Abstract
Skin cancer risk is elevated in solid organ transplant recipients (OTRs). Studies of skin cancer awareness and sun-protection behaviors in pediatric transplant recipients (pOTRs) have not been reported. We measured effects over time of a multimodal educational intervention on knowledge of sun-protection practices and skin cancer risk, engagement in sun-protection behaviors, and self-efficacy and perceived barriers to photoprotection in pOTRs, their guardians, and a comparison group of children and guardians. Knowledge about skin cancer risk increased in pOTRs and their guardians (P ≤ .01) and frequency of pOTRs’ sun-protection behaviors reported by pOTRs and their guardians also improved.
Keywords: organ transplants, skin cancer, education, pediatrics
INTRODUCTION
Skin cancer risk is elevated in solid organ transplant recipients (OTRs) due to their need for chronic immunosuppression.(1, 2) Skin cancer is the most frequent malignancy in OTRs, and when skin cancers do occur, they are often more aggressive than in immunocompetent patients.(1, 3, 4) Thus, skin cancer represents a major medical issue for transplant recipients, leading to decreased quality of life, morbidity, and even mortality.(1, 5, 6) Risk factors for the development of skin cancer in OTRs include fair skin, cumulative sun exposure, and intensity and duration of immunosuppression.(1) When OTRs adopt better sun-protection practices, their rate of skin cancer development decreases.(2, 3) Studies have shown that awareness and understanding of skin cancer risk in adult OTRs are low: only 20–40% of OTRs are aware of their increased skin cancer risk, and many transplant patients do not understand the reasoning behind sun-protection instructions.(6–8) Recent studies of targeted educational interventions for adult kidney transplant recipients have shown efficacy in improving compliance with sun-protection recommendations and promoting skin self-exams.(9, 10)
Studies of skin cancer awareness and sun-protection behaviors in pediatric solid-organ transplant recipients (pOTRs) have not been reported in the literature; however, these issues are likely to be equally as important in children as they are in adults. Skin cancer is the most common malignancy following renal transplant in children, and is second only to post-transplant lymphoproliferative disorder in nonrenal transplants.(11) As outcomes improve and children survive longer after transplant (and therefore undergo increasing duration of immunosuppression), it is expected that rates of skin cancer in patients who received their transplant during childhood will increase. Although the increased risk for skin cancer may be relatively remote (up to 10–20 years) from the time of transplant,(11, 12) it is imperative that pOTRs and their parents/guardians receive skin cancer risk education to encourage use of sun-protective behaviors that can mitigate the effects of immunosuppression on development of skin cancers.
The aims of this study were to 1) evaluate baseline skin cancer knowledge, sun-protection behaviors, and self-efficacy and perceived barriers to photoprotection in pOTRs, their guardians, and a comparison group of participants, and 2) assess changes over time in these areas after a multimodal educational intervention on skin cancer risk and photoprotection practices in pOTRs and their guardians.
PATIENTS AND METHODS
Study Population
Following approval by the Washington University School of Medicine Institutional Review Board, a convenience sample of patients was recruited from June 2013 to January 2014. The intervention group included pOTRs between 10–17 years old and their guardians. These participants were recruited during routine follow-up transplant clinic visits and hospital admissions; all pOTRs had received solid-organ transplants at least 1 year before enrollment. Comparison-group participants were recruited during routine visits in the dermatology clinic and included children, matched to pOTR participants based on age, sex, and physician-estimated skin type, and their guardians. Inclusion required participants to speak and read English and be willing and able to provide written consent (guardians)/assent (children). We excluded children with a personal history of skin cancer.
Study design
We conducted a prospective, non-randomized study. At the initial visit, all participants completed the baseline survey, which included questions about demographic information, medical history, skin type, knowledge of sun-protection practices and risk for skin cancer, knowledge about the appearance of non-melanoma skin cancers, talking to anyone about skin care and skin cancer risk, current sun-protection behaviors, and self-efficacy of and perceived barriers to engaging in sun-protection behaviors. Items were worded the same for transplant and comparison groups and worded appropriately for children and guardians. The outcome measures are described below.
Knowledge
Questions about skin cancer risk and non-melanoma skin cancer recognition were developed for this study; several questions were designed previously by medical students and faculty at Washington University and Saint Louis University Schools of Medicine for their Sun Protection Outreach Teaching by Students program. Scores were the total number of correct answers for the11-item knowledge measure (measure available upon request).
