Abstract
It is now well understood that once in contact with biological fluids, nanoscale objects lose their original identity and acquire a new biological character, referred to as a protein corona. The protein corona changes many of the physicochemical properties of nanoparticles, including size, surface charge, and aggregation state. These changes, in turn, affect the biological fate of nanoparticles, including their pharmacokinetics, biodistribution, and therapeutic efficacy. It is progressively being accepted that even slight variations in the composition of a protein source (e.g., plasma and serum) can substantially change the composition of the corona formed on the surface of the exact same nanoparticles. Recently it has been shown that the protein corona is strongly affected by the patient’s specific disease. Therefore, the same nanomaterial incubated with plasma proteins of patients with different pathologies adsorb protein coronas with different compositions, giving rise to the concept of personalized protein corona. Herein, we review this concept along with recent advances on the topic, with a particular focus on clinical relevance.
Keywords: nanoparticles, personalized protein corona, nano-bio interface, therapeutic efficacy
Introduction
In a physiological milieu, a shell of active biomolecules forms around NPs referred to as a protein corona (PC). 1 The PC, also known as the biomolecular corona, is mainly composed of proteins. However, researchers also expect to find other biomolecules such as lipids, metabolites, and sugars in future investigations.2,3 The phenomenon of PC formation is frequent among all known NPs, except for a few with coatings such as zwitterionic,4,5 and has an important impact on the NP’s properties. PC-coated NPs strongly differ in size, surface charge and aggregation state compared to pristine NPs.6–8 PC composition is affected by both NP characteristics (e.g., physicochemical properties) and environmental factors (e.g., temperature, protein source, type of disease present). The effect of NPs’ physicochemical properties on corona formation have been extensively examined and already comprehensively reviewed by us and others.1,6,9–13 However, many environmental factors (e.g., protein and ionic concentrations,14 temperature,15 origin [human or murine],16 protein source [fetal bovine serum, serum or plasma],17 choice of anticoagulant,16 and flow status [dynamic vs static]18) have been only recently introduced19 while several others (e.g., personalized protein corona and disease-specific protein corona)20 are not yet understood. It is well known that the dynamic nature of the vascular system and its constituents are altered in pathological conditions.21 Importantly, changes in the abundance of several proteins in the plasma have been used as biomarkers to help diagnose and/or forecast the severity of different diseases.22–25 Keeping in mind that each disease is characterized by different plasma proteomes, our group has hypothesized and demonstrated that different diseases induce the formation of different PCs on the same nanomaterial.20 We investigated the effects of alterations in the plasma proteome due to different pathological conditions on the PC composition of commercially available NPs, thus introducing the novel concept of a “personalized protein corona” (PPC) (Figure 1).20 Other groups have proven that the plasma proteome is not always consistent, even in healthy individuals, either in terms of composition or abundance of certain proteins.26
Figure 1. Disease-dependent personalized protein corona.

The biological environment that comes into contact with NPs affects the protein corona (PC): plasma protein alterations due to disease conditions affect the type, amount, and conformation of proteins that compose the corona. Reproduced from Ref. [20] with permission from Royal Society of Chemistry.
Herein, we expand the concept of “personalized protein corona” to include not only the PC formed around NPs during incubation with plasma from human patients with specific diseases, but also the PC formed from plasma of healthy individuals of different ages and genders or with certain lifestyles, habits, temporary conditions, and geographical origins (Figure 2). Despite having been thus far overlooked, the PPC plays a crucial role in the biological fate of nanoparticles, and represents one possible explanation for the unsuccessful clinical results of some nano-products in clinical trials. In this mini-review, we highlight the importance of this new concept for avoiding misinterpretation of PC data, report recent studies on the PPC and discuss its impact in the clinical setting.
Figure 2. Personalized protein corona general concept.
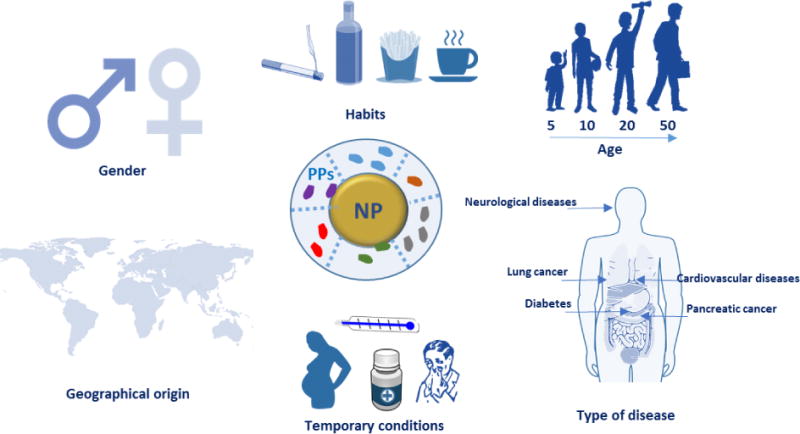
Gender, habits, age, diseases, temporary drug consumption, pregnancy, and geographical origin all potentially affect the protein plasma composition. This, in turn, affects the protein corona composition. As a consequence, this information has to be provided when working with human plasma, not only to better interpret the obtained results but also to give useful information for the design of the safe and efficient nanoparticles in a disease-specific manner. NP: nanoparticle, PPs: plasma proteins
Plasma proteins as disease biomarkers
Human blood can contain biomarkers for various diseases. 27–32 In the case of cancer, blood components such as some specific cell types, 33 peptides, 34 microRNAs, 35 metabolites 36 and proteins37 are used as indicators of pathological status 27. Plasma protein profiles have been widely investigated as biomarkers. In certain cases, even the level of post-translational modifications of plasma proteins has been used to distinguish patients with a given disease from healthy individuals.38,39 For example, highly altered glycosylation levels (i.e., sialylation and fucosylation) of complement C3, histidine-rich glycoprotein and kininogen-1 have been correlated with colorectal cancer progression.38 On the other hand, protein carbonylation of plasma proteins (e.g., VEGFR-2, MMP-1, and complement C5) is associated with obesity-induced type 2 diabetes mellitus.39
