Abstract
Background
The prevalence of HIV and Hepatitis C Virus (HCV) are significantly lower among people who inject drugs (PWID) in San Diego, CA, USA compared with PWID in Tijuana, Mexico, located directly across the border. We investigated associations between cross-border injection drug use (IDU), HIV and HCV seroprevalence and engagement in injecting risk behaviours while on each side of the border.
Methods
Using baseline interviews and serologic testing data from STAHR II, a longitudinal cohort study of PWID in San Diego, bivariate and multivariable logistic regression analyses examined associations between recent (past six months) cross-border IDU and HIV and HCV antibody seropositivity, socio-demographics, drug use characteristics, and participants’ connections to, and perceptions about Mexico. Chi-squared tests and McNemar tests examined associations between cross-border IDU and injecting risk behaviours.
Results
Of the 567 participants (93% US-born, 73% male, median age 45 years), 86 (15%) reported recent cross-border IDU. Cross-border IDU was not associated with HIV (OR: 0.85, 95% CI: 0.37–1.95) or HCV seropositivity (OR: 1.01, 95% CI: 0.62–1.65). Age, identifying as Hispanic or Latino/a, and being concerned about risk of violence when travelling to Mexico were independently associated with decreased odds of recent cross-border IDU. Injecting cocaine at least weekly, having ever lived in Mexico and knowing PWID who reside in Mexico were associated with increased odds of recent cross-border IDU. PWID who reported cross-border IDU were significantly less likely to engage in receptive needle sharing, equipment sharing, and public injection while in Mexico compared with in San Diego (all p<0.001).
Conclusion
Prevalence of HIV and HCV infection was similar among PWID who had and had not injected in Mexico, possibly due to practicing safer injecting while in Mexico. Research is needed to elucidate contextual factors enabling U.S. PWID to inject safely while in Mexico.
Keywords: Injection drug use, Mexico, HIV, Hepatitis C virus, Risk behaviour, Border crossing
Introduction
Population mobility plays an important role in health, particularly in relation to infectious diseases (Hirsch, 2014; Michalopoulos, Aifah, & El-Bassel, 2016; Rachlis et al., 2007; Weine & Kashuba, 2012). Although there is often a concern that mobile populations can introduce infectious diseases to populations in the settings to which they travel (Grove & Zwi, 2006; Kamper-Jorgensen et al., 2012), they may also be exposed to new or increased risks in these settings compared with their place of origin (Goldenberg, Strathdee, Perez-Rosales, & Sued, 2012; Rachlis et al., 2007; Weine & Kashuba, 2012). This vulnerability is particularly important as mobile populations can act as bridge populations when infected travellers transmit infections upon returning home (Kramer et al., 2008; Rachlis et al., 2007; Rai et al., 2014).
The United States (U.S.)-Mexico border region spans 10 states, and is characterised by extensive cross-border mobility for the purposes of employment, trade, visiting family and friends, and tourism (Lee et al., 2013; Murià & Chávez, 2011; Romo & Marquez, 2010). The border crossing between San Diego, California, and Tijuana, Baja California is the busiest in the world, with an estimated 33 million crossings in each direction in 2015 (San Diego Association of Governments, 2016). Located on a prominent drug trafficking route, Tijuana is experiencing a syndemic of injection drug use (IDU) and HIV (Brouwer et al., 2006; Instituto Nacional de Salud Pública, 2008; Strathdee, Magis-Rodriguez, Mays, Jimenez, & Patterson, 2012).
Cross-border travel for the purposes of buying and injecting drugs has been reported among people who inject drugs (PWID) in the U.S-Mexico border region, as well as international settings including the China-Vietnam and China-Myanmar border regions (Hammett et al., 2005; Li, Assanangkornchai, Duo, McNeil, & Li, 2014; Williams, Liu, & Levy, 2011). In San Diego, approximately one-third of PWID have ever injected drugs in Mexico, with cheaper price, ease of access to drugs and higher quality drugs the most commonly reported reasons for cross-border injection (Volkmann et al., 2011; K. D. Wagner et al., 2012). In August 2009, Mexico enacted drug policy reform which decriminalised small amounts of drugs for personal use (Mackey et al., 2014), potentially influencing patterns of cross-border IDU among U.S. PWID, and prompting a need for research to characterise PWID who engage in this behaviour, in order to appropriately target services.
Cross-border IDU in this region may have significant implications for infectious disease transmission. First, there is disparity in disease prevalence, with prevalence of HIV and Hepatitis C Virus (HCV) among PWID in San Diego estimated at 4% and 27–51%, respectively, compared with 4–10% and 96% among PWID in Tijuana, respectively (Garfein et al., 2013; Gunn et al., 2003; Strathdee, Lozada, Ojeda, et al., 2008; Strathdee, Lozada, Pollini, et al., 2008; White et al., 2007). Second, contextual factors that impact PWIDs’ ability to practice safe injecting may also differ. Compared to established residents, newcomers often engage in riskier injecting practices, including sharing injecting equipment and injecting in public spaces (Rachlis et al., 2007), potentially due to a lack of resources and established social networks. Although syringe possession is legal and pharmacies may sell syringes without a prescription in Tijuana, reports from Mexican PWID suggest that access to sterile syringes is limited and drug use commonly occurs in informal settings with poor amenities (e.g. shooting galleries), creating barriers to safe injecting (Davidson et al., 2012; Philbin et al., 2008; Smith et al., 2016). Little is known about whether these conditions extend to U.S. PWID who inject in Mexico.
Although evidence from a binational disease surveillance system has identified cross-border travel as a risk factor for acute viral hepatitis in the U.S.-Mexico border region (Spradling et al., 2013), few studies have examined cross-border IDU specifically. Despite some evidence of receptive syringe sharing while in Mexico (Volkmann et al., 2011), no significant associations between cross-border IDU and HIV or HCV seropositivity were detected in earlier cross-sectional studies (Garfein et al., 2013; Volkmann et al., 2011), however these studies did not examine injecting risk behaviours specific to each setting. Consequently, the objective of this paper was to explore in detail the relationships between cross-border IDU, HIV/HCV prevalence and injecting risk behaviours. Specifically, the primary aim was to measure the prevalence of recent (past six-month) cross border IDU, test for associations between recent cross-border IDU and HIV and HCV seropositivity, and identify independent correlates of recent cross-border IDU in order to identify sub-populations of mobile PWID who may be in need of health information and prevention resources. To help interpret the results of this primary analysis, a secondary analysis was conducted which aimed to: 1) compare self-reported engagement in injecting risk behaviours between PWID who did and did not report recent cross-border IDU, and 2) compare self-reported injecting risk behaviours among those who report cross-border IDU during injection events in each location.
Methods
Study methods
Data were drawn from the Study of Tuberculosis, AIDS, and Hepatitis C Risk (STAHR II), a mixed methods longitudinal cohort study designed to assess the putative consequences of Mexico’s drug policy reform on U.S. PWID. Study methods have been described in detail elsewhere (Robertson et al., 2014). In brief, 574 participants were recruited from sites across San Diego County between 2012 and 2014, using targeted outreach methods. Eligible individuals were those aged 18 years and over who had injected illicit drugs within the past 30 days, spoke English or Spanish, and had no plans to move away from San Diego County in the next two years. The study received ethical approval from the University of California San Diego Human Research Protections Program.
