Introduction
Moldova, a land-locked country of 3 million people in Eastern Europe that borders Romania and Ukraine, has rising HIV incidence, especially among people who inject drugs (PWID). HIV prevalence in PWIDs is estimated as 28% (UNAIDS, 2014) and criminalization of drugs results in PWIDs being concentrated within the criminal justice system, and therefore in increased numbers of people living with HIV (PLH) in prisons (Walmsley, 2014). For example, HIV prevalence in Moldova is 0.7% nationally, yet 2.7-fold greater (1.9%) among prisoners. Similar to other countries of the former Soviet Union (FSU), HIV, PWID and incarceration in Moldova are syndemic (Dolan et al., 2007). Unless internationally recommended evidence-based harm reduction programs like opioid agonist therapies (OAT) with methadone and buprenorphine and needle/syringe exchange programs (NSP) are implemented, there is a risk of HIV transmission being amplified in prisons, as well as the risks of relapse to drug use and overdose after release (Dolan et al., 2015).
OAT is internationally recognized as the most effective form of treatment for chronic opioid dependence; only methadone is available in Moldova. OAT reduces HIV transmission, criminal activity, relapse to drug use, overdose and recidivism (Keen, Rowse, Mathers, Campbell, & Seivewright, 2000; Mattick, Breen, Kimber, & Davoli, 2009). For PLH, it improves access to HIV care, ART adherence, retention in HIV care and viral suppression (Altice, Kamarulzaman, Soriano, Schechter, & Friedland, 2010). Despite this wealth of evidence and unlike most of Western Europe, Moldova, Armenia and Kyrgyzstan are the only FSU countries that have implemented OAT in prisons. Restrictions on OAT expansion in the region are in part due to continued and pervasive influence of Russian Federation; where evidence-based harm reduction services like needle exchange programs and OAT are viewed as corrupting influences of the West (Wolfe, 2007). Moldova’s harm reduction programs in prisons are progressive relative to other countries in the region, where high levels of stigma and prejudice towards OAT prevail (Kazatchkine, 2014). Despite a decade of experience with OAT in Moldova, however, expansion within prison has been slow, with many eligible patients in prisons and communities refusing to enroll. Nationally, only 880 patients are on OAT, with 259 (29.4%) patients enrolled in seven prisons where they are tapered off methadone before release (Zabransky et al., 2012).
OAT scale-up efforts have been thwarted on many fronts in FSU countries, and have been influenced more by moral biases and prejudices than by the scientific evidence (Torrens, Fonseca, Castillo, & Domingo-Salvany, 2013). Even where the legal framework supports OAT expansion, negative attitudes remain a significant barrier to OAT enrollment, while positive attitudes promote treatment entry and retention (Peterson et al., 2010). Currently, no data explore attitudes toward OAT among prisoners in FSU countries, where such attitudes are often amplified within prison subcultures where PWIDs are concentrated.
Materials and methods
Participants
A comparison study of 56 opioid-dependent PWIDs that were recently released from prison was conducted to better understand suboptimal OAT enrollment in Moldovan prisons, where it is readily available. Eligibility included: (1) age ≥18 years; (2) ICD-10 criteria for opioid dependence; and (3) released to communities within the past 3 months where OAT was available in both prisons and communities. Participants were recruited from a NGO that provides HIV prevention services to current and former prisoners. Recently released prisoners were assessed to avoid within-prison repercussions for participation. OAT group participants (N = 29) were compared to those in the No OAT group (N = 27) because we expected them to differ in their attitudes and within-prison experiences. In June 2014, eligible and consented participants met with trained staff in Chisinau and Balti, Moldova’s only two cities that provide OAT where they completed an anonymous online survey and were paid ~$10 USD after completion. Institutional review boards at Yale University and the Ukrainian Institute on Public Health Policy approved the study.
Hypotheses
Because current research shows the attitudes toward OAT is negative within the region (Polonsky et al., 2015), we anticipated them to be low in Moldova as well. We expect those who have received OAT in prisons to hold higher knowledge about the benefits of OAT, subscribe less to myths about OAT, have more positive attitudes toward OAT, and perceive OAT to be more effective, relative to PWIDs who have not received OAT during incarceration. We also hypothesized that stigma and negative attitudes toward OAT will translate into different within-prison experiences for these two groups and we therefore explicitly explored differences in their experience with bullying and perceived personal safety.