Some plasma proteins are components of the acute/chronic inflammatory response. These “inflammation-sensitive plasma proteins” (ISPs) have been associated with myocardial infarction, stroke, diabetes, and prediabetes conditions (i.e., impaired glucose tolerance).40–47 In particular, increased levels of fibrinogen-alpha, α-antitrypsin, and C-reactive protein have been connected with diabetes,47 while C-reactive protein, tumor necrosis factor alpha, and other inflammatory markers have been identified as biomarkers for the prediction of cardiovascular diseases.45 Moderate systemic inflammation is associated with the pathology of chronic heart failure and causes several further problems such as myocardial remodeling and cardiac arrhythmia.48 Many epidemiological studies have connected higher plasma levels of inflammatory markers with the incidence of cardiovascular diseases.49,50 Indeed, population-based cohort studies with follow-up ~20 years revealed that plasma levels of ISPs, including fibrinogen and alpha-1-antitrypsin, are correlated to incidence of hospitalization for heart failure.43
Another plasma protein strongly affected by the presence of inflammation is albumin, the major protein in plasma51 and, for this reason, one of the first proteins to be absorbed in the PC of the majority of known nanomaterials.52,53 Albumin is synthesized by the liver and is fundamental for the transport of hormones and vitamins throughout the body.51 Complications inducing liver malfunction and disorders change the level of albumin in the plasma. Moreover, albumin levels are also indicators of different pathological conditions, such as poor nutrition and infection. 54
To further complicate the situation, several studies have also reported modulations of the levels of plasma proteins in patients with neurological disturbances.24,55–58 Immunoglobulin IgM, complement C3c, complement C4, and α-antitrypsin have all been found to be elevated in patients with depression, while less albumin and transferrin were found than in the plasma of healthy volunteers.57 Meanwhile, plasma levels of complement factor-H and alpha-2-macroglobulin in Alzheimer’s disease patients are dramatically higher than in healthy people and their abundance was also correlated with the severity of the disease.56,58,59 Though these findings are certainly important for the diagnosis and prediction of all the above-mentioned diseases, they are also crucial evidence that human plasma, like other biological fluids, cannot be considered homogeneous. This concept should be incorporated into the design of PC-based studies. For instance, in planning investigations of the effect of PC formation on NPs’ targeting, distribution, and/or toxicity, it is essential to utilize plasma or sera from patients for whom there is data on the type of disease, stage, and their gender/age/lifestyle and geographical origin. These details should be reported to better interpret findings and to allow other researchers to customize their particles in a patient-specific manner.
Disease-induced variability in the protein corona composition
As mentioned above, various diseases can cause variations in the composition of the plasma proteome and/or the conformation of proteins. This, in turn, implies potential changes in the identity and conformation of the PC’s components. Below we will discuss how changes in protein conformations affect the PC. Herein we introduce two recent studies featuring extensive analysis of changes in the PC composition in a wide range of diseases. 20,26
In the first study, PPCs formed on silica-and-polystyrene NPs were investigated using plasma derived from patients with diseases such as cancer, diabetes, hypercholesterolemia, rheumatism, fauvism, hemophilia, hypofibrinogenemia, and healthy individuals with different lifestyle factors including smoking and fat-rich diets or temporary conditions such as pregnancy.20 Protein patterns of the PCs on silver-stained SDS-PAGE gels clearly showed that the PCs associated with various diseases differed both in terms of composition and amount. Furthermore, PCs generated using plasma from patients suffering from the same disease and with the same lifestyle were quite similar, with only slight differences. Lastly, even in the case of plasma from healthy subjects of the same gender and age, PCs were not always consistent. 20
The results of the first study were confirmed by Colapicchioni et al. 26 (Figure 3) in the course of evaluating PPCs formed on clinically approved liposomes (AmBisome) in gastric, breast, and pancreatic cancer patients (10 individuals per disease). The authors found that changes in the liposome’s size attributable to the PC were similar between healthy volunteers and cancer patients. PC-coated liposomes were less negatively charged in pancreatic cancer patients than in breast and gastric patients, thus indicating higher levels of cationic plasma proteins. PC profiles analyzed by SDS-PAGE were similar in various cases, with specific bands more abundant in the PC associated with pancreatic cancer, confirming the surface charge findings. Among the most abundant bands, one at MW ≈37 kDa associated with heavy chains of immunoglobulin alpha (IgA) and immunoglobulin gamma (IgG) was identified.26 Cancer patients show important changes in the concentration of Igs, that are correlated with the presence of autoantibodies produced as immunodefense against tumors. This finding is of particular interest because it opens the way for the use of NP-PC-based technology in screens for earlydiagnostic tumor biomarkers (e.g. autoantibodies). 60–63
Figure 3. Personalized protein corona in healthy volunteers.
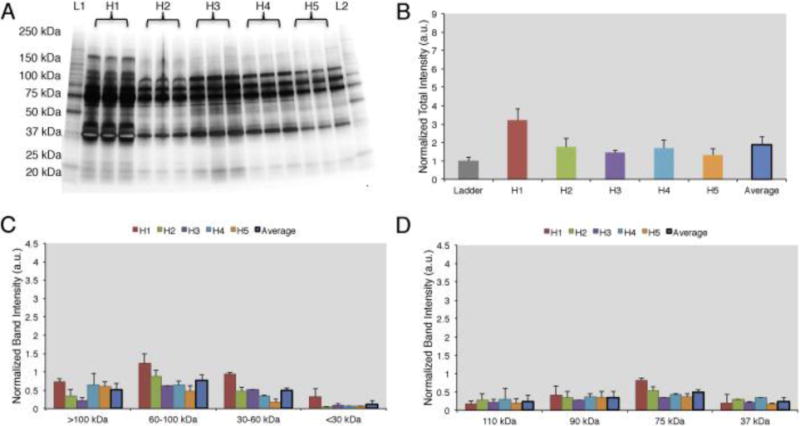
A) 1D-SDS PAGE image of the protein corona profiles formed around liposomes when incubated for 1h with human plasma from five healthy volunteers. B) Intensity of lanes analyzed by ImageJ showing that the protein coronas are different in abundance among the 5 healthy donors. C) Band intensity according to the molecular weights. D) The top 4 most abundant band intensities are compared among the 5 samples. Results are presented as average ± SD. Reproduced from Ref. [26] with permission from Elsevier publishing group.
