Abstract
Objective
To assess whether the implementation of a package of activities through the joint action of the three international healthcare professionals associations (HCPAs) increased the use of intrapartum and postnatal essential interventions (EIs) in two hospitals in Uganda.
Methods
A non-controlled before-and-after study was undertaken to evaluate the effect of a package of activities designed to change practice relating to nine EIs among providers. Coverage of the EIs was measured in a 3-month pre-implementation period and a 3-month post-implementation period in 2014. Data were obtained for women older than 18 years who delivered vaginally or by cesarean.
Results
Overall, 4816 women were included. Level of use remained high for EIs used widely at baseline. Some EIs that had low use at baseline did not show improvement after the implementation. Promotion of breastfeeding showed a significant improvement in the Kampala hospital, from 8.5% (8/94) to 25.6% (30/117; P=0.001), whereas promotion of hygiene in cord care improved at the Mbarara hospital, from 0.1% (2/1592) to 46.0% (622/1351; P<0.001).
Conclusion
These exploratory results show that a package delivered through the joint work of the three HCPAs was feasible to implement along with rigorous data collection. Although the data show disparities, trends suggest that improvement could be achieved.
Keywords: Childbirth, Essential interventions, Health provider, Neonatal health, Professional associations
1 INTRODUCTION
In 2011, the first ever multi-stakeholder consensus on what works for reproductive, maternal, newborn, and child health (RMNCH) along the continuum of care, based on comprehensive scientific evidence, culminated in the development of the Essential Interventions, Commodities and Guidelines for RMNCH [1]. WHO and the Partnership for Maternal, Newborn and Child Health (PMNCH) urged the healthcare professional associations (HCPAs) to lead a movement to accelerate the dissemination of these guidelines and make a change in health providers’ practice, with a focus on improving quality of care.
In line with this strategy two key constituencies of the PMNCH—the academic constituency represented by the Institute for Clinical Effectiveness and Health Policy and HCPAs represented by the International Federation of Gynecology and Obstetrics (FIGO), the International Confederation of Midwives (ICM), and the International Pediatric Association (IPA)—developed a proposal to test the effectiveness and impact of a package of activities to accelerate the implementation of selected essential interventions (EIs) in maternal and newborn health care through joint work. The aim of the resulting study was to assess whether the implementation of a package of activities in Uganda through the joint action of the three international HCPAs and national affiliates—the Association of Obstetricians and Gynecologists of Uganda, the Uganda Private Midwives Associations, and the Ugandan Pediatrics Association—increased the use of selected EIs in two hospitals. In 2010, Uganda had a high maternal mortality ratio of 420 per 100,000 live births and a neonatal mortality rate of 22 per 1000 live births [2].
2 MATERIALS AND METHODS
The present non-controlled before-and-after study was undertaken in 2014. The three international HCPAs created an effective governance, leadership, and advisory framework for the study by establishing an international steering committee (ISC). The three national HCPAs, civil societies, and academia formed the national steering committee (NSC) to support the operationalization of the study. In the NSC, the representatives had an equal role in the study planning, conduct, monitoring and supervision, and dissemination of results. The NSC appointed a National Coordinator to coordinate all activities and become the intermediator for collaboration with international project staff. Approval for the present study was obtained from the institutional review boards of Tulane University (New Orleans, LA, USA), Mbarara University of Science and Technology, and St. Francis Hospital Nsambya. All participants provided written informed consent.
A global review of the key interventions related to RMNCH [1] identified 56 evidence-based EIs that have the greatest impact on maternal and neonatal outcomes, and the maximum potential to reduce maternal and neonatal deaths. The ISC identified 17 EIs for implementation, but data were collected for only nine to ensure study viability (Table 1). The selection of nine EIs was based on several criteria, including a requirement to select at least two general interventions and one specific intervention for childbirth and newborns, applicability to all women and newborns, measurability of coverage rate, prevalence, feasibility of data collection, and acceptability to health workers.
Table 1.