After providing written informed consent, participants completed a structured interviewer-administered questionnaire using computer-assisted personal interviewing technology. The interview assessed socio-demographics, patterns of drug use and associated risk behaviours, health status and health behaviours, and experiences of travel to and drug use in Mexico. Testing for HIV and HCV was performed using the Uni-Gold Recombigen (Trinity Biotech PLC, Bray, Ireland), and OraQuick® (OraSure Technologies, Bethlehem, USA) rapid antibody testing kits, respectively. Positive HIV test results were confirmed with a second rapid antibody test (OraQuick ADVANCE®, OraSure Technologies, Bethlehem, USA), and confirmatory testing conducted by the San Diego County Public Health Laboratory (Robertson et al., 2014). Pre- and post-test counselling was provided, and participants with positive test results were referred to health services. Participants completed behavioural and biological testing bi-annually for two years, and were reimbursed $25 for completion of baseline interview and serologic testing, with escalating incentives for follow-up visits.
Measures
The primary measures of interest for this analysis were recent (past six month) cross-border IDU (yes vs. no) and HIV and HCV antibody seropositivity (yes vs. no; assessed using rapid testing as described above). Although an incidence analysis would be a more informative way to assess the relationship between cross-border IDU and infectious diseases transmission, current serostatus was selected as the primary outcome as there was a high baseline prevalence of HCV, some loss to follow-up, and preliminary data analysis suggested a low incidence of both HIV and HCV, limiting power to conduct such analyses.
Recent (past six month) injecting risk behaviours were secondary measures of interest. Four risk behaviours known to be associated with HIV and/or HCV risk, or with reduced likelihood of safe and hygienic injecting practices (Fuller et al., 2003; Marshall, Kerr, Qi, Montaner, & Wood, 2010; Palmateer et al., 2013; Pouget, Hagan, & Des Jarlais, 2012; Tim Rhodes et al., 2006) were examined: (1) receptive syringe sharing; (2) sharing of cotton, cookers or water; (3) injecting in a public place; and (4) injecting in a shooting gallery. Receptive syringe sharing and sharing of cotton/cookers /water in San Diego were derived from participants’ responses on a 5-point Likert Scale (Never/Less than half the time/About half the time/More than half the time/Always); however, in relation to drug use in Mexico, these questions were asked with binary (yes vs. no) response categories. As such, responses regarding drug use in San Diego were dichotomised to enable comparisons. Injecting in a public place was defined as injecting in any of the following locations: construction site, alleyway, on the street, vacant lot, park, freeway overpass, bridge, or canyon.
Our analysis of potential correlates of cross-border IDU was exploratory in nature and was informed by a risk environment framework (T. Rhodes, 2002). We focused on individual and socio-environmental variables as these have been associated with a variety of drug use behaviours in this setting, including cross-border IDU (e.g. Munoz, Burgos, Cuevas-Mota, Teshale, & Garfein, 2015; Ramos et al., 2009; Volkmann et al., 2011; K. D. Wagner et al., 2012). These included sociodemographic characteristics (age, sex, country of birth, ethnic identity, educational attainment, marital status, income, homelessness, incarceration history, and recent arrest) and drug use characteristics (age at first injection, duration of injecting, patterns of heroin, cocaine and methamphetamine injecting in the past six months, engagement in drug treatment, and perceptions about the price and purity of heroin and methamphetamine, the most commonly used drugs among the sample). As previous qualitative research highlighted the importance of familiarity with the border region in cross-border drug use (K. D. Wagner et al., 2012) we also examined participants’ connections to, and perceptions about Mexico, including: duration of residence in San Diego, Spanish language proficiency (spoken), ever residing in Mexico, having family or friends in Mexico, knowing PWID who live in Mexico, knowing PWID in San Diego who have travelled to Mexico to buy or use drugs, having a current passport, perceptions and level of concern about risk of violence in Mexico, and familiarity with the Mexican drug law reform. Familiarity with Mexican drug laws was assessed using the following questions: “Has anyone ever told you that you are not subject to arrest or detention if you are carrying a small amount of drugs considered for personal use?” and if ‘yes’, “Where does this law apply?” Participants were coded as being familiar with Mexican drug law reform if they answered ‘yes’ to the first question and correctly reported that this law applied in Mexico only. Participants who did not know about decriminalisation or incorrectly reported that this law applied in the U.S. alone or in both U.S. and Mexico were coded as being unfamiliar with the Mexican drug law reform. These questions were added to the survey part-way through baseline data collection; participants who were not asked (n=232, 41%) were coded as ‘Question not asked’ for this analysis.
Data analysis
This analysis draws on baseline quantitative interviews from the cohort. Seven participants with missing data on recent cross-border IDU were excluded from analysis, resulting in sample of 567 participants.
Descriptive statistics were used first to examine baseline characteristics of the sample, cross-border IDU characteristics, HIV and HCV seroprevalence, and engagement in injecting risk behaviours.
To address our primary aim, we used logistic regression to test for associations between recent cross-border IDU and HIV and HCV seroprevalence, and identify independent correlates of recent cross-border IDU. Bivariate logistic regression models were run to assess the association between cross-border IDU and HIV and HCV seroprevalence, as well as socio-demographics, drug use characteristics, and participants’ connections to, and perceptions about Mexico. As this was an exploratory analysis, we used a statistically-driven approach to build a parsimonious multivariable model. We began with all variables where p<0.2 in bivariate analysis. After removing multicollinear variables, we used a backwards stepwise process to eliminate variables until we reached a final model that retained only significant variables (all p-values <0.05). We ran both a complete model including all variables considered in bivariate analysis and a series of additional models where hypothesised important confounders were retained in the multivariable model, however findings did not change appreciably (data not shown).
To better understand the results of the primary analysis, we conducted two secondary analyses. First, we compared self-reported engagement in injecting risk behaviours between PWID who did and did not report recent cross-border IDU using chi-squared tests. Second, we compared self-reported engagement in injecting risk behaviours during injection events in San Diego and Mexico among those who reported cross-border IDU. For this analysis, we grouped participants into four mutually exclusive categories: 1) those who engaged in a specified risk behaviour in both San Diego and Mexico; 2) those who engaged in the risk behaviour in neither setting; 3) those who did so in San Diego, but not in Mexico; and 4) those who did so in Mexico, but not in San Diego. McNemar tests for paired nominal data were used to compare these categories. These tests assess discordant pairs only (i.e. groups three and four above). Significance for all tests was set at p<0.05. All analyses were conducted using Stata 13.1 (Statacorp LP, TX, USA).
Results
Participant characteristics
The sample was predominantly male (73%; Table 1), U.S.-born (93%), with a median age of 45 years (Range: 18–70 years). One-third of participants (31%) identified as Hispanic or Latino/a, among whom 80% identified as Mexican. One-quarter (25%) had ever lived in Mexico. The median duration of injecting among the cohort was 20 years (Interquartile Range [IQR]: 9–32 years). Around half (56%) reported daily IDU at the time of interview, with heroin and methamphetamine the most commonly injected drugs.
Table 1.
