Abstract
The relationship between the prevalence of chronic diseases and income level has now become a main theme in poor national economic situations. We examined the prevalence of well-controlled chronic diseases according to income level. Data from the 2008 to 2014 Korea National Health and Nutrition Examination Survey, conducted by using a stratified, multistage, probability-cluster sampling method, were used. Systolic blood pressure (SBP) inversely correlated with income level (P < 0.001). Diastolic blood pressure (DBP) showed no relationship. In the low-income group, the prevalence rates of hypertension and diabetes mellitus (DM) were highest but the proportion of patients with well-controlled chronic disease and the SBPs of the patients with hypertension showed a decreasing trend. In the high-income group, the proportions of patients with well-controlled DM and chronic kidney disease were higher than those in other groups. After adjusting for age, body mass index, SBP, DBP, HbA1c level, and serum creatinine level, income level significantly affected the prevalence of chronic diseases (for income, β=0.184; 95% confidence interval, 1.105–1.042). The daily sodium intake estimated by using spot urine samples was higher in the low- and low-to-mid-income groups. The prevalence of not using essential medical service for chronic disease was highest in the low- and low-to-mid-income groups for economic reasons. In the low- and low-to-mid-income groups, the prevalence of chronic disease was higher and the proportion of patients with well-controlled chronic disease was lower than in the other groups.
Keywords: blood pressure, chronic disease, diabetes mellitus, hypertension, income, renal insufficiency
1. Introduction
Owing to the increase in the aging population, the prevalence of chronic diseases is also increasing. In particular, according to the 2014 Senior Survey Report published by the Korean Ministry of Health and Welfare about 90% of the elderly population had a chronic disease, 56.7% had hypertension, and 22.6% had diabetes mellitus (DM).[1] Despite the increasing prevalence of hypertension, the percentages of undiagnosed patients were 20% among all the patients with hypertension and 15% among those with DM in South Korea. Thus, chronic diseases have been poorly managed.[2] Especially hypertension and DM are important risk factors of cardiovascular and cerebrovascular diseases, but people usually would not know the importance of management owing to the fact that only few symptoms could affect the management of chronic diseases. Currently, the point of view that the socioeconomic aspect should be investigated as the factor that could affect the management of chronic diseases is becoming more popular. Previous studies analyzed the relationship between socioeconomic levels and hypertension, and showed that socioeconomic levels could be an important risk factor for the development of hypertension in lower-income populations.[3,4] In cases where access to medical services was affected by economic factors, cardiovascular mortality could be high.[5] Dietary habits that could trigger hypertension were associated with income level.[6] Many reports have investigated whether socioeconomic level influences the incidence of chronic disease. However, only one study investigated the management of chronic diseases according to income level, but the study was not conducted in the general population but in patients with type 1 DM.[7] In addition, for the management of chronic diseases, low-sodium diets should be imposed, as elevated sodium intake increases blood pressure,[8] blood glucose level,[9] and proteinuria in patients with chronic kidney disease (CKD).[10] Therefore, high salt intake could hinder the management of chronic diseases. Many previous research studies confirmed that dietary habits are affected by economic status.[11] Thus, we investigated the prevalence and management of chronic diseases, and salt intake according to income level.
2. Materials and methods
2.1. Study design and settings
This study analyzed data from the 2008 to 2014 Korea National Health and Nutrition Examination Survey (KNHANES) in South Korea. A stratified, multistage, probability-cluster sampling method was used. The detailed design of the KNHANES is described in a previously published study.[12] The survey was conducted by the Korean Ministry of Health and Welfare. It was composed of 3 sections, namely, a health survey, health consultations, and a nutrition survey. The health questionnaire was used to survey income levels and cases of hypertension and diabetes. Health consultations were used to survey blood pressure (BP), weight, waist circumference, body mass index (BMI), and levels of HbA1c, total cholesterol, serum creatinine, urinary protein, urinary sodium, and urinary creatinine. The survey data included information regarding the use of the necessary health care service, job type, and educational level. Blood pressure, body weight, height, and levels of urinary sodium, total cholesterol, HbA1c, and urinary creatinine were measured.
