Abstract
BACKGROUND:
Verification of the correct placement of the endotracheal tube (ETT) has been one of the most challenging issues of airway management in the field of emergency medicine. Early detection of oesophagal intubation through a reliable method is important for emergency physicians.
AIM:
The aim of this study was to assess the diagnostic accuracy of tracheal rapid ultrasound exam (TRUE) to assess endotracheal tube misplacement during emergency intubation.
METHODS:
This was an observational prospective study performed in the emergency department of the major tertiary referral hospital in the city. We included a consecutive selection of 100 patients. TRUE was performed for all these patients, and subsequently, quantitative waveform capnography was done. The later test is considered as the gold standard.
RESULTS:
From our total 100 eligible patients, 93 (93%) participants had positive TRUE results (tracheal intubation) and 7 (7%) patients have negative TRUE results (esophageal intubation). Quantitative waveform capnography report of all 93 (100%) patients who had positive TRUE was positive (appropriate tracheal placement). Sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV) of TRUE for detecting appropriate tracheal placement of ETT were 98.9% (95% CI, 93.3% to 99.8%), 100% (95% CI, 51.6% to 100%), 100% (95% CI, 95.1% to 100%) and 85.7% (95% CI, 42% to 99.2%) respectively.
CONCLUSIONS:
Performing TRUE is convenient and feasible in many emergency departments and pre-hospital settings. We would recommend emergency units explore the possibility of using TRUE as a method in the assessment of proper ETT placement.
Keywords: trachea, ultrasonography, intubation, emergencies
Introduction
Verification of the correct placement of the endotracheal tube (ETT) has been one of the most challenging issues of airway management in the field of emergency medicine [1]. Oesophagal intubation could result in a devastating outcome; however, if diagnosed properly and instantly, there will be no sequela for the patient [2]. It has been reported that under emergency circumstances there is a chance of 6 to 16% of unintentional oesophagal intubation [3, 4]. Then, early detection of this problem through a reliable method is important for emergency physicians.
There are different methods for evaluation of tracheal placement of the ETT such as direct visualization of the endotracheal tube passing, auscultation of the lung and epigastrium, chest radiography, qualitative capnography (colorimetric carbon dioxide detector), quantitative capnography (continuous waveform capnography), checking the missing in the endotracheal tube, negative pressure devices, direct fiber optic visualization of the trachea, esophageal detector tool and ultrasonography (US) [5-17]. All of these methods have their pros and cons [18]. However, based on the 2010 American Heart Association (AHA) Guidelines for Cardiopulmonary Resuscitation (CPR) and Emergency Cardiovascular Care (ECC), quantitative waveform capnography is the gold standard for confirming correct endotracheal tube placement [19].
US are a real-time, fast and promising procedure for the evaluation of the ETT position [20]. Ultrasonography is a widely accessible tool in the emergency setting. It has broad availability, is suitable for carrying, fairly economical, and has good safety profiles; in other words, it is portable and has no radiation risk.
There are direct and indirect methods for the assessment of the ETT position through ultrasonography. In the direct procedure, the sonographer evaluates the entire upper airway system from the cricothyroid membrane to the suprasternal notch. In the indirect method, a convex transducer is placed in the suprasternal notch window using the tracheal rapid ultrasound exam (TRUE) technique. Another indirect method, the trans-cricothyroid membrane US technique, is performed with a linear transducer applied on the cricothyroid membrane [21, 22].
In this study, we evaluated the accuracy of TRUE which was performed by emergency physicians for the evaluation and verification of the position of the ETT in the emergency department.
Method
Study Design
This was an observational, prospective, single-center study, conducted between July 2013 and August 2014. All patients were recruited from the emergency department of the major tertiary referral hospital of the city. The approvals of the Institutional Review Board, as well as the Ethics Committee of the affiliated medical university, were obtained before the start of the study.
Training in Ultrasonography
Researchers were emergency physicians who underwent a three weeks training consisting of one week of theoretical training about the performance of TRUE and two weeks’ practice and since their prior training has a substantial impact on the results and the applicability of this study. Once the training was complete, the participating emergency physicians and residents were able to conduct ultrasonography with accuracy.
