Abstract
Introduction:
The rising cost of healthcare requires rethinking in terms of resource utilisation care delivery. Nurse-led PSA phone follow-up clinics may provide a suitable option.
Materials and methods:
815 patients were recruited for the nurse-led stable prostate cancer telephone follow-up service. A convenience sample was selected for postal questionnaire assessment of their satisfaction.
Results:
815 patients had 3683 phone-call follow ups over 10 years. Patients’ own understanding of condition varied from average (76.3%) and good (9.2%) in the majority. 87.2% found the service convenient and 75.6% informative. 95.3% found the telephone assessment preferable to attending the outpatient department. 87.2% were keen on savings on transport/travel. 53.5% found it more reassuring. 91.9% of patients felt that everything they wanted to talk about was covered.
Discussion:
This service can be delivered in a high volume nurse-led service, with high levels of patient satisfaction, as an innovative service development.
Keywords: PSA, nurse led, phone, prostate cancer
Introduction
Patients find attending hospital problematic in terms of time, loss of control, and anxiety. Currently, patients are required to travel to hospital, find and pay for parking, sit in overcrowded waiting rooms for outpatient clinics that often run late, to see a physician for less than 15 minutes, and to receive results of blood tests and investigations. Hospital-based care is now recognized to be inferior for chronic conditions and community-based survivorship models, especially in cancer. New models that put patients at the center of their care are imperative in all developed health systems.
A total of 41 736 men were diagnosed with prostate cancer in the United Kingdom according to the latest figures in 2011, with 10 837 men dying of the disease in 2012. It is recognized that the number of cancer survivors is increasing by approximately 3% per year, with an 86% 5-year survival for prostate cancer. The incidence of prostate cancer is likely to rise, due to an aging population, continuing earlier diagnosis, the changing ethnic composition of society, and the influence of a westernized lifestyle (1,2). This places a significant burden of health-care costs on the health system (3).
The use of traditional outpatient follow-up assessment has been questioned in relation to prostate cancer (4) and other cancers (5,6). The issue of delivering care in the appropriate setting is of paramount importance. New models of care can bring considerable advantages to patients. The UK Cancer Reform Strategy sets out a range of ways in which service models for cancer could be improved, based on 2 key principles—first that care should be delivered locally wherever possible to maximize patient convenience and second that services should be centralized where necessary to improve outcomes (7).
Similarly, demands on clinician and nursing time and the European working time directive all have implications in relation and cost of follow-up of patients with prostate cancer. There are potentially large cohorts of men with “stable” prostate-specific antigen (PSA) levels that are suitable for a telephone follow-up assessment. This consists of those patients under active surveillance, post-prostatectomy, post-radiotherapy, and those on Luteinising hormone releasing hormone (LHRH) analogues.
The aim of our study was to assess patients with stable prostate cancer using regular telephone-based clinical assessment and PSA as a surrogate for clinic attendance. Secondly, we sought to assess whether patients were satisfied with phone call follow-up assessment. Triggers to prompt further clinical review included rising PSA, worsening bone pain, Eastern Cooperative Oncology Group (ECOG) or International prostate symptom score (IPSS) status, and patient choice.
Materials and Methods
Since May 2004 to May 2014, a total of 815 patients have been referred to the urology cancer clinical nurse specialist for the stable prostate cancer telephone follow-up service. These patients were referred exclusively by urology and oncology medical staff.
Inclusion criteria were patients post-radical radiotherapy >12 months with a stable or falling PSA, post-radical prostatectomy >6 months with a PSA <0.2 ng/mL, patients on hormone manipulation whose PSA and symptoms are stable for >6 months, and patients who had surgery and radiotherapy. All patients had an expected survival of over 6 months. Exclusion criteria were patients suitable for active surveillance or watchful waiting (who all require digital rectal examination), PSA lability, patient preference for clinic attendance, and inability to assess over the telephone (dementia, hearing loss, etc).
All patients were assessed every 6 months by phone at a preagreed time and date. This consisted of a recent PSA test and assessment of IPSS score, ECOG status, and side effects from treatment or any new symptoms consistent with local or metastatic disease progression. Triggers to discuss patients with their consultant included any change in symptoms or rise in PSA nadir.
For patients who failed to be present for their phone call, or who developed any problem that precluded telephone assessment, a letter was written to them to ascertain whether they wanted telephone or clinic follow-up.