Cancer biomarkers are found at low concentrations during the early stages of a disease, making them very difficult to detect. However, adsorption in the PC creates a “nano-concentrator”26 of proteins not easily detectable under other conditions. It is accepted that the most abundant plasma proteins are the first to be absorbed by NPs; they form a short-term layer of low-affinity proteins defined as the soft corona. However, PC formation is dynamic, and the soft corona is soon replaced by a hard corona of proteins with higher affinity to the selected NP despite being less abundant in the plasma.64 This makes these relatively rare proteins much more easily detectable as biomarkers. For example, Zheng et al. 61 developed a simple PC-based assay for the early screening of prostate cancer using gold nanoparticles, which has been shown to be more specific than the current standard test for detection of early-stage prostate cancer (i.e., prostate-specific antigen test).
Disease-induced variability in protein corona conformation
When proteins interact with NPs, changes in their conformational state can occur 65–67. The denaturation of proteins adsorbed on NPs’ surface induces the exposure of epitopes normally hidden.68 This can increase NPs’ immunogenicity and/or trigger inflammatory responses, as in the case of gold NPs functionalized with poly(acrylic) acid.69 Deng et al. 69 demonstrated that functionalized gold NPs induced the unfolding of adsorbed fibrinogen. Fibrinogen possesses a region with a binding affinity toward the leukocyte receptor MAC-1. However, when it is folded, functional active fibrinogen does not interact with MAC-1 because the hydrophobic MAC-1 affinity region is facing the internal hydrophobic core.70 Instead, when bound to gold NPs, fibrinogen changed its conformation and, once unfolded, could interact with MAC-1. This interaction activated an inflammatory cascade 69 and established the basis for the introduction of a novel mechanism underlying the inflammatory response to NPs, mediated by the PC.
On the other hand, several pathologies arise from the presence of proteins in conformational states different from their original one, i.e., misfolded (Figure 4A). These diseases, also known as proteinopathies or conformational diseases, include neurodegenerative disorders, 71,72 amyloidosis, 73,74 and many others 75,76 (several examples are reported in Figure 4B) and are generally characterized by misfolded proteins whose conformational change triggers their tendency to aggregate with each other. While several diseases can bring variations in the protein composition of plasma, conformational diseases induce changes in the conformation of proteins, thus affecting their interactions with NPs and, consequently, their PC. In theory, the plasma of a patient with a conformational disease changes not in terms of protein composition. The interaction of the same protein in two different conformations with a given NP is not the same (Figure 4C). For this reason, it is crucial to study not only the identity but also the conformational state of proteins in the corona. As the protein corona is a complex system, current approaches (e.g., circular dichroism) to defining protein conformation cannot be employed. To overcome this shortcoming, we used fluorescence resonance energy transfer (FRET)-labeled fibronectin, enabling us to monitor the conformation of this protein in the protein corona in situ. The investigation of the molecular motifs (potentially recognized by receptors of cells) exposed by the proteins in the corona is now becoming a topic of great interest in the field.77
Figure 4. Disease-dependent protein conformational changes.
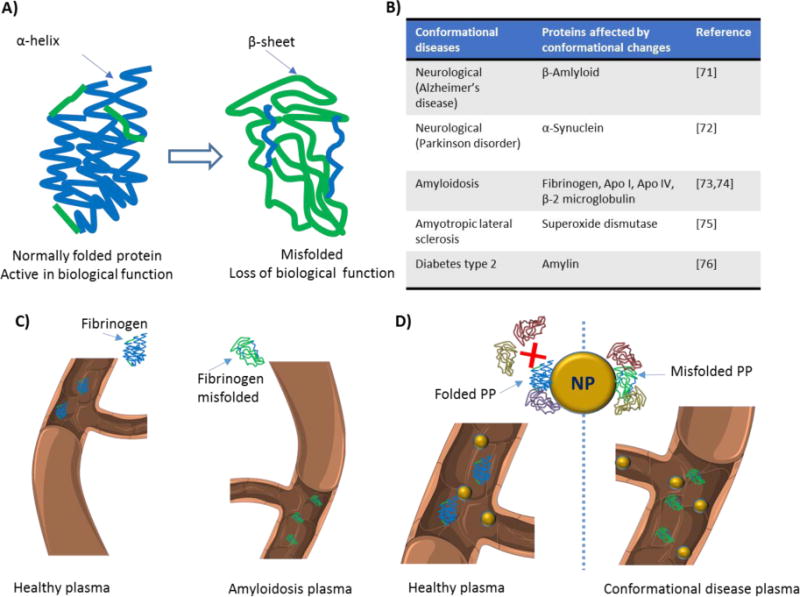
A) When a protein conformational change occurs, the secondary or tertiary structure of a protein is modified and its biological function is affected. B) Various diseases arise from protein conformational changes. C) The same protein in the plasma of patients with different diseases can have a different conformation D) This affects the interaction of the protein with the surface of nanoparticles and consequently alters participation of other proteins in the corona composition. NP: nanoparticle; PP: plasma protein.
