Abstract
Objective
To determine the lifetime and phase-specific cost of anal cancer management and the economic burden of anal cancer care in elderly (≥66 years) patients in the United States.
Methods
For this study, we used Surveillance Epidemiology and End Results-Medicare linked database (1992–2009). We matched newly diagnosed anal cancer patients (by age and sex) to non-cancer controls. We estimated survival time from the date of diagnosis until death. Lifetime and average annual cost by stage and age at diagnosis were estimated by combining survival data with Medicare claims. The average lifetime cost, proportion of patients who were elderly, and the number of incident cases were used to estimate the economic burden.
Results
The average lifetime cost for patients with anal cancer was US$50,150 (N=2,227) (2014 US dollars). The average annual cost in men and women was US$8,025 and US$5,124, respectively. The overall survival after the diagnosis of cancer was 8.42 years. As the age and stage at diagnosis increased, so did the cost of cancer-related care. The anal cancer-related lifetime economic burden in Medicare patients in the US was US$112 million.
Conclusion
Although the prevalence of anal cancer among the elderly in the United States is small, its economic burden is considerable.
Keywords: Cost analysis, anal cancer, SEER-Medicare, lifetime cost
Introduction
The estimated number of people who will be diagnosed with and die from anal cancer in the United States in 2014 is 7,210 and 950, respectively.1–3 Data from the Surveillance Epidemiology and End Results (SEER) program show that the incidence of anal cancer rapidly increased from 1973 to 2009 from 1.2 to 2.8 cases per 100,000.4
Cost is an important consideration when seeking cancer care that accounts for approximately 6% of the total healthcare expenditures in the United States.5 In health services research, cost information is required for economic evaluation studies, burden of disease studies, and budget impact analyses. The current available estimates of the cost of anal cancer treatment and the economic burden of anal cancer in the United States6 were approximated from a 2003 Canadian costing study,7 and these estimates are now outdated. The direct medical care costs and economic burden of anal cancer using US-based data have never been estimated.
In the present study, we estimated the total and disease-specific per-patient lifetime costs as well as the economic burden of anal cancer management in the United States using a phase-based model of cancer care for elderly patients. The SEER-Medicare data were used to create descriptive cost profiles corresponding to the episode of care during anal cancer treatment. The costs were estimated by patients’ disease stage and age at diagnosis. The costs were characterized by age and disease stage because treatment guidelines and the aggressiveness of treatment and screening are age and disease stage dependent.
Material and Methods
Overview
We estimated the average lifetime and phase-specific costs and economic burden of anal cancer treatment and surveillance using a methodology similar to that applied in prior cancer studies.8,9 We first estimated survival time for patients with anal cancer from the date of diagnosis until their death or the end of the follow-up period, which was defined as the end of Medicare claims. We then divided the period of time after the initial diagnosis of anal cancer into the following phases of treatment: (1) initial care, (2) continuation care, and (3) terminal care. Anal cancer-related costs were estimated using age- and sex-matched controls who were assigned the same index date (i.e., both cases and controls were monitored from the date of cancer detection until their death or the end of Medicare claims). The average lifetime cost, the proportion of the patients who were 66 years or older from the SEER statistics, and the number of incident cases as determined from American Cancer Society data were used to estimate the lifetime economic burden associated with anal cancer in patients ≥66 years and older in the United States.
Patient population
We used the SEER-Medicare data to obtain information on survival and Medicare payments for the patients diagnosed with stage I–IV anal cancer from 1992 to 2009. The 15 SEER registries collect detailed information about cancer incidence and survival in defined geographic areas, including clinical, demographic, and cause-of-death data for persons with cancer. Of the US population, 25% is included in the SEER registries. The SEER program selects high-quality cancer registries that represent diverse geographic areas across the United States.
Medicare data are longitudinal and include claims for all covered fee-for-service health care from the time of eligibility until death. The Medicare data are divided across 8 files and contain claims data for hospitalization, physician care, home health, hospice, etc. All Medicare claims contain information about dates of service, procedures, and diagnoses. Diagnoses are coded using International Classification of Diseases-9th revision diagnosis codes. Procedures are coded using International Classification of Diseases-9th revision procedure codes, Current Procedural Terminology/Healthcare Common Procedure Coding System codes, and Revenue Center codes. The details of the SEER-Medicare database are provided elsewhere.10
To be included in the study, patients must have been 66 years or older and enrolled in Medicare at the time of diagnosis, must have had continuous Parts A and B coverage during the entire observation period, and must have had histologically confirmed anal cancer. Patients were excluded if they were enrolled in Medicare managed care, if they were diagnosed only at death, or if the month of their diagnosis was unknown.
The American Joint Committee on Cancer classification of malignant tumors (i.e., tumor, node, metastasis staging) was not available for the patients diagnosed between 1992 and 2004. A stage variable for those patients was created using the information on the size of the primary tumor, extent of spread to nearby lymph nodes, and tumor metastasis to other organs of the body (Please refer to the Supplementary Appendix 1).
