Abstract
In the current study, we investigated that how sagittal femoral bowing can affect the sagittal alignment of the femoral component in total knee arthroplasty (TKA).
There were 25 patients underwent TKA. Long leg radiography in lateral view was performed. The sagittal femoral bowing (SFB) and component alignment in relation to the sagittal mechanical axis and distal anterior cortical line (DACL) were measured. Finally, the correlation of component alignment and SFB was examined.
Mean SFB was 7±2.7 degrees. The component was in flexion position in relation to mechanical axis and DACL as 8.4±2.9 degrees and 1.7±0.9 degrees, respectively. The flexion alignment of the component was significantly correlated with SFB.
Mechanical alignment of the limb in both coronal and sagittal axes should be preserved in TKA. SFB can significantly increased the flexion alignment of the femoral component.
Keywords: Alignment, Sagittal femoral bowing, Total knee arthroplasty
Introduction
Total Knee Arthroplasty (TKA) is a major orthopedic surgery with favorable results (1). Annually, numerous TKAs are performed all over the world which substantially improves the patients’ quality of life.
There are several factors affecting the outcomes of TKA, in which, alignment of components is an important one (2-6). Currently, the pre- and post-operative alignment of lower extremities and components of knee prostheses are routinely evaluated in coronal plane, while less attention is paid to sagittal alignment. However, based on the recent studies, position of components in sagittal plane can seriously influence the surgical outcome and survival of prosthesis. It has been shown that hyper flexion of femoral component impinges upon anterior part of polyethylene and anterior edge of the intercondyler notch, and thus increases polyethylene wear (7-10). Furthermore, hyperextension of femoral component creates a notch in the femoral cortex, resulting in increased likelihood of supracondylar fracture (8, 11-13).
Clearly, alignment of the femoral component in sagittal plane is determined by several factors including implant design, sagittal femoral bowing (SFB), the entry point of intramedullary guide, depth of guide insertion, and reamer diameter. Recently, it has been shown that SFB can affect the position of femoral component in sagittal plane (14-16). Due to the sagittal curvature of the femur, utilizing long intramedullary rod will create anterior sliding of the entry point leading to anterior translation of the cutting block, which increases the flexion gap. In current study, we investigated the effects of SFB on alignment of femoral component in sagittal plane. We hypothesized that the greater SFB values result in greater flexion of femoral component.
Materials and Methods
This retrospective descriptive-analytical study was conducted on 25 patients who had undergone TKA by the same surgeon (M.K) using the same prosthesis (cruciate retaining knee prosthesis, Stryker company, USA) from winter 2012 to winter 2013 in Akhtar Hospital. The patients with any history of fracture or previous hip, knee, or ankle surgery were excluded. The patients signed an informed consent. After clinical examinations, digital weight-bearing long leg radiography in true lateral view was performed.
On x-rays, the angle between tangents to distal and proximal anterior femoral cortices was measured as SFB [Figure 1; α angle] (15). The perpendicular line to the plane where implant pegs were located was considered as implant alignment in sagittal plane [Figure 2]. In current study, two reference lines were used to evaluate the femoral component alignment; the first was the mechanical femoral axis in sagittal plane. There was no consensus on definition of this axis, however, we used the mechanical axis determined by implant manufacturer (Stryker Company). This axis is defined as the line extending from the center of femoral head to a point one centimeter anterior to Blumensaat’s line in sagittal plane [Figure 1; red line] (15). The second reference line was the distal anterior cortical line (DACL) drawn tangent to the anterior cortex of distal femur [Figure 2].
Figure 1.
