Abstract
Hepatocellular carcinoma is one of the most common cancers in the world, and it is influenced by agents such as DEN, 2-AAF, phenobarbital, alcohol, aflatoxin B1 metabolite or hepatitis viruses (B and C). Oxidative stress is becoming recognized as a key factor in the progression of hepatocarcinogenesis. Reactive oxygen species can play a leading role in initiation and promotion of hepatic carcinogenesis. The metabolites of DEN Diethylnitrosamine (DEN) mediate the binding of tumour promoters by covalently binding to the DNA with one or two oxidation-providing electrons. 2-AAF is the inducer of DEN, and it is involved in tumour formation in the bladder and liver. Reactive Oxygen species (ROS); carbohydrates, lipids, DNA and enzymes, such as affect all important structures. Additionally, an excessive amount of ROS is highly toxic to cells. Antioxidants are protects against ROS, toxic substances, carcinogens. This review focuses on the literature on studies of Hepatic Carcinogenesis, oxidative stress and antioxidant therapy.
Keywords: Hepatic Carcinogenesis, Oxidative stress, Reactive Oxygen Species, Antioxidants, DEN, 2-AAF
Introduction
Hepatic carcinogenesis is the fifth most common cancer which third most common cause of cancer-related death globally and it is influenced by agents such as DEN, 2-AAF, phenobarbital (PB), alcohol, aflatoxin B1 metabolite or hepatitis viruses (B and C) [1-2].
Animal models are viewed as crucial tools in the study of hepatic carcinogenesis. Because of the physiologic and genetic similarities between rodents and humans, the short lifespan, the breeding capacity and the variety of manipulating methods, animal models are often used for cancer research [3]. Studies on induction of liver cancer in rats use chemical agents such as DEN, 2-AAF, PB and aflatoxin B1 [4].
2-AAF exhibits its carcinogenic effect through the formation of DNA adducts, over production of reactive oxygen species (ROS) and oxidative DNA damage [5]. Nitrosamines are widely recognized as carcinogenic compounds, but they require metabolic activation to exert their cytotoxic and carcinogenic activity. DEN is a nitrosamine compound that induces the formation of hepatic carcinoma. They showed that DEN increased lipid peroxidation in studies performed. This may increase the tumour [6-7].
Our aim in this study is to reveal the relationship between antioxidants and oxidative stress in experimental hepatic carcinogenesis studies. And to report chemopreventive natural antioxidants used as inhibitors.
Reactive oxygen species (ROS)
Reactive oxygen radicals; (O2·-), hydrogen peroxide (H2O2) and hydroxyl radical (OH·), which are present in small quantities during normal oxygen metabolism. Molecular oxygen (O2) has two unpaired (unpaired) electrons with parallel spin states. An atom, group of atoms or molecules containing an unpaired electron, are defined as free radicals. Transition metals such as Fe3+, Cu2+, Mn2+ and Mo5+, however, are not considered free radicals even if they have unpaired electrons. But they play an important role in the formation of free radicals [8]. They are lipids that are most affected by reactive oxygen species. Since cell membranes are rich in polyunsaturated fatty acids (PUFAs) and cholesterol, they are easily affected by oxidant radicals. Lipid peroxidation, where the unsaturated lipids are present, is a complex process that takes place with reactions involving molecular oxygen and is formed by lipid hydroperoxides. Lipid peroxidation is rather harmful as it is an autocatalytic and irreversible reaction [9-10]. Lipid peroxidation produces a wide variety of oxidation products, such as malondialdehyde (MDA), propanal, hexanal, and 4-hydroxy nonanal (4-HNE). MDA appears to be the most mutagenic product of lipid peroxidation, but 4-HNE is most toxic. MDA is one of the most popular and reliable markers that determine oxidative stress in research [11]. Proteins are less sensitive to the effects of radicals than lipids. Protein oxidation results in the covalent modification of peptide bonds or amino acid side chains with ROS or oxidative stress products. In particular, the interaction of free radicals with unsaturated bonds and sulphide inclusion molecules is excessive. ROS may have direct or indirect effects on proteins. Amino acids such as peptide bonds, proline and lysine are quite easily affected by free radicals [12].
Protein oxidation occurs in the formation of carbonyl groups in amino acids such as histidine, tyrosine, phenylalanine. Products made by lipid peroxidation form covalent bonds with cysteine sulfhydryl groups or with lysine and histidines, leading to fragments and cross-linking of proteins. These events result in the deterioration of the structure and function of the proteins. Protein carbonyl levels area well-used marker for oxidative stress. [8-15].