Bivariate analysis of serological testing results, sociodemographic characteristics, drug use characteristics, and connections to and perceptions about Mexico associated with recent cross-border injection drug use among people who inject drugs residing in San Diego (N=567)
| Variable | Total N=567 n (%) |
Recent cross-border IDU
|
Unadjusted Odds Ratio (95% CI) | p- value | |
|---|---|---|---|---|---|
| No N=481 n (%) |
Yes N=86 n (%) |
||||
|
| |||||
| Serological testing | n=5451 | n=460 | n=85 | ||
|
| |||||
| HIV seropositive2 | 51 (9) | 44 (10) | 7 (8) | 0.85 (0.37–1.95) | 0.699 |
|
| |||||
| HCV seropositive2 | 358 (66) | 302 (66) | 56 (66) | 1.01 (0.62–1.65) | 0.967 |
|
| |||||
| Socio-demographic characteristics | |||||
|
| |||||
| Age, Median (IQR) | 45 (33– 52) | 45 (35– 53) | 38 (27– 49) | 0.96 (0.95–0.98) | <0.001 |
|
| |||||
| Sex | |||||
| Female | 148 (26) | 130 (27) | 18 (21) | 1 | |
| Male (incl. transgender) | 419 (74) | 351 (73) | 68 (79) | 1.40 (0.80–2.44) | 0.237 |
|
| |||||
| Country of Birth | |||||
| USA | 531 (94) | 448 (93) | 83 (97) | 1 | |
| Other | 36 (6) | 33 (7) | 3 (3) | 0.49 (0.15–1.64) | 0.247 |
|
| |||||
| Identify as Hispanic or Latino/a2 | 177(31) | 156 (32) | 21 (24) | 0.67 (0.40–1.14) | 0.141 |
|
| |||||
| Marital status | |||||
| Single/never married | 308 (54) | 254 (53) | 54 (63) | 1 | |
| Married/common law/other3 | 259 (56) | 227 (47) | 32 (37) | 0.66 (0.41–1.06) | 0.088 |
|
| |||||
| Highest level of school completed | |||||
| Grade 11 or below | 361 (64) | 308 (64) | 53 (62) | 1 | |
| Grade 12 or higher | 206 (36) | 173 (36) | 33 (38) | 1.11 (0.69–1.78) | 0.669 |
|
| |||||
| Income amount (last 12m) | |||||
| <$10,000 | 384 (68) | 330 (69) | 54 (63) | 1 | |
| ≥$10,000 | 181 (32) | 149 (31) | 32 (37) | 1.31 (0.81–2.12) | 0.265 |
|
| |||||
| Main income source (last 6m) | |||||
| Employed with regular salary | 77 (14) | 65 (14) | 12 (14) | 1 | |
| Public assistance/disability | 149 (26) | 131 (27) | 18 (21) | 0.74 (0.34–1.64) | 0.463 |
| Selling drugs/running drugs/touting | 35 (6) | 27 (6) | 8 (9) | 1.60 (0.59–4.37) | 0.354 |
| Other | 302 (54) | 255 (53) | 47 (55) | 1.00 (0.50–1.99) | 0.996 |
|
| |||||
| Homeless (last 6m)2 | 345 (61) | 288 (60) | 57 (66) | 1.32 (0.81–2.13) | 0.263 |
|
| |||||
| Ever incarcerated in U.S.2 | 512 (90) | 434 (91) | 78 (91) | 0.94 (0.43–2.09) | 0.886 |
|
| |||||
| Arrested (last 6m)2 | 154 (27) | 123 (26) | 31 (36) | 1.63 (1.00–2.64) | 0.050 |
|
| |||||
| Drug use characteristics | |||||
|
| |||||
| Age at first injection, Median (IQR) | 20 (17– 26) | 20 (17– 26) | 20 (17– 24) | 0.96 (0.93–0.99) | 0.016 |
|
| |||||
| Duration of injecting, Median (IQR) | 20 (9– 32) | 21 (10– 32) | 16 (6–30) | 0.99 (0.97–1.00) | 0.091 |
|
| |||||
| Typically injected ≥ daily (last 6m)2 | 316 (56) | 265 (56) | 51 (60) | 1.19 (0.75–1.91) | 0.459 |
|
| |||||
| Injected heroin ≥ daily (last 6m)2 | 212 (39) | 174 (38) | 38 (45) | 1.36 (0.85–2.17) | 0.201 |
|
| |||||
| Injected MA ≥ weekly (last 6m)2 | 221 (40) | 182 (39) | 39 (46) | 1.30 (0.82–2.08) | 0.263 |
|
| |||||
| Injected cocaine ≥ weekly (last 6m)2 | 18 (3) | 11 (2) | 7 (8) | 3.76 (1.41–10.00) | 0.008 |
|
| |||||
| Heroin/cocaine co–injection (last 6m)2 | 91 (19) | 73 (18) | 18 (22) | 1.25 (0.70–2.24) | 0.448 |
|
| |||||
| Heroin/MA co-injection (last 6m)2 | 110 (24) | 81 (21) | 29 (37) | 2.21 (1.32–3.73) | 0.003 |
|
| |||||
| Ever prescribed opioid substitution therapy2 | 134 (24) | 109 (23) | 25 (31) | 1.50 (0.89–2.52) | 0.125 |
|
| |||||
| Perceived heroin price increase (last 6m)2 | 84 (20) | 68 (19) | 16 (23) | 1.19 (0.64–2.21) | 0.582 |
|
| |||||
| Perceived heroin purity decrease (last 6m)2 | 263 (46) | 212 (63) | 51 (71) | 1.41 (0.81–2.45) | 0.226 |
|
| |||||
| Perceived MA price increase (last 6m)2 | 106 (25) | 93 (26) | 13 (20) | 0.71 (0.37–1.36) | 0.297 |
|
| |||||
| Perceived MA purity decrease (last 6m)2 | 250 (44) | 212 (58) | 38 (58) | 0.98 (0.58–1.66) | 0.939 |
|
| |||||
| Connections to and perceptions about Mexico | |||||
|
| |||||
| Years lived in San Diego, Median (IQR) | 25 (12– 40) | 27 (13– 42) | 17 (8–28) | 0.97 (0.95–0.98) | <0.001 |
|
| |||||
| Proficient in Spanish (spoken)2 | 162 (29) | 138 (29) | 24 (28) | 0.96 (0.58–1.60) | 0.882 |
|
| |||||
| Ever lived in Mexico 2 | 137 (25) | 94 (20) | 43 (50) | 4.01 (2.48–6.48) | <0.001 |
|
| |||||
| Have family and/or friends in Mexico2 | 205 (36) | 151 (32) | 54 (63) | 3.64 (2.26–5.87) | <0.001 |
|
| |||||
| Know at least one PWID who lives in Mexico1 | 161(30) | 107 (23) | 54 (64) | 5.71 (3.49–9.34) | <0.001 |
|
| |||||
| Know at least one person from San Diego who has bought or used drugs in Mexico2 | 383 (76) | 312 (74) | 71 (87) | 2.32 (1.18–4.53) | 0.014 |
|
| |||||
| Have a current passport2 | 68 (12) | 53 (11) | 15 (17) | 1.70 (0.91–3.18) | 0.097 |
|
| |||||
| Read/heard media about drug-related violence in Mexico (past 6m)2 | 419 (79) | 345 (77) | 74 (86) | 1.82 (0.95–3.49) | 0.070 |
|
| |||||
| Concerned about risk of violence when travelling to Mexico2 | 256 (51) | 220 (53) | 36 (42) | 0.66 (0.41–1.05) | 0.082 |
|
| |||||
| Familiar with Mexican drug law reform2,4 | 10 (2) | 6 (1) | 4 (5) | 3.67 (1.00–13.46) | 0.050 |
Excludes 22 participants who did not complete testing;
Yes vs. no;
Other includes separated, divorced and widowed participants;
Question added part-way through baseline data collection–denominator includes 232 participants coded as ‘question not asked’ (data not shown)
Missing data excluded.