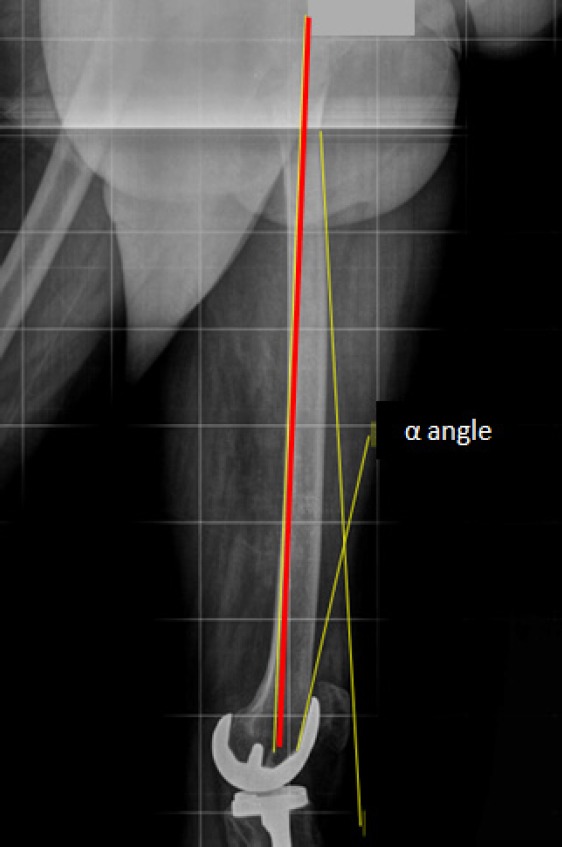
The measurement method of sagittal femoral bowing (α angle) and sagittal mechanical axis of the femur (red line).
Figure 2.
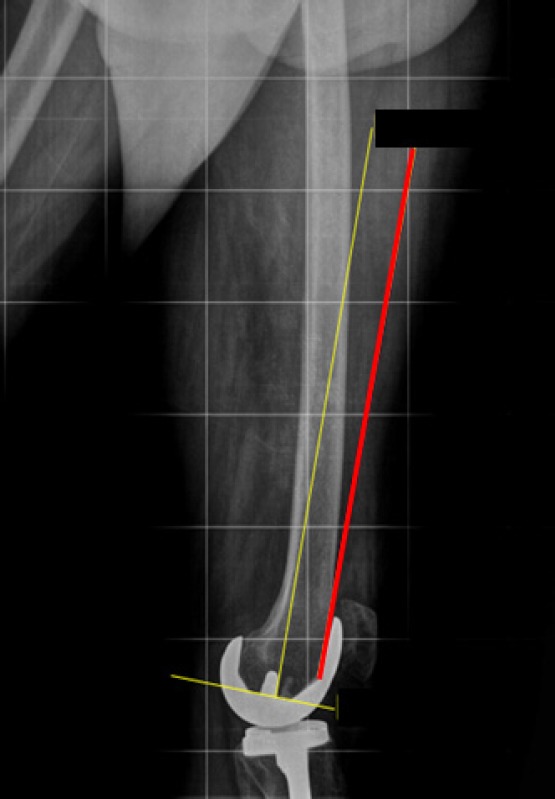
Implant alignment in sagittal plane (yellow line) and the distal anterior cortical line (red line).
To assess position of femoral component in relation to each of these reference lines, the acute angle between these lines and component alignment line was measured as femoral component flexion. All measurements were performed by two orthopedists using Micro Dicom software. In a pilot study, inter observer and intra observer reliability were found greater than 0.9. The mean of two measurements was considered as the final value of component flexion. The correlation between values of SFB and femoral component flexion was determined using Pearson’s correlation test. Statistical analyses were performed using SPSS statistical software (version 16.0) P<0.05 was considered significant.
Results
Twenty five patients (11 males and 14 females) were evaluated in the current study. Patients aged 61.5±13.7 years (Range: 53 to 72). The mean interval from the surgery to final visit was 1.1±0.9 years. Mean SFB was determined 7±2.7 degrees (Range: 4 to 16.3 degrees).
The femoral component was in flexion position related to the mechanical axis in all of the patients. Regarding the DACL, the femoral component was in neutral position in some of the patients and small flexion in others. Amount of flexion in relation to mechanical axis and DACL was 8.4±2.9 degrees (range: 4 to 14.3 degrees) and 1.7±0.9 degrees (range: 0 to 3 degrees), respectively. Pearson’s correlation test showed a significant positive correlation between femoral component flexion in relation to mechanical axis and amount of SFB (r=0.798, P<0.001) [Figure 3].