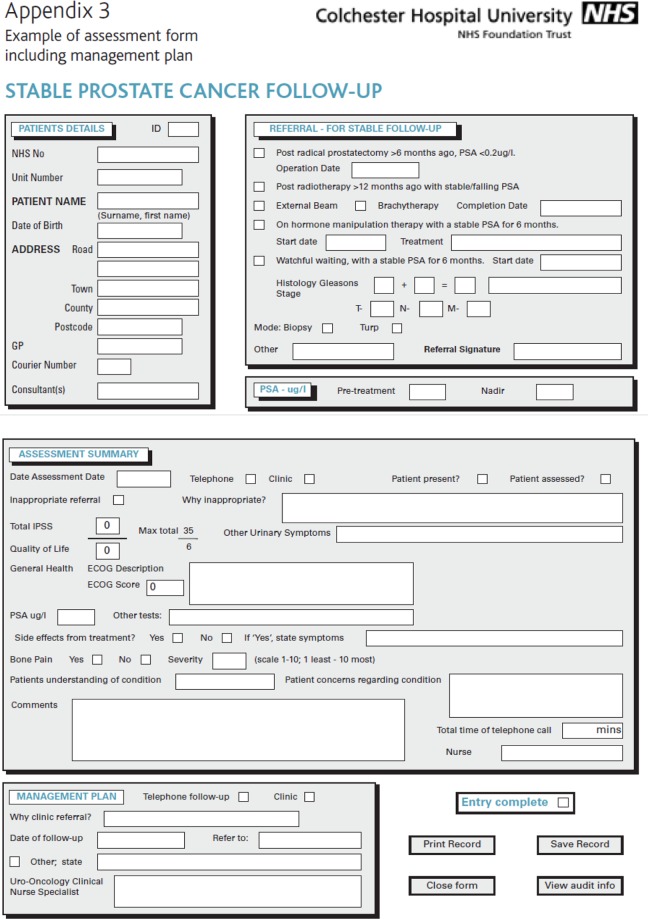
Data collection was performed using a dedicated bespoke software package designed in-house, and the key demographic pages are displayed in Figure 1. This computerized pro forma allows collection of a number of key pieces of data including key demographic information, PSA data, ECOG and IPSS scores, symptoms, bone pain, and time spent on consultation. Patient data were stored securely on a password-protected computer in the urology department.
Figure 1.
Screenshot of computerized database.
A convenience sample of the most recent 100 patients was selected from the telephone follow-up service database for postal questionnaire assessment. The list was then checked by the NHS patient tracking service to ensure surveys were not being sent to patients who may have since deceased in the community. After tracking, 98 patients were cleared to be sent surveys, from which a total of 86 were returned. This questionnaire consisted of a 6-part survey based on patient satisfaction (Table 1).
Table 1.
Patient Satisfaction Survey.a
| % | ||
|---|---|---|
| Q1. Did you find the telephone call from the urology cancer nurse specialist offering you the telephone assessment service? | Intrusive | 2.3 |
| Informative | 75.6 | |
| Convenient | 87.2 | |
| Timely | 47.7 | |
| Q2. Did you prefer the telephone assessment to attending a clinic in the outpatients department? | Yes | 96.4 |
| No | 1.2 | |
| Neither | 1.2 | |
| Don’t know | 1.2 | |
| Q2a. If yes, could you please elaborate on your answer? | Saved on travel | 91 |
| Saved taking time off work | 4.5 | |
| Saved taking time off family | 4.5 | |
| Q3. If you did not find the telephone assessment easier than attending clinic in outpatients, please give your reasons: | 0 | |
| Q4. From your previous experience of outpatient department clinics, with a consultation from a doctor, did you find your telephone consultation with the nurse: | More thorough | 36 |
| Less thorough | 7 | |
| More reassuring | 53.5 | |
| Less reassuring | 3.5 | |
| Q5. During the telephone consultation, did you cover everything you wanted to talk about? | Yes | 92 |
| No | 8 | |
| Q6. Was there an issue you thought about after the telephone follow-up? | Yes | 6 |
| No | 94 | |
| Q6a. Would you have felt comfortable in phoning the nurse specialist back to discuss any issues that you missed during the initial telephone assessment? | Yes | 78 |
| No | 5 | |
| Unanswered | 10 | |
| Don’t know | 7 |
aN = 86.