Behaviors
We developed 11 items for children and 9 items for guardians to measure sun-protection behaviors; these questions reflected behaviors also assessed by the self-efficacy and perceived barriers measures. Seven items inquired about the frequency of sunscreen use and reapplication, wearing hats and sun-protective clothing, playing/sitting in shade, limiting time outside, and monthly skin self-examination, and were evaluated using responses on a 5-point scale from “never” (1) to “always” (5). Higher scores indicated greater frequency of engaging in each sun-protection behavior. These results are reported. The remaining questions asked about who applied sunscreen (child or guardian), reason to use sunscreen, and whether or not children would report changes in their skin to their parents (data not shown).
Self-efficacy and perceived barriers
To measure self-efficacy for and perceived barriers to sun-protection behaviors, we adapted items from a study of parents who were melanoma survivors and had children under 12 years of age.(13) We included 5 items from this study measuring self-efficacy, with responses ranging from “not at all confident “(1) to “extremely confident” (5). We included 11 items (children) and 13 items (guardians) measuring perceived barriers to sun-protection behaviors with responses ranging from “strongly disagree” (1) to “strongly agree” (5). We calculated mean scores with higher scores indicating greater self-efficacy for and greater agreement with perceived barriers to engaging in sun-protection behaviors.
Intervention
Following administration of the baseline survey, we delivered a multimodal educational intervention to pOTRs and their guardians; content was delivered using verbal instruction, a video, and printed materials to take home, with time for questions and discussion. The intervention content was based on the International Transplant Skin Cancer Collaborative guidelines and included information about skin cancer risk, recognizing skin cancer, effective sun-protection behaviors, and skin self-examination. Detailed information about the educational intervention is available online (Supplement).
Pediatric transplant participants and their guardians answered the knowledge questions again 1 week after the intervention. At 3- and 6-month follow-up, pOTRs and their guardians completed the full survey; at the 6-month follow-up, they also completed a 5-item questionnaire about recall and impressions of the intervention. Comparison-group participants completed baseline surveys only.
Data analysis
The factor structure of the newly developed self-efficacy and perceived barriers measures was determined separately for children and guardians using exploratory principal components analysis with varimax rotation of baseline data. Since the sample was small, we also used Lautenschlager’s parallel analysis criteria(14) to determine the number of factors for each measure. Cronbach’s standardized alpha measured the internal consistency of items on each emerging factor. We report descriptive statistics for sample characteristics (sample mean, M) and for each outcome of interest (knowledge, each sun-protection behavior, self-efficacy, and perceived barriers scores) at baseline for all participants and follow-up assessments for pOTRs and their guardians. Mann-Whitney U-tests examined differences in baseline measures of each outcome by study group (transplant and comparison), gender, and race (white vs. non-white). Spearman’s rho correlations measured associations among age and the outcomes. Wilcoxon paired signed-rank tests measured changes in the outcomes for pOTRs and their guardians at each follow-up compared with baseline. Two-tailed P values < .05 were considered significant.
RESULTS
Eighty participants (20 pairs of pOTRs and guardians; 20 pairs of comparison-group children and guardians) enrolled in the study. Participants’ baseline characteristics are summarized in Table 1. A greater proportion of pOTR guardians than comparison-group guardians talked with someone about their child’s risk for skin cancer, but 50% of pOTR guardians had not talked with anyone about this risk. We did not observe a significant difference between guardian groups in having previous discussions with someone about their child’s skin care. Physical exam performed at the baseline visit for pOTRs detected lesions on 3 patients requiring biopsy, including a basal cell carcinoma on the participant with history of a cardiac transplant.
Table 1.