Measures
We hypothesized that those receiving OAT within prison would potentially differ in terms of their OAT attitudes and knowledge, as well as harassment experiences. Several standardized scales were used, including a 10-item, seven-point Likert-type response instrument assessing OST knowledge and attitudes (Springer & Bruce, 2008), with higher numbers reflecting higher knowledge and positive attitudes. OAT knowledge (α = 0.89) used four seven-point Likert-type items that measured an individual’s knowledge about the positive effects of OAT on other health outcomes. An example of a knowledge item is “OAT improves adherence to HIV medications in HIV-infected, opioid dependent individuals.” OAT attitudes (α = 0.90), consisted of six items which measured an individual’s favorable attitudes toward OAT (e.g., “OAT services should be available in the community so that all people who suffer from opioid addiction and want substitution therapy can receive it”). Myths about methadone (OAT myths, α = 0.81) were measured using 10 five-point Likert-type items with higher scores indicating stronger beliefs in prevailing myths about methadone (e.g., “methadone is a Western conspiracy”). OAT effectiveness (α = 0.79) was measured by four Likert-type items with higher scores indicating higher perceived effectiveness of OAT treatment (e.g., “MMT is an effective treatment for drug addiction”). Two harassment constructs included being bullied, and perceived personal safety. Consequences of being a victim of bullying were measured by five items (Bullying, α = 0.77) from Responses to Victimization scale (Ireland, 1999), which used a five-point Likert-type response from 1 “never” to 5 “often” (e.g., “Threaten to harm him/herself”). Personal Safety (Safety, α = 0.78) was measured using a four 5-point Likert-type items with higher numbers indicating higher perceived safety (e.g., “One needs to constantly look over his/her shoulder”).
We also asked the participants whether they have heard that methadone is not a good treatment for drug addiction (yes/no) including the source they might have heard it from: doctors, narcologists (addiction physicians), family members, other prisoners. Finally, we asked the participants to indicate their intention (yes/no) to continue (OAT group) or initiate (No OAT group) OAT treatment in the future.
Analysis
Analyses were conducted using SPSS, version 22. We used correlation and multiple regression to assess multivariate relationships among the variables. Independent sample t-tests were utilized to determine differences between OAT and No OAT groups in attitudinal constructs (OAT attitudes, myths, and effectiveness), OAT knowledge, as well as within-prison harassment experiences (bullying and perceived personal safety), and the effect size Cohen’s d (noted a “d” throughout) for each mean comparison was calculated separately. Non-parametric procedures (i.e., chi-square and descriptive statistics) were used to analyze study participants’ categorical responses.
Results
The sample consisted of 56 OAT and No OAT participants who did not differ demographically: mean age = 36 years, female (20%), and unmarried (47%). While OAT knowledge and attitudes correlated with each other, as did the three harassment constructs, there were no relationships among the attitudinal and harassment variables. The results of multiple regression with OAT knowledge and myths as predictors and OAT attitudes as an outcome produced R2 = 0.44, F(2, 54) = 20.11, p < 0.01, and revealed that knowledge about OAT (β = 0.43, p < 0.01) and myths about OAT (β = −0.40, p < 0.01) have had independent opposing effects of a similar magnitude on OAT attitudes.
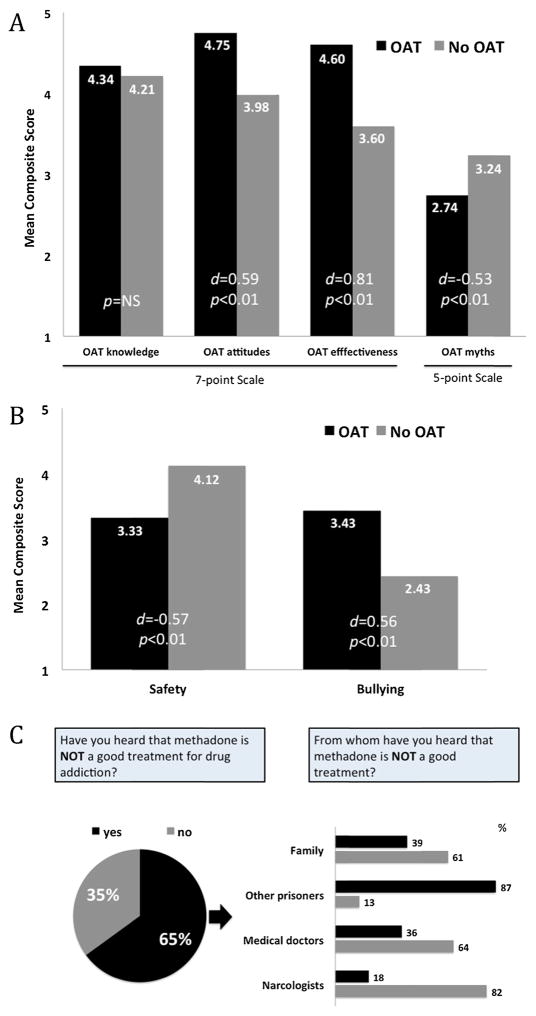