Study Population
While the researchers where available in the emergency department, the participants were prospectively registered and evaluated. Inclusion criteria were those patients above eighteen years who underwent emergency intubation due to various reasons including impending respiratory failure, multiple trauma, cardiac arrest, shock, etc. Those patients who were excluded from the study had neck trauma, neck tumours or history of neck operation, or tracheostomy. We randomly sampled among patients who met the inclusion and exclusion criteria for the purpose of our study. Although we sampled from the pool of existing patients for convenience, randomization was not influenced by the work schedule of physicians or time of day.
Study Protocol
The flow chart of the study is demonstrated in Figure 1. All the emergency intubations on the selected patients were performed by a single emergency physician. Confirmation of ETT placement was performed by another emergency physician right after the intubation through auscultation, pulse oximetry and quantitate waveform capnography. Immediately after intubation, TRUE was executed by another emergency physician. All the three emergency physicians were the investigators of the projects.
Figure 1.
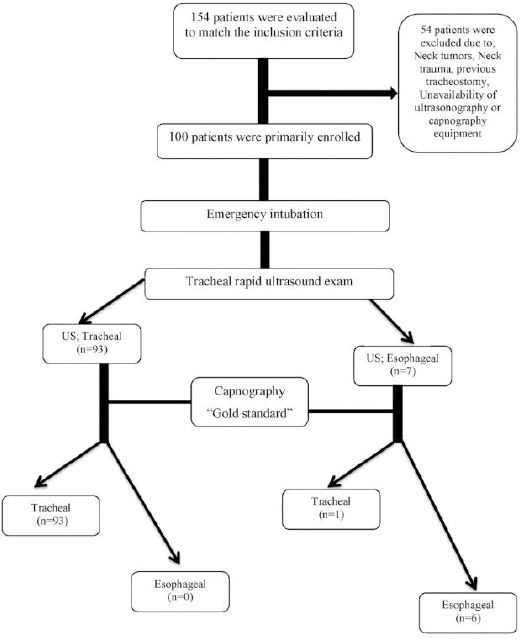
The flowchart of the study
The third emergency physician, the sonographer who was a well-trained resident of emergency medicine that has had enough experience to get involved in this study, was neither aware of the primary capnography and auscultation findings nor involved in the resuscitation process. A curtain had visually separated the sonographer to follow the conduct of a blinded study. Also, he wore earplugs during the ultrasonography to avoid any effects resulting from verbal interactions among staff being involved in the resuscitation. Also, nothing related to the patients’ history and physical examination were revealed to him. All data were gathered and registered by one of the nursing staff. According to the study algorithm, he was asked to report his rapid ultrasonography only in brief which was “in trachea” or “in oesophagus”. Therefore, there was no descriptive report of ultrasonography by the sonographer.
Tracheal Rapid Ultrasound Exam
Participants underwent TRUE according to a standardised protocol, taking into consideration that ultrasonography can detect the placement of ETT, and confirm the correct tracheal placement, in emergency settings. Real-time imaging of the trachea was performed for each subject by an experienced emergency physician, using a Sono Ace X4 ultrasound machine (Sono Ace X4, SAMSUNG MEDISON Co., Seoul, South Korea) with a 3.5-MHz convex transducer probe. The ultrasonography probe was placed transversely on the anterior part of the neck just superior to the suprasternal notch (Figure 2). A hyper-echoic air-mucosa interface with a reverberation artefact posteriorly (comet-tail artefact) was indicative of the position of the trachea. Accordingly, the detected ETT position was explained as below.
Figure 2.

For tracheal rapid ultrasonography exam (TRUE), the transducer should be placed superior to the suprasternal notch
The gold standard for the confirmation of the tracheal intubation was the positive result of quantitative waveform capnography. A positive result from this test was set as the detection of appropriate exhaled carbon dioxide, i.e. more than four mm Hg after at least 5 breaths, with a typical CO2 waveform.
The goal of this study was to compare the results of TRUE in comparison with the results of quantitative waveform capnography, as the standard, for the verification of the ETT position in emergency situations. We aimed to explore the possibility of replacing the current gold standard (i.e. capnography) with the US.
Statistical Analysis
All data analyses were performed using Statistical Package for the Social Sciences (SPSS Inc., Chicago, Illinois, USA) version 17. Data are reported as the mean ± standard deviation (SD) or proportions, as appropriate. Waveform capnography report was considered the gold standard and the diagnostic accuracy of TRUE for determining the tracheal placement of the ETT was evaluated accordingly. Hence, the accuracy, sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV) of TRUE were calculated.