The nine essential interventions selected for the present study.
| Essential intervention | Definition of successful implementation |
|---|---|
| Promotion and provision of thermal care for all newborns to prevent hypothermia (immediate drying, warming, skin-to-skin contact, delayed bathing) | The neonate was dried with a towel or cloth immediately after birth including head while cord still attached, AND bathing of the neonate delayed 6 hours after being born, AND neonate placed on its mother’s chest immediately after birth while being dried for at least 2 hours OR placed on its mother’s abdomen immediately after birth while being dried for at least 2 hours (among all live newborns) |
| Promotion and provision of hygienic cord and skin care | Hand hygiene on behalf of the health provider before manipulating the newborn’s skin or cord, AND cord clamping more than 1 min after the birth or when cord pulsation has ceased, AND use of chlorhexidine before manipulating the newborn’s skin or cord |
| Promotion and support for early initiation of breastfeeding (within the first hour) | Initiation of breastfeeding within the hour after birth (among all live newborns) |
| Prophylactic uterotonic to prevent postpartum hemorrhage | Use of uterotonics in all deliveries |
| Social support during childbirth | The woman had a companion during labor, AND health workers allowed the woman to have a companion of her choice to provide social support, AND health workers provided information to the companion during the labor among all deliveries |
| Prophylactic antibiotics for cesarean delivery | Use of prophylactic antibiotics in all cesarean deliveries |
| Induction of labor for prolonged pregnancy | Induced initiation of labor among all pregnancies >41 wk |
| Kangaroo mother care for preterm neonates and/or neonates weighing <2000 g, live births. | Provision of kangaroo mother care (among preterm and/or <2000-g newborns live births). |
| Continuous positive airway pressure to manage preterm neonates with respiratory distress syndrome | Provision of continuous positive airway pressure (among all live newborns with respiratory distress syndrome) |
Two hospitals were selected: St. Rafael of St Francis Hospital Nsambya in Kampala and Mbarara Regional Referral Hospital in Mbarara (Table 2). These hospitals were chosen by the ISC in collaboration with the NSC on the basis of their substantial case load (allowing interventions to have a high impact), their mix of health professionals (allowing collaboration between obstetricians, midwives, and pediatricians), their status as teaching hospitals (ideal locations for introducing/strengthening good practices), their diverse location, and ownership and availability of data collection systems.
Table 2.
Hospital characteristics.a
| Characteristic | Kampala | Mbarara |
|---|---|---|
| Name | St. Rafael of St. Francis Hospital Nsambya | Mbarara Regional Referral Hospital |
| Location | Urban | Rural |
| Type of facility | General not-for-profit private hospital | Regional tertiary referral facility |
| Estimated no. of deliveries in 2012 | 7878 | 10 000 |
| Bed capacity | 361 | 450 |
| Maternal mortality ratio | 1010 per 100 000 live births | 270 per 100 000 live births |
| Cesarean rate, % | 26.6 | 30 |
| Obstetricians b | 25/91 (27.5) | 31/66 (47.0) |
| Midwives b | 55/91 (60.4) | 20/66 (30.3) |
| Pediatricians b | 11/91 (12.1) | 15/66 (22.7) |
Data were provided by Hospital Director.
Includes consultants, residents, and interns; values are given as number/total skilled birth attendants working in participating hospitals (percentage).
Coverage of EIs related to childbirth and postnatal care was measured and compared between a 3-month pre-implementation baseline period (between March 11 and June 10, 2014) and a 3-month post-implementation period (June 11 to October 11, 2014). All consecutive women older than 18 years who signed an informed consent form and had a vaginal or cesarean delivery, either with or without complications, were included along with their newborns receiving care in the neonatal units of the study hospitals. Women with mental or physical impairments that prevented them from being interviewed were ineligible.
The primary outcomes were the rates of use of the selected EIs for childbirth and postnatal care. Data were collected from paper medical records using specifically designed paper clinical research forms. Trained in-hospital data collectors performed daily revision of the clinical research forms, data validation, and transmission to a centralized web based repository. A comprehensive tracking system for the clinical research forms was implemented, and data quality reports were generated on a weekly basis by the data center at the Institute for Clinical Effectiveness and Health Policy, Buenos Aires, Argentina. Additionally, mothers were asked to complete an interview before discharge to complement and validate data about social support during childbirth, thermal care, and promotion and support for early initiation of breastfeeding and exclusive breastfeeding. For each woman in the study, an alphanumeric number was assigned. Names and other personal identifiers were recorded in a separate form that was securely kept at the health facility to preserve participants’ anonymity.