Results
In total, there were 815 patients in the database amounting to total phone assessments of 3683 (96.4% successfully assessed) over 10 years. This gives an average of 4.5 assessments per person. Each patient was assessed every 6 months over a 10-year period since the telephone clinic service commenced. The median time on phone call follow-up was 64 months. Inappropriate referrals consisted of 3 patients (patient with deterioration of Alzheimer disease, PSA instability, and vascular dementia). Fifty-one (3.2%) of 1570 assessments were referred back to consultant-run clinics because of the reasons in Table 2: inappropriate referral for active surveillance (3.9%), consultant request (3.9%), Digital rectal examination (DRE) abnormality that needed consultant review (3.9%), worsening lower urinary tract symptoms (LUTS) (19.6%), and PSA rise (60.8%). Further issues included other raised blood tests (4%) and patient concern regarding phimosis (2%).
Table 2.
Clinical parameters of patient cohort.a
| % | |
|---|---|
| Indication | |
| Post-radiotherapy | 50.8 |
| Post-prostatectomy | 22.5 |
| Surgery and radiotherapy | 3 |
| Brachytherapy | 0.7 |
| Hormonal therapy only | 23 |
| Active surveillance/watchful waiting | 0 |
| Gleason score | |
| Well differentiated (≤6) | 15 |
| Moderately differentiated (8) | 65 |
| Poorly differentiated (≥8) | 20 |
| Clinical stage | |
| T1a | 3.5 |
| T1b | 1.5 |
| T1c | 13.6 |
| T2a | 15.2 |
| T2b | 9 |
| T2c | 8.8 |
| T3a | 36.7 |
| T3b | 1.8 |
| T4 | 2.4 |
| Tx | 4.8 |
| Nodal status | |
| N0, N1, N2, Nx | 7.5, 0.9, 0.2, 91.5 |
| Bone metastases | |
| Yes, no, unknown | 7.2, 63.1, 25.3 |
| ECOG status | |
| 1, 2, 3, 4, 5 | 76.7, 19.1, 2.5, 1.2, 0.5 |
| Referred back | |
| PSA rise | 60.8 |
| LUTS | 19.6 |
| DRE concerns | 3.9 |
| Consultant request | 3.9 |
| Active surveillance required | 3.9 |
| Raised creatinine | 3.9 |
| Other raised blood tests | 2 |
| Tight foreskin | 2 |
Abbreviation: DRE, Digital rectal examination; ECOG, Eastern Cooperative Oncology Group; LUTS, lower urinary tract symptoms; PSA, prostate specific antigen.
aN = 815.
The mean age of patients was 75 years (range: 38-94 years). The diagnostic mode was biopsy in 78%, transurethral prostate resection in 12.9%, and clinical in 9.1%. Pretreatment average PSA was 32 ng/mL (range: 0.5-95 ng/mL). A total of 4.4% of patients pretreatment PSA were not known/recorded in medical notes. The nadir average was 0.9 (range: ≤ 0.1-13.5). Demographic and staging parameters are given in Table 2, with the majority being moderately differentiated, organ-confined patients either following radiotherapy or “hormonal-only” treatment.
The vast majority of patients had good ECOG performance scores (Table 2), low IPSS scores (mean = 3), and good quality-of-life IPSS subscores (mean = 1). Ninety-one (20%) patients experienced bone pain. The severity of the bone pain was generally low. Severity of bone pain was measured on a scale of 1 to 10, where 1 least and 10 most, with the majority of these 20 patients experiencing bone pain severity scale ≤3 (Table 2).
A total of 151 patients said that they had experienced side effects from the various prostate cancer treatments or LUTS related to their disease (Table 3). Patients’ own understanding of condition varied from average (76.3%), good (9.2%), poor (6.2%), and not stated (8.4%). Eleven percent of patients expressed concerns about their condition. The variation between individual concerns by patients is too much to quantify in the majority of cases; however, 26% of these patients expressed the same concern regarding rising PSA. For the remainder, there were concerns regarding standard urinary symptoms, incontinence, LUTS, medication effects, details about appointments, and possible referrals for nonurinary symptoms.
Table 3.