Abbreviations: IQR = Interquartile Range; MA = methamphetamine; PWID = people who injects drugs
Overall, 86% of participants (n=486) had ever travelled to Mexico, of whom 32% (n=154) had done so in the six months preceding interview, with a median of four trips (IQR: 2–20). Reasons for travel to Mexico included dining at restaurants (41%), enjoying the nightlife (38%), shopping (35%) and visiting family or friends (31%). Drug-related reasons for travel to Mexico were also common, with 41% ever purchasing illicit drugs, 34% using illicit drugs and 11% purchasing syringes in Mexico.
Correlates of recent cross-border IDU
Eighty-six participants (15% of the total sample; 56% of those who had travelled to Mexico in the past six months) had injected drugs in Mexico in the six months preceding interview. The most commonly injected drugs while in Mexico were heroin (70%), methamphetamine (45%) and powder cocaine (8%). Commonly reported motivations for purchasing drugs in Mexico were cheaper price (69%), greater availability (60%), and perceived better drug quality (48%).
Table 1 presents results from bivariate regression analyses. There were no significant differences between participants who did and did not report recent cross-border IDU in the seroprevalence of HIV (8% vs. 10%, Odds Ratio [OR]: 0.85, 95% Confidence Interval [CI]: 0.37–1.95) or HCV (66% in both groups, OR: 1.01, 95% CI: 0.62–1.65). Variables significantly associated with decreased odds of cross-border IDU were age, age at first injection, and duration of residence in San Diego. Variables associated with increased odds of recent cross-border IDU were injecting cocaine at least weekly in the past six months, heroin/methamphetamine co-injection in the past six months, having ever lived in Mexico, having family and/or friends in Mexico, knowing PWID who reside in Mexico, and knowing PWID from San Diego who have travelled to Mexico to buy or use drugs.
Variables independently associated with reduced odds of recent cross-border IDU in the final multivariable model (Table 2) were: age (Adjusted Odds Ratio [AOR]: 0.95, 95% CI: 0.93–0.98), identifying as Hispanic or Latino/a (AOR: 0.43, 95% CI: 0.23–0.82), and being concerned about risk of violence when travelling to Mexico (AOR: 0.57, 95% CI: 0.33–0.99). Variables independently associated with increased odds of recent cross-border IDU were injecting cocaine at least weekly (AOR: 3.98, 95% CI: 1.03–15.44), having ever lived in Mexico (AOR: 2.50, 95% CI: 1.39–4.50) and knowing PWID who reside in Mexico (AOR: 6.09, 95% CI: 3.35–11.07).
Table 2.
Multivariable logistic regression analysis of factors independently associated with recent cross-border injection drug use among people who inject drugs in San Diego (N=471)
| Variable1 | Adjusted Odds Ratio (95% CI) | p-value |
|---|---|---|
| Age (per 1-year increase) | 0.95 (0.93–0.98) | <0.001 |
| Identify as Hispanic or Latino/a2 | 0.43 (0.23–0.82) | 0.010 |
| Concerned about risk of violence when travelling to Mexico2 | 0.57 (0.33–0.99) | 0.046 |
| Injected cocaine ≥ weekly (last 6m)2 | 3.98 (1.03–15.44) | 0.046 |
| Ever lived in Mexico2 | 2.50 (1.39–4.50) | 0.002 |
| Know at least one PWID who lives in Mexico2 | 6.09 (3.35–11.07) | <0.001 |
Variables not included in model due to collinearity: Duration of injecting (collinear with age), duration of residence in San Diego (collinear with age), and have family and/or friends in Mexico (collinear with having ever lived in Mexico);
Yes vs. no
Missing data excluded
Abbreviations: PWID = people who injects drugs
Hosmer-Lemeshow Goodness-of-fit p=0.4198
Engagement in injecting risk behaviours in San Diego, stratified by recent cross-border IDU
Our secondary analysis aims were developed to examine the relationships between self-reported engagement in injecting risk behaviours and cross-border IDU, in order to better understand the relationships between cross-border IDU and HIV and HCV seropositivity.
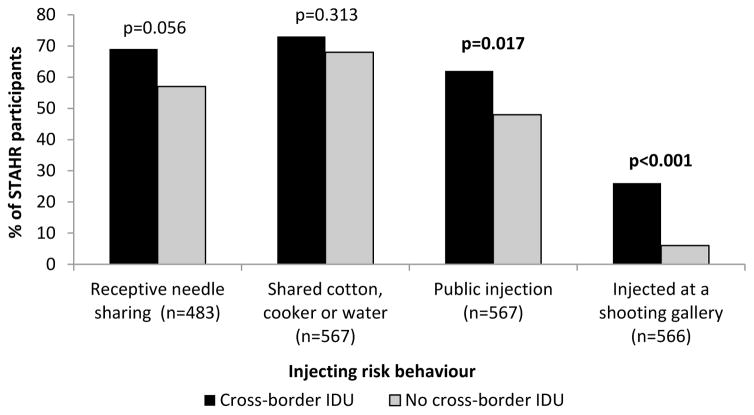
Among the complete sample (N=567), compared with PWID who did not report recent cross-border IDU, those who did were more likely to report public injection (62% vs. 48%, χ2 p=0.017), and injecting at a shooting gallery (26% vs. 6%, χ2 p<0.001; Figure 1). There were no statistically significant differences in receptive syringe sharing (69% vs. 57%, χ2 p=0.056) and ancillary equipment sharing (73% vs. 68%, χ2 p=0.313).
Figure 1. Risk behaviours practiced while injecting in San Diego, stratified by recent cross-border IDU (N=567).
χ2 p-values reported, significant results (p<0.05) bolded.
