Abstract
The health impacts of recent global infectious disease outbreaks and other disasters have demonstrated the importance of strengthening public health systems to better protect communities from naturally occurring and human-caused threats. Public health emergency management (PHEM) is an emergent field of practice that draws on specific sets of knowledge, techniques, and organizing principles necessary for the effective management of complex health events.
We highlight how the nascent field of PHEM has evolved in recent years.
We explore this development by first examining multiple sites of intersection between the fields of public health and emergency management. We then analyze 2 of the principal pillars on which PHEM was built: organizational and programmatic (i.e., industry) standards and the incident management system. This is followed by a sketch of the key domains, or functional areas, of PHEM and their application to the emergency management cycle. We conclude with some observations about PHEM in a global context and discuss how the field might continue to evolve.
In recent years, the health impacts of infectious disease outbreaks, natural disasters, industrial and environmental catastrophes, and conflict have captured the world’s attention and reinforced the importance of strengthening public health systems to better protect communities and populations from naturally occurring and human-caused threats. Various approaches and programs have been developed to address these needs in domestic and global contexts, including initiatives to strengthen public health preparedness and global health security. Although much has been written about these approaches,1,2 there are few reports on the interface between public health and emergency management—and even less about what we call “public health emergency management” (PHEM).
PHEM is an emergent field of practice that draws on specific sets of knowledge, techniques, and organizing principles found in the fields of emergency management and public health that are necessary for the effective management of complex health events and emergencies with serious health impacts. Although concepts such as public health preparedness and global health security include significant components of PHEM, the various terms should not be conflated.
We highlight some of the ways the nascent field of PHEM has evolved in recent years. We explore this development by first examining multiple sites of intersection between the fields of public health and emergency management. We then analyze 2 of the principal pillars on which PHEM has been built: organizational and programmatic (i.e., industry) standards and the incident management system (IMS). This is followed by a sketch of the key domains, or functional areas, of PHEM and their application to the emergency management cycle. We conclude with some observations about PHEM in a global context and discuss how the field might continue to evolve.
PUBLIC HEALTH AND EMERGENCY MANAGEMENT
Public health and, of course, emergency management have long histories of engagement in disasters and complex emergencies. Before public health practitioners worked from emergency operations centers (EOCs) or had even heard of an IMS, they were leading or supporting response efforts in numerous infectious disease emergencies, such as those caused by yellow fever, smallpox, and HIV/AIDS, as well as environmental and technological catastrophes, including hurricanes, floods, and industrial chemical releases. Similarly, the field of emergency management, defined here as “the managerial function charged with creating the framework within which communities reduce vulnerability to hazards and cope with disasters,”3 has long been oriented toward an array of emergencies, including but not limited to public health events.
Early forerunners to the field of emergency management were characterized by a mix of efforts such as volunteer disaster relief services, enhancing fire code safety, improving actuarial assessments of insurable risk, and civil defense.4–6 Although modern emergency management is a younger field than is public health, it has become an increasingly professionalized field with its own disciplinary knowledge, professional associations, credentialing, and university-based programs of study.
For much of their respective histories, interactions between public health and emergency management were rare, and for decades little attempt was made to coordinate or align their missions. Moves toward closer alignment can be traced at least as far back as the 1970s, when the field of emergency management began to shift away from its orientation to civil defense, which was focused on nuclear attacks, to a greater range of natural and human-caused hazards and threats (later to be termed “all hazards”).6 In the 1990s, public health similarly broadened its scope, with increased attention to atypical threats such as biological and chemical terrorism, pandemic influenza, and other emergent threats—natural and intentional.
The relationship between public health and emergency management came into sharper focus after the events of September 11, 2001, and efforts to strengthen ties have continued to evolve. Critical drivers to accomplish this include the advent of homeland security as an apparatus of government, which eventually led to the wide-scale adoption of the National Incident Management System by government agencies and state and local recipients of federal preparedness funds.7 The National Incident Management System helps guide the management of incidents and emergency operations and adheres to principles of incident management.
