Abstract
Background
Increased upper lip procumbency is commonly associated with maxillary dentoalveolar protrusion with the major goal of reducing maxillary dentoalveolar protrusion. The treatment plan usually includes extraction of the maxillary first premolars, followed by retraction of anterior teeth with maximum anchorage. Dental implants have been widely accepted as successful adjuncts for obtaining maximum anchorage in orthodontic treatment.
Methods
50 subjects between the ages of 13 and 17 years having bimaxillary dentoalveolar protrusion were included in the study. The patients were divided into two groups. Both groups received treatment with 0.022″ MBT prescription preadjusted edgewise appliance system. In addition, subjects of Group ‘I’ received the Nance button and lingual arch as anchorage reinforcement in the upper and lower arches, respectively. Subjects of Group ‘II’ received self-drilling titanium OI for anchorage reinforcement.
Results
Significant retraction was achieved in all cases with good vertical control. Anchor loss was observed in both groups. Anchor loss was much higher in Group I compared to Group II, and an intergroup comparison for anchor loss was highly significant.
Conclusion
Implants as anchorage, for en masse retraction, can be incorporated into orthodontic practice. The use of orthodontic implants for anchorage is a viable alternative to conventional molar anchorage.
Keywords: Orthodontics, Anchorage, Bimaxillary protrusion, Implants
Introduction
Over the past two decades, dentistry has seen a dramatic increase in the use of dental implants. The vast majority of dental implant research is centered on the use of endosseous implants for replacement of missing teeth. Previously, the use of dental implants within the specialty of orthodontics was limited to integration of implants into treatment plans strictly to facilitate tooth replacement.
Integration of dental implants into contemporary orthodontic practice has advantages of serving as a method of increasing orthodontic anchorage, virtually eliminating patient compliance issues and occasionally permitting orthodontic treatments previously thought to be impossible without surgery.
The practice of clinical orthodontics is largely dependent on the availability of anchorage. According to Proffit,1 in treatment planning of orthodontics, it is simply not possible to consider only the teeth whose movement is desired. Reciprocal effects throughout the dental arches must be carefully analyzed, evaluated, and controlled. An important aspect of treatment is maximizing the tooth movement that is desired, while minimizing undesirable side effects.
Increased upper lip procumbency is commonly associated with maxillary dentoalveolar protrusion.2 Patients with this feature often seek orthodontic treatment to improve their facial esthetics. With the major goal of reducing maxillary dentoalveolar protrusion, the treatment plan usually includes extraction of the maxillary first premolars, followed by retraction of anterior teeth with maximum anchorage.3
There are numerous ways in which orthodontics has tried to augment anchorage, including auxiliary devices, such as headgear, transpalatal arches, Nance button, and other appliances. Many of these appliances like headgears are extraoral and are awkward or uncomfortable for patients, often leading to less than desired levels of compliance. Thus, treatment outcomes may become compromised.
In recent years, the concept of using dental implants has been widely accepted as successful adjuncts for obtaining maximum anchorage in orthodontic treatment.
The present study was carried out with the aim of evaluating the efficacy of orthodontic implant (OI) as anchorage reinforcement method when compared with conventional intraoral methods for anchorage reinforcement.
The objectives of this study were:
-
(i)
To quantify the amount of anchor loss if any by using intraoral anchorage enhancement.
-
(ii)
To compare the amount of anchor loss if any in patients treated with conventional intraoral methods with OIs.
-
(iii)
To compare the time taken for space closure in both the methods of anchorage reinforcement.
Materials and methods
This research was carried out after a formal approval from the ethical committee of the institution. This study included all bimaxillary protrusion cases reporting to this orthodontic center between April 2009 and September 2009.
The original sample consisted of 57 subjects between the ages of 13 and 17 years seeking orthodontic treatment and clinically and radiographically diagnosed as having bimaxillary dentoalveolar protrusion. All patients had lip incompetence ≥4 mm. From this group, 50 subjects with the following additional inclusion criteria were selected:
-
(a)
Bimaxillary proclination with Angles Class I molar relation. ANB angle from 1° to 3°.
-
(b)
No indication for orthognathic surgical intervention for correction of the malocclusion.
-
(c)
Need for extraction of all four first bicuspids to be carried out as confirmed by clinical examination, cephalometric analysis, and model analysis in order to achieve the desired facial changes.
-
(d)
Need for maximum anchorage. Presence of permanent dentition.
-
(e)
No congenitally missing permanent teeth (except for the third molars).
-
(f)
No history of deleterious oral habits or previous orthodontic treatment.
-
(g)
Absence/unrestorable teeth due to caries/periodontal disease. Absence of any systemic illness.