The patient identification algorithm is presented in Supplementary Appendix 2.
Length of treatment phases and survival analysis
The major portions of cancer treatment costs are incurred in the initial phase when the disease is diagnosed and in the terminal phase when the physicians extend their efforts to improve the patient’s quality of life.
We examined three treatment phases—initial, continuation, and terminal care—as well as the entire longitudinal profile of each patient from the date of diagnosis to death. The initial phase of care included the primary course of therapy and any adjuvant therapy within the first 6 months of diagnosis. These services usually included surgery, radiation therapy, and chemoradiotherapy. The continuation phase included surveillance activities for detecting recurrence and new primary cancers. The complications deriving from the initial course of therapy after 6 months were included in the continuation phase. The continuation care phase started after the first 6 months of primary treatment for anal cancer and ended 1 year before death. The terminal care phase was defined as the last 12 months of life. For patients surviving less than 18 months, the final 12 months of follow-up were allocated to the terminal phase, and the preceding months were designated as the initial phase. Thus, the cost profile was allocated depending upon survival:
Survival longer than 18 months: first 6 months after diagnosis, initial phase; last 12 months before death, terminal phase; and the time between the initial and terminal phases, continuation phase.
Survival between 12 and 18 months: last 12 months of life, terminal phase; preceding months, initial phase.
Survival less than 12 months: all months were characterized as terminal phase.
For the patients diagnosed with stage I, II, or III disease who were still alive at the end of the study period, we assumed that their survival was comparable to that of the US general population. Age- and sex-specific data from the US life table11 were used to estimate these patients’ survival. For patients diagnosed with stage IV disease who were alive at the end of the study, we used a parametric regression model12 to estimate the median survival time since the life table method was not deemed appropriate to estimate the life expectancy of these patients, as their survival probability is much lower than that of the US general population. The model assumed that the survival time follows the Weibull distribution, and it used age and sex as independent variables to predict the median survival time.
Estimation of Lifetime Total and Anal Cancer-Related Treatment Costs
For the patients who died before the end of the study period, the lifetime costs (i.e., from the date of diagnosis until death) were estimated using the entire profile. The lifetime costs for the patients who were still alive at the end of the follow-up period were estimated by multiplying phase-specific monthly costs by the number of months a patient would spend in that phase. Mathematically, this can be expressed as the following:
where, MIC = months of initial care, ICC = average monthly initial care cost from population at age of patient, MCC = months of continuation care, CCC = average monthly continuation care cost from population at age of patient, MTC = months of terminal care, and TCC = average monthly terminal care cost from population at age of patient.
The patients with anal cancer were matched by age and sex to patients without cancer from a 5% sample of Medicare beneficiaries. This non-cancer cohort was used to estimate the background medical costs unrelated to anal cancer. The controls were assigned the same index date (i.e., both cases and controls were monitored from the date of diagnosis until death or the end of Medicare claims). The incremental difference in the average treatment phase costs between cases and controls was defined as anal cancer-related costs.
We used the Medicare payer perspective to conduct the analysis. All payments were adjusted to 2014 US dollars using Center for Medicare and Medicaid Services (CMS) market basket index levels.13 The Office of the Actuary, within the CMS, is responsible for producing the CMS market baskets, which are used to update payments and costs in the CMS payment systems. Two sets of market basket index levels—one for Medicare Part A and another for Part B—were used. Future costs were discounted using a 3% discount rate.
Estimation of economic burden
According to the American Cancer Society, there will be 7,210 incident anal cancer cases in 2014.2 We estimated the proportion of the patients who were 66 years or older from the SEER statistics (39.6% of the total incident cases were ≥ 66 years old). We then applied the proportion from the SEER statistics to the number of incident cases to estimate the number of incident cases that were 66 years and older. The number of incident cases was then multiplied by the lifetime anal cancer treatment cost estimates to calculate the aggregate total and anal cancer-related burden of medical care among patients who were 66 years or older. These estimates were adjusted for patient age. In addition, we also estimated age-specific values. The annual cost of anal cancer care in the United States was estimated by dividing the lifetime economic burden of anal cancer per patient by the average number of years a patient with anal cancer would survive.