Disease-induced nanotoxicity
Identical NPs employed to treat patients with different diseases are characterized by different (i.e., personalized) PCs. These PPCs affect NPs’ biological fate in ways we still find hard to predict. To improve the efficiency and safety of personalized nanomaterials for clinical applications, it is crucial to elucidate how the PPCs influence the therapeutic impact of NPs. We have evaluated the therapeutic/toxic impact of graphene oxide (GO) sheets coated by PPCs obtained using plasma from human subjects with various pathological conditions.78 GO sheets have attracted the attention of many researchers due to their peculiar physicochemical properties. They are already employed in several applications, including neural network regeneration, cancer therapy, and stem cell tissue regeneration.79 GO sheets were incubated with the plasma of patients with seven different diseases: thalassemia (major and minor), blood cancer, diabetes, fauvism, rheumatism, and hypercholesterolemia. The plasma from pregnant women in the same gestation period and of similar age was also used to create a PPC on GO sheets. Then, interactions between PPC-coated GO sheets and breast cancer cell lines (MCF-7 and MDA-MB-231) were evaluated in terms of cellular toxicity, apoptosis/necrosis (Figure 5 A–J), cellular uptake, production of reactive oxygen species, cellular inflammation, and lipid peroxidation.78 The results showed significantly different effects of the PPCs-coated NPs on each of these biological processes, underlining once again that detailed information on patients’ clinical history, lifestyle, and habits must be carefully considered in the development of ad hoc-designed nanomaterials.
Figure 5. Disease-dependent apoptosis and necrosis.
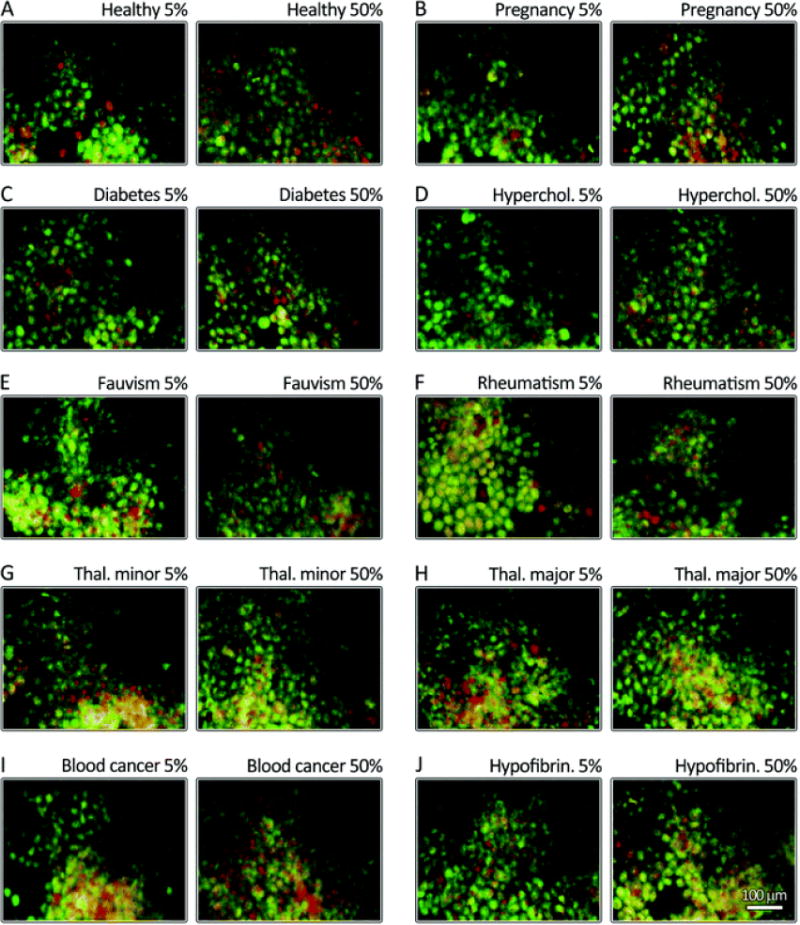
MCF-7 breast cancer cells were stained using propidium iodide (nuclei, green) and annexinV (membrane, yellow to red). The cells were then incubated for 24h with corona-coated GO from patients with different diseases (A-J). The results show that the protein coronas from different diseases have different impacts on apoptosis (green) and late apoptosis/necrosis (yellow/green-red) levels. GO: graphene oxide. Reproduced from Ref. [77] with permission from Royal Society of Chemistry.
Similar conclusions were obtained by Shannahan and coworkers. 80 The authors aimed at developing in vitro approaches to study NPs’ toxicity for cardiovascular applications. As already mentioned, individuals with cardiovascular pathologies have an altered plasma composition, potentially affecting PC formation. Moreover, many NPs are conceived for intravenous injection and are directly exposed to the vasculature. This can cause vascular inflammation, the formation of atherosclerotic plaques, and oxidative stress, 81–84 demonstrating the need for a better understanding of the cardiovascular toxicity induced by NPs. PCs were obtained by incubating magnetite iron oxide NPs (Fe3O4) with normal/healthy and lipid-rich rat serum.80 Authors first tested whether the lipid-rich serum induced the formation of a different PC (PPC) compared with the normal serum, then investigated the toxicological consequences induced by PPCs. Rat aortic endothelial cells (RAECs) were incubated with PC-coated NPs under flow conditions to better mimic the in vivo scenario. PCs from both sera induced a slight increase in the hydrodynamic diameters of NPs. As expected, the amount of cholesterol in the PC formed using the lipid-rich serum was higher than that of the PC formed from normal serum. The two PCs had 92 protein components in common, while 29 unique proteins were identified only in the hyperlipidemic PC. Both normal and lipid-rich PCs reduced the association of NPs with RAECs, while the PC formed using lipid-rich serum induced intensified endothelial cell activation and inflammatory response (i.e. increased expression of IL-6, tumor necrosis factor alpha, VCAM-1),80 demonstrating the importance of physiological impact in determining NP biological response.
Clinical relevance of personalized protein corona
Despite recent progress in nanomedicine, only a few NPs have been assessed in clinical trials, and even fewer have reached clinical practice. Recent findings show that one of the reasons behind the incongruence between experimental discoveries and clinical outcomes lies in the lack of clear information on what happens at the nano-bio interface. The formation of the PC around NPs led many research groups to consider the biological identity of NPs as a fundamental actor in the definition of NPs’ biological fate. Many studies have investigated the proteins that compose the PCs of many different organic and inorganic NPs; however, results from different laboratories sometimes did not match, even when the same nanomaterial was employed.85,86 With the introduction of the new concept of PPC, the widely accepted view that identical nanomaterials have similar or identical toxic effects on individuals with different pathological conditions should be considered outdated. Data from a single patient cannot be generalized to other patients. Additionally, each individual exhibits a distinct plasma proteome on the basis of his/her specific health conditions, gender, lifestyle, and genetic background, leading to the formation of a PPC around therapeutic NPs. Characterizing disease-related PPCs can help in the prediction of the biological outcomes of NPs and in turn speed up clinical translation. In the near future, we can expect to witness the development of disease-specific custom NPs.
