Abstract
Recently, 2 new anthropometric indices, the A Body Shape Index (ABSI) and Body Roundness Index (BRI), have been developed. Our study was to compare the associations between different anthropometric indices, including ABSI, BRI, body mass index (BMI), waist circumference (WC) and waist-to-hip ratio (WHR), and hypertension in a rural population of northeast China.
This cross-sectional study was conducted in the rural areas of northeast China from January 2012 to August 2013 using a multistage, stratified random cluster-sampling scheme. All eligible permanent residents aged ≥35 years (a total of 14,016 individuals) in each village were invited to participate in the study. A final sample size of 11,345 (5253 males and 6092 females) were included in this study.
All the 5 anthropometric measures were positively correlated with hypertension. The prevalence of hypertension increased across quartiles for ABSI, BMI, BRI, WC, and WHR. Multivariable logistic regression analysis of the presence of hypertension for the highest quartile versus the lowest quartile of each anthropometric measure, showed that BRI had the largest values of ORs (OR: 3.49, 95% CI: 2.86–4.21 in men; OR: 3.06, 95% CI: 2.56–3.67 in women) and ABSI had the smallest ORs (OR: 1.30, 95% CI: 1.06–1.58 in men; OR: 1.19, 95% CI: 1.04–1.34 in women). BRI had the highest AROCs for hypertension (AROC: 0.65, 95% CI: 0.64–0.67 for men and AROC: 0.68, 95% CI: 0.67–0.70 for women), while ABSI had the lowest AROCs for hypertension (AROC: 0.60, 95% CI: 0.58–0.61 for men and AROC: 0.59, 95% CI: 0.58–0.61 for women).
Our results showed that ABSI, BMI, BRI, WC, and WHR were all associated with hypertension. ABSI showed the weakest association with hypertension, while BRI showed potential for use as an alternative obesity measure in assessment of hypertension.
Keywords: a body shape index, body mass index, body roundness index, hypertension, waist circumference, waist-to-hip ratio
1. Introduction
Hypertension is a universal disease with increasing prevalence worldwide, in both adults and children, in both urban and rural areas.[1–3] Hypertension is a known risk factor for cardiovascular disease (CVD), such as ischemic heart disease, stroke, or hypertensive heart disease, and is the leading cause of morbidity and mortality worldwide.[4] It is therefore essential to identify the risk factors associated with hypertension and adopt primary preventions. The relationships between obesity and hypertension have been well established ,[5] and body mass index (BMI) has been the most commonly used anthropometric measure for defining obesity recommended by WHO.[6] Subsequently, studies found that BMI could not reflect abdominal fat and therefore waist circumference (WC) and waist-to-hip ratio (WHR) were suggested as an indicator of central adiposity for its relevance with fat distribution.[7–9] However, people have gradually found that neither BMI, WC, nor WHR could discriminate fat and muscle mass and therefore left pregnant women, athletes, and body builders categorized incorrectly.[10,11] Consistently, both cross-sectional and longitudinal studies also confirmed that BMI, WC, and WHR had similar degree of association with the prevalence of hypertension.[12–14]
These inconsistent results might be due to their single index rather than considering the combined information of general obesity and abdominal general. Previous study demonstrated that hypertension might not be only affected by the amount of body fat but also distribution.[15] Various studies have reported that subjects with more abdominal fat will have higher risks of CVD and other related diseases including hypertension, type 2 diabetes, and high cholesterol.[15,16] BMI could just reflect the amount of body fat. As the previous study[15] demonstrated, although WC and WHR could indicate relative abdominal shape more clearly, they still provided limited information on the fat distribution.
Recently, a new anthropometric measure, named a body shape index (ABSI), has been developed by Krakauer and Krakauer.[17] ABSI was calculated using the following equation:
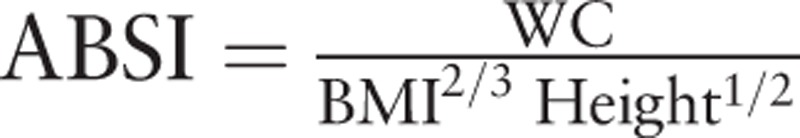 |
. They standardized WC for BMI and height with the scaling exponents 2/3 and 1/2 in the denominator, which made ABSI uncorrelated to BMI. This lack of correlation is important for improving predictive ability that cannot be explained by BMI. Krakauer and Krakauer[17] found ABSI to be more associated with mortality hazards than BMI and WC did in the American population sample they studied. And this was further confirmed by their subsequent study.[18] In 2013, Thomas et al[19] developed another new anthropometric index called the body roundness index (BRI) that was based on height and WC, and it could predict the percentage of body fat and therefore evaluate health status. BRI was calculated using the following equation:
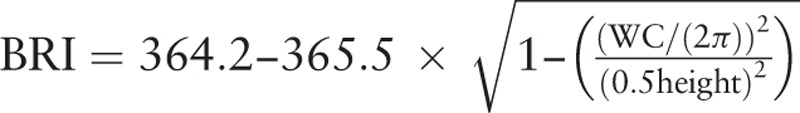 |
. The values of BRI closer to 1 were related to leaner individuals, and larger values were associated with rounder individuals. However, it is unknown so far whether ABSI and BRI are associated with the presence of hypertension in rural Chinese population.