Standard orthodontic diagnostic records comprising of study models, lateral cephalograms, orthopantomogram, and intra- and extraoral photographs were taken for all patients.
All patients and/or their parents were informed about the purpose of this study and a written consent was obtained. Maximum anchorage was predicted on the need to restrict mesial movement of posterior teeth to have a Class I molar relation and an optimal overjet and overbite at the end of orthodontic treatment. Two patients did not agree to participate in this study and therefore were not included. In addition, one patient moved out to another city and hence was excluded from the study.
Those who fulfilled the inclusion criteria and agreed to take part were allocated alternately to Group I – the conventional anchorage group, or Group II – the OI group.
Both groups received treatment with 0.022″ MBT prescription preadjusted edgewise appliance system; molar tubes were welded to preformed first molar bands and therapeutic extraction of all first premolar teeth.
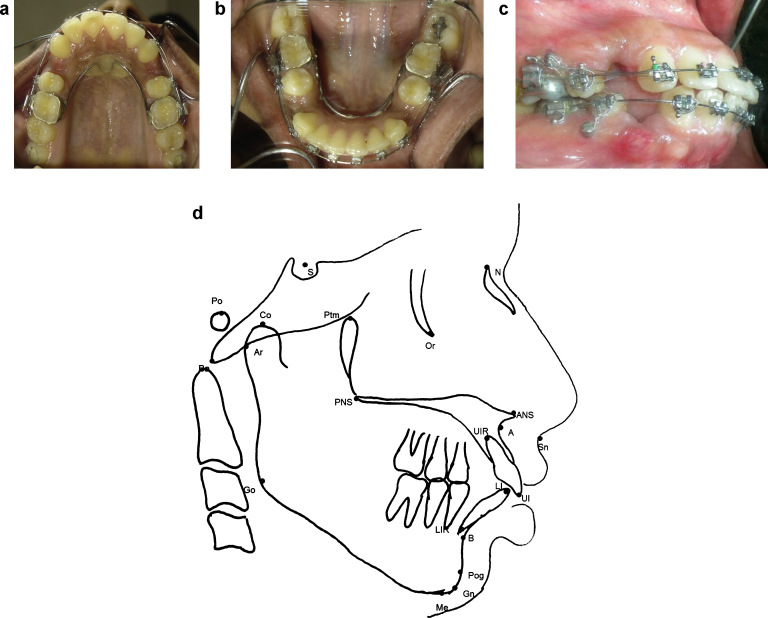
In addition, subjects of Group ‘I’ received Nance button and lingual arch as anchorage reinforcement in upper and lower arches, respectively (Fig. 1a and b). Subjects of Group ‘II’ received self-drilling titanium OI for anchorage reinforcement (Fig. 1c). The OIs were placed in the buccal alveolar bone in the region of the attached gingiva, between the second premolars and first molars in all the four quadrants.
Fig. 1.
(a) Nance button in situ. (b) Lingual arch in situ. (c) Indirect anchorage with OI. (d) Skeletal, dental and soft tissue landmarks used in cephalometric analysis.
All OIs were inserted by a single operator. Prior to insertion, an intraoral periapical radiograph was taken of the interdental space between the maxillary second premolar and maxillary first molar using a paralleling technique to assess root angulations and the amount of interradicular bone present between the roots of the adjacent teeth.
Stability and mobility of the inserted mini-screw implants was checked with the help of cotton tweezers by holding the head of the mini-screw and gently applying lateral force. If there was any discernible mobility, the OI was considered to have failed. A postinsertion periapical radiograph was taken for each case to confirm the position of the implant.
All patients were recalled 3 days after insertion to check the OI for mobility, swelling, or acute inflammation with discharge. The OIs were checked for stability and were ligated to the premolar bracket with a 0.010-in. stainless steel ligature wire.
Leveling and alignment of the dental arches in both the groups was carried out until 0.019 in. × 0.025 in. stainless steel archwires were placed. En masse retraction was undertaken using Nitinol closed coil springs, which were engaged from the molar tube hooks to the canine power arms to provide a continuous force of 150 g.
Follow-up appointments were scheduled after 3 days and 7 days of placement of the OI and subsequently every 3–5 weeks until the desired amount of tooth movement had been achieved. At each appointment, the implants were assessed to be a success or a failure. The force level was maintained and clinical observations made. Orthodontic adjustments were completed as necessary. The same clinician made the observations and determinations of success or failure in every patient. On completion of space-closure phase, customary orthodontic treatment proceeded without interruption.
All pretreatment and postretraction cephalometric lateral cephalograms were taken by a single operator using the same cephalostat and subsequently hand traced on acetate paper. The landmarks were marked (Fig. 1d; Table 1) and predetermined cephalometric angular and linear measurements (Table 2) were recorded.