After the 3-month baseline period, a package of activities was implemented. The activities were chosen for their effectiveness in leading to change in practice [3], and the package was implemented by the three types of health professionals. The package of activities and the implementation guidelines [4,5] were designed jointly by the ISC and NSC. They expanded on an evidence-based conceptual framework, supported by a communication strategy. The package included six activities: dissemination workshops, reminder development, birth simulation sessions, team building, case reviews, and academic visits in the wards. A booklet explaining the nine EIs was produced for dissemination, as well as a checklist and monitoring cards for other activities.
A group of health providers, identified as opinion leaders (henceforth, facilitators), were selected at each participating hospital. The facilitators were trained in a 2-day workshop by national HCPAs on how to implement and disseminate the package of activities. The workshop focused on the dissemination of guidelines followed by reinforcement through integration with other activities in the package.
The activities included in the dissemination workshop had three components: dissemination of WHO standards for the EIs through dissemination workshops and reminders [6], observation of clinical practice by a team of hospital facilitators during academic visits [7], and discussion platforms joining the three professions through simulation, case reviews, and team-building sessions.
The facilitators implemented the package of activities to health providers in the facilities. This approach was used to engage and encourage participation by all staff in the maternity team. The facilitators and HCPAs endorsed these activities and used a multifaceted approach to disseminate, and implement the guidelines through design and use of reminders, feedback, educational and team-building sessions, and use of birth and resuscitation simulators. The approach involved strong dissemination of the guidelines among all actors involved in patient care. The national coordinator met periodically with each facilitators’ team to assess completion of activities.
The secondary outcomes of the study were health providers’ participation in implementation activities and perceptions about their knowledge regarding the EIs to evaluate the joint work of obstetrician/gynecologists, midwives, and pediatricians. All skilled health providers working in the maternity and neonatal ward of the selected hospitals completed an anonymous, self-administered questionnaire at the end of the study period in October 2014, after enrollment finished. The questionnaire assessed their participation in the different activities that comprised the package of activities and their knowledge regarding their professional capacity on the selected EIs. Providers were asked to answer the survey thinking back to their knowledge of the EIs in March 2014 in comparison with their current knowledge.
Originally, the study was designed with a longer timeframe; however, owing to financial constraints, a before and after approach was used. The sample size was calculated to detect a change in the frequency of use of the EIs of between 15% and 20% (from 10% and 50% at baseline to 25% and 70% after implementation), assuming the interventions were applicable to 20% of patients. A sample size between 350 and 1250 women was necessary to power the study at 80% with a significance level of 5%.
To test the primary outcomes—rates of use of the nine EIs—the hospitals were considered as the unit of analysis. We were interested in observing the absolute difference in the percentages of women and newborns who received the EIs between the baseline period and the post-implementation period. The outcome rate was computed for each hospital at baseline and the post-implementation period for each intervention, and the outcome difference was then calculated.
Coverage or adherence to the EIs was quantified by dividing the number of eligible patients who received the item by the total number of eligible patients. Results were expressed in percentages. Descriptive statistics were used to calculate the demographics and clinical characteristics of the women giving birth and the newborns. The frequency of all EIs was calculated by study period and compared using a t test.
Health providers’ survey responses were reported for the entire sample of respondents who provided consent and at country level. Descriptive statistics were used to describe the sample characteristics. For questions with yes/no answers, the percentage of positive answers was reported. For questions with multiple answers (none, poor, good, or excellent ), responses were recoded using the dichotomous variables “poor” (none and poor) and “excellent” (good and excellent). Percentages of good-excellent answers are reported. The McNemar test was used to compare answers. P<0.05 was considered significant.
All variables included in the analysis of the present report were computed as dichotomized answers. Don’t know/data not available answers were entered as missing data. Thermal care was considered accomplished when three of the four items that compose this EI were present (items 3 and 4 were interchangeable). However, for cord care hygiene and skin care, all three components must have been present.
Analysis was performed in Stata 11.0 (StataCorp, College Station, TX, USA). P<0.05 was considered significant.
3 RESULTS
A total of 4816 women were enrolled during the 6-month period of the study in the two sites: 3075 at the Mbarara hospital and 1740 at the Kampala hospital. The proportion of women aged 19 or younger was higher in Mbarara than Kampala, as was rate of stillbirth (Table 3). Other characteristics were similar between hospitals (Table 3).
Table 3.