DNA Damage and Free Radicals
The DNA molecule can undergo spontaneous chemical oxidative damage like carbohydrates and proteins. It has been suggested that every cell DNA of the human body is exposed to oxidative damage 103 times a day [8]. Due to the balance between DNA damage and repair, very low levels of damage are also found in healthy individuals. Oxidative base modification (8-OHdG) has been shown even in newborn rats [16]. All changes that occur due to the effects of endogenous or exogenous factors in molecular integration are called DNA damage. 8-OHdG indicates DNA damage [17-18]. In recent years, base damage has frequently been analysed as an indicator of oxidative DNA damage. Since Cu2 + ions are highly localized in the regions rich in G-C in DNA, the oxidative damage is the most exposed base guanine. 8-OHdG is a mutation that occurs in DNA, resulting from reactive oxygen species produced during normal oxidative metabolism [19]. All of the factors that lead to increased ROS production contribute to the formation of 8-OHdG, that is, oxidative DNA damage. The formation of 8-OHdG by substances such as cigarette smoke, x-rays, oxidized unsaturated fatty acids, gamma rays, polyphenols, paraquat, kainic acid, diethyl butyl sterol, benzene, fecapenene, furocoumarins hydroperoxide and heavy metals has been shown in vitro [20]. For example, Cigarette smoke contains carcinogenic substances such as nitrosamines and polycyclic aromatic hydrocarbons and causes the increased of 8-hydroxy-deoxyguanosine [19]. For this reason, the most commonly measured base damage is 8-OHdG. Therefore, 8-OHdG is considered as the “biological marker” of DNA damage [17]. Increased ROS production and oxidative DNA damage associated with hepato-carcinogenesis have been demonstrated in studies. Multivariate analysis found that levels of 8-OHdG and fibrosis were significant risk factor for hepatocellular carcinoma, especially in patients with hepatitis C virus infection [21]. The marker of oxidative stress, such as 8-OHdG is commonly elevated in the livers of patients with chronic viral hepatitis infection, which is known to be a risk factor for HC.
Experimental Hepatic Carcinogenesis
Hepatic carcinogenesis can be created experimentally in experimental animals by the application of various chemicals such as aromatic amines, nitrogen containing dyes, nitrosamines and aflatoxins [22]. Xenobiotics are carcinogenic to animals such as DEN, 2-AAF and phenobarbital, mouse, rat, hamster, rabbit, dog, pig and monkey. DEN and 2-AAF are the chemicals that cause tumours to form in the biological system. [23-24-25]. Co-administration of DEN and 2-AAF initiates hepatocarcinogenesis in rodents and causes preneoplastic initiation in hepatocytes. [26-27-28]. In a study with FB acting as a promoter, such as DEN and 2-AAF, it was reported that they caused a mutation in codon 61 of H-Ras [29].
Figure 1.
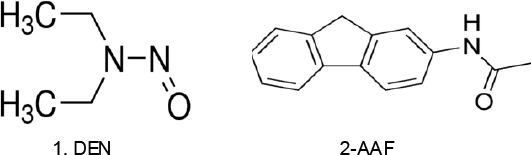
DEN and 2-AAF of structure
Role of DEN in tumorigenesis
DEN is mostly used as tumour inducer in cancer researches [30-31]. In the structure of DEN; Amide, urease and carbon containing compounds are available [32]. It has been reported that DENs are composed of intoxicates, from agrochemicals and nitrattan, from those in cigarette smoke, as well as the formation of nutrients and nutrient nitrates [27-33]. DEN has a direct effect on cancer formation. This means that DEN spontaneously hydrolyzes, regardless of the enzymes. This biological activation of the active DEN by two hydroxylation reactions is catalysed by cytochrome p450. One strong mechanistic link between cancer is through the increased production of free radicals at the site of the resulting molecular changes, which include lipid peroxidation and oxidative DNA damage [34-35].
The role of 2-AAF in tumorigenesis.
2-AAF occurs as a result of the acetylation of the 2-amino floran in the synthetic arylamine structure. 2-AAF acts in the second phase of the detoxification reactions and after the first step of DEN, it binds to guanine base for the second time in DNA and creates a toxic effect This toxic effect occurs in the form of preneoplastic, neoplastic, benign neoplasm and malignant neoplasm, respectively, resulting in mutations [36-39]. If the levels of DEN and 2-AAF chemical tumour inducing agents increase in cells, the smooth endoplasmic reticulum enzymes are synthesized and detoxified [40-42].
Antioxidant Systems Against Reactive oxygen Species
İn the cells and extracellular fluid there are antioxidant defence mechanisms that try to bring the reactive oxygen radicals to a harmless state,
Antioxidant enzyme systems, which convert ROS into less toxic products: Superoxide dismutase (SOD), catalase (CAT) and glutathione redox cycle enzymes (such as glutathione peroxidase (GSH-Px), glutathione reductase, etc.). SOD enzymatically converts superoxide anion to hydrogen peroxide and molecular oxygen. Hydrogen peroxide is reduced by water and oxygen with two important intracellular enzymes, catalase and glutathione peroxidase [43-46].