Conclusions
To date, the majority of investigations on phenomena at the nano-bio interface have overlooked the contribution of the physiological environment to PC formation, focused instead on the effects of the NPs’ properties on the PC. Differences in the PC based on the biological environment can help explain various discordant findings of recent years, such as i) the considerable variability in results among different research groups analyzing PCs formed on the same NPs; ii) variations between in vitro and in vivo studies; iii) differences between cell lines with different media; and more importantly iv) the unsuccessful clinical results of NPs that had shown promising in vitro and in vivo results. A large body of work must be carried out to gain a better understanding of nano-bio interactions. We believe that the novel concept of the personalized protein corona, combined with other recent findings regarding the role of the biological milieu in the PC’s formation, will allow us to better design future experiments in this field and accelerate clinical translation.
Acknowledgments
This work was supported by the grants US National Institutes of Health (NIH) CA151884 (O.C.F.) and EB015419 (O.C.F.). We thank Servier Medical Art for the high-quality image bank.
Footnotes
Competing interests statement:
O.C.F. declares financial interests in Selecta Biosciences, Tarveda Therapeutics and Placon Therapeutics.
References
- 1.Monopoli MP, Åberg C, Salvati A, Dawson KA. Nat Nanotechnol. 2012;7:779–786. doi: 10.1038/nnano.2012.207. [DOI] [PubMed] [Google Scholar]
- 2.Wan S, Kelly PM, Mahon E, Stöckmann H, Rudd PM, Caruso F, Dawson KA, Yan Y, Monopoli MP. ACS Nano. 2015;9:2157–2166. doi: 10.1021/nn506060q. [DOI] [PubMed] [Google Scholar]
- 3.Hellstrand E, Lynch I, Andersson A, Drakenberg T, Dahlbäck B, Dawson KA, Linse S, Cedervall T. FEBS J. 2009;276:3372–3381. doi: 10.1111/j.1742-4658.2009.07062.x. [DOI] [PubMed] [Google Scholar]
- 4.Mahmoudi M, Bertrand N, Zope H, Farokhzad OC. Nano Today. 2016 [Google Scholar]
- 5.Safavi-Sohi R, Maghari S, Raoufi M, Jalali SA, Hajipour MJ, Ghassempour A, Mahmoudi M. ACS Appl Mater Interfaces. 2016;8:22808–22818. doi: 10.1021/acsami.6b05099. [DOI] [PubMed] [Google Scholar]
- 6.Monopoli MP, Walczyk D, Campbell A, Elia G, Lynch I, Baldelli Bombelli F, Dawson KA. J Am Chem Soc. 2011;133:2525–2534. doi: 10.1021/ja107583h. [DOI] [PubMed] [Google Scholar]
- 7.Tenzer S, Docter D, Kuharev J, Musyanovych A, Fetz V, Hecht R, Schlenk F, Fischer D, Kiouptsi K, Reinhardt C, Landfester K, Schild H, Maskos M, Knauer SK, Stauber RH. Nat Nanotechnol. 2013;8:772–781. doi: 10.1038/nnano.2013.181. [DOI] [PubMed] [Google Scholar]
- 8.Koh WL, Tham PH, Yu H, Leo HL, Yong Kah JC. Nanomed. 2016;11:2275–2287. doi: 10.2217/nnm-2016-0173. [DOI] [PubMed] [Google Scholar]
- 9.Tasciotti E, Molinaro R, Taraballi F, Toledano Furman N, Sherman M, Parodi A, Salvatore F, Corbo C. Int J Nanomedicine. 2016;11:3049–3063. doi: 10.2147/IJN.S109059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Corbo C, Molinaro R, Parodi A, Toledano Furman NE, Salvatore F, Tasciotti E. Nanomed. 2016;11:81–100. doi: 10.2217/nnm.15.188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mahmoudi M, Lynch I, Ejtehadi MR, Monopoli MP, Bombelli FB, Laurent S. Chem Rev. 2011;111:5610–5637. doi: 10.1021/cr100440g. [DOI] [PubMed] [Google Scholar]
- 12.Saha K, Rahimi M, Yazdani M, Kim ST, Moyano DF, Hou S, Das R, Mout R, Rezaee F, Mahmoudi M, Rotello VM. ACS Nano. 2016;10:4421–4430. doi: 10.1021/acsnano.6b00053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bigdeli A, Palchetti S, Pozzi D, Hormozi-Nezhad MR, Baldelli Bombelli F, Caracciolo G, Mahmoudi M. ACS Nano. 2016;10:3723–3737. doi: 10.1021/acsnano.6b00261. [DOI] [PubMed] [Google Scholar]
- 14.Caracciolo G, Pozzi D, Capriotti AL, Cavaliere C, Foglia P, Amenitsch H, Laganà A. Langmuir. 2011;27:15048–15053. doi: 10.1021/la202912f. [DOI] [PubMed] [Google Scholar]
- 15.Mahmoudi M, Abdelmonem AM, Behzadi S, Clement JH, Dutz S, Ejtehadi MR, Hartmann R, Kantner K, Linne U, Maffre P, Metzler S, Moghadam MK, Pfeiffer C, Rezaei M, Ruiz-Lozano P, Serpooshan V, Shokrgozar MA, Nienhaus GU, Parak WJ. ACS Nano. 2013;7:6555–6562. doi: 10.1021/nn305337c. [DOI] [PubMed] [Google Scholar]