Results
Patient demographics and survival
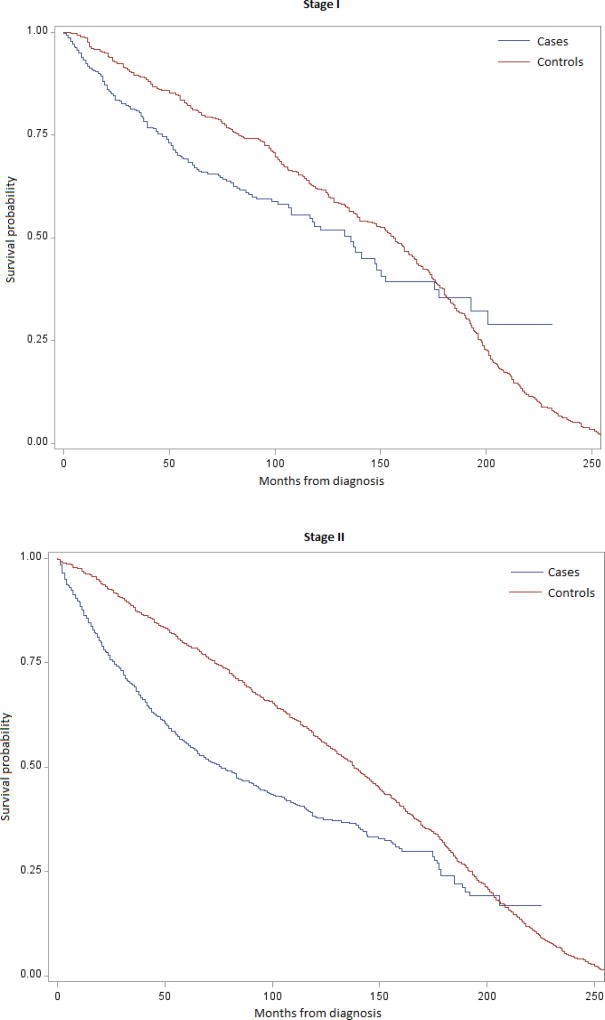
We identified 2,227 patients who met our selection criteria. Demographic characteristics and predicted survival of the patients are presented in Table 1. In Figure 1, we compared the stage-stratified differences in the survival probability of the cases and age- and sex-matched controls. We validated the results of survival analysis as our estimated 5-year survival probability approximated to those of the estimates by the American Cancer Society.14 Of the 2,227 patients, 19.04%, 53.61%, 18.77%, and 8.58% were diagnosed with stage I, stage II, stage III, and stage IV cancer, respectively. The majority of the patients were female, and most patients resided in the SEER west area. The overall mean survival time was 101.44 months. The predicted mean survival time among the patients with stage I, II, III, and IV disease was 134.93, 110.10, 84.21, and 11.08 months, respectively. The overall phase-specific survival time was 5.73 ± 1.08 months, 114.16 ± 82.25 months, and 10.83 ± 2.13 months for the initial, continuation, and terminal care phases, respectively. Similar to the overall survival time, the average phase-specific survival time was shortest among the patients with stage IV disease at diagnosis.
Table 1.
Demographic Characteristics and Survival by Disease Stage at Diagnosis
| Patient Characteristics | Stage I | Stage II | Stage III | Stage IV | All Patients | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| N, % | 424 | 19.04 | 1,194 | 53.61 | 418 | 18.77 | 191 | 8.58 | 2227 | 100.00 |
|
| ||||||||||
| Year of diagnosis, N, % | ||||||||||
| 1992–1999 | 84 | 19.82 | 291 | 24.37 | 70 | 16.75 | 27 | 14.14 | 472 | 21.20 |
| 2000–2004 | 167 | 39.39 | 524 | 43.89 | 141 | 33.73 | 63 | 32.98 | 895 | 40.19 |
| 2005–2009 | 173 | 40.80 | 379 | 31.74 | 207 | 49.52 | 101 | 52.88 | 860 | 38.62 |
|
| ||||||||||
| Sex, N, % | ||||||||||
| Male | 143 | 33.36 | 383 | 32.08 | 96 | 22.97 | 82 | 42.93 | 704 | 31.61 |
| Female | 281 | 66.27 | 811 | 67.92 | 322 | 77.03 | 109 | 57.07 | 1523 | 68.39 |
|
| ||||||||||
| Age at diagnosis | ||||||||||
| Mean (SD) | 75.62 | 6.86 | 76.65 | 7.25 | 77.10 | 7.11 | 77.33 | 7.33 | 76.60 | 7.17 |
| Median (range) | 74.04 | 66–100 | 75.59 | 66–102 | 76.67 | 66–104 | 76.50 | 66–97 | 75.59 | 66–104 |
| Age categories | ||||||||||
| 66–69 | 101 | 23.82 | 260 | 21.78 | 79 | 18.90 | 34 | 17.80 | 474 | 21.28 |
| 70–74 | 135 | 31.84 | 295 | 24.71 | 99 | 23.68 | 47 | 21.61 | 576 | 25.86 |
| 75–79 | 77 | 18.16 | 260 | 21.78 | 94 | 22.49 | 50 | 26.18 | 481 | 21.60 |
| ≥80 | 111 | 26.18 | 379 | 31.74 | 146 | 34.93 | 60 | 31.41 | 696 | 31.25 |
|
| ||||||||||
| SEER areas | ||||||||||
| Midwest | 41 | 9.67 | 155 | 12.98 | 53 | 12.68 | 26 | 13.61 | 275 | 12.35 |
| Northeast | 65 | 15.33 | 225 | 18.84 | 71 | 16.99 | 33 | 17.28 | 394 | 17.69 |
| South | 93 | 21.93 | 230 | 19.26 | 98 | 23.44 | 40 | 20.94 | 461 | 20.70 |
| West | 225 | 53.07 | 584 | 48.91 | 196 | 46.89 | 92 | 48.17 | 1097 | 49.26 |
|
| ||||||||||
| Predicted mean survival time (SD) in months | 135 | 87.13 | 110 | 88.30 | 84.21 | 86.12 | 11.08 | 5.86 | 101 | 89.57 |
|
| ||||||||||
| Phase specific mean survival time (SD) in months | ||||||||||
| Initial care | 5.91 | 0.97 | 5.61 | 1.33 | 4.51 | 2.23 | 5.73 | 1.08 | ||
| Continuation care | 131.92 | 81.95 | 103.37 | 81.84 | 23.28 | 26.23 | 114.16 | 82.25 | ||
| Terminal care | 11.66 | 2.54 | 10.33 | 3.55 | 7.02 | 4.50 | 10.83 | 2.13 | ||
SEER = Surveillance Epidemiological and End Results
SD = Standard deviation
Figure 1.