Antioxidants that catch and neutralize the radicals: Alpha Tocopherol (E vitamin) and Ascorbic acid (C vitamin) function as antioxidants. Vitamin E prevents lipid peroxidation in the cell membrane. Ascorbic acid shows antioxidant activity in the cytoplasm and extracellular fluids and inhibits the inactivation of antiproteases with oxidants. Additionally, Glutathione is a multifunctional intracellular antioxidant, α-Lipoic acid (ALA), which is a sulfur-containing antioxidant with metal-chelating and antiglycation capabilities. N-acetyl-L-cysteine is a thiol containing an antioxidant that has been used to decrease conditions of oxidative stress. The most reported activity of flavonoids is protection against oxidative stress. Thus flavonoids can help scavenger ROS and are effective inhibitors of lipid peroxidation [47].
Systems that prevent the formation of ROS and prevent the formation of ROS
Structures such as ceruloplasmin, ferritin, transferrin, lactoferrin, zinc, selenium, cytochrome oxidase reduce ROS. For example; Zinc has been serving as a metal that prevents lipid peroxidation and DNA damage [48-49].
Experimental Investigations
Most of the factors that influence tumour formation cause radical production in the cell. These factors also induce tumour formation and development by affecting the initiation, development and progression stages of carcinogenesis. Various animal model studies have been done on this subject. As seen in Table 1, many natural antioxidants have been tried.
| Models | Animals | Materials | Effect | Dose | References |
|---|---|---|---|---|---|
| DEN (90 mg/kg) | Mice | Lawsonia inermis extract | MDA ↓; GSH ↑ | LIE group was given 200 mg/100 ml drinking water from the first day of DEN injection until the end of week | [50] |
| 2-AAF (50 mg/kg) | Wistar albino Rats | Tannic acid | GSH↑,GSH-Px↑,SOD↑, MDA↓ | 125 and 250 mg/kg | [51] |
| DEN (200 mg/kg) | Wistar albino Rats | Caesalpinia bonducella leaves | SOD ↑ CAT↑ GSH ↑; MDA ↓ | 100 and 200 mg/kg body weight (b.w) | [52] |
| 2-AAF (200 mg/kg) | Wistar albino rats | Garcinia kola Seed Extract | MDA ↓; GSH ↑ | 100 and 200 mg kolaviron/kg | [53] |
| DEN(200 mg/kg)+ 2-AAF (0,2 g/kg) | Rattus norwegicus rats | Tocotrienol | GSH ↑ | 30 mg/kg | [54] |
| DEN (200 mg/kg) | Rats | Vaccinium corymbosum Leaf (Blue berry) | PC↓ MDA ↓GSH ↑ | 5 and 10% BB- Chow,diet | [27] |
| 2-AAF (0.02 %) | Wistar albino rats | Geraniol (GE) | SOD↑, CAT↑, GSH ↑; MDA ↓ | 100 and 200 mg/kg (b.w) | [33] |
| DEN (200 mg/kg) | Wistar albino rats | Thymoquinone (Nigella sativa seeds) | CAT↑, GSH-Px, ↑GSH ↑; (MDA)TBARS ↓ | The rats were given Thymoquinone (4 mg/kg) in drinking water. | [55] |
| 0.01% DEN – Drinking water | Wistar strain albino rats | Carvacrol | SOD↑, CAT↑, GSH-Px, ↑GSH ↑; MDA ↓ | 15 mg/kg (b.w)-orally | [56] |
| DEN (200 mg/kg -i.p.) | Wistar albino rats | Cassia fistula Linn. leaf extract | SOD↑, CAT↑; MDA ↓ | 500 mg/kg (b.w.) | [57] |
| 2-AAF (0.02%) in diet + DEN 200 mg/kg (i.p) | Wistar rats | Aegle marmelos | GSH-Px↑ | (50 mg/kg and 25mg/kg) | [58] |
| DEN (20 mg/kg –i.p) | Mice and IL-17A knockout mice | - | 8-OHdG ↑ | - | [59] |
| DEN (200 mg/kg-i.p), | Sprague-Dawley rats | Nano curcumin | SOD↑, CAT↑, GSH ↑; MDA ↓ | 20 mg/kg (b.w) | [60] |
In conclusion, the relationship between HC and oxidative stress is a research area. ROS contributes to the initiation and progression of HC. In current clinical trials, the mechanisms of HC treatment of drugs or compounds may be partly due to anti-oxidative ability, especially the effect originating from ROS. Therefore, antioxidant therapeutics play an important role in the treatment of HC. Time, effective doses and reliable doses require further investigation of antioxidant absorption and bioavailability.