A–B. Baseline characteristics of pediatric solid organ transplant recipients and comparison-group children (A) and guardians (B)
| A. Children | ||
|---|---|---|
| Characteristics | pOTRs (N = 20) | Comparison-group children (N = 20) |
| Mean age, y (range) | 13 (10–17) | 13 (10–17) |
| Female sex, N (%) | 11 (55) | 11 (55) |
| Self-identified Fitzpatrick skin type, N (%)a | ||
| I | 2 (11) | 0 (0) |
| II | 4 (21) | 1 (5) |
| III | 4 (21) | 14 (70) |
| IV | 4 (21) | 3 (15) |
| V | 4 (21) | 2 (10) |
| VI | 1 (5) | 0 (0) |
| Race, N (%) | ||
| White | 16 (80) | 18 (90) |
| Black | 2 (10) | 2 (10) |
| Other | 2 (10) | 0 (0) |
| Organ transplanted, N (%)b | ||
| Kidney | 11 (55) | |
| Liver | 7 (35) | |
| Double lung | 2 (10) | |
| Heart | 1 (5) | |
| Mean time from first transplant, y (range) | 7 (2–13) | |
| Mean number of current immunosuppressant medications, (SD) | 2 (.65) | |
| Physical exam findings, N (%) | ||
| Basal cell carcinoma | 1 (5%) | |
| Porokeratoses | 1 (5%) | |
| Clinically atypical nevus (benign histopathology) | 1 (5%) | |
| B. Guardians | ||
| Characteristics | pOTR guardians (N = 20) | Comparison-group guardians (N = 20) |
| Mean age, years (range) | 42 (26–59) | 45 (35–55)c |
| Female sex, N (%) | 14 (70) | 16 (80) |
| Education, N (%)d | ||
| High school graduate or less, N (%) | 7 (35) | 3 (15) |
| Some college or more, N (%) | 13 (65) | 17 (85) |
| “Has anyone talked with you about caring for your child’s skin (post-transplant)?”e | ||
| Yes, N (%) | 15 (75) | 17 (85) |
| No, N (%) | 5 (25) | 3 (15) |
| “Have you discussed your child’s risk for skin cancer with anyone (post-transplant)?f | ||
| Yes, N (%) | 10 (50) | 2 (10) |
| No, N (%) | 10 (50) | 18 (90) |
N, number of patients
pOTR = pediatric solid organ transplant recipient
One pOTR did not answer
One patient had both liver and kidney transplants
n=19 for comparison-group guardian age calculations
Level of education did not differ significantly between the groups (chi-square = 2.133, P = .14)
Talking with someone about caring for child’s skin did not differ significantly between groups (chi-square = .625, P = .43). “Post-transplant” wording included for pOTR guardians.
Talking with someone about child’s risk of skin cancer differed significantly between groups (chi-square = 7.619, P = .006). “Post-transplant” wording included for pOTR guardians.
Note: race data was not collected for guardians
Knowledge
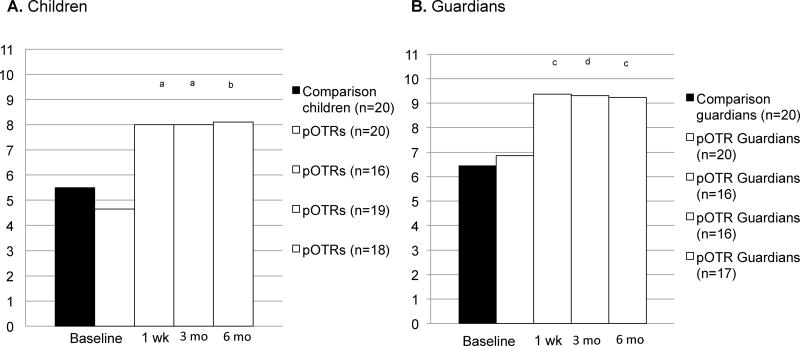
Baseline knowledge did not differ significantly between pOTR and comparison-group children (P = .21, Figure 1A) or by gender (P = .26). Greater knowledge was reported by white (vs. non-white) children (M=5.56 vs. M=2.50; P = .003). Knowledge increased significantly in pOTRs after the educational intervention (Figure 1A).
Figure 1.
A–B. Knowledge at baseline and pOTR children’s and guardians’ knowledge over time.
A. Children
B. Guardians
pOTR = pediatric solid organ transplant recipient
Significance testing vs. pOTRs’ baseline (Wilcoxon paired signed-rank test), a P < .001, b P = .001
Significance testing vs. pOTR guardians’ baseline (Wilcoxon paired signed-rank test), c P = .002, d P = .001
Guardians of pOTRs and of comparison-group children did not differ significantly in baseline knowledge (P = .24, Figure 1B). Guardians’ level of education (P = .34) was not associated with baseline knowledge. Knowledge increased significantly in pOTR guardians after the intervention (Figure 1B).
