiting alcohol intake could prevent cancer.6 A study of Australian adults in 2009 found that fewer than half were aware that alcohol caused cancer and suggested that efforts, including initiatives to increase awareness of the long-term health consequences of alcohol use, were needed to reduce alcohol consumption among adults, particularly those aged 18–44 years.50 A study of adults in the United Kingdom found that, regardless of age, fewer than half identified cancer as a consequence of alcohol use when offered a selection of seven health conditions and that awareness differed by cancer type, with 18.0% aware of the link with breast cancer and 80% with liver cancer although a considerable fraction incorrectly considered some cancers such as brain cancer to be caused by alcohol use.51 A study of college students aged 18–25 years showed that most respondents knew about the association between alcohol use and liver cancer (86.0%), colorectal cancer (60.0%), and head and neck cancer (23.0%), but only 3% were aware that alcohol use was a risk factor for breast cancer.52 Better understanding of the cancer risk associated with alcohol use may prompt some young adults to reduce their alcohol use. Alcohol SBI is effective at reducing excessive alcohol use, and healthcare providers can also counsel patients that lower levels of consumption or abstinence may reduce cancer risk. However, providers have to be informed about the relationship between cancer and alcohol themselves. General practitioners in New South Wales and South Australia reported having broad understanding of alcohol as a cancer risk factor but not detailed knowledge of the associated cancer types and some misunderstandings of the causal links. Further, they often did not raise the issue of alcohol use with their patients unless the patients were aged 45–49 years and there was evidence of dependence, suspicion of binge drinking with young people, abnormal biochemical test results, or other factors that suggested an issue with alcohol use.53
The risks of some cancers, including those of the mouth, pharynx, larynx, and esophagus, are even higher for people who use both alcohol and tobacco. Risky alcohol use is highly correlated with cigarette smoking, and for patients who smoke, it may be helpful for successful tobacco-cessation efforts to encourage them to also abstain from alcohol.54
Counseling by healthcare providers can be instrumental in changing health-related behaviors.55 A recent study using BRFSS data examined five health-related behaviors, including avoiding tobacco use, limiting alcohol consumption, getting enough physical activity, maintaining a healthy weight, and getting enough sleep. Results showed that only about one in 20 young adults aged 21–44 years reported engaging in all five of the aforementioned behaviors and fewer than a third reported at least four of these behaviors.56 The authors state that the impact of interventions could be increased by a comprehensive approach addressing multiple risk factors. When counseling young adults, healthcare providers can frame limiting alcohol consumption as part of a healthy lifestyle that will reduce the risk of several chronic diseases, including cancer.
Some young adults may have risk factors that put them at higher risk of cancer, such as a family history of breast cancer or possessing variant alcohol dehydrogenase genes. The few studies that have examined the interaction between alcohol use and family history of breast cancer have not found evidence of a synergistic association.57 A recent meta-analysis found weak to moderate evidence of an inverse association between the fast metabolizing ADH1B*2 and ADH1C*1 alleles and cancer of the oral cavity and pharynx, although the authors cautioned that bias could not be ruled out.58 Regardless, healthcare providers can advise young adults already at high risk of cancer that there are some risk factors, such as alcohol use, that can be modified to reduce their cancer risk.59
CONCLUSIONS
Early adulthood represents a significant opportunity to address a common preventable risk factor for cancer: risky drinking. Even one drink a day can increase the risk for some forms of cancer. Alcohol SBI is an evidence-based clinical preventive service that is underutilized currently. Alcohol SBI holds promise as a way to address this risk through a conversation between providers and their young adult patients about reducing their alcohol consumption if they exceed guidelines for excessive use or are otherwise at risk for cancer outcomes.
Acknowledgments
Publication of this article was supported by the U.S. Centers for Disease Control and Prevention (CDC), an Agency of the U.S. Department of Health and Human Services, under contract number: 200-2017-M-94637. The findings and conclusions in this article are those of the authors and do not necessarily represent the official position of CDC.
Dr. McKnight-Eily takes responsibility for the integrity of the manuscript content. Study concept and design by McKnight-Eily and Henley. Drafting and revision of manuscript by McKnight-Eily, Henley, Green, Hungerford, and Odom. Article content has been presented previously elsewhere.
No financial disclosures were reported by the authors of this paper.
Footnotes
This article is part of a supplement issue titled Opportunities for Cancer Prevention During Early Adulthood.