Abbreviations
- HCC: Hepatocellular carcinoma
- HC: Hepatic carcinogenesis
- 4-HNE : 4-Hydroxynonenal
- MDA: Malondialdehyde
- 8-OHdG: 8-Oxo-7-hydroxydeoxyguanosine
- DEN: Diethyl nitrosamine
- 2-AAF: 2-Acetylaminofluorene
- DNA: Deoxyribonucleic acid
- SOD: Superoxide dismutase
- CAT
- Catalase
- GSH-Px: Glutathione peroxidise
- GSH:Glutathione
- B.W: Body weight
Footnotes
Funding: This was study supported by a grant from the Research Foundation of university Kahramanmaraş Sütçü imam, Kahramanmaraş, Turkey (Project No: 2013/1-3 YLS).
Competing Interests: The authors have declared that no competing interests exist.
References
- 1.Kuroda HI, Ohtsuru AK, Futakuchi MI, Kawashita YU, Nagayama YU, Fukuda EI, Namba HI, Shirai TO, Kanematsu TA, Yamashita SH. Distinctive gene expression of receptor-type tyrosine kinase families during rat hepatocarcinogenesis. International journal of molecular medicine. 2002;9(5):473–80. https://doi.org/10.3892/ijmm.9.5.473. [PubMed] [Google Scholar]
- 2.Wood GA, Sarma DS, Archer MC. Inheritance of resistance to the promotion of preneoplastic liver lesions in Copenhagen rats. Experimental Biology and Medicine. 2001;226(9):831–835. doi: 10.1177/153537020122600904. https://doi.org/10.1177/153537020122600904 PMid:11568305. [DOI] [PubMed] [Google Scholar]
- 3.He L, Tian DA, Li PY, He XX. Mouse models of liver cancer:Progress and recommendations. Oncotarget. 2015;6(27):23306. doi: 10.18632/oncotarget.4202. https://doi.org/10.18632/oncotarget.4202 PMid:26259234 PMCid:PMC4695120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Itze L, Vesselinovitch SD, Rao KV. Estimation of the rate of DNA synthesis in newborn, regenerating and intact mice livers. Physiologia Bohemoslovaca. 1972;22(5):457–460. [PubMed] [Google Scholar]
- 5.Hasan SK, Sultana S. Geraniol attenuates 2-acetylaminofluorene induced oxidative stress, inflammation and apoptosis in the liver of wistar rats. Toxicology Mechanisms and Methods. 2015;25(7):559–573. doi: 10.3109/15376516.2015.1070225. PMid:26364502. [DOI] [PubMed] [Google Scholar]
- 6.Magee PN, Barnes JM. (1956) The production of malignant primary hepatic tumours in the rat by feeding dimethylnitrosamine. British journal of cancer. 1956;10(1):114. doi: 10.1038/bjc.1956.15. https://doi.org/10.1038/bjc.1956.15 PMid:13342328 PMCid:PMC2074083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yamada KI, Yamamiya I, Utsumi H. In vivo detection of free radicals induced by diethylnitrosamine in rat liver tissue. Free Radical Biology and Medicine. 2006;40(11):2040–204. doi: 10.1016/j.freeradbiomed.2006.01.031. https://doi.org/10.1016/j.freeradbiomed.2006.01.031 PMid:16716904. [DOI] [PubMed] [Google Scholar]
- 8.Halliwell B, Gutteridge JM. Free radicals in biology and medicine. Oxford University Press: USA; 2015. https://doi.org/10.1093/acprof:oso/9780198717478.001.0001. [Google Scholar]
- 9.Arican O, Ozturk P, Kurutas EB, Unsal V. Status of oxidative stress on lesional skin surface of plantar warts. Journal of the European Academy of Dermatology and Venereology. 2003;27(3):365–369. doi: 10.1111/j.1468-3083.2011.04419.x. https://doi.org/10.1111/j.1468-3083.2011.04419.x PMid:22221210. [DOI] [PubMed] [Google Scholar]
- 10.Slater TF. Overview of methods used for detecting lipid peroxidation. Methods in enzymology. 1984;105:283–293. doi: 10.1016/s0076-6879(84)05036-9. https://doi.org/10.1016/S0076-6879(84)05036-9. [DOI] [PubMed] [Google Scholar]
- 11.Esterbauer H, Eckl P, Ortner A. Possible mutagens derived from lipids and lipid precursors. Mutation Research/Reviews in Genetic Toxicology. 1990;238(3):223–233. doi: 10.1016/0165-1110(90)90014-3. https://doi.org/10.1016/0165-1110(90)90014-3. [DOI] [PubMed] [Google Scholar]
- 12.Stadtman ER, Levine RL. Free radical-mediated oxidation of free amino acids and amino acid residues in proteins. Amino acids. 2003;25(3-4):207–218. doi: 10.1007/s00726-003-0011-2. https://doi.org/10.1007/s00726-003-0011-2 PMid:14661084. [DOI] [PubMed] [Google Scholar]
