Abstract
Background
Medicinal plants are the basic source of health care in the Pearl Valley District Poonch, Azad Jammu, and Kashmir. The basic aim of present study was to record information about the use of plants in herbal preparation and quantification of recorded data.
Materials and methods
The research was conducted with the null hypothesis that there was no differential distribution of knowledge among the communities between genders and among different age groups in the study area and across cultural medicinal uses of the plants are similar. To check these hypotheses information about medicinal plants was collected from 46 laypeople and 18 herbalists by using an open ended and semistructured questionnaire. Different ethnobotanical indices were calculated in order to quantify the knowledge on the medicinal plants reported in the study.
Results
Our study recorded 136 species of medicinal plants belonging to 45 families with Asteraceae (14 species) as the dominant family of the area. Decoction (26 species), juice and powder (24 species each) were most common methods of preparation. Spearman’s correlation analysis showed that age and gender had the significant effect on both numbers of mentioned species and different uses. A number of known medicinal plants and the number of different uses (H: 38.51; p < 0.001) differ significantly as indicated by Kruskal-Wallis tests. These results showed that the knowledge about the plant varies among different age groups, which were the first hypothesis of the present study. The highest use values (UVs) were reported for Berberis lyceum and Ajuga bracteosa (1.13 each) followed by Abies pindrow (1.03). Highest informant consensus factor (ICF) values were recorded for digestive system diseases (ICF = 0.90) and muscular and skeletal system diseases (ICF = 0.89). The value of Jaccarad index ranged from 6.11 to 32.97 with an average value of 19.84, percentage of similarity was highest between study area and Pir Lasura National Park (34.62%).
Conclusion
High similarity might be due to the fact that the communities living in these areas have same sociocultural values and have more opportunities to exchange their traditional knowledge. The present study provides practical evidence about the use of medicinal plants among the inhabitants of the Pearl Valley.
Introduction
Ethnobiological knowledge consists of the body of knowledge, beliefs, traditions, and practices that reflect the perception of the local environment by indigenous communities. Within the field of ethnobiology, several pieces of research have been devoted to the study of plants used for medical purposes, one of the oldest forms of ethnobotanical and ethnomedical research known [1–3].
Quantitative ethnobotany may be defined as "the application of quantitative techniques to the direct analysis of contemporary plant use data" [4, 5]. Quantification and associated hypothesis-testing help to generate quality information, which in turn contributes substantially to resource conservation and development. Further, the application of quantitative techniques to data analysis necessitates refinement of methodologies for data collection. Close attention to methodological issues not only improves the discipline of ethnobotany but also enhances the image of ethnobotany among other scientists " [4, 5]. This paper attempts to highlight these unexpected patterns of ethnobotanical knowledge across age, gender and method used.
The variables known to affect medicinal plant knowledge include education, occupation, age, gender and psychosocial variables [6–10]. Age and gender are generally the factors most examined for their influence on knowledge about plants. One of the most studied resources is medicinal plant knowledge because it is a structural component of local medical systems [11]; it is the focus of this study. Much of this knowledge is traditional, that is, learned long ago and passed on with varying degrees of faithfulness for at least two or three generations. However, ethnobiological knowledge can change rapidly. Every tradition had a beginning cf. [12], and was itself a new creation in its time. Ecosystems change, new plants and animals arrive, and people learn new ways of thinking; ethnobiological systems change accordingly, and are typically flexible and dynamic. Field-workers have observed new knowledge being incorporated into systems around the world.
Divergences in knowledge and practice between two cultural groups that live within the same ecosystem are intriguing as they can provide insight into how the lens of culture can not only alter human viewpoints of the environment but even guide human interactions with resources embedded in the ecosystem. To explore the question of what role culture plays in shaping the human–nature interface, we conducted field research in Pearl Vellay in Rawalakot that hosts an incredibly rich repertoire of cultural, linguistic and biological diversity. We hypothesize that two distinct cultural groups living in the same ecosystem will share a similar pattern of use of wild flora for daily subsistence and medical practices, and that distinctions will arise only for those taxa that play a key role in culture-specific ritual, food or health practices [13].
Researchers have previously studied the association between ethnobotanical knowledge and socio-economic factors. Among the factors previously studied researchers have focused on the age [4, 6, 14, 15], sex, the educational level, origin, and the occupation and the wealth of informantion of informents. Among those, researchers have found that those having a stronger influence on shaping ethnobotanical knowledge distribution are age, sex, education level and wealth.
For example, several studies have found a positive association between age and traditional ethnobotanical knowledge [14], although some other studies have not found such association [6]. In contrast, the differences in ethnobotanical knowledge between men and women seem to be more consistent, with studies finding that men have a larger knowledge than women [6, 14, 16, 17], although the trend seems to be inverse in relation to medicinal plants [18]. Such differences are generally explained by sexual distribution of work [19]. Some research also suggest that ethnobotanical knowledge decreases with the increase of education [15, 20–22] and wealth. Several of those characteristics are also linked to the process of acculturation and the loss of indigenous languages (among indigenous communities) [15, 20, 22]. Some studies highlight the importance of occupation on traditional knowledge [21, 23]. Martínez-Ballesté et al. [21] find that larger involvement in agricultural activities resulted in a loss of traditional ecological knowledge, as a consequence of the environmental transformation and loss of biodiversity. In contrast, those activities more dependent on the natural environment are associated to maintenance of traditional knowledge.
Given those previous findings, we hypothesize that the distribution of traditional knowledge will be patterned across socio-economic characteristics. Specifically, we expect to find that men, older people, people born in the area, and poorer people will have higher levels of traditional knowledge than people without those characteristics. We also hypothesize that people whose occupation depends on the environment, like people who practice extensive agriculture and stockbreeding, might also have larger levels of traditional knowledge.
Ethnobotanical knowledge in Poonch Valley (an administrative division of Azad Jammu and Kashmir) has been scarcely investigated, with the exception of a few studies [24–27] Local people have developed a rich ethnobotanical knowledge and use medicinal plants for treating several common diseases. In particular, traditional healers or herbalists play an important role in ensuring some health service to 75% of the rural population [28]. The study was aimed to record and discuss knowledge on medicinal plant uses in the local traditional practices, including (i) Description of preparation and use of plants as medicines. (ii) The differential distribution of knowledge about plants and medinal properties among sectors of the society, and (iii) identifying new forms of use compared with those reported for other neighbouring areas.
Materials and methods
Study area
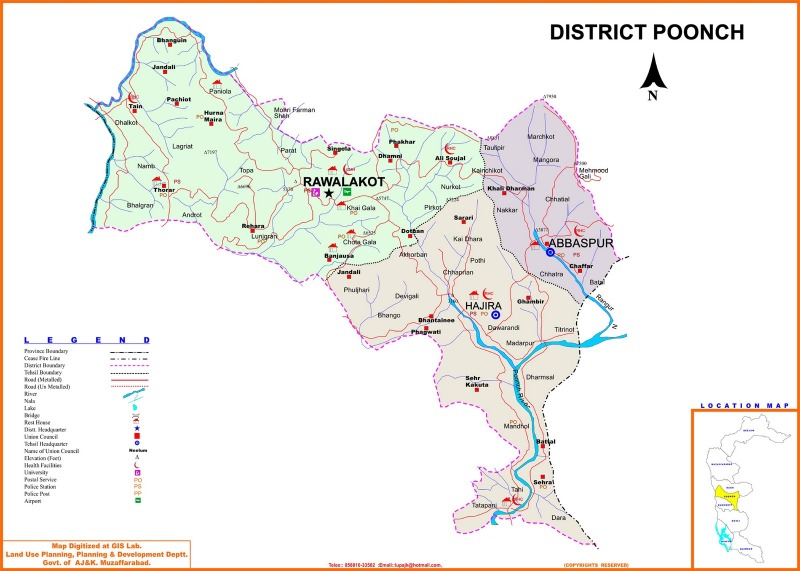
The study has been carried out in Rawalakot, also known as Pearl Valley, located in the core of Poonch district (Latitude 33°51'32.18"N, Longitude 73° 45'34.93"E) “Fig 1”. It is a saucer-shaped valley with an altitude of 1615 m a.s.l. The climate can be classified as subtropical highland (Cwa) under the Köppen climate classification due to high altitude. The average annual temperature is 15.3°C ranging from 38°C during the mid-summer months to– 3°C during the winter months. The annual rainfall is very variable year by year and ranges from 500 to 2000 mm, most of which is irregular and falls as intense storms during the monsoon season stretching from July to September. Woodlands, dominated by conifers such as Abies pindrow, Cedrus deodara, Pinus roxburghii, and Pinus wallichiana, and open grasslands, mainly cover the area.
Fig 1. Map of the study area (http://www.pakimag.com/politics/by-election-la-22-sidhnoti-poonch-ajk-assembly.html/attachment/district-poonch-azad-kashmir-detail-map).
The ethnic composition of the region is quite diverse and complex: Gujjars, Sudhans, Rajputs and Jats are considered to be the major ethnic groups living in the area. Gujjars are the largest group; Rajputs who are spread across the region and Sudhans, mostly settled in Rawalakot, are regarded as the influential ethnic groups in Azad Kashmir. Almost all of them are Muslims. According to the last census in 2014 there are 4,980 households in Rawalakot and each household comprises an average of 7.6 members. This high demographic density can be explained by the higher work opportunities in Rawalakot where most dwellers are engaged, directly or indirectly, with the tourism sector. In contrast, the rural population largely depends on subsidence agriculture, livestock, forestry and formal employment. Agriculture is based on rain-fed cropping system and the main crop of the region is maize.
Ethnobotanical data collection
Fieldwork was carried out from August 2013 to July 2014. Before initiating of our survey Ethical approval for the study was obtained from the COMSATS Institute of Information Technology ethics Committee. Legal permission was taken from representatives of the municipality for conducting the interview. All respondents were asked to sign a prior informed- consent form after the objectives and possible consequences of the study had been explained. The prior informed consent (PIC) form was translated into the local Pothwari language. Ethnobotanical information was collected from native inhabitants of the valley by using semi-structured questionnaires. This method allows a large number of participants to be interviewed in a relatively short period of time by asking the same questions within a flexible framework. All the interviews were carried out in the local dialect, Pothohari. A total of 64 informants, ranging in age from 35 to 70 years, were selected by convenience sampling (i.e., a sampling method in which units are selected based on easy access or availability) “Table 1”.
Table 1. Medicinal Flora of Pearl Valley Tehsil Rawalakot, District Poonch AJ&K.