Patient Urinary and Treatment Symptoms.a
| Urinary Symptoms Experienced by Patients | n | Side Effects From Treatment | % |
|---|---|---|---|
| Catheter symptoms | 5 | Gynecomastia | 9.3 |
| Poor flow | 6 | Hot flushes | 43 |
| Hesitancy | 3 | Erectile dysfunction | 17.9 |
| Frequency | 2 | Loose stools | 12.6 |
| Hematuria | 4 | Radiation proctitis | 5.3 |
| Incomplete emptying | 3 | Other | 11.9 |
| Incontinence | 2 | ||
| Nocturia | 23 | ||
| Urgency | 8 | ||
| Pad or penile sheath requirement | 7 |
aN = 815.
Table 1 lists the questions put to patients in the patient satisfaction survey. In response to question 1, 87.2% found the service convenient and 75.6% informative. A total of 95.3% of patients responding to question 2 found the telephone assessment preferable to attending the outpatient department to see a doctor. On elaboration of the benefits of a phone call follow-up, 87.2% were keen on savings on transport/travel. This tended to be older men on androgen suppression with advanced cancer.
No patients found the clinic easier to attend than a phone call follow-up according to the questionnaire. In response to question 4, 36% of patients found the phone call follow-up more thorough than an outpatient consultation with a doctor. Seven percent found it less thorough. A total of 53.5% found it more reassuring and 3.5% less reassuring. In response to the question, a follow-up question (4a) regarding “more thorough” confirmed patients generally stated that they had more time, more personal, opportunity to ask questions and discuss other areas of prostate health. Those men who found it “less thorough” found it generally missed the opportunity to ask the doctor questions. Seven percent found it “less thorough” stating that it was not a doctor seeing the patient. In those men who found it “more reassuring” (53.5%), they stated that there was more understanding, time for discussion and questions, less noise, blood tests immediately available, and a better relationship with the nurse. They also felt it was more convenient to be able to have the results at home. The 3.5% that found it “less reassuring” stated that they would have preferred to talk to a doctor. During the telephone consultation, 91.9% of patients felt that everything they wanted to talk about was covered (question 5). However, 3 patients answered negatively stating that they had concerns regarding the validity of PSA and wanted consultant review. Only 5 patients felt there was an issue that they thought about after the telephone call (question 6). Overall, 77.9% felt comfortable phoning the nurse specialist back to discuss any issue that was missed during the initial telephone assessment (question 6a).
Discussion
Nurse-led PSA telephone follow-up services were recommended with the publication of the NICE (2008) guidelines on “Improving Urology Cancers,” when it was suggested that after at least 2 years, men with a stable PSA who have had no significant treatment complications should be offered follow-up outside hospital (eg, in primary care or through a clinical nurse specialist) by telephone (8). However, this has not led to widespread adoption in the NHS to date.
This is the first prospective study with a large clinical cohort, of 3683 assessments on 815 patients, where nurse-led PSA phone call clinics are effective and lead to high patient satisfaction.
In a urology-based study by Vieira et al (9), both patients and professionals wanted follow-up in the hospital with face-to-face consultation. While this perceived benefit of routine follow-up with doctors every 6 months, in this study, was overwhelming, it was recognized that 95% of patients felt that it was important to have easy access to the urology cancer nurses and doctors. Our study found only 2 patients who felt the service was “impersonal” and that they missed having an examination by a doctor. Perhaps, a small percentage of patients might find having the examination more reassuring in some way. However, Vieira et al did recognize that in order to change, a new service would be needed that met patient requirements, with easy access to expert advice and support and back to urology services was needed. We have found that once patients make this change to the new nurse-led phone call service, the perceived loss of direct contact with a health professional disappears and was not a barrier to change. As stated, each patient was assessed every 6 months over a 10-year period since the telephone clinic service commenced. The median time on phone call follow-up was 64 months.
There is evidence from other, nonurology, specialties that nurse-led follow-up services improve service delivery, are more efficient and convenient, and increase patient satisfaction, as they often receive treatment tailored to their individual needs (2,10,11). Such services are successful and popular because there is no travelling to hospital, no car parking fees, and no delays in an overcrowded waiting room. Telephone follow-up can also benefit health-care providers, as the intervention allows clinicians to spend more time with those patients who require clinical review. This has been shown to increase the capacity of already overburdened clinics, help to reduce the waiting times for new and other follow-up patients (12), and as a result, decrease the workload in outpatient clinics (13,14).