In order to assess the capacity of ABSI and BRI to identify hypertension and to evaluate whether ABSI and BRI are more strongly associated with hypertension than traditional anthropometric indices of obesity, we compared the associations of ABSI, BMI, BRI, WC, and WHR with hypertension in this population-based cross-sectional study conducted in the rural areas of northeast China.
2. Methods
2.1. Study population
This study was conducted in Liaoning Province, located in Northeast China. From January 2012 to August 2013, a representative sample of individuals aged ≥35 years was selected to participate in assessing the associations between 2 new body indices (ABSI and BRI) and hypertension in a rural population of northeast China. The study adopted a multistage, stratified random cluster-sampling scheme. In the first stage, 3 counties (Dawa, Zhangwu, and Liaoyang County) were selected randomly from the rural areas of Liaoning province, and in the second stage, 1 town was randomly selected from each of the 3 counties. In the third stage, 26 rural villages in 3 towns were randomly selected for inclusion in the study. All eligible permanent residents aged ≥35 years (a total of 14,016 individuals) in each village were invited to participate in the study. Of those, 11,956 participants (i.e., response rate of 85.3%) agreed to participate and completed the present study. Only participants with a complete set of data regarding the variables analyzed in the present study were included, for a final sample size of 11,345 (5253 males and 6092 females), as shown in Fig. 1. The study protocol was approved by the Ethics Committee of China Medical University, Shenyang, China, and all procedures were performed in accordance with good ethical standards. Written consents were obtained from all participants after they had been informed of the objectives, benefits, medical items, and confidentiality of personal information. If the participants were illiterate, written informed consent was obtained from their proxies.
Figure 1.
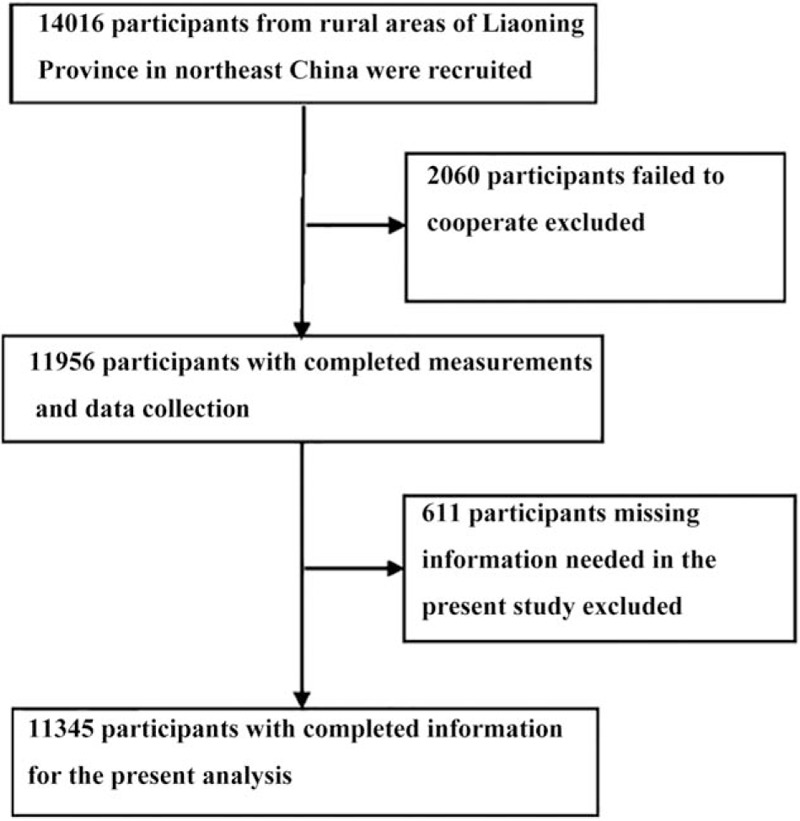
Flow chart of study design.
2.2. Lifestyle factors
Our survey was performed by cardiologists and trained nurses during a single visit at a clinic in each village. Information on covariates, such as age, gender, and lifestyle, was collected using a standard questionnaire by face-to-face interview. Prior to conducting the survey, all eligible investigators were invited to attend a training session that covered topics including the purpose of the study, how to administer the questionnaire, the standard method of measurement, the importance of standardization, and study procedures. After completing the training session, each potential investigator was required to obtain a perfect score (≥85 points) on a training test if they were to participate in the study. Additionally, the investigators received further instructions and support during periods of data collection. Each study participant's ethnicity was classified as either Han or other (which included ethnic minorities such as Mongol and Manchu). Family income was classified as ≤5000, 5000 to 20,000, and >20,000 CNY/y. Educational level was categorized as low (no schooling, incomplete primary education, and primary education), middle (3 or 4 years of secondary education), and high (college and university education). Physical activity was classified into 3 groups using a detailed description of the methods presented elsewhere.[20] Briefly, participants were asked with a question: “which type do you think your occupational physical activity belongs to?” Occupational physical activity was grouped into 3 categories: low was defined as participants who reported light levels of occupational physical activity, such as the elderly, cripple, and paralysis; moderate was defined as participants who reported moderate occupational physical activity, such as driver and office worker; high was defined as participants who reported high level of occupational physical activity, such as manual agricultural activities and miner. Self-reported salt intake per month was obtained from the questionnaire. All study participants were asked whether or not they were currently smokers or drinkers.