Engagement in injecting risk behaviours in San Diego and Mexico among those reporting cross-border IDU
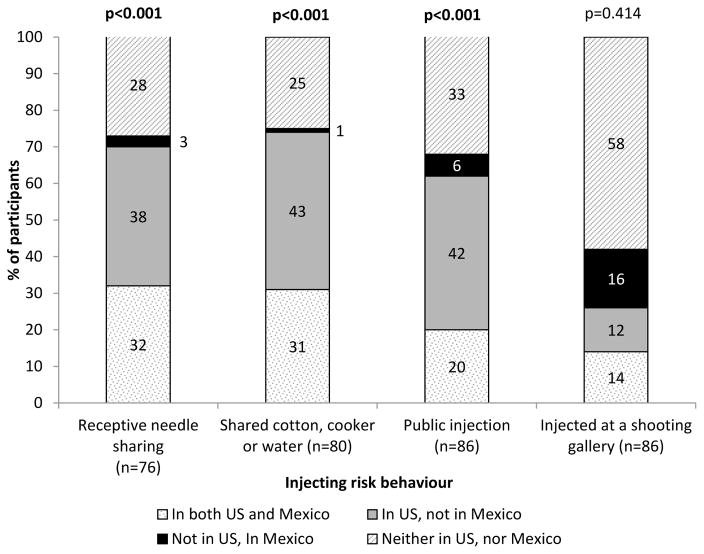
Among the 86 participants who reported recent cross-border IDU, two thirds (66%) of participants reported engaging in one or more injecting risk behaviours in Mexico in the six months preceding interview (median number of injecting risk behaviours engaged in: 1, IQR: 0–2). The most prevalent risk behaviour engaged in was receptive needle sharing (33%), followed by sharing injecting equipment (30%), public injection (26%) and injecting in a shooting gallery (26%). Thirty-two percent of participants reported engaging in receptive syringe sharing in both San Diego and Mexico, 31% shared injecting equipment, 20% reported public injection and 14% injected in a shooting gallery in both settings (Figure 2). The percentage of PWID who reported receptive syringe sharing, sharing injecting equipment and public injection while injecting in Mexico but not in San Diego was significantly lower than the percentage reporting engaging in these injecting risk behaviours while injecting in San Diego but not in Mexico (receptive syringe sharing: 3% reported this behaviour while in Mexico, but not in the U.S. vs. 38% in the U.S., but not in Mexico; sharing injecting equipment: 1% vs. 42%; public injection: 6% vs. 42%; McNemar’s p<0.001 for all comparisons; Figure 2). The proportion of PWID reporting shooting gallery use was similar in both groups (16% vs. 12%, McNemar’s p=0.414).
Figure 2. Risk behaviours practiced among participants reporting recent cross-border IDU, stratified by injecting location (N=86).
McNemar test p-values reported. McNemar test assesses discordant pairs only (i.e. includes only those who engaged in injecting risk behaviour in the U.S. but not in Mexico [coloured grey in figure], or in Mexico but not the U.S. [coloured black in figure]). Significant results (p<0.05) bolded.
Discussion
Among this large sample of PWID residing in the U.S.-Mexico border region, although travel to Mexico was common, only 15% of participants reported injecting drugs in Mexico in the six months preceding interview. The prevalence of recent cross-border IDU among this sample is comparable to earlier studies in this setting (Volkmann et al., 2011; K. D. Wagner et al., 2012). Despite concerns that U.S. PWID may be increasingly likely to travel to Mexico to inject drugs following the implementation of Mexico’s drug law reform, awareness of this reform was extremely low among our sample, with only 2% of participants familiar with this law (3% of those who answered this question) up to five years after implementation. It is possible that as an increasing number of U.S. PWID become aware of this law once it is better established, they may be more likely to travel to Tijuana to inject drugs. It is also possible, however, that changes in law and policing practice are unlikely to influence U.S. PWIDs’ decisions about whether or not to engage in cross-border drug use. A recent analysis exploring our study participants’ experiences with law enforcement in Mexico found that although they perceived it was likely they would be stopped by law enforcement and may be targeted for bribes, they felt they were unlikely to be arrested or detained (Wood et al., 2017). As the relationship between the Mexican drug law reform and cross-border IDU remains unclear, continued monitoring of patterns of cross-border IDU among U.S. PWID including future analysis of longitudinal data from the current study, will be important.
The prevalence of both HIV (9%) and HCV (66%) in our sample was higher than reported in previous studies in San Diego (Garfein et al., 2013; Gunn et al., 2003) but lower than national estimates (Nelson et al., 2011; Spiller, Broz, Wejnert, Nerlander, & Paz-Bailey, 2015). This likely reflects the older age and longer duration of injecting among our current sample, resulting in a higher cumulative risk of HIV/HCV.
Despite mobility being a known risk factor for infectious disease transmission, we found no significant associations between cross-border IDU and HIV or HCV seropositivity, consistent with previous research in this setting (Garfein et al., 2013; Volkmann et al., 2011). In international settings varying results have been reported, with no significant association between cross-border IDU and HIV seropositivity detected on the China-Vietnam border (Hammett et al., 2005), and a marginally significant association detected on the China-Myanmar border (Williams et al., 2011). These studies have conducted only cross-sectional analyses and are thus not able to examine associations between cross-border IDU and HIV/HCV seroconversion, which may yield different results. Longitudinal studies with large sample sizes are needed to conduct these more informative analyses.
Our findings regarding the lack of association between cross-border IDU and HIV/HCV seropositivity could be explained by our findings regarding engagement in injecting risk behaviours. Although participants who report cross-border IDU were significantly more likely to engage in risky injection behaviours in San Diego compared to those who did not, engagement in injecting risk behaviours in Mexico was relatively uncommon. Moreover, when we examined engagement in injecting risk behaviours in each location, we found that, with the exception of attending a shooting gallery (where there was no significant difference), a significantly smaller percentage reported engaging in risk behaviours in Mexico but not in the US compared to those engaging in risk behaviours in the US but not Mexico. Thus, injecting in Mexico does not appear to confer extra risk for HIV or HCV transmission. This is an important finding which shows that it is possible to practice safe injecting behaviours even in high-risk settings such as Tijuana.
There are several possible explanations for the finding that PWID practice fewer injecting risk behaviours in Mexico compared with in San Diego. First, recent evidence suggests that U.S. PWID injecting in Mexico take precautions to avoid drawing attention to themselves in order to minimise likelihood of police encounters (Wood et al., 2017); in particular this type of behaviour may explain the low prevalence of public injection and injecting at shooting galleries that we observed. Second, they may be aware of the high prevalence of HIV and HCV among local PWID populations and be fearful of becoming infected, so take extra precautions during injecting events that they do not take at home, either due to choice or barriers to syringe access. Third, they may have small injecting networks in Mexico or may be more likely to inject alone, reducing opportunities for syringe or other equipment sharing (De, Cox, Boivin, Platt, & Jolly, 2007). Fourth, they may not experience the same barriers to safe injecting as local PWID; for example, Mexican PWID report experiencing discrimination when attempting to purchase syringes at pharmacies (Davidson et al., 2012), a barrier which might not exist for U.S. PWID. There is a need for further research, particularly qualitative research, to better understand the contextual factors enabling U.S. PWID to inject safely in Mexico, given this finding conflicts with international literature which has found riskier injection behaviours among mobile populations (Rachlis et al., 2007). Future studies may inform harm reduction interventions which could be implemented on both sides of the border, particularly since over half of participants reported syringe sharing while at home in the U.S.
This study generated important findings regarding correlates of cross-border IDU in a highly mobile binational setting. First, PWID with established connections to Mexico (i.e. participants who had ever lived in Mexico; those who knew PWID residing in Mexico) were significantly more likely to engage in cross-border IDU, and those who were concerned about risk of violence when travelling to Mexico were significantly less likely to report cross-border IDU. As suggested in earlier qualitative research, this may reflect greater familiarity with the Mexican border context, lower risk perceptions and a greater level of comfort travelling to Mexico (K. D. Wagner et al., 2012). In recent years, travel through the San Diego-Tijuana border has become increasingly restrictive. For example, prior to 2015 a state-issued identification card (e.g. driver’s license) was sufficient documentation for crossing into the U.S., but a valid passport is now required (L. Wagner, 2015). Although some study participants reported crossing without a passport, and having a passport was not associated with cross-border IDU, it may be that those who are unfamiliar with the process perceive it to be complex and burdensome, deterring them from travel. Additionally, although around one-third of our sample reported that a reason they travelled to Mexico was to use illicit drugs, social reasons for travel to Mexico were also common. It is possible that PWID with established connections to Mexico travelled for social reasons and used illicit drugs opportunistically within social contexts, rather than travelling for the express purpose of using drugs. PWID with established connections to Mexico may also have a higher ‘comfort level’ with injecting in Mexico specifically, potentially being better able to navigate processes such as drug procurement and pharmacy syringe purchases.