We divided the participants into 4 groups according to monthly average income in the household equivalence scale
(low-, low-to-mid, mid-to-high, and high-income groups). The income threshold groups were determined based on the quartiles of monthly average income in the household equivalence scale. Sodium intake was calculated by using the Tanaka equation.[13] First, we estimated the salt intake per day by using spot urine samples. Second, sodium intake was measured by using the 24-hour recall method.
2.2. Definitions used in study
High BP was defined as taking antihypertensive medication or a systolic blood pressure (SBP) of ≥140 mm Hg or a diastolic blood pressure (DBP) of ≥90 mm Hg. DM was defined as a fasting plasma glucose level of ≥126 mg/dL or taking antidiabetic medication. CKD was defined as an estimated glomerular filtration rate (eGFR) of <60 mL/(min·1.73 m2), according to the definition in the Modification of Diet in Renal Disease (MDRD) study.
eGFR was calculated by using the 4-variable MDRD formula as follows: eGFR (mL/min·1.73 m2) = 175 × serum creatinine level (mg/dL)−1.154 × age−0.203 × 0.742 (if female).[14] The definition of the metabolic syndrome was based on the diagnosis category[15] for the presence of ≥3 of the following: ① abdominal obesity of >90 cm in men or >80 cm in women; ② triglyceride level of ≥150 mg/dL or taking medication; ③ high-density lipoprotein cholesterol level of <40 mg/dL in men or <50 mg/dL in women, or taking medication; ④ SBP ≥ 130 mm Hg and/or DBP ≥ 85 mm Hg or taking medication; ⑤ fasting plasma glucose level of ≥100 mg/dL or taking medication. Thresholds for abdominal obesity were defined based on the Asian population.[16]
In the patients with hypertension, well-controlled BP was defined as BP controlled to <140/90 mm Hg according to the Joint National Committee (JNC) 8th Directive. In the patients with DM, controlled blood glucose level was defined as an HbA1c level of <7%. Well-controlled CKD was defined as negative proteinuria in a dip-stick test. Adequate sodium intake was defined as <2000 mg/d according to the recommendation of the World Health Organization (WHO).
Educational level was expressed as a number as follows: 1: completed up to elementary school graduation, 2: completed middle school, 3: completed high school, and 4: college level or higher.
A total of 45,303 survey respondents were investigated, and those who did not report spot urine sodium level and economic status were excluded from the study. At result, 30,107 persons were included in the study.
The KNHANES was approved by the institutional review board of the Korea Centers for Disease Control and Prevention (KCDC), and all the participants provided written informed consent. The study protocol conformed to the ethics guidelines of the 1975 Declaration of Helsinki and was approved by the institutional review board of the KCDC (No. 2013-12EXP-03-5C).
2.3. Statistical analysis
For continuous variables, to determine the subjects’ characteristics, a descriptive analysis was performed. Categorical variables were analyzed by using the χ2 test to determine the correlation between the different variables. We divided the subjects into 4 groups according to income level to allow comparisons of the variables. To determine differences in characteristics between the groups, we used the analysis of variance. In the regression analysis of the incidence of chronic diseases, we adjusted for confounding factors, including age, BMI, SBP, DBP, HbA1c level, and serum creatinine level. Significance was defined when the P value was <0.05. R version 3.1.1. (R Foundation for Statistical Computing, Vienna, Austria) was used for the statistical analysis.