2.3. Blood pressure measurements and definition of hypertension
Based on the recommended AHA's protocol,[21] blood pressure (BP) was measured 3 times at 2-min intervals after at least 5 min of rest using a standardized automatic electronic sphygmomanometer (HEM-907; Omron, Kyoto, Japan). The participants were advised to avoid caffeinated beverages and exercise for at least 30 minutes before the measurement. During the measurement, each participant was seated with their tested arm supported at the level of the heart. The mean of 3 BP measurements was calculated and used in all analyses. According to the JNC-7 report,[22] hypertension was defined as systolic blood pressure (SBP) ≥140 mm Hg and/or diastolic blood pressure (DBP) ≥90 mm Hg and/or use of antihypertensive medications.
2.4. Anthropometric measurements
Weight and height were measured to the nearest 0.1 kg and 0.1 cm, respectively, with the participant in light-weight clothing and without shoes. WC was measured at the umbilicus using a nonelastic tape (to the nearest 0.1 cm), and with the participant in a standing posture at the end of a normal expiration. BMI was calculated as the individual's weight in kilograms divided by the square of the height in meters. WHR was calculated by dividing WC by hip circumference. ABSI was calculated using the following formula[17]:
 |
. BRI was calculated using the formula[19]:
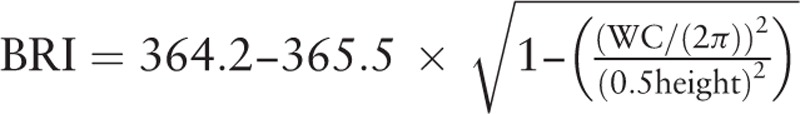 |
.
2.5. Serum analysis
A fasting blood sample was collected from each participant in the morning after at least 12 hours of fasting. Blood samples were obtained from an antecubital vein and collected in vacutainer tubes containing EDTA. Values for fasting plasma glucose (FPG), total cholesterol (TC), low-density lipoprotein cholesterol (LDL-C), high-density lipoprotein cholesterol (HDL-C), triglyceride (TG), and other routine blood biochemical indexes were obtained using an autoanalyzer. All laboratory equipment was calibrated, and blinded duplicate samples were used.
2.6. Statistical analyses
The general characteristics of hypertensive and normotensive in both sexes were compared using the parametric test for continuous variables and χ2 for categorical variables. Spearman rank test was used to examine the relationship between hypertension and each anthropometric measure (ABSI, BMI, BRI, WC, and WHR). Area under the receiver-operating characteristic curve (AROC) and 95% confidence intervals (CIs) were used to assess the discriminatory power of each anthropometric measure to assess the risk for hypertension. For BMI, BRI, and WHR, quartiles were created and the prevalence of hypertension in each quartile was calculated. Previous study indicated that ABSI was strongly correlated with age and sex.[17] So ABSI was classified into 4 age groups (age 35–44, age 45–54, age 55–64, and age ≥65), and then the quartiles of ABSI were determined within each age group for males and females separately.[17] To calculate the prevalence of hypertension in each ABSI quartile, subjects within the same ABSI quartile were merged. For WC, the quartiles were classified by sex and the prevalence of hypertension in each quartile was calculated. Multivariable logistic regression analysis was used to calculate the odds ratios (ORs) and their 95% CIs for the presence of hypertension, with adjustments for age, ethnicity, family income, education, physical activity, salt intake, smoking and alcohol status, FPG, and serum lipid. The lowest quartile served as a reference. All the statistical analyses were performed using SPSS Statistics for Windows, Version 17.0 (SPSS, Chicago, IL). P values <0.05 were considered statistically significant. Furthermore, tests for 2 AROCs were further analyzed using PASS 14 (http://www.ncss.com), using the algorithm suggested by Hanley and McNeil.[23]
3. Results
A total of 11,345 subjects (5253 males and 6092 females) aged ≥35 years participated in the study. Table 1 shows clinical and demographic characteristics of the study population according to sex and BP. Participants with hypertension were older than normotensive in both sexes (P < 0.001). Overall, the educational levels and family incomes in the rural areas were low. Participants with hypertension were less active in physical activity than normotensive. Additionally, the vast majority of participants were Han ethnicity. Men were more likely to be smokers or drinkers (P < 0.05, by χ2 test). Participants with hypertension were more likely to take more salt and have higher values of TC, TG, LDL-c, and FPG than normotensive. In terms of anthropometric measures, the mean levels of ABSI, BMI, BRI, WC, and WHR were significantly higher among hypertensive.
Table 1.
Baseline characteristics of study population.
