Abstract
Background:
Neuroendocrine carcinoma is rare with a proportion of less than 2% in gallbladder malignancies, cases of gallbladder neuroendocrine cell carcinoma coexisting with adenocarcinoma are exceptionally rare, and the prognosis is dismal.
Methods:
Herein, we presented an unusual case of poorly differentiated gallbladder neuroendocrine cell carcinoma coexisting with poorly differentiated adenocarcinoma who survived 20 months after the multimodal treatment (MT) of extended surgery and postoperative chemotherapy.
Results:
Our result indicated that for advanced gallbladder neuroendocrine cell carcinoma coexisting with adenocarcinoma, MT including extended surgical approach combined with postoperative chemotherapy may contribute to a relatively good survival outcome.
Conclusion:
MT may contribute to a relatively good survival outcome for advanced gallbladder neuroendocrine cell carcinoma coexisting with gallbladder adenocarcinoma.
Keywords: adenocarcinoma, gallbladder, multimodal treatment, neuroendocrine
1. Introduction
Gallbladder malignant lesions are almost adenocarcinomas; the gallbladder mucosa is absence of neuroendocrine cell, this is the reason why neuroendocrine carcinoma is rare with a proportion of less than 2% in gallbladder malignancies,[1] cases of gallbladder neuroendocrine cell carcinoma coexisting with adenocarcinoma are exceptionally rare, the clinic features and treatment options are also unclear. Considering the malignant biologic potency of neuroendocrine carcinoma and advanced tumor stage, the prognosis is dismal even after curative resection. It was reported patients with the conjunction of the 2 tumor types have a median survival time of 4 months and seldom survived longer than 1 year,[2,3] and it is still a headache faced by surgeons.
Herein, we presented an unusual case of poorly differentiated gallbladder neuroendocrine cell carcinoma coexisting with poorly differentiated adenocarcinoma who survived 20 months after the multimodal treatment (MT) of extended surgery and postoperative chemotherapy to help recognize the clinical features and treatment options of this disease.
2. Case presentation
A woman, aged 40 years, was admitted due to epigastric pain and discomfort for half a month. She has no history of gastrointestinal illness or immunological diseases. Surgical history included 1 cesarean section 18 years prior and hysteromyomectomy 15 years ago. No special abnormality was found on physical examination. The laboratory tests (including routine blood, liver and kidney function, and serum tumor markers) were well within the normal scope. Serological tests of hepatitis B and C were also negative. Contrast-enhanced computed tomography revealed soft tissue density shadows (2.7 × 4.1 cm2) at the gallbladder plica with obvious enhancement (Fig. 1). The patient was suspected as gallbladder malignancy and underwent extended radical resection. Laparotomy was initially performed; by gross inspection, no peritoneal seeding or periaortic node metastasis was found. Then, we underwent lymph nodes biopsy of groups 13 and 16, and the result was negative; moreover, completed cholecystectomy, partial liver resection (segments IV b and V), and common bile duct excision was carried out. We also conducted hepatoduodenal ligaments and the celiac trunk lymph nodes dissection.
Figure 1.
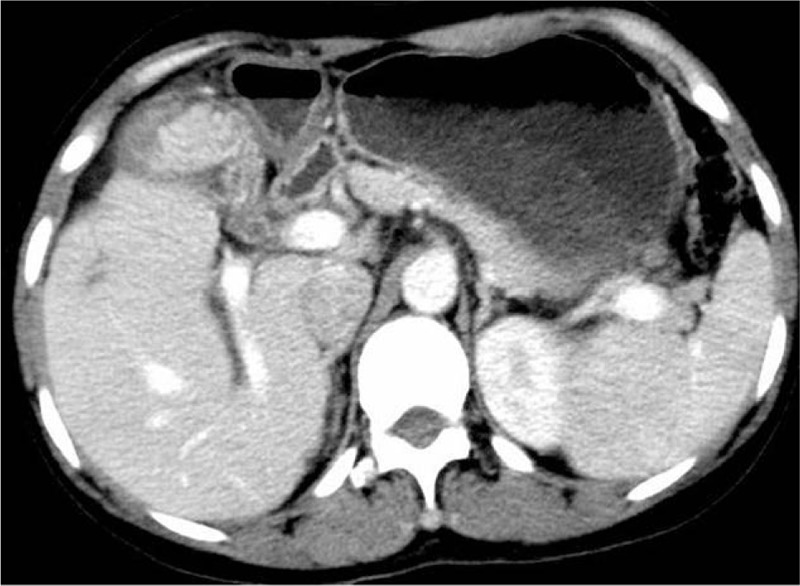
Contrast-enhanced computed tomography revealed soft tissue density shadows (2.7 × 4.1 cm2) at the gallbladder plica with obvious enhancement.