Two-hundred-fifty-month Survival Probability for Cases and Controls by Stage at Diagnosis
Phase-specific monthly treatment costs
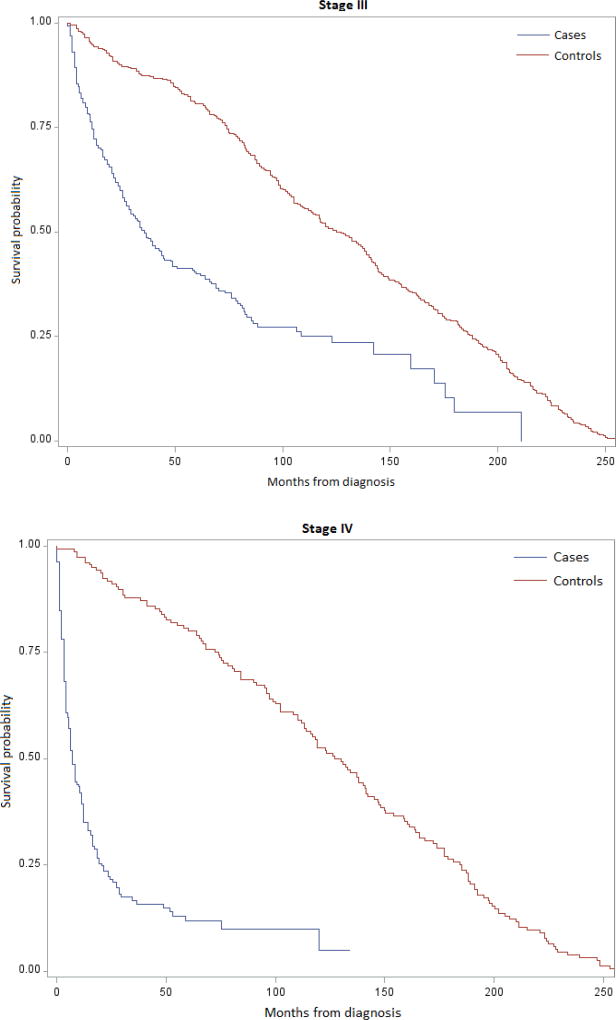
As expected, the average costs of initial monthly care and terminal monthly care were higher than the average cost of continuation monthly care in patients with stage I–III disease at diagnosis (Figure 2). The average monthly care costs in patients with stage IV disease at diagnosis were approximately three times higher than the average monthly care costs in patients with stage I–III disease at diagnosis. For male patients with stage I disease at diagnosis, no difference in continuation care cost was observed. With the increase in cancer stage at diagnosis, the average monthly initial, continuation, and terminal care cost increased.
Figure 2.
Excess Cancer-Related Health Care Costs (US$2014) per Month of Survival, by Cancer Stage
Total lifetime and anal cancer-related (excess) costs
Predicted survival, total lifetime costs, and anal cancer-related costs are presented by age and disease stage at diagnosis in Tables 3 and 4 for men, women, and all patients. The predicted average survival of the women aged 66–69 years, 70–74 years, 75–79 years, and 80 years and older exceeded the predicted average survival of the men by 4.31 years, 2.28 years, 0.75 years, and 0.88 years, respectively. The average anal cancer-related (excess) costs of care were higher for men than for women. For the age groups 66–69 years, 70–74 years, 75–79 years, and 80 years and older, the annual anal cancer-related cost of care for men was US$4,702, US$4,973, US$10,050, and US$21,912, respectively, and the annual anal cancer-related cost of care for women was US$1,970, US$2,575, US$6,759, and US$14,118, respectively. The overall average anal cancer-related cost per year in men and women was US$8,025 and US$5,124, respectively. The overall annual cost of care increased as patients’ ages increased.
