Abstract
Lung cancer is one of the most fatal cancers in the world. To early distinguish benign and malignant pulmonary nodule is critical for disease prognosis. Confocal laser endomicroscopy (CLE) can be used to explore bronchus mucous membrane, alveolar elastic fiber structures and microvessels, and could be helpful for the diagnostic imaging and for the localization guidance. In this report, we presented two cases of peripheral pulmonary nodule. Under the guidance of X-ray and endobronchial ultrasound, needle-based confocal laser endomicroscopy (nCLE) could directly approach the peripheral pulmonary nodule via an exploratory puncture needle. The results indicated that the utility of the nCLE is helpful to precise positioning and characterize the peripheral pulmonary nodule. This report presents for the first time the application of nCLE for positioning the peripheral extraluminal nodule and describe the different confocal imaging features between adenocarcinoma and tuberculosis.
Keywords: Needle-based confocal laser endomicroscopy (nCLE), bronchoscopy, peripheral pulmonary nodule, lung cancer, diagnosis
Introduction
The morbidity and mortality of lung cancer are increasing, early and accurate diagnosis for peripheral pulmonary nodules can effectively improve the survival rate and have been receiving more and more attention. The increasing development of pulmonary interventional techniques has potential for improving the diagnostic yield.
Confocal laser endomicroscopy (CLE) is a new endoscopic technique that can obtain in real-time microscopic examination of lung tissue, as well as alveoli and microvessels, with 400 times magnification. Several studies (1,2) reported that CLE is promising for lung cancer exploration and improving diagnostic yield. Compared to the conventional probe-based confocal laser endomicroscopy (pCLE), the novel needle-based confocal laser endomicroscopy (nCLE) is characterized by a smaller miniprobe (AQ-Flex 19, Mauna Kea Technologies, Paris, France) with an external diameter of 0.9 mm, a resolution of 3.5 µm and a penetration depth of 40 to 50 µm. Under the guidance of bronchoscope and guiding sheath, the nCLE-miniprobe can be positioned in the paratracheal tumor to perform real-time exploration and guide the biopsy (3).
At present, studies related to the application of nCLE in the exploration of peripheral pulmonary nodules and the imaging features for differentiation between benign and malignant lesions are limited. We present here two cases to show how nCLE miniprobe positioned to the peripheral extraluminal nodule for exploration, and describe the CLE imaging characteristics of benign and malignant nodule respectively.
Case presentation
Case 1
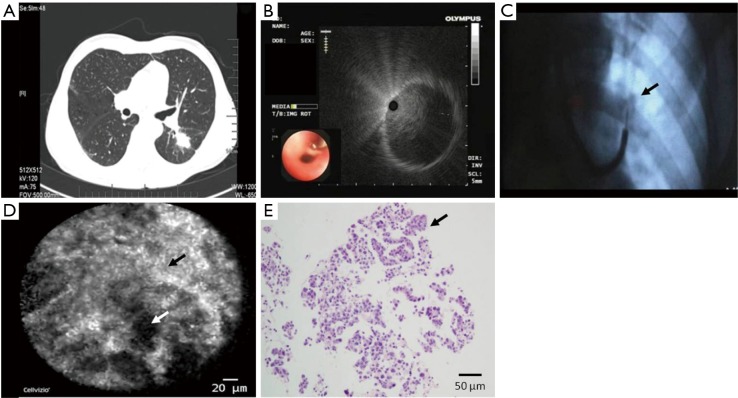
A 66-year-old male patient, heavy smoker, was found to have a pulmonary nodule in the left lower lobe by X-ray examination. The enhanced chest CT revealed an irregular heterogeneous soft-tissue nodule in the dorsal segment of the left lower lung, with a size of 3.0 cm × 2.8 cm × 2.5 cm and multiple short burrs at the edge (Figure 1A). Bronchoscopy (260F, OLYMPUS, Japan, 4.0 mm outer diameter with 2.0 mm working channel) suggested the absence of neoplasm in the airway lumen. Through bronchoscopy with radial probe endobronchial ultrasound exploration, it was confirmed that the lesion was located outside the bronchial lumen (Figure 1B). An 18 G puncture needle (Flexneedle, Broncus Medical, USA) was inserted into the extraluminal lesion in left lower lung under the guidance of C-arm X-ray (Figure 1C). The nCLE-Miniprobe was inserted along the puncture needle to reach the lesion and capture images for software analysis (Cellvizio viewer, version 1.6.0; Mauna Kea Technologies, Paris, France). The confocal endomicroscopic images revealed no alveolar space and septa in the nodule, the fibrous tissue reconstruction was disordered and highlighted with a heterogeneous density, accompanied with a spot or black hole structure (Figure 1D). After removing the nCLE-Miniprobe, aspiration biopsy was performed in the bronchial extraluminal lesion under the guidance of C-arm X-ray. The procedures of positioning and biopsy took about 25 minutes. The quantity and quality of tissue sampling was sufficient for pathological examination. The histopathological analysis showed acinous and papillary cancer cells (Figure 1E), confirming lung adenocarcinoma diagnosis. Mutation-analysis demonstrated EGFR mutation on exon 19.