- 13.Suzuki YJ, Carini M, Butterfield DA. Protein carbonylation. Antioxidants & redox signaling. 2010;12(3):323–325. doi: 10.1089/ars.2009.2887. https://doi.org/10.1089/ars.2009.2887 PMid:19743917 PMCid:PMC2821144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dalle-Donne I, Giustarini D, Colombo R, Rossi R, Milzani A. Protein carbonylation in human diseases. Trends in molecular medicine. 2003;9(4):169–176. doi: 10.1016/s1471-4914(03)00031-5. https://doi.org/10.1016/S1471-4914(03)00031-5. [DOI] [PubMed] [Google Scholar]
- 15.Kehler JP, Smith CV Free radical in biology:Sources, reactivities and roles in the etiology of human disease. Natural Antioxidants in Human Heaith and Disease. Academie Press: San Diego; 1994. pp. 25–62. [Google Scholar]
- 16.Randerath K, Zhou GD, Monk SA, Randerath E. Enhanced levels in neonatal rat liver of 7, 8-dihydro-8-oxo-2’-deoxyguanosine (8-hydroxydeoxyguanosine), a major mutagenic oxidative DNA lesion. Carcinogenesis. 1997;18(7):1419–21. doi: 10.1093/carcin/18.7.1419. https://doi.org/10.1093/carcin/18.7.1419 PMid:9230290. [DOI] [PubMed] [Google Scholar]
- 17.Cooke MS, Evans MD, Dizdaroglu M, Lunec J. Oxidative DNA damage:mechanisms, mutation, and disease. The FASEB Journal. 2003;17(10):1195–1214. doi: 10.1096/fj.02-0752rev. https://doi.org/10.1096/fj.02-0752rev PMid:12832285. [DOI] [PubMed] [Google Scholar]
- 18.Dizdaroglu M, Jaruga P, Birincioglu M, Rodriguez H. Free radical-induced damage to DNA:mechanisms and measurement 1, 2. Free Radical Biology and Medicine. 2002;32(11):1102–1115. doi: 10.1016/s0891-5849(02)00826-2. https://doi.org/10.1016/S0891-5849(02)00826-2. [DOI] [PubMed] [Google Scholar]
- 19.Waris G, Ahsan H. Reactive oxygen species:role in the development of cancer and various chronic conditions. Journal of carcinogenesis. 2006;5(1):14. doi: 10.1186/1477-3163-5-14. https://doi.org/10.1186/1477-3163-5-14 PMid:16689993 PMCid:PMC1479806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Shoji Fukushima MG, Kakehashi A, Wanibuchi H. Qualitative and Quantitative Assessments on Low-Dose Carcinogenicity of Genotoxic Hepatocarcinogens:Dose–Response for Key Events in Rat Hepatocarcinogenesis. Thresholds of Genotoxic Carcinogens:From Mechanisms to Regulation. 2016 [Google Scholar]
- 21.Chuma M, Hige S, Nakanishi M, Ogawa K, Natsuizaka M, Yamamoto Y, Asaka M. (2008). 8-Hydroxy-28242-deoxy-guanosine is a risk factor for development of hepatocellular carcinoma in patients with chronic hepatitis C virus infection. Journal of gastroenterology and hepatology. 2008;23(9):1431–1436. doi: 10.1111/j.1440-1746.2008.05502.x. https://doi.org/10.1111/j.1440-1746.2008.05502.x PMid:18854000. [DOI] [PubMed] [Google Scholar]
- 22.Glauert HP, Calfee-Mason K, Stemm DN, Tharappel JC, Spear BT. Dietary antioxidants in the prevention of hepatocarcinogenesis:a review. Molecular nutrition & food research. 2010;54(7):875–896. doi: 10.1002/mnfr.200900482. https://doi.org/10.1002/mnfr.200900482 PMid:20512789. [DOI] [PubMed] [Google Scholar]
- 23.Ahn B, Han BS, Kım DJ, Ohshıma H. Immunohistochemical Localization of Inducible Nitric Oxide Synthase And 3-Nitrotyrosine in Rat Liver Tumors Induced by N-Nitrosodimethylamine. Carcinogenesis. 1999;20(7):1337–1344. doi: 10.1093/carcin/20.7.1337. https://doi.org/10.1093/carcin/20.7.1337 PMid:10383909. [DOI] [PubMed] [Google Scholar]
- 24.Barbason H, Mormont C, Massart S, Bouzahzah B. Anti-carcinogenic action of phenobarbital given simultaneously with diethylnitrosamine in the rat. European Journal of Cancer and Clinical Oncology. 1986;22(9):1073–1078. doi: 10.1016/0277-5379(86)90008-8. https://doi.org/10.1016/0277-5379(86)90008-8. [DOI] [PubMed] [Google Scholar]