Sun-protection behaviors
Behaviors reported by children at baseline and over time are in Table 2A. There were no significant differences between pOTRs and comparison-group children for baseline sun-protection behaviors. Compared with baseline, pOTRs reported more frequent engagement in multiple sun-protection behaviors at 6-month follow-up. At both 3-month (P = .002) and 6-month (P = .02) follow-up, pOTRs reported improvements in frequency of examining their skin monthly for changes.
Table 2.
A–B. Means (standard deviations) of the frequencies of children’s self-reported sun-protection behaviors (A) and guardians’ reports of their children’s behaviors (B)
| A. Children’s self-reported sun-protection behaviors | |||||||
|---|---|---|---|---|---|---|---|
| Comparison-group children | pOTRs | ||||||
| Baseline | Baseline | p-valuea | 3 months | p-valueb | 6 months | p-valueb | |
| Wear SPF ≥ 15 | 2.95 (1.28) | 3.50 (1.36) | .16 | 3.63 (1.12) | .90 | 3.74 (.81) | .72 |
| Reapply sunscreen every 2 hours | 2.90 (1.21) | 2.70 (1.34) | .53 | 3.05 (1.27) | .12 | 3.63 (1.12) | .003 |
| Wear wide-brimmed hats | 1.90 (1.02) | 2.15 (.81) | .26 | 2.37 (1.07) | .26 | 2.42 (1.35) | .43 |
| Wear sun-protective clothing | 2.25 (.97) | 2.85 (1.04) | .12 | 3.00 (1.37) | .31 | 3.21 (1.32) | .16 |
| Play/sit in the shade when possible | 3.25 (.91) | 3.50 (1.05) | .46 | 3.63 (1.21) | .46 | 4.11 (1.10) | .02 |
| Limit time outside 10am–4pm | 2.30 (1.17) | 2.55 (1.36) | .62 | 2.79 (1.55) | .27 | 3.32 (1.38) | .02 |
| Examine skin for changes once per monthc | 2.25 (1.37) | 2.70 (1.26) | .20 | 3.84 (1.01) | .002 | 3.74 (1.15) | .02 |
| B. Guardians’ reports of their children’s behaviors | |||||||
| Comparison-group guardians | pOTR guardians | ||||||
| Baseline | Baseline | p-valued | 3 months | p-valuee | 6 months | p-valuee | |
| Wear SPF ≥ 15 | 3.16 (1.01) | 3.79 (1.36) | .05 | 3.94 (.93) | .94 | 3.56 (.86) | .29 |
| Reapply sunscreen every 2 hours | 2.95 (1.00) | 2.60 (.94) | .23 | 3.13 (1.09) | .05 | 3.28 (1.07) | .005 |
| Wear wide-brimmed hats | 1.30 (.47) | 1.85 (1.18) | .16 | 2.56 (1.46) | .03 | 2.44 (1.34) | .01 |
| Wear sun-protective clothing | 2.00 (.92) | 2.65 (.93) | .03 | 3.19 (1.22) | .11 | 3.11 (1.08) | .14 |
| Play/sit in the shade when possible | 2.55 (.89) | 3.45 (.76) | .002 | 3.94 (.68) | .10 | 3.78 (.73) | .31 |
| Limit time outside 10am–4pm | 1.95 (.69) | 2.65 (1.14) | .04 | 3.44 (1.03) | .004 | 3.56 (1.04) | .002 |
| Examine skin for changes once per monthf | 2.30 (1.30) | 2.50 (1.15) | .49 | 2.81 (1.11) | .08 | 3.56 (1.10) | .007 |
pOTR = pediatric solid organ transplant recipient
significance testing is pOTRs vs. comparison children at baseline, p-values calculated by Mann-Whitney U-tests
significance testing is pOTRs vs. their baseline, p-values calculated by Wilcoxon paired signed-rank test
Skin self-exam
significance testing is guardians of pOTRs vs. guardians of comparison patients at baseline, p-values calculated by Mann-Whitney U-tests
significance testing is guardians of pOTRs vs. their baseline, p-values calculated by Wilcoxon paired signed-rank test
Guardians’ examination of their children’s skin
Behaviors reported by guardians are in Table 2B. At baseline, pOTR guardians reported their children more often wore sun-protective clothing (P = .03) and played/sat in the shade (P = .002), and that they more often limited the time their children spent outside between 10am and 4pm (P = .04) than comparison-group guardians.
At 6-month follow-up, pOTR guardians reported increases in the frequencies that their children reapplied sunscreen (P = .005) and that they examined their children’s skin monthly (P = .007) compared with baseline.