| Scientific Name and voucher number | Local name and habit | Family | Part Used | Method of preparation/property | Mode of application | Disease treated | FC | RFC | UV | |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Abies pindrow Royle (HF-99) | Partal, Paluder silver fir, Tree | Pinaceae | Leaf | paste | External | Swelling | 48 | 0.75 | 1.03 |
| Juice | Internal | Antypiretic | ||||||||
| Bark | Powder | Internal | Cough chronic asthma. | |||||||
| Bark | Tea | Internal | Rheumatism | |||||||
| Resin | Resin | External | Wounds. | |||||||
| Root | Decoction | Internal | Cough, bronchitis | |||||||
| 2 | Achillea millefolium L. (HF-77) | Yarrow, Herb | Asteraceae | Flower | Extract | Internal | Refrigerante | 24 | 0.38 | 0.33 |
| Leaves | Powder | External | Toothache | |||||||
| 3 | Achyranthes aspera var. perphyristachya Hook. F. (HF-128) | Puth kanda, Herb | Amaranthaceae | Root | Decoction | Internal | Inflammation | 21 | 0.33 | 0.38 |
| Leaves | Pain | |||||||||
| 4 | Adhatoda zeylanica L. (HF-139) | Bahkar, Herb | Acanthaceae | Bark | Powder | Internal | Stomachache | 35 | 0.55 | 0.59 |
| Constipation | ||||||||||
| Leaves | Asthma | |||||||||
| Root | Cough | |||||||||
| 5 | Adiantum capillus-veneris L. (HF-101) | Hansraj, Sraj fern | Adiantaceae | Leaves | Decoction | Internal | Cough | 57 | 0.89 | 0.97 |
| Boils | ||||||||||
| Asthma | ||||||||||
| Jaundice | ||||||||||
| Fever | ||||||||||
| Diabetes | ||||||||||
| Eczema | ||||||||||
| Measles | ||||||||||
| Chest pain | ||||||||||
| 6 | Adiantum incisum Foressk (HF-120) | Sumbul, Hansraj, Fern | Leaves | Juice | Internal | Scabies | 44 | 0.69 | 0.64 | |
| Cough | ||||||||||
| Antypiretic | ||||||||||
| Bodyache | ||||||||||
| 7 | Aesculus indica (Wall.ex Camb.) Hook.f. (HF-91) | Bankhore, Horsechestnut, Tree | Hippocastanaceae | Bark | Infusion | Internal | Tonic | 33 | 0.52 | 0.5 |
| Fruits | Eaten | Internal | Colic, Rheumatim | |||||||
| Seed | Powder | Internal | Leucorrhoea | |||||||
| 8 | Ajuga bracteosa Wall, ex Benth (HF-82) | Ratti booti, Herb | Lamiaceae | Aerial parts | Extract | Internal | Blood purifier | 58 | 0.91 | 1 |
| Pimples | ||||||||||
| Eruption | ||||||||||
|
Leaves |
Extract |
Internal |
Inflammation | |||||||
| Earache | ||||||||||
| Pain | ||||||||||
| Toothache | ||||||||||
| Boils | ||||||||||
| 9 | Albizia lebbeck L. Bth. (HF-89) | Shirin, Tree | Mimoaceae | Seeds | External | Inflammation | 57 | 0.89 | 0.83 | |
| Leukoderma | ||||||||||
| Leprosy | ||||||||||
| Eczema | ||||||||||
| Bark | Powdered | External | Strengthen spongy gums | |||||||
| Bark and seeds | Extract | Internal | Haemorroids | |||||||
| Dysentery | ||||||||||
| Diarrhea | ||||||||||
| Flowers | Paste | External | Carbuncles | |||||||
| Eczema | ||||||||||
| Swelling | ||||||||||
| Boils | ||||||||||
| Seed | Oil | External | Snake bite | |||||||
| Asthma | ||||||||||
| 10 | Allium griffithianum Boiss (HF-83) | Piazi, Herb | Alliaceae | Aerial parts | Cooked | Internal | Carminative | 29 | 0.45 | 0.53 |
| Dyspepsia | ||||||||||
| Pain | ||||||||||
| 11 | Alysicarpus bupleurifolius L. D.C (HF-84) | Buffalo clover, Herb | Paplionaceae | Leaves | Juice | Internal | Blood purifier | 15 | 0.23 | 0.22 |
| 12 | Anaphalis adnata D.C (HF-20) | Dialect, Herb | Asteraceae | Leaves | Powder | External | Bleeding | 19 | 0.3 | 0.42 |
| Wound | ||||||||||
| 13 | Androsace rotundifolia Hardwicke (HF-10) | Thandi jari, Herb | Primulaceae | Rhizome | Extract | Internal | Ophthalmic | 25 | 0.39 | 0.67 |
| Leaves | Infusion | Internal | Stomachache | |||||||
| Emetic | ||||||||||
| 14 | Anemone tetrasepala Royle (HF-61) | Herb | Ranunculaceae | Roots | Juice | External | Boils | 12 | 0.19 | 0.34 |
| 15 | Aquilegia pubiflora Wall ex Royle. (HF-61) | Herb | Ranunculaceae | Root | Paste | External | Snake bite | 37 | 0.58 | 0.45 |
| Toothache | ||||||||||
| Emetic | ||||||||||
| Flower | Paste | External | Skin burns | |||||||
| Wound | ||||||||||
| 16 | Artemisia absinthium L. (HF-46) | Afsanthene, Herb | Asteraceae | Leaves | Infusion, paste | Internal | Anthelmintic | 51 | 0.8 | 0.98 |
| Cuts | ||||||||||
| Wounds | ||||||||||
| Stomach disorders | ||||||||||
| Pain | ||||||||||
| 17 | Artemisia dubia Wall. ex Bess. (HF-17) | Asfanthene, Herb | Asteraceae | Seeds | Cooked | Internal | Weakness after delivery. | 23 | 0.36 | 0.52 |
| Leaves | Paste | External | Cuts | |||||||
| Ear diseases | ||||||||||
| Wounds | ||||||||||
| Aerial parts | External | External | Vermicide | |||||||
| 18 | Artemisia maritime L. (HF-16) | Afsanthene, Herb | Asteraceae | Leaves | Paste | External | Skin infections. | 41 | 0.64 | 0.77 |
| Leaf and stem | Powder | Internal | Intestinal parasites. | |||||||
| 19 | Asparagus filicinus Ham. in D.Don (HF-23) | Macher ghas, Herb | Liliaceae | Root | Decoction | Internal | Nervous stimulant. | 38 | 0.59 | 0.66 |
| 20 | Athyrium tenuifrons Wall.apud Moore ex. R.Sim (HF-123) | Dandasa, Fern | Adiantaceae | Root | Tea | Internal | Bodyache | 32 | 0.5 | 0.58 |
| Root | Powder | External | Wound | |||||||
| 21 | Berberis aristata DC. (HF-26) | Doody, Indian barberry, Herb | Berberidaceae | Bark |
Tooth stick | External | Mouth Inflammation | 21 | 0.33 | 0.38 |
| Leaves | Decoction | Internal | Backache | |||||||
| Fruit | Paste | External | Dental, Prophylaxis | |||||||
| 22 | Berberis lycium Royle (HF-81) | Sumblu, Shrub | Berberidaceae | Roots | Extract | Internal | Tonic | 59 | 0.92 | 0.98 |
| Pustules | ||||||||||
| Hemorrhoids | ||||||||||
| Diabetes | ||||||||||
| Eye lotion | ||||||||||
|
Roots |
Paste |
External |
Skin disease | |||||||
| Chronic diarrhea | ||||||||||
| Blood purifier | ||||||||||
| Scabies | ||||||||||
| Fracture | ||||||||||
| 23 | Bergenia ciliata (Haw.)Sternb. (HF-18) | Zakhm-e-Hayat, Herb | Saxifragaceae | Aerial parts | Powder | Internal | Urinary tract troubles | 29 | 0.45 | 0.39 |
| Earache | ||||||||||
| Leaves | Juice | External | Cough | |||||||
| Root | Juice | Internal | Cold | |||||||
| Kidney stones | ||||||||||
| 24 | Calendula officinalis L. (HF-138) | Sadberga, Herb | Asteraceae | Young branches |
Extract | Internal | Kidney stones | 46 | 0.72 | 0.98 |
| 25 | Calotropis procera (Aiton) W.T.Aiton (HF-59) | Ak, Shurb | Asclepiadaceae | Latex | Latex | External | Aphrodisiacs | 35 | 0.55 | 0.59 |
| Root | Power | Internal | Boils | |||||||
| 26 | Caltha alba var. alba Camb. var. alba (HF-26) | Herb | Ranunculaceae | Aerial parts | Juice | Internal | Antispasmodic | 29 | 0.45 | 0.28 |
| Sedative | ||||||||||
| 27 | Campanula benthamii Wall. (HF-63) | Herb | Companulaceae | Root | Chewing | External | Strengthen heart | 19 | 0.3 | 0.36 |
| Earach | ||||||||||
| 28 |
Carissa opaca Stapf. ex Haines (HF-32) |
Garanda, Small tree | Apocynaceae | Fruit | Powder | Internal | Pain | 35 | 0.55 | 0.59 |
| Stem | Inflammation | |||||||||
| 29 | Carthamus tinctorius L. (HF-42) | Kasumba (zafran) | Astreaceae | Flowers | Rubbing | Internal | Pneumonia | 29 | 0.45 | 0.66 |
| Boil | External | |||||||||
| 30 | Castanea sativa Mill. (HF-19) | Chita sanghara, Chest nut, Tree | Fagaceae | Leaves | Infusion | Internal | Antypiretics | 21 | 0.33 | 0.38 |
| Leaves | Decoction | Internal | ||||||||
| Pharyngitis | ||||||||||
| 31 | Cedrela serrata Royle. (HF-24) | Drawa, Tree | Melliaceae | Stem and bark | Paste | External | Round worms. | 54 | 0.84 | 0.83 |
| Root | Juice | Internal | Dyspepsia, Diabetes | |||||||
| Leaves | Decoction | External | Refrigerante shampoo | |||||||
| Bark | Poultice | Internal | Ulcers | |||||||
| Bark | Powder | Internal | Chronic infantile dysentery. | |||||||
| 32 | Celtis caucasica Willd (HF-72) | Batkaral, Tree | Ulmaceae | Aerial parts | Juice | Internal | Pain, Amenorrhea. | 17 | 0.27 | 0.45 |
| 33 | Cichorium intybus L. (HF-142) | Kahsni, Herb | Asteraceae | Roots | Juice | Internal | Antypiretic | 33 | 0.52 | 0.73 |
| 34 | Clematis buchananiana DC. (HF-84) | Langi, Shrub | Ranunculaceae | Leaves | Paste | External | Eczema | 43 | 0.67 | 0.75 |
| Psoriasis (type of skin diseases) | ||||||||||
| Wound | ||||||||||
| Roots | Crushing and wrapping | External | Bleeding | |||||||
| Roots | Poultice Juice |
External Internal |
Swellings, inflammation | |||||||
| Peptic ulcers | ||||||||||
| 35 | Clematis montana Buch. (HF-118) | Langi, Shrub | Ranunculaceae | Leaves | Extract | Internal | Diabetes | 27 | 0.42 | 0.33 |
| Flowers | Decoction | Internal | Cough | |||||||
| 36 | Conyza bonariensis (L.) Cronq. (HF-51) | Buti, Herb | Asterceae | Aerial parts | Infusion | Internal | Diarrhea | 41 | 0.64 | 0.77 |
| Haemorroids | ||||||||||
| Dysentery | ||||||||||
| 37 | Cuscuta reflexa Roxb. (HF-131) | Neela dari, Climber | Cuscutaceae | Whole plant | Juice | Internal | Jaundice | 21 | 0.33 | 0.38 |
| External | Dandruff | |||||||||
| 38 | Dalbergia sissoo Roxb. (HF-09) | Tahli, Tree | Fabaceae | Stem bark | Juice | External | Eczema | 39 | 0.61 | 0.77 |
| Crushed leaves | Juice | Internal | Blood purifier | |||||||
| Leaves | Washing | External | Increase hair length | |||||||
| 39 | Debregeasia salicifolia D.Don Rendle (HF-78) | Sandari, Shrub | Urticaceae | Aerial parts | Paste | External | Eczema, dermatitis | 15 | 0.23 | 0.41 |
| 40 | Desmodium polycarpum DC. (HF-83) | Mangkit-parang, Shrub | Paplinioaceae | Roots | Juice | Internal | Antypiretic | 34 | 0.53 | 0.88 |
| Helminthiasis | ||||||||||
| Haemorroid | ||||||||||
| Antypiretic | ||||||||||
| Cough | ||||||||||
| Cardiac tonic | ||||||||||
| Diuretic | ||||||||||
| Loss of appetite | ||||||||||
| Carminative | ||||||||||
| Diarrhea | ||||||||||
| Dysentery | ||||||||||
| 41 | Desmostachya bipinnata L. Stapf. (HF-13) | Dab, Grass | Poaceae | Roots | Tea | Internal | Hypertension | 14 | 0.22 | 0.17 |
| 42 | Dicliptera bupleuroides Nees (HF-58) | Kirch, Somni, Herb | Acanthaceae | Leaves | Paste | External | Wounds | 52 | 0.81 | 0.86 |
| Eczema | ||||||||||
| Leaves | Decoction | External | Tonic | |||||||
| Cough | ||||||||||
| 43 | Dioscorea bulbifera L. (HF-57) | Herb | Dioscoreaceae | Aerial parts | Juice | Internal | Contraceptive. | 41 | 0.64 | 0.81 |
| 44 | Dioscorea deltoideaWall. ex Kunth (HF-50) | Herb | Dioscoreaceae | Rhizome | Taken as raw form | Internal | Insect killer | 36 | 0.56 | 0.48 |
| Snake bite | ||||||||||
| 45 | Duchesnea Andrews) Focke (HF-84) | Budimewa, Herb | Rosaceae | Fruit | Juice | Internal | Eye Infection | 33 | 0.52 | 0.61 |
| Tonic | ||||||||||
| 46 | Elaeagnus angustifolia L. (HF-92) | Sinjit, Tree | Elaeagnaceae | Ripe fruits | Boiled | Internal | Pharyngitis, Antypiretic | 29 | 0.45 | 0.66 |
| Fruit | Taken as raw form | Internal | Cough Fever |
