Abstract
Background
Some types of sexually transmitted infection (STI) have higher prevalence in females than males, and among black, relative to white, females. Identifying mechanisms of STI risk is critical to effective intervention. We tested a model in which alcohol and marijuana use serve as mediating factors in the associations between depression and conduct problems with sexual risk behavior (SRB) and STI in adolescent females.
Methods
The Pittsburgh Girls Study is a longitudinal observational study of females who have been followed annually to track the course of mental and physical health conditions. The three oldest cohorts (n=1750; 56.8% black; 43.2% white) provided self-reports of substance use, depression and conduct problems, SRB, and STI at ages 16–18. A path model tested alcohol and marijuana use at age 17 as mechanisms that mediate the associations of depression and conduct problems at age 16 with SRB and STI at age 18.
Results
Race was involved in two risk pathways. In one pathway, white females reported greater alcohol use, which was associated with greater SRB. In another pathway, black females reported earlier sexual onset, which was associated with subsequent SRB. Public assistance use was independently associated with early sexual onset and STI. SRB, but not substance use, mediated the association of depression and conduct problems with STI.
Conclusions
Differences by race in pathways of risk for SRB and STI, involving, for example, alcohol use and early sexual onset, were identified for young white and black females, respectively. Depression and conduct problems may signal risk for SRB and STI in young females, and warrant attention to improve health outcomes.
Keywords: Adolescent, female, sexually transmitted infection, risky sexual behavior, alcohol, marijuana
INTRODUCTION
Sexually transmitted infection (STI) prevalence escalates in adolescence and peaks in young adulthood.1 In the United States, prevalence of some STIs (e.g., chlamydia) is higher in women than men, and STI prevalence is higher among black, relative to white, females.1 These observations justify a focus on adolescent females as a high risk group, and the exploration of the role of race in pathways of risk for STI. Among the modifiable personal risk factors that have been associated with sexual risk behavior (SRB) and STI, substance use and psychopathology, specifically depression and conduct problems, are relatively prevalent and serve as important targets for prevention of SRB and STI in females. Few studies, however, have examined how these factors are associated within distinct pathways of risk in young females.
A meta-analysis of the association between substance use and SRB (e.g., early sexual onset, multiple sexual partners) in adolescence found small to moderate effect sizes.2 Further, some research indicates racial differences in types of SRB.3 For example, black youth tend to have earlier age of sexual onset compared to their white counterparts,4 suggesting the utility of examining age of sexual onset separately from other types of SRB.5,6 In addition, the strength of the association between substance use and SRB is generally weaker in black, relative to white youth.2,7 This difference by race may be partially explained by higher rates of alcohol use among White, relative to black, females, whereas black females had higher rates of marijuana use,8 suggesting that risk pathways for SRB/STI may differ by race and type of substance use.
Internalizing (e.g., depression) and externalizing (e.g., conduct problems) behaviors have been studied as precursors to both substance use9 and SRB.10,11 For example, depression predicted self-reported STI at 1-year follow-up among 7th to 12th graders in the Add Health study.12 Other research indicates that trajectories of conduct problems and substance use were associated with SRB across ages 12–18.13 One longitudinal study of teenage mothers, which analyzed both internalizing and externalizing behaviors as predictors of SRB and STI, found that externalizing, but not internalizing, behaviors were concurrently associated with young adult SRB and STI.14 In the study of teenage mothers, SRB mediated the association between early marijuana use (prior to age 15) and young adult STI.14
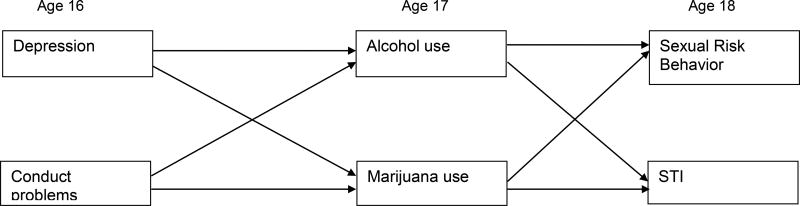
Although existing research supports associations between internalizing and externalizing behaviors, substance use, and SRB/STI, there is a gap in knowledge regarding the temporal ordering of these variables. Thus, we tested a conceptual model (Figure 1) that specifies a sequence of associations over time, starting with depression and conduct problems because they often precede and predict substance use.9 In turn, substance use, a mediator, was proposed to predict SRB and STI.2,15 Strengths of testing mediation using longitudinal data include the ability to make stronger inferences regarding the direction of influence of one variable on another, and the identification of possible mechanisms that can help to explain how psychopathology may be related to SRB/STI.
