Abstract
Objectives:
Because of state and federal health care reform, local health departments play an increasingly prominent role leading and coordinating disease prevention programs in the United States. This case study shows how a local health department working in chronic disease prevention and management can use systems science and evidence-based decision making to inform program selection, implementation, and assessment; enhance engagement with local health systems and organizations; and possibly optimize health care delivery and population health.
Methods:
The authors built a systems-science agent-based simulation model of diabetes progression for the San Antonio Metropolitan Health District, a local health department, to simulate health and cost outcomes for the population of San Antonio for a 20-year period (2015-2034) using 2 scenarios: 1 in which hemoglobin A1c (HbA1c) values for a population were similar to the current distribution of values in San Antonio, and the other with a hypothetical 1-percentage-point reduction in HbA1c values.
Results:
They projected that a 1-percentage-point reduction in HbA1c would lead to a decrease in the 20-year prevalence of end-stage renal disease from 1.7% to 0.9%, lower extremity amputation from 4.6% to 2.9%, blindness from 15.1% to 10.7%, myocardial infarction from 23.8% to 17.9%, and stroke from 9.8% to 7.2%. They estimated annual direct medical cost savings (in 2015 US dollars) from reducing HbA1c by 1 percentage point ranging from $6842 (myocardial infarction) to $39 800 (end-stage renal disease) for each averted case of diabetes complications.
Conclusions:
Local health departments could benefit from the use of systems science and evidence-based decision making to estimate public health program effectiveness and costs, calculate return on investment, and develop a business case for adopting programs.
Keywords: agent-based modeling, diabetes, local health departments, population health, systems science
As a result of state and federal health care reform, local health departments play an increasingly prominent role in leading disease prevention efforts and coordinating programs with community-based organizations and health care delivery systems across the United States.1,2 Coordination between local health departments and hospitals has resulted in improved disease monitoring, better surveillance and planning (eg, community health needs assessments), and more efficient coordination of resources.3,4 Payment reform and the shift to value-based care should promote even more collaboration among these groups, and the implementation of more robust local chronic disease prevention efforts is likely to result in health benefits and cost savings. Because local health departments have experience in managing population health strategies, they are well positioned to help bring these groups together and foster the redesign of chronic disease prevention and management programs.5
Local health departments are tasked with a wide spectrum of public health responsibilities, and they must make program decisions with financial and capacity constraints in mind. They are also required to incorporate into those decisions the best scientific evidence available on the effectiveness of any proposed programs or strategies.6–8 Evidence-based decision making entails “making decisions on the basis of the best available scientific evidence, using data and information systems systematically, applying program-planning frameworks, engaging the community in decision making, conducting sound evaluation, and disseminating what is learned.”6 Although most local health departments embrace the use of evidence-based decision making in public health practice, they often encounter implementation difficulties because of a lack of relevant data, resources, or expertise.9,10 In addition, limited research has examined the degree to which some evidence-based practices can be adapted for use in local contexts.11
One promising approach to incorporating evidence-based decision making into public health practice involves the use of systems science. The types of traditional data and statistical analyses often used in public health may be inadequate for studying the complex systems that are most commonly encountered.12 Systems science draws on the natural and social sciences, mathematics, computer science, and engineering to address complex problems. Examples of systems-science methodologies used to study dynamic, interrelated factors are network analysis (eg, to evaluate the connections of various people within a group), system dynamics (eg, to assess population dynamics and feedback loops), and agent-based modeling (eg, to understand the consequences of a person’s actions and the role of interactions with other people). Agent-based modeling is particularly relevant for use in public health because it uses computer simulation to study complex systems by examining how individual elements of a system (agents) behave as a function of individual properties, their environment, and their interactions with each other.12 In addition, agent-based modeling provides powerful “simulation laboratories” in which various types of public health interventions, programs, and policies can be tested when more traditional outcome studies are not possible.12