Table 3.
Excess Lifetime Anal Cancer-Related Health Care Costs and Survival, by Cancer Stage (US$2014)*
| Men | |||||
| Study Measure | Stage I | Stage II | Stage III | Stage IV | All |
| Number of patients, N | 143 | 383 | 96 | 82 | 704 |
| Average total costs for cases, US$ | 133,792 | 141,297 | 123,913 | 95,019 | 132,011 |
| Average total costs for controls, US$ | 106,667 | 74,904 | 30,622 | 21,841 | 71,098 |
| Anal cancer-related lifetime costs, US$ | 27,125 | 66,393 | 93,291 | 73,178 | 60,913 |
| Average years of survival, y | 10.84 | 8.12 | 6.57 | 0.65 | 7.59 |
| Total costs per year, US$ | 12,342 | 17,401 | 18,860 | 146,183 | 17,393 |
| Anal cancer-related costs per year, US$ | 2,502 | 8,176 | 14,200 | 112,581 | 8,025 |
|
| |||||
| Women | |||||
| Study Measure | Stage I | Stage II | Stage III | Stage IV | All |
| Number of patients, N | 281 | 811 | 322 | 109 | 1523 |
| Average total costs cases, US$ | 114,957 | 138,172 | 138,638 | 96,656 | 131,015 |
| Average total costs for controls, US$ | 98,916 | 92,633 | 60,599 | 33,380 | 85,665 |
| Anal cancer-related costs, US$ | 16,041 | 45,539 | 78,039 | 63,276 | 45,350 |
| Average years of survival, y | 11.45 | 9.67 | 7.15 | 1.13 | 8.85 |
| Total costs per year, US$ | 10,040 | 14,289 | 19,390 | 85,536 | 14,804 |
| Anal cancer-related costs per year, US$ | 1,401 | 4,709 | 10,915 | 55,996 | 5,124 |
|
| |||||
| All Patients | |||||
| Study Measure | Stage I | Stage II | Stage III | Stage IV | All |
| Number of patients, N | 424 | 1194 | 418 | 191 | 2227 |
| Average total costs for cases, US$ | 121,309 | 139,174 | 135,256 | 95,954 | 131,331 |
| Average total costs for controls, US$ | 101,446 | 87,287 | 53,712 | 27,702 | 81,181 |
| Anal cancer-related costs, US$ | 19,863 | 51,887 | 81,554 | 68,252 | 50,150 |
| Average years of survival, y | 11.25 | 9.16 | 7.01 | 0.92 | 8.42 |
| Total costs per year, US$ | 10,783 | 15,194 | 19,294 | 104,297 | 15,597 |
| Anal cancer-related costs per year, US$ | 1,766 | 5,665 | 11,613 | 74,186 | 5,957 |
Future costs were discounted at a 3% discount rate
The predicted average survival in women exceeded the predicted average survival in men with stage I, II, III, and IV disease at diagnosis by 0.61 years, 1.55 years, 0.58 years, and 0.48 years, respectively. The average anal cancer-related costs and the average anal cancer-related cost per year were highest for both male and female patients with stage IV disease at diagnosis. The average total anal cancer-related cost in male patients diagnosed with stage I, stage II, stage III, and stage IV disease at diagnosis was US$27,125, US$66,393, US$93,291, and US$73,178, respectively, and in women, this cost was US$16,041, US$45,539, US$78,039, and US$63,276, respectively. The average anal cancer-related cost per year of survival in male patients diagnosed with stage I, II, III, and IV disease was US$2,502, US$8,176, US$14,200, and US$112,581, respectively, and in women, this cost was US$1,401, US$4,709, US$10,915, and US$55,996, respectively.
The large increase in the average annual cost of cancer care in stage IV patients was due to the relatively large cost of cancer-related care accrued over a short survival time. These costs were largely distributed in the initial and terminal phases of care.
Economic burden of anal cancer in elderly patients
In 2014, the proportion of patients diagnosed with anal cancer who are 66 years or older will be about 30.941%15; that is, approximately 2,230 new cancer cases will be identified among the elderly population. Aggregate lifetime total costs, anal cancer-related lifetime costs, and the annual cost of anal cancer care for these cases were estimated to be approximately US$293 million, US$112 million, and US$13 million, respectively. The aggregate (i.e., age-adjusted) and age-specific lifetime total costs, anal cancer-related lifetime costs, and the annual cost of anal cancer care are presented in the Supplementary Appendix 3.