Characteristics of women and newborns at the participating health facilities.a
| Characteristic | Total (n=4815) | Kampala (n=1740) | Mbarara (n=3075) |
|---|---|---|---|
| Maternal | |||
| Age, y | |||
| ≤19 | 390/4743 (8.2) | 23/1729 (1.3) | 367/3014 (12.2) |
| ≥35 | 445/4743 (9.4) | 230/1729 (13.3) | 215/3014 (7.1) |
| Parity | |||
| 0 | 1214/4747 (25.6) | 428/1729 (24.8) | 786/3018 (26.0) |
| ≥4 | 776/4747 (16.3) | 271/1729 (15.7) | 505/3018 (16.7) |
| Pregnancy length ≤37 wk | 656/3945 (16.6) | 119/1618 (7.4) | 130/2270 (5.7) |
| Cesarean delivery | 1730/4812 (36.0) | 683/1736 (39.3) | 1047/3076 (34.0) |
| Died before discharge | 3/4739 (0.1) | 1/1722 (0.1) | 2/3017 (0.1) |
| Neonatal | |||
| Birth weight <2500 g | 298/4537 (6.6) | 124/1643 (7.5) | 174/2894 (6.0) |
| Status at discharge | |||
| Stillborn | 121/4746 (2.5) | 17/1727 (1.0) | 104/3019 (3.4) |
| Alive | 4595/4746 (96.8) | 1699/1727 (98.4) | 2896/3019 (95.9) |
| Referred | 18/4746 (0.4) | 2/1727 (0.1) | 16/3019 (0.5) |
| Died | 12/4746 (0.3) | 9/1727 (0.5) | 3/3019 (0.1) |
Values are given as number/total number (percentage).
The proportions of EI compliance during and after deliveries by site before and after implementation are given in Table 4. At baseline, promotion and provision of thermal care, prophylactic uterotonics to prevent postpartum hemorrhage, and social support during childbirth showed similar high use in the two hospitals. However, promotion and support for early initiation of breastfeeding, and use of prophylactic antibiotics were much rarer in Kampala than in Mbarara.
Table 4.
Adherence to the nine essential interventions during and after deliveries before and after implementation of the package of activities.a
| Essential intervention | Before implementation | After implementation | P value b |
|---|---|---|---|
| Promotion and provision of thermal care for all newborns to prevent hypothermia | |||
| Kampala | 493/682 (72.3) | 471/579 (81.3) | <0.001 |
| Mbarara | 1026/1159 (88.5) | 857/970 (88.4) | 0.900 |
| Promotion and provision of hygienic cord and skin care | |||
| Kampala | ND | ND | ND |
| Mbarara | 2/1592 (0.1) | 622/1351 (46.0) | <0.001 |
| Promotion and support for early initiation of breastfeeding | |||
| Kampala | 8/94 (8.5) | 30/117 (25.6) | 0.001 |
| Mbarara | 778/804 (96.8) | 1267/1277 (99.2) | <0.001 |
| Prophylactic uterotonic to prevent postpartum hemorrhage | |||
| Kampala | 892/893 (99.9) | 829/829 (100.0) | 0.335 |
| Mbarara | 1594/1604 (99.4) | 1417/1419 (99.9) | 0.035 |
| Social support during childbirth | |||
| Kampala | 880/910 (96.7) | 670/828 (80.9) | <0.001 |
| Mbarara | 1643/1654 (99.3) | 1417/1419 (99.9) | 0.026 |
| Prophylactic antibiotics for cesarean delivery | |||
| Kampala | 32/316 (10.1) | 8/205 (3.9) | 0.009 |
| Mbarara | 169/205 (82.4) | 351/353 (99.4) | <0.001 |
| Induction of labor for prolonged pregnancy | |||
| Kampala | 56/153 (36.6) | 30/106 (28.3) | 0.163 |
| Mbarara | 10/230 (4.3) | 5/203 (2.5) | 0.285 |
| Kangaroo mother care for preterm neonates and/or neonates weighing <2000 g | |||
| Kampala | 23/26 (88.5) | 8/12 (66.7) | 0.107 |
| Mbarara | 6/10 (60.0) | 4/8 (50.0) | 0.677 |
| Continuous positive airway pressure to manage preterm neonates with respiratory distress syndrome | |||
| Kampala | 28/28 (100.0) | 26/27 (96.3) | 0.304 |
| Mbarara | 6/8 (75.0) | 1/1 (100.0) | 0.571 |
Abbreviation: ND, no data.