Table 1.
Definition of skeletal, dental, and soft tissue landmarks used in manual cephalometric analysis.
| S. No. | Landmark | Abbreviation | Definition |
|---|---|---|---|
| Skeletal | |||
| 1. | Nasion | N | Most anterior point of frontonasal suture in the median plane. |
| 2. | Sella | S | Midpoint of the hypophyseal fossa. |
| 3. | Point A | A | Deepest midline point in the curved bony outline from the base to the alveolar process of maxilla. |
| 4. | Anterior nasal spine | ANS | Tip of the bony anterior nasal spine in the median plane. |
| 5. | Posterior nasal spine | PNS | Intersection of the continuation of the anterior wall of the pterygopalatine fossa and the floor of the nose. |
| 6. | Basion | Ba | Lowest point on the anterior margin of the foramen magnum in the median plane. |
| 7. | Condylion | Co | Superior most point on the head of the condyle. |
| 8. | Articulare | Ar | Point of intersection of the posterior margin of ascending ramus and the outer margin of the cranial base. |
| 9. | Point B | B | The deepest point of concavity between chin and superior aspect of mandibular alveolar process. |
| 10. | Pogonion | Pog | Most anterior point of the chin. |
| 11. | Gnathion | Gn | Most anteroinferior point of the chin. |
| 12. | Menton | Me | Most inferior point of the chin. |
| 13. | Gonion | Go | Most posterior and inferior point on outline of mandibular angle. |
| 14. | Orbitale | Or | Lowermost point of the orbit. |
| 15. | Porion | Po | Uppermost point of the external auditory meatus. |
| 16. | Pterygoid vertical | PTV | Line that passes through the pterygomaxillary fissure and is perpendicular to the Frankfurt Plane. |
| Dental | |||
| 17. | Upper central incisor | UI | The most labial point on the crown of the maxillary central incisor. |
| 18. | Lower central incisor | LI | The most labial point on the crown of the mandibular central incisor. |
| 19. | Upper first molar | U6 | The mesiobuccal cusp tip of the maxillary first permanent molar. |
| 20. | Lower first molar | L6 | The mesiobuccal cusp tip of the mandibular first permanent molar. |
| Soft tissue | |||
| 21. | Soft tissue pogonion | Pog’ | The most anterior point on the chin in the mid saggital plane. |
| 22. | Lower lip anterior/labrale inferius | LL/Li | Most anterior point of lower lip. |
| 23. | Nasal tip/pronasal | NT/Pn | The most anterior point of the nose. |
| 24. | Subnasal | Sn | The point at which the columella (nasal septum) merges with the upper lip in the mid saggital plane. |
Table 2.
Cephalometric parameters measured.
| S. No. | Cephalometric parameter | Abbreviation | Definition |
|---|---|---|---|
| Skeletal | |||
| 1. | SNA | SNA | The inferior posterior angle formed by the intersection of lines SN and NA. |
| 2. | SNB | SNB | The inferior posterior angle formed by the intersection of lines SN and NB. |
| 3. | ANB | ANB | Difference between SNA and SNB. |
| 4. | Na perpendicular to point A | N perp-A | Perpendicular distance between nasion perpendicular and point A. |
| 5. | Na perpendicular to Pog | N perp-Pog | Perpendicular distance between nasion perpendicular and pogonion. |
| Dental | |||
| 6. | U1–NA (°) | U1-NA (°) | Angle formed by long axis of most prominent upper incisor (U1) and NA plane. |
| 7. | U1 to NA (mm) | U1-NA (mm) | Linear distance between long axis of most prominent upper incisor and NA plane. |
| 8. | PTV to U6 (mm) | PTV-U6 (mm) | Distance from the pterygoid vertical to mesiobuccal cusp of maxillary first molar. |
| 9. | L1 to NB (degree) | L1-NB (°) | Angle formed by long axis of most prominent lower incisor (L1) and NB plane. |
| 10. | L1 to NB (mm) | L1-NB (mm) | Linear distance between long axis of most prominent lower incisor and NB plane. |
| 11. | PTV to L6 (mm) | PTV-L6 (mm) | Distance from the pterygoid vertical to mesiobuccal cusp of mandibular first molar. |
| 12. | U1 to L1 (angle) | U1-L1(°) | Angle formed by long axis of most prominent upper incisor and between long axis of most prominent lower incisor. |
| Growth pattern | |||
| 13. | Saddle angle | Saddle angle | Angle formed by nasion, sella, and articulare. |
| 14. | Articulare angle | Articulare angle | Angle formed by sella, articulare, and gonion. |
| 15. | Gonial angle | Gonial angle | Angle formed by articulare, gonion, and menton. |
| 16. | Sum of Saddle, Articulare and Gonial angle | Sum (Bjork angle) | Sum of saddle, articulare, and gonial angles. |
| 17. | FMA | FMA | Angle formed by Go-Me plane and Frankfort horizontal plane. |
| 18. | Go-Gn to Sn | Go-Gn to Sn | Angle formed by Go-Gn plane and sella nasion plane. |
| Soft tissue | |||
| 19. | Nasolabial angle | Nasolabial angle | Angle formed by columella and philtrum of upper lip. |
| 20. | Lower lip to E line/inferior E plane | Li-E line | Linear distance between E line and lower lip anterior/labrale inferius. |
On achieving desired angulation and inclination of teeth and optimum overjet and overbite, debonding and debanding of the cases was done. The implant was removed at this appointment by engaging the screwdriver and turning it in the anticlockwise direction, without the use of any local anesthesia. Retainers were given to the patients. The Nance button and lingual arch were also removed at the time of debonding/debanding.