Figure 1.
Conceptual model of proposed longitudinal associations among psychopathology, substance use, and sexual risk behavior and sexually transmitted infection
Figure Legend
Note: The figure shows only the main (not all possible) pathways of interest. Race is not included in the figure, although pathways to sexual risk behavior and sexually transmitted infection (STI) are hypothesized to differ by race.
We tested the mediation model in the Pittsburgh Girls Study, a large longitudinal community sample of black and white adolescent females. We hypothesized that black, compared to white, females would report earlier sexual onset and higher rates of SRB/STI,1 but lower rates of alcohol use.8 We also tested the hypothesis that frequency of alcohol and marijuana use at age 17 would mediate the associations of depression and conduct problems at age 16 with SRB and STI at age 18. We explored the role of race in these associations, predicting, for example, that the association between alcohol use and SRB/STI would be stronger among white, relative to black, females.7,15
METHODS
Participants
The Pittsburgh Girls Study16,17 is an urban sample of girls first assessed at ages 5–8 (4 age cohorts), who completed annual interviews. The analysis sample included 1,750 girls identified by their caretaker as being of black or white race (black n=994, 56.8%; white n=756, 43.2%) in the three oldest cohorts (85.6% retention at ages 16–18).
Procedure
The university’s Institutional Review Board approved all study procedures. For minors, written (from caregiver) and verbal (from the girl) informed consent was obtained. At age 18, participants provided their own written informed consent. Participants were compensated.
Measurement
Sexual behavior was assessed with the Adolescent Sexual Activity Index.18 A sexual risk behavior score (range: 0–3)7,19 represented the sum of sexual intercourse with ≥2 partners in the past year (0=no, 1=yes); did not ‘always’ use birth control (0=no, 1=yes); and did not use condoms (0=no, 1=yes). Girls were asked about STIs, “In the past year, have you been diagnosed or treated for a sexually transmitted disease? Examples: gonorrhea, chlamydia, herpes, HIV, genital warts, or other” (0=no, 1=yes). The Nicotine, Alcohol, and Drug Substance Use20 measure assessed past year alcohol and marijuana use at ages 16–17, coded as: 0=none through 7=daily. Covariates included: public assistance use at age 16 (0=no, 1=yes), and age at onset of sexual intercourse with a male (mean= 16.8, SD=1.8). At age 16, depression and conduct problems were self-reported using the Adolescent Symptom Inventory-4 (ASI-4).21
Statistical Analysis
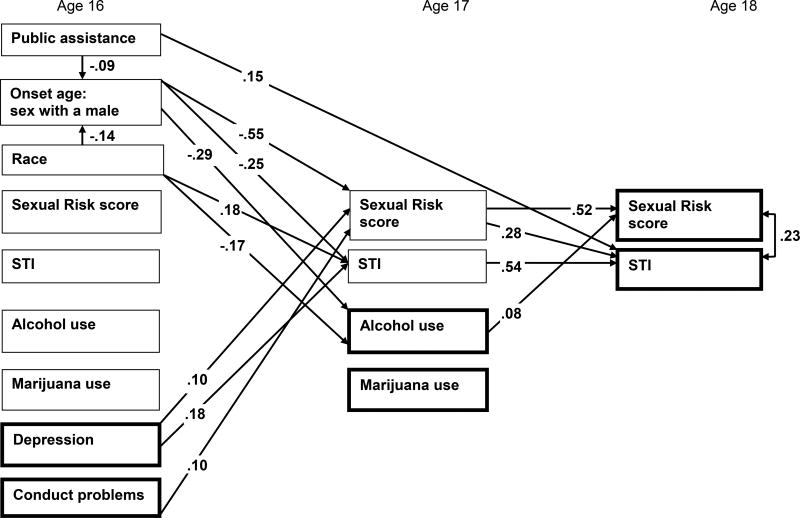
Mplus 7.1322 tested a path model (Figure 2) of potential age 17 mediators (e.g., alcohol, marijuana use) of the association between age 16 risk factors (e.g., poverty, depression, conduct problems) and age 18 SRB and STI status. The model specified direct effects from each age 16 variable to all age 17 variables, and from each age 17 variable to the two age 18 outcomes (SRB score, and STI status). Preliminary multiple group analyses by race did not result in a unique solution that fit the data, so analyses using the total sample in a path model, which included race as a covariate, are reported. Since race1 and socioeconomic status (SES)23 have been associated with SRB and STI (see supplementary table), the path model included direct effects of race (1=white, 2=black) and public assistance on the two age 18 outcomes, and direct effects of race and public assistance on sexual onset age. Missing data at follow-up were handled in the analysis using full information maximum likelihood estimation. Indirect (mediation) effects were estimated using the indirect command. A significant indirect effect was identified if 0 was not included in the 95% bias corrected bootstrap confidence interval.