Fig. 1A demonstrates differences between OAT and No OAT groups. Aside from OAT knowledge (t(55) = 0.49, p = 0.62), all attitudinal variables differed significantly. Compared to PWIDs who didn’t receive within-prison OAT, those who did held more positive attitudes (M = 4.75, SD = 0.68 vs. 3.98, SD = 1.69, t(55) = 2.27, p < 0.05, d = 0.59), perceived OAT effectiveness to be higher (M = 4.60, SD = 0.72 vs. M = 3.60, SD = 1.60, t(54) = 3.06, p < 0.01, d = 0.81), and were less likely to endorse myths about OAT (M = 2.74, SD = 0.80 vs. M = 3.24, SD = 1.08, t(55) = −2.01, p < 0.05, d = −0.53). Harassment experiences also differed (Fig. 1B). Compared to PWIDs not receiving within-prison OAT, those who did were significantly less likely to report feeling safe (M = 3.33, SD = 1.40 vs. M = 4.12, SD = 1.37, t(55) = −2.114, p < 0.05, d = −0.57) and more likely to have been bullied (M = 3.43, SD = 1.77 vs. M = 2.43, SD = 1.77, t(55) = 2.15, p < 0.05, d = 0.56).
Fig. 1.
(A) Group differences for knowledge, attitudes, effectiveness, and. myths about opioid agonist therapy (OST); (B) Differences in Perceived Personal Safety and Bullying; (C) The origin of the view that opioid agonist therapy is not a good treatment for opioid addiction.
Nearly two-thirds (65%) had previously heard that methadone was not a “good” treatment for addiction (Fig. 1C). Among these, most (87%) had heard this from other prisoners, while a critical minority had also heard this from physicians (39%) and family members (36%). Finally, only one participant in the No OAT group expressed the intention to initiate OAT treatment in the future, while five participants in the OAT group expressed the desire to discontinue OAT.
Discussion
To our knowledge, this is the first study to explore OAT attitudes and harassment experiences among prisoners in a FSU country where OAT is readily available within prisons and where comparisons can be made between those accessing and not accessing OAT. We found that higher knowledge about OAT was associated with positive attitudes toward OAT, echoing similar findings among Ukrainian prison personnel, where OAT knowledge was positively correlated with OAT attitudes (Polonsky et al., 2015). Importantly and to our surprise, however, we found that OAT knowledge and myths had opposing and independent effects on OAT attitudes, and that knowledge did not differ between the two groups, but that attitudes toward and myths about OAT did. These results imply that knowledge and myths about methadone may coexist and are not mutually exclusive, and illustrate that ideological origins of attitudes count just as much as accurate information. That is, a person may know about the benefits of OAT, and yet, be prejudiced against it, which is supported by seminal psychological work on attitude formation (Zajonc, 1980).
After a decade of treating and educating prisoners about OAT in Moldova, our findings reveal a potential ceiling effect of knowledge-based interventions that do not also focus on affective and ideological aspects of prevailing attitudes (Breckler, 1984). It can be argued that although PWIDs in Moldova are relatively well-informed about OAT, they are embedded within a stigmatizing prison culture that is against it and therefore may be continuously exposed to and endorse negative myths about OAT. Similar to being the amplifiers of diseases (Azbel, Wickersham, Grishaev, Dvoryak, & Altice, 2013; Springer & Altice, 2007, chap. 30), prisons may also serve as amplifiers of prejudice and stigmatizing attitudes toward OAT. Moreover, while other prisoners seem to be the source of most negative attitudes toward OAT, both physicians and family members also reinforce these notions, which may influence both prison- and community-based OAT expansion. Successful interventions, including peer-driven interventions (Broadhead et al., 1998, 2002), are likely to target primarily other prisoners, but comprehensively incorporate physicians, family and prison personnel.
Our results underscore the negative impact of within-prison harassment, as bullying was higher and personal safety lower among those that actually accessed within-prison OAT. In the presence of high levels of negative attitudes toward OAT by other prisoners, many prisoners do not access the treatment. We believe these interpersonal negative influences contribute to the unwillingness expressed by those not on methadone to consider enrolling in treatment post-release, and the intention to discontinue it expressed by those who received methadone within prison. These effects undermine both within-prison and community OAT expansion efforts.