In agreement with this evidence and our study is a study by Cox and Wilson (10) who found that patients are receptive to nurse-led services and welcome this addition to their health care. The majority of patients with “stable prostate cancer” preferred the approach of a telephone follow-up, making it more convenient, more informative, and perceived it as more thorough than if they had attended a standard consultant clinic. Results from another UK questionnaire survey in patients with prostate cancer indicate that patients who saw a specialist nurse were more likely to have received written information and clear explanations about their tests and treatment options and about sources of help and support. Also in this study, patients who saw a specialist nurse were more likely to say that they had made the treatment decision themselves (15). Patients described the availability of the specialist nurse in terms of the amount of time the specialist nurse was able to spend with them in contrast with other medical staff such as consultants and the possibility of patient-initiated contact with the specialist nurse. This concurs with the study of Boxhall and Dougherty (16) in which patients valued the extra time available to them with specialist nurses compared to doctors. The second unique aspect of the specialist nurse role was that specialist nurses were seen as being in a position to liaise between the medical system and the patient. This included providing or restating information about diagnosis and treatment in terms which were clearly understandable to the patient and acting as an advocate for the patient to facilitate the care process. These 2 key aspects of care have been advocated as important to the specialist nurse role, and this study indicates that these aspects of the role are recognized and valued by patients.
Finally, a randomized trial of outpatient doctor-led versus nurse-led telephone on-demand follow-up of patients with prostate cancer has shown it to be effective (17). Medical safety during the first 3 years of the observation period was similar between groups as was the total number of interventions due to symptoms from prostate cancer. The analysis of accessibility and the anxiety scale showed no significant differences between the groups. The mean outpatient cost (excluding pharmaceutical costs) per patient was lower in the nurse-led group, especially among patients without metastases at inclusion (37% lower). The study results show that this alternative follow-up is cost-effective, especially in men without metastases. In our study, we have not examined this issue of safety of phone interventions in comparison with a nonphone call groups as the majority of our patients are eligible for phone call assessment. We have found that the rate of nontreatment-related problems is low (63 of 815 = 7.7%), even in our patient group that includes those with metastatic prostate cancer. We therefore cannot determine whether this is due to patients having greater access to nursing phone time.
Our study is the biggest of its kind currently published in the world literature with a clinical cohort of 3683 assessments on 815 patients. We have demonstrated many of the previously described actual and theoretical advantages to the patient in this study.
In financial terms, the numbers in this study demonstrates that in an average 1-year period, the PSA phone follow-up system generates income of approximately £27 229 (US$39058.37) based on an agreed secondary care payment basis of £73 (US$104.71) per patient per follow-up. This is based on 815 patients with 3683 assessments with an average or 4.5 assessments per person. There is also saving of approximately £15,105 (US$21667.22) based on telephone follow-up as opposed to attendance at a urology clinic. This cost saving and income generation allow better deployment of clinical staff and a source of funding for nurse-led clinics such as this.
Our study has a number of shortcomings. Firstly, the postal questionnaire was administered by the nurse who carried out the phone follow-up, thus potentially causing response bias. Secondly, there is no objective assessment of patient anxiety or satisfaction using a standardized, validated questionnaire as used in some studies. Finally, this study had no comparator groups; however, there has previously been a study that did randomize patients to outpatient review versus nurse-led follow-up that answers this question (17).
The evidence from this study, and a previous smaller study from the United Kingdom (18), has shown that long-term follow-up after treatment for prostate cancer is an integral part of patient management. Cancer guidelines (7) support lifetime follow-up as patients may experience recurrence or changes in their condition at any time following treatment. Nurse-led clinics do support and improve patient care, but whether this can be done as well or more holistically in a GP setting remains unanswered (2,10,11).
Ongoing demand for reductions in the number of patients attending for conventional follow-up in the outpatient department, better use of resources, and the ever-increasing need for higher standards of care highlights the need for innovative approaches such as a PSA telephone follow-up service.
Author Biographies
RG Casey is a consultant uro-oncology surgeon who specializes in prostate surgery and service redesign.
L Powell is a specialist uro-oncology nurse who runs the PSA phone call service.
M Braithwaite is a specialist uro-oncology nurse who runs the PSA phone call service.
CM Booth is a retired urologist who initially set up the service in conjunction with specialist nurses.
B Sizer is a consultant oncologist who specializes in prostate cancer and contributes patients to the service.
JG Corr is a consultant uro-oncology surgeon who specialises in prostate cancer and provides patients for the service.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. http://publications.cancerresearchuk.org/downloads/Product/CS_KF_PROSTATE.pdf. Published 2014. Updated April, 2014. Accessed March, 2015.