Figure 3.
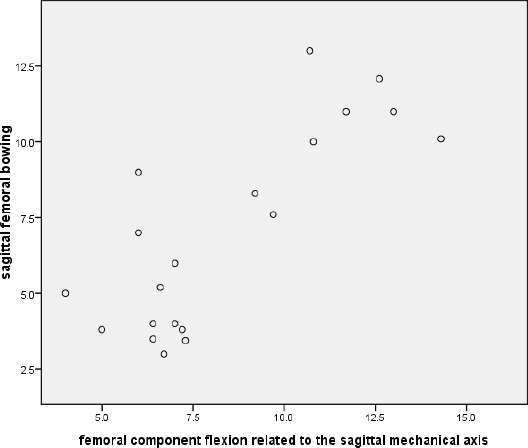
The correlation between flexion of the femoral component in relation to the sagittal mechanical axis and sagittal femoral bowing.
Discussion
The results of the current study showed that sagittal alignment of femoral component is affected by SFB. In other word, femoral component flexion increased significantly with improved SFB.
There are limited studies addressed sagittal alignment of femoral component. We did not find considerable information regarding sagittal alignment of the knee prosthesis in major orthopedic reference books. In general, there is no consensus on sagittal mechanical axis of the alignment of femoral bone and femoral component. The appropriate reference line for evaluating the femoral component alignment is controversial.
The purpose of TKA is to achieve an alignment similar or near to the normal biomechanical alignment of the lower limb in both coronal and sagittal planes (17). Therefore, it is necessary to consider the sagittal mechanical axis of the lower extremity in TKA and find strategies to achieve normal mechanical axis after the operation. Recently, Kim et al. proposed that to increase the survival of the knee prosthesis, over all anatomic alignment of the knee should be placed in 3-7.5 degrees valgus. In addition, femoral component should be placed in 2-8 degrees valgus in coronal plane and 0 to 3 degrees in sagittal plane. Moreover, tibial component should be placed in 90 degrees in coronal plane and 0-7 degrees in sagittal plane. Both components should have 2-5 degrees external rotation (18).
In 2005, Tang et al. studied the alignment of femur in sagittal plane in Chinese population. They found that lateral view of the bone looks like a hockey stick. This exaggerated bowing on the distal end of the femur can affect sagittal position of the femoral component. They also argued that implant design should account for this femoral contour (14). Similar results were obtained in another study in China by Lu et al. (2012), who stated that such morphological features are indicative of the need for changes in how intramedullary guide rods are used (19). In a study in the United States, Yahyawi et al. (2007) showed that sagittal femoral bowing was smaller in distal third compared to proximal third and has less effect on the final amount of femoral component flexion (10). However, it is possible that distal femoral bowing is not sufficiently large in the Caucasian race to draw the surgeons’ attention prior to surgery.
Like the above-mentioned Chinese studies, in our current study, the overall SFB was correlated to and affected the amount of femoral component flexion. Due to the lack of knowledge about the pre- and post-operative sagittal alignment of the lower limb and the correct position of the femoral component, different techniques are utilized to determine the prosthesis alignment and to measure the bowing. It can dramatically affect the results of the studies and reminds the necessity of defining a comprehensive method.
There are various definitions for sagittal femoral mechanical axis, but since the Stryker implants was used in current study, we utilized the mechanical axis defined by this company (15). Regarding the mechanical axis (which is the most important reference line in determining the alignment of the prosthesis), the amount of femoral component flexion was significantly correlated to SFB, and increased with increasing bowing. The femoral component was placed in neutral position or minimal flexion position (0-3 degrees) in relation to the DACL. It should be noticed that, intra operatively, the surgeon considers the DACL as the reference line and tries to align the femoral component parallel to this line. However, this angle may attributed to the surgeon’s technical error. Furthermore, the optimal reference line is the mechanical axis which cannot be determined exactly during procedure.
When inserting intramedullary rod, the surgeon should not merely focus on distal femur, because alignment of prosthesis is affected by the total bowing of the femur in sagittal plane.