Though not measured here, some of perpetuation of negative OAT attitudes and myths, alongside the increased harassment towards OAT patients, might be explained due to within-prison instigated and perpetuated stigma and discrimination. Stigma is propagated to maintain power and to reinforce social hierarchies, and in controlled prison settings, would likely be wielded for power-related purposes. OAT patients are likely to feel stigmatized or discriminated against in prison individually and/or as a group, and may become alienated, ostracized, and harassed by other prisoners (Kurzban and Leary, 2001). The role of stigma in interpersonal and inter-group violence is manifest here as bullying and concerns about personal safety (Schaller and Neuberg, 2008, 2012).
Last, OAT implementation and enrollment in Moldovan prisons are influenced by ideological biases and myths that are largely formed, reinforced, and often magnified behaviorally in restricted prison settings. Future interventions that expand OAT in prisons should target individual-level myths and ideological prejudices, potentially through peer-driven interventions that harness the collection power of other prisoners or former prisoners who have had positive experiences with OAT, as well as the prisoner environment.
Acknowledgments
Funding
This research received funding from the National Institute on Drug Abuse for research (R01 DA029910, Altice, PI and R01 DA033679), career development (K24 DA017072 for Altice and K01 DA038529 for Wickersham), and the NIH Fogarty Research Training Grant (R25 TW009338, Polonsky).
Footnotes
Conflict of interest
All authors declare that they have no conflicts of interest.
References
- Altice FL, Kamarulzaman A, Soriano VV, Schechter M, Friedland GH. Treatment of medical, psychiatric, and substance-use comorbidities in people infected with HIV who use drugs. Lancet. 2010;376(9738):367–387. doi: 10.1016/S0140-6736(10)60829-X. http://dx.doi.org/10.1016/S0140-6736(10)60829-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Azbel L, Wickersham JA, Grishaev Y, Dvoryak S, Altice FL. Burden of infectious diseases, substance use disorders, and mental illness among Ukrainian prisoners transitioning to the community. PLOS ONE. 2013;8(3):e59643. doi: 10.1371/journal.pone.0059643. http://dx.doi.org/10.1371/journal.pone.0059643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breckler SJ. Empirical validation of affect, behavior, and cognition as distinct components of attitude. Journal of Personality and Social Psychology. 1984;47(6):1191. doi: 10.1037//0022-3514.47.6.1191. [DOI] [PubMed] [Google Scholar]
- Broadhead RS, Heckathorn DD, Altice FL, van Hulst Y, Carbone M, Friedland GH, et al. Increasing drug users’ adherence to HIV treatment: results of a peer-driven intervention feasibility study. Social Science & Medicine. 2002;55(2):235–246. doi: 10.1016/s0277-9536(01)00167-8. Retrieved from: http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=12144138. [DOI] [PubMed] [Google Scholar]
- Broadhead RS, Heckathorn DD, Weakliem DL, Anthony DL, Madray H, Mills RJ, et al. Harnessing peer networks as an instrument for AIDS prevention: results from a peer-driven intervention. Public Health Reports. 1998;113(Suppl 1):42–57. [PMC free article] [PubMed] [Google Scholar]
- Dolan K, Kite B, Black E, Aceijas C, Stimson GV Reference Group on HIV/AIDS Prevention Care among Injecting Drug Users in Developing and Transitional Countries. HIV in prison in low-income and middle-income countries. The Lancet Infectious Diseases. 2007;7(1):32–41. doi: 10.1016/S1473-3099(06)70685-5. http://dx.doi.org/10.1016/S1473-3099(06)70685-5. [DOI] [PubMed] [Google Scholar]
- Dolan K, Moazen B, Noori A, Rahimzadeh S, Farzadfar F, Hariga F. People who inject drugs in prison: HIV prevalence, transmission and prevention. International Journal of Drug Policy. 2015;26(Suppl 1):S12–S15. doi: 10.1016/j.drugpo.2014.10.012. http://dx.doi.org/10.1016/j.drugpo.2014.10.012. [DOI] [PubMed] [Google Scholar]
- Ireland JL. Bullying behaviors among male and female prisoners: A study of adult and young offenders. Aggressive Behavior. 1999;25(3):161–178. [Google Scholar]