- 16.Schöttler S, Klein K, Landfester K, Mailänder V. Nanoscale. 2016;8:5526–5536. doi: 10.1039/c5nr08196c. [DOI] [PubMed] [Google Scholar]
- 17.Pozzi D, Caracciolo G, Capriotti AL, Cavaliere C, La Barbera G, Anchordoquy TJ, Laganà A. J Proteomics. 2015;119:209–217. doi: 10.1016/j.jprot.2015.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pozzi D, Caracciolo G, Digiacomo L, Colapicchioni V, Palchetti S, Capriotti AL, Cavaliere C, Zenezini Chiozzi R, Puglisi A, Laganà A. Nanoscale. 2015;7:13958–13966. doi: 10.1039/c5nr03701h. [DOI] [PubMed] [Google Scholar]
- 19.Mahmoudi M, Lohse SE, Murphy CJ, Fathizadeh A, Montazeri A, Suslick KS. Nano Lett. 2014;14:6–12. doi: 10.1021/nl403419e. [DOI] [PubMed] [Google Scholar]
- 20.Hajipour MJ, Laurent S, Aghaie A, Rezaee F, Mahmoudi M. Biomater Sci. 2014;2:1210. doi: 10.1039/c4bm00131a. [DOI] [PubMed] [Google Scholar]
- 21.Rajendran P, Rengarajan T, Thangavel J, Nishigaki Y, Sakthisekaran D, Sethi G, Nishigaki I. Int J Biol Sci. 2013;9:1057–1069. doi: 10.7150/ijbs.7502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Beck HC, Overgaard M, Melholt Rasmussen L. Transl Proteomics. 2015;7:40–48. [Google Scholar]
- 23.Surinova S, Schiess R, Hüttenhain R, Cerciello F, Wollscheid B, Aebersold R. J Proteome Res. 2011;10:5–16. doi: 10.1021/pr1008515. [DOI] [PubMed] [Google Scholar]
- 24.Kiddle SJ, Steves CJ, Mehta M, Simmons A, Xu X, Newhouse S, Sattlecker M, Ashton NJ, Bazenet C, Killick R, Adnan J, Westman E, Nelson S, Soininen H, Kloszewska I, Mecocci P, Tsolaki M, Vellas B, Curtis C, Breen G, Williams SCR, Lovestone S, Spector TD, Dobson RJB. Transl Psychiatry. 2015;5:e584. doi: 10.1038/tp.2015.78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Schley G, Köberle C, Manuilova E, Rutz S, Forster C, Weyand M, Formentini I, Kientsch-Engel R, Eckardt K-U, Willam C. PLOS ONE. 2015;10:e0145042. doi: 10.1371/journal.pone.0145042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Colapicchioni V, Tilio M, Digiacomo L, Gambini V, Palchetti S, Marchini C, Pozzi D, Occhipinti S, Amici A, Caracciolo G. Int J Biochem Cell Biol. 2016;75:180–187. doi: 10.1016/j.biocel.2015.09.002. [DOI] [PubMed] [Google Scholar]
- 27.Hanash SM, Pitteri SJ, Faca VM. Nature. 2008;452:571–579. doi: 10.1038/nature06916. [DOI] [PubMed] [Google Scholar]
- 28.Blennow K, Hampel H, Weiner M, Zetterberg H. Nat Rev Neurol. 2010;6:131–144. doi: 10.1038/nrneurol.2010.4. [DOI] [PubMed] [Google Scholar]
- 29.Addona TA, Abbatiello SE, Schilling B, Skates SJ, Mani DR, Bunk DM, Spiegelman CH, Zimmerman LJ, Ham A-JL, Keshishian H, Hall SC, Allen S, Blackman RK, Borchers CH, Buck C, Cardasis HL, Cusack MP, Dodder NG, Gibson BW, Held JM, Hiltke T, Jackson A, Johansen EB, Kinsinger CR, Li J, Mesri M, Neubert TA, Niles RK, Pulsipher TC, Ransohoff D, Rodriguez H, Rudnick PA, Smith D, Tabb DL, Tegeler TJ, Variyath AM, Vega-Montoto LJ, Wahlander Å, Waldemarson S, Wang M, Whiteaker JR, Zhao L, Anderson NL, Fisher SJ, Liebler DC, Paulovich AG, Regnier FE, Tempst P, Carr SA. Nat Biotechnol. 2009;27:633–641. doi: 10.1038/nbt.1546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Xu A. Clin Chem. 2006;52:405–413. doi: 10.1373/clinchem.2005.062463. [DOI] [PubMed] [Google Scholar]
- 31.El-Agnaf OMA. FASEB J. 2006;20:419–425. doi: 10.1096/fj.03-1449com. [DOI] [PubMed] [Google Scholar]
- 32.Hurst JR, Donaldson GC, Perera WR, Wilkinson TMA, Bilello JA, Hagan GW, Vessey RS, Wedzicha JA. Am J Respir Crit Care Med. 2006;174:867–874. doi: 10.1164/rccm.200604-506OC. [DOI] [PubMed] [Google Scholar]
- 33.Riethdorf S, Fritsche H, Muller V, Rau T, Schindlbeck C, Rack B, Janni W, Coith C, Beck K, Janicke F, Jackson S, Gornet T, Cristofanilli M, Pantel K. Clin Cancer Res. 2007;13:920–928. doi: 10.1158/1078-0432.CCR-06-1695. [DOI] [PubMed] [Google Scholar]
- 34.Petricoin EF, Belluco C, Araujo RP, Liotta LA. Nat Rev Cancer. 2006;6:961–967. doi: 10.1038/nrc2011. [DOI] [PubMed] [Google Scholar]