Discussion
To our knowledge, this is the first study to estimate the direct anal cancer-related cost of care in the United States. We found that the lifetime total costs and lifetime anal cancer-related (excess) costs in the United States are substantial. The costs vary by the phase of cancer care, disease stage at diagnosis, and age at diagnosis. The costs of cancer care were higher among men than among women, although the average survival among men was shorter than that of women. As age and disease stage increased, the cost of cancer-related care increased. The overall average lifetime cancer-related cost was US$50,150, and the anal cancer-related lifetime economic burden in patients who were 66 years and older was approximately US$112 million. Compared to the overall cost of cancer care of $157 billion in the US,16 the anal cancer related burden is relatively small; however, given that anal cancer prevalence constitutes only 0.003% of all cancer sites,17 the economic burden of anal cancer in elderly patients is still substantial.
The higher costs of care in the patients who were diagnosed with stage IV cancer may indicate that these tumors require more intensive and expensive treatments. Moreover, the patients diagnosed with stage IV tumors had very short median survival times; therefore, the cost per year of survival was substantial relative to the patients diagnosed with stage I, II, and III tumors. This signifies the importance of earlier detection of cancer as a means of minimizing medical care expenditures.
We compared the costs of anal cancer care to other non-US published studies. Heitland et al. estimated the annual cost of hospitalization, inpatient rehabilitation, and sick leave of patients with anal cancer in Germany.18 Based on a retrospective cross-sectional analysis, the annual costs of anal cancer were €28.72 million (i.e., approximately US$40 million), of which almost 90% (i.e., US$36 million) were direct costs.18 A total of 5,774 hospitalizations were identified by Heitland et al.; therefore, the cost per hospitalization would be approximately US$62,000, which is much higher than the cost of anal cancer care in the United States. According to a study by Olsen et al.19, the total cost of anogenital cancer in the hospital sector in Denmark was estimated to be €7.7 million (i.e., approximately US$11 million) per year, a majority of which was attributed to anal and vulvar cancer. The total cost per patient per year was estimated to be €38,289 (i.e., approximately US$53,000), which approximates to the costs of anal cancer care in the United States as estimated in the present study. Another study in France estimated the economic burden of anal cancer management by evaluating hospitalization, outpatient, and daily allowance costs.20 According to this study, the costs of anal cancer management are high and are comparable to the costs of cervical cancer management.20 Our estimate of the annual cost of anal cancer care in the United States was $13 million, which is between the annual cost of anal cancer care in Germany and Denmark.
Ours is the first study to evaluate costs for anal cancer management and economic burden of anal cancer in the US. A previous study by Hu and Goldie approximated costs for anal cancer management from a Canadian costing study7 of rectal cancer management.6 The estimated discounted lifetime cost per anal cancer case was approximately US$27,660.6 The costs estimated by Hu and Goldie included diagnostic assessment, staging work-up, initial treatment, surveillance, treatment of recurrent disease, management of metastatic disease, and terminal care. Hu and Goldie also estimated the total lifetime cost of all human papillomavirus-attributable incidence of anal cancer in 2003 to be US$92 million (range, US$44 million–US$178 million).6 When the estimation of Hu and Goldie were inflated using consumer price indices,21 the estimated cost of anal cancer care in the United States in 2010 was determined to be US$38,011 (range, US$18,998–US$76,024) per patient, which underestimates the cost of anal cancer care. The estimates by Hu and Goldie take into account the population across all age groups. Our estimates, however, were limited to patients 66 years and older.
We found that majority of anal cancer cases (almost 50%) were residing in the SEER west region. This is because—(1) the West region has more sites than other SEER regions (SEER west region include San Francisco-Oakland, San Jose, Monterey, Los Angeles, and the rest of California; New Mexico; Seattle/Puget Sound; Utah). (2) Consistent with our findings, a study reported that patients in the West are at highest risk for anal cancer.22 Another study found that the patients residing in SEER West region are likely to have four fold higher risk of having an in situ anal tumor and 39% lower mortality risk than those reported from registries outside California.23 It has also been reported that the increased incidence of anal cancer in the West is attributed to the large proportion of men who have sex with men (MSM) residing in that region (with relative incidence of approximately 100 times high than the general population, MSM are known to be at highest risk of anal cancer).22,24 Similarly, it has also been reported that the incidence of anal cancer in women residing in the SEER West region is higher than the overall incidence of anal cancer in the US women.22
Our study is not without limitations. Like other claims analyses, our study was subject to potential coding errors and incomplete data. The costs of care pertained only to patients 66 years or older; therefore, although our findings may be generalizable to the US population of older anal cancer patients covered by Medicare, costs associated with anal cancer treatment and health services use may differ in younger patients, owing to their age and insurance coverage. The SEER-Medicare registries contain claims for only fee-for-services care. Since health maintenance organization enrollees comprise almost 14% of the Medicare population nationwide, the lack of claims data for them is a significant limitation of the database.10 Finally, indirect costs of care were not included in the study; the true economic burden of the disease cannot be determined by focusing only on direct medical care costs.