The cephalometric measurements were made at the start of the treatment (T1) and on completion of treatment (T2). Anchorage loss was assessed by the difference (T2–T1) of pterygoid vertical to mesiobuccal cusp of maxillary first molar (U6) and pterygoid vertical to mandibular first and mandibular arch, respectively. Treatment duration was calculated by comparing the time taken between T1 and T2. Comparisons were made within the two groups and between the two groups.
Descriptive data that included means and standard deviations were calculated for linear and angular parameters. Pre- and post-treatment measurements were carried out twice, 3 weeks apart, on retraced cephalometric radiographs in order to rule out measurement error. In order to rule out the fractional differences in repeat measures (if any), the mean value of the two measurements was taken as the final value. All the analysis of data was performed with this final value. Comparisons of within group changes (pretreatment versus post-treatment) were undertaken using a paired t-test. Change between Group I and Group II was undertaken using an independent sample's t-test. For comparing the mean values of the variables between the two groups, Student's unpaired t-test was performed for each variable and Bonferroni's modified adjusted p values were also calculated. A ‘p’ value of less than or equal to 0.05 (95% level of confidence interval) was set for statistical significance. The data were analyzed using Statistical Package for Social Sciences Version 17.0.
Results
Each group had 12 male and 13 female patients. The mean age of patients at the start of treatment in both groups was well matched (Table 3).
Table 3.
Demographic information of the 50 subjects in this study.
| Group I | Group II | |
|---|---|---|
| Patients (number) | 25 | 25 |
| Mean age (years) | 15.08 ± 1.53 | 15.12 ± 1.42 |
| Mean age (years) females | 14.62 ± 1.26 | 15 ± 1.29 |
| Mean age (years) males | 15.58 ± 1.67 | 15.25 ± 1.60 |
| Mean treatment duration (months) | 21.76 ± 1.54 | 21.16 ± 1.62 |
The sum of the first maxillary premolar width for each patient was calculated by adding the first maxillary premolar width of the right and left sides and a mean of the value was taken as the first maxillary premolar width for that patient. A similar method was employed for the first mandibular premolar width for each patient. The difference in premolar width for both groups was not statistically significant (Table 4, Table 5).
Table 4.
Mean first premolar width.
| Group I | Group II | |
|---|---|---|
| Mean premolar width (in mm) | ||
| Maxilla | 7.12 ± 0.87 | 7.00 ± 0.50 |
| Mandible | 7.00 ± 0.48 | 7.00 ± 0.49 |
| Mean treatment duration (months) | ||
| Females | 21.62 ± 1.80 | 21.07 ± 1.81 |
| Males | 21.92 ± 1.24 | 21.25 ± 1.48 |
| Mean anchor loss (%) | ||
| Maxilla | 28.08 | 2.86 |
| Mandible | 30.00 | 2.86 |
Table 5.
Comparison of mean first premolar width (two group's unpaired Student's t-test).
| SD | t | p | Bonferroni adj p | |
|---|---|---|---|---|
| Mean premolar width (maxilla) | 2.087 | 0.575 | 0.57 | 0.571 |
| Mean premolar width (mandible) | 1.544 | 0.065 | 0.94 | 0.949 |
Though the mean time taken for treatment in Group I was marginally more than in Group II (Table 3), it was not statistically significant (Table 4). The mean time taken in females in both groups was less than males for the corresponding groups (Table 4).
In Group I, one patient had inflammation associated with the Nance button and two patients reported with gingival overgrowth over the anterior region of the lingual arch.