- 35.Mitchell PS, Parkin RK, Kroh EM, Fritz BR, Wyman SK, Pogosova-Agadjanyan EL, Peterson A, Noteboom J, O’Briant KC, Allen A, Lin DW, Urban N, Drescher CW, Knudsen BS, Stirewalt DL, Gentleman R, Vessella RL, Nelson PS, Martin DB, Tewari M. Proc Natl Acad Sci. 2008;105:10513–10518. doi: 10.1073/pnas.0804549105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lokhov PG, Dashtiev MI, Moshkovskii SA, Archakov AI. Metabolomics. 2010;6:156–163. [Google Scholar]
- 37.Diamandis EP, van der Merwe DE. Clin Cancer Res. 2005;11:963–965. [PubMed] [Google Scholar]
- 38.Qiu Y, Patwa TH, Xu L, Shedden K, Misek DE, Tuck M, Jin G, Ruffin MT, Turgeon DK, Synal S, Bresalier R, Marcon N, Brenner DE, Lubman DM. J Proteome Res. 2008;7:1693–1703. doi: 10.1021/pr700706s. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bollineni RC, Fedorova M, Blüher M, Hoffmann R. J Proteome Res. 2014;13:5081–5093. doi: 10.1021/pr500324y. [DOI] [PubMed] [Google Scholar]
- 40.Engström G, Stavenow L, Hedblad B, Lind P, Eriksson K-F, Janzon L, Lindgärde F. Diabetes. 2003;52:442–447. doi: 10.2337/diabetes.52.2.442. [DOI] [PubMed] [Google Scholar]
- 41.Engstrom G, Hedblad B, Stavenow L, Lind P, Janzon L, Lindgarde F. Diabetes. 2003;52:2097–2101. doi: 10.2337/diabetes.52.8.2097. [DOI] [PubMed] [Google Scholar]
- 42.Engstrom G. Circulation. 2002;105:2632–2637. doi: 10.1161/01.cir.0000017327.69909.ff. [DOI] [PubMed] [Google Scholar]
- 43.Engström G, Hedblad B, Tydén P, Lindgärde F. Atherosclerosis. 2009;202:617–622. doi: 10.1016/j.atherosclerosis.2008.05.038. [DOI] [PubMed] [Google Scholar]
- 44.Lind P, Hedblad B, Stavenow L, Janzon L, Eriksson KF, Lindgärde F. Arterioscler Thromb Vasc Biol. 2001;21:452–458. doi: 10.1161/01.atv.21.3.452. [DOI] [PubMed] [Google Scholar]
- 45.Ridker PM, Hennekens CH, Buring JE, Rifai N. N Engl J Med. 2000;342:836–843. doi: 10.1056/NEJM200003233421202. [DOI] [PubMed] [Google Scholar]
- 46.N Engl J Med. 2000;343:512–513. [Google Scholar]
- 47.Festa A, D’Agostino R, Tracy RP, Haffner SM. Diabetes. 2002;51:1131–1137. doi: 10.2337/diabetes.51.4.1131. [DOI] [PubMed] [Google Scholar]
- 48.Korantzopoulos P, Kolettis T, Siogas K, Goudevenos J. Med Sci Monit Int Med J Exp Clin Res. 2003;9:RA225–229. [PubMed] [Google Scholar]
- 49.Danesh J, Wheeler JG, Hirschfield GM, Eda S, Eiriksdottir G, Rumley A, Lowe GDO, Pepys MB, Gudnason V. N Engl J Med. 2004;350:1387–1397. doi: 10.1056/NEJMoa032804. [DOI] [PubMed] [Google Scholar]
- 50.Lowe GDO. J Thromb Haemost. 2005;3:1618–1627. doi: 10.1111/j.1538-7836.2005.01416.x. [DOI] [PubMed] [Google Scholar]
- 51.2015 BiochemDen.com.
- 52.Cedervall T, Lynch I, Lindman S, Berggard T, Thulin E, Nilsson H, Dawson KA, Linse S. Proc Natl Acad Sci. 2007;104:2050–2055. doi: 10.1073/pnas.0608582104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Nel AE, Mädler L, Velegol D, Xia T, Hoek EMV, Somasundaran P, Klaessig F, Castranova V, Thompson M. Nat Mater. 2009;8:543–557. doi: 10.1038/nmat2442. [DOI] [PubMed] [Google Scholar]
- 54.Don BR, Kaysen G. Semin Dial. 2004;17:432–437. doi: 10.1111/j.0894-0959.2004.17603.x. [DOI] [PubMed] [Google Scholar]
- 55.Muenchhoff J, Poljak A, Thalamuthu A, Gupta VB, Chatterjee P, Raftery M, Masters CL, Morris JC, Bateman RJ, Fagan AM, Martins RN, Sachdev PS. Sci Rep. 2016;6:29078. doi: 10.1038/srep29078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Thambisetty M, Tripaldi R, Riddoch-Contreras J, Hye A, An Y, Campbell J, Sojkova J, Kinsey A, Lynham S, Zhou Y, Ferrucci L, Wong DF, Lovestone S, Resnick SM. J Alzheimers Dis JAD. 2010;22:1099–1109. doi: 10.3233/JAD-2010-101350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Song C, Dinan T, Leonard BE. J Affect Disord. 1994;30:283–288. doi: 10.1016/0165-0327(94)90135-x. [DOI] [PubMed] [Google Scholar]
- 58.Hye A, Lynham S, Thambisetty M, Causevic M, Campbell J, Byers HL, Hooper C, Rijsdijk F, Tabrizi SJ, Banner S, Shaw CE, Foy C, Poppe M, Archer N, Hamilton G, Powell J, Brown RG, Sham P, Ward M, Lovestone S. Brain. 2006;129:3042–3050. doi: 10.1093/brain/awl279. [DOI] [PubMed] [Google Scholar]
- 59.ManafiRad A, Farzadfar F, Habibi L, Azhdarzadeh M, Aghaverdi H, Tehrani KH, Lotfi M, Kehoe PG, Sheidaei A, Ghasemian A, Darzi ER, Mahmoodi R, Mahmoudi M. J Alzheimers Dis. 2014;42:69–85. doi: 10.3233/JAD-140321. [DOI] [PubMed] [Google Scholar]
- 60.Scott AM, Wolchok JD, Old LJ. Nat Rev Cancer. 2012;12:278–287. doi: 10.1038/nrc3236. [DOI] [PubMed] [Google Scholar]