Values are given as number/total number (percentage) unless indicated otherwise.
χ2 test.
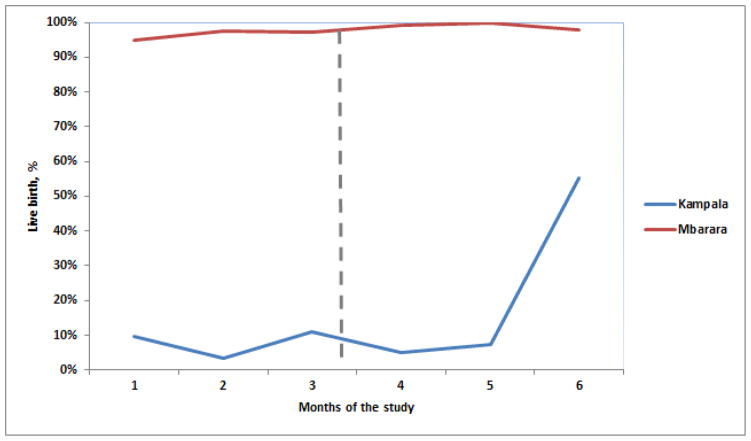
Different patterns of change were seen among the EIs after implementation. Level of use remained high for the EIs used widely at baseline: promotion and provision of thermal care, kangaroo mother care, social support, and prophylactic uterotonics in both hospitals, and promotion and support of early initiation of breastfeeding and prophylactic antibiotics for cesarean in Mbarara. Social support did decrease significantly in Kampala but the value remained high from a clinical perspective. Some EIs that had low use in the baseline period did not show improvement after implementation, including induction of labor for prolonged pregnancy and prophylactic antibiotics for cesarean in Kampala. Promotion and support for early initiation of breastfeeding showed a significant improvement after implementation in Kampala (Figure 1). Additionally, promotion of cord care improved in Mbarara.
Figure 1.
Proportion of live births for which breastfeeding was initiated within 1 hour of birth. The dotted line indicates when implementation began.
There were 157 healthcare workers from both sites were invited to participate in the health providers’ survey. The response rate of the survey was 46.5%. Most of the respondents were midwives (n=40 [54.8%]), with a mean of 6–7 years working in the health system (Table 5). More than half the providers participated in dissemination sessions, use of reminders, follow-up visits, case reviews, and team building sessions (data non shown). Most respondents rated their knowledge as good or excellent for each of the EIs at baseline, but noted an improvement in their knowledge after the project in all of the EIs under study except for induction of labor (Table 6).
Table 5.
Healthcare providers’ characteristics. a
| Characteristic | Obstetricians (n=25) | Midwives (n=40) | Pediatricians (n=8) |
|---|---|---|---|
| Female | 7/25 (28) | 36/40 (90) | 4/8 (50) |
| Hospital | |||
| Kampala | 10/25 (40) | 27/40 (68) | 3/8 (38) |
| Mbarara | 15/25 (60) | 13/40 (33) | 5/8 (63) |
| Time in system, y | 7.1 ± 5.9 | 7.5 ± 6.9 | 6.2 ± 5.3 |
| Time in facility, y | 5.0 ± 5.6 | 6.3 ± 5.8 | 3.1 ± 2.2 |
| Deliveries in facility | |||
| <250 | 5/21 (24) | 3/29 (10) | 4/6 (67) |
| >250 | 16/21 (76) | 26/29 (90) | N/A |
| Place of work | |||
| Labor ward | 12/23 (52) | 19/40 (48) | N/A |
| Postnatal ward | 4/23 (17) | 12/40 (30) | N/A |
| Neonatal unit | N/A | 8/40 (20) | 7/8 (88) |
| Other | 7/23 (30) | 1/40 (3) | 1/8 (13) |
Abbreviation: N/A, not available.
Values are given as number/total number (percentage) or mean ± SD.
Table 6.