|||||||
| 47 | Elaeagnus umbellata Thunb. (HF-94) | Chota zaton, Russian olive, Tree | Elaeagnaceae | Leaves | Decoction | Internal | Cough | 33 | 0.52 | 0.73 |
| Flowers | Decoction | Internal | Heart diseases. | |||||||
| Seeds | Taken as raw form | Internal | Immunity | |||||||
| Branch | Exude | External | Toothache | |||||||
| 48 | Eriobotrya japonica Thumb. Lindler (HF-55) | Loquat, Tree | Rosaceae | Leaves | Poultice | External | Swellings. | 44 | 0.69 | 0.89 |
| Fruits | Taken as raw form | Internal | Sedative | |||||||
| Emetic | ||||||||||
| Leaves | Infusion | Internal | Relieve diarrhea. | |||||||
| Flowers | Infusion | Internal | Refrigerante | |||||||
| 49 | Euphorbia helioscopia L. (HF-87) | Dhodhal, Dandlion, Herb | Euphorbiaceae | Seeds | Juice | Internal | Cholera | 49 | 0.77 | 0.72 |
| Roots | Paste | Internal | Anthelmintic | |||||||
| 50 | Euphorbia wallichii Hk.f (HF-80) | Dhodhal Dandlion, Herb | Euphorbiaceae |
Aerial parts |
Latex Juice |
Internal |
Purgative | 42 | 0.66 | 0.91 |
| Dyspepsia | ||||||||||
| Purgative | ||||||||||
| Warts | ||||||||||
| Skin infections | ||||||||||
| 51 | Ficus carica L. (HF-54) | Phagwar, Tree | Moraceae | Fruit | Taken as raw form | Internal | Stomachache | 52 | 0.81 | 0.95 |
| Haemorroids | ||||||||||
| Cystitis | ||||||||||
| Anemia | ||||||||||
| Constipation | ||||||||||
| Leaves | Latex | External | Wounds | |||||||
| Latex | Rubbing | External | Extract thorns from feet or other body organs. | |||||||
| 52 | Ficus palmate Forssk. (HF-32) | Phaghwar, Anjir, Tree | Moraceae | Fruit | Taken as raw form | Internal | Demulcent | 37 | 0.58 | 0.84 |
| Purgative | ||||||||||
| Lungs diseases | ||||||||||
| Refrigerante | ||||||||||
| Cystitis | ||||||||||
| Aerial parts | Paste | External | Freckles | |||||||
| Latex | External | Eczeema | ||||||||
| 53 | Fragaria nubicola Lindl. ex Lacaita (HF-87) | Budi meva, Wild Straberry, Herb | Rosaceae | Fruit | Chewed | Internal | Purgative | 35 | 0.55 | 0.5 |
| Mouth infection | ||||||||||
| Purgative | ||||||||||
| 54 | Fumaria indica (Hausskn.) Pugsley (HF-48) | Papra, Herb | Fumaricaceae | Aerial parts | Juice, Paste | Internal | Antypiretic | 48 | 0.75 | 0.84 |
| Skin infection | ||||||||||
| Purify blood | ||||||||||
| Pimples, | ||||||||||
| Constipation | ||||||||||
| Eczima | ||||||||||
| 55 | Galium aparine L. (HF-40) | Lainda, Herb | Rubicaceae | Aerial parts | Powder | External | Bleeding | 15 | 0.23 | 0.31 |
| 56 | Galium asperifolium Wall (HF-80) | Lainda, Herb | Rubicaceae | Aerial parts | Juice | Internal | Diuretic | 22 | 0.34 | 0.38 |
| Kidney Infections | ||||||||||
| 57 | Gerbera gossypina (Royle) Beauverd (HF-65) | Put Potula, Herb | Asteraceae | Leaves | Paste | External | Skin diseases | 37 | 0.58 | 0.66 |
| Bone fracture | ||||||||||
| Wounds and cuts | ||||||||||
| Pain | ||||||||||
| 58 | Hedera nepalensis K. Koch (HF-112) | Harbumbal epiphyte | Araliaceae | Leaves | Decoction | Internal | Diabetes | 11 | 0.17 | 0.13 |
| 59 | Heracleum cachemirica C.B. Clarke (HF-76) | Tukar, Shrub | Apiaceae | Aerial parts | Juice | Internal | Nerve disorders. | 18 | 0.28 | 0.19 |
| Nausea | ||||||||||
| 60 | Heracleum candicans Wall ex. DC (HF-85) | Herb | Apiaceae | Aerial parts | Tea | Internal | Nerve disorders. | 12 | 0.19 | 0.14 |
| 61 | Hypericum perforatum L. (HF-02) | Herb | Guttiferae | Flowers | Infusion | Internal | Snake bite | 47 | 0.73 | 0.61 |
| Wounds | ||||||||||
| Swellings | ||||||||||
| Rheumatism | ||||||||||
| Sores | ||||||||||
| Ulcers | ||||||||||
| 62 | Ipomoea carnea Jac. (HF-142) | Jungli bakhir, Shurb | Convolvulaceae | Leaves | Paste | External | Athlete foot. | 33 | 0.52 | 0.73 |
| 63 | Isodon rugosus (Wall.ex.Benth.) Codd. (HF-35) | Khwangere, Shrub | Lamiaceae | Leaves | Decoction | Internal | Blood pressure | 37 | 0.58 | 0.75 |
| Toothache | ||||||||||
| Fever | ||||||||||
| Rheumatism | ||||||||||
| 64 | Jasminum mesnyi Hance (HF-70) | Pili chambali, Shrub | Oleaceae | Leaves | Powder | External | Dandruff | 51 | 0.80 | 0.67 |
| Pains | ||||||||||
| Leaves | Chewing | Internal | Mouth ulcers | |||||||
| Leaves | Decoction | Internal | Pyorrhea | |||||||
| Branches | Ash | External | Headache | |||||||
| Joint pain | ||||||||||
| Dried flower | Powder | Internal | Hepatic disorders. | |||||||
| 65 | Juglans regia L. (HF-71) | Akhrot, Khore, Tree | Juglandaceae | Leave | Decoction | External | Antispasmodic | 51 | 0.8 | 0.92 |
| Bark | Rubbing | External | Prophylaxis | |||||||
| Lips and gums dye | ||||||||||
| Seeds | Oil | External | Rheumatim | |||||||
| Roots and leaves | Powder | External | Antiseptic | |||||||
| 66 | Launaea taraxacifolia (Willd.) Amin (HF-134) | Hand, Herb | Asteraceae | Whole plant | Taken as raw form | Internal | Diabetes | 29 | 0.45 | 0.66 |
| Pain | ||||||||||
| 67 | Lepidium sativum L. (HF-136) | Haleon, Herb | Brassicaceae | Seeds | Cooked | Internal | Backache | 17 | 0.27 | 0.45 |
| 68 | Lespedeza juncea L.f. (HF-06) | Herb | Paplionaceae | Root | Juice | Internal | Diarrhea | 26 | 0.41 | 0.38 |
| Dysentery | ||||||||||
| 69 | Ligustrum lucidum Ait.f. (HF-111) | Guliston, Shrub | Oleaceae | Aerial parts | Extracts | Internal | Antitumor | 23 | 0.36 | 0.5 |
| 70 | Malvastrum coromandelianum (L.) Garcke (HF-03) | Herb | Malvaceae | Aerial parts | Decoction | Internal | Kill worms | 38 | 0.59 | 0.41 |
| Dysentery | ||||||||||
| 71 | Melilotus alba Desr (HF-04) | Herb | Papilionaceae | Leaves | Paste | External | Joint inflammation. | 15 | 0.23 | 0.3 |
| 72 | Mentha royleana subsp. hymalaiensis Briq. (HF-07) | Podina, Herb | Lamiaceae | Leaves | Juice, Powder to make chattni | Internal | Stomach disorder | 58 | 0.91 | 0.97 |
| Cough | ||||||||||
| Antypiretic | ||||||||||
| Cholera | ||||||||||
| Emetic | ||||||||||
| Indigestion | ||||||||||
| Gas trouble | ||||||||||
| 73 | Momordica charantia L. (HF-129) | Khrella, Climber | Cucurbitaceae | Fruit | Juice | Internal | Diabetes | 21 | 0.33 | 0.38 |
| Pain | ||||||||||
| Leaves | External | Swelling | ||||||||
| 74 | Momordica dioica Roxb. ex Willd (HF-152) | Epiphyte | Cucurbitaceae | Roots | Cooked | Internal | Haemorroids | 15 | 0.23 | 0.17 |
| Urinary problem | ||||||||||
| 75 | Myrsine africana L. (HF-60) | Gorkhan, Chapra, Bebrang, Shrub | Myrsinaceae | Fruits | Powder | Internal | Stomachache | |||
| Purgative | ||||||||||
| Anthelmintic | ||||||||||
| Parminative | ||||||||||
| Leaves | Decoction | Internal | Blood purifier | |||||||
| 76 | Nepeta erecta (Boyle ex Benth.) Berth. (HF-50) | Herb | Lamiaceae | Flowers | Juice | Internal | Cough | 53 | 0.83 | 0.78 |
| Leaves | Juice | Internal | Blood | |||||||
| Pressure | ||||||||||
| Toothache | ||||||||||
| Flu | ||||||||||
| Antypiretic | ||||||||||
| Fever | ||||||||||
| 77 | Nepeta laevigata D.Don Hand (HF-53) | Herb | Lamiaceae | Fruit | Infusion | Internal | Dysentery | 17 | 0.27 | 0.22 |
| 78 | Nerium oleander L. (HF-37) | Kanair, Tree | Apocynaceae | Leave | Paste | External | Cutaneous eruption | 46 | 0.72 | 0.98 |
| Leave | Decoction | Internal | Wounds | |||||||
| Swelling | ||||||||||
| Bark | Decoction | Internal | Eczema, leprosy | |||||||
| Roots | Powder | Internal | Abortion | |||||||
| Roots | Paste | External | Scorpion sting, snakebite. | |||||||
| 79 | Oenothera rosea L.Her. ex. Ait (HF-91) | Buti, Herb | Onagraceae | Leaves | Infusion | Internal | Hepatic pain | 45 | 0.7 | 0.64 |
| Kidney disorders | ||||||||||
| 80 | Opuntia dillenii Haw. (HF-142) | Thor, Shurb | Cactaceae | Whole plant | Paste | External | Joints pain | 33 | 0.52 | 0.5 |
| 81 | Parthenium hysterophorus L. (HF-07) | Herb | Asteraceae | Root | Decoction | Internal | Eczema | 35 | 0.55 | 0.59 |
| Dysentery | ||||||||||
| 82 | Pimpinella stewartii Dunn. E.Nasir (HF-08) | Tarpakki, Herb | Apiaceae | Fruit | Taken as raw form | Internal | Stomachache | 12 | 0.19 | 0.3 |
| 83 | Pinus roxburgii Roxb (HF-94) | Chir, Tree | Pinaceae | Leaves bark Powder | Juice | Internal | Dysentery. | 58 | 0.91 | 1.13 |
| Resin | Poultice | Internal | Ulcer | |||||||
| Tumor | ||||||||||
| Bleeding | ||||||||||
| Cough | ||||||||||
| Snake bite | ||||||||||
| Wound | ||||||||||
| 84 | Pinus wallichiana A.B. Jackson (HF-58) | Biar, blue pine, Tree | Pinaceae | Resin | Poultice | External | Wound | 42 | 0.66 | 0.84 |
| 85 | Pistacia chinensis ssp. Integerrima (J. L. Stewart) Rech. f. (HF-22) | Kangar, Tree | Anacardiaceae | Stem gum | Powder | Internal | Dysentery. | 43 | 0.67 | 0.91 |
| Bark | Paste | External | Cracked heels | |||||||
| Wound | ||||||||||
| 86 | Plantago lanceolata L. (HF-88) | Ispgol, Herb | Plantaginaceae | Leaves | Paste | External | Wound | 53 | 0.83 | 0.91 |
| Seeds | Extract | Internal | Toothache | |||||||
| Purgative | ||||||||||
| Hemostatic | ||||||||||
| Dysentery | ||||||||||
| 87 | Poa nepalensis Walls ex. Duthie. (HF-131) | Grass | Poaceae | Leaves | Decoction mixed with water | External | Anti-lice | 29 | 0.45 | 0.42 |
| 88 | Podophyllum emodi Wall ex Royle (HF-87) | Banhakri Herb | Podophyllaceae | Root | Extract | Internal | Purgative, | 48 | 0.75 | 0.83 |
| Liver | ||||||||||
| Stomachache | ||||||||||
| 89 | Polygonatum multiflorum L. Smith (HF-78) | Herb | Liliaceae | Leave | Paste | External | Wound | 17 | 0.27 | 0.19 |
| 90 | Polystichum squarrosum (D. Don) Fée (HF-114) | Gha, Fern | Dryopteridaceae | Root | Decoction | Internal | Pyloricdisease | 13 | 0.2 | 0.3 |
| 91 | Prunella vulgaris L. (HF-63) | Herb | Lamiaceae | Seeds | Taken as raw form | Internal | Purgative | 58 | 0.91 | 0.98 |
| Antipyretic | ||||||||||
| Tonic | ||||||||||
| Eye sight weakness | ||||||||||
| Astama | ||||||||||
| Heart diseases | ||||||||||
| Inflammation | ||||||||||
| Diuretic | ||||||||||
| 92 | Prunus armeniaca L. (HF-24) | Hari, Khubani, Apricot, Tree | Rosaceae | Fruit | Taken as raw form | Internal | Purgative | 31 | 0.48 | 0.39 |
| Seed | Oil | External | Softening effect on the skin. | |||||||
| 93 | Prunus domestica L. (HF-31) | Lucha, Alu bukhara, Tree | Rosaceae | Fruit | Taken as raw form | Internal | Miscarriage | 34 | 0.53 | 0.84 |
| Irregular menstruation debility | ||||||||||
| 94 | Prunus persica L.Batch (HF-49) | Aru, Peach, Tree | Rosaceae | Leaves | Juice | Internal | Chest infection | 44 | 0.69 | 0.88 |
| Gastritis | ||||||||||
| Whooping cough | ||||||||||
| Bronchitis | ||||||||||
| Intestinal Anthalmatic | ||||||||||
| Anthalmatic for cattles | ||||||||||
| 95 | Pteris cretica L.(HF-158) | Cretan brake, Fern | Pteridaceae | Leaves | Paste | Internal | Wound | 9 | 0.14 | 0.17 |