- 25.Kowsalya R, Kaliaperumal J, Vaishnavi M, Namasivayam E. Anticancer activity of Cynodon dactylon L. root extract against diethyl nitrosamine induced hepatic carcinoma. South Asian journal of cancer. 2015;4(2):83. doi: 10.4103/2278-330X.155691. https://doi.org/10.4103/2278-330X.155691 PMid:25992348 PMCid:PMC4418089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Thirunavukkarasu C, Sakthisekaran D. Stabilization of membrane bound enzyme profiles by sodium selenite in N-nitrosodiethylamine induced and phenobarbital promoted hepatocarcinogenesis in rats. Biomedicine & pharmacotherapy. 2003;57(3):117–123. doi: 10.1016/s0753-3322(03)00016-7. https://doi.org/10.1016/S0753-3322(03)00016-7. [DOI] [PubMed] [Google Scholar]
- 27.Bingül İ, Başaran-Küçükgergin C, Tekkeşin MS, Olgaç V, Doğru-Abbasoğlu S, Uysal M. Effect of blueberry pretreatment on diethylnitrosamine-induced oxidative stress and liver injury in rats. Environmental toxicology and pharmacology. 2013;36(2):529–538. doi: 10.1016/j.etap.2013.05.014. https://doi.org/10.1016/j.etap.2013.05.014 PMid:23811110. [DOI] [PubMed] [Google Scholar]
- 28.Ustuner MC, Degirmenci I, Kiran I, Ozden H, Civi K, Ustuner D, Gunes HV. The protective effects of demethoxyviridine and 1-alpha-hydroxy-demethoxyviridine in the livers of male rats treated with diethylnitrosamine and 2-acetylaminflourene. Saudi medical journal. 2008;29(9):1241–1246. PMid:18813404. [PubMed] [Google Scholar]
- 29.Aydinlik H, Nguyen TD, Moennikes O, Buchmann A, Schwarz M. Selective pressure during tumor promotion by phenobarbital leads to clonal outgrowth of [beta]-catenin-mutated mouse liver tumors. Oncogene. 201(20(53)):7812. doi: 10.1038/sj.onc.1204982. [DOI] [PubMed] [Google Scholar]
- 30.Barbisan LF, Scolastici C, Miyamoto M, Salvadori F, Maria D, Ribeiro LR, Viana de Camargo JL. Effects of crude extracts of Agaricus blazei on DNA damage and on rat liver carcinogenesis induced by diethylnitrosamine. Genetics and Molecular Research. 2003:295–308. PMid:14966678. [PubMed] [Google Scholar]
- 31.Tolba R, Kraus T, Liedtke C, Schwarz M, Weiskirchen R. (2015) Diethylnitrosamine (DEN)-induced carcinogenic liver injury in mice. Laboratory animals. 2015;49(Suppl. 1):59–69. doi: 10.1177/0023677215570086. https://doi.org/10.1177/0023677215570086 PMid:25835739. [DOI] [PubMed] [Google Scholar]
- 32.Hotchkiss JH, Cassens RG. Nitrate, nitrite and nitroso compounds in foods. A scientific status summary by the Institute of Food Technologists’Expert Panel on food safety and nutrition. Food Technol Aust. 1988;40(3):100–105. [Google Scholar]
- 33.Sawada S, Okano JI, Imamoto R, Yasunaka Y, Abe R, Koda M, Isomoto H. Preventive Effect of Geraniol on Diethylnitrosamine-Induced Hepatocarcinogenesis in Rats. Yonago acta medica. 2016;59(1):37. PMid:27046949 PMCid:PMC4816747. [PMC free article] [PubMed] [Google Scholar]
- 34.Magee PN. Toxicity of nitrosamines:Their possible human health hazards. Food and cosmetics toxicology. 1971;9(2):207–218. doi: 10.1016/0015-6264(71)90306-3. https://doi.org/10.1016/0015-6264(71)90306-3. [DOI] [PubMed] [Google Scholar]
- 35.Montesano R, Bartsch H. Mutagenic and carcinogenic N-nitroso compounds:possible environmental hazards. Mutation Research/Reviews in Genetic Toxicology. 1976;32(3-4):179–227. doi: 10.1016/0165-1110(76)90001-4. https://doi.org/10.1016/0165-1110(76)90001-4. [DOI] [PubMed] [Google Scholar]
- 36.Finnberg N, Silins I, Stenius U, Högberg J. Characterizing the role of MDM2 in diethylnitrosamine induced acute liver damage and development of pre-neoplastic lesions. Carcinogenesis. 2004;25(1):113–122. doi: 10.1093/carcin/bgg185. https://doi.org/10.1093/carcin/bgg185 PMid:14555611. [DOI] [PubMed] [Google Scholar]