Health providers’ perception about their level of knowledge regarding the nine essential interventions before and after the implementation of a package of activities. a
| Essential intervention | Before implementation (n=73) | After implementation (n=73) | P value b |
|---|---|---|---|
| Promotion and provision of thermal care for all newborns (good or excellent) | 81.8 | 93.7 | 0.001 |
| Promotion and provision of hygienic cord and skin care (good or excellent) | NA c | NA | NA |
| Promotion and support for early initiation of breastfeeding (good or excellent) | 81.8 | 93.7 | 0.001 |
| Prophylactic uterotonic to prevent postpartum hemorrhage(good or excellent) | 93.6 | 95.0 | 0.563 |
| Promotion of social support during childbirth (good or excellent) | 81.6 | 100 | 0.004 |
| Prophylactic antibiotics for cesarean delivery (good or excellent) | 69.2 | 84.2 | <0.001 |
| Induction of labor for prolonged pregnancy (good or excellent) | 69.2 | 69.2 | >0.99 |
| Kangaroo mother care for preterm neonates and/or neonates weighing <2000 g (good or excellent) | 76.6 | 87.3 | 0.011 |
| Continuous positive airway pressure to manage preterm neonates with respiratory distress syndrome (good or excellent) | 66.7 | 82.5 | <0.001 |
Values are given as percentage unless indicated otherwise.
McNemar test.
Data not available.
4 DISCUSSION
The present study has highlighted the ability and capacity of the three international HCPAs (FIGO, ICM, and IPA) to mobilize and support a task force of national organizations to participate in initiatives to improve the care of mothers and newborns. The national organizations showed leadership, took ownership and developed capacity to establish a prospective database, and to implement (in an escalating manner) a package of activities through coordinated efforts to improve the implementation of EIs during delivery and the postpartum period at urban and regional hospitals in Uganda.
The study found there was minimal change after implementation in the EIs that were frequently used at baseline, whereas there was increase in some EIs that had not been used regularly. However, some EIs with low baseline use did not show improvement after implementation. Although it is difficult to show significant behavioral change in short periods of time, substantial improvement has been made because the implementation of the package of activities increased the health providers’ self-perception of their knowledge.
Among childbirth interventions, the present study showed that almost all women enrolled in both periods received prophylactic uterotonics to prevent postpartum hemorrhage. This finding is encouraging, because this intervention prevents a lethal condition responsible for many maternal deaths [8,9]. Similarly, social support in childbirth also showed high compliance, in accordance with the recommendations of the scientific evidence [10]. However, induction of labor for prolonged pregnancy is was quite rare. For postnatal interventions, early initiation of breastfeeding has been found to be very well adopted among health providers and mothers, with high values in Mbarara and an increase in Kampala to 25.6%, as well as hygienic cord and skin care increasing from almost no use in Mbarara to approximately half (46.0%) after the intervention. High use of provision of thermal care was shown.
The present study has several strengths. A high-standard data collection system was established in two hospitals of a low-income-country, and a remote data collection structure was developed with a specialized data center following good practice guidelines. This confirms that data collection is feasible in a low-income setting. A careful monitoring and data plan resulted not only in the development of proper trained local teams involving data managers, data collectors, and hospital and national coordinators, but also in the collection of a proper dataset.
Nevertheless, the present study has many limitations. As a result of financial constraints the study needed to be shortened and instead of a time-series design a before and after design was used. Secular trends or sudden changes make it difficult to attribute observed changes to the implementation of the package of activities. Implementation could be accompanied by other changes in care or additional resources that confound any attempt to infer causality directly [11]. Analysis of the effect of confounders (urban/rural, policy, context) was not done in the present study. It is common in this type of study design to overestimate effects. Consequently, results should be interpreted with caution. Regarding this last statement, major variations in the outcomes than can be justified by the package of activities only have been highlighted; minor changes in the outcomes could only be attributed to the activities with caution.
In conclusion, the present study shows that the joint work of the three HCPAs (FIGO, ICM and IPA) at international and national levels led to the implementation of a package of activities to improve the use of the EIs at two hospitals in Uganda. The process involved shows that it could be possible to implement in other settings, although it would be interesting to assess the sustainability of such a package and test it in other countries.
Synopsis.
A package of activities led by three healthcare professional associations improved the use of essential interventions related to childbirth and neonatal health in Uganda.