| 96 | Punica granatum L. (HF-22) | Druna, Tree | Punicacea | Fruit | Taken as raw form | Internal | Cough, tonic | 52 | 0.81 | 1 |
| Leaves | Juice | Internal | Dysentery | |||||||
| Bark stem and root | Decoction | Internal | Mouthwash | |||||||
| Anthelmintic for tapeworms | ||||||||||
| Expectorant | ||||||||||
| 97 | Pyrus malus L. (HF-26) | Saib, Tree | Rosaceae | Fruit | Juice, paste | Internal | Rheumatism | 46 | 0.72 | 0.81 |
| Hypertension | ||||||||||
| Tonic for vigorous body | ||||||||||
| Fracails | ||||||||||
| Strengthen bones | ||||||||||
| Constipation | ||||||||||
| 98 | Pyrus pashia Ham.ex.D.Don (HF-17) | Butangi, Tree | Rosaceae | Fruit | Taken as raw form | Internal | Eye dark circles | 49 | 0.77 | 0.95 |
| 99 | Quercus baloot Griff (HF-90) | Rein, Shah baloot, Oak, Tree | Fagaceae | Bark | Powder | Internal | Asthma | 43 | 0.67 | 0.86 |
| Nut | Decoction | Internal | Urinary problems, cough, cold. | |||||||
| 100 | Quercus dilatata Royle (HF-68) | Oak, Barungi, Tree | Fagaceae | Fruit | Powder | Internal | Tonic | 47 | 0.73 | 0.36 |
| Bark | Decoction | Internal | Dysentery | |||||||
| 101 | Quercus incana Roxb. (HF-49) | Rein, Ban, Rinji, Tree | Fagaceae | Bark | Powder | Internal | Asthma | 41 | 0.64 | 0.95 |
| Antypiretic | ||||||||||
| Rheumatism | ||||||||||
| Backache | ||||||||||
| Cough | ||||||||||
| 102 | Ranunculus muricatus L. (HF-76) | Herb | Ranunculaceae | Aerial parts | Cooked | Internal | Asthma | 14 | 0.22 | 0.19 |
| 103 | Robinia pseudoacacia L. (HF-83) | Kikar, Tree | Papilionaceae | Bark | Chewing | External | Toothache | 31 | 0.48 | 0.8 |
| 104 | Rosa brunonii Lindl. (HF-121) | Chal, Tarni, Musk Rose, Shrub | Rosaceae | Flower | Decoction | Internal | Constipation | 49 | 0.77 | 0.84 |
| Flowers |
Powder |
Internal |
Diarrhea | |||||||
| Heart tonic | ||||||||||
| Eye diseases | ||||||||||
| Eczema | ||||||||||
| Wounds | ||||||||||
| 105 | Rubus fruticosus Hk f. non L (HF-50) | Garachey, Shrub | Rosaceae | Leaves | Infusion | Internal | Diarrhea | 57 | 0.89 | 0.98 |
| Antypiretic | ||||||||||
| Bark | Soaking | Internal | Diabetes | |||||||
| 106 | Rubus niveus Thunb. (HF-100) | Garachey, Shrub | Rosaceae | Leaves | Extract | External | Urticaria (skin disease) |
32 |
0.5 |
0.59 |
| Leaves | Powder | Internal | Diarrhea | |||||||
| Diuretic | ||||||||||
| Antypiretic | ||||||||||
| Root | Decoction | Internal | Dysentery | |||||||
| Colic pains | ||||||||||
| Whooping coughs | ||||||||||
| Diarrhea | ||||||||||
| 107 | Rumex dentatus L. (HF-101) | Jangli Palak Herb | Polygoneaceae | Leaves | Paste | External | Wound | 41 | 0.64 | 0.59 |
| Roots | Paste | External | Eczema | |||||||
| 108 | Rumex hastatus L. (HF-44) | Khatimal, Shrub | Polygonoceae | Roots | Juice | Internal | Asthma | 32 | 0.5 | 0.64 |
| Weakness in cattle | ||||||||||
| Antypiretic | ||||||||||
| Cough | ||||||||||
| 109 | Salix acmophylla Boiss. (HF-85) | Beens, Bed, Gaith, Tree | Salicaceae | Leaves | Paste, boiled with Robinia pseudoacacia and Cotula anthemoids | Internal | Boils | 51 | 0.8 | 0.98 |
| Branch | Chewing | Internal | Hernia | |||||||
| Antypiretic | ||||||||||
| Joints Inflammation | ||||||||||
| Stomachache | ||||||||||
| 110 | Salix denticulata Andersson (HF-79) | Terik, Jangali Bed, Tree | Salicaceae | Stem and root bark | Boiled | Internal | Headache | 34 | 0.53 | 0.39 |
| Antypiretic | ||||||||||
| Paralysis | ||||||||||
| Leaves, branches | Paste | External | Itching | |||||||
| Eczema | ||||||||||
| 111 | Salvia hians Royle (HF-107) | Herb | Lamiaceae | Leaves | Juice | Internal | Cough | 31 | 0.48 | 0.66 |
| Fever | ||||||||||
| Anxiety | ||||||||||
| 112 | Salvia lanata Roxb. (HF-51) | Herb | Lamiaceae | Leaves | Poultice | External | Eczema | 27 | 0.42 | 0.48 |
| Wound | ||||||||||
| 113 | Salvia moorcroftiana Wall. Ex Benth (HF-59) | Kaljari, Herb | Lamiaceae | aerial parts | Juice | Internal | Diarrhea | 51 | 0.8 | 0.89 |
| Gas trouble | ||||||||||
| Cough | ||||||||||
| Stomachache | ||||||||||
| 114 | Sambucus wightiana Wall. ex Wight & Arn. (HF-52) | Gandala, Herb | Caprifoliaceae | Fruit | Taken as raw form | Internal | Stomachache | 19 | 0.3 | 0.5 |
| Anthelmintic | ||||||||||
| 115 | Sapindus mukorossi Gaertn. (HF-79) | Ritha, Soap nut, Tree | Sapindaceae | Seeds | Powdered | External | Anthalmantic | 47 | 0.73 | 0.77 |
| Fruits | Rubbing | External | Boils | |||||||
| 116 | Sarcococca saligna D. Don Muell (HF-66) | Bansathra, Shrub | Buxaceae | Leaves and shoots | Decoction | Internal | Joints pain | 23 | 0.36 | 0.23 |
| Blood purifier | ||||||||||
| Purgative | ||||||||||
| Leaves | Powder | External | Burns | |||||||
| Root | Juice | Internal | Gonorrhea. | |||||||
| 117 | Saussurea candolleana Wall. Ex. D.C Clarke (HF-84) | Herb | Asteraceae | Roots | Extract | Internal | Tonic | 23 | 0.36 | 0.28 |
| 118 | Skimmia laureola DC. Sieb (HF-08) | Nazar Panra, Tree | Rutaceae | Leaves | Powdered | External | Smallpox, anthalmatic, colic. | 48 | 0.75 | 0.59 |
| 119 | Smilax glaucophylla Klotroch (HF-115) | Epiphyte | Smilicaceae | Aerial parts | Infusion | Internal | Carminative | 32 | 0.5 | 0.55 |
| Dog bite | ||||||||||
| Spasm | ||||||||||
| Antypiretic | ||||||||||
| 120 | Sophora mollis (Royle) Baker (HF-56) | Buna, Sakina, Shrub | Paplionaceae | Flowers | Powder | External | Pimples | 21 | 0.33 | 0.36 |
| Wound | ||||||||||
| Inflammation | ||||||||||
| Sun burns | ||||||||||
| 121 | Swertia ciliate G.Don B. L. Burtt (HF-75) | Herb | Gentianaceae | Aerial part | Decoction | Internal | Cough | 48 | 0.75 | 0.88 |
| Cold | ||||||||||
| Antypiretic | ||||||||||
| 122 | Taraxacum officinale F.H. Wigg (HF-102) | Handh, Herb | Asteraceae | Roots | Decoction | Internal | Jaundice | 56 | 0.88 | 0.92 |
| Leaves | Cooked | Internal | Swellings | |||||||
| Diuretic | ||||||||||
| Tonic | ||||||||||
| 123 | Themeda ananthra Nees ex Steud.Anderss. (HF-39) | Grass | Poaceae | Aerial parts | Poultice | External | Backche | 41 | 0.64 | 0.5 |
| Leaves | Decoction | Internal | Blood purifier | |||||||
| 124 | Thymus liniaris Benth. Subsp. Liniaris Jalas (HF-105) | Herb | Lamiaceae | leaves and flowers | Powder | Internal | Strengthen teeth and gum | 32 | 0.5 | 0.64 |
| Bleeding | ||||||||||
| Flower | Grounded seeds of Carum carvi with flowers | Internal | Digestion | |||||||
| 125 | Trichodesma incanum (Bunge) A. DC. (HF-145) | Handusi booti Herb | Borangniceae | Leaves | Boiling | Internal | Flu | 31 | 0.48 | 0.48 |
| Cough | ||||||||||
| 126 | Trichodesma indicum (L.) R. Br.(HF-178) | Handusi, Herb | Boraginaceae | Whole plant | Cooked | Internal | Backache | 41 | 0.64 | 0.5 |
| Internal | Weakness | |||||||||
| External | Kidney stone | |||||||||
| 127 | Valeraina jatamansi Joes (HF-77) | Herb | Valerianaceae | Aerial parts | Oil | Internal | Constipation | 19 | 0.3 | 0.41 |
| 128 | Verbascum thapsus L. (HF-107) | Gider tabacoo Herb | Valerianaceae | Roots | Decoction | Internal | Toothache | 17 | 0.27 | 0.25 |
| Convulsions | ||||||||||
| Bleeding gum | ||||||||||
| 129 | Vibernum nervosum D.Don (HF-78) | Taliana, Shrub | Caprifoliaceae | Fruit | Taken as raw form | Internal | Stomachache | 15 | 0.23 | 0.3 |
| Anemia | ||||||||||
| 130 | Viburnum cotinifolium D. Don (HF-95) | Taliana, Shrub | Caprifoliaceae | Fruit | Taken as raw form | Internal | Purgative | 31 | 0.48 | 0.33 |
| Blood Purifier | ||||||||||
| Leaves | Extract | Internal | Menorrhagia | |||||||
| 131 | Viburnum grandiflorum Wall.ex.DC (HF-47) | Guch, Shrub | Caprifoliaceae | Seed | Juice | Internal | Typhoid | 25 | 0.39 | 0.2 |
| Whooping cough | ||||||||||
| 132 | Vincetoxicum hirundinaria Medicres (HF-109) | Herb | Asclepidaceae | Aerial parts | Decoction | Internal | Boils | 48 | 0.75 | 0.8 |
| Pimples | ||||||||||
| 133 | Viola canescens Wall.ex Roxb. (HF-108) | Banafsha. Herb | Violaceae | Leaves | Juice | Internal | Cough | 51 | 0.8 | 0.84 |
| Jaundice | ||||||||||
| Antypiretic | ||||||||||
| Fever | ||||||||||
| 134 | Viola pilosa Blume (HF-11) | Banafsha. Herb | Violaceae | Leaves | Decoction | Internal | Pain | 47 | 0.73 | 0.81 |
| Antypiretic | ||||||||||
| Stomach ulcer | ||||||||||
| 135 | Zanthoxylum armatum DC. Prodr (HF-88) | Timbar, Shrub | Rutaceae | Fruit, branches | Juice | Internal | Carminative | 60 | 0.94 | 1.13 |
| Cholera | ||||||||||
| Stomachache | ||||||||||
| Gum, toothache | ||||||||||
| Indigestion | ||||||||||
| Haemorroids | ||||||||||
| Stomachache | ||||||||||
| Seed | Powder | Internal | Stomachache | |||||||
| Toothache | ||||||||||
| Gums problems | ||||||||||
| Chewed | Internal | Antipyretic | ||||||||
| Stomachic | ||||||||||
| Diuretic | ||||||||||
| 136 | Ziziphus nummularia (Burm. f.) Wight & Arn. (HF-88) | Ber, Tree | Rhamnaceae | Fruit | Decoction | External | Dandruff | 51 | 0.8 | 0.98 |
| Bark | Mixed with Milk and honey | Internal | Diarrhea and dysentery |
Key words: FC = Frequency of citation; RFC = Relative Frequency of Citation; UV = Use Value
Interviews were carried out complying with the ethics guidelines commonly followed in ethnobotanical studies, and the informants’ written consent was obtained prior to the interviews. In order to ensure that the information was as unbiased as possible, we tried to avoid the presence of other people during the interviews. Participant observation was also used in order to better interpret and analyze the data reported by informants. The information collected concerned both diseases (the most frequent ones, ways of classifying and diagnosing them, etc.) and medicinal plants (local names, indications of use, plant parts used, places/methods/rituals of gathering, utilization and administration).
Voucher specimens were gathered using the informants’ indications, prepared according to standard taxonomic methods, and conserved in our lab for future reference. For plant identification, we consulted the Flora of Pakistan (www.eflora.com). Botanical nomenclature is presented in accordance with the International Plant Name Index (IPNI) (www.ipni.org).
Research hypothesis
The hypothesis for the present study was, older people know more uses of plants than younger, formal education is not predictive of knowledge level about plants, and men tend to know more plant species/users than women. Species of plants are of unequal usage/importance to people. Across the range of species, its importance will vary, even among communities with the same cultural origin. In addition, it was also hypothesized that closely related plants are exploited in the treatment of almost similar diseases in cultures that are not much related thus are more likely to be independent discoveries of similar plant compounds and disease mechanisms.