Interest among public health practitioners and policy makers in applying systems science to answer complex questions and to conduct counterfactual studies (comparing what happens in an intervention with what would have happened in its absence) is growing; the science can be applied to topics ranging from infectious disease control to chronic disease prevention.12–15 Two recent studies demonstrated the potential of systems science to complement public health community-based participatory research as well as dissemination and implementation research.16,17 Community-based participatory research promotes partnerships in which community members, organizational representatives, and researchers participate equitably in all aspects of the research process. Dissemination and implementation research seeks to understand how best to apply scientific advances in the real world, by pushing evidence-based knowledge into routine use. Both types of research are critically important to local health departments as they aim to coordinate population health programs and translate public health knowledge into action.16,17 Indeed, local health departments have used systems science successfully as a cost-effective approach to facilitate evidence-based decision making, through fostering the use of modeling tools to project population health trends, engaging community members and other stakeholders through data visualization, and enabling the comparison of various programs that may improve population health.18
This case study shows how a local health department working in chronic disease prevention and management can use systems science and evidence-based decision making to inform program selection, implementation, and assessment; enhance engagement with local health systems and organizations; and possibly optimize health care delivery and population health. The technical assistance approach and the partnership dynamics described in this study offer actionable lessons and a replicable model of collaboration that can be used by others to inform public health practice in disease prevention and management.
Methods
With funding from the Robert Wood Johnson Foundation, those of us working as researchers at the Center for Health Innovation at The New York Academy of Medicine provided technical assistance to the San Antonio Metropolitan Health District (Metro Health), a local health department, to help project health and cost outcomes (ie, cost-effectiveness) of diabetes prevention and self-management interventions through the use of systems-science simulation modeling. This study was considered exempt from institutional review board approval at The New York Academy of Medicine.
Our technical assistance was intended to support Metro Health’s implementation of its Delivery System Reform Incentive Payment programs. These programs are part of Medicaid delivery-system reform, providing states with funding that can be used to support hospitals and other providers in changing how they provide care to Medicaid beneficiaries. Metro Health’s Delivery System Reform Incentive Payment programs were initiated under the Transformation and Quality Improvement Waiver in Texas.19 Under this Medicaid 1115 waiver, $11.4 billion was made available during a 5-year period (2012-2016) in Texas to help improve public health infrastructure and redesign health care delivery.19 One unique aspect of the Delivery System Reform Incentive Payment program in Texas was the inclusion of public health agencies; the Delivery System Reform Incentive Payment program is typically limited to traditional health care providers.20 Metro Health was one of the public health agencies taking advantage of this new funding opportunity to target highest-priority health issues in its region.
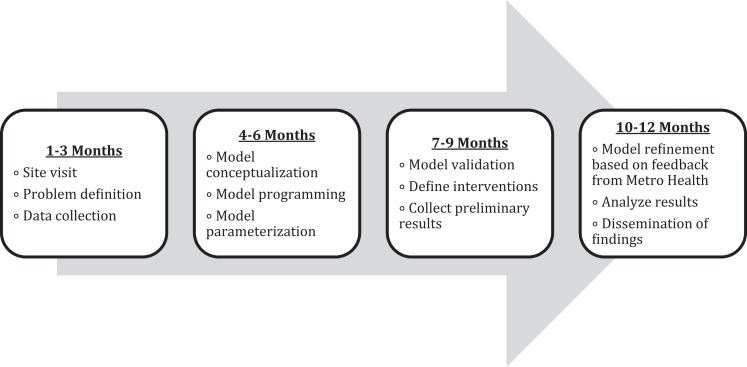
We were enlisted to work with Metro Health on its Delivery System Reform Incentive Payment Community Diabetes Project. The project, which was designed in 2012, had the goal of expanding access to diabetes prevention and management programs for individuals and families in San Antonio, Texas. Our technical assistance project involved a close working relationship with Metro Health for 12 months and included multiple phases along a defined timeline (Figure 1). As part of the project, we provided (1) biweekly communication with all team members, consultants, and stakeholders; (2) instructions on data collection required to support the Delivery System Reform Incentive Payment Community Diabetes Project; (3) progress updates; and (4) simple models and tools that could be used by Metro Health to estimate benefits, costs avoided, and other relevant outcomes of programs to prevent diabetes in the community.