3. Results
3.1. Participant characteristics
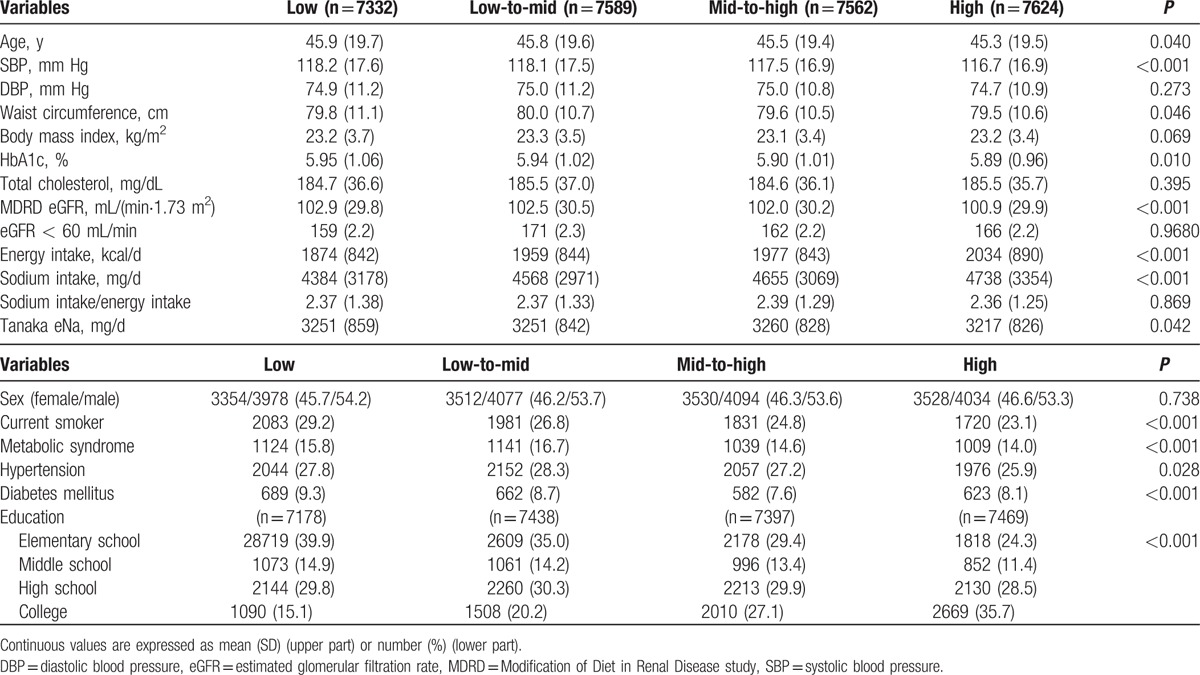
The mean age of all the participants was 45.6 ± 19.5 years. The male to female ratio was 46.2:53.8. The ratio of the educational levels (1:2:3:4) was 32.0:13.5:29.7:24.7. Age showed significant differences among the income groups. SBP inversely correlated with income level (P < 0.001), but DBP did not. Smoking rate was highest in the low-income group. The prevalence of metabolic syndrome was highest in the low-to-mid-income group. The prevalence rates of hypertension and diabetes were highest in the low-to-mid-income group. In the low- and low-to-mid income groups, HbA1c level was higher than in the other groups. The prevalence of CKD showed no significant differences among the 4 groups. The high-income group showed lower estimated sodium intake by Tanaka's formula than the other 3 groups (Table 1).
Table 1.
Baseline characteristics (n = 48,832,940; weighted).
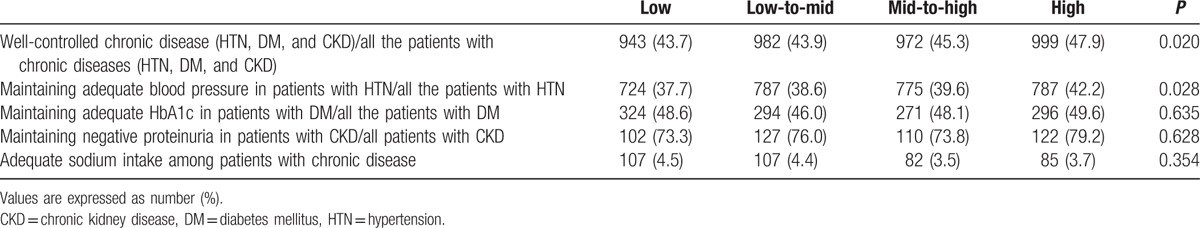
3.2. Chronic disease management status according to income level
In the low-income group, the proportion of patients with well-controlled chronic diseases and BPs among those with hypertension were low. The proportion of patients with well-controlled diabetes among those with DM showed no significant differences among the income groups (Table 2). In the low-income group, the proportion of patients with well-controlled CKD was lower than in the other groups.