The gallbladder wall was obviously incrassate and the tumor (measuring 4.7 × 3 × 2.5 cm3) appeared as hoary, firm, and cauliflower-like. Histological results manifested that the tumor composed of 2 ingredients: neuroendocrine carcinoma cells and adenocarcinoma cells with a transitional mixed section (Fig. 2A). Immunohistochemical staining revealed the conventional poorly differentiated adenocarcinoma (Ki-67 index, 80%) with CD 56 (neural cell adhesion molecule), chromogranin A (CgA), synaptophysin (Syn), and neuron specific enolase (NSE) negative. Moreover, on the other part, it was positivity for CD 56, CgA (Fig. 2B), Syn (Fig. 2C), and NSE, with Ki-67 index of 60%, indicating the diagnosis of poorly differentiated neuroendocrine carcinoma. Finally, the patient was diagnosed as gallbladder neuroendocrine cell carcinoma coexisted with adenocarcinoma. After multidisciplinary team consultation, the patient subsequently underwent 6 cycles of chemotherapy using cisplatin (75 mg/m2) on day 1 and etoposide (100 mg/m2) days 1 to 3, repeated every 21 days. She was well followed up at our outpatient department and survived 20 months after surgery.
Figure 2.
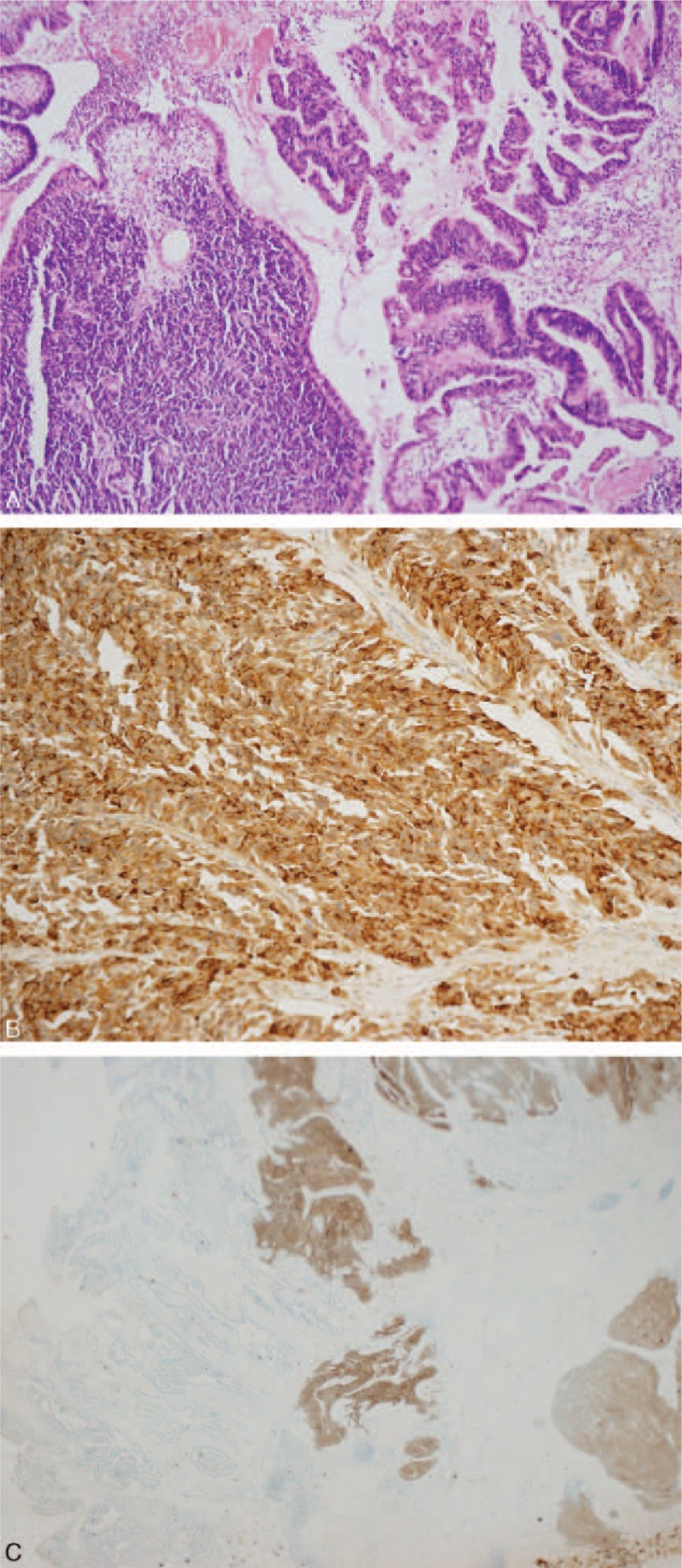
Pathologically identified gallbladder neuroendocrine carcinoma coexisted with adenocarcinoma. (A) Hematoxylin–eosin staining manifested a combination of neuroendocrine carcinoma cells and adenocarcinoma cells with a transitional mixed section. (B) Immunohistochemical staining indicating that the neuroendocrine carcinoma cells were positive for CgA. (C) Immunohistochemical staining indicating that the neuroendocrine carcinoma cells were positive for Syn. CgA = chromogranin A, Syn = synaptophysin.