Self-efficacy
A single-factor solution emerged for children’s (Cronbach’s alpha = .756) and guardians’ (Cronbach’s alpha = .795) self-efficacy at baseline following principal components analysis; alphas indicated acceptably high internal consistency of items on this measure. As shown in Table 3, pOTRs reported significantly higher self-efficacy than comparison-group children (P = .02) at baseline. White children reported higher self-efficacy than non-white children (M=3.32 vs. M=2.47; P = .04), but self-efficacy did not differ significantly by gender. Similarly, pOTR guardians reported significantly higher self-efficacy than comparison-group guardians at baseline (P = .02), but guardians’ self-efficacy did not differ significantly by education nor relationship to child (mother/father). Results over time are shown in Table 3.
Table 3.
Self-efficacy [mean (standard deviation)] of children and guardians
| Comparison children | pOTRs | p-value | Comparison guardians | pOTR guardians | p-value | |
|---|---|---|---|---|---|---|
| Baselinea | 2.92 (.76) | 3.46 (.73) | .02 | 2.91 (.72) | 3.41 (.54) | .02 |
| 3 monthsb | 3.73 (.65) | .08 | 3.79 (.68) | .04 | ||
| 6 monthsb | 3.88 (.53) | .009 | 3.67 (.59) | .12 |
pOTR = pediatric solid organ transplant recipient
significance testing is for comparison of baseline values, p-values calculated by Mann-Whitney U-tests
significance testing is for pOTRs and pOTR guardians vs. their baseline, p-values calculated by Wilcoxon paired signed-rank test
Perceived barriers
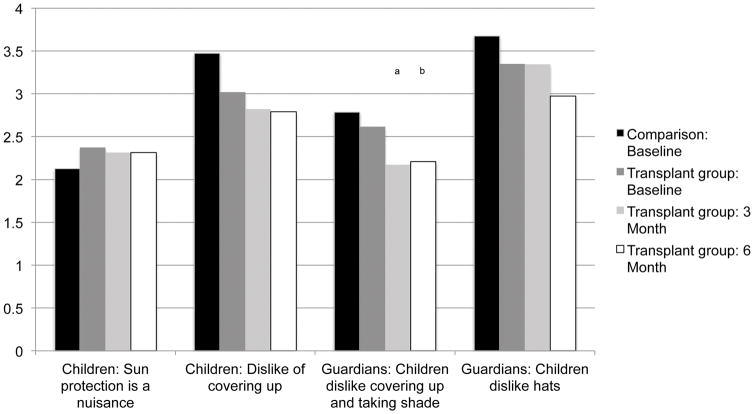
A 2-factor solution emerged for each group following principal components analysis at baseline, with different factors for children and guardians (eTable 1). Gender was not associated with either factor in children, but non-white children reported greater perceptions that sun protection was a nuisance than white children at baseline (M=2.92 vs. M=2.13; P = .03). However, there were no significant differences at baseline between pOTR and comparison-group children on either factor, and no significant change in pOTRs’ perceived barriers on either factor at follow-up (Figure 2).
Figure 2.
Children and guardians: Perceived barriers at baseline (all participants) and over time (pOTRs and their guardians)
pOTR = pediatric solid organ transplant recipient
Significance testing vs. pOTR guardians’ baseline (Wilcoxon paired signed-rank test), a P = .002, b P = .009
Guardians with education beyond high school (vs. high school or less) reported greater agreement with perceived barriers to protecting their children from the sun at baseline (M=2.84 vs. M=2.28; P = .03). There was no significant difference at baseline between pOTR and comparison-group guardians on either factor. At both 3 and 6 months, pOTR guardians reported fewer perceived barriers to protecting their children from the sun (P = .002 and P = .009, respectively), but no significant change in their perceptions that their children dislike wearing hats (Figure 2).
Correlations among age and outcomes
Older age was associated with greater knowledge, which was in turn correlated with greater self-efficacy in children (eTable 2). Greater self-efficacy in children was correlated with lower perceived barriers for covering up. Similarly, guardian’s greater knowledge was significantly correlated with less perception of barriers in that their children dislike hats.
Intervention evaluation
Almost all pOTRs (18/19) and their guardians (16/17) remembered receiving the educational intervention. Most of the pOTRs (14/18) and all of the guardians (16/16) who remembered receiving the intervention thought it was relevant to them and reported they would recommend a similar session to other transplant patients and family members.