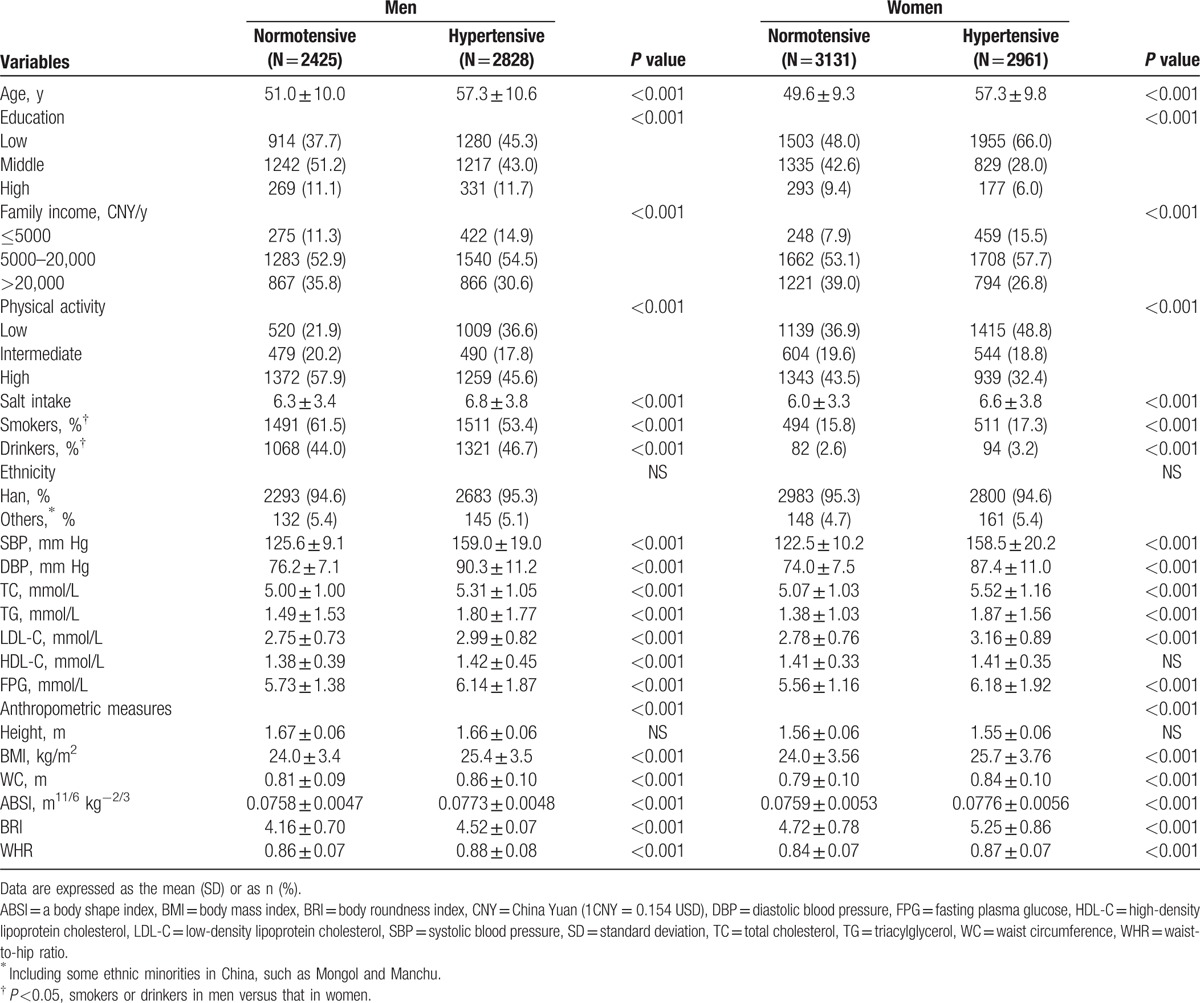
Table 2 shows the results of Spearman rank test of anthropometric measures (ABSI, BMI, BRI, WC, and WHR) and hypertension. BRI showed the highest Spearman correlation coefficient for hypertension (r = 0.264 for men and r = 0.317 for women, both P < 0.001), whereas ABSI showed the lowest (r = 0.163 for men and r = 0.161 for women, both P < 0.001) in both sexes.
Table 2.
Spearman rank test of anthropometric measures (ABSI, BMI, BRI, WC, and WHR) and hypertension.
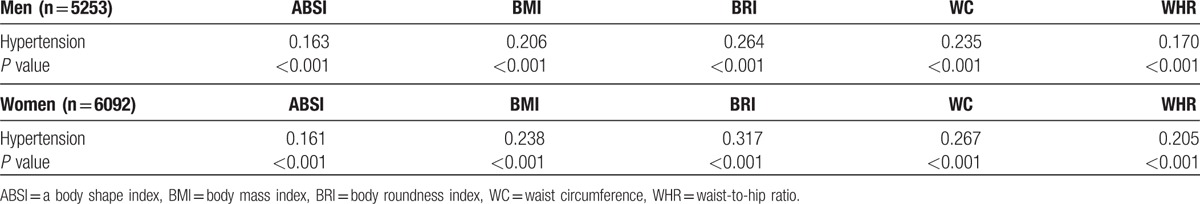
Table 3 shows the prevalence of hypertension in quartiles of ABSI, BRI, BMI, WC, and WHR. We classified the subjects in our study into quartiles according to each anthropometric index. The prevalence of hypertension increased per quartile for all 4 anthropometric indices (first quartile vs fourth quartile) in both sexes: ABSI 47.3% versus 61.7% for men, ABSI 44.4% versus 49.5% for women; BMI 40.1% versus 65.6% for men, BMI 33.9% versus 64.1% for women; BRI 39.4% versus 74.9% for men, BRI 25.8% versus 65.8% for women; WC 39.0% versus 69.0% for men, WC 33.6% versus 65.7% for women; WHR 42.4% versus 65.0% for men, WHR 35.0% versus 65.6% for women (all P < 0.05).