It should be noted that among factors affecting sagittal alignment of the femoral component, no changes can be made in SFB without osteotomy, but other factors can be modified. Therefore, femoral bowing effect should be reduced as much as possible by making changes in other influential factors, such as use of appropriate prosthesis design. Nowadays, the available prostheses, are designed and manufactured based on the morphological data from western societies, yet there are some anatomical and morphological differences between Western and Asian populations (20-22). Hence, in prosthesis design, attention to morphological features in Asian populations is essential. Choosing the appropriate entry point and the appropriate insertion depth for rod and reamer with the correct diameter, can have a major role in improving implant alignment. In recent years, design of navigation and Patient Specific Instrumentation (PSI) has been of huge interest. This can be very helpful in this regard, however, assessment of their efficiency requires further studies.
One of the limitations of the present study was its small sample size. The main problem was lack of sufficient information about how to determine and measure sagittal alignment of the knee prosthesis components, which requires more extensive studies.
To achieve better results in knee arthroplasty, mechanical alignment of the limb in both coronal and sagittal axes should be preserved. SFB can significantly affect the sagittal alignment of the femoral component which should be greatly considered indesigning the knee prosthesis and during the total knee arthroplasty.
Table 1.
The base line characteristics of patients
| SA | GA | P | ||
|---|---|---|---|---|
| Sex | Male | 42 (84%) | 38 (76%) | 0.31 |
| Female | 8 (16%) | 12 (24%) | ||
| Age | 66.22±5.17 | 65.98±4.76 | 0.81 | |
| BMI | 24.73±2.87 | 24.75±2.75 | 0.97 | |
| ASA | 1 | 6 (12%) | 8 (16%) | 0.84 |
| 2 | 33 (66%) | 31 (62%) | ||
| 3 | 11 (22%) | 11 (22%) |
Table 2.
The characteristics of patients during surgery and recovery
| SA | GA | P | ||
|---|---|---|---|---|
| Duration of operation | 87.24±4.33 | 95.68±3.27 | 0.001 | |
| SBP (during surgery) | 10 (min) | 121.44±19.12 | 120.18±20.50 | 0.75 |
| 20 | 118.56±15.03 | 119.74±19.31 | 0.73 | |
| 30 | 116.84±13.95 | 121.76±17.76 | 0.13 | |
| DBP (during surgery) | 10 (min) | 72.82±13.88 | 70.56±12.60 | 0.4 |
| 20 | 70.98±13.13 | 70.64±13.07 | 0.9 | |
| 30 | 69.10±12.34 | 72.44±13.01 | 0.19 | |
| HR (during surgery) | 10 (min) | 85.80±16.04 | 83±13.55 | 0.40 |
| 20 | 81.94±13.21 | 78.90±12.48 | ||
| 30 | 79.04±11.59 | 80.38±13.18 | ||
| MAP (during surgery) | 10 (min) | 87.80±14.54 | 87.31±14.07 | 0.10 |
| 20 | 85.78±13.87 | 86.63±14.84 | ||
| 30 | 84.24±12.30 | 88.14±14.01 | ||
| 40 | 84.22±11.34 | 89.84±12.22 | ||
| 50 | 85.14±11.75 | 88.80±10.60 | ||
| 60 | 84.56±11.43 | 89.7310.79 | ||
| 70 | 85.65±10.61 | 89.71±9.80 | ||
| 80 | 86.65±10.62 | 91.13±10.34 | ||
| SBP (during recovery) | 10 (min) | 117.26±12.26 | 131.62±19.52 | 0.000 |
| 20 | 115.82±11.96 | 13.24±18.30 | 0.000 | |
| 30 | 115.64±12 | 127.22±16.40 | 0.000 | |
| DBP (during recovery) | 10 (min) | 72.22±10.53 | 78.92±11.44 | 0.003 |
| 20 | 72.26±10.89 | 78.48±10.82 | 0.005 | |
| 30 | 71.68±11.612 | 75.28±10.62 | 0.109 | |
| HR (during recovery) | 10 (min) | 77.75±12.76 | 84.44±14.37 | 0.32 |
| 20 | 76.85±12.38 | 83.33±13.28 | ||
| 30 | 75.55±12.002 | 81.20±13.79 | ||
| MAP (during recovery) | 10 (min) | 86.89±10.08 | 95.83±12.84 | 0.004 |
| 20 | 86.06±10.43 | 94.87±12.23 | ||
| 30 | 85.84±11.09 | 92.14±11.53 | ||
| 40 | 86.5±10.53 | 94.710.19 | ||
Table 3.