References
- 1.Shoemaker ML, Holman DM, Henley SJ, White MC. News from CDC: applying a life course approach to primary cancer prevention. Transl Behav Med. 2015;5(2):131–133. doi: 10.1007/s13142-015-0309-0. https://doi.org/10.1007/s13142-015-0309-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Holman DM, White MC, Shoemaker ML, Massetti GM, Puckett MC, Brindis CD. Cancer prevention during early adulthood: highlights from a meeting of experts. Am J Prev Med. 2017;53(3S1):S5–S13. doi: 10.1016/j.amepre.2017.04.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Colditz GA, Bohlke K, Berkey CS. Breast cancer risk accumulation starts early: prevention must also. Breast Cancer Res Treat. 2014;145(3):567–579. doi: 10.1007/s10549-014-2993-8. https://doi.org/10.1007/s10549-014-2993-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.McCracken M, Jiles R, Blanck HM. Health behaviors of the young adult U.S. population: Behavioral Risk Factor Surveillance System, 2003. Prev Chronic Dis. 2007;4(2):A25. www.cdc.gov/pcd/issues/2007/apr/06_0090.htm. [PMC free article] [PubMed] [Google Scholar]
- 5.National Institute of Alcohol Abuse and Alcoholism. Tenth special report to the US Congress on alcohol and health. Bethesda, MD: NIH; 2000. https://pubs.niaaa.nih.gov/publications/10report/10thspecialreport.pdf. [Google Scholar]
- 6.Hawkins NA, Berkowitz Z, Peipins LA. What does the public know about preventing cancer? Results from the Health Information National Trends Survey (HINTS) Health Educ Behav. 2010;37(4):490–503. doi: 10.1177/1090198106296770. https://doi.org/10.1177/1090198106296770. [DOI] [PubMed] [Google Scholar]
- 7.CDC. Vital Signs: Binge Drinking Prevalence, Frequency, and Intensity Among Adults—United States, 2010. [Accessed March 29, 2017];MMWR Morb Mortal Wkly Rep. 2012 61(1):14–19. www.cdc.gov/mmwr/preview/mmwrhtml/mm6101a4.htm. [PubMed] [Google Scholar]
- 8.Community Preventive Services Task Force. Excessive alcohol consumption. [Accessed July 17, 2017];The Community Guide. https://www.thecommunityguide.org/topic/excessive-alcohol-consumption.
- 9.Jonas DE, Garbutt JC, Amick HR, et al. Behavioral counseling after screening for alcohol misuse in primary care: a systematic review and meta-analysis for the U.S. Preventive Services Task Force. Ann Intern Med. 2012;157(9):645–654. doi: 10.7326/0003-4819-157-9-201211060-00544. https://doi.org/10.7326/0003-4819-157-9-201211060-00544. [DOI] [PubMed] [Google Scholar]
- 10.Moyer VA U S. Preventive Services Task Force. Screening and behavioral counseling interventions in primary care to reduce alcohol misuse: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2013;159(3):210–218. doi: 10.7326/0003-4819-159-3-201308060-00652. https://doi.org/10.7326/0003-4819-159-3-201308060-00652. [DOI] [PubMed] [Google Scholar]
- 11.O’Donnell A, Anderson P, Newbury-Birch D, et al. The impact of brief alcohol interventions in primary healthcare: A systematic review of reviews. Alcohol Alcohol. 2014;49(1):66–78. doi: 10.1093/alcalc/agt170. https://doi.org/10.1093/alcalc/agt170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.International Agency for Research on Cancer. IARC monographs on the evaluation of carcinogenic risks to humans: Volume 100E: Personal habits and indoor combustion: consumption of alcoholic beverages. Lyon, France: International Agency for Research on Cancer?; 2012. [Accessed October 24, 2016]. http://monographs.iarc.fr/ENG/Monographs/vol100E/mono100E.pdf. [Google Scholar]