Table 3.
Prevalence of hypertension in quartiles of ABSI, BRI, BMI, WC, and WHR.
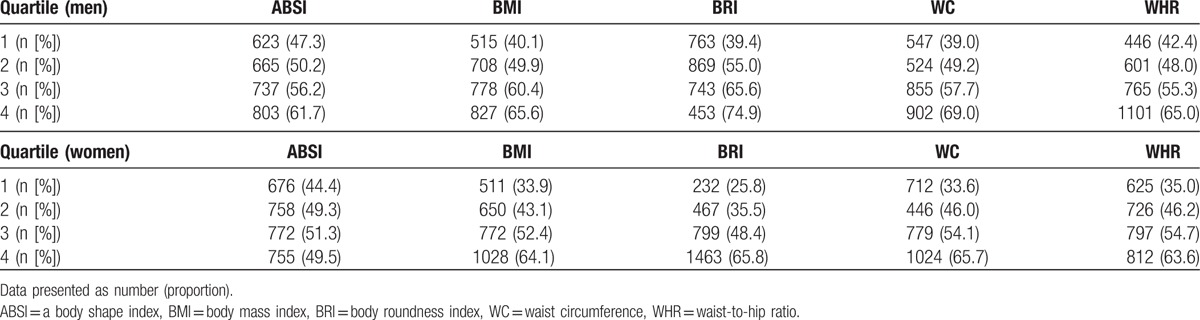
Table 4 shows the multivariable-adjusted ORs (95% CIs) of the presence of hypertension for the highest quartile versus the lowest quartile of each anthropometric index after adjustment for age, ethnicity, family income, education, physical activity, salt intake, smoking and alcohol status, FPG, and serum lipid. BRI had the largest ORs (95% CI) for hypertension in both sexes (OR: 3.49, 95% CI: 2.86–4.21 in men; OR: 3.06, 95% CI: 2.56–3.67 in women). While ABSI had the smallest ORs for hypertension (OR: 1.30, 95% CI: 1.06–1.58 in men; OR: 1.19, 95% CI: 1.04–1.34 in women).
Table 4.
Odds ratios (95% CIs) of the presence of hypertension for each anthropometric index∗.
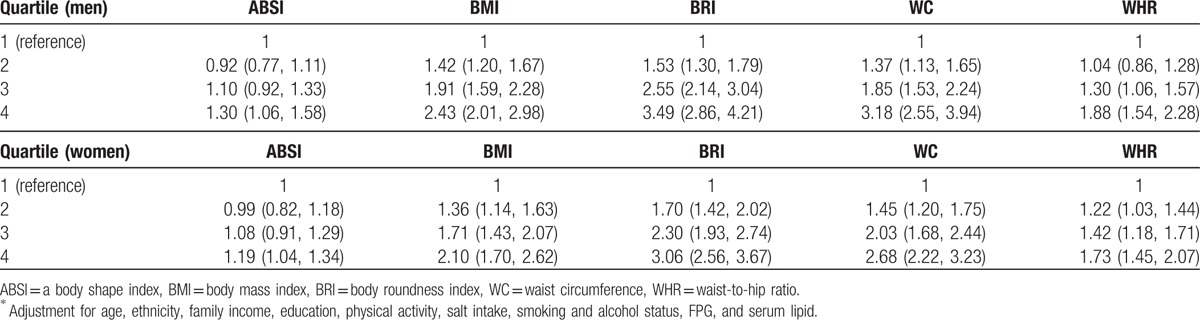
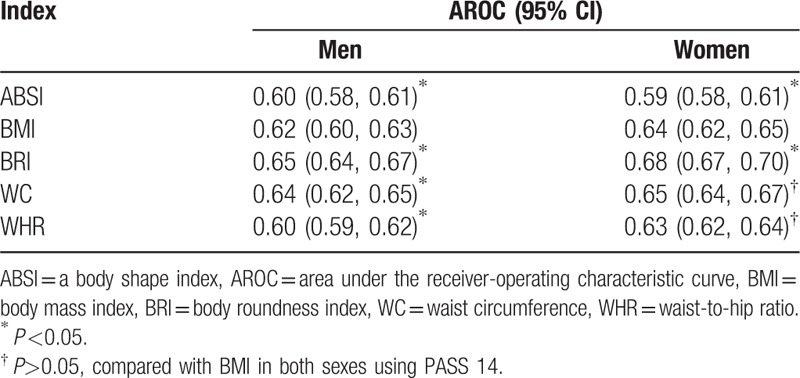
Table 5 shows the AROCs (and 95% CIs) of hypertension in relation to anthropometric indices. BRI showed the highest AROC values for hypertension in both men (AROC: 0.65, 95% CI: 0.64–0.67) and women (AROC: 0.68, 95% CI: 0.67–0.70). While ABSI had the lowest AROCs for hypertension in both sex categories (AROC: 0.60, 95% CI: 0.58–0.61 for men; AROC: 0.59, 95% CI: 0.58–0.61 for women). Two AROCs were further tested using PASS 14. We found AROCBRI was significantly larger than AROCBMI and AROCABSI was significantly smaller than AROCBMI in both sexes.