Results
Of the 154 patients who were evaluated primarily, a total of 100 patients were registered through convince sampling method (Figure 1). Their demographics and clinical characteristics were listed in Table 1. In our study, we set the quantitative waveform capnography report as the standard of care for diagnosing tracheal intubation. So the results of other alternative tests were compared to the standard. A total of 100 intubations were performed during the study period.
Table 1.
The demographic and medical characteristics of intubated patients in the ED
| Tracheal intubation (n=94) | Esophageal intubation (n=6) | |
|---|---|---|
| Age, years | 64.4 ± 11.9 | 65.4 ± 12.4 |
| Female gender | 34 (36.1) | 1 (16.6) |
| BMI | 23.6 ± 4.2 | 24 ± 3.8 |
| Intubation indication | ||
| Cardiac disease | 35 (37.2) | 2 (33.3) |
| Neurologic disease | 9 (9.5) | 0 (0) |
| Pulmonary disease | 24 (25.5) | 1 (16.6) |
| Trauma | 16 (17) | 2 (33.3) |
| Sepsis | 9 (9.5) | 1 (16.6) |
| Other | 1 (1.01) | 0 (0) |
| Medical history | ||
| Hypertension | 30 (31.9) | 3 (50) |
| Diabetes mellitus | 25 (26.5) | 4 (66.6) |
| Coronary artery disease | 19 (20.2) | 2 (33.3) |
| Neurologic disease | 11 (11.7) | 1 (16.6) |
| Pulmonary disease | 14 (14.8) | 1 (16.6) |
| Malignancy | 19 (20.0) | 0 (0) |
Abbreviations: ED, emergency department; BMI, body mass index. Data are presented as Mean ± SD or No. (%).
From our total 100 patients, 93 (93%) individuals had positive TRUE results (tracheal intubation), and seven (7%) patients had negative TRUE results (oesophagal intubation). Waveform capnography reports of all 93 (100%) patients who had positive TRUE tests showed successful tracheal intubation, and none of the capnography reports indicated oesophagal intubation in this group (Table 2).
Table 2.
TRUE reports of patients underwent intubation in ED and subsequent quantitative waveform capnography outcomes
| Ultrasonography | Quantitative waveform capnography | ||
|---|---|---|---|
| (+) Tracheal intubation | (-) Esophageal intubation | Total | |
| (+) Tracheal intubation | 93 | 0 | 93 |
| (-) Esophageal intubation | 1 | 6 | 7 |
| Total | 94 | 6 | 100 |
Abbreviation: TRUE, tracheal rapid ultrasound exam; ED, emergency department.
Seven (7%) patients had negative TRUE results (esophageal intubation) and out of which, 6 (85.7%) patients had negative waveform capnography reports, which was in favor of esophageal intubation, and the rest of them (n = 1; 14.3%) had undergone appropriate tracheal intubation based on positive waveform capnography.
Table 3 indicates the sensitivity and specificity of TRUE for detection of successful tracheal intubation in emergency department which were 98.9% (CI 95%: 93.3 – 99.8) and 100% (CI 95%: 51.6 – 100), respectively. All 93 patients (positive TRUE) were positive regarding capnography which indicates 100% (CI 95%: 95.1 – 100) as PPV (Positive Predictive value) while six subjects out of 7 (negative TRUE) patients were negative according to capnography report which indicates 85.7% (CI 95%: 42 – 99.2) as NPV (Negative predictive value). Finally, the accuracy of TRUE for detection of appropriate tracheal intubation in our study was 99%.
Table 3.
Predictive value of TRUE for confirmation of tracheal intubation in ED
| Value | 95% CI | ||
|---|---|---|---|
| Lower limit | Upper limit | ||
| Sensitivity, % | 98.9 | 93.3 | 99.8 |
| Specificity, % | 100 | 51.6 | 100 |
| Positive predictive value, % | 100 | 95.1 | 100 |
| Negative predictive value, % | 85.7 | 42 | 99.2 |
Abbreviation: TRUE, tracheal rapid ultrasound exam; ED, emergency department; CI, confidence interval.
Discussion
The aim of this observational study was to evaluate the accuracy of TRUE for confirmation of a successful tracheal intubation in the ED. Our results showed high sensitivity and specificity and, therefore, this method of tracheal ultrasonography can be a reliable way to verify the place of ETT.