Quantitative ethnobotanical data analysis
To determine whether a statistically significant correlation exists between the numbers of plants mentioned and the informant’s age, we used the Spearmann test. The Mann-Whiney U and Kruskal-Wallis tests were used to find significant differences between two and among 5 groups related groups, respectively, all set at 0.5 alpha level of significance.
Some quantitative indices commonly adopted in ethnobotanical studies were used to analyze the data collected through the interviews [29]. Relative frequency of citations (RFC) and use value (UV) was used to access relative importance of plant species cited by informants.
Frequency of citations was estimated as
Where FC is the number of informants reporting the use of a particular species and N is the total number of informants.
Use value [30] was estimated as
Where Ui is the number of uses mentioned by each informant for a given species and N is the total number of informants.
Informant consensus factor (ICF)
Informant consensus factor was used to identify the most trusted healing plants for those disease categories that were claimed to be most common in the area following the approach of [31] by using the following formula:
Where Nur is the number of use-reports in each disease category and Nt is number of species used.
Jaccard index (JI)
JI was calculated in order to compare data reported in our study with previously published data collected from neighboring regions by using the following formula
Where
a = number of species found only in area A
b = number of species found only in area B
c = number of species common to both areas
Results and discussion
Diversity of medicinal plants in the studied area
A total of 136 medicinal plant species belonging to 98 genera and 45 families were reported “Table 1”. They represent about 19–23% of the pool of medicinal plants that constitute the pharmaceutical ethnoflora in alpine areas of Pakistan [32]. The most represented botanical family was Asteraceae (14 species, 10%), followed by Lamiaceae (11 species, 8.1%), Fabaceae and Rosaceae (5 species each, 3.7%), and Ranuncolaceae (4 species, 2.9%). The other 41 families contributed with less than 4 species; among these 41 families, 26 (58% of all cited families) were represented with only 1 species. These results were in accordance with other ethnobotanical studies carried out in Pakistan [33–35] and were not surprising. In fact, Asteraceae, Lamiaceae, Fabaceae, Rosaceae are large, mostly cosmopolitan families that are known worldwide to be medicinal; for example, Asteraceae and Lamiaceae are rich in essential oils and are widely used in popular medicine around the world [36–38]. Rosaceae is rich in phenols, a group of substances that play an important role as anti-oxidants in the human diet [38]. Ranuncolaceae is rich in active secondary metabolites and have a high number of pharmacological properties [39, 40]. On the other hand, all of these botanical families contain some plants commonly found in the Pakistan flora. In terms of the life form, most of the used species were herbaceous (55%) followed by trees (26%), shrubs (17%), and climbers (2%). As is generally found in alpine areas (see for example [24]), the use of herbaceous species is more frequent than the use of perennial woody species. This finding can be related to the composition and the structure of the vegetation of high altitude areas, where tree growth is made difficult by climatic conditions; on the other hand, herbal preparation methods and extraction of active metabolites are easier to carry out with herbaceous plants than woody materials [41].
Herbal drug preparation and utilization
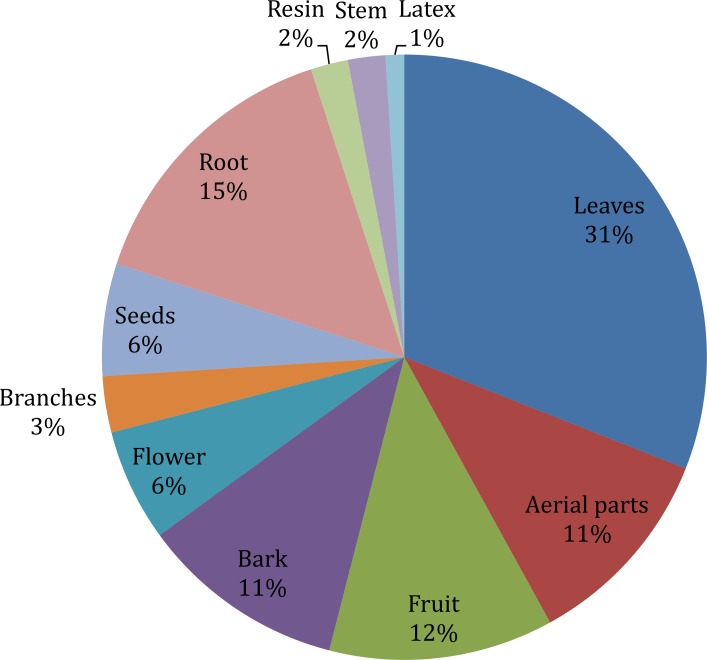
Different plant parts are used differently in herbal medicines depending upon the cultural knowledge and availability of those parts to local inhabitants. Similarly to what reported in other studies [42, 43], leaves (31%) were the most common plant part used in herbal preparations followed by roots (15%) and fruits (12%) “Fig 2”. Leaves are the plant part directly involved in photosynthesis, producing several active compounds like sugars but also storing important secondary metabolites like terpenes, alkaloids, cyanogenic glycosides; these chemical substances are involved in complex plant-to-plant and plant-to-animal relations including defense against a variety of pests and predators and allelopathy and most of these substances are of medicinal value. Roots were the favored plant part in many other cases, possibly because hypogeous organs normally have a high content of secondary metabolites [44]. As reported in previous studies conducted in other areas of Pakistan [45, 46], the utilization of fruits is found to play an important role in the local pharmacopoeia; this can be related to the importance that some wild edible fruits assume as nutraceuticals and in preventing nutritional deficiencies. In 67 cases, different parts of the same plant were used to treat different diseases, for example, roots of Berberis lyceum were used internally for the treatment of chronic diarrhea, piles, diabetes, pustules and scabies while externally these were used to heal fractured bone and swellings.
Fig 2. Plants parts use in herbal recipes.
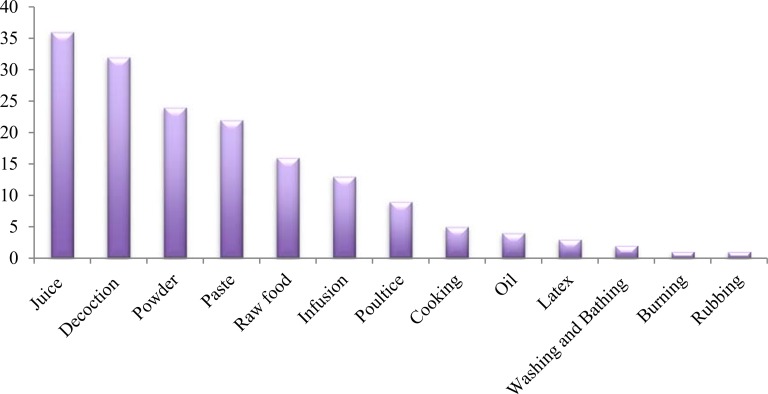
The main method of preparation was decoctions (26 species) followed by juice and powder (24 species each), paste (22), chewing (eating in raw form as salad or fruits) (16 species), extract (11 species), infusion (10 species) and poultice (8 species) “Fig 3”. These results were in agreement with those reported in other studies [47–51]. Quantity and dosage of medicinal drugs were found to differ with age, state of health of the patient and severity of the treated disease for example decoction of Elaeagnus umbellata for heart diseases if someone is suffering from chronic cardiac problem then he must use this decoction for long time as compare to the patient who was suffering acute cardiac problems. Ficus carica is very effective in constipation, for child two to three fruits were effective but for adult four to five fruits were effective for the relief of constipation. The high usage of freshly prepared juice in ethnomedicines was an indication of the high abundance of medicinal plants in the study areas that can be freshly available and harvested anytime for use. The other reasons for the repeated use of fresh plant juice could be the facts that the drying process contributes to the loss of volatile oil and that proteins become denatured at a high temperature. The measurements used to determine the dosages are not standardized and depend on the age and physical appearance of the patient, sociocultural explanation of the illness, diagnosis, and experience of the individual herbalist. Usually, the treatment of the patient is completed within a single day or a couple of days. When patients did not show any indication of improvement from their sickness following the completion of treatment, the physician referred them to a modern health center in an urban area for further examination [46, 52, 53].
Fig 3. Method of preparation of herbal recipes.
Most of the cited plant drugs were administrated (82) as they are, but in some herbal preparations (50) they were mixed with other ingredients like milk, water, honey, oil or butter to treat specific diseases. Few species (4) were used in combination with other herbs, for example, leaves of Salix acmophylla boiled with Robinia pseudoacacia (leaves) and Cotula anthemoids (leaves) to treat fever and hernia. As hypothesized in other studies it is possible that interactions among different species involve strengthening of therapeutic effects as well as attenuation of toxicity or of adverse effects of some plants composing the mixture. Most of the herbal preparations were taken internally (68%) while few were also used externally (32%).
Most plants (84; 61.8%) were used in only one (42) or two (42) categories. Berberis lyceum and Prunella vulgaris were the most versatile species because their use was cited in 8 different medicinal categories followed by Albizia lebbeck (7 categories), Desmodium polycarpum, Jasminum mesnyi and Pinus roxburghii (6 categories). Medicinal plants were mainly used to treat digestive disorders (63 species), followed by skin problems (59 species) and respiratory problem.
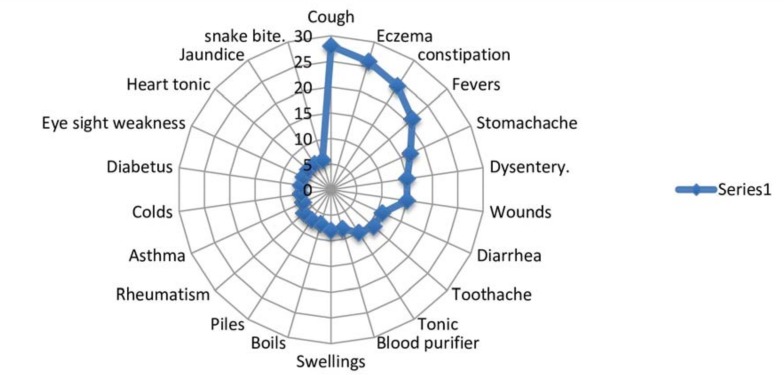
Among the subcategories mentioned (corresponding to detailed medicinal uses), cough was treated with the highest number of different plants (28 species), followed by eczema (26), constipation (24), and fever (21). Thirty-nine subcategories (36%) were treated with only one species: for example, typhoid was treated with juice extracted from the seeds of Viburnum grandiflorum, psoriasis with a paste of leaves of Clematis buchananiana, gonorrhea with juice extracted from the roots of Sarcococca saligna, and athlete’s foot with a paste of leaves of Ipomoea carnea. According to Albuquerque [54], the presence of a large number of species for the same medicinal use would result in maintenance of that use, i.e., it's resilience in the local ethnomedical system. On the other hand, categories associated with only one species could be considered more vulnerable to perturbations. As observed by Numa [55] any change leading to the disappearance of that single species could induce a change in local medical practices, such as searching for alternatives for treating that specific illness.
According to other studies conducted in neighboring areas [56–58] and in our research most species (28) were used to treat a cough and related respiratory problems. Climatic factors, such as rarefied air due to the reduction in oxygen found at high altitudes and low-temperature regime experienced throughout the year, combined with high demographic density and poor housing conditions, could explain the high prevalence of contagious diseases. Moreover, the lack of awareness about personal hygiene and cleanliness practices is probably responsible for the high number of plants (26) reported to treating skin problems “Fig 4”.
Fig 4. Different disease treated by the plants in the study area.
Quantitative indices
The relative frequency of citation (RFC) shows the local importance of each species with reference to informants who cited these medicinal plant species. We found that the species with the highest RCF values in the study area were Zanthoxylum armatum (0.94), Berberis lyceum (0.92), Ajuga bracteosa (0.91), Prunella vulgaris (0.91), Pinus roxburghii (0.91), Adiantum capillus-veneris (0.89), Rosa brunonii (0.89), Albizia lebbeck (0.89), Cedrella serrata (0.84), Punica granatum (0.81) and Jasminum mesnyi (0.80) “Table 1”. Use value (UV) is an index commonly adopted to measure the relative importance of a given species known within a local community. It is high when many uses are reported (i.e., when a species is frequently quoted by informants in the treatment of various diseases) and approaches zero when few uses are mentioned. In this study, the highest use values were reported for Berberis lyceum and Ajuga bracteosa (1.13 each), Abies pindrow (1.03), Prunella vulgaris and Adiantum capillus-veneris (1.00 each), and Desmodium polycarpum and Pinus roxburghii (0.98 each) “Table 1”. Because these plants were native and recorded as very common in the area, they combine the cultural value pointed out by our study with a high ecological and landscape importance. These findings were also in accordance with the “appearance hypothesis” [59]: the more common a plant is in an area, the greater the folk knowledge about its use; that is, more common plants would allow local people to have more experience of their properties and consequently would have a greater probability of being introduced into the local culture. UV is dynamic and changes between different areas and even within the same area over time. For example, P. roxburghii was found to be one of the least cited medicinal plants (UV = 0.01) in the Sudanhoti district (AJK), although the use of this plant for timber, fuel, and construction was well known in the area [59]. On the other hand, Achyranthes aspera and Momordica charantia had among the highest UVs in the study by [60], while showing low UVs (0.38) in our study. According to some authors [29, 61, 62], medicinal plant species with high RFCs and UVs should be tested to assess and prove their pharmacological activity. On the other hand, plants with low UVs are not necessarily unimportant, but their low values indicate that locals are not aware of their uses, and this could put knowledge about their use at the risk of not being transmitted [19].