In Group II, five of the OI failed in three patients, two implants each in two patients and one implant in the third patient; two of these patients were females and one was a male. One implant in maxilla and two in mandible of females failed. One implant, each of maxilla and mandible of the male subject, failed. The overall success rate was 95.24% for all implants (100 of 55 OI). Three implants failed in the mandible. Four of the implants that failed were of the right side of the patient. Peri-implantitis was observed with all the failed implants.
Anchor loss was observed in both groups. Expectedly, the anchor loss was much higher in Group I compared to Group II and an intergroup comparison for anchor loss was highly significant (Table 6).
Table 6.
Intergroup comparisons for anchor loss and treatment duration (two group unpaired Student's t-test).
| SD | t | p | Bonferroni adj p | |
|---|---|---|---|---|
| Percentage of anchor loss (maxilla) | 9.413 | 14.034 | 0.05 | 0.054 |
| Percentage anchor loss (mandible) | 12.494 | 10.830 | 0.04 | 0.048 |
| Duration of treatment | 2.432 | 1.233 | 0.22 | 0.229 |
Significant retraction was achieved in all cases with good vertical control (Table 7). The anchor loss for maxilla in Group I was 2.00 ± 0.65 mm (28.08%) and in Group II it was 0.20 ± 0.35 mm (2.86%). The anchor loss for mandible in Group II was 2.10 ± 0.75 mm (30%) and in Group II it was 0.20 ± 0.35 mm (2.86%). The percentage of anchor loss was derived from values obtained by subtracting the anchor loss as measured in millimeters (mm) from the pterygoid vertical to the mesiobuccal cusp tip of the first molar from the mean first premolar width of the respective arch (i.e. maxillary or mandibular).
Table 7.
Mean pre- and post-treatment cephalometric changes.
| S. No. | Variable | Group | Pretreatment mean ± SD | Post-treatment mean ± SD | Change (pre–post) mean ± SD | p value for change between groups | p value for change within groups |
|---|---|---|---|---|---|---|---|
| 1. | SNA | I | 82.36 ± 4.39 | 82.24 ± 4.28 | 0.12 ± 0.33 | 0.03 | 0.61 |
| II | 81.80 ± 3.24 | 81.32 ± 3.25 | 0.48 ± 0.71 | 0.44 | |||
| 2. | SNB | I | 77.36 ± 4.22 | 77.24 ± 4.28 | 0.12 ± 0.33 | 0.16 | 0.55 |
| II | 76.72 ± 3.29 | 76.44 ± 3.38 | 0.28 ± 0.46 | 0.47 | |||
| 3. | ANB | I | 5.00 ± 0.82 | 5.00 ± 0.76 | 0.00 ± 0.29 | 0.18 | 0.78 |
| II | 5.08 ± 1.19 | 4.96 ± 1.02 | 0.12 ± 0.33 | 0.88 | |||
| 4. | N Perp A | I | −0.64 ± 02.36 | −0.76 ± 2.30 | 0.12 ± 0.36 | 0.18 | 0.12 |
| II | 0.36 ± 02.04 | 0.08 ± 2.08 | 0.28 ± 0.46 | 0.18 | |||
| 5. | N Perp Pog | I | −6.84 ± 3.93 | −6.72 ± 3.90 | −0.12 ± 0.39 | 0.02 | 0.80 |
| II | −6.56 ± 3.93 | −6.76 ± 4.04 | −0.20 ± 0.50 | 0.97 | |||
| 6. | U1-NA (°) | I | 42.32 ± 6.37 | 35.20 ± 5.83 | 7.12 ± 1.51 | 0.8 | 0.12 |
| II | 40.68 ± 5.06 | 33.44 ± 5.24 | 7.24 ± 1.05 | 0.36 | |||
| 7. | U1-NA (mm) | I | 8.68 ± 2.80 | 6.52 ± 2.37 | 2.16 ± 1.03 | 0.6 | 0.80 |
| II | 8.36 ± 2.252 | 6.06 ± 1.77 | 2.30 ± 0.92 | 0.86 | |||
| 8. | Li-NB (°) | I | 36.08 ± 4.743 | 31.48 ± 4.38 | 6.76 ± 1.44 | 0.3 | 0.32 |
| II | 35.68 ± 3.84 | 28.48 ± 3.57 | 7.20 ± 1.56 | 0.60 | |||
| 9. | L1-NB (mm) | I | 7.16 ± 2.29 | 5.24 ± 1.84 | 1.92 ± 0.73 | 0.3 | 0.66 |
| II | 7.84 ± 2.51 | 5.68 ± 2.21 | 2.16 ± 0.75 | 0.08 | |||
| 10. | Saddle angle | I | 125.08 ± 6.78 | 125.0 ± 6.78 | 0 | 0 | 0.74 |
| II | 124.48 ± 4.00 | 124.48 ± 4.00 | 0 | 0.70 | |||
| 11. | Articulare angle | I | 144.08 ± 7.97 | 144.08 ± 7.97 | 0 | 0 | 0.32 |
| II | 145.24 ± 6.03 | 145.24 ± 6.03 | 0 | 0.56 | |||
| 12. | Gonial angle | I | 118.24 ± 7.57 | 119.28 ± 7.81 | −1.04 ± 0.93 | 0 | 0.71 |