Figure 1.
Timeline of the Center for Health Innovation at The New York Academy of Medicine Technical Assistance Project for the San Antonio Metropolitan Health District Delivery System Reform Incentive Payment Community Diabetes Project, 2015-2016. The Center for Health Innovation provided technical assistance, which included the use of systems-science simulation modeling, to help the San Antonio (Texas) Metropolitan Health District (Metro Health) assess the cost and health outcomes (cost-effectiveness) of diabetes prevention and self-management during a 20-year period (2015-2034).
Agent-Based Modeling
Our technical assistance project also involved providing systems-science simulation modeling to help Metro Health estimate the potential outcomes of diabetes prevention and self-management initiatives. For this task, we built an agent-based model of diabetes progression to simulate health and cost outcomes under various scenarios. The models simulate the simultaneous operations and interactions of multiple agents in an attempt to predict the occurrence of complex phenomena. As a relatively new research tool for public health professionals, agent-based modeling can be used to capture the complex interplay among multiple factors contributing to the development of chronic diseases and to evaluate the long-term effects of various interventions.21–23
Diabetes Agent-Based Model for Metro Health
We built the diabetes agent-based model for this study, taking into account previous work on population health management and cardiovascular disease prevention that had led to the development of The New York Academy of Medicine Cardiovascular Health Simulation model. The New York Academy of Medicine Cardiovascular Health Simulation model has been proposed as a tool to support evidence-based decision making by local health departments when they are designing obesity and cardiovascular disease prevention policies.18,24
Hemoglobin A1c
During development of the model, we engaged staff members and the leadership team at Metro Health, and we incorporated their input and feedback into the model design and structure. As a result, we chose to use the model to create diabetes progression estimates based on a health indicator, hemoglobin A1c (HbA1c), rather than on any intervention or group of interventions. We chose HbA1c in part because Metro Health was interested in having an indicator that could be used across a wide array of programs. Metro Health was working with many partners in the community, including the YMCA, local clinics, and large health systems. In addition, these partners were using various programs targeting diabetes prevention and management, with interventions directed at multiple issues, including lifestyle changes and medication management. However, the one aspect that was common to all interventions and programs was that they were designed to improve blood glucose control, and HbA1c is a reliable indicator of blood glucose control. Another reason we chose HbA1c was that a diabetes mellitus/HbA1c registry (based on HbA1c laboratory test results) was available and it provided a large volume of information about diabetes onset and progression in San Antonio.25
Given the heterogeneity of the interventions and programs being used by Metro Health and its partners, it was a challenge to determine for the model a feasible and relevant hypothetical scenario for an HbA1c decrease. After multiple discussions with Metro Health and other San Antonio community organizations, we determined that a 1-percentage-point decrease in HbA1c would be appropriate. Examples of interventions that could lead to a 1-percentage-point drop in HbA1c are diet-based interventions and primary care-based disease management programs.26,27 For our project, we determined that it would be sufficient to use this single HbA1c-change scenario, because if interventions or programs led to reductions in HbA1c that were either larger or smaller than 1 percentage point, then the use of this scenario would still allow end users (ie, Metro Health or other community-based organizations using our estimates) to adjust proportionally their expectations for health and cost outcomes.