Informant consensus factor
The informant consensus factor (ICF) calculated for each category ranged from 0.69 to 0.90 with a mean value of 0.87. The highest values were recorded for digestive system diseases (ICF = 0.90), muscular and skeletal system diseases (ICF = 0.89), and mouth/pharynx diseases and diabetes (ICF = 0.86 each). The lowest ICF value was found for the hair care category (0.69) “Table 2”. ICF values are influenced by the number of informants and are more significant when calculated for uses cited by many informants. In general, ICF values were high in our study, revealing that the informants tend to agree on which plants to use in the treatment of common illnesses. According to Heinrich [63], high ICF can help in identifying potentially effective medicinal plants. It must be highlighted that in our study the highest agreement level was recorded for diseases reported as the most widespread in rural communities of the Poonch district and other areas of Pakistan [64]. The prevalence of gastrointestinal disorders in the study area may be attributed to the low availability of hygienic food and drinking water. According to the District Census Report carried out in 1998, the population with access to safe drinking water inside the house was 16.28%; in 2005 the water access, although improved (21%), was still strongly lacking. This situation was compounded by the devastating earthquake, in which several water-supply schemes were damaged and the drinking water supply was obtained from contaminated surface water sources [65].
Table 2. Informant consensus factor (ICF) of Pearl Valley Tehsil Rawalakot, District Poonch AJ&K.
| S. NO. | Diseases | Detailed categories | Ntax | Nur | ICF | Most Used Plants |
|---|---|---|---|---|---|---|
| 1 | Colds, respiratory tract diseases | Asthma, breathing difficulties, bronchitis, chest pain, cough, expectorant, Flu, lungs diseases | 41 | 236 | 0.83 | Mentha royleana, Polygonatum multiflorum, Punica granatum, Pyrus pashia, Salvia moorcroftiana, Prunella vulgaris |
| 2 | Digestive system disorders | Anthelmintic, Cholera, constipation, diarrhea, dysentery, dyspepsia, flatulence, gastritis, jaundice, liver and bile diseases, nausea, stomachache, typhoid, vomiting | 114 | 1162 | 0.90 | Mentha royleana, Zanthoxylum armatum, Berberis lyceum, Eriobotrya japonica, Punica granatum, Ziziphus numelaria, Artemisia absinthium |
| 3 | Urinary and sexual-reproductive system diseases | Abortion, amenorrhea, aphrodisiac, contraceptive, diuretic, gonorrhea, irregular menstruation, kidney diseases, kidney stones, leucorrhoea, menorrhagia, miscarriage, urinary tract diseases | 16 | 91 | 0.83 | Aesculus indica, Prunus domestica, Bergenia ciliata, Galium asperifolium, Oenothera rosea, Eriobotrya japonica, |
| 4 | Muscular and skeletal system diseases | Antispasmodic, bone fracture, backache, body and joint inflammations, cramps, muscular pains, joint pains, paralysis, rheumatism | 11 | 100 | 0.89 | Hypericum perforatum, Juglans regia, Pyrus malus, Pyrus malus |
| 5 | Nervous system diseases | Convulsions, depression, general pain, headache, nervous problems, sedative, toothache | 16 | 86 | 0.82 | Juglans regia, Pyrus malus, Heracleum candicans |
| 6 | Circulatory system diseases | Bleeding, hemorrhoids, hearth diseases, hearth tonic, hypertension, pressure | 6 | 25 | 0.79 | Rosa brunonii,Oenothera rosea,Viola canscens, Adiantum capillus-veneris, Desmostachya bipinnata,Pyrus malus |
| 7 | Blood and lymphatic system | Anemia, blood purification | 15 | 76 | 0.81 | Dalbergia sissoo, Rosa brunonii, Berberis lyceum,Vibernum nervosum, |
| 8 | Skin diseases, burns and wounds | Athlete foot, boils, burns, carbuncles, cracked heels, cuts and wounds, dandruff, eczema, eruption, freckles, itching and allergy, leprosy, leukoderma, measles, not specified skin problems, pimples, scabies, skin parasites, smallpox, sun burns, swellings, ulcers, urticaria, warts | 47 | 306 | 0.85 | Fumaria indica, Adiantum incisum, Euphorbia wallichii, Gallium asperifolium, Rosa brunonii |
| 9 | Fever | Fever | 32 | 138 | 0.77 | Smilax glaucophylla, Abies pindrow, Castanea sativa, Cichorium intybus, Elaeagnus angustifoli, Quercus incana |
| 10 | Mouth-pharynix diseases | Gum infection, mouth infection and inflammation, pyorrhea, sore throats, strengthening of spongy gums, teeth cleaning | 42 | 306 | 0.86 | Berberis aristata, Juglans regia, Thymus liniaris, Castanea sativa,Pistacia chinensis ssp. Integerrima, Zanthoxylum armatum, Ajuga bracteosa |
| 11 | Antidote | Dog bite, scorpion sting, snake bite | 8 | 31 | 0.77 | Nerium oleander, Dioscorea deltoidea, Hypericum perforatum |
| 12 | Ear and eye diseases | Earache, eyes diseases, eye sight weakness | 38 | 186 | 0.80 | Rosa brunonii, Androsace rotundifolia,Bergenia ciliata |
| 13 | Hair care | Hair washing, hair conditioner | 9 | 27 | 0.69 | Juglans regia, Poa nepalensis |
| 14 | General weakness in men and animals | Weakness, loss of appetite, tonic | 45 | 258 | 0.83 | Fumaria indica, Asparagus filicinus,Castanea sativa, Viola canscens, Trichodesma indicum, Punica granatum, Berberis lyceum, Ligustrum lucidum |
| 15 | Diabetes | 6 | 36 | 0.86 | Berberis lyceum, Clematis montana, Rubus fruticosus, | |
| 14 | Others | Demulcent, body temperature, cooling agent, immunity, tumor | 15 | 58 | 0.75 | Pinus roxburgii, Ligustrum lucidum, Cedrela serrata, Viola canscens, Ficus palmate, Elaeagnus umbellata |
Key words:Ntax = Number of taxa; Nur = Number of use Reports; ICF = Informant consensus factor
Medicinal plant knowledge
Each informant mentioned on average 3.75 (± 2.96; minimum: 1; maximum: 15) species and 11.84 (± 10.52; minimum: 2; maximum: 39) different uses. Many studies have shown that age and gender are two important factors to consider when evaluating the distribution of knowledge within a group of informants [66, 67]. However, very few studies have analyzed the effect of these variables on the distribution of ethnomedicinal knowledge in Pakistan (see, for example, Ahmad et al. [48] and none of them used statistical analyses for validation of the collected data. 58% of the 64 informants reporting the use of medicinal plants were over 40 years old (37 informants); of these, 17 (26.5% of the informants) were aged between 41 and 50 while 20 (31.5%) were over 50 (Table 1). Spearman’s correlation analysis showed significant positive differences between the age and the number of both number of mentioned species (rs = 0.49; p < 0.05) and different uses (rs = 0.45; p < 0.05), indicating that there is a trend of older people being more knowledgeable that younger people “Table 3”. When we analyzed the age groups individually, significant differences were observed only among some groups “Table 3”. The youngest informants (from the ages of 19 to 30) knew fewer species (1.33 ± 0.55) and uses (3.00 ± 1.11) than other groups. The informants belonging to the 41–50 and 51–60 age groups cited a higher number of species and uses than the other groups “Table 3”. This trend is widely observed in literature; on the other hand, elderly people are expected to have accumulated more experiences about the uses of medicinal plants for a longer period of time than others. It might also be hypothesized that young people are not interested in learning the use of medicinal plants as a consequence of the socio-economic transition occurring in Pakistan. Comparing the knowledge held by men and women, men had much higher knowledge on medicinal plants (Z = 3.20; p < 0.01) and their uses (Z = 3.96; p< 0.001): they reported 4.66 (±3.31) species and 15.72 (±11.40) uses, while women 2.32 (±1.43) species and 5.08 (±4.72) uses. There is no consensus in the literature about the effect of gender, though women are generally shown to hold a wider competence concerning medicinal plants than men [66]. Ahmad et al. [48], studied medicinal resources in the mountainous region of Chail valley (Pakistan), observed that females had a higher knowledge about the preparation and administration of herbal drugs compared to males. Similar was observed by [67] in a study concerning the ethnobotanical knowledge of Fulni-ô in north-eastern Brasil, our finding could be explained considering the harvesting dynamics, in which men are the main collectors of medicinal plants growing in the local forest. As for education level, 21 informants (33% of all informants) were uneducated, 8 (12%) received only some primary education 20 (31%) had attended middle or intermediary school and 9 (14%) held a university degree. The education level of informants proved to be significantly associated with both the number of species (H = 10.09; p < 0.05) and the number of uses (H = 38.58; p < 0.001). Informants who were less educated (from primary to middle education level) had highest medicinal plant knowledge “Table 3”. It’s important to note that this result is affected by the relationship existing between the education grade and the work activities of the informants: traditional healers having higher level of medicinal knowledge (see below) belonged to the group with lower education level; on the contrary housewives, knowing the lowest number of species and uses, were all uneducated. Informants with higher education were the less knowledgeable: it’s possible to presume that a better scholastic career may expose people to the influence of the academic knowledge and to the allopathic medicinal practices. During the study, seventeen traditional healers having ages ranging from 45 to 60 years were interviewed. Most of the healers were involved in healing practices from more than two to five years and were vastly experienced while only five healers had more than 10 years of experience. When grouped according to profession, Kruskal-Wallis tests show that there is a significant difference among informants in both the number of known medicinal plants and the number of different uses (H: 38.51; p < 0.001). As we expected, both the mean number of species and the mean number of uses resulted higher for “professional” healers (traditional healers + midwives) vs laypeople “Table 3”. Yet, in Rawalakot even the knowledge held by laypeople appears more considerable: lay villagers also reported 42% of the species mentioned by healers. The role of laypeople in preserving and transmitting the ethnomedicinal knowledge has been pointed out by some studies (see for example Bruschi et al. [68]), in particular, laypeople were reported to know and use medicinal plants mainly to treat common ailments such as digestive troubles, injuries and wounds, cough, headache. People turn instead to healers for other diseases considered more severe.
Table 3. Informants and knowledge about TAB. F = female; M = male.
| informants | # | # KNOWN SPECIES | # CITED DIFFERENT USES | |||
|---|---|---|---|---|---|---|
| F | M | F | M | F | M | |
| Total | 25 | 39 | 2.32±1.43 | 4.66±3.31 | 5.08±4.72 | 15.72±11.40 |
| Age class | ||||||
| 19–30 | 9 | 1.33±0.55 | 3.00±1.11 | |||
| 31–40 | 18 | 3.38±2.99 | 10.00±9.93 | |||
| 41–50 | 17 | 4.53±3.02 | 17.65±3.02 | |||
| 51–60 | 20 | 4.50±3.03 | 12.55±8.28 | |||
| Education level | ||||||
| Uneducated | 21 | 2.29±1.27 | 6.43±4.43 | |||
| Primary school | 14 | 5.50±4.31 | 14.36±11.51 | |||
| Intermediary school | 8 | 3.00±1.52 | 10.50±9.28 | |||
| Middle school | 12 | 5.08±3.14 | 20.0±14.01 | |||
| University degree | 9 | 3.33±2.18 | 10.88±8.49 | |||
|
Profession Traditional healers and midwives |
20 | 7.15±2.96 | 25.03±8.00 | |||
| Housewives | 8 | 1.87±0.83 | 5.00±2.98 | |||
| Teachers | 13 | 2.38±0.87 | 6.15±3.16 | |||
| Farmers | 10 | 2.10±1.10 | 5.50±2.81 | |||
| Other | 13 | 2.30±1.37 | 5.92±4.42 | |||
Comparison with other studies in neighboring regions and Novelty
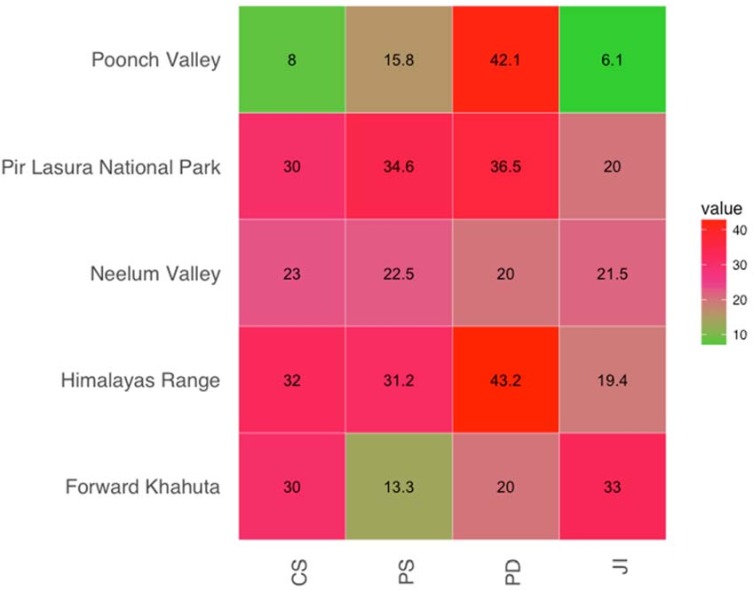
When we compared the data from this study with the findings of other studies carried out in neighboring areas, we observed a percentage of similarity in uses of plant species ranging from 13.33% [69] to 34.62% [70] with an average value of 22.53%. The percentage of dissimilarity ranged from 43.20 [71] to 20.00 [72] with an average value of 37.03 “Fig 5”. The maximum level of similarity was found with studies conducted by Ch et al. [69] and Kayani et al. [71], which showed JI values of 32.97 and 19.39, respectively, while the lowest index of similarity was found with the study conducted by Khan et al. [26]which had a JI of 6.11. As observed in other studies [71, 73–75], villagers inhabiting neighboring areas tend to use the same medicinal plants. Presumably, the plant communities occurring in closer areas have more similar plant uses than the communities of more distant areas. A high level of similarity might also be attributed to the fact that the communities living in nearby areas have the same sociocultural values and have more opportunities to exchange their traditional knowledge. The results of this survey provide new insights into the knowledge about medicinal plants of Pakistan: 60% of the plant uses recorded in this research have not been previously reported for AJ&K. Moreover, some of the uses reported by our informants were unknown in the worldwide’s literature “Table 4” Examples include the use of Opuntia dillenii for the treatment of joint pain, of Dalbergia sissoo for hair growth, and of Pistacia chinensis ssp. integerrima for wound healing. Species listed in “Table 4” could be appropriate candidates for further studies addressed to the development of new drugs. The number of first time reported plants in the present study indicated a high degree of ethnobotanical novelty for the studied area and confirmed the importance of ethnomedicinal research, also when dealing with already known medicinal plants.