The characteristics of patients in recovery
| Group | SA(%) | GA | P |
|---|---|---|---|
| Vomiting in recovery | 1 (2%) | 9 (18%) | 0.006 |
| Ephedrine (during operation) | 4 (8%) | 2 (4%) | 0.39 |
| Morphine (mg) | 0.89±1.52 | 2.66±1.63 | 0.001 |
| Bleeding (ml) (during operation) | 365.00±62.99 | 513.70±151.19 | 0.001 |
| VAS | 2.36±1.85 | 4.86±1.75 | 0.001 |
| Time to discharge (min) Alderte score>9 | 41.26±8.37 | 35.04±3.39 | 0.001 |
References
- 1.Cherian JJ, Banerjee S, Kapadia BH, Jauregui JJ, Harwin SF, Mont MA. Cementless total knee arthroplasty: a review. J Knee Surg. 2014;27(3):193–7. doi: 10.1055/s-0034-1374811. [DOI] [PubMed] [Google Scholar]
- 2.Moon HK, Han CD, Yang IH, Cha BS. Factors affecting outcome after total knee arthroplasty in patients with diabetes mellitus. Yonsei Med J. 2008;49(1):129–37. doi: 10.3349/ymj.2008.49.1.129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Santaguida PL, Hawker GA, Hudak PL, Glazier R, Mahomed NN, Kreder HJ, et al. Patient characteristics affecting the prognosis of total hip and knee joint arthroplasty: a systematic review. Can J Surg. 2008;51(6):428–36. [PMC free article] [PubMed] [Google Scholar]
- 4.Stan G, Orban H, Gruionu L, Gheorghe P. Coronal malposition effects in total knee arthroplasty: a finite element analysis. Eur J Orthop Surg Traumatol. 2013;23(6):685–90. doi: 10.1007/s00590-012-1051-7. [DOI] [PubMed] [Google Scholar]
- 5.Rienmüller A, Guggi T, Gruber G, Preiss S, Drobny T. The effect of femoral component rotation on the five-year outcome of cemented mobile bearing total knee arthroplasty. Int Orthop. 2012;36(10):2067–72. doi: 10.1007/s00264-012-1628-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Liau JJ, Cheng CK, Huang CH, Lo WH. The effect of malalignment on stresses in polyethylene component of total knee prostheses--a finite element analysis. Clin Biomech (Bristol, Avon) 2002;17(2):140–6. doi: 10.1016/s0268-0033(01)00109-7. [DOI] [PubMed] [Google Scholar]
- 7.O’Rourke MR, Callaghan JJ, Goetz DD, Sullivan PM, Johnston RC. Osteolysis associated with a cemented modular posterior-cruciate-substituting total knee design. J Bone Joint Surg Am. 2002;84(8):1362–71. doi: 10.2106/00004623-200208000-00011. [DOI] [PubMed] [Google Scholar]
- 8.Piazza SJ, Delp SL, Stulberg SD, Stern SH. Posterior tilting of the tibial component decreases femoral rollback in posterior-substituting knee replacement: a computer simulation study. J Orthop Res. 1998;16(2):264–70. doi: 10.1002/jor.1100160214. [DOI] [PubMed] [Google Scholar]
- 9.Puloski SK, McCalden RW, MacDonald SJ, Rorabeck CH, Bourne RB. Tibial post wear in posterior stabilized total knee arthroplasty. An unrecognized source of polyethylene debris. J Bone Joint Surg Am. 2001;83-A(3):390–7. doi: 10.2106/00004623-200103000-00011. [DOI] [PubMed] [Google Scholar]
- 10.Yehyawi TM, Callaghan JJ, Pedersen DR, O’Rourke MR, Liu SS. Variances in sagittal femoral shaft bowing in patients undergoing TKA. Clin Orthop Relat Res. 2007;464(1):99–104. doi: 10.1097/BLO.0b013e318157e4a2. [DOI] [PubMed] [Google Scholar]