Assessment of the ETT position, both by confirmatory techniques and clinical evaluation, was highlighted in the latest AHA guidelines for CPR and ECC [19]. Nevertheless, the disadvantages of each method created challenges for emergency physicians. Previous studies proved that emergency physicians should not count only on their clinical assessment for verification of place of ETT, as it is unreliable and could endanger patient life [11].
Ultrasonography is a non-invasive, real-time and repeatable diagnostic modality [5]. It is also one of the most popular tools in hospitals and EDs. The usefulness of ultrasonography in various aspects of patients with critical situations (assessment of hemodynamics, cardiac function, etc.) has been well proven before [23, 24].
Several previous studies showed promising results regarding the use of US. Chun et al. [25] stated the results of their study on 30 patients using a portable, hand-held, ultrasound machine in which the sonographic recordings of the chest wall visceral-parietal pleural interface were analysed. They declared that thoracic ultrasonography might be another method that could be used to verify proper ETT placement. Application of US to detect ETT placement was published in 2006 [26]. In this study, the performance of the US sliding lung sign as a predictor of ETT placement was assessed, and the authors proved that this method of US could be an accurate way for confirmation of ETT placement in a cadaver model. Although these procedures of US are different from TRUE; however, its findings were remarkable.
In a pilot study of 33 patients, Werner et al. [27] revealed that two emergency physicians experienced in the US were able to detect placement of endotracheal tubes precisely during intubation in select patients in the operating room, with sensitivity or specificity that reached 100% for each physician. A cadaver model survey in 2007 indicated a 97 sensitivity and 100 specificities of the dynamic trans cricothyroid US by emergency physicians to detect appropriate placement of ETT in the trachea [22]. In another study, of 40 patients who underwent elective surgery, the US by emergency physicians revealed sensitivity and specificity of 100% and 97%, respectively for detecting oesophagal intubation [18]. Another study of 112 patients by Chou et al. [28] indicated the sensitivity, specificity, positive predictive value, and negative predictive value of 98.9%, 94.1%, 98.9% and 94.1%, respectively.
In addition to these findings in adult patients, a 2009 study of thirty healthy children with normal airways requiring tracheal intubation revealed that the US could be useful and appropriate in paediatric settings [29]. Another study about children with larger sample size and higher analysis power indicated that bedside US could be used to precisely and rapidly define the presence of the ETT within the trachea in paediatric patients [30].
A recent randomised clinical trial on 150 patients showed a promising result of 100% for both sensitivity and specificity [31]. In spite of the fact that double blinding was performed, the most important disadvantage of this study is that the ultrasonographer had done the US and no emergency physician had been involved. Although emergency physicians could be trained to perform the US, the US assessment outcome maybe more reliable and accurate if an ultrasonographer performs the procedure due to having a greater experience (i.e. higher frequency of performing the procedure) and more in-depth academic training. Additionally, the trial has been conducted in non-emergency surgical patients. Even though the results could be generalised to real ED situations, it is clear that in some cases, the medical condition of ED patients is far more critical and hazardous than elective individuals in the operating room.
The advantages of TRUE would be more prominent in special environments, such as in remote, pre-hospital settings, in rural hospitals and medical centres, or during aerospace, medical transports. In all these situations auscultation may be compromised by background noise, and capnography or X-ray equipment may not be available.
Limitations and Advantages
All our included patients were selected randomly from various types of patients referred to the emergency ward. Although we sampled from the pool of existing patients for convenience, randomization was not influenced by the work schedule of physicians or time of day. We acknowledge the underlying cause of respiratory arrest may impact the performance and outcome of tracheal intubation. However, the effect maybe limited due to a random selection of subjects from the pool of patients. Future trials can look into the matter by including more patients categorised into different groups based on the primary aetiology of the respiratory arrest.
A strength of our study was involvement of emergency physicians in all aspects of the study including intubation, capnography and US assessment. To reach accurate and reliable results promptly, it was crucial for all procedures and medical assessments to be performed by three independent emergency physicians, and not by anesthesiologists or ultrasonographers (Rudraraju & Eisen, 2009; Salem, 2001). The number of medical physicians involved in the procedure may suggest issues of applicability to emergency rooms where fewer physicians are available, or training in ultrasonography or trained ultrasonographers is limited or non-existent.
Mastering the technique may prove beneficial for emergency physicians because they are the first line of evaluation and treatment of critical patients 10 and it is not always feasible or economic to involve other specialists during resuscitation, intubation and medical care of severely ill patients in the setting of ED.