Figure 2.
Path model showing selected paths (p<.05) predicting sexually transmitted infection status and sexual risk score at age 18
Legend
Note: N=1750. Bolded boxes represent the variables in the conceptual model depicted in Figure 1. The main outcomes of interest are age 18 sexual risk score and STI status. To provide a stringent test of the conceptual model, covariates were added to the path model, such as race, age 16 public assistance, age of onset for sex with a male. The model also controlled for age 16 alcohol and marijuana use, and sexual risk behavior and STI status, when predicting age 17 alcohol and marijuana use, and sexual risk behavior and STI status. Only statistically significant paths of interest, as described in text are depicted (see supplementary materials for the path model with all statistically significant paths shown).
A weighted least squares means and variance adjusted (WLSMV) estimator was used. Standardized estimates and significant (p<.05) paths are shown. A direct effect of race on age of sexual onset was included, given racial differences in this variable and sexual onset was only included at one time point. Covariances between other baseline variables and between age 18 variables were modeled, but are not shown. Race coded 1=White, 2=Black. Public Assistance use is coded 0=no, 1=yes. STI= self-report of a past year diagnosis of sexually transmitted infection (chlamydia, gonorrhea, trichomoniasis), coded 0=no, 1=yes. Mediation was tested using the indirect command and 1000 bias corrected bootstrap samples.
R2 values for endogenous variables: age of sexual onset= 0.04, age 17 alcohol frequency= 0.36, age 17 marijuana frequency= 0.36, age 17 sexual risk score= 0.52, age 17 STI= 0.24, age 18 sexual risk behavior score= 0.38, age 18 STI= 0.58.
RESULTS
Sample description and comparison of black and white girls
At ages 16 to 18, 2.8 to 3.8% of girls self-reported a past year STI (see Table) representing chlamydia (73.2 to 79.2%), gonorrhea (7.1 to 8.9%), or trichomoniasis (8.6 to 9.5%). At ages 16–18, black girls were more likely than white girls to report an STI, and to have a higher SRB score. Black, relative to white, girls had a lower mean age of sexual onset (mean age=16.6 [SD=1.9) vs 17.2 [SD=1.8]). White, compared to black, girls reported greater frequency of alcohol use at ages 16 and 17. However, black, relative to white, girls reported more frequent marijuana use at ages 16 and 17. Depression severity at age 16 did not differ by race, although black girls reported more conduct problems at age 16.
Table.
Descriptive statistics by race
| Black N=994 |
White N=756 |
Black versus White | |||
|---|---|---|---|---|---|
| n | % | n | % | ||
| Age 16: Public assistance (n=1501) | 443 | 50.9 | 109 | 17.3 | X2(df=1)=177.1, p<.01 |
| Mean (SD) | Mean (SD) | ||||
| Age at onset: Sex with a male (n=1339) | 16.6 (1.9) | 17.2 (1.8) | t(df=1210.5)=6.0, p<.01 | ||
| STI reported (past year) | n | % | n | % | |
| Age 16 (n=1488) | 35 | 4.0 | 7 | 1.1 | X2(df=1)=11.1, p<.01 |
| Age 17 (n=1472) | 37 | 4.3 | 8 | 1.3 | X2(df=1)=10.3, p<.01 |
| Age 18 (n=1507) | 51 | 5.7 | 7 | 1.1 | X2(df=1)=20.6, p<.01 |
| Sexual Risk Behavior Score | Mean (SD) | Mean (SD) | |||
| Age 16 (n=1485) | 0.7 (1.0) | 0.4 (0.7) | t(df=1476.0)= −5.8, p<.01 | ||
| Age 17 (n=1474) | 0.8 (1.0) | 0.6 (0.8) | t(df=1415.8)= −5.0, p<.01 | ||
| Age 18 (n=1513) | 1.0 (0.9) | 0.9 (0.9) | t(df=1511.0)= −3.0, p<.01 | ||
| Alcohol use (past year) | Mean (SD) | Mean (SD) | |||
| Age 16 (n=1489) | 0.4 (1.0) | 0.8 (1.2) | t(df=1155.7)= 6.4, p<.01 | ||
| Age 17 (n=1472) | 0.6 (1.1) | 1.1 (1.4) | t(df=1107.9)= 8.2, p<.01 | ||
| Marijuana use (past year) | Mean (SD) | Mean (SD) | |||
| Age 16 (n=1488) | 0.7 (1.7) | 0.5 (1.3) | t(df=1482.0)= −3.5, p<.01 | ||
| Age 17 (n=1472) | 0.9 (1.9) | 0.6 (1.5) | t(df=1449.4)= −3.1, p<.01 | ||
| Psychopathology | Mean (SD) | Mean (SD) | |||
| Age 16 Depression (n=1489) | 7.1 (4.8) | 7.0 (4.9) | ns | ||
| Age 16 Conduct Problems (n=1491) | 1.5 (2.3) | 1.1 (1.9) | t(df=1463.9)= −3.5, p<.01 | ||
Notes: STI= sexually transmitted infection. STI includes chlamydia, gonorrhea, and trichomoniasis. ns=not statistically significant (p≥.05).