| II | 123.20 ± 6.25 | 123.36 ± 6.197 | −0.16 ± 0.37 | 0.05 | |||
| 13. | Bjorks angle | I | 387.40 ± 6.29 | 388.44 ± 6.55 | −1.04 ± 0.94 | 0 | 0.02 |
| II | 392.84 ± 8.22 | 393.00 ± 8.22 | −0.16 ± 0.37 | 0.20 | |||
| 14. | FMA | I | 21.20 ± 5.49 | 22.08 ± 5.71 | −0.88 ± 0.78 | 0 | 0.01 |
| II | 24.32 ± 7.15 | 24.48 ± 7.11 | −0.16 ± 0.37 | 0.53 | |||
| 15. | Go-Gn SN | I | 25.16 ± 6.27 | 25.88 ± 6.42 | −0.72 ± 0.61 | 0 | 0.09 |
| II | 27.12 ± 8.93 | 27.28 ± 8.96 | −0.16 ± 0.37 | 0.31 | |||
| 16. | Nasolabial angle | I | 81.68 ± 5.27 | 88.48 ± 5.55 | −6.8 ± 1.41 | 0.04 | 0.37 |
| II | 81.64 ± 3.03 | 89.16 ± 3.18 | −7.5 ± 0.87 | 0.10 | |||
| 17. | Lower lip -E line | I | 3.24 ± 1.51 | 0.58 ± 1.59 | 2.66 ± 0.79 | 0.79 | 0.97 |
| II | 2.96 ± 1.37 | 0.24 ± 1.67 | 2.72 ± 0.78 | 0.05 | |||
| 18. | Pterygoid vert to U6 | I | 19.56 ± 2.29 | 21.56 ± 2.26 | 2 ± 0.65 | 0.05 | 0.50 |
| II | 20.16 ± 1.84 | 20.36 ± 1.80 | 0.20 ± 0.35 | 0.00 | |||
| 19. | Pterygoid vert to L6 | I | 21.96 ± 2.15 | 24.06 ± 1.94 | 2.10 ± 0.75 | 0.05 | 0.37 |
| II | 19.88 ± 1.74 | 20.08 ± 1.72 | 0.20 ± 0.35 | 0.10 |
Discussion
The success rate of the OI in the present study was 90.9%. Five implants failed during the study in three patients, two females and one male. The implant failures included three implants in the mandible and two in the maxilla. Four implants of the right side failed and one on the left side. Peri-implantitis was observed with all the failed implants. Hence, suboptimal oral hygiene could have been a contributing factor for failure of the OIs. In the present study, none of the OIs fractured during placement and removal. When the OIs failed, new ones were placed into a neighboring area.
In the present study, the overall success rate of the OIs was higher than the 37.0% reported by Kim and Choi,4 70% by Fritz et al.,5 78.6% by Moon,6 70.73% reported by Garfinkle et al.,7 83.33% reported by Chopra et al.,8 83.9–85.0% by Miyawaki et al.,9 81.1% reported by Kuroda et al.,10 83.8% by Moon,11 and 85.7% by Chen et al.12 However, the success rate in the present study was similar to the 80.0–93.6% reported by Park et al.13
In the present study, males had a higher success rate than females, unlike the studies of Moon et al.,11 Park et al.,13 and Miyawaki et al.,9 who found that gender was not related to the clinical success of the OI.
The findings in the present study were similar to that of Park et al.13 who reported a higher screw survival rate in the maxilla. However, in a study by Miyawaki et al.,9 they found more success in the mandible than in the maxilla.
In the present study, the success rate of OIs for the left side was higher compared to that on the right side. This is in agreement with the results of Park et al.13 who reported that the left side had a significantly higher success rate than the right side. The results of the present study were in disagreement with the results of Moon et al.11 who found no difference in the success rate on either the right or left side. The higher success on left side than the right may be explained by better hygiene on the left side of the dental arch by right-handed patients, who are most of the population.14 Better hygiene could reduce inflammation around the OIs.
En masse retraction of the six anterior teeth, instead of canine retraction followed by retraction of four incisors, can reduce treatment time and allow an early change of the facial profile. This increases patient cooperation in treatment. Hence, en masse retraction was used in the present study.