DISCUSSION
In 2013, 1,818 solid-organ transplants were performed in patients younger than 18 years of age, compared with 1,607 pediatric transplants in 2000 and 1,396 in 1990 (based on Organ Procurement and Transplantation Network data as of August 11, 2015). Accordingly, there are increasing numbers of pOTRs at risk for early development of skin cancer. Despite their higher risk, pOTRs and their guardians in our study did not have greater knowledge about skin cancer than comparison-group participants at baseline. Thus, both groups demonstrated a substantial knowledge gap regarding pOTRs’ skin cancer risk. Educational interventions for children require targeting both guardians and the pOTRs; younger patients rely on their parents to guide behavior and, as they age, children assume more responsibility for their behaviors and have more autonomy in their choices. The goals of educating pOTRs and their guardians are to decrease risk for skin cancer and increase early recognition of skin cancers.
Our multimodal educational intervention was feasible and was an effective way to deliver information about skin cancer risk and sun-protection strategies, as both pOTRs and their guardians demonstrated significantly increased knowledge 1 week after their educational session, and gains persisted to the 6-month follow-up. Although pOTRs’ perceived barriers to sun-protection behaviors did not change significantly over follow-up, they reported significant improvements in the frequency of engaging in 2 key behaviors: reapplying sunscreen every 2 hours and examining their skin monthly for changes. The baseline questionnaire was administered from June–August in 9 pOTRs and September–November in 11 pOTRs. Thus, the season in which baseline data were collected cannot explain the increase in re-application behavior. Skin self-examination was taught as an important adjunct to regular dermatologic and transplant follow-up, and children reported increased skin self-examination after instruction, similar to the changes seen in adult kidney transplant patients after instruction.(10) The lack of change in perceived barriers might be explained by the lack of information in the educational intervention addressing perceived barriers to sun protection. Interventions targeting these barriers and ways to overcome them could include discussions of peer pressure and autonomy.
Future research may evaluate whether patient and parent education can result in decreased rates of skin cancers in pOTRs. Longer-term follow-up data to examine whether pOTRs who receive educational interventions are more likely to seek dermatologic care would also be useful to help determine the long-term efficacy of such interventions. Educational materials developed by dermatologists and widely distributed could aid transplant teams and facilitate delivery of detailed education about skin cancer and sun protection to greater numbers of patients and their families.
Small sample size and recruitment at a single institution are limitations to this pilot and feasibility study. We enrolled a comparison group of children without transplants, which allowed us to compare pOTRs to their peers on the variables of interest at baseline. In spite of the small sample, we observed improvements in many of these variables among pOTRs. However, because this was not a randomized controlled trial, we cannot make causal inferences from these findings.
Nevertheless, this educational-intervention study of pOTRs and their guardians is the largest of its kind. Identifying a skin cancer in one participant during the intervention showed the utility of dermatologic exam and positively impacted the child’s care.
CONCLUSIONS
The benefits of educating both pOTRs and their guardians were shown in the increased knowledge of both groups at follow-up. Moreover, participants’ endorsement of the session’s relevance and their willingness to recommend a similar session to other pOTRs motivate us to move forward with larger-scale work in this area.
Supplementary Material
eTable 1. Perceived barriers: factor solutions for each group
eTable 2. Spearman’s rho correlations among age and the continuous outcomes of interest at baseline between children and guardians
Footnotes
Author contributions:
Dr. Coughlin: concept/design, data collection, data analysis/interpretation, drafting of the article, critical revision of article. Ms. Perez: data analysis/interpretation, statistics, drafting of the article, critical revision of the article. Dr. Kumar: data collection, approval of the article. Dr. Jeffe: data analysis/interpretation, statistics, critical revision of the article. Dr. Bayliss: concept/design, approval of the article. Dr. Sternhell-Blackwell: concept/design, critical revision of the article.