Table 5.
The AROCs and 95% CIs of each anthropometric measure for the presence of hypertension in both genders.
4. Discussion
In this cross-sectional study, we compared the associations between 5 anthropometric indices (ABSI, BMI, BRI, WC, and WHR) and hypertension in a rural population of northeast China. Overall, in our study, all anthropometric indices could identify the presence of hypertension because they all had AROC >0.5 and ORs > 1 (P < 0.05). Furthermore, our study also indicated that ABSI showed the weakest association with hypertension, while BRI showed potential for use as an alternative obesity measure in assessment of hypertension.
There were well-established evidences that obesity was closely associated with increased risk for hypertension.[5] Furthermore, it was higher accumulation of visceral adipose tissue rather than heavier body weight that was more associated with cardiovascular disease (CVD) such as hypertension.[24,25] And Lear et al[26] found that even within normal BMI, people with larger WC were at higher risk of CVD and premature death. Therefore, several experts suggested that WC should be used for both children and adults when identifying potential CVD.[27,28] Our study based on the rural populations consistently showed that WC was superior to BMI when accessing the presence of hypertension in both sexes.
Krakauer and Krakauer[17] claimed that the ABSI was more related to visceral than peripheral fat, and was more associated with mortality hazards than BMI and WC did. However, subsequent studies had completely inconsistent conclusions about whether ABSI was superior for identifying diseases to BMI or WC. Some cohort studies found that ABSI outperformed BMI and WC in predicting mortality.[17,18] On the contrary, He and Chen[29] did not found the superiority of ABSI in identifying diabetes mellitus in the Chinese population compared with BMI or WC. Another study found that ABSI could not determine the presence of CVD and CVD risk factors after adjustment for sex, age, and smoking.[30] In a study of Portuguese adolescents, BMI showed the expected positive association with BP but the ABSI showed a negative association with BP.[31] Furthermore, ABSI did not appear to represent an improvement for assessing the association of abdominal obesity with risk of 4 obesity-related cancers.[32] In our study, we found that ABSI was the weakest predictor for identifying the presence of hypertension and was not superior to BMI or WC. The underlying mechanism of these conflicting results was not clear. However, ethnic and gender differences might be a possible explanation for the contrasting findings. Cheung[33] therefore suggested that the same structure but different coefficients for men and women should be adopted when applying ABSI as a public health and clinical indicator in the Indonesian population. And finally, the equations used in the above study to calculate the ABSI for men and women were modified as follows:
 |
for men and
 |
for women. Additionally, age should also be taken into consideration when applying ABSI in different populations. As suggested by Xu et al,[34] the appropriate scaling exponents for standardizing waist circumference for BMI and height in Chinese adolescents were 0.45 and 0.55, respectively. Further studies should focus on applicability of ABSI in different populations and especially the cut-points for diagnosing obesity.
BRI was developed in 2013 and there were few data available for it up to now. As Thomas et al[19] demonstrated, BRI could improve predictions of % body fat and % visceral adipose tissue (VAT) compared with the traditional metrics of BMI or WC. It was a pity that they did not show how BRI related to mortality and other diseases such as CVD or diabetes. One study[30] applying BRI which found that BRI as a novel anthropometric index to identify CVD showed similar instead of superior capabilities to BMI and WC. Our results indicated that BRI had a similar predictive ability for identifying the presence of hypertension to BMI and WC. The possible reason was that BRI could predict % body fat and % VAT, which was more associated with CVD such as hypertension than heavier body weight.[24,25] Though BRI could improve upon predictive accuracy of some CVD such as hypertension, it was not as simple as BMI or WC to apply in clinical settings or daily life. In the future, we might deliver it in an easily usable software platform that could better inform and guide treatment to improve obesity related health, as Thomas et al[19] proposed.
4.1. Limitations
First, as ABSI was first developed to predict mortality hazard in a follow-up study, we assessed its association with hypertension in cross-sectional study, which may be the main reason that ABSI did not show superior usefulness to identify subjects with hypertension. In future studies, the longitudinal relation between the 2 new anthropometric indices and hypertension should be studied. Second, our study was conducted based on rural populations in northeast China, whose unique lifestyle could influence both body shape and metabolic indices. Third, neither internal nor external validation was done in our manuscript. Additional studies evaluating the internal and external validation are clearly needed and the potential solutions can be found in previous study.[35]
5. Conclusions
In the present study, we demonstrated that all the 5 anthropometric indices could determine the presence of hypertension. ABSI showed the weakest association with hypertension, while BRI showed potential for use as an alternative obesity measure in assessment of hypertension. BRI may be used as a practical criterion or supplement to BMI and WC for identifying adiposity-related health risks in clinical assessments. We looked forward to more studies in other global populations that could further demonstrate the advantages and disadvantages of these new anthropometric indices.