Health Outcomes
We used a series of diabetes complications to represent the primary health outcome, diabetes progression, in the model. We used the model to estimate the 20-year prevalence in San Antonio (Bexar County) of the following health outcomes: blindness, end-stage renal disease, lower-extremity amputation, myocardial infarction, and stroke. The model also incorporated evidence-based equations for other biomarkers and health risk factors (eg, body mass index, smoking, hypertension) that are known to potentially influence the prevalence of diabetes complications. The model logic and embedded equations were the product of research conducted by The New York Academy of Medicine, incorporating critical analyses of and improving on existing diabetes simulation models and risk calculators, such as the Centers for Disease Control and Prevention–Research Triangle Institute Diabetes Cost-effectiveness Model,28 the Michigan Model for Diabetes,29 and the United Kingdom Prospective Diabetes Study Risk Engine.30 The New York Academy of Medicine Center for Health Innovation programmed the model using AnyLogic 7, a multimethod simulation software package.31
To obtain baseline information on the prevalence of diabetes complications for the model, we used 2011 and 2014 health and behavioral data for adults aged ≥18 living in households in San Antonio from the Behavioral Risk Factor Surveillance System. The Behavioral Risk Factor Surveillance System collects data on health-related risk behaviors, chronic health conditions, and use of preventive services from a sample of the noninstitutionalized adult population in the United States.32,33
Scenarios
Using the diabetes agent-based model, we combined data from the Behavioral Risk Factor Surveillance System with 2011 data from the local HbA1c registry program to project the 20-year prevalence of the 5 diabetes complications that indicated disease progression (blindness, end-stage renal disease, lower-extremity amputation, myocardial infarction, and stroke) under the current HbA1c distribution for the population of adults with prediabetes or diabetes in San Antonio.25–27 Then, we directly compared the 20-year diabetes complication prevalence projections from 2 scenarios: the “current HbA1c” scenario, in which the simulated population had the same HbA1c distribution as the distribution estimated from the Diabetes HbA1c Registry in San Antonio, and the “reduce HbA1c by 1 percentage point” scenario, in which each person in the simulated population had a 1-percentage-point reduction in HbA1c at the beginning of the simulation. Using the model, we also estimated the number of each type of diabetes complication that would be averted in the “reduce HbA1c by 1 percentage point” scenario. We determined estimates of averted diabetes complications by subtracting the projected number of complications under the “reduce HbA1c by 1 percentage point” scenario from the projected number of complications under the “current HbA1c” scenario. Finally, we estimated the annual direct medical cost savings associated with each averted diabetes complication, using estimates in 2010 US dollars for diabetes simulation modeling from a health care system perspective, and adjusting those to 2015 US dollars based on the Consumer Price Index for medical care.34
Results
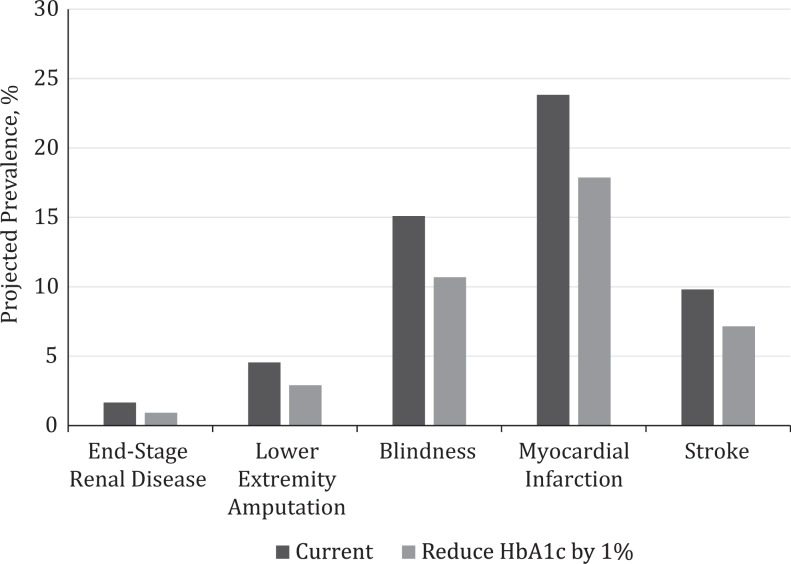
When compared with the population in the “current HbA1c” scenario, the population in the “reduce HbA1c by 1 percentage point” scenario was projected to have a decrease in the 20-year prevalence of blindness from 15.1% to 10.7%, end-stage renal disease from 1.7% to 0.9%, lower-extremity amputation from 4.6% to 2.9%, myocardial infarction from 23.8% to 17.9%, and stroke from 9.8% to 7.2% (Figure 2).