Figure 1.
Images of peripheral pulmonary nodule obtained from CT, EBUS, X-ray, nCLE and histopathologic examination in case 1. (A) The chest CT showed soft-tissue mass in the dorsal segment of left lower lobe, with no bronchial sign; (B) radial probe endobronchial ultrasound confirmed the lesion location outside the bronchial lumen; (C) the puncture needle was inserted into the lesion (black arrow) under the guidance of C-arm X-ray; (D) the confocal endomicroscopic images showed highlighted fibrous tissues (black arrow) with a disordered arrangement, accompanied with spot or black hole structures (white arrow); (E) the histopathological images showed acinous, papillary cancer cells (black arrow) in the lung tissues (hematoxylin-eosin stain, 200×). nCLE, novel needle-based confocal laser endomicroscopy.
Case 2
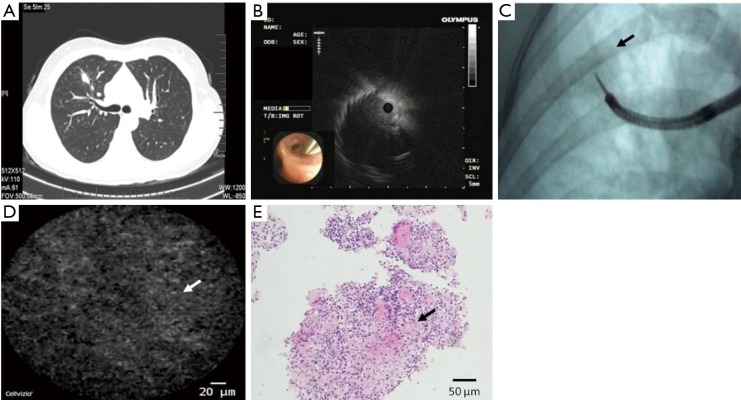
A 29-year-old female patient, non-smoker, presented with cough for 2 months. The enhanced chest CT showed an irregular solid nodule in the anterior segment of the right upper lung, with a size of 1.9 cm × 1.7 cm × 2.1 cm (Figure 2A). Following the exploration and confirmation of radial probe endobronchial ultrasound for the extraluminal lesion (Figure 2B), a puncture needle was inserted into the peripheral pulmonary nodule under the guidance of C-arm X-ray (Figure 2C). The confocal microprobe was accessed to the pulmonary nodule via puncture needle and put in contact with tissues. The confocal endomicroscopic images showed a homogeneous matrix density and disordered tissue structures, without highlighted fibers or black hole structure (Figure 2D). The histopathological data showed fibrin exudation, inflammatory granulation tissues and epithelioid foci at the edge (Figure 2E), diagnosed as tuberculosis.
Figure 2.
Images of peripheral pulmonary nodule obtained from CT, EBUS, X-ray, nCLE and histopathologic examination in case 2. (A) The chest CT showed an irregular solid nodule in the anterior segment of right upper lobe, with no bronchial sign; (B) radial probe endobronchial ultrasound confirmed the lesion location outside the bronchial lumen; (C) the puncture needle was inserted into the right upper lobe lesion under the guidance of C-arm X-ray (black arrow); (D) the confocal endomicroscopic images showed matrix destruction and partial disordered tissue structure (white arrow), with a homogeneous density, without an increased fluorescence of the fibers and spot structures; (E) the histopathological images showed fibrin exudation, inflammatory granulation tissues and epithelioid foci (black arrow) at the edge (hematoxylin-eosin stain, 200×). nCLE, novel needle-based confocal laser endomicroscopy.
Discussion
CLE is a novel technique for exploration of alveolar structures and mucosal tissues in vivo. Elastin accounts for 50% of connective tissue fibers in peripheral pulmonary (4), possesses the autofluorescent properties with an excitation wavelength of 488 nm (5), which makes it the major visible structure under the exploration of confocal endomicroscopy (6,7). Previous studies reported that confocal endomicroscopy with pCLE probes could detect the changes of elastin composition in the airway and alveolar in the lung cancer tissues (8). In the first case of our report, nCLE images showed that the septa structures of alveoli in lung adenocarcinoma were destroyed and disappeared. The tissue reconstruction formed irregular connective tissues and amorphous chaotic structures, exhibiting high fluorescent and hollow area in confocal images. In the second case, CLE imaging of tuberculosis showed partial disordered tissue structures, homogeneous matrix density, mild gray images without increased of fiber fluorescence or black hole structures.