Interestingly, participants who identified as Hispanic or Latino/a were less likely to report cross-border injecting, an association in the opposite direction from other ‘connections to Mexico’ variables. It is possible that these participants may be visibly perceived as Mexican and felt concerned about unwanted attention from police in Mexico, or experiencing problems when attempting to re-enter the U.S. (Sabo et al., 2014). Conversely, it is also possible that this reflects a sub-group of participants with few ties to Mexico, or perhaps to this region of Mexico in particular. Qualitative research may help to explain this unexpected finding.
Older participants in our study were less likely to report cross-border IDU. It is possible that older PWID perceive cross-border IDU as a high-risk practice; this finding would be consistent with previous research which found significant relationships between increasing age and lower engagement in high-risk injecting practices (Degenhardt et al., 2008; Horyniak et al., 2013). In our dataset, age was collinear with duration of residence in San Diego; it is possible that longer-term residents of San Diego may be less likely to engage in cross-border IDU due to entrenched negative perceptions of Tijuana resulting from high levels of drug-related violence in the late 2000’s (Heinle, Molzahn, & Shirk, 2015) or due to having more established connections to the San Diego drug market and, therefore less motivation to travel to Tijuana to purchase drugs (K. D. Wagner et al., 2012).
Finally, PWID who engaged in at least weekly cocaine injection were more likely to report cross-border IDU. There is some evidence of an increase in purity-adjusted price of cocaine in the U.S. (United Nations Office on Drugs and Crime, 2016). As most cocaine entering the U.S. is trafficked through Mexico (Bucardo et al., 2005), lower cocaine prices in Mexico could make cross-border IDU appealing to cocaine users specifically. Among the small number of participants reporting high-frequency cocaine injection, 86% reported cheaper price as a reason for buying drugs in Mexico, supporting this theory. Given cocaine injection has been associated with high risk of HIV acquisition (Tavitian-Exley, Vickerman, Bastos, & Boily, 2015; Tyndall et al., 2003), cocaine injectors who travel to Mexico may be particularly at risk. Future research is needed to explore this association in more detail, and to assess whether there is a need for targeted interventions to reduce HIV risk among this group.
This study has some limitations. First, although we used multiple recruitment methods to minimise selection bias, participants were not systematically recruited into the study, so findings might not be generalisable to all PWID in San Diego. Second, as analyses were cross-sectional, temporal relationships between cross-border IDU and infectious disease seropositivity cannot be established. As noted earlier, although data were drawn from a prospective cohort study, preliminary analysis indicated a low incidence of both HIV and HCV. Options for future analyses measuring incidence rather than prevalence or potentially examining recent infections at baseline, which could provide a more informative assessment of the association between cross-border IDU and infectious disease transmission, are currently being explored and will be the focus of a forthcoming manuscript. Third, as our analysis of correlates of cross-border IDU was exploratory we used a statistically-driven approach to model building, which may be susceptible to Type 1 errors. Fourth, our survey relied on self-reported data on engagement in injecting risk behaviours, which may be subject to socially desirable responding. However, there is no reason to believe that this would differ between those who did and did not report cross-border IDU, so the effect of this bias would be a reduction in odds ratios toward null findings. Finally, we did not capture information about the frequency of injecting events in Mexico; it is possible that participants reported lower engagement in injecting risk behaviours during injecting events in Mexico compared with in San Diego because they had few injection events, and thus few opportunities to engage in these behaviours.
Conclusion
Recent cross-border IDU was relatively uncommon among PWID residing on the US-Mexico border region, and was not associated with HIV or HCV seropositivity. This may be due to PWID engaging in safer behaviours while injecting in Mexico. Qualitative research could shed light on contextual factors contributing to U.S. PWID injecting safely in Mexico.
Acknowledgments
Funding Sources This study was supported by the National Institutes of Drug Abuse (NIDA R01 DA031074). Dr. Horyniak is supported by the Australian National Health & Medical Research Council (Early Career Fellowship 1092077). Dr. Wagner and Dr. Armenta were supported by NIDA (K01 DA031031 - Wagner; Diversity Supplement R01 DA031074-01S1 - Armenta; T32 DA023356 - Armenta).
The funding bodies played no role in the study design, collection, analysis or interpretation of data, or preparation of the manuscript for publication.
Footnotes
Author contributions RG, KW and DH conceptualised the manuscript. DH conducted data analysis and wrote the initial draft of the manuscript. All authors commented and contributed text, and gave approval for the manuscript to be submitted.