References
- 1.Zwald FO, Brown M. Skin cancer in solid organ transplant recipients: advances in therapy and management: part I. Epidemiology of skin cancer in solid organ transplant recipients. Journal of the American Academy of Dermatology. 2011 Aug;65(2):253–61. doi: 10.1016/j.jaad.2010.11.062. quiz 62. [DOI] [PubMed] [Google Scholar]
- 2.Euvrard S, Kanitakis J, Claudy A. Skin cancers after organ transplantation. The New England journal of medicine. 2003 Apr 24;348(17):1681–91. doi: 10.1056/NEJMra022137. [DOI] [PubMed] [Google Scholar]
- 3.Ulrich C, Jurgensen JS, Degen A, Hackethal M, Ulrich M, Patel MJ, et al. Prevention of non-melanoma skin cancer in organ transplant patients by regular use of a sunscreen: a 24 months, prospective, case-control study. The British journal of dermatology. 2009 Nov;161( Suppl 3):78–84. doi: 10.1111/j.1365-2133.2009.09453.x. [DOI] [PubMed] [Google Scholar]
- 4.Zwald FO, Christenson LJ, Billingsley EM, Zeitouni NC, Ratner D, Bordeaux J, et al. Melanoma in solid organ transplant recipients. American journal of transplantation : official journal of the American Society of Transplantation and the American Society of Transplant Surgeons. 2010 May;10(5):1297–304. doi: 10.1111/j.1600-6143.2010.03078.x. [DOI] [PubMed] [Google Scholar]
- 5.Berg D, Otley CC. Skin cancer in organ transplant recipients: Epidemiology, pathogenesis, and management. Journal of the American Academy of Dermatology. 2002 Jul;47(1):1–17. doi: 10.1067/mjd.2002.125579. quiz 8–20. [DOI] [PubMed] [Google Scholar]
- 6.Robinson JK, Rigel DS. Sun protection attitudes and behaviors of solid-organ transplant recipients. Dermatologic surgery : official publication for American Society for Dermatologic Surgery [et al] 2004 Apr;30(4 Pt 2):610–5. doi: 10.1111/j.1524-4725.2004.30145.x. [DOI] [PubMed] [Google Scholar]
- 7.Cowen EW, Billingsley EM. Awareness of skin cancer by kidney transplant patients. Journal of the American Academy of Dermatology. 1999 May;40(5 Pt 1):697–701. doi: 10.1016/s0190-9622(99)70149-0. [DOI] [PubMed] [Google Scholar]
- 8.Kim NN, Boone SL, Ortiz S, Mallett K, Stapleton J, Turrisi R, et al. Squamous cell carcinoma in solid organ transplant recipients: influences on perception of risk and optimal time to provide education. Archives of dermatology. 2009 Oct;145(10):1196–7. doi: 10.1001/archdermatol.2009.247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Clowers-Webb HE, Christenson LJ, Phillips PK, Roenigk RK, Nguyen TH, Weaver AL, et al. Educational outcomes regarding skin cancer in organ transplant recipients: Randomized intervention of intensive vs standard education. Archives of dermatology. 2006 Jun;142(6):712–8. doi: 10.1001/archderm.142.6.712. [DOI] [PubMed] [Google Scholar]
- 10.Robinson JK, Turrisi R, Mallett KA, Stapleton J, Boone SL, Kim N, et al. Efficacy of an educational intervention with kidney transplant recipients to promote skin self-examination for squamous cell carcinoma detection. Archives of dermatology. 2011 Jun;147(6):689–95. doi: 10.1001/archdermatol.2011.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Euvrard S, Kanitakis J, Cochat P, Claudy A. Skin cancers following pediatric organ transplantation. Dermatologic surgery : official publication for American Society for Dermatologic Surgery [et al] 2004 Apr;30(4 Pt 2):616–21. doi: 10.1111/j.1524-4725.2004.30146.x. [DOI] [PubMed] [Google Scholar]
- 12.Penn I. De novo malignances in pediatric organ transplant recipients. Pediatric transplantation. 1998 Feb;2(1):56–63. [PubMed] [Google Scholar]
- 13.Tripp MK, Diamond PM, Vernon SW, Swank PR, Dolan Mullen P, Gritz ER. Measures of parents’ self-efficacy and perceived barriers to children’s sun protection: construct validity and reliability in melanoma survivors. Health education research. 2012 Nov 30; doi: 10.1093/her/cys114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lautenschlager GJ. A comparison of alternatives to conducting Monte Carlo analyses for determining parallel analysis criteria. Multivariate Behavioral Research. 1989;24(3):365–95. doi: 10.1207/s15327906mbr2403_6. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. Perceived barriers: factor solutions for each group
eTable 2. Spearman’s rho correlations among age and the continuous outcomes of interest at baseline between children and guardians