- 13.Bauer UE, Briss PA, Goodman RA, Bowman BA. Prevention of chronic disease in the 21st century: elimination of the leading preventable causes of premature death and disability in the USA. Lancet. 2014;384(9937):45–52. doi: 10.1016/S0140-6736(14)60648-6. https://doi.org/10.1016/S0140-6736(14)60648-6. [DOI] [PubMed] [Google Scholar]
- 14.International Agency for Research on Cancer. IARC monographs on the evaluation of carcinogenic risks to humans: Volume 96: alcohol consumption and ethyl carbamate. Lyon, France: International Agency for Research on Cancer; 2010. [Accessed October 24, 2016]. http://monographs.iarc.fr/ENG/Monographs/vol96/mono96.pdf. [PMC free article] [PubMed] [Google Scholar]
- 15.Scoccianti C, Straif K, Romieu I. Recent evidence on alcohol and cancer epidemiology. Future Oncol. 2013;9(9):1315–1322. doi: 10.2217/fon.13.94. https://doi.org/10.2217/fon.13.94. [DOI] [PubMed] [Google Scholar]
- 16.Bagnardi V, Rota M, Botteri E, et al. Light alcohol drinking and cancer: a meta-analysis. Ann Oncol. 2013;24(2):301–308. doi: 10.1093/annonc/mds337. https://doi.org/10.1093/annonc/mds337. [DOI] [PubMed] [Google Scholar]
- 17.McKenzie F, Biessy C, Ferrari P, et al. Healthy lifestyle and risk of cancer in the European Prospective Investigation Into Cancer and Nutrition Cohort Study. Medicine (Baltimore) 2016;95(16):e2850. doi: 10.1097/MD.0000000000002850. https://doi.org/10.1097/MD.0000000000002850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.U.S. DHHS, U.S. Department of Agriculture. [Accessed October 24, 2016];2015–2020 Dietary Guidelines for Americans. (8). 2015 Dec; http://health.gov/dietaryguidelines/2015/guidelines/
- 19.Cederbaum AI. Alcohol metabolism. Clin Liver Dis. 2012;16(4):667–685. doi: 10.1016/j.cld.2012.08.002. https://doi.org/10.1016/j.cld.2012.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.CDC. Planning and Implementing Screening and Brief Intervention for Risky Alcohol Use: A Step-by-Step Guide for Primary Care Practices. Atlanta, GA: CDC, National Center on Birth Defects and Developmental Disabilities; 2014. [Accessed October 24, 2016]. www.cdc.gov/ncbddd/fasd/documents/alcoholsbiimplementationguide.pdf. [Google Scholar]
- 21.National Institute on Alcohol Abuse and Alcoholism. [Accessed March 9, 2017];Harmful Interactions: Mixing Alcohol with Medicines. https://pubs.niaaa.nih.gov/publications/medicine/harmful_interactions.pdf.
- 22.National Institute on Alcohol Abuse and Alcoholism. [Accessed August 1, 2017];Alcohol Alert No. 27, Alcohol-Medication Interactions. https://pubs.niaaa.nih.gov/publications/aa27.htm. Updated October 2000.
- 23.Saitz R. Unhealthy alcohol use. N Engl J Med. 2005;352(6):596–607. doi: 10.1056/NEJMcp042262. https://doi.org/10.1056/NEJMcp042262. [DOI] [PubMed] [Google Scholar]
- 24.Henley SJ, Kanny D, Roland KB, et al. Alcohol control efforts in comprehensive cancer control plans and alcohol use among adults in the USA. Alcohol Alcohol. 2014;49(6):661–667. doi: 10.1093/alcalc/agu064. https://doi.org/10.1093/alcalc/agu064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kanny D, Liu Y, Brewer RD, Lu H. Binge drinking—United States, 2011. [Accessed October 24, 2016];MMWR Suppl. 2013 62(3):77–80. www.cdc.gov/mmwr/preview/mmwrhtml/su6203a13.htm. [PubMed] [Google Scholar]
- 26.National Institute on Alcohol Abuse, and Alcoholism. [Accessed October 24, 2016];Helping Patients Who Drink Too Much: A Clinicians Guide, Updated 2005 guidelines. http://pubs.niaaa.nih.gov/publications/Practitioner/CliniciansGuide2005/guide.pdf.