Between-group comparisons were conducted on unadjusted means and proportions.
Path model of SRB and STI status
The path model (Figure 2) had good fit according to most indices, including CFI= .98, and WRMR =.66, with RMSEA=.06 (90% CI: .05, .07) and TLI= .87 indicating mediocre fit.24 Race (standardized Beta, β= −.14, p<.01) and receipt of public assistance (β= −.09, p<.01) had a direct effect on age of sexual onset, such that girls who identified as black and those who reported public assistance use had earlier sexual onset than white girls and those not reporting public assistance. Report of public assistance, but not race, had a direct effect (β= .15, p<.05) on age 18 STI status. At age 17, higher SRB score was predicted by younger age of sexual onset (β= −.55, p<.01), and severity of depression (β= .10, p<.01) and conduct problems (β= .10, p<.01). Age 17 STI was predicted by race (β=.18, p<.05; black girls more likely to report age 17 STI), younger age of sexual onset (β= −.25, p<.05), and age 16 depression severity (β= .18, p<.01). At age 18, higher SRB score was predicted by higher SRB score at age 17 (β= .52, p<.01) and greater frequency of alcohol use at age 17 (β= .08, p<.01). STI at age 18 was predicted by STI at age 17 (β= .54, p<.01) and higher SRB score at age 17 (β= .28, p<.01).
Tests of indirect effects indicated multiple mediated pathways of interest to age 18 SRB score and STI. In predicting age 18 SRB score, two indirect pathways involving age 17 alcohol use were identified. In one path, race had an indirect effect on SRB score through alcohol use frequency (bootstrap estimate= −0.037, 95% CI: −0.080, −0.007), such that white girls tended to report more frequent alcohol use, and greater alcohol use was associated with higher SRB score. In the other path, age of sexual onset had an indirect effect on SRB score through alcohol use (bootstrap estimate= −0.017, 95% CI: −0.170, −0.005), indicating that earlier sexual onset was associated with more frequent alcohol use, which in turn was associated with higher SRB score. Despite significant bivariate correlations (supplementary table), age 16 alcohol and marijuana use were not significantly associated with age 17 SRB score in the path model.
Regarding age 18 STI, SRB score at age 17 mediated several pathways. Specifically, age 17 SRB score was a mediator of the association between age 18 STI and age 16 predictors that included depression severity (bootstrap estimate= 0.009, 95% CI: 0.003, 0.019), conduct problem severity (bootstrap estimate= 0.020, 95% CI: 0.006, 0.044), and age of sexual onset (bootstrap estimate= −0.129, 95% CI: −0.300, −0.054). The pathway that included sexual onset could be extended to include race (race→sexual onset→age 17 SRB score→age 18 STI), controlling for public assistance, such that black girls had earlier age of sexual onset, which was associated with higher SRB score at age 17 and STI at age 18 (bootstrap estimate= 0.067, 95% CI: 0.024, 0.159). In another pathway, report of public assistance, controlling for race, was associated with age of sexual onset, which in turn was associated with age 17 SRB score, and age 18 STI (bootstrap estimate= 0.043, 95% CI: 0.009, 0.121). Age 17 alcohol and marijuana use were not associated with age 18 STI in the path model, although there was a small bivariate association between age 17 marijuana use and age 18 STI (r=.11, p<.01).