Fig 5. Heat map showing percentage similarity, dissimilarity and Jaccrad Index (JI) of Pearl Valley with neighbouring areas.
Table 4. Novel uses of plant in Pearl Valley Tehsil Rawalakot, District Poonch AJ&K.
| Plants Names | Novel Uses |
|---|---|
| Opuntia dillenii Haw. | Paste of whole plant used for treating joint pain |
| Dalbergia sissoo Roxb. | Leaves extract used for hair growth |
| Pistacia chinensis ssp. integerrima (J. L. Stewart) Rech. | Bark paste used as cicatrizant |
| Pinus roxburgii Roxb. | Resin use to stop bleeding |
| Adiantum capillus-veneris L. | Leave decoction used against measles |
| Aesculus indica (Wall.ex Camb.) Hook.f. | Seed powder use against leucorrhoea |
| Alysicarpus bupleurifolius L. D.C | Leaves fresh juice use as blood purifier |
| Anaphalis adnata D.C | Leaves powder used as cicatrizant |
| Bergenia ciliate (Haw.) Sternb. | Root juice and leaves to remove kidney stone |
| Caltha alba var. alba Camb. var. alba | Aerial parts juice used as sedative |
| Poa nepalensis Walls ex. Duthie. | Leaves decoction used against body and head lices |
The annual temperature in Pearl Valley was 38°C during summer and– 3°C during the winter and rainfall ranged from 500 to 2000 mm. Due to huge variation in climatic conditions the region is biodiversity hotspot and contains representative of almost all life forms. The study areas selected for comparision with present study had low temperature during in winter and moderate temperature during summer. Geographic distance, climatic conditions and cultural values of Pir Lasura National Park are similar to study area so there are more chances of exchange of knowledge between these areas. The argument was supported by highest value of similarity index 34.62% between two areas. Similarly, the areas that are far apart from study area had least similarity in uses, thus plant the present in these areas with similar uses and methods of preprations to those of plants in study area, should be considered to have higher potential than other plants that may be used for a particular disease in only one culture.
Conservation status of the plants
Projects aimed to safeguard and enhance ethnobotanical knowledge about medicinal plants must be associated with to specific strategies for the conservation and sustainable use of plants in order to ensure the convergence of development and conservation goals [76]. Extractive activity can play an important role in local health care systems, but a high collection rate of medicinal plants can lead to over-exploitation and can have a strong impact on local plant diversity. According to the IUCN Red List (version 3.1), Pinus roxburghii and Zanthoxylum armatum were reported as vulnerable (VU), while Punica granatum was indicated as endangered (EN); people living in the area use different parts of these plants not only as medicine but also for more destructive uses such as fuelwood, construction, and furniture. Several other plants shown in Table 2 are reported to be of least concern (LC). The most important factors considered by local informants as threats to the survival of the flora were deforestation, agricultural expansion, overgrazing, fire, and drought. The continuous environmental degradation of the collection habitats could hasten the depletion of medicinal plants and the rarefaction of the associated knowledge. In recent years, some traditional practitioners have started to cultivate medicinal plants in their home gardens, but this effort seems to be insufficient given that only 18% of the medicinal plants reported in this study were cultivated.
Conclusions
This study was the first to document the uses of medicinal plants in the District Rawalakot area. Our data show that medicinal plants are an important source for local people (136 species reported by 64 informants) and point out that both traditional healers and laypeople have developed a rich knowledge base on their experience. In more remote areas, where health services have struggled to reach, this knowledge can provide first aid for treating the most common diseases occurring in the area. The plants having high values of UV and RFC are biologically active and had good healing potential for specific ailments. A study area was located at higher altitude so respiratory problems were most common diseases in the area, similarly due to low temperature during most of the days of year skin problem were ranked second among different cited diseases. A significant effect of gender and age on the distribution of ethnobotanical knowledge was recorded during an interview and was confirmed statistically. Spearman’s correlation analysis depected that there is positive differences between the age and the number of both number of mentioned species (rs = 0.49; p < 0.05) and different uses (rs = 0.45; p < 0.05), indicating that there is a trend of older people being more knowledgeable than younger people. When we compare the knowledge held by men and women, men showed a much higher knowledge on medicinal plants (Z = 3.20; p < 0.01) than women. The distance between areas was the main determinant of change in jaccard index value. Areas located closer to each other have more opportunities for exchange of traditional knowledge and similarities among neighboring areas also depend upon environmental factors. The highest similarity between the study area and Pir Lasura National Park may be due to the sharing of a similar flora and the cross-cultural exchange of medicinal plant knowledge in past and present. Less similarity between the areas may be because they are so distantly related that they are very unlikely to have communicated medicinal plant uses to each other, they are disconnected through mountain ranges and other cultural variations. Any related plants used by these areas to treat related diseases are independent discoveries. We believe that results of the present study may represent useful information that could contribute to preserving the local indigenous knowledge about the use of medicinal plants and also attract the future generations toward the traditional healing practices. Moreover, this study provides baseline information for further studies aimed at the identification and isolation of bioactive molecules that can serve as starting materials in the discovery of new plant based drugs and also create awareness about the conservation and protection of biocultural diversity.
Supporting information
(DOCX)
(DOCX)
Acknowledgments
The authors are grateful to the local informants of the study area for their contribution and sharing their precious indigenous knowledge. I would also like to thank Dr. Piero Bruschi for his precious time for the proofreading and English language correction.
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
The authors received no specific funding for this work.
References
- 1.Nikbakht A, Kafi M, Haghighi M, editors. The abilities and potentials of medicinal plants production and herbal medicine in Iran. VIII International People-Plant Symposium on Exploring Therapeutic Powers of Flowers, Greenery and Nature 790; 2004.
- 2.Saad B, Azaizeh H, Said O. Tradition and perspectives of Arab herbal medicine: a review. Evidence-Based Complementary and Alternative Medicine. 2005;2(4):475–9. doi: 10.1093/ecam/neh133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Azaizeh H, Saad B, Cooper E, Said O. Traditional Arabic and Islamic medicine, a re-emerging health aid. Evidence-Based Complementary and Alternative Medicine. 2010;7(4):419–24. doi: 10.1093/ecam/nen039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Phillips O, Gentry AH. The useful plants of Tambopata, Peru: I. Statistical hypotheses tests with a new quantitative technique. Economic Botany. 1993;47(1):15–32. [Google Scholar]
- 5.Phillips O, Gentry AH. The useful plants of Tambopata, Peru: II. Additional hypothesis testing in quantitative ethnobotany. Economic Botany. 1993;47(1):33–43. [Google Scholar]
- 6.Hanazaki N, Tamashiro JY, Leitão-Filho HF, Begossi A. Diversity of plant uses in two Caiçara communities from the Atlantic Forest coast, Brazil. Biodiversity and Conservation. 2000;9(5):597–615. [Google Scholar]
- 7.Ayantunde AA, Briejer M, Hiernaux P, Udo HM, Tabo R. Botanical knowledge and its differentiation by age, gender and ethnicity in Southwestern Niger. Human Ecology. 2008;36(6):881–9. [Google Scholar]
- 8.Silva FdS Ramos MA, Hanazaki N Albuquerque UPd. Dynamics of traditional knowledge of medicinal plants in a rural community in the Brazilian semi-arid region. Revista Brasileira de Farmacognosia. 2011;21(3):382–91. [Google Scholar]
- 9.Rangel CDFCB, Ramos MA, de Amorim ELC, de Albuquerque UP. A comparison of knowledge about medicinal plants for three rural communities in the semi-arid region of northeast of Brazil. Journal of ethnopharmacology. 2010;127(3):674–84. doi: 10.1016/j.jep.2009.12.005 [DOI] [PubMed] [Google Scholar]
- 10.van Andel T, Carvalheiro LG. Why urban citizens in developing countries use traditional medicines: the case of Suriname. Evidence-Based Complementary and Alternative Medicine. 2013;2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kleinman A. Concepts and a model for the comparison of medical systems as cultural systems. Social Science & Medicine Part B: Medical Anthropology. 1978;12:85–93. [DOI] [PubMed] [Google Scholar]
- 12.Hobsbawm E, Ranger T. The invention of tradition: Cambridge University Press; 2012. [Google Scholar]
- 13.Quave CL, Pieroni A. A reservoir of ethnobotanical knowledge informs resilient food security and health strategies in the Balkans. Nature Plants. 2015;1:14021 doi: 10.1038/nplants.2014.21 [DOI] [PubMed] [Google Scholar]
- 14.Case RJ, Pauli GF, Soejarto DD. Factors in maintaining indigenous knowledge among ethnic communities of Manus Island. Economic Botany. 2005;59(4):356–65. [Google Scholar]
- 15.Saynes-Vásquez A, Caballero J, Meave JA, Chiang F. Cultural change and loss of ethnoecological knowledge among the Isthmus Zapotecs of Mexico. Journal of ethnobiology and ethnomedicine. 2013;9(1):40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Byg A, Balslev H. Factors affecting local knowledge of palms in Nangaritza Valley in South-Eastern Ecuador. Journal of Ethnobiology. 2004;24(2):255–78. [Google Scholar]
- 17.Kristensen M, Balslev H. Perceptions, use and availability of woody plants among the Gourounsi in Burkina Faso. Biodiversity and Conservation. 2003;12(8):1715–39. [Google Scholar]
- 18.Voeks RA, Leony A. Forgetting the forest: assessing medicinal plant erosion in eastern Brazil. Economic Botany. 2004;58(sp1):S294–S306. [Google Scholar]
- 19.Camou-Guerrero A, Reyes-García V, Martínez-Ramos M, Casas A. Knowledge and use value of plant species in a Rarámuri community: a gender perspective for conservation. Human ecology. 2008;36(2):259–72. [Google Scholar]
- 20.Benz BF, Cevallos J, Santana F, Rosales J, Graf S. Losing knowledge about plant use in the Sierra de Manantlan biosphere reserve, Mexico. Economic Botany. 2000;54(2):183–91. [Google Scholar]
- 21.Martínez-Ballesté A, Martorell C, Caballero J. Cultural or ecological sustainability? The effect of cultural change on Sabal palm management among the lowland Maya of Mexico. Ecology and Society. 2006;11(2). [Google Scholar]
- 22.Zent S. Acculturation and ethnobotanical knowledge loss among the Piaroa of Venezuela: demonstration of a quantitative method for the empirical study of traditional ecological knowledge change. On Biocultural diversity: linking language, knowledge, and the environment Washington: Smithsonian Institution Press; 2001. [Google Scholar]
- 23.Oteros-Rozas E, Ontillera-Sánchez R, Sanosa P, Gómez-Baggethun E, Reyes-García V, González J. Traditional ecological knowledge among transhumant pastoralists in Mediterranean Spain. Ecology and Society. 2013;18(3). [Google Scholar]
- 24.Khan MA, Khan MA, Hussain M, Ghulam GM. An ethnobotanical inventory of Himalayan region Poonch valley Azad Kashmir (Pakistan). Ethnobotany Research and Applications. 2010;8:107–23. [Google Scholar]
- 25.Ishtiaq M, Maqbool M, Hussain T, Shah A. Role of indigenous knowledge in biodiversity conservation of an area: A case study on tree ethnobotany of Soona Valley, District Bhimber Azad Kashmir, Pakistan. Pakistan Journal of Botany. 2013;45:157–64. [Google Scholar]
- 26.Khan M, Khan MA, Mujtaba G, Hussain M. Ethnobotanical study about medicinal plants of Poonch valley Azad Kashmir. J animal plant Sci. 2012;22:493–500. [Google Scholar]
- 27.Hamayun M. Ethnobotanical profile of Utror and Gabral valleys, district Swat, Pakistan. Ethnobotanical Leaflets. 2005;2005(1):9. [Google Scholar]
- 28.Shaukat SA, Shah SZA, Ahmad MJ, Shaukat SK, Shoukat SW. Ethnobotanical study of some medicinal plants of union council Bangoin, Tehsil Rawalakot, AJ&K. Agricultural Advances. 2012;1(4):105–9. [Google Scholar]
- 29.Tardío J, Pardo-de-Santayana M. Cultural importance indices: a comparative analysis based on the useful wild plants of Southern Cantabria (Northern Spain) 1. Economic Botany. 2008;62(1):24–39. [Google Scholar]
- 30.Rossato SC, De LeitãO-Filho HF, Begossi A. Ethnobotany of caiçaras of the Atlantic Forest coast (Brazil). Economic botany. 1999;53(4):387–95. [Google Scholar]
- 31.Ferreira FS, Brito SV, Ribeiro SC, Saraiva AA, Almeida WO, Alves RR. Animal-based folk remedies sold in public markets in Crato and Juazeiro do Norte, Ceará, Brazil. BMC complementary and alternative medicine. 2009;9(1):1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Shinwari ZK. Medicinal plants research in Pakistan. J Med Plants Res. 2010;4(3):161–76. [Google Scholar]
- 33.Ullah R, Hussain Z, Iqbal Z, Hussain J, Khan FU, Khan N, et al. Traditional uses of medicinal plants in Darra Adam Khel NWFP Pakistan. J Med Plants Res. 2010;4(17):1815–21. [Google Scholar]
- 34.Inayatullah S, Irum R, Ateeq-ur-Rehman, Fayyaz Chaudhary M, Mirza B. Biological evaluation of some selected plant species of Pakistan. Pharmaceutical Biology. 2007;45(5):397–403. [Google Scholar]
- 35.Zia-Ul-Haq M, Ćavar S, Qayum M, Imran I, Feo Vd. Compositional studies: antioxidant and antidiabetic activities of Capparis decidua (Forsk.) Edgew. International journal of molecular sciences. 2011;12(12):8846–61. doi: 10.3390/ijms12128846 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Menezes F, Kaplan M. Plantas da subfamília Ocimoideae utilizadas na medicina popular: Etnofarmacologia vc Química. Rev Bras Farm. 1992;73:30–1. [Google Scholar]
- 37.Santos SdC, Mello Jd, Simões C. Taninos. SIMÕES, CMO; SCHENKEL, EP; GOSMANN, G; MELLO, JCP. 2004:615–56.