A tracheal rapid ultrasound exam may be an accurate, feasible, and reproducible method to confirm the appropriate placement of the ETT in emergency conditions. Thus, TRUE could be considered an alternative for primary verification method after intubation by emergency physicians. Nonetheless, future prospective, double-blind, randomised clinical trials in this area can help us better understand merits and issues of TRUE, overcome our study limitations and establish the necessary groundwork for a possible recommendation to use the US as the primary verification method after intubation in emergency rooms.
Acknowledgments
The authors are going to thanks, all patients and hospital staffs to participate in this study.
Footnotes
Funding: This research did not receive any financial support.
Competing Interests: The authors have declared that no competing interests exist.
References
- 1.Sagarin MJ, Barton ED, Chng YM, Walls RM. National Emergency Airway Registry. Airway management by US and Canadian emergency medicine residents:a multicenter analysis of more than 6,000 endotracheal intubation attempts. Ann Emerg Med. 2005;46(4):328–336. doi: 10.1016/j.annemergmed.2005.01.009. https://doi.org/10.1016/j.annemergmed.2005.01.009 PMid:16187466. [DOI] [PubMed] [Google Scholar]
- 2.Dittrich KC. Delayed recognition of oesophagal intubation. CJEM. 2002;4(1):41–44. doi: 10.1017/s1481803500006047. https://doi.org/10.1017/S1481803500006047 PMid:17637147. [DOI] [PubMed] [Google Scholar]
- 3.Mort TC. Unplanned tracheal extubation outside the operating room:a quality improvement audit of hemodynamic and tracheal airway complications associated with emergency tracheal reintubation. Anesth Analg. 1998;86(6):1171–1176. doi: 10.1097/00000539-199806000-00006. PMid:9620498. [DOI] [PubMed] [Google Scholar]
- 4.Schwartz DE, Matthay MA, Cohen NH. Death and other complications of emergency airway management in critically ill adults. A prospective investigation of 297 tracheal intubations. Anesthesiology. 1995;82(2):367–376. doi: 10.1097/00000542-199502000-00007. https://doi.org/10.1097/00000542-199502000-00007 PMid:7856895. [DOI] [PubMed] [Google Scholar]
- 5.Cardoso MM, Banner MJ, Melker RJ, Bjoraker DG. Portable devices used to detect endotracheal intubation during emergency situations:a review. Crit Care Med. 1998;26(5):957–964. doi: 10.1097/00003246-199805000-00036. https://doi.org/10.1097/00003246-199805000-00036 PMid:9590328. [DOI] [PubMed] [Google Scholar]
- 6.Foutch RG, Magelssen MD, MacMillan JG. The esophageal detector device:a rapid and accurate method for assessing tracheal versus esophageal intubation in a porcine model. Ann Emerg Med. 1992;21(9):1073–1076. doi: 10.1016/s0196-0644(05)80647-x. https://doi.org/10.1016/S0196-0644(05)80647-X. [DOI] [PubMed] [Google Scholar]
- 7.Grmec S. Comparison of three different methods to confirm tracheal tube placement in emergency intubation. Intensive Care Med. 2002;28(6):701–704. doi: 10.1007/s00134-002-1290-x. https://doi.org/10.1007/s00134-002-1290-x PMid:12107674. [DOI] [PubMed] [Google Scholar]
- 8.Kerrey BT, Geis GL, Quinn AM, Hornung RW, Ruddy RM. A prospective comparison of diaphragmatic ultrasound and chest radiography to determine endotracheal tube position in a pediatric emergency department. Pediatrics. 2009;123(6):e1039–1044. doi: 10.1542/peds.2008-2828. https://doi.org/10.1542/peds.2008-2828 PMid:19414520. [DOI] [PubMed] [Google Scholar]
- 9.Li J. A prospective multicenter trial testing the SCOTI device for confirmation of endotracheal tube placement. J Emerg Med. 2001;20(3):231–239. doi: 10.1016/s0736-4679(00)00317-6. https://doi.org/10.1016/S0736-4679(00)00317-6. [DOI] [PubMed] [Google Scholar]