Declarations of Interest The authors have no conflicts of interest to declare.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Brouwer KC, Case P, Ramos R, Magis-Rodriguez C, Bucardo J, Patterson TL, Strathdee SA. Trends in the Production and Trafficking and Consumption of Methamphetamine and Cocaine in Mexico. Substance Use and Misuse. 2006;41:707–727. doi: 10.1080/10826080500411478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bucardo J, Brouwer KC, Magis-Rodriguez C, Ramos R, Fraga M, Perez SG, … Strathdee SA. Historical Trends in the Production and Consumption of Illicit Drugs in Mexico: Implications for the Prevention of Blood Borne Infections. Drug and Alcohol Dependence. 2005;79:281–293. doi: 10.1016/j.drugalcdep.2005.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davidson PJ, Lozada R, Rosen PC, Macias A, Gallardo M, Pollini RA. Negotiating access: Social barriers to purchasing syringes at pharmacies in Tijuana, Mexico. International Journal of Drug Policy. 2012;23(4):286–294. doi: 10.1016/j.drugpo.2012.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De P, Cox J, Boivin JF, Platt RW, Jolly AM. The importance of social networks in their association to drug equipment sharing among injection drug users: a review. Addiction. 2007;102(11):1730–1739. doi: 10.1111/j.1360-0443.2007.01936.x. [DOI] [PubMed] [Google Scholar]
- Degenhardt L, Kinner SA, Roxburgh A, Black E, Bruno R, Fetherston J, Fry CL. Drug use and risk among regular injecting drug users in Australia: does age make a difference? Drug and Alcohol Review. 2008;27(4):357–360. doi: 10.1080/09595230701750643. [DOI] [PubMed] [Google Scholar]
- Fuller CM, Vlahov D, Latkin CA, Ompad DC, Celentano DD, Strathdee SA. Social circumstances of initiation of injection drug use and early shooting gallery attendance: implications for HIV intervention among adolescent and young adult injection drug users. Journal of Acquired Immune Deficiency Syndromes. 2003;32(1):86–93. doi: 10.1097/00126334-200301010-00013. [DOI] [PubMed] [Google Scholar]
- Garfein RS, Rondinelli A, Barnes RF, Cuevas J, Metzner M, Velasquez M, … Teshale EH. HCV infection prevalence lower than expected among 18–40-year-old injection drug users in San Diego, CA. Journal of Urban Health. 2013;90(3):516–528. doi: 10.1007/s11524-012-9728-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldenberg SM, Strathdee SA, Perez-Rosales MD, Sued O. Mobility and HIV in Central America and Mexico: a critical review. Journal of Immigrant and Minority Health. 2012;14(1):48–64. doi: 10.1007/s10903-011-9505-2. [DOI] [PubMed] [Google Scholar]
- Grove NJ, Zwi AB. Our health and theirs: forced migration, othering, and public health. Social Science and Medicine. 2006;62(8):1931–1942. doi: 10.1016/j.socscimed.2005.08.061. [DOI] [PubMed] [Google Scholar]
- Gunn RA, Murray PJ, Brennan CH, Callahan DB, Alter MJ, Margolis HS. Evaluation of screening criteria to identify persons with hepatitis C virus infection among sexually transmitted disease clinic clients: results from the San Diego Viral Hepatitis Integration Project. Sexually Transmitted Diseases. 2003;30(4):340–344. doi: 10.1097/00007435-200304000-00013. [DOI] [PubMed] [Google Scholar]
- Hammett TM, Johnston P, Kling R, Liu W, Ngu D, Tung ND, … Des Jarlais DC. Correlates of HIV status among injection drug users in a border region of southern China and northern Vietnam. Journal of Acquired Immune Deficiency Syndromes. 2005;38(2):228–235. doi: 10.1097/00126334-200502010-00016. [DOI] [PubMed] [Google Scholar]
- Heinle K, Molzahn C, Shirk DA. Drug violence in Mexico: Data and analysis through 2014. San Diego: University of San Diego; 2015. [Google Scholar]
- Hirsch JS. Labor migration, externalities and ethics: theorizing the meso-level determinants of HIV vulnerability. Social Science and Medicine. 2014;100:38–45. doi: 10.1016/j.socscimed.2013.10.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horyniak D, Dietze P, Degenhardt L, Higgs P, McIlwraith F, Alati R, … Burns L. The relationship between age and risky injecting behaviours among a sample of Australian people who inject drugs. Drug and Alcohol Dependence. 2013;132(3):541–546. doi: 10.1016/j.drugalcdep.2013.03.021. [DOI] [PubMed] [Google Scholar]
- Instituto Nacional de Salud Pública. Encuesta Nacional de Adicciones 2008. Cuernavaca, Mexico: Instituto Nacional de Salud Pública; 2008. [Google Scholar]
- Kamper-Jorgensen Z, Andersen AB, Kok-Jensen A, Kamper-Jorgensen M, Bygbjerg IC, Andersen PH, … Lillebaek T. Migrant tuberculosis: the extent of transmission in a low burden country. BMC Infectious Diseases. 2012;12:60. doi: 10.1186/1471-2334-12-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kramer MA, van Veen MG, de Coul EL, Geskus RB, Coutinho RA, van de Laar MJ, Prins M. Migrants travelling to their country of origin: a bridge population for HIV transmission? Sexually Transmitted Infections. 2008;84(7):554–555. doi: 10.1136/sti.2008.032094. [DOI] [PubMed] [Google Scholar]
- Lee E, Wilson CE, Lara-Valencia F, de la Parra CA, Van Schoik R, Patron-Soberano K, … Selee A. The State of the Border Report: A Comprehensive Analysis of the U.S.-Mexico Border. Washington D.C., USA: Mexico Institute, Woodrow Wilson International Center for Scholars; 2013. [Google Scholar]
- Li L, Assanangkornchai S, Duo L, McNeil E, Li J. Cross-border activities and association with current methamphetamine use among Chinese injection drug users (IDUs) in a China-Myanmar border region. Drug and Alcohol Dependence. 2014;138:48–53. doi: 10.1016/j.drugalcdep.2014.01.021. [DOI] [PubMed] [Google Scholar]
- Mackey TK, Werb D, Beletsky L, Rangel G, Arredondo J, Strathdee SA. Mexico's "ley de narcomenudeo" drug policy reform and the international drug control regime. Harm Reduction Journal. 2014;11(1):31. doi: 10.1186/1477-7517-11-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marshall BDL, Kerr T, Qi J, Montaner JSG, Wood E. Public injecting and HIV risk behaviour among street-involved youth. Drug and Alcohol Dependence. 2010;110(3):254–258. doi: 10.1016/j.drugalcdep.2010.01.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michalopoulos LM, Aifah A, El-Bassel N. A Systematic Review of HIV Risk Behaviors and Trauma Among Forced and Unforced Migrant Populations from Low and Middle-Income Countries: State of the Literature and Future Directions. AIDS and Behavior. 2016;20(2):243–261. doi: 10.1007/s10461-015-1014-1. [DOI] [PubMed] [Google Scholar]
- Munoz F, Burgos JL, Cuevas-Mota J, Teshale E, Garfein RS. Individual and socio-environmental factors associated with unsafe injection practices among young adult injection drug users in San Diego. AIDS and Behavior. 2015;19(1):199–210. doi: 10.1007/s10461-014-0815-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murià M, Chávez S. Shopping and Working in the Borderlands: Enforcement, Surveillance and Marketing in Tijuana, Mexico. Surveillance & Society. 2011;8(3):355–373. [Google Scholar]
- Nelson PK, Mathers BM, Cowie B, Hagan H, Des Jarlais D, Horyniak D, Degenhardt L. Global epidemiology of hepatitis B and hepatitis C in people who inject drugs: results of systematic reviews. Lancet. 2011;378(9791):571–583. doi: 10.1016/S0140-6736(11)61097-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palmateer NE, Hutchinson SJ, Innes H, Schnier C, Wu O, Goldberg DJ, Hickman M. Review and meta-analysis of the association between self-reported sharing of needles/syringes and hepatitis C virus prevalence and incidence among people who inject drugs in Europe. International Journal of Drug Policy. 2013;24(2):85–100. doi: 10.1016/j.drugpo.2012.08.006. [DOI] [PubMed] [Google Scholar]