There are very few studies available that quantify the anchor loss with en masse retraction in both maxilla and mandible. Most studies are related to individual canine retraction and retraction in maxillary arch.
The present study was unique, as it evaluated anchor loss for en masse retraction in both maxillary arch and mandibular arch; other similar studies have commented only on the anchor loss in the maxillary arch. In the present study, the mean anchorage loss of 2.00 ± 0.65 mm (28.8%) in the maxillary arch of Group I; 0.2 ± 0.35 mm (2.86%) in the maxillary arch of Group II; 2.10 ± 0.75 mm (30%) in the mandibular arch of Group I, and 0.20 ± 0.35 mm (2.86%) in the mandibular arch of Group II were observed. The anchor loss was 28.8% and 30% in the maxilla and mandible, respectively of Group I and 2.86% for both maxilla and mandible in Group II (Table 4). Storey and Smith15 showed that 5–50% of the total extraction space could be taken up by an anchor unit made up of the first molar and the second premolar when used to retract a canine.
The anchor loss in the maxillary arch of Group I of the present study was similar to that in a study by Wook et al.16 and Upadhyay et al.17 Anchor loss with en masse retraction up to 2.4 mm of anchor loss was observed.18, 19, 20
Upadhyay et al.17 reported no anchor loss with en masse retraction in the maxillary arch with direct OI anchorage. However, in the present study, anchor loss of 2.86% occurred in Group II with use of indirect OI anchorage. Liou et al.21 have found that mini-screw implants might move 0.4 mm according to orthodontic loading in some patients. Thus, the minor anchor loss in Group II may be attributed to the drift of the OIs and the subsequent movement of molars with it.
Expectedly, there was a significant statistical difference in anchor loss between the two groups (Table 4).
In the present study, cephalometrics was used, which is two-dimensional, but low cost and easily available. However, in the future, three-dimensional imaging modalities may be utilized for conducting a similar study.
Conclusion
The overall success rate of titanium OIs in the present study was 90.90%. There was no statistical difference in the mean treatment time for patients treated with OIs for anchorage enhancement as compared to the patients provided with conventional anchorage (21.76 ± 1.54 months). The anchor loss with OI anchorage was significantly lower (0.2 ± 0.35 mm in the maxillary arch and 0.20 ± 0.35 mm in the mandibular arch) than with conventional anchorage (2.00 ± 0.65 mm in the maxillary arch and 2.10 ± 0.75 mm in the mandibular arch). However, within the two groups, there was no significant difference in anchor loss in the maxillary arch as compared to the mandibular arch.
Peri-implant inflammation was the only complication observed. The OIs remained positionally stable while sustaining orthodontic forces of 150 g. Therefore, OIs can be used for orthodontic anchorage predictably and consistently in routine orthodontic practice. The OIs used in the present study offered better orthodontic anchorage compared with conventional anchorage.
It can be concluded that, with proper patient and implant selection, implants as anchorage for en masse retraction can be incorporated into orthodontic practices with complete success. The use of OIs for anchorage is a viable alternative to conventional molar anchorage.
Conflicts of interest
The authors have none to declare.
Acknowledgements
-
(a)
This paper is based on Armed Forces Medical Research Committee Project No. 4004/2009 funded granted by the Office of the Directorate General Armed Forces Medical Services and Defence Research Development Organization, Government of India.
-
(b)
Mr. DR Basannar, Scientist ‘F’, Dept of Community Medicine, AFMC, Pune.