Table 2.
The prevalence of maintaining adequate blood pressure in hypertension, glucose level in diabetes mellitus, and proteinuria in chronic kidney disease (n = 48,832,940; weighted).
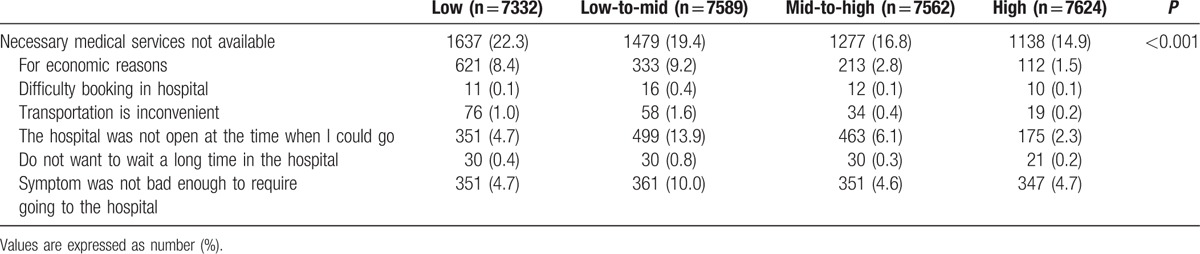
3.3. Use of essential medical services according to income level
Essential medical services were used less frequently by those with low and low-to-mid income levels, usually for economic reasons. The subjects in the low- and mid-to-low-income groups could not use the necessary medical services because of economic reasons, inconvenient transportation, and lack of time to meet with physician (Table 3).
Table 3.
The prevalence of not using the necessary medical services and its causes: survey results (n = 48,832,940; weighted).
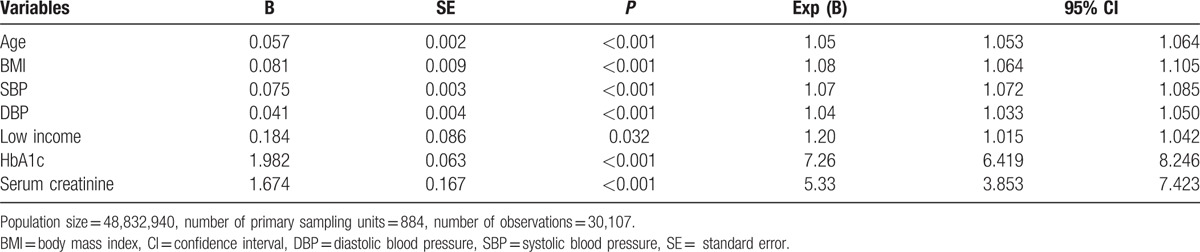
3.4. Prevalence factors of chronic diseases
The logistic regression analysis for the prevalence of chronic disease was performed after adjustment for age, BMI, SBP, DBP, HbA1c level, and serum creatinine level. Income level significantly affected the prevalence of chronic diseases (for income: odds ratio [OR], 0.184; 95% confidence interval [CI], 1.015–1.042) (Table 4).
Table 4.
Results of the logistic regression analysis of the prevalence of chronic diseases (hypertension, diabetes mellitus, and chronic kidney disease).
4. Discussion
An increasing trend was observed in the prevalence of chronic diseases such as hypertension and DM in the low-income group. The low social class groups (lower educational and income levels) showed higher prevalence of chronic diseases and lower awareness of ill-health status.[17] One study reported about the prevalence of chronic disease depending on educational and income levels, and showed that the prevalence of chronic diseases was increased in the patients with low educational and income levels.[18] In addition, awareness of damaged health was better and prevalence of chronic diseases was higher in the high-income groups, who were earning >1.5 million won, than in the low-income group, who were earning <0.5 million won.[17] The effects of the differences in educational and income levels on health status were reported to be due to differences in health care, purchasing power, and access to health-care services.[18,19] In this study, the prevalence of chronic diseases such as hypertension and DM was higher in the low-income groups, except for CKD. Owing to the definition of CKD in this study, its prevalence did not significantly differ among the groups. The prevalence of metabolic syndrome, which affected the occurrence of cardiovascular diseases, was high in the low-income group. These results were the same as those obtained in previous studies that reported that the degree of difference observed between educational levels was in accordance with the income level. We can conclude that the lower-income group showed lower educational levels.