- Kazatchkine M. Russia’s ban on methadone for drug users in Crimea will worsen the HIV/AIDS epidemic and risk public health. BMJ: British Medical Journal. 2014:348. doi: 10.1136/bmj.g3118. [DOI] [PubMed] [Google Scholar]
- Keen J, Rowse G, Mathers N, Campbell M, Seivewright N. Can methadone maintenance for heroin-dependent patients retained in general practice reduce criminal conviction rates and time spent in prison? British Journal of General Practice. 2000;50(450):48–49. Retrieved from: http://www.ncbi.nlm.nih.gov/pubmed/10695069. [PMC free article] [PubMed] [Google Scholar]
- Kurzban R, Leary MR. Evolutionary origins of stigmatization: The functions of social exclusion. Psychological Bulletin. 2001;127(2):187–208. doi: 10.1037/0033-2909.127.2.187. [DOI] [PubMed] [Google Scholar]
- Mattick RP, Breen C, Kimber J, Davoli M. Methadone maintenance therapy versus no opioid replacement therapy for opioid dependence. Cochrane Database of Systematic Reviews. 2009;(3):CD002209. doi: 10.1002/14651858.CD002209. http://dx.doi.org/10.1002/14651858.CD002209.pub2. [DOI] [PubMed]
- Peterson JA, Schwartz RP, Mitchell SG, Reisinger HS, Kelly SM, O’Grady KE, et al. Why don’t out-of-treatment individuals enter methadone treatment programmes? International Journal of Drug Policy. 2010;21(1):36–42. doi: 10.1016/j.drugpo.2008.07.004. http://dx.doi.org/10.1016/j.drugpo.2008.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polonsky M, Azbel L, Wickersham JA, Taxman FS, Grishaev E, Dvoryak S, et al. Challenges to implementing opioid substitution therapy in Ukrainian prisons: Personnel attitudes toward addiction, treatment, and people with HIV/AIDS. Drug and Alcohol Dependence. 2015;148:47–55. doi: 10.1016/j.drugalcdep.2014.12.008. http://dx.doi.org/10.1016/j.drugalcdep.2014.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schaller M, Neuberg SL. Intergroup prejudices and intergroup conflicts. In: Crawford C, Krebs DL, editors. Foundations of evolutionary psychology. Mahwah, NJ: Lawrence Erlbaum Associates; 2008. pp. 399–412. [Google Scholar]
- Schaller M, Neuberg SL. Danger, disease, and the nature of prejudice(s) In: Olson JM, Zanna MP, editors. Advances in experimental social psychology. Vol. 46. Burlington, VT: Academic Press; 2012. pp. 1–54. [Google Scholar]
- Springer SA, Altice FL. Public health behind bars: From prisons to communities. New York, NY: Springer Publishing Company; 2007. Improving the care for HIV-infected prisoners: An integrated prison-release health model. [Google Scholar]
- Springer SA, Bruce RD. A pilot survey of attitudes and knowledge about opioid substitution therapy for HIV-infected prisoners. Journal of Opioid Management. 2008;4(2):81. doi: 10.5055/jom.2008.0012. Retrieved from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2476214/pdf/nihms-56896.pdf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Torrens M, Fonseca F, Castillo C, Domingo-Salvany A. Methadone maintenance treatment in Spain: The success of a harm reduction approach. The Bulletin of the World Health Organization. 2013;91(2):136–141. doi: 10.2471/BLT.12.111054. http://dx.doi.org/10.2471/BLT.12.111054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- UNAIDS. 2014 Retrieved from: http://www.unaids.org/en/regionscountries/countries/republicofmoldova.
- Walmsley R. World Prison Population List. (10) 2014 Retrieved from London, England: http://www.prisonstudies.org/sites/prisonstudies.org/files/resources/downloads/wppl_10.pdf.
- Wolfe D. Paradoxes in antiretroviral treatment for injecting drug users: access, adherence and structural barriers in Asia and the former Soviet Union. International Journal of Drug Policy. 2007;18(4):246–254. doi: 10.1016/j.drugpo.2007.01.012. Retrieved from http://ac.els-cdn.com/S0955395907000138/1-s2.0-S0955395907000138-main.pdf?_tid=cf16aa94-8953-11e3-805e-00000aab0f6c&acdnat=1391048060_fa8635062a5e0bedeb90d7dabda5b24c. [DOI] [PubMed] [Google Scholar]
- Zabransky T, Grund JP, Latypov A, Otiashvili D, Stuikyte R, Scutelniciuc O, et al. Harm reduction in substance use and high-risk behaviour: International policy and practice summaries. 2012. Harm reduction in Central and Eastern Europe; pp. 301–321. [Google Scholar]
- Zajonc RB. Feeling and thinking – Preferences need no inferences. American Psychologist. 1980;35(2):151–175. http://dx.doi.org/10.1037//0003-066x.35.2.151. [Google Scholar]