- 10.O’Connor CJ, Mansy H, Balk RA, Tuman KJ, Sandler RH. Identification of endotracheal tube malpositions using computerized analysis of breath sounds via electronic stethoscopes. Anesth Analg. 2005;101(3):735–739. doi: 10.1213/01.ane.0000167068.71601.e4. https://doi.org/10.1213/01.ane.0000167068.71601.e4 PMid:16115984 . [DOI] [PubMed] [Google Scholar]
- 11.Takeda T, Tanigawa K, Tanaka H, Hayashi Y, Goto E, Tanaka K. The assessment of three methods to verify tracheal tube placement in the emergency setting. Resuscitation. 2003;56(2):153–157. doi: 10.1016/s0300-9572(02)00345-3. https://doi.org/10.1016/S0300-9572(02)00345-3. [DOI] [PubMed] [Google Scholar]
- 12.Tanigawa K, Takeda T, Goto E, Tanaka K. Accuracy and reliability of the self-inflating bulb to verify tracheal intubation in out-of-hospital cardiac arrest patients. Anesthesiology. 2000;93(6):1432–1436. doi: 10.1097/00000542-200012000-00015. https://doi.org/10.1097/00000542-200012000-00015 PMid:11149438. [DOI] [PubMed] [Google Scholar]
- 13.Baratto L, Park SY, Hatami N, et al. 18F-FDG silicon photomultiplier PET/CT:A pilot study comparing semi-quantitative measurements with standard PET/CT. PLoS One. 2017;12(6):e0178936. doi: 10.1371/journal.pone.0178936. https://doi.org/10.1371/journal.pone.0178936 PMid:28582472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wu F, Jamali M, Hatami N, Sonni I, Baratto L, Guo HH. 99mTc-MDP scintigraphy vs. 18F-NaF PET/CT for detection of skeletal metastases. Journal of Nuclear Medicine. 2016;57(supplement 2):599–599. [Google Scholar]
- 15.Sonni I, Park S, Baratto L, Hatami N, Davidzon G. Initial Experience with a SiPM-based PET/CT Scanner:Influence of Acquisition Time on Image Quality. Journal of Nuclear Medicine. 2017;58(supplement 1):1369–1369. doi: 10.1186/s40658-018-0207-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Baratto L, Park S, Hatami N, Davidzon G, Srinivas S. SiPM PET/CT vs. Standard PET/CT:A Pilot Study Comparing Semi-Quantitative Measurements in Normal Tissues and Lesions. Journal of Nuclear Medicine. 2017;58(supplement 1):432–432. [Google Scholar]
- 17.Park S, Hatami N, Rutledge O, Koglin N, Loo B, Fan A. Pilot study of 18F-FSPG vs. 18F-FDG PET imaging for response assessment in cancer. Journal of Nuclear Medicine. 2017;58(supplement 1):118–118. [Google Scholar]
- 18.Milling TJ, Jones M, Khan T, et al. Transtracheal 2-d ultrasound for identification of esophageal intubation. J Emerg Med. 2007;32(4):409–414. doi: 10.1016/j.jemermed.2006.08.022. https://doi.org/10.1016/j.jemermed.2006.08.022 PMid:17499696. [DOI] [PubMed] [Google Scholar]
- 19.Neumar RW, Otto CW, Link MS, et al. Part 8:adult advanced cardiovascular life support:2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2010;122(18 Suppl 3):S729–767. doi: 10.1161/CIRCULATIONAHA.110.970988. https://doi.org/10.1161/CIRCULATIONAHA.110.970988 PMid:20956224. [DOI] [PubMed] [Google Scholar]
- 20.Abbasi S, Farsi D, Zare MA, Hajimohammadi M, Rezai M. Direct ultrasound methods:a confirmatory technique for proper endotracheal intubation in the emergency department. Eur J Emerg Med. 2015;22(1):10–16. doi: 10.1097/MEJ.0000000000000108. https://doi.org/10.1097/MEJ.0000000000000108 PMid:24441884. [DOI] [PubMed] [Google Scholar]
- 21.Adi O, Chuan TW, Rishya M. A feasibility study on bedside upper airway ultrasonography compared to waveform capnography for verifying endotracheal tube location after intubation. Crit Ultrasound J. 2013;5(1):7. doi: 10.1186/2036-7902-5-7. https://doi.org/10.1186/2036-7902-5-7 PMid:23826756 PMCid:PMC3772703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ma G, Davis DP, Schmitt J, Vilke G M, Chan TC, Hayden S. The sensitivity and specificity of transcricothyroid ultrasonography to confirm endotracheal tube placement in a cadaver model. J Emerg Med. 2007;32(4):405–407. doi: 10.1016/j.jemermed.2006.08.023. https://doi.org/10.1016/j.jemermed.2006.08.023 PMid:17499695. [DOI] [PubMed] [Google Scholar]