- 37.Tozzi Spinardi AL, Kaneno R, Rodrigues MAM, Salvadori DMF, Rocha NS, Barbisan LF, Camargo JLV. Natural Killer Activity in a Medium-term Multi-organ Bioassay for Carcinogenesis. Japanese journal of cancer research. 1999;90(1):101–107. doi: 10.1111/j.1349-7006.1999.tb00672.x. https://doi.org/10.1111/j.1349-7006.1999.tb00672.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Chakraborty T, Ghosh S, Datta S, Chakraborty P, Chatterjee M. Vanadium suppresses sister-chromatid exchange and DNA–protein crosslink formation and restores antioxidant status and hepatocellular architecture during 2-acetylaminofluorene-induced experimental rat hepatocarcinogenesis. Journal of Experimental Therapeutics and Oncology. 2003;3(6):346–362. doi: 10.1111/j.1533-869x.2003.01107.x. https://doi.org/10.1111/j.1533-869X.2003.01107.x PMid:14678523. [DOI] [PubMed] [Google Scholar]
- 39.Pietrowska MO, Lanuszewska JO, Walter Z, Rzeszowska-Wolny JO, Widlak P. Detection and characterization of rat protein recognizing DNA damaged by N-acetoxy-acetylaminofluorene. Cellular and Molecular Biology Letters. 2000;5(4):423–32. [Google Scholar]
- 40.Cai Y, Wang H, Xiao Y, Ren J. Altered expression of cytochrome P450 and possible correlation with preneo plastic changes in early stage of rat hepatocarcinogenesis. Acta Pharmacologica Sinica. 2005;26(6):737–44. doi: 10.1111/j.1745-7254.2005.00737.x. https://doi.org/10.1111/j.1745-7254.2005.00737.x PMid:15916741. [DOI] [PubMed] [Google Scholar]
- 41.Pinto LFR, Moraes E, Albano RM, Silva MC, Godoy W, Glisovic T, Lang MA. Rat oesophageal cytochrome P450 (CYP) monooxygenase system:comparison to the liver and relevance in N-nitrosodiethylamine carcinogenesis. Carcinogenesis. 2001;22(11):1877–1883. doi: 10.1093/carcin/22.11.1877. https://doi.org/10.1093/carcin/22.11.1877 PMid:11698352. [DOI] [PubMed] [Google Scholar]
- 42.Marnett LJ. Oxy radicals, lipid peroxidation and DNA damage. Toxicology. 2002;181:219–222. doi: 10.1016/s0300-483x(02)00448-1. https://doi.org/10.1016/S0300-483X(02)00448-1. [DOI] [PubMed] [Google Scholar]
- 43.McCord JM, Fridovich I. Superoxide dismutase an enzymic function for erythrocuprein (hemocuprein) Journal of Biological chemistry. 1969;244(22):6049–6055. PMid:5389100. [PubMed] [Google Scholar]
- 44.Roos DIRK, Weening RS, Wyss SR, Aebi HE. Protection of human neutrophils by endogenous catalase:studies with cells from catalase-deficient individuals. Journal of Clinical Investigation. 1980;65(6):1515. doi: 10.1172/JCI109817. https://doi.org/10.1172/JCI109817 PMid:7410555 PMCid:PMC371491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Halliwell B. Free radicals, antioxidants, and human disease:curiosity, cause, or consequence? The lancet. 1994;344(8924):721–724. doi: 10.1016/s0140-6736(94)92211-x. https://doi.org/10.1016/S0140-6736(94)92211-X. [DOI] [PubMed] [Google Scholar]
- 46.Aydogan F, Unlu İ, Aydin E, Yumusak N, Devrim E, Samim EE, Seyhan N. The effect of 2100 MHz radiofrequency radiation of a 3G mobile phone on the parotid gland of rats. American journal of otolaryngology. 2015;36(1):39–46. doi: 10.1016/j.amjoto.2014.10.001. https://doi.org/10.1016/j.amjoto.2014.10.001 PMid:25456509. [DOI] [PubMed] [Google Scholar]
- 47.Kurutas EB. The importance of antioxidants which play the role in cellular response against oxidative/nitrosative stress:current state. Nutrition Journal. 2016;15(1):71. doi: 10.1186/s12937-016-0186-5. https://doi.org/10.1186/s12937-016-0186-5 PMid:27456681 PMCid:PMC4960740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Silva DD, Aust SD. Ferritin and ceruloplasmin in oxidative damage:review and recent findings. Canadian journal of physiology and pharmacology. 1993;71(9):715–720. doi: 10.1139/y93-107. https://doi.org/10.1139/y93-107. [DOI] [PubMed] [Google Scholar]
- 49.Unsal V, Kurutaş EB, Öztürk P. The effects of the H1-receptor blockers on Adenosine Deaminase, xhanthine oxidase and Trace elements ın patıents with chronic idiopathic Urtıcaria. European Journal of Pharmaceutical and Medical Research. 2017;4(3):117–121. [Google Scholar]