3. Discussion
Under normal conditions, gallbladder malignant lesions are almost adenocarcinomas; neuroendocrine carcinoma, accounting for 1.25% of all malignant tumors, is rare with a proportion of less than 2% in gallbladder malignancies.[2,4–6] Since the normal gallbladder mucosa does not produce the neuroendocrine cells, it is now acknowledged that the normal gallbladder mucosa may undergo intestinal or gastric metaplasia due to the influence of chronic cholecystitis or cholelithiasis, expressing a variety of neuroendocrine cells.[7,8] The clinical manifestation and imaging testing of gallbladder neuroendocrine carcinoma are atypical and lack specificity, thus the diagnosis is rarely drawn before surgery and postoperative pathological diagnosis becomes the golden rule to make a precise diagnosis.
According to the current world health organization classification, neuroendocrine tumors can be classified into 3 categories: well differentiated neuroendocrine tumors, which demonstrate benign feature or inconclusive malignant potential; moderately differentiated neuroendocrine carcinomas, which are marked as low-grade malignancy; and poorly differentiated neuroendocrine carcinomas, which are characterized by high-grade malignancy.[9,10] Cases of gallbladder neuroendocrine cell carcinoma coexisting with adenocarcinoma are exceptionally rare, with no more than 150 cases reported in the literature. Considering the malignant biologic potency of neuroendocrine carcinoma, it has a high tendency to invade the adjacent hepatic tissues and has the character of early lymph node metastases, fatal vessel invasion, and distant metastases, resulting an exceedingly poor prognosis even after curative resection.[11,12] The prognosis becomes even worse when the patient possesses another poorly differentiated adenocarcinoma, evidence of displaying elevated Ki 67 index and high mitotic index also lead to a poor survival outcome.[7]
In our present study, we encountered a case of poorly differentiated neuroendocrine carcinoma combined with poorly differentiated adenocarcinoma in the gallbladder. We adopted aggressive surgical methods including extended resection of the liver parenchyma, the gallbladder, and lymph nodes followed by 6 cycles of adjuvant chemotherapy, although the histopathology results found that both of the 2 tumor types were poorly differentiated with elevated Ki 67 indexes, the patients have survived 20 months, and the relatively longer survival may owed to the extensive surgical approach and postoperative chemotherapy. Complete en bloc tumor removal appears to be the only curative therapeutic proposal for gallbladder neuroendocrine carcinoma, especially for patients detected at an earlier stage. Since these tumors are insensitive to traditional radiotherapy, we adopted adjuvant chemotherapy postoperatively; the role of chemotherapy also remains unpredictable. In our present study, the 2 tumor types were poorly differentiated, and the Ki 67 indexes were also highly elevated, the patient survived obviously longer than the previous median survival time, we think that the chemotherapy have played a vital role. However, the feasibility and effectiveness of chemotherapy in patients with both poorly differentiated neuroendocrine and poorly differentiated adenocarcinoma in the gallbladder needs to be further examined in future larger number of patient cases to demonstrate this observation. By illustrating this case, we believe a combination of early diagnosis, completed surgical treatment, MT, and proper postoperative detection may contribute to a better prognosis. Furthermore, an increased awareness of the biological feature and treatment option of this tumor is urgently required.