Figure 2.
Prevalence projections for diabetic complications occurring before and after reducing hemoglobin A1c (HbA1c) by 1% among adults with prediabetes and diabetes in San Antonio, Texas, during a 20-year period (2015-2034). In the “current” scenario (before reducing HbA1c by 1 percentage point), the simulated population had the same HbA1c distribution that was estimated from the Diabetes HbA1c Registry in San Antonio, 2011. In the “reduce HbA1c by 1 percentage point” scenario (after reducing the HbA1c by 1 percentage point), each person in the simulated population had a 1-percentage-point reduction in HbA1c at the beginning of the simulation.
During a 20-year period, compared with the population in the “current HbA1c” scenario, the population in the “reduce HbA1c by 1 percentage point” scenario was projected to have 11 548 averted cases of blindness, 1942 averted cases of end-stage renal disease, 4304 averted cases of lower-extremity amputation, 15 616 averted cases of myocardial infarction, and 6981 averted cases of stroke. Furthermore, the annual direct medical cost savings (in 2015 US dollars) of reducing HbA1c by 1 percentage point were estimated to be $7784 for each averted case of blindness, $39 800 for each averted case of end-stage renal disease, $19 850 for each averted case of lower-extremity amputation, $6842 for each averted case of myocardial infarction, and $6930 for each averted case of stroke (Table).
Table.
Estimated frequency of averted diabetes complications, annual direct medical costsa per person with and without diabetes complications, and annual direct medical cost savingsa associated with each averted diabetes complication, after reducing hemoglobin A1c by 1% among adults with prediabetes or diabetes, San Antonio, Texas, 2015-2034
| Variable | End-Stage Renal Disease | Lower-Extremity Amputation | Blindness | Myocardial Infarction | Stroke |
|---|---|---|---|---|---|
| No. of averted diabetes complications | 1942 | 4304 | 11 548 | 15 616 | 6981 |
| Annual cost per persona without the diabetes complicationb | $7490 | $6371 | $6961 | $5554 | $7694 |
| Annual cost per persona with the diabetes complicationb | $47 290 | $26 221 | $14 745 | $12 396 | $14 624 |
| Annual cost savingsa associated with each averted diabetes complication | $39 800 | $19 850 | $7784 | $6842 | $6930 |
Discussion
We used an innovative systems-science approach to project the long-term effect of diabetes control strategies on health and cost outcomes. We demonstrated that a hypothetical 1-percentage-point reduction in HbA1c in a population could result in substantial reductions in the prevalence of 5 common diabetes complications during a 20-year period in San Antonio. Moreover, using estimates of annual direct medical cost savings associated with averted diabetes complications, we also provided valuable information to Metro Health about the magnitude of cost savings that could potentially be achieved through various diabetes prevention and management strategies.
The diabetes agent-based model that we used to project potential changes in the prevalence of diabetes complications was an example of a systems-science tool that local health departments could use to enhance the process of evidence-based decision making when designing chronic disease management strategies. One important feature of this diabetes agent-based model was that it provided a graphic user interface that policy makers could use to (1) define populations of interest, (2) define system parameters, (3) visualize dynamic changes in health factors and outcomes, (4) predict health and cost outcomes for user-defined interventions, (5) perform cost-effectiveness analyses, and (6) report simulation results graphically. An interface such as this can provide policy makers with the capability to easily evaluate and compare chronic disease prevention or treatment strategies, and it can inform their responses to complex policy questions.