- 61.Zheng T, Pierre-Pierre N, Yan X, Huo Q, Almodovar AJO, Valerio F, Rivera-Ramirez I, Griffith E, Decker DD, Chen S, Zhu N. ACS Appl Mater Interfaces. 2015;7:6819–6827. doi: 10.1021/acsami.5b00371. [DOI] [PubMed] [Google Scholar]
- 62.Perfézou M, Turner A, Merkoçi A. Chem Soc Rev. 2012;41:2606–2622. doi: 10.1039/c1cs15134g. [DOI] [PubMed] [Google Scholar]
- 63.Bakhtiary Z, Saei AA, Hajipour MJ, Raoufi M, Vermesh O, Mahmoudi M. Nanomedicine Nanotechnol Biol Med. 2016;12:287–307. doi: 10.1016/j.nano.2015.10.019. [DOI] [PubMed] [Google Scholar]
- 64.Casals E, Pfaller T, Duschl A, Oostingh GJ, Puntes V. ACS Nano. 2010;4:3623–3632. doi: 10.1021/nn901372t. [DOI] [PubMed] [Google Scholar]
- 65.Teichroeb JH, Forrest JA, Jones LW. Eur Phys J E. 2008;26:411–415. doi: 10.1140/epje/i2007-10342-9. [DOI] [PubMed] [Google Scholar]
- 66.Shang W, Nuffer JH, Dordick JS, Siegel RW. Nano Lett. 2007;7:1991–1995. doi: 10.1021/nl070777r. [DOI] [PubMed] [Google Scholar]
- 67.Lundqvist M, Sethson I, Jonsson BH. Langmuir. 2004;20:10639–10647. doi: 10.1021/la0484725. [DOI] [PubMed] [Google Scholar]
- 68.Lynch I, Salvati A, Dawson KA. Nat Nanotechnol. 2009;4:546–547. doi: 10.1038/nnano.2009.248. [DOI] [PubMed] [Google Scholar]
- 69.Deng ZJ, Liang M, Monteiro M, Toth I, Minchin RF. Nat Nanotechnol. 2011;6:39–44. doi: 10.1038/nnano.2010.250. [DOI] [PubMed] [Google Scholar]
- 70.Lishko VK, Podolnikova NP, Yakubenko VP, Yakovlev S, Medved L, Yadav SP, Ugarova TP. J Biol Chem. 2004;279:44897–44906. doi: 10.1074/jbc.M408012200. [DOI] [PubMed] [Google Scholar]
- 71.Carrell RW, Gooptu B. Curr Opin Struct Biol. 1998;8:799–809. doi: 10.1016/s0959-440x(98)80101-2. [DOI] [PubMed] [Google Scholar]
- 72.Conway KA, Harper JD, Lansbury PT. Biochemistry (Mosc) 2000;39:2552–2563. doi: 10.1021/bi991447r. [DOI] [PubMed] [Google Scholar]
- 73.Chiti F, Dobson CM. Annu Rev Biochem. 2006;75:333–366. doi: 10.1146/annurev.biochem.75.101304.123901. [DOI] [PubMed] [Google Scholar]
- 74.Kelly JW. Curr Opin Struct Biol. 1996;6:11–17. doi: 10.1016/s0959-440x(96)80089-3. [DOI] [PubMed] [Google Scholar]
- 75.Yim MB, Kang JH, Yim HS, Kwak HS, Chock PB, Stadtman ER. Proc Natl Acad Sci U S A. 1996;93:5709–5714. doi: 10.1073/pnas.93.12.5709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Hayden MR, Tyagi SC, Kerklo MM, Nicolls MR. JOP J Pancreas. 2005;6:287–302. [PubMed] [Google Scholar]
- 77.Lo Giudice MC, Herda LM, Polo E, Dawson KA. Nat Commun. 2016;7:13475. doi: 10.1038/ncomms13475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Hajipour MJ, Raheb J, Akhavan O, Arjmand S, Mashinchian O, Rahman M, Abdolahad M, Serpooshan V, Laurent S, Mahmoudi M. Nanoscale. 2015;7:8978–8994. doi: 10.1039/c5nr00520e. [DOI] [PubMed] [Google Scholar]
- 79.An SS, Wu SY, Hulme J. Int J Nanomedicine. 2015;9 doi: 10.2147/IJN.S88285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Shannahan JH, Fritz KS, Raghavendra AJ, Podila R, Persaud I, Brown JM. Toxicol Sci. 2016;152:406–416. doi: 10.1093/toxsci/kfw097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Molinaro R, Boada C, del Rosal GM, Hartman KA, Corbo C, Andrews ED, Toledano-Furman NE, Cooke JP, Tasciotti E. Methodist DeBakey Cardiovasc J. 2016;12:169–174. doi: 10.14797/mdcj-12-3-169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Han SG, Newsome B, Hennig B. Toxicology. 2013;306:1–8. doi: 10.1016/j.tox.2013.01.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Vesterdal LK, Mikkelsen L, Folkmann JK, Sheykhzade M, Cao Y, Roursgaard M, Loft S, Møller P. Toxicol Lett. 2012;214:19–26. doi: 10.1016/j.toxlet.2012.07.022. [DOI] [PubMed] [Google Scholar]
- 84.Wingard CJ, Walters DM, Cathey BL, Hilderbrand SC, Katwa P, Lin S, Ke PC, Podila R, Rao A, Lust RM, Brown JM. Nanotoxicology. 2011;5:531–545. doi: 10.3109/17435390.2010.530004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Alkilany AM, Mahmoud NN, Hashemi F, Hajipour MJ, Farvadi F, Mahmoudi M. Chem Res Toxicol. 2016;29:943–948. doi: 10.1021/acs.chemrestox.6b00108. [DOI] [PubMed] [Google Scholar]
- 86.Azhdarzadeh M, Saei AA, Sharifi S, Hajipour MJ, Alkilany AM, Sharifzadeh M, Ramazani F, Laurent S, Mashaghi A, Mahmoudi M. Nanomed. 2015;10:2931–2952. doi: 10.2217/nnm.15.130. [DOI] [PubMed] [Google Scholar]