4. Conclusion
We reported a rare case of poorly differentiated neuroendocrine carcinoma combined with poorly differentiated adenocarcinoma in the gallbladder, the prognosis is dismal in previous studies. The therapeutic progress of our patient demonstrates that MT, including completed surgical treatment and postoperative chemotherapy, may contribute to a better prognosis.
4.1. Informed consent statement
Patient's informed consent could not be obtained because the patient died due to progression of the disease before we wrote the case report.
Acknowledgments
The authors thank the financial support from National Nature Science of China (30801111 and 30972923) and Science & Technology Support Project of Sichuan Province (no. 2014SZ0002-10).
Footnotes
Abbreviation: MT = multimodal treatment.
Author contributions: H-JH and R-XZ have contributed equally to the article and were the co–first authors; H-JH and R-XZ contributed to the data acquisition and analysis and drafted the manuscript. W-JM, QY, J-KW, Q-YJ, and S-JW contributed to data acquisition and analysis of the manuscript. N-SC and Y-QT were involved in the revision of the manuscript. F-YL contributed to the study design and revision of the manuscript. All authors read and approved the final manuscript.
Ethical approval: This article is a retrospective study and does not contain any studies with human participants or animals performed by any of the authors.
Funding/support: The work was supported by the National Nature Science of China (30801111 and 30972923) and Science & Technology Support Project of Sichuan Province (no. 2014SZ0002-10).
The authors have no conflicts of interest to disclose.
References
- 1.Chen H, Shen YY, Ni XZ. Two cases of neuroendocrine carcinoma of the gallbladder. World J Gastroenterol 2014; 20:11916–11920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kim DI, Seo HI, Lee JY, et al. Curative resection of combined neuroendocrine carcinoma and adenocarcinoma of the gallbladder. Tumori 2011; 97:815–818. [DOI] [PubMed] [Google Scholar]
- 3.Tsuchiya A, Endo Y, Yazawa T, et al. Adenoendocrine cell carcinoma of the gallbladder: report of a case. Surg Today 2006; 36:849–852. [DOI] [PubMed] [Google Scholar]
- 4.Liu W, Wang L, He XD, et al. Mixed large cell neuroendocrine carcinoma and adenocarcinoma of the gallbladder: a case report and brief review of the literature. World J Surg Oncol 2015; 13:114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yadav R, Jain D, Mathur SR, et al. Cytomorphology of neuroendocrine tumours of the gallbladder. Cytopathology 2015; 27:97–102. [DOI] [PubMed] [Google Scholar]
- 6.Albores-Saavedra J, Batich K, Hossain S, et al. Carcinoid tumors and small-cell carcinomas of the gallbladder and extrahepatic bile ducts: a comparative study based on 221 cases from the Surveillance, Epidemiology, and End Results Program. Ann Diagn Pathol 2009; 13:378–383. [DOI] [PubMed] [Google Scholar]
- 7.Eltawil KM, Gustafsson BI, Kidd M, et al. Neuroendocrine tumors of the gallbladder: an evaluation and reassessment of management strategy. J Clin Gastroenterol 2010; 44:687–695. [DOI] [PubMed] [Google Scholar]
- 8.Chen H. Two cases of neuroendocrine carcinoma of the gallbladder. World J Gastroenterol 2014; 20:11916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.KlÖPpel G, Perren A, Heitz PU. The gastroenteropancreatic neuroendocrine cell system and its tumors: the WHO classification. Ann N Y Acad Sci 2004; 1014:13–27. [DOI] [PubMed] [Google Scholar]
- 10.Klimstra DS, Modlin IR, Coppola D, et al. The pathologic classification of neuroendocrine tumors: a review of nomenclature, grading, and staging systems. Pancreas 2010; 39:707–712. [DOI] [PubMed] [Google Scholar]
- 11.Shimizu T, Tajiri T, Akimaru K, et al. Combined neuroendocrine cell carcinoma and adenocarcinoma of the gallbladder: report of a case. J Nippon Med Sch 2006; 73:101–105. [DOI] [PubMed] [Google Scholar]
- 12.Modlin IM, Lye KD, Kidd M. A 5-decade analysis of 13,715 carcinoid tumors. Cancer 2003; 97:934–959. [DOI] [PubMed] [Google Scholar]