Despite these limitations, our findings have substantial implications. The costs estimated in this study could be used (1) as input in cost-effectiveness and budget impact analyses of anal cancer prevention and treatment alternatives and policy research, (2) as a component of the overall cancer-related economic burden, or (3) for shaping policy decisions. Used by itself, this study demonstrates the magnitude of the economic burden of anal cancer. Although the prevalence of the disease is relatively small compared to other cancers, its economic burden is considerable.
Supplementary Material
Table 2.
Excess Lifetime Anal Cancer-related Health Care Costs and Survival, by Age at Diagnosis (US$2014)*
| Men | |||||
| Study Measure | Age 66–69 | Age 70–74 | Age 75–79 | Age ≥ 80 | All |
| Number of patients, N | 181 | 199 | 147 | 177 | 704 |
| Average total costs for cases, US$ | 146,905 | 120,555 | 127,473 | 133,430 | 132,011 |
| Average total costs for controls, US$ | 97,959 | 75,553 | 58,429 | 52,539 | 71,098 |
| Anal cancer-related lifetime costs, US$ | 48,946 | 45,002 | 69,044 | 80,891 | 60,913 |
| Average years of survival, y | 10.41 | 9.05 | 6.87 | 3.69 | 7.59 |
| Total costs per year, US$ | 14,112 | 13,321 | 18,555 | 36,160 | 17,393 |
| Anal cancer-related costs per year, US$ | 4,702 | 4,973 | 10,050 | 21,921 | 8,025 |
|
| |||||
| Women | |||||
| Study Measure | Age 66–69 | Age 70–74 | Age 75–79 | Age ≥ 80 | All |
| Number of patients, N | 293 | 377 | 334 | 519 | 1523 |
| Average total costs cases, US$ | 133,297 | 132,903 | 128,028 | 130,280 | 131,015 |
| Average total costs for controls, US$ | 104,667 | 103,725 | 76,528 | 65,763 | 85,665 |
| Anal cancer-related costs, US$ | 28,630 | 29,178 | 51,503 | 64,517 | 45,350 |
| Average years of survival, y | 14.54 | 11.33 | 7.62 | 4.57 | 8.85 |
| Total costs per year, US$ | 9,168 | 11,730 | 16,802 | 28,508 | 14,804 |
| Anal cancer-related costs per year, US$ | 1,970 | 2,575 | 6,759 | 14,118 | 5,124 |
|
| |||||
| All Patients | |||||
| Study Measure | Age 66–69 | Age 70–74 | Age 75–79 | Age ≥ 80 | All |
| Number of patients, N | 474 | 576 | 481 | 696 | 2227 |
| Average total costs for cases, US$ | 138,493 | 128,637 | 127,858 | 131,081 | 131,331 |
| Average total costs for controls, US$ | 102,420 | 94,007 | 71,287 | 61,198 | 81,181 |
| Anal cancer-related costs, US$ | 33,073 | 34,630 | 56,571 | 69,883 | 50,150 |
| Average years of survival, y | 12.96 | 10.59 | 7.38 | 4.34 | 8.42 |
| Total costs per year, US$ | 10,686 | 12,147 | 17,325 | 30,203 | 15,597 |
| Anal cancer-related costs per year, US$ | 2,552 | 3,271 | 7,665 | 16,102 | 5,957 |
Future costs were discounted at a 3% discount rate
Acknowledgments
Role of the funding source:
This work was supported by the US National Cancer Institute (R01 CA163103), The Janice Davis Gordon Postdoctoral Fellowship in Colorectal Cancer Prevention, Duncan Family Institute, and the National Institutes of Health through The University of Texas MD Anderson Cancer Center Support Grant CA016672.
The authors wish to thank the anonymous reviewer for their valuable comments and suggestions, Jennifer M. Gatilao and Markeda Wade for editorial contributions that enhanced the quality of the manuscript.
This study used the Surveillance, Epidemiology and End Results (SEER)-Medicare linked database. The interpretation and reporting of these data are solely the responsibility of the authors. The authors acknowledge the efforts of the Applied Research Program, National Cancer Institute; the Office of Research, Development and Information, Centers for Medicare and Medicaid Services; Information Management Services Inc.; and the SEER Program tumor registries in creating the SEER-Medicare linked database.