For the low-income group, we thought that the management of chronic diseases was not good, but no previous research has been conducted on the management of chronic diseases according to income level. In this study, the proportion of patients with well-controlled chronic diseases such as hypertension, DM, and CKD based on the presence of proteinuria was determined and was found to be higher in the high-income group. In case of DM, no significant difference in the proportion of patients with well-controlled DM was observed among the groups. However, the mean HbA1c level was higher in the low- and low-to-mid-income groups. Regardless of the national insurance services in South Korea, medical expenses are relatively too high for low-income earners to afford. Medical expenses include the cost of transportation to go to the hospital, the cost of drugs, the cost laboratory tests, and the consultation fee. According to Statistics Korea, the lower the income, the greater the increase in the medical expenses. Hence, the low-income group could not use the essential health services because of financial problems.
Perhaps for this reason, the low-income group showed poor control of their chronic illnesses. Accessibility of the health system was rather difficult for low-income earners, which may be due to the difference in the level of care they expect to receive. Thus, in future study, we would like to examine differences in the extent of use of medical systems in accordance with income level.
In South Korea, the government has been providing basic pension to old-aged people since 2014. For people aged >65 years with <70% income grade, the government provides 250,000 won. The characteristics of this pension were akin to the basis of the distribution. In 2015, the government found through an investigation that the lower the income, the greater the priority of using the pension for medical purposes. Therefore, the basic income was guaranteed in the lower-income group. With this, the management of chronic diseases in the lower-income group may improve.
The common belief is that educating the low-income group about dietary practices such as low-sodium intake is difficult. Thus, this group is easily thought to have higher sodium intakes than the high-income group. However, this study showed that the higher-income group had higher sodium and energy intakes than the low-income group. The number of meals consumed per day did not significantly differ but eating out was more frequent in the high-income group. Perhaps, the high frequency of eating out caused the higher sodium intake. The higher-income group showed high energy and sodium intakes, but the estimated daily sodium intake measured in spot urine samples was higher in the low- and low-to-mid income groups. The difference in sodium intake among the groups might be due to the difference in measurement method used. However, it is important to note that none of the groups met the 2000-mg/d recommendation of the WHO. In a future study, 24-hour urine collection will be needed for this reason. We thought that when people are diagnosed with chronic disease, they would reduce their sodium intake. However, most of the subjects in this study had high salt intakes irrespective of income level.
This study has some limitations. First, this was a cross-sectional study; hence, recall bias was a strong confounder. As chronic diseases could negatively affect people's economic status, which between the 2 is the cause or effect is unclear. Second, without the use of 24-hour urine collection, the single urine sodium test and the method for estimating salt intake could be erroneous. Third, we could not use the official definition of CKD because only a single blood test was performed. Thus, the prevalence of CKD might have been shown to be lower than the actual prevalence. Fourth, we used the term prevalence but a gap could exist between the prevalence reported in this study and that in the real world. Fifth, because of the relatively long duration of the survey, the analyzed economic status could differ from the actual status.
5. Conclusion
In the low- and low-to-mid-income groups, the prevalence of chronic diseases was higher and the proportion of patients with well-controlled chronic diseases was lower than in the other groups.
Footnotes
Abbreviations: BMI = body mass index, CKD = chronic kidney disease, DBP = diastolic blood pressure, DM = diabetes mellitus, SBP = systolic blood pressure.
Funding/support: This work was supported by a 2012 Inje University research grant (20120745).
The authors have no conflicts of interest to disclose.