- 27.Esser MB, Hedden SL, Kanny D, Brewer RD, Gfroerer JC, Naimi TS. Prevalence of alcohol dependence among U.S. adult drinkers, 2009–2011. Prev Chronic Dis. 2014;11:E206. doi: 10.5888/pcd11.140329. https://doi.org/10.5888/pcd11.140329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Miller WR, Rollnick S. Motivational Interviewing: Helping People Change. 3. New York: The Guilford Press; 2013. [Google Scholar]
- 29.Gallagher KM, Updegraff JA. Health message framing effects on attitudes, intentions, and behavior: a meta-analytic review. Ann Behav Med. 2012;43(1):101–116. doi: 10.1007/s12160-011-9308-7. https://doi.org/10.1007/s12160-011-9308-7. [DOI] [PubMed] [Google Scholar]
- 30.Linden-Carmichael AN, Lanza ST, Dziak JJ, Bray BC. Contemporary alcohol use patterns among a national sample of U.S. adult drinkers. J Addict Dis. doi: 10.1080/10550887.2017.1338816. In press. Online June 8, 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Maciosek MV, LaFrance AB, Debmer SP, et al. Updated priorities among effective clinical preventive services. Am Fam Med. 2017;15:14–22. doi: 10.1370/afm.2017. https://doi.org/10.1370/afm.2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.WHO, Department of Mental Health and Substance Dependence. AUDIT, The Alcohol Use Disorders Identification Test: guidelines for use in primary care, second edition. Geneva, Switzerland: WHO; 2001. [Accessed October 24, 2016]. http://apps.who.int/iris/bitstream/10665/67205/1/WHO_MSD_MSB_01.6a.pdf. [Google Scholar]
- 33.McKnight-Eily LR, Liu Y, Brewer RD, et al. Vital signs: communication between health professionals and their patients about alcohol use—44 states and the District of Columbia, 2011. MMWR Morb Mortal Wkly Rep. 2014;63(1):16–22. [PMC free article] [PubMed] [Google Scholar]
- 34.Hingson R, Zha W, White A, Simons-Morton B. Screening and brief alcohol counseling of college students and persons not in school. JAMA Pediatr. 2015;169(11):1068–1070. doi: 10.1001/jamapediatrics.2015.2231. https://doi.org/10.1001/jamapediatrics.2015.2231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hingson RW, Heeren T, Edwards EM, Saitz R. Young adults at risk for excess alcohol consumption are often not asked or counseled about drinking alcohol. J Gen Intern Med. 2012;27(2):179–184. doi: 10.1007/s11606-011-1851-1. https://doi.org/10.1007/s11606-011-1851-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Koh HK, Sebelius KG. Promoting prevention through the Affordable Care Act. N Engl J Med. 2010;363(14):1296–1299. doi: 10.1056/NEJMp1008560. https://doi.org/10.1056/NEJMp1008560. [DOI] [PubMed] [Google Scholar]
- 37.Mertens JR, Chi FW, Weisner CM, et al. Physician versus non-physician delivery of alcohol screening, brief intervention and referral to treatment in adult primary care: the ADVISe cluster randomized controlled implementation trial. Addict Sci Clin Pract. 2015;10:26. doi: 10.1186/s13722-015-0047-0. https://doi.org/10.1186/s13722-015-0047-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.American College of Obstetricians and Gynecologists, Committee on Health Care for Underserved Women. Committee opinion no. 496: At-risk drinking and alcohol dependence: obstetric and gynecologic implications. Obstet Gynecol. 2011;118(2 Pt 1):383–388. doi: 10.1097/AOG.0b013e31822c9906. https://doi.org/10.1097/AOG.0b013e31822c9906. [DOI] [PubMed] [Google Scholar]
- 39.American College of Surgeons–Committee on Trauma, U.S. DHHS, Department of Transportation. [Accessed October 24, 2016];Alcohol screening and brief intervention (SBI) for trauma patients: COT quick guide. 2007 http://apps.who.int/iris/bitstream/10665/67205/1/WHO_MSD_MSB_01.6a.pdf.
- 40.McCambridge J, Saitz R. Rethinking brief interventions for alcohol in general practice. BMJ. 2017;356:j116. doi: 10.1136/bmj.j116. https://doi.org/10.1136/bmj.j116. [DOI] [PubMed] [Google Scholar]
- 41.Tansil KA, Esser MB, Sandhu P, et al. Alcohol electronic screening and brief intervention: a Community Guide Systematic review. Am J Prev Med. 2016;51(5):801–811. doi: 10.1016/j.amepre.2016.04.013. https://doi.org/10.1016/j.amepre.2016.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.CDC. [Accessed October 24, 2016];Fetal alcohol spectrum disorders: training & education. 2016 www.cdc.gov/ncbddd/fasd/training.html.