- 50.Abdel-Hamid NM, Mohafez OM, Nazmy MH, Farhan A, Thabet K. The effect of co-administration of Lawsonia inermis extract and octreotide on experimental hepatocellular carcinoma. Environmental health and preventive medicine. 2015;20(3):195–203. doi: 10.1007/s12199-015-0451-9. https://doi.org/10.1007/s12199-015-0451-9 PMid:25726025 PMCid:PMC4434234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Sehrawat A, Sharma S, Sultana S. Preventive effect of tannic acid on 2-acetylaminofluorene induced antioxidant level, tumor promotion and hepatotoxicity:a chemopreventive study. Redox Report. 2006;11(2):85–95. doi: 10.1179/135100006X101066. https://doi.org/10.1179/135100006X101066 PMid:16686999. [DOI] [PubMed] [Google Scholar]
- 52.Kumar RS, Sivakumar T, Sunderam RS, Gupta M, Mazumdar UK, Gomathi P, Rajeshwar Y, Saravanan S, Kumar MS, Murugesh K, Kumar KA. Antioxidant and antimicrobial activities of Bauhinia racemosa L. stem bark. Brazilian journal of medical and biological research. 2005;38(7):1015–24. doi: 10.1590/s0100-879x2005000700004. https://doi.org/10.1590/S0100-879X2005000700004 PMid:16007272. [DOI] [PubMed] [Google Scholar]
- 53.Farombi EO, Tahnteng JG, Agboola AO, Nwankwo JO, Emerole GO. Chemoprevention of 2-acetylaminofluorene-induced hepatotoxicity and lipid peroxidation in rats by kolaviron—a Garcinia kola seed extract. Food and Chemical Toxicology. 2000;38(6):535–41. doi: 10.1016/s0278-6915(00)00039-9. https://doi.org/10.1016/S0278-6915(00)00039-9. [DOI] [PubMed] [Google Scholar]
- 54.Rahmat A, Ngah WZ, Shamaan NA, Gapor A, Abdul KK. Long-term administration of tocotrienols and tumor-marker enzyme activities during hepatocarcinogenesis in rats. Nutrition (Burbank, Los Angeles County, Calif.) 1993;9(3):229–32. PMid:8102564. [PubMed] [Google Scholar]
- 55.Sayed-Ahmed MM, Aleisa AM, Al-Rejaie SS, Al-Yahya AA, Al-Shabanah OA, Hafez MM, Nagi MN. Thymoquinone attenuates diethylnitrosamine induction of hepatic carcinogenesis through antioxidant signaling. Oxidative medicine and cellular longevity. 2010;3(4):254–261. doi: 10.4161/oxim.3.4.12714. https://doi.org/10.4161/oxim.3.4.12714 PMid:20972371 PMCid:PMC2952085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Jayakumar S, Madankumar A, Asokkumar S, Raghunandhakumar S, Kamaraj S, Divya MGJ, Devaki T. Potential preventive effect of carvacrol against diethylnitrosamine-induced hepatocellular carcinoma in rats. Molecular and cellular biochemistry. 2012;360(1-2):51–60. doi: 10.1007/s11010-011-1043-7. https://doi.org/10.1007/s11010-011-1043-7 PMid:21879312. [DOI] [PubMed] [Google Scholar]
- 57.Pradeep K, Mohan CVR, Gobianand K, Karthikeyan S. Effect of Cassia fistula Linn. leaf extract on diethylnitrosamine induced hepatic injury in rats. Chemico-Biological Interactions. 2007;167(1):12–18. doi: 10.1016/j.cbi.2006.12.011. https://doi.org/10.1016/j.cbi.2006.12.011 PMid:17289008. [DOI] [PubMed] [Google Scholar]
- 58.Husain Khan T, Sultana S. (2011) Effect of Aegle marmelos on DEN initiated and 2-AAF promoted hepatocarcinogenesis:a chemopreventive study. Toxicology mechanisms and methods. 2011;21(6):453–462. doi: 10.3109/15376516.2011.564677. https://doi.org/10.3109/15376516.2011.564677 PMid:21417629. [DOI] [PubMed] [Google Scholar]
- 59.Sun C, Kono H, Furuya S, Hara M, Hirayama K, Akazawa Y, Nakata Y, Fujii H. Interleukin-17A plays a pivotal role in chemically induced hepatocellular carcinoma in mice. Digestive diseases and sciences. 2016;61(2):474–88. doi: 10.1007/s10620-015-3888-1. https://doi.org/10.1007/s10620-015-3888-1 PMid:26467699. [DOI] [PubMed] [Google Scholar]
- 60.Hassan SK, Mousa AM, Eshak MG, Farrag AERH, Badawi AEFM. (2014) Therapeutic and chemopreventive effects of nano curcumin against diethylnitrosamine induced hepatocellular carcinoma in rats. Int J Pharm Pharm Sci. 2014;6(3):54. [Google Scholar]