DISCUSSION
Study results provide new information regarding a sequence of associations between psychopathology (conduct problems and depression), alcohol and marijuana use, and SRB/STI among black and white adolescent females. Specifically, frequency of alcohol use at age 17 mediated the association of race with SRB at age 18, and the association of age of sexual onset with SRB at age 18. In contrast, marijuana use was not a mediator in the path model, suggesting the relative importance of alcohol use in risk for SRB at ages 16–18. Furthermore, the finding that alcohol use frequency at age 17 was a mediator in risk pathways for SRB, but not STI, may reflect that for the ages examined, SRB typically precedes STI, and SRB may not always result in STI.
Contrary to the proposed hypothesis, the association of depression and conduct problems at age 16 with SRB and STI at age 18 was not mediated by frequency of alcohol or marijuana use. Instead, SRB at age 17 mediated the association of depression and conduct problems with STI at age 18. The current findings extend prior research12 by showing that, in young females, both depression and conduct problems are associated with greater SRB, and subsequent STI.
The path model also indicated that early sexual onset was linked to STI at age 18 through SRB at age 17, a pathway that could be extended to include both race and use of public assistance as independent predictors of early sexual onset. Although early sexual onset and SRB have been associated with STI in prior research,5,6 the current study is one of few to test a specific sequence of personal risk factors that may lead to SRB and STI in adolescent females.
Study limitations warrant consideration. Results may have limited generalizability beyond white and black adolescent females sampled in an urban community. Self-report of substance use and psychopathology is subject to possible bias. We did not study other factors (e.g., dating violence, other trauma exposure, health care availability, partner engagement, desire to become pregnant) that may be associated with STI/SRB risk.
This longitudinal study addressed gaps in knowledge regarding specific pathways of risk associated with SRB and STI in a community sample of black and white adolescent females. Differences by race were observed for two pathways leading to SRB, one in which white females reported greater alcohol use, and another in which black females reported earlier sexual onset. Results also indicated that alcohol, relative to marijuana, use was more strongly associated with SRB. More generally, depression and conduct problems may serve as early warning signs of risk for SRB and STI in young females.
Supplementary Material
Acknowledgments
FUNDING
This work was supported by NIDA R01 DA012237, NIMH R01 MH056630, The Office of Juvenile Justice and Delinquency Prevention (2013-JF-FX-0058), the FISA Foundation, and the Falk Fund. The funders had no role in design and conduct of the study; collection, management, analysis, or interpretation of the data; or review or approval of the manuscript.
Footnotes
The authors have no conflicts of interest to declare.
AUTHOR CONTRIBUTIONS
TC conceived and conducted the analyses, and drafted the ms; AH and SS oversaw data collection; FY oversaw statistical analyses; AH, SS, FY EM, SB, and MH provided feedback on the analyses, participated in drafting the ms, and reviewed the final ms.
References
- 1.Centers for Disease Control and Prevention. Sexually Transmitted Disease Surveillance 2013. Atlanta: U. S. Department of Health and Human Services; 2014. [Google Scholar]
- 2.Ritchwood TD, Ford H, DeCoster J, Sutton M, Lochman JE. Risky Sexual Behavior and Substance Use among Adolescents: A Meta-analysis. Child Youth Serv Rev. 2015;52:74–88. doi: 10.1016/j.childyouth.2015.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fergus S, Zimmerman MA, Caldwell CH. Growth trajectories of sexual risk behavior in adolescence and young adulthood. Am J Public Health. 2007;97(6):1096–1101. doi: 10.2105/AJPH.2005.074609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Biello KB, Ickovics J, Niccolai L, Lin H, Kershaw T. Racial differences in age at first sexual intercourse: residential racial segregation and the black-white disparity among U.S. adolescents. Public Health Rep. 2013;128(Suppl 1):23–32. doi: 10.1177/00333549131282S103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kaestle CE, Halpern CT, Miller WC, Ford CA. Young age at first sexual intercourse and sexually transmitted infections in adolescents and young adults. Am J Epidemiol. 2005;161(8):774–780. doi: 10.1093/aje/kwi095. [DOI] [PubMed] [Google Scholar]