Incorporating evidence-based decision making into an innovative systems-science approach that relies on local population data is likely to be both practical and useful for local health departments and other public health stakeholders. In this project, we were able to use this methodology to provide Metro Health with the data needed to assess the potential benefits that could be associated with various diabetes prevention and management interventions and programs. Our methods of communication and our approach to reporting the results and making the case for diabetes prevention and management were well received by Metro Health, which subsequently expressed interest in having us share what we learned through this process with other local public health practitioners and researchers. Given the success of this working relationship and partnership, we believe that this project provides a template for how a research team might work together with a funder, a local health department, and/or other community partners to use simulation modeling to inform public health intervention decisions and strategies.
We had some challenges and learned some important lessons that might be informative for those designing similar partnerships in other areas of the United States. First, to evaluate various diabetes prevention strategies, we needed local data from multiple sources. We were provided with data related to the delivery and use of services that were part of local Delivery System Reform Incentive Payment interventions, but some other relevant data (eg, health insurance claims data or health indicator data not directly related to the Delivery System Reform Incentive Payment initiative) were not readily available. However, we overcame this challenge by incorporating data from other sources and by using simulation. Second, unexpected changes in leadership at San Antonio Metro Health during our project required working with the new interim leadership to rapidly reassess, realign, and coordinate priorities. We overcame this challenge by requesting in-person interactions whenever possible and by conducting frequent site visits. We believe that these strategies played important roles in helping us build rapport with the key stakeholders involved in the project and in enabling us to build trust within the partnership.
Another salient lesson learned from this project concerned the vital role that other partners and allies (including nonprofit and philanthropic foundations) can play in leveraging local network resources. The organization funding our project helped us access materials (eg, software to calculate costs averted by preventing diabetes complications) and contextual information (eg, basic structures of Delivery System Reform Incentive Payment diabetes prevention programs, descriptions of other Delivery System Reform Incentive Payment projects at San Antonio Metro Health) that we needed to provide technical assistance. Our funder also helped us identify organizations that provided other forms of technical assistance in the San Antonio community (eg, quality improvement tools). This type of support helped us to better align our efforts toward achieving project goals.
Finally, we believe our project, although confined to diabetes, also influenced how Metro Health, on a broader level, thought about chronic disease prevention activities and their effects on population health and health care expenditures. For example, we observed that having the results from our agent-based model simulations on the effect of changes in HbA1c on diabetes complications inspired Metro Health to think about how this type of information could be best shared with the wider local health care community (eg, health systems, clinicians, and other community-based organizations). Indeed, since completing our project, Metro Health has presented and continues to share our findings with various community partners and organizations. This information sharing has fostered a growing coalition in San Antonio that will be able to act together on this evidence, using it along with the collective effect model of collaboration to sustain efforts to improve diabetes prevention and management locally.
Conclusions
As the US health care delivery system moves from fee-for-service to value-based payments, the use of Medicaid funds to support chronic disease prevention strategies through 1115 Medicaid waivers is likely to grow. Using these funds, local health departments have the potential to affect health care use and costs by leading or coordinating various public health disease prevention and management programs. However, many local health departments lack the infrastructure or personnel required to conduct the necessary health and cost analyses or to estimate the return on investment of interventions or programs. These local health departments could benefit from technical assistance, involving the use of innovative methods such as systems science, to show how their programs might improve the health of populations and to be able to demonstrate the possible financial effect of adopting these public health programs.
The use of systems-science modeling is an innovative approach to better inform the planning and delivery of public health and health care services. Changes in payment systems provide a new opportunity to evaluate how health care systems are designed and how they operate. Simulation modeling is a novel way to prioritize programs and, ultimately, engage communities and stakeholders using results and projections about potential outcomes and costs.
Footnotes
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was funded through a grant from the Robert Wood Johnson Foundation (Project Number 72 516).
References
- 1. Robert Wood Johnson Foundation Culture of Health Blog. What’s the role of local health departments in implementing the Affordable Care Act? http://www.rwjf.org/en/culture-of-health/2013/07/what_s_the_role_ofl.html. Published 2013. Accessed May 31, 2016.