It remains challenging to identify early malignant pulmonary nodules with conventional bronchoscopy, the rate of contributive transbronchial biopsy remains low, varying from 14% to 63% (9). The application of radial probe endobronchial ultrasound has improved the diagnostic yield (77%) of peripheral pulmonary nodules (10,11). However, Kurimoto et al. (10) reported that the ultrasonic probe located adjacent to the lesion had a significantly lower diagnostic yield (42%) than that within the lesion (87%). Consequently, endobronchial ultrasound has its limitation for accurate localization and biopsy guidance for extraluminal lesions. nCLE has a smaller size of probe that allows it to insert through the needle and represents in real-time the morphologies and structures of lung tissues. The accurate analysis of confocal microstructure of intrapulmonary tissues can help to precisely localize a biopsy site, significantly improving the diagnostic yield of bronchoscope biopsy. The exploration of CLE for neoplastic changes could be predicted with a sensitivity of 96.0%, specificity 87.1% and accuracy 91.0% (2). In these two cases, the radial probe endobronchial ultrasound was used to perform exploration and confirm the lesion located outside the lumen. Following a needle punctured into the peripheral pulmonary nodule under the guidance of C-arm X-ray, the confocal miniprobe was then inserted through the needle to perform real-time endomicroscopic imaging of the extraluminal lesion. This method combines multiple endoscopic techniques to achieve accurate localization and synchronously conduct a point-to-point aspiration biopsy, both cases were successfully completed without complications such as hemorrhage and pneumothorax.
This report showed that confocal endomicroscopy was feasible to access the extraluminal pulmonary nodules via a puncture needle for exploration. The nCLE imaging criteria for benign and malignant pulmonary lesion was applied to identify the disordered tissue structures, fluorescent fibers with heterogeneous densities, and spot of black hole structures. This method allowed synchronous insertion of the confocal probe and biopsy needle into the lesion and insures accurate localization, exploration, and matching between the selected tissue biopsy specimens and confocal images.
In conclusion, this report for the first time shows the application of nCLE for microscopic imaging and positioning target biopsies in two cases of peripheral pulmonary nodules. A large atlas of structure criteria of benign or malignant lesion images is necessary for further exploration, while correlation between confocal imaging and pathology needs additional study.
Acknowledgements
Funding: This study was supported by the research special fund for public welfare industry of health (No. 201402024).
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- 1.Hassan T, Piton N, Lachkar S, et al. A Novel Method for In Vivo Imaging of Solitary Lung Nodules Using Navigational Bronchoscopy and Confocal Laser Microendoscopy. Lung 2015;193:773-8. 10.1007/s00408-015-9769-8 [DOI] [PubMed] [Google Scholar]
- 2.Fuchs FS, Zirlik S, Hildner K, et al. Confocal laser endomicroscopy for diagnosing lung cancer in vivo. Eur Respir J 2013;41:1401-8. 10.1183/09031936.00062512 [DOI] [PubMed] [Google Scholar]
- 3.Wijmans L, de Bruin DM, Meijer SL, et al. Real-Time Optical Biopsy of Lung Cancer. Am J Respir Crit Care Med 2016;194:e10-e1. 10.1164/rccm.201603-0657IM [DOI] [PubMed] [Google Scholar]
- 4.Mercer RR, Crapo JD. Spatial distribution of collagen and elastin fibers in the lungs. J Appl Physiol (1985) 1990;69:756-65. [DOI] [PubMed] [Google Scholar]
- 5.Deyl Z, Macek K, Adam M, et al. Studies on the chemical nature of elastin fluorescence. Biochim Biophys Acta 1980;625:248-54. 10.1016/0005-2795(80)90288-3 [DOI] [PubMed] [Google Scholar]
- 6.Thiberville L, Salaun M, Lachkar S, et al. Confocal fluorescence endomicroscopy of the human airways. Proc Am Thorac Soc 2009;6:444-9. 10.1513/pats.200902-009AW [DOI] [PubMed] [Google Scholar]
- 7.Thiberville L, Salaun M, Lachkar S, et al. Human in vivo fluorescence microimaging of the alveolar ducts and sacs during bronchoscopy. Eur Respir J 2009;33:974-85. 10.1183/09031936.00083708 [DOI] [PubMed] [Google Scholar]
- 8.Wellikoff AS, Holladay RC, Downie GH, et al. Comparison of in vivo probe-based confocal laser endomicroscopy with histopathology in lung cancer: A move toward optical biopsy. Respirology 2015;20:967-74. 10.1111/resp.12578 [DOI] [PubMed] [Google Scholar]
- 9.Baaklini WA, Reinoso MA, Gorin AB, et al. Diagnostic yield of fiberoptic bronchoscopy in evaluating solitary pulmonary nodules. Chest 2000;117:1049-54. 10.1378/chest.117.4.1049 [DOI] [PubMed] [Google Scholar]
- 10.Kurimoto N, Miyazawa T, Okimasa S, et al. Endobronchial ultrasonography using a guide sheath increases the ability to diagnose peripheral pulmonary lesions endoscopically. Chest 2004;126:959-65. 10.1378/chest.126.3.959 [DOI] [PubMed] [Google Scholar]
- 11.Chen CH, Cheng WC, Wu BR, et al. Improved diagnostic yield of bronchoscopy in peripheral pulmonary lesions: combination of radial probe endobronchial ultrasound and rapid on-site evaluation. J Thorac Dis 2015;7:S418-25. [DOI] [PMC free article] [PubMed] [Google Scholar]