- 6.Upchurch DM, Mason WM, Kusunoki Y, Kriechbaum MJ. Social and behavioral determinants of self-reported STD among adolescents. Perspect Sex Reprod Health. 2004;36(6):276–287. doi: 10.1363/psrh.36.276.04. [DOI] [PubMed] [Google Scholar]
- 7.Hipwell A, Stepp S, Chung T, Durand V, Keenan K. Growth in alcohol use as a developmental predictor of adolescent girls' sexual risk-taking. Prev Sci. 2012;13(2):118–128. doi: 10.1007/s11121-011-0260-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Johnston LD, O'Malley PM, Miech RA, Bachman JG, Schulenberg JE. Monitoring the Future national results on adolescent drug use: Overview of key findings, 2014. Ann Arbor, MI: Institute for Social Research, the University of Michigan; 2015. [Google Scholar]
- 9.Chassin L, Ritter J. Vulnerability to substance use disorder in childhood and adolescence. In: Ingram RE, Price JM, editors. Vulnerability to psychopathology: Risk across the lifespan. New York: Guilford; 2001. pp. 107–134. [Google Scholar]
- 10.Donenberg GR, Pao M. Youths and HIV/AIDS: psychiatry's role in a changing epidemic. J Am Acad Child Adolesc Psychiatry. 2005;44(8):728–747. doi: 10.1097/01.chi.0000166381.68392.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Seth P, Patel SN, Sales JM, DiClemente RJ, Wingood GM, Rose ES. The impact of depressive symptomatology on risky sexual behavior and sexual communication among African American female adolescents. Psychol Health Med. 2011;16(3):346–356. doi: 10.1080/13548506.2011.554562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shrier LA, Harris SK, Beardslee WR. Temporal associations between depressive symptoms and self-reported sexually transmitted disease among adolescents. Arch Pediatr Adolesc Med. 2002;156(6):599–606. doi: 10.1001/archpedi.156.6.599. [DOI] [PubMed] [Google Scholar]
- 13.Mustanski B, Byck GR, Dymnicki A, Sterrett E, Henry D, Bolland J. Trajectories of multiple adolescent health risk behaviors in a low-income African American population. Dev Psychopathol. 2013;25(4 Pt 1):1155–1169. doi: 10.1017/S0954579413000436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.De Genna N, Cornelius M, Cook R. Marijuana use and sexually transmitted infections in young women who were teenage mothers. Women Health Iss. 2007;17:300–309. doi: 10.1016/j.whi.2007.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sales JM, Brown JL, Vissman AT, DiClemente RJ. The association between alcohol use and sexual risk behaviors among African American women across three developmental periods: a review. Curr Drug Abuse Rev. 2012;5(2):117–128. doi: 10.2174/1874473711205020117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hipwell AE, Loeber R, Stouthamer-Loeber M, Keenan K, White HR, Kroneman L. Characteristics of girls with early onset disruptive and antisocial behaviour. Crim Behav Ment Health. 2002;12(1):99–118. doi: 10.1002/cbm.489. [DOI] [PubMed] [Google Scholar]
- 17.Keenan K, Hipwell A, Chung T, et al. The Pittsburgh Girls Study: overview and initial findings. J Clin Child Adolesc Psychol. 2010;39(4):506–521. doi: 10.1080/15374416.2010.486320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hansen W, Paskett E, Carter L. The Adolescent Sexual Activity Index (ASAI): A standardized strategy for measuring interpersonal heterosexual behaviors among youth. Health Educ Res. 1999;14:485–490. doi: 10.1093/her/14.4.485. [DOI] [PubMed] [Google Scholar]
- 19.Locke T, Newcomb M. Correlates and predictors of HIV risk among inner-city African American female teenagers. Health Psychol. 2008;27:337–348. doi: 10.1037/0278-6133.27.3.337. [DOI] [PubMed] [Google Scholar]
- 20.Pandina R, Labouvie E, White HR. Potential contributions of the life span developmental approach to the study of adolescent alcohol and drug use: The Rutgers Health and Human Development Project, a working model. J Drug Issues. 1984;14:253–268. [Google Scholar]
- 21.Gadow KD, Sprafkin J. Revised Norms and Scoring Guide Child Symptom Inventory-4. Stony Brook, NY: Checkmate Plus; 1999. [Google Scholar]
- 22.Muthen B, Muthen L. Mplus User’s Guide. Venice, CA: Author; 2008–2014. [Google Scholar]
- 23.Crichton J, Hickman M, Campbell R, Batista-Ferrer H, Macleod J. Socioeconomic factors and other sources of variation in the prevalence of genital chlamydia infections: A systematic review and meta-analysis. BMC Public Health. 2015;15:729. doi: 10.1186/s12889-015-2069-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Little T. Longitudinal Structural Equation Modeling. New York: Guilford; 2013. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.