- Philbin M, Pollini RA, Ramos R, Lozada R, Brouwer KC, Ramos ME, … Strathdee SA. Shooting Gallery Attendance among IDUs in Tijuana and Ciudad Juarez, Mexico: Correlates, Prevention Opportunities, and the Role of the Environment. AIDS and Behavior. 2008;12(4):552–560. doi: 10.1007/s10461-008-9372-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pouget ER, Hagan H, Des Jarlais DC. Meta-analysis of hepatitis C seroconversion in relation to shared syringes and drug preparation equipment. Addiction. 2012;107(6):1057–1065. doi: 10.1111/j.1360-0443.2011.03765.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rachlis B, Brouwer KC, Mills EJ, Hayes M, Kerr T, Hogg RS. Migration and transmission of blood-borne infections among injection drug users: Understanding the epidemiologic bridge. Drug and Alcohol Dependence. 2007;90(2–3):107–119. doi: 10.1016/j.drugalcdep.2007.03.014. [DOI] [PubMed] [Google Scholar]
- Rai T, Lambert HS, Borquez AB, Saggurti N, Mahapatra B, Ward H. Circular labor migration and HIV in India: exploring heterogeneity in bridge populations connecting areas of high and low HIV infection prevalence. Journal of Infectious Diseases. 2014;210(Suppl 2):S556–561. doi: 10.1093/infdis/jiu432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramos R, Ferreira-Pinto JB, Brouwer KC, Ramos ME, Lozada RM, Firestone-Cruz M, Strathdee SA. A tale of two cities: Social and environmental influences shaping risk factors and protective behaviors in two Mexico-US border cities. Health and Place. 2009;15(4):999–1005. doi: 10.1016/j.healthplace.2009.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rhodes T. The ‘risk environment’: a framework for understanding and reducing drug-related harm. International journal on drug policy. 2002;13:85–94. [Google Scholar]
- Rhodes T, Kimber J, Small W, Fitzgerald J, Kerr T, Hickman M, Holloway G. Public injecting and the need for ‘safer environment interventions’ in the reduction of drug-related harm. Addiction. 2006;101(10):1384–1393. doi: 10.1111/j.1360-0443.2006.01556.x. [DOI] [PubMed] [Google Scholar]
- Robertson AM, Garfein RS, Wagner KD, Mehta SR, Magis-Rodriguez C, Cuevas-Mota J, … Strathdee SA. Evaluating the impact of Mexico's drug policy reforms on people who inject drugs in Tijuana, B.C., Mexico, and San Diego, CA, United States: a binational mixed methods research agenda. Harm Reduction Journal. 2014;11:4. doi: 10.1186/1477-7517-11-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Romo H, Marquez R. Who’s Who across the U.S.-Mexico Border: Identities in Transition. In: Zartman IW, editor. Understanding Life in the Borderlands. Athens, USA: University of Georgia Press; 2010. [Google Scholar]
- Sabo S, Shaw S, Ingram M, Teufel-Shone N, Carvajal S, de Zapien JG, … Rubio-Goldsmith R. Everyday violence, structural racism and mistreatment at the US-Mexico border. Social Science and Medicine. 2014;109:66–74. doi: 10.1016/j.socscimed.2014.02.005. [DOI] [PubMed] [Google Scholar]
- San Diego Association of Governments. 2015 San Diego-Baja California Border Crossings and Trade Statistics: File Number 3400200. 2016 http://www.sandag.org/index.asp?projectid=451&fuseaction=projects.detail.
- Smith DM, Werb D, Abramovitz D, Magis-Rodriguez C, Vera A, Patterson TL, Strathdee SA. Predictors of needle exchange program utilization during its implementation and expansion in Tijuana, Mexico. American Journal on Addictions. 2016;25(2):118–124. doi: 10.1111/ajad.12326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spiller MW, Broz D, Wejnert C, Nerlander L, Paz-Bailey G. HIV infection and HIV-associated behaviors among persons who inject drugs--20 cities, United States, 2012. MMWR; Morbidity and Mortality Weekly Report. 2015;64(10):270–275. [PMC free article] [PubMed] [Google Scholar]
- Spradling PR, Xing J, Phippard A, Fonseca-Ford M, Montiel S, Guzman NL, … Waterman SH. Acute viral hepatitis in the United States-Mexico border region: data from the Border Infectious Disease Surveillance (BIDS) Project, 2000-2009. Journal of Immigrant and Minority Health. 2013;15(2):390–397. doi: 10.1007/s10903-012-9604-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strathdee SA, Lozada R, Ojeda VD, Pollini RA, Brouwer KC, Vera A, … Patterson TL. Differential effects of migration and deportation on HIV infection among male and female injection drug users in Tijuana, Mexico. PLoS ONE. 2008;3(7):e2690. doi: 10.1371/journal.pone.0002690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strathdee SA, Lozada R, Pollini RA, Brouwer KC, Mantsios A, Abramovitz DA, … Patterson TL. Individual, social, and environmental influences associated with HIV infection among injection drug users in Tijuana, Mexico. Journal of Acquired Immune Deficiency Syndromes. 2008;47(3):369–376. doi: 10.1097/QAI.0b013e318160d5ae. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strathdee SA, Magis-Rodriguez C, Mays VM, Jimenez R, Patterson TL. The emerging HIV epidemic on the Mexico-U.S. border: an international case study characterizing the role of epidemiology in surveillance and response. Annals of Epidemiology. 2012;22(6):426–438. doi: 10.1016/j.annepidem.2012.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tavitian-Exley I, Vickerman P, Bastos FI, Boily MC. Influence of different drugs on HIV risk in people who inject: systematic review and meta-analysis. Addiction. 2015;110(4):572–584. doi: 10.1111/add.12846. [DOI] [PubMed] [Google Scholar]
- Tyndall MW, Currie S, Spittal P, Li K, Wood E, O'Shaughnessy MV, Schechter MT. Intensive injection cocaine use as the primary risk factor in the Vancouver HIV-1 epidemic. AIDS. 2003;17(6):887–893. doi: 10.1097/01.aids.0000050859.71999.ae. [DOI] [PubMed] [Google Scholar]
- United Nations Office on Drugs and Crime. World Drug Report 2016, United Nations publication, Sales No. E.16.XI.7. Vienna: United Nations Office on Drugs and Crime; 2016. [Google Scholar]
- Volkmann T, Shin SS, Garfein RS, Patterson TL, Pollini RA, Wagner KD, … Strathdee SA. Border Crossing to Inject Drugs in Mexico Among Injection Drug Users in San Diego, California. Journal of Immigrant and Minority Health. 2011;14(2):281–286. doi: 10.1007/s10903-011-9462-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wagner KD, Moynihan MJ, Strathdee SA, Cuevas-Mota J, Clark M, Zuniga ML, … Garfein RS. The social and environmental context of cross-border drug use in Mexico: findings from a mixed methods study of young injection drug users living in San Diego, CA. Journal of Ethnicity in Substance Abuse. 2012;11(4):362–378. doi: 10.1080/15332640.2012.735182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wagner L. New Rules Go Into Effect At Busy U.S.-Mexico Border Crossing. NPR News. 2015 Aug 20; Retrieved from http://www.npr.org/sections/thetwo-way/2015/08/20/433155278/new-rules-go-into-effect-at-busy-u-s-mexico-border-crossing.
- Weine SM, Kashuba AB. Labor migration and HIV risk: a systematic review of the literature. AIDS and Behavior. 2012;16(6):1605–1621. doi: 10.1007/s10461-012-0183-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White EF, Garfein RS, Brouwer KC, Lozada R, Ramos R, Firestone Cruz M, … Strathdee SA. Prevalence of hepatitis C virus and HIV infection among injection drug users in two Mexican cities bordering the U.S. Salud Publica de Mexico. 2007;49(3):165–172. doi: 10.1590/S0036-36342007000300001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams CT, Liu W, Levy JA. Crossing over: drug network characteristics and injection risk along the China-Myanmar border. AIDS and Behavior. 2011;15(5):1011–1016. doi: 10.1007/s10461-010-9764-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wood EF, Werb D, Beletsky L, Rangel G, Cuevas Mota J, Garfein RS, … Wagner KD. Differential experiences of Mexican policing by people who inject drugs residing in Tijuana and San Diego. International Journal of Drug Policy. 2017;41:132–139. doi: 10.1016/j.drugpo.2016.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]