References
- 1.2014 Senior Survey Report published by the Korean Ministry of Health and Welfare. Research Report. Seoul: Ministry of Health and Welfare, 2014. [Google Scholar]
- 2.2014 Korea National Health and Nutrition Examination Survey (KNHANES). Available at: http://www.cdc.go.kr/CDC/contents/CdcKrContentView.jsp?cid=60599&menuIds=HOME001-MNU1130-MNU1639-MNU1640-MNU1645 Accessed June 2016. [Google Scholar]
- 3.Batty GD, Shipley MJ, Gunnell D, et al. Height, wealth, and health: an overview with new data from three longitudinal studies. Econ Hum Biol 2009; 7:137–152. [DOI] [PubMed] [Google Scholar]
- 4.Marmot M, Feeney A. General explanations for social inequalities in health. IARC Sci Publ 1997; 138:207–228. [PubMed] [Google Scholar]
- 5.Kaplan GA, Keil JE. Socioeconomic factors and cardiovascular disease: socioeconomic factors and cardiovascular disease: a review of the literature. Circulation 1993; 88:1973–1998. [DOI] [PubMed] [Google Scholar]
- 6.Jeongok R, Hyuna K. A study on the knowledge, dietary behavior related to sodium, attitudes towards a low-salt diet of adults in the Jeonbuk area. Korean J Hum Ecol 2013; 22:693–705. [Google Scholar]
- 7.Rawshani A, Svensson AM, Rosengren A, et al. Impact of socioeconomic status on cardiovascular disease and mortality in 24,947 individuals with type 1 diabetes. Diabetes Care 2015; 38:1518–1527. [DOI] [PubMed] [Google Scholar]
- 8.INTERSALT. Intersalt: an international study of electrolyte excretion and blood pressure. Results for 24 hour urinary sodium and potassium excretion. Intersalt Cooperative Research Group. Br Med J 1988; 297:319–328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hu G1, Jousilahti P, Peltonen M, et al. Urinary sodium and potassium excretion and the risk of type 2 diabetes: a prospective study in Finland. Diabetologia 2005; 48:1477–1483. [DOI] [PubMed] [Google Scholar]
- 10.Swift PA, Markandu ND, Sagnella GA, et al. Modest salt reduction reduces blood pressure and urine protein excretion in black hypertensives: a randomized control trial. Hypertension 2005; 46:308–312. [DOI] [PubMed] [Google Scholar]
- 11.Koichi M, Yixuan S, Setsuko T, et al. Socioeconomic status is significantly associated with dietary salt intakes and blood pressure in Japanese workers (J-HOPE Study). Int J Environ Res Public Health 2013; 10:980–993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sanghui K, Yuna K, Myoung-jin J, et al. Data resource profile: the Korea National Health and Nutrition Examination Survey (KNHANES). Int J Epidemiol 2014; 43:69–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tanaka T, Okamura T, Miura K, et al. A simple method to estimate populational 24-h urinary sodium and potassium excretion using a casual urine specimen. J Hum Hypertens 2002; 16:97–103. [DOI] [PubMed] [Google Scholar]
- 14.Levey AS, Coresh J, Greene T, et al. Expressing the Modification of Diet in Renal Disease Study equation for estimating glomerular filtration rate with standardized serum creatinine values. Clin Chem 2007; 53:766–772. [DOI] [PubMed] [Google Scholar]
- 15.Alberti K, Eckel RH, Grundy SM, et al. Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation 2009; 120:1640–1645. [DOI] [PubMed] [Google Scholar]
- 16.Hara K, Matsushita Y, Horikoshi M, et al. A proposal for the cutoff point of waist circumference for the diagnosis of metabolic syndrome in the Japanese population. Diabetes Care 2006; 29:1123–1124. [DOI] [PubMed] [Google Scholar]
- 17.Mia S. The relationship of social class and health behaviors with morbidity in Korea. Korean J Prev Med 2002; 35:57–64. [Google Scholar]
- 18.Hye Ryun K. The relationship of socioeconomic position and health behaviors with morbidity in Seoul, Korea. KIHASA 2005; 25:3–35. [Google Scholar]
- 19.Seung Gon K. Socioeconomic status and chronic diseases prevalence inequalities in late life. Korean Assoc Health Med Soc 2004; 12:155–177. [Google Scholar]