- 2. Hall E, Melton R, Broderick A, Wang A. Health Reform and Local Health Departments: Opportunities for the Centers for Disease Control and Prevention. Oakland, CA: Public Health Institute; 2010. http://www.phi.org/resources/?resource=health-reform-and-local-health-departments-opportunities-for-the-centers-for-disease-control-and-prevention. Accessed May 31, 2016. [Google Scholar]
- 3. New York State Department of Health. Template: New York State 2016 community health assessment and improvement plan and community service plan. https://www.health.ny.gov/prevention/prevention_agenda/2013-2017/docs/letter_community_planning_guidance_2016_18.pdf. Published 2015. Accessed May 31, 2016.
- 4. Gates A, Rudowitz R, Guyer J. An Overview of Delivery System Reform Incentive Payment (DSRIP) Waivers. Menlo Park, CA: Henry J. Kaiser Family Foundation; 2014. http://kff.org/medicaid/issue-brief/an-overview-of-delivery-system-reform-incentive-payment-waivers. Accessed May 31, 2016. [Google Scholar]
- 5. Lewis VA, McClurg AB, Smith J, Fisher ES, Bynum JPW. Attributing patients to accountable care organizations: performance year approach aligns stakeholders’ interests. Health Aff (Millwood). 2013;32(3):587–595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Brownson RC, Gurney JG, Land GH. Evidence-based decision making in public health. J Public Health Manag Pract. 1999;5(5):86–97. [DOI] [PubMed] [Google Scholar]
- 7. Brownson RC, Fielding JE, Maylahn CM. Evidence-based public health: a fundamental concept for public health practice. Annu Rev Public Health. 2009;30:175–201. [DOI] [PubMed] [Google Scholar]
- 8. McGinnis JM. Does proof matter? Why strong evidence sometimes yields weak action. Am J Health Promot. 2001;15(5):391–396. [DOI] [PubMed] [Google Scholar]
- 9. Sosnowy CD, Weiss LJ, Maylahn CM, Pirani SJ, Katagiri NJ. Factors affecting evidence-based decision making in local health departments. Am J Prev Med. 2013;45(6):763–768. [DOI] [PubMed] [Google Scholar]
- 10. Tabak RG, Duggan K, Smith C, Aisaka K, Moreland-Russell S, Brownson RC. Assessing capacity for sustainability of effective programs and policies in local health departments. J Public Health Manag Pract. 2016;22(2):129–137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Dumchev K. Imported “evidence-based” or locally grown interventions: a false dichotomy and some hard choices in implementation science. Subst Use Misuse. 2015;50(8-9):1092–1096. [DOI] [PubMed] [Google Scholar]
- 12. Luke DA, Stamatakis KA. Systems science methods in public health: dynamics, networks, and agents. Annu Rev Public Health. 2012;33:357–376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Mabry PL, Milstein B, Abraido-Lanza AF, Livingood WC, Allegrante JP. Opening a window on systems science research in health promotion and public health. Health Educ Behav. 2013;40(suppl 1):5S–8S. [DOI] [PubMed] [Google Scholar]
- 14. Maglio PP, Mabry PL. Agent-based models and systems science approaches to public health. Am J Prev Med. 2011;40(3):392–394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Wang Y, Xue H, Liu S. Applications of systems science in biomedical research regarding obesity and noncommunicable chronic diseases: opportunities, promise, and challenges. Adv Nutr. 2015;6(1):88–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Frerichs L, Lich KH, Dave G, Corbie-Smith G. Integrating systems science and community-based participatory research to achieve health equity. Am J Public Health. 2016;106(2):215–222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Burke JG, Lich KH, Neal JW, Meissner HI, Yonas M, Mabry PL. Enhancing dissemination and implementation research using systems science methods. Int J Behav Med. 2015;22(3):283–291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Li Y, Kong N, Lawley M, Weiss L, Pagán JA. Advancing the use of evidence-based decision-making in local health departments with systems science methodologies. Am J Public Health. 2015;105(suppl 2):S217–S222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Jahnke L, Siddiqui N, Andrulis D, Reddy S. Snapshot of Medicaid 1115 waiver and other state-based delivery system transformations. https://sph.uth.edu/research/centers/dell/resources/Blue%20Shield%20DSRIP%20Issue%20Brief.pdf. Published 2015. Accessed May 31, 2016.