References
- 1.DeSantis CE, Lin CC, Mariotto AB, et al. Cancer treatment and survivorship statistics, 2014. CA Cancer J Clin. 2014;64:252–71. doi: 10.3322/caac.21235. [DOI] [PubMed] [Google Scholar]
- 2.American Cancer Society. Cancer Facts and Figures 2014. American Cancer Society; 2014. [Google Scholar]
- 3.Siegel R, Ma J, Zou Z, et al. Cancer statistics, 2014. CA Cancer J Clin. 2014;64:9–29. doi: 10.3322/caac.21208. [DOI] [PubMed] [Google Scholar]
- 4.Nelson RA, Levine AM, Bernstein L, et al. Changing patterns of anal canal carcinoma in the United States. J Clin Oncol. 2013;31:1569–75. doi: 10.1200/JCO.2012.45.2524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Olin G, Rhoades J. Civilian Noninstitutionalized Population. Rockville, MD: Agency for Healthcare Research and Quality; 2005. The Five Most Costly Medical Conditions, 1997 and 2002: Estimates for the U.S. [Google Scholar]
- 6.Hu D, Goldie S. The economic burden of noncervical human papillomavirus disease in the United States. Am J Obstet Gynecol. 2008;198:500 e1–7. doi: 10.1016/j.ajog.2008.03.064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Maroun J, Ng E, Berthelot JM, et al. Lifetime costs of colon and rectal cancer management in Canada. Chronic Dis Can. 2003;24:91–101. [PubMed] [Google Scholar]
- 8.Ramsey SD, Berry K, Etzioni R. Lifetime cancer-attributable cost of care for long term survivors of colorectal cancer. Am J Gastroenterol. 2002;97:440–5. doi: 10.1111/j.1572-0241.2002.05483.x. [DOI] [PubMed] [Google Scholar]
- 9.Stokes ME, Ishak J, Proskorovsky I, et al. Lifetime economic burden of prostate cancer. BMC Health Serv Res. 2011;11:349. doi: 10.1186/1472-6963-11-349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Warren JL, Klabunde CN, Schrag D, et al. Overview of the SEER-Medicare data: content, research applications, and generalizability to the United States elderly population. Med Care. 2002;40:IV-3–18. doi: 10.1097/01.MLR.0000020942.47004.03. [DOI] [PubMed] [Google Scholar]
- 11.Arias E. National vital statistics reports U.S. Department of Health and Human Services Centers for Disease Control and Prevention National Center for Health Statistics National Vital Statistics System. 2014 [Google Scholar]
- 12.Allison PD. Survival Analysis Using SAS: A Practical Guide, Second Edition. Cary, NC: SAS Institute Inc.; 2010. [Google Scholar]
- 13.Center for Medicare and Medicaid Services. Actual regulation market basket change and Medicare payment updates as published in the "Federal Register", Market Basket Data. Baltimore, MD: 2014. [Google Scholar]
- 14.American Cancer Society. Survival rates for anal cancer by stage. 2014 [Google Scholar]
- 15.National Cancer Institute S, Epideiology, and End Results Program. SEER Stat Fact Sheets: Anal Cancer. 2014 [Google Scholar]
- 16.Mariotto AB, Yabroff KR, Shao Y, et al. Projections of the cost of cancer care in the United States: 2010–2020. J Natl Cancer Inst. 2011;103:117–28. doi: 10.1093/jnci/djq495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.SEER: Cancer statistics. National Cancer Institute; 2015. [Google Scholar]
- 18.Heitland W, Schadlich PK, Chen X, et al. Annual cost of hospitalization, inpatient rehabilitation and sick leave of anal cancer in Germany. J Med Econ. 2013;16:364–71. doi: 10.3111/13696998.2012.759582. [DOI] [PubMed] [Google Scholar]
- 19.Olsen J, Jorgensen TR, Kofoed K, et al. Incidence and cost of anal, penile, vaginal and vulvar cancer in Denmark. BMC Public Health. 2012;12:1082. doi: 10.1186/1471-2458-12-1082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Abramowitz L, Remy V, Vainchtock A. Economic burden of anal cancer management in France. Rev Epidemiol Sante Publique. 2010;58:331–8. doi: 10.1016/j.respe.2010.06.165. [DOI] [PubMed] [Google Scholar]
- 21.The United States Department of Labor, editor. Bureau of Labor Statistics. Consumer Price Index - All Urban Consumers. 2010. [Google Scholar]
- 22.Cress RD, Holly EA. Incidence of anal cancer in California: increased incidence among men in San Francisco, 1973–1999. Prev Med. 2003;36:555–60. doi: 10.1016/s0091-7435(03)00013-6. [DOI] [PubMed] [Google Scholar]
- 23.Amirian ES, Fickey PA, Jr, Scheurer ME, et al. Anal cancer incidence and survival: comparing the greater San-Francisco bay area to other SEER cancer registries. PLoS One. 2013;8:e58919. doi: 10.1371/journal.pone.0058919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Truong HM, Kellogg T, Klausner JD, et al. Increases in sexually transmitted infections and sexual risk behaviour without a concurrent increase in HIV incidence among men who have sex with men in San Francisco: a suggestion of HIV serosorting? Sex Transm Infect. 2006;82:461–6. doi: 10.1136/sti.2006.019950. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.