- 11.Lesh ML, Schneider DJ, Deol G, Davis B, Jacobs CR, Pellegrini VD., J The consequences of anterior femoral notching in total knee arthroplasty. A biomechanical study. J Bone Joint Surg Am. 2000;82-A(8):1096–101. doi: 10.2106/00004623-200008000-00005. [DOI] [PubMed] [Google Scholar]
- 12.Ritter MA, Thong AE, Keating EM, Faris PM, Meding JB, Berend ME, et al. The effect of femoral notching during total knee arthroplasty on the prevalence of postoperative femoral fractures and on clinical outcome. J Bone Joint Surg Am. 2005;87(11):2411–4. doi: 10.2106/JBJS.D.02468. [DOI] [PubMed] [Google Scholar]
- 13.Shawen SB, Belmont PJ, Jr, Klemme WR, Topoleski LD, Xenos JS, Orchowski JR. Osteoporosis and anterior femoral notching in periprosthetic supracondylar femoral fractures: a biomechanical analysis. J Bone Joint Surg Am. 2003;85-A(1):115–21. doi: 10.2106/00004623-200301000-00018. [DOI] [PubMed] [Google Scholar]
- 14.Tang WM, Chiu KY, Kwan MF, Ng TP, Yau WP. Sagittal bowing of the distal femur in Chinese patients who require total knee arthroplasty. J Orthop Res. 2005;23(1):41–5. doi: 10.1016/j.orthres.2004.06.013. [DOI] [PubMed] [Google Scholar]
- 15.Chung BJ, Kang YG, Chang CB, Kim SJ, Kim TK. Differences between sagittal femoral mechanical and distal reference axes should be considered in navigated TKA. Clin Orthop Relat Res. 2009;467(9):2403–13. doi: 10.1007/s11999-009-0762-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Seo JG, Kim BK, Moon YW, Kim JH, Yoon BH, Ahn TK, et al. Bony landmarks for determining the mechanical axis of the femur in the sagittal plane during total knee arthroplasty. Clin Orthop Surg. 2009;1(3):128–31. doi: 10.4055/cios.2009.1.3.128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.McCormack D. Mechanical axis deviation: definitions, measurements and consequences. Irish J Orthopaed Surg. 2004;2(1):1–9. [Google Scholar]
- 18.Kim YH, Park JW, Kim JS, Park SD. The relationship between the survival of total knee arthroplasty and postoperative coronal, sagittal and rotational alignment of knee prosthesis. Int Orthop. 2014;38(2):379–85. doi: 10.1007/s00264-013-2097-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lu ZH, Yu JK, Chen LX, Gong X, Wang YJ, Leung KK. Computed tomographic measurement of gender differences in bowing of the sagittal femoral shaft in persons older than 50 years. J Arthroplasty. 2012;27(6):1216–20. doi: 10.1016/j.arth.2011.12.024. [DOI] [PubMed] [Google Scholar]
- 20.Nagamine R, Miura H, Bravo CV, Urabe K, Matsuda S, Miyanishi K, et al. Anatomic variations should be considered in total knee arthroplasty. J Orthop Sci. 2000;5(3):232–7. doi: 10.1007/s007760050157. [DOI] [PubMed] [Google Scholar]
- 21.Harvey WF, Niu J, Zhang Y, McCree PI, Felson DT, Nevitt M, et al. Knee alignment differences between Chinese and Caucasian subjects without osteoarthritis. Ann Rheum Dis. 2008;67(11):1524–8. doi: 10.1136/ard.2007.074294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cooke TD, Harrison L, Khan B, Scudamore A, Chaudhary MA. Analysis of limb alignment in the pathogenesis of osteoarthritis: a comparison of Saudi Arabian and Canadian cases. Rheumatol Int. 2002;22(4):160–4. doi: 10.1007/s00296-002-0218-7. [DOI] [PubMed] [Google Scholar]