- 23.Hernandez C, Shuler K, Hannan H, et al. CAUSE:Cardiac arrest ultra-sound exam--a better approach to managing patients in primary non-arrhythmogenic cardiac arrest. Resuscitation. 2008;76(2):198–206. doi: 10.1016/j.resuscitation.2007.06.033. https://doi.org/10.1016/j.resuscitation.2007.06.033 PMid:17822831. [DOI] [PubMed] [Google Scholar]
- 24.Breitkreutz R, Price S, Steiger HV, et al. Emergency Ultrasound Working Group of the Johann Wolfgang Goethe-University Hospital. Focused echocardiographic evaluation in life support and peri-resuscitation of emergency patients:a prospective trial. Resuscitation. 2010;81(11):1527–1533. doi: 10.1016/j.resuscitation.2010.07.013. https://doi.org/10.1016/j.resuscitation.2010.07.013 PMid:20801576. [DOI] [PubMed] [Google Scholar]
- 25.Chun R, Kirkpatrick AW, Sirois M, et al. Where’s the tube? Evaluation of hand-held ultrasound in confirming endotracheal tube placement. Prehosp Disaster Med. 2004;19(4):366–369. doi: 10.1017/s1049023x00002004. https://doi.org/10.1017/S1049023X00002004 PMid:15645633. [DOI] [PubMed] [Google Scholar]
- 26.Weaver B, Lyon M, Blaivas M. Confirmation of endotracheal tube placement after intubation using the ultrasound sliding lung sign. Acad Emerg Med. 2006;13(3):239–244. doi: 10.1197/j.aem.2005.08.014. https://doi.org/10.1111/j.1553-2712.2006.tb01685.x PMid:16495415. [DOI] [PubMed] [Google Scholar]
- 27.Werner SL, Smith CE, Goldstein JR, et al. Pilot study to evaluate the accuracy of ultrasonography in confirming endotracheal tube placement. Ann Emerg Med. 2007;49(1):75–80. doi: 10.1016/j.annemergmed.2006.07.004. https://doi.org/10.1016/j.annemergmed.2006.07.004 PMid:17014927. [DOI] [PubMed] [Google Scholar]
- 28.Chou HC, Tseng WP, Wang CH, et al. Tracheal rapid ultrasound exam (T.R.U.E.) for confirming endotracheal tube placement during emergency intubation. Resuscitation. 2011;82(10):1279–1284. doi: 10.1016/j.resuscitation.2011.05.016. https://doi.org/10.1016/j.resuscitation.2011.05.016 PMid:21684668. [DOI] [PubMed] [Google Scholar]
- 29.Marciniak B, Fayoux P, Hebrard A, et al. Airway management in children:ultrasonography assessment of tracheal intubation in real time? Anesth Analg. 2009;108(2):461–465. doi: 10.1213/ane.0b013e31819240f5. https://doi.org/10.1213/ane.0b013e31819240f5 PMid:19151273. [DOI] [PubMed] [Google Scholar]
- 30.Galicinao J, Bush AJ, Godambe SA. Use of bedside ultrasonography for endotracheal tube placement in pediatric patients:a feasibility study. Pediatrics. 2007;120(6):1297–1303. doi: 10.1542/peds.2006-2959. https://doi.org/10.1542/peds.2006-2959 PMid:18055679. [DOI] [PubMed] [Google Scholar]
- 31.Muslu B, Sert H, Kaya A, et al. Use of sonography for rapid identification of esophageal and tracheal intubations in adult patients. J Ultrasound Med. 2011;30(5):671–676. doi: 10.7863/jum.2011.30.5.671. https://doi.org/10.7863/jum.2011.30.5.671 PMid:21527615. [DOI] [PubMed] [Google Scholar]
- 32.Salem MR. Verification of endotracheal tube position. Anesthesiol Clin North America. 2001;19(4):813–839. doi: 10.1016/s0889-8537(01)80012-2. https://doi.org/10.1016/S0889-8537(01)80012-2. [DOI] [PubMed] [Google Scholar]
- 33.Rudraraju P, Eisen LA. Confirmation of endotracheal tube position:a narrative review. J Intensive Care Med. 2009;24(5):283–292. doi: 10.1177/0885066609340501. https://doi.org/10.1177/0885066609340501 PMid:19654121. [DOI] [PubMed] [Google Scholar]