- 20. Schlenker T, Huber CA. A unique funding opportunity for public health in Texas. J Public Health Manag Pract. 2015;21(suppl 1):S81–S86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Nianogo RA, Arah OA. Agent-based modeling of noncommunicable diseases: a systematic review. Am J Public Health. 2015;105(3):e20–e31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Li Y, Lawley MA, Siscovick DS, Zhang D, Pagán JA. Agent-based modeling of chronic diseases: a narrative review and future research directions. Prev Chronic Dis. 2016;13:E69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Li Y, Zhang D, Pagán JA. Social norms and the consumption of fruits and vegetables across New York City neighborhoods. J Urban Health. 2016;93(2):244–255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Li Y, Kong N, Lawley MA, Pagán JA. Using systems science for population health management in primary care. J Prim Care Community Health. 2014;5(4):242–246. [DOI] [PubMed] [Google Scholar]
- 25. Texas Department of State Health Services and San Antonio Metropolitan Health District. Diabetes Mellitus/Hemoglobin A1c Registry Program. Austin, TX: Texas Department of State Health Services; 2013. [Google Scholar]
- 26. Rothman RL, Malone R, Bryant B, et al. A randomized trial of a primary care-based disease management program to improve cardiovascular risk factors and glycated hemoglobin levels in patients with diabetes. Am J Med. 2005;118(3):276–284. [DOI] [PubMed] [Google Scholar]
- 27. Crawford P. Effectiveness of cinnamon for lowering hemoglobin A1c in patients with type 2 diabetes: a randomized, controlled trial. J Am Board Fam Med. 2009;22(5):507–512. [DOI] [PubMed] [Google Scholar]
- 28. Hoerger TJ, Bethke AD, Richter A, et al. ; CDC Diabetes Cost-Effectiveness Group. Cost-effectiveness of intensive glycemic control, intensified hypertension control, and serum cholesterol level reduction for type 2 diabetes. JAMA. 2002;287(19):2542–2551. [DOI] [PubMed] [Google Scholar]
- 29. Zhou H, Isaman DJ, Messinger S, et al. A computer simulation model of diabetes progression, quality of life, and cost. Diabetes Care. 2005;28(12):2856–2863. [DOI] [PubMed] [Google Scholar]
- 30. Stevens RJ, Coleman RL, Adler AI, Stratton IM, Matthews DR, Holman RR. Risk factors for myocardial infarction case fatality and stroke case fatality in type 2 diabetes: UKPDS 66. Diabetes Care. 2004;27(1):201–207. [DOI] [PubMed] [Google Scholar]
- 31. AnyLogic Co. AnyLogic Version 7.3. Chicago: AnyLogic Co; 2016. [Google Scholar]
- 32. Texas Department of State Health Services. 2011 Behavioral Risk Factor Surveillance System Texas. Public Use Data File Codebook. Austin, TX: TDSHS Center for Health Statistics; 2015. [Google Scholar]
- 33. Texas Department of State Health Services. 2014 Behavioral Risk Factor Surveillance System Texas. Public Use Data File Codebook. Austin, TX: TDSHS Center for Health Statistics; 2015. [Google Scholar]
- 34. Li R, Bilik D, Brown MB, et al. Medical costs associated with type 2 diabetes complications and comorbidities. Am J Manag Care. 2013;19(5):421–430. [PMC free article] [PubMed] [Google Scholar]