- 2. Faithfull S, Corner J, Meyer L, Huddart R, Dearnaley D. Evaluation of nurse-led follow up for patients undergoing pelvic radiotherapy. Br J Cancer. 2001;85:1853–64. PubMed PMID: 11747326. Pubmed Central PMCID: 2364007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Holmberg H, Carlsson P, Kalman D, Varenhorst E. Impact on health service costs of medical technologies used in management of prostatic cancer. Scand J Urol Nephrol. 1998;32:195–9. PubMed PMID: 9689698. [DOI] [PubMed] [Google Scholar]
- 4. Oh J, Colberg JW, Ornstein DK, Johnson ET, Chan D, Virgo KS, et al. Current followup strategies after radical prostatectomy: a survey of American Urological Association urologists. J Urol. 1999;161:520–3. PubMed PMID: 9915439. [DOI] [PubMed] [Google Scholar]
- 5. Snee M. Follow-up of women treated for breast cancer. Clin Oncol (R Coll Radiol). 1996;8:85–9. PubMed PMID: 8859604. [DOI] [PubMed] [Google Scholar]
- 6. Kjeldsen BJ, Thorsen H, Whalley D, Kronborg O. Influence of follow-up on health-related quality of life after radical surgery for colorectal cancer. Scand J Gastroenterol. 1999;34:509–15. PubMed PMID: 10423068. [DOI] [PubMed] [Google Scholar]
- 7. Richards M. Cancer Reform Strategy: Crown; 2007. http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_081006. Accessed April 3, 2012.
- 8. National Institute for Health and Clinical Excellence. Prostate cancer: diagnosis and treatment. 2008. http://tinyurl.com/39tna9r. Accessed April 3, 2012.
- 9. Vieira I, Burke L, Marks-Maran D. Prostate cancer follow-up needs: do patients and professionals agree? Br J Nurs. 2014;23:S12–9. PubMed PMID: 24820509. [DOI] [PubMed] [Google Scholar]
- 10. Cox K, Wilson E. Follow-up for people with cancer: nurse-led services and telephone interventions. J Adv Nurs. 2003;43:51–61. PubMed PMID: 12801396. [DOI] [PubMed] [Google Scholar]
- 11. Booker J, Eardley A, Cowan R, Logue J, Wylie J, Caress AL. Telephone first post-intervention follow-up for men who have had radical radiotherapy to the prostate: evaluation of a novel service delivery approach. Eur J Oncol Nurs. 2004;8:325–33. PubMed PMID: 15550362. [DOI] [PubMed] [Google Scholar]
- 12. Freeman M. NHS Innovations in Urology Trent: NHS. 2004. http://www.innovationinurology.nhs.uk/pathways/prostate/follow_up/good_hope/case_study.htm. Accessed April 2, 2012.
- 13. Lewis R, Neal RD, Williams NH, France B, Wilkinson C, Hendry M, et al. Nurse-led vs. conventional physician-led follow-up for patients with cancer: systematic review. J Adv Nurs. 2009;65:706–23. PubMed PMID: 19278415. [DOI] [PubMed] [Google Scholar]
- 14. Lewis R, Hendry M. A review comparing the effectiveness of nurse-led follow up for cancer with conventional care. Nurs Times. 2009;105:25–7. PubMed PMID: 19882852. [PubMed] [Google Scholar]
- 15. Tarrant C, Sinfield P, Agarwal S, Baker R. Is seeing a specialist nurse associated with positive experiences of care? The role and value of specialist nurses in prostate cancer care. BMC Health Serv Res. 2008;8:65 PubMed PMID: 18371192. Pubmed Central PMCID: 2294119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Boxhall S, Dougherty M. An evaluation of a specialist nursing role for men with prostate cancer. Urol Nurs. 2003;23:148–52. PubMed PMID: 12778829. [PubMed] [Google Scholar]
- 17. Helgesen F, Andersson SO, Gustafsson O, Varenhorst E, Goben B, Carnock S, et al. Follow-up of prostate cancer patients by on-demand contacts with a specialist nurse: a randomized study. Scand J Urol Nephrol. 2000;34:55–61. PubMed PMID: 10757272. [DOI] [PubMed] [Google Scholar]
- 18. Anderson B. The benefits to nurse-led telephone follow-up for prostate cancer. Br J Nurs. 2010;19:1085–90. PubMed PMID: 20871511. [DOI] [PubMed] [Google Scholar]