Acknowledgments
The authors thank all the researchers and participants for participating in this study.
Footnotes
Abbreviations: ABSI = a body shape index, AROC = area under the receiver-operating characteristic curve, BMI = body mass index, BRI = body roundness index, CI = confidence interval, CNY = China Yuan (1CNY = 0.154 USD), CVD = cardiovascular disease, DBP = diastolic blood pressure, FPG = fasting plasma glucose, HDL-C = high-density lipoprotein cholesterol, LDL-C = low-density lipoprotein cholesterol, OR = odds ratio, SBP = systolic blood pressure, SD = standard deviation, TC = total cholesterol, TG = triacylglycerol, VAT = visceral adipose tissue, WC = waist circumference, WHR = waist-to-hip ratio.
This work was supported by the National Science and Technology Support Program of China (Grant No. 2012BAJ18B02), Natural Science Foundation of Liaoning Province (Grant No. 2013021090), and Liaoning Research Center for Translational Medicine of Cardiovascular Disease (Grant No. 2014225017).
The authors have no conflicts of interest to disclose.
References
- 1.Poirier P, Giles TD, Bray GA, et al. Obesity and cardiovascular disease: pathophysiology, evaluation, and effect of weight loss: an update of the 1997 American Heart Association Scientific Statement on Obesity and Heart Disease from the Obesity Committee of the Council on Nutrition, Physical Activity, and Metabolism. Circulation 2006; 113:898–918. [DOI] [PubMed] [Google Scholar]
- 2.Klein S, Burke LE, Bray GA, et al. Clinical implications of obesity with specific focus on cardiovascular disease: a statement for professionals from the American Heart Association Council on Nutrition, Physical Activity, and Metabolism: endorsed by the American College of Cardiology Foundation. Circulation 2004; 110:2952–2967. [DOI] [PubMed] [Google Scholar]
- 3.Li Z, Guo X, Zheng L, et al. Grim status of hypertension in rural China: results from Northeast China Rural Cardiovascular Health Study 2013. J Am Soc Hypertens 2015; 9:358–364. [DOI] [PubMed] [Google Scholar]
- 4.Ezzati M, Lopez AD, Rodgers A, et al. Selected major risk factors and global and regional burden of disease. Lancet 2002; 360:1347–1360. [DOI] [PubMed] [Google Scholar]
- 5.Lu Y, Hajifathalian K, Ezzati M, et al. Global Burden of Metabolic Risk Factors for Chronic Diseases Collaboration (BMI Mediated Effects). Metabolic mediators of the effects of body-mass index, overweight, and obesity on coronary heart disease and stroke: a pooled analysis of 97 prospective cohorts with 1.8 million participants. Lancet 2014; 383:970–983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Physical status: the use, interpretation of anthropometry. Report of a WHO Expert Committee. World Health Organ Tech Rep Ser 1995; 854:1–452. [PubMed] [Google Scholar]
- 7.Daniels SR, Khoury PR, Morrison JA. Utility of different measures of body fat distribution in children and adolescents. Am J Epidemiol 2000; 152:1179–1184. [DOI] [PubMed] [Google Scholar]
- 8.Li C, Ford ES, McGuire LC, et al. Increasing trends in waist circumference and abdominal obesity among US adults. Obesity 2007; 15:216–224. [DOI] [PubMed] [Google Scholar]
- 9.Esmaillzadeh A, Mirmiran P, Azizi F. Waist-to-hip ratio is a better screening measure for cardiovascular risk factors than other anthropometric indicators in Tehranian adult men. Int J Obes Relat Metab Disord 2004; 28:1325–1332. [DOI] [PubMed] [Google Scholar]
- 10.Heymsfield SB, Scherzer R, Pietrobelli A, et al. Body mass index as a phenotypic expression of adiposity: quantitative contribution of muscularity in a population-based sample. Int J Obes 2009; 33:1363–1373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Muller MJ, Lagerpusch M, Enderle J, et al. Beyond the body mass index: tracking body composition in the pathogenesis of obesity and the metabolic syndrome. Obes Rev 2012; 13 (suppl 2):6–13. [DOI] [PubMed] [Google Scholar]
- 12.Deng WW, Wang J, Liu MM, et al. Body mass index compared with abdominal obesity indicators in relation to prehypertension and hypertension in adults: the CHPSNE study. Am J Hypertens 2013; 26:58–67. [DOI] [PubMed] [Google Scholar]
- 13.Lin S, Cheng TO, Liu X, et al. Impact of dysglycemia, body mass index, and waist-to-hip ratio on the prevalence of systemic hypertension in a lean Chinese population. Am J Cardiol 2006; 97:839–842. [DOI] [PubMed] [Google Scholar]
- 14.Nyamdorj R, Qiao Q, Soderberg S, et al. Comparison of body mass index with waist circumference, waist-to-hip ratio, and waist-to-stature ratio as a predictor of hypertension incidence in Mauritius. J Hypertens 2008; 26:866–870. [DOI] [PubMed] [Google Scholar]