- 43.McKnight-Eily LR, Okoro CA, Mejia R, et al. Screening for excessive alcohol use and brief counseling of adults—17 states and the District of Columbia, 2014. MMWR Morb Mortal Wkly Rep. 2017;66(12):313–319. doi: 10.15585/mmwr.mm6612a1. https://doi.org/10.15585/mmwr.mm6612a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Nelson DE, Jarman DW, Rehm J, et al. Alcohol-attributable cancer deaths and years of potential life lost in the United States. Am J Public Health. 2013;103(4):641–648. doi: 10.2105/AJPH.2012.301199. https://doi.org/10.2105/AJPH.2012.301199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Maheswaran R, Beevers M, Beevers DG. Effectiveness of advice to reduce alcohol consumption in hypertensive patients. Hypertension. 1992;19(1):79–84. doi: 10.1161/01.hyp.19.1.79. https://doi.org/10.1161/01.HYP.19.1.79. [DOI] [PubMed] [Google Scholar]
- 46.Baker AL, Thornton LK, Hiles S, Hides L, Lubman D. Psychological interventions for alcohol misuse among people with co-occurring depression or anxiety disorders: A systematic review. J Affect Disord. 2012;139(3):217–229. doi: 10.1016/j.jad.2011.08.004. https://doi.org/10.1016/j.jad.2011.08.004. [DOI] [PubMed] [Google Scholar]
- 47.Fleming M, Brown R, Brown D. The efficacy of a brief alcohol intervention combined with CDT feedback in patients being treated for Type 2 diabetes and/or hypertension. J Stud Alcohol. 2004;65(5):631–637. doi: 10.15288/jsa.2004.65.631. https://doi.org/10.15288/jsa.2004.65.631. [DOI] [PubMed] [Google Scholar]
- 48.Wilson GB, Wray C, McGovern R, et al. Intervention to reduce excessive alcohol consumption and improve comorbidity outcomes in hypertensive or depressed primary care patients: two parallel cluster randomized feasibility trials. Trials. 2014;15:235. doi: 10.1186/1745-6215-15-235. https://doi.org/10.1186/1745-6215-15-235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.López-Pelayo H, Miquel L, Altamirano J, Blanch JL, Gual A, Lligoña A. Alcohol consumption in upper aerodigestive tract cancer: Role of head and neck surgeons’ recommendations. Alcohol. 2016;51:51–56. doi: 10.1016/j.alcohol.2016.01.002. https://doi.org/10.1016/j.alcohol.2016.01.002. [DOI] [PubMed] [Google Scholar]
- 50.Cotter T, Perez D, Dunlop S, Kite J, Gaskin C. Knowledge and beliefs about alcohol consumption, longer-term health risks, and the link with cancer in a sample of Australian adults. N S W Public Health Bull. 2013;24(2):81–86. doi: 10.1071/NB12089. https://doi.org/10.1071/NB12089. [DOI] [PubMed] [Google Scholar]
- 51.Buykx P, Li J, Gavens L, et al. Public awareness of the link between alcohol and cancer in England in 2015: a population-based survey. BMC Public Health. 2016;16:1194. doi: 10.1186/s12889-016-3855-6. https://doi.org/10.1186/s12889-016-3855-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Merten JW, Parker A, Williams A, King JL, Largo-Wight E, Osmani M. Cancer risk factor knowledge among young adults. J Cancer Educ. doi: 10.1007/s13187-016-1093-3. In press. Online August 6, 2016. https://doi.org/10.1007/s13187-016-1093-3. [DOI] [PubMed]
- 53.Wellard L, Corsini N, Hughes C. Discussing alcohol and cancer with patients: knowledge and practices of general practitioners in New South Wales and South Australia. Aust Fam Physician. 2016;45(8):588–593. [PubMed] [Google Scholar]
- 54.Okuyemi KS, Nollen NL, Ahluwalia JS. Interventions to facilitate smoking cessation. Am Fam Physician. 2006;74(2):262–271. [PubMed] [Google Scholar]
- 55.National Academy of Medicine. Individuals and families: models and interventions. Health and Behavior: The Interplay of Biological, Behavioral, and Societal Influences. Washington, DC: National Academies Press; 2001. www.ncbi.nlm.nih.gov/books/NBK43749/ [PubMed] [Google Scholar]
- 56.Liu Y, Croft JB, Wheaton AG, Kanny D, Cunningham TJ, Lu H. Clustering of five health-related behaviors for chronic disease prevention among adults, United States, 2013. Prev Chron Dis. 2016;13:160054. doi: 10.5888/pcd13.160054. https://doi.org/10.5888/pcd13.160054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.McDonald JA, Goyal A, Terry MB. Alcohol intake and breast cancer risk: Weighing the overall evidence. Curr Breast Cancer Rep. 2013;5(3):208–221. doi: 10.1007/s12609-013-0114-z. https://doi.org/10.1007/s12609-013-0114-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Chang JS, Straif K, Guha N. The role of alcohol dehydrogenase genes in head and neck cancers: a systematic review and meta-analysis of ADH1B and ADH1C. Mutagenesis. 2012;27(3):275–286. doi: 10.1093/mutage/ger073. https://doi.org/10.1093/mutage/ger073. [DOI] [PubMed] [Google Scholar]
- 59.Hendershot CS, Otto JM, Collins SE, Liang T, Wall TL. Evaluation of a brief web-based genetic feedback intervention for reducing alcohol-related health risks associated with ALDH2. Ann Behav Med. 2010;40(1):77–88. doi: 10.1007/s12160-010-9207-3. https://doi.org/10.1007/s12160-010-9207-3. [DOI] [PMC free article] [PubMed] [Google Scholar]