References
- 1.Proffit W.R. 5th ed. Mosby; St. Louis: 2012. Contemporary Orthodontics; p. 344. [chapter 9] [Google Scholar]
- 2.Chae J.M. A new protocol of Tweed-Merrifield directional force technology with microimplant anchorage. Am J Orthod Dentofac Orthop. 2006;130:100–109. doi: 10.1016/j.ajodo.2005.10.020. [DOI] [PubMed] [Google Scholar]
- 3.Melsen B., Bosch C. Different approaches to anchorage: a survey and an evaluation. Angle Orthod. 1997;67:23–30. doi: 10.1043/0003-3219(1997)067<0023:DATAAS>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 4.Kim Y.H., Choi J.H. The study about retention of miniscrews used for intraoral anchorage. J Korean Dent Assoc. 2001;39:684–687. [Google Scholar]
- 5.Fritz U., Ehmer A., Diedrich P. Clinical suitability of titanium microscrews for orthodontic anchorage-preliminary experiences. J Orofac Orthop. 2004;65:410–418. doi: 10.1007/s00056-004-0408-x. [DOI] [PubMed] [Google Scholar]
- 6.Moon C.H. vol. 3–4. Narae Publishing Inc.; Seoul: 2002. pp. 14–79. (Clinical Use and Failure of Skeletal Anchorage System). [Google Scholar]
- 7.Garfinkle J.S., Cunningham L.L., Beeman C.S., Kluemper G.T., Hicks E.P., Kimf M.O. Evaluation of orthodontic mini-implant anchorage in premolar extraction therapy in adolescents. Am J Orthod Dentofac Orthop. 2008;133:642–653. doi: 10.1016/j.ajodo.2006.04.053. [DOI] [PubMed] [Google Scholar]
- 8.Chopra S.S., Chakranarayan A. Clinical evaluation of immediate loading of titanium orthodontic implants. Med J Armed Forces India. 2015 doi: 10.1016/j.mjafi.2012.06.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Miyawaki S., Koyama I., Inoue M., Mishima K., Sugahara T., Takano-Yamamoto T. Factors associated with the stability of titanium screws placed in the posterior region for orthodontic anchorage. Am J Orthod Dentofac Orthop. 2003;124:373–378. doi: 10.1016/s0889-5406(03)00565-1. [DOI] [PubMed] [Google Scholar]
- 10.Kuroda S., Sugawara Y., Deguchi T., Kyung H.M., Yamamotoc T.T. Clinical use of miniscrew implants as orthodontic anchorage: success rates and postoperative discomfort. Am J Orthod Dentofac Orthop. 2007;131:9–1576. doi: 10.1016/j.ajodo.2005.02.032. [DOI] [PubMed] [Google Scholar]
- 11.Moon C.H., Lee D.G., Lee H.S., Im J.S., Baek S.H. Factors associated with the success rate of orthodontic miniscrews placed in the upper and lower posterior buccal region. Angle Orthod. 2008;78:101–106. doi: 10.2319/121706-515.1. [DOI] [PubMed] [Google Scholar]
- 12.Chen C.H., Chang C.S., Hsieh C.H. The use of microimplants in orthodontic anchorage. J Oral Maxillofac Surg. 2006;64:1209–1213. doi: 10.1016/j.joms.2006.04.016. [DOI] [PubMed] [Google Scholar]
- 13.Park H.S., Jeong S.H., Kwon O.W. Factors affecting the clinical success of screw implants used as orthodontic anchorage. Am J Orthod Dentofac Orthop. 2006;130:18–25. doi: 10.1016/j.ajodo.2004.11.032. [DOI] [PubMed] [Google Scholar]
- 14.Byoun N.Y., Nam E.H., Yoon Y.A., Kim I.K. Three-dimensional finite element analysis for stress distribution on the diameter of orthodontic mini-implants and insertion angle to the bone surface. Korean J Orthod. 2006;36:178–187. [Google Scholar]
- 15.Storey E., Smith R. Force in orthodontics and its relation to tooth movement. Aust J Dent. 1952;56:13. [Google Scholar]
- 16.Wook H., Dong-Seok N., Seung-Hak B. En masse retraction and two-step retraction of maxillary anterior teeth in adult Class I women – a comparison of anchorage loss. Angle Orthod. 2007;77:937–978. doi: 10.2319/111706-464.1. [DOI] [PubMed] [Google Scholar]
- 17.Upadhyay M., Yadav S., Patil S. Mini-implant anchorage for en-masse retraction of maxillary anterior teeth: a clinical cephalometric study. Am J Orthod Dentofac Orthop. 2008;134:803–810. doi: 10.1016/j.ajodo.2006.10.025. [DOI] [PubMed] [Google Scholar]
- 18.De Clerck H., Geerinckx V., Siciliano S. The zygoma anchorage system. J Clin Orthod. 2002;36:455–459. [PubMed] [Google Scholar]
- 19.Wehrbein H., Merz B.R., Diedrich P., Glatzmaier J. The use of palatal implants for orthodontic anchorage. Design and clinical application of the orthosystem. Clin Oral Implants Res. 1996;7:410–416. doi: 10.1034/j.1600-0501.1996.070416.x. [DOI] [PubMed] [Google Scholar]
- 20.Roberts W.E., Engen D.W., Schneider P.M., Hohlt W.F. Implant anchored orthodontics for partially edentulous malocclusions in children and adults. Am J Orthod Dentofac Orthop. 2004;126:302–304. doi: 10.1016/j.ajodo.2004.06.008. [DOI] [PubMed] [Google Scholar]
- 21.Liou E.J., Pai B.C., Lin J.C. Do miniscrews remain stationary under orthodontic forces? Am J Orthod Dentofac Orthop. 2004;126:42–47. doi: 10.1016/j.ajodo.2003.06.018. [DOI] [PubMed] [Google Scholar]