- 15.Wang S, Liu Y, Li F, et al. A novel quantitative body shape score for detecting association between obesity and hypertension in China. BMC Public Health 2015; 15:7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wells JC, Treleaven P, Cole TJ. BMI compared with 3-dimensional body shape: the UK National Sizing Survey. Am J Clin Nutr 2007; 85:419–425. [DOI] [PubMed] [Google Scholar]
- 17.Krakauer NY, Krakauer JC. A new body shape index predicts mortality hazard independently of body mass index. PLoS One 2012; 7:e39504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Krakauer NY, Krakauer JC. Dynamic association of mortality hazard with body shape. PLoS One 2014; 9:e88793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Thomas DM, Bredlau C, Bosy-Westphal A, et al. Relationships between body roundness with body fat and visceral adipose tissue emerging from a new geometrical model. Obesity 2013; 21:2264–2271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hu G, Tuomilehto J, Silventoinen K, et al. Joint effects of physical activity, body mass index, waist circumference and waist-to-hip ratio with the risk of cardiovascular disease among middle-aged Finnish men and women. Eur Heart J Dec 2004; 25:2212–2219. [DOI] [PubMed] [Google Scholar]
- 21.Pickering TG, Hall JE, Appel LJ, et al. Recommendations for blood pressure measurement in humans and experimental animals: part 1: blood pressure measurement in humans: a statement for professionals from the Subcommittee of Professional and Public Education of the American Heart Association Council on High Blood Pressure Research. Circulation 2005; 111:697–716. [DOI] [PubMed] [Google Scholar]
- 22.Chobanian AV, Bakris GL, Black HR, et al. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA 2003; 289:2560–2572. [DOI] [PubMed] [Google Scholar]
- 23.Hanley JA, McNeil BJ. A method of comparing the areas under receiver operating characteristic curves derived from the same cases. Radiology 1983; 148:839–843. [DOI] [PubMed] [Google Scholar]
- 24.Gus M, Fuchs SC, Moreira LB, et al. Association between different measurements of obesity and the incidence of hypertension. Am J Hypertens 2004; 17:50–53. [DOI] [PubMed] [Google Scholar]
- 25.Wang TD, Goto S, Bhatt DL, et al. Ethnic differences in the relationships of anthropometric measures to metabolic risk factors in Asian patients at risk of atherothrombosis: results from the REduction of Atherothrombosis for Continued Health (REACH) Registry. Metabolism 2010; 59:400–408. [DOI] [PubMed] [Google Scholar]
- 26.Lear SA, James PT, Ko GT, et al. Appropriateness of waist circumference and waist-to-hip ratio cutoffs for different ethnic groups. Eur J Clin Nutr 2010; 64:42–61. [DOI] [PubMed] [Google Scholar]
- 27.Lee JM, Davis MM, Woolford SJ, et al. Waist circumference percentile thresholds for identifying adolescents with insulin resistance in clinical practice. Pediatr Diabetes 2009; 10:336–342. [DOI] [PubMed] [Google Scholar]
- 28.Freedman DS, Serdula MK, Srinivasan SR, et al. Relation of circumferences and skinfold thicknesses to lipid and insulin concentrations in children and adolescents: the Bogalusa Heart Study. Am J Clin Nutr 1999; 69:308–317. [DOI] [PubMed] [Google Scholar]
- 29.He S, Chen X. Could the new body shape index predict the new onset of diabetes mellitus in the Chinese population? PLoS One 2013; 8:e50573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Maessen MF, Eijsvogels TM, Verheggen RJ, et al. Entering a new era of body indices: the feasibility of a body shape index and body roundness index to identify cardiovascular health status. PLoS One 2014; 9:e107212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Duncan MJ, Mota J, Vale S, et al. Associations between body mass index, waist circumference and body shape index with resting blood pressure in Portuguese adolescents. Ann Hum Biol 2013; 40:163–167. [DOI] [PubMed] [Google Scholar]
- 32.Kabat GC, Xue X, Kamensky V, et al. Risk of breast, endometrial, colorectal, and renal cancers in postmenopausal women in association with a body shape index and other anthropometric measures. Cancer Causes Control 2015; 26:219–229. [DOI] [PubMed] [Google Scholar]
- 33.Cheung YB. “A Body Shape Index” in middle-age and older Indonesian population: scaling exponents and association with incident hypertension. PLoS One 2014; 9:e85421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Xu Y, Yan W, Cheung YB. Body shape indices and cardiometabolic risk in adolescents. Ann Hum Biol 2015; 42:70–75. [DOI] [PubMed] [Google Scholar]
- 35.Zhan Y, Holtfreter B, Meisel P, et al. Prediction of periodontal disease: modelling and validation in different general German populations. J Clin Periodontol 2014; 41:224–231. [DOI] [PubMed] [Google Scholar]