- 38.Miller NJ, Ruiz-Larrea MB. Flavonoids and other plant phenols in the diet: Their significance as antioxidants. Journal of nutritional & environmental medicine. 2002;12(1):39–51. [Google Scholar]
- 39.Milliken W, Albert B, Gomez GG, Rutherford J. Yanomami: A forest people: Royal Botanic Gardens, Kew; 1999. [Google Scholar]
- 40.Savoia D. Plant-derived antimicrobial compounds: alternatives to antibiotics. Future microbiology. 2012;7(8):979–90. doi: 10.2217/fmb.12.68 [DOI] [PubMed] [Google Scholar]
- 41.SABO I. PHYTOCHEMICAL AND ANTI BACTERIAL STUDIES ON THE STEM BARK OF LANNEA BARTERI.(OLIV.) ENGL.(ANACARDIACEAE 2015.
- 42.Šavikin K, Zdunić G, Menković N, Živković J, Ćujić N, Tereščenko M, et al. Ethnobotanical study on traditional use of medicinal plants in South-Western Serbia, Zlatibor district. Journal of ethnopharmacology. 2013;146(3):803–10. doi: 10.1016/j.jep.2013.02.006 [DOI] [PubMed] [Google Scholar]
- 43.Abbasi AM, Khan MA, Shah MH, Shah MM, Pervez A, Ahmad M. Ethnobotanical appraisal and cultural values of medicinally important wild edible vegetables of Lesser Himalayas-Pakistan. Ethnobiol Ethnomed. 2013;9:84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Noctor G, Foyer CH. Ascorbate and glutathione: keeping active oxygen under control. Annual review of plant biology. 1998;49(1):249–79. [DOI] [PubMed] [Google Scholar]
- 45.Awan MR, Iqbal Z, Shah SM, Jamal Z, Jan G, Afzal M, et al. Studies on traditional knowledge of economically important plants of Kaghan Valley, Mansehra District, Pakistan. J Med Plants Res. 2011;5:3958–67. [Google Scholar]
- 46.Arshad M, Ahmad M, Ahmed E, Saboor A, Abbas A, Sadiq S. An ethnobiological study in Kala Chitta hills of Pothwar region, Pakistan: multinomial logit specification. Journal of ethnobiology and ethnomedicine. 2014;10(1):1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Islam MK, Saha S, Mahmud I, Mohamad K, Awang K, Uddin SJ, et al. An ethnobotanical study of medicinal plants used by tribal and native people of Madhupur forest area, Bangladesh. Journal of ethnopharmacology. 2014;151(2):921–30. doi: 10.1016/j.jep.2013.11.056 [DOI] [PubMed] [Google Scholar]
- 48.Ahmad M, Sultana S, Fazl-i-Hadi S, ben Hadda T, Rashid S, Zafar M, et al. An Ethnobotanical study of Medicinal Plants in high mountainous region of Chail valley (District Swat-Pakistan). J Ethnobiol Ethnomed. 2014;10(36):4269–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Siew Y-Y, Zareisedehizadeh S, Seetoh W-G, Neo S-Y, Tan C-H, Koh H-L. Ethnobotanical survey of usage of fresh medicinal plants in Singapore. Journal of ethnopharmacology. 2014;155(3):1450–66. doi: 10.1016/j.jep.2014.07.024 [DOI] [PubMed] [Google Scholar]
- 50.El Amri J, El Badaoui K, Zair T, Bouharb H, Chakir S, Alaoui TEM. Ethnobotanical study of medicinal plants in the region El Hajeb (central Morocco). Journal of Research in Biology. 2015;4(8):1568–80. [Google Scholar]
- 51.Nondo RS, Zofou D, Moshi MJ, Erasto P, Wanji S, Ngemenya MN, et al. Ethnobotanical survey and in vitro antiplasmodial activity of medicinal plants used to treat malaria in Kagera and Lindi regions, Tanzania. Journal of Medicinal Plants Research. 2015;9(6):179–92. [Google Scholar]
- 52.Tahraoui A, El-Hilaly J, Israili Z, Lyoussi B. Ethnopharmacological survey of plants used in the traditional treatment of hypertension and diabetes in south-eastern Morocco (Errachidia province). Journal of ethnopharmacology. 2007;110(1):105–17. doi: 10.1016/j.jep.2006.09.011 [DOI] [PubMed] [Google Scholar]
- 53.Delfan B, Bahmani M, Eftekhari Z, Jelodari M, Saki K, Mohammadi T. Effective herbs on the wound and skin disorders: a ethnobotanical study in Lorestan province, west of Iran. Asian Pacific Journal of Tropical Disease. 2014;4:S938–S42. [Google Scholar]
- 54.Albuquerque UP, Lucena RF, Monteiro JM, Florentino AT, Almeida CdFC. Evaluating two quantitative ethnobotanical techniques. 2006. [Google Scholar]
- 55.Numa C, Verdú JR, Sánchez A, Galante E. Effect of landscape structure on the spatial distribution of Mediterranean dung beetle diversity. Diversity and Distributions. 2009;15(3):489–501. [Google Scholar]
- 56.Abbasi AM, Khan SM, Ahmad M, Khan MA, Quave CL, Pieroni A. Botanical ethnoveterinary therapies in three districts of the Lesser Himalayas of Pakistan. Journal of ethnobiology and ethnomedicine. 2013;9(1):84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Kayani S, Ahmad M, Zafar M, Sultana S, Khan MPZ, Ashraf MA, et al. Ethnobotanical uses of medicinal plants for respiratory disorders among the inhabitants of Gallies–Abbottabad, Northern Pakistan. Journal of ethnopharmacology. 2014;156:47–60. doi: 10.1016/j.jep.2014.08.005 [DOI] [PubMed] [Google Scholar]
- 58.Schoene RB. Lung disease at high altitude Hypoxia: Springer; 1999. p. 47–56. [DOI] [PubMed] [Google Scholar]
- 59.de Lucena RFP, de Alburquerque UP. Can apparency affect the use of plants by local people in tropical forests? Interciencia: Revista de ciencia y tecnología de América. 2005;30(8):506–11. [Google Scholar]
- 60.Yasuda S, Shohtsu A, Ide M, Takagi S, Takahashi W, Suzuki Y, et al. Chronic thyroiditis: diffuse uptake of FDG at PET. Radiology. 1998;207(3):775–8. doi: 10.1148/radiology.207.3.9609903 [DOI] [PubMed] [Google Scholar]
- 61.Logan MH. Informant consensus: a new approach for identifying potentially effective medicinal plants. Plants in indigenous medicine and diet: Biobehavioral approaches. 1986:91. [Google Scholar]
- 62.Mukherjee PK, Nema NK, Venkatesh P, Debnath PK. Changing scenario for promotion and development of Ayurveda–way forward. Journal of ethnopharmacology. 2012;143(2):424–34. doi: 10.1016/j.jep.2012.07.036 [DOI] [PubMed] [Google Scholar]
- 63.Heinrich M, Ankli A, Frei B, Weimann C, Sticher O. Medicinal plants in Mexico: Healers' consensus and cultural importance. Social Science & Medicine. 1998;47(11):1859–71. [DOI] [PubMed] [Google Scholar]
- 64.Murad W, Azizullah A, Adnan M, Tariq A, Khan KU, Waheed S, et al. Ethnobotanical assessment of plant resources of Banda Daud Shah, District Karak, Pakistan. Journal of ethnobiology and ethnomedicine. 2013;9(1):1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Magan N, Aldred D, Hope R, Mitchell D. Environmental factors and interactions with mycobiota of grain and grapes: effects on growth, deoxynivalenol and ochratoxin production by Fusarium culmorum and Aspergillus carbonarius. Toxins. 2010;2(3):353–66. doi: 10.3390/toxins2030353 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Torres-Avilez W, Medeiros PMd, Albuquerque UP. Effect of Gender on the Knowledge of Medicinal Plants: Systematic Review and Meta-Analysis. Evidence-Based Complementary and Alternative Medicine. 2016;2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.de Albuquerque UP, Soldati GT, Sieber SS, Ramos MA, de Sá JC, de Souza LC. The use of plants in the medical system of the Fulni-ô people (NE Brazil): a perspective on age and gender. Journal of ethnopharmacology. 2011;133(2):866–73. doi: 10.1016/j.jep.2010.11.021 [DOI] [PubMed] [Google Scholar]
- 68.Bruschi P, Morganti M, Mancini M, Signorini MA. Traditional healers and laypeople: a qualitative and quantitative approach to local knowledge on medicinal plants in Muda (Mozambique). Journal of Ethnopharmacology. 2011;138(2):543–63. doi: 10.1016/j.jep.2011.09.055 [DOI] [PubMed] [Google Scholar]
- 69.Ch MI, Ahmed F, Maqbool M, Hussain T. Ethnomedicinal inventory of flora of Maradori valley, District Forward Khahuta, Azad Kashmir, Pakistan. 2013. [Google Scholar]
- 70.Amjad MS, Arshad M, Qureshi R. Ethnobotanical inventory and folk uses of indigenous plants from Pir Nasoora National Park, Azad Jammu and Kashmir. Asian Pacific Journal of Tropical Biomedicine. 2015;5(3):234–41. [Google Scholar]
- 71.Kayani S, Ahmad M, Sultana S, Shinwari ZK, Zafar M, Yaseen G, et al. Ethnobotany of medicinal plants among the communities of Alpine and Sub-alpine regions of Pakistan. Journal of ethnopharmacology. 2015;164:186–202. doi: 10.1016/j.jep.2015.02.004 [DOI] [PubMed] [Google Scholar]
- 72.Mahmood A, Riffat N, Zabta K, Aqeel M. Ethnobotanical survey of plants from Neelum, Azad Jammu and Kashmir, Pakistan. Pak J Bot. 2011;43:105–10. [Google Scholar]
- 73.Yaseen G, Ahmad M, Sultana S, Alharrasi AS, Hussain J, Zafar M. Ethnobotany of medicinal plants in the Thar Desert (Sindh) of Pakistan. Journal of ethnopharmacology. 2015;163:43–59. doi: 10.1016/j.jep.2014.12.053 [DOI] [PubMed] [Google Scholar]
- 74.Altundag E, Ozturk M. Ethnomedicinal studies on the plant resources of east Anatolia, Turkey. Procedia-Social and Behavioral Sciences. 2011;19:756–77. [Google Scholar]
- 75.Heywood V. The Mediterranean region: a major centre of plant diversity. Wild food and non-food plants: Information networking Chania: CIHEAM-IAMC; 1999:5–13. [Google Scholar]
- 76.Gupta AK. Wipo-Unep Study on the Role of Intellectual Property Rights in the Sharing of Benefits Arising from the Use of Biological Resources and Associated Traditional Knowledge-Study: WIPO; 2004. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
(DOCX)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.