Acknowledgments
The authors acknowledge Laerdal Medical AS for the provision of 10 MamaNatalie simulators and Glowm for their contribution of USB sticks with videos on maternal and child care. Funding for the present study (phase 1) was provided by PMNCH. PMNCH is supporting phase 2 to replicate the study in Nepal and examine sustainability of activities in Uganda. The present study was partly funded by the Fogarty Maternal and Child Health Research Training Program (D43 TW005492)/Fogarty International Center/National Institutes of Health.
Footnotes
Author contributions
CS was the lead author and drafted the manuscript. CS, MB, EGE, and JMB led analysis of quantitative data; AK and SJ led that of qualitative data. AK, SJ, HR, PC, FD-S, and JMB were instrumental in study design. CS, AK, SJ, DA, JN, CPN, RB, MB, and EGE were responsible for conduct of study activities and provided oversight of all activities. All authors reviewed and approved this manuscript before submission.
Conflicts of interest
The authors have no conflicts of interest.
References
- 1.The Partnership for Maternal, Newborn and Child Health. Essential Interventions, Commodities and Guidelines for Reproductive, Maternal, Newborn and Child Health. [Accessed, June, 8th, 2017];A Global Review of the Key Interventions Related to Reproductive, Maternal, Newborn and Child health (RMNCH) 2011 http://www.who.int/pmnch/topics/part_publications/essential_interventions_18_01_2012.pdf.
- 2.WHO, UNICEF, UNFPA, World Bank Group and the United Nations Population Division. [Accessed June 8th, 2017];Trends in maternal mortality, 1990 – 2015. 2016 :56. http://www.who.int/reproductivehealth/publications/monitoring/maternal-mortality-2015/en/
- 3.Grimshaw JM, Thomas RE, MacLennan G, et al. Effectiveness and efficiency of guideline dissemination and implementation strategies. Health Technology Assessment. 2004;8:1–72. doi: 10.3310/hta8060. [DOI] [PubMed] [Google Scholar]
- 4.Jacob S, Kwizera A. [Accessed September, 27, 2016];Essential interventions for safer maternal and newborn health: Guide to support implementation by practitioners. http://www.figo.org/sites/default/files/uploads/project-publications/PMNCH/Guide%20booklet%20A5_Package%20of%20activities_Joint%20initiative%20EIs%20toolkit_FIGO%20ICM%20IPA%202014.pdf. Published 2014.
- 5.Kwizera A, Jacob S. [Accessed September, 27, 2016];Essential interventions for safer maternal and newborn health: Package of activities: Cards and checklists. http://www.figo.org/sites/default/files/uploads/project-publications/PMNCH/Cards%20and%20check%20list%20A5_Package%20of%20activities_Joint%20initiative%20EIs%20toolkit_FIGO%20ICM%20IPA%202014.pdf. Published 2014.
- 6.Cheung A, Weir M, Mayhew A, et al. Overview of systematic reviews of the effectiveness of reminders in improving healthcare professional behavior. Systematic reviews. 2012;1(1):1–36. doi: 10.1186/2046-4053-1-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.O’brien M, Rogers S, Jamtvedt G, et al. Educational outreach visits: effects on professional practice and health care outcomes (Review) The Cochrane Library. 2008;3:1–64. doi: 10.1002/14651858.CD000409.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Westhoff G, Cotter AM, Tolosa JE. Prophylactic oxytocin for the third stage of labour to prevent postpartum haemorrhage. Cochrane Database of Systematic Reviews. 2013;(10) doi: 10.1002/14651858.CD001808.pub2. Art. No.: CD001808. [DOI] [PubMed] [Google Scholar]
- 9.Salam RA, Mansoor T, Mallick D, et al. Essential childbirth and postnatal interventions for improved maternal and neonatal health. Reprod Health. 2014;11(Suppl 1):S3. doi: 10.1186/1742-4755-11-S1-S3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hodnett ED, Gates S, Hofmeyr GJ, et al. Continuous support for women during childbirth. Cochrane Database of Systematic Reviews. 2013;(7) doi: 10.1002/14651858.CD003766.pub5. Art. No.: CD003766. [DOI] [PubMed] [Google Scholar]
- 11.Grimshaw J, Campbell M, Eccles M, et al. Experimental and quasi-experimental designs for evaluating guideline implementation strategies. Family practice. 2000;(Suppl 1):S11–6. doi: 10.1093/fampra/17.suppl_1.s11. [DOI] [PubMed] [Google Scholar]