Congressional funding for preparedness programs such as the Public Health Emergency Preparedness program administered by the US Centers for Disease Control and Prevention (CDC) has also been a key driver in bringing public health and emergency management closer together by creating emergency response capacity in health departments at the state and local levels. These various efforts have been accompanied by the establishment and refinement of national-level doctrine codifying the relationship between public health and emergency management in such documents as the National Response Framework8 and its corresponding Emergency Support Function and Biological Incident Annexes.9,10 Guidance has also been offered that describes public health and health care preparedness capabilities that emergency response entities such as health departments and hospitals are expected to have or have access to.11,12
Public health and emergency management have also come together in the professional associations of each field. For example, the International Association of Emergency Managers has organized several caucuses addressing the ramifications of a range of health-related emergencies. Similarly, the National Emergency Management Association has partnered with the Association of State and Territorial Health Officials to form a joint policy work group. This group coordinates federal grant program activities between emergency management agencies and public health departments and aligns exercise requirements across multiple programs, among other things. The National Association of City and County Health Officers, a leading policy and advocacy organization for local health departments in the United States, holds an annual conference focused on issues of public health and health care preparedness, response, and recovery.
Finally, several repositories and producers of knowledge contain or generate content at the intersection of public health and emergency management, including specialized peer-reviewed journals such as Health Security (formerly Biosecurity and Bioterrorism: Biodefense Strategy, Practice and Science) and Disaster Medicine and Public Health Preparedness, and programs housed at academic institutions such as the Preparedness and Emergency Response Research Centers and Learning Centers, which were previously funded by the CDC.
THE EMERGENCY MANAGEMENT CYCLE
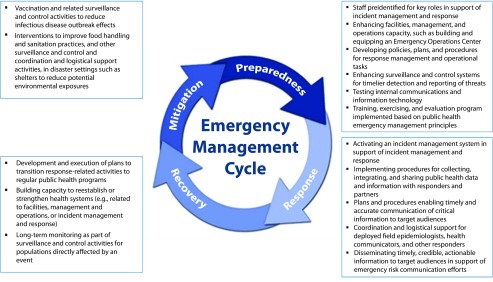
A useful heuristic to understand the relationship between public health and emergency management is the emergency management cycle, which has been described in emergency management curricula, textbooks, and government sources using different models.8,13,14 We adopted a 4-stage model of this cycle that includes mitigation, preparedness, response, and recovery (Figure 1). These 4 phases are useful for describing the capacities and activities of an emergency management system and are closely related to but different from the 5 mission areas and corresponding core capabilities described in the most recent edition (June 2016) of the Federal Emergency Management Agency’s National Response Framework.8
FIGURE 1—
Examples of Public Health Emergency Management (PHEM) Activities Across Phases of the Emergency Management Cycle
Mitigation focuses on reducing hazard losses or risk and controlling anticipated damage; activities in this phase can be carried out before, during, or after an event. “Mitigation” is an infrequently used term in public health or PHEM contexts. Examples of mitigation are targeted human and animal vaccination efforts, animal culling, and other public health control measures, including food safety and sanitation practices to reduce the impact of an infectious disease outbreak or environmental exposure risks in the context of a disaster (e.g., at a shelter or other congregate setting). Preparedness activities occur before an event and center on building or maintaining staff, systems, and infrastructure capacity as well as carrying out the planning, training, and exercising necessary to identify gaps and improve emergency response capabilities. Examples are the development, testing, and evaluation of emergency response plans, notification and warning systems, and surge staffing procedures as well as training staff and enhancing physical and information technology infrastructure such as EOCs and surveillance and reporting systems.
Response in the emergency management cycle occurs in recognition of a hazard that threatens to overwhelm day-to-day functions or capacities. In the public health context, emergency response activities can vary widely but generally include the following:
coordinating select public health response functions across multiple entities or partners;
collecting, integrating, and analyzing epidemiologic, laboratory testing, and other data;
sharing information with partners;
developing and disseminating guidance, emergency risk communication messages, and other recommendations to targeted audiences or at-risk populations; and
coordinating the implementation of control measures such as the distribution and dispensing of appropriate medical countermeasures.
Finally, the recovery phase occurs during and after the response and encompasses efforts to return or adapt to “new” normal conditions after an event. In the public health context, this may include efforts to implement an orderly transition of response-related activities to regular public health programs and functions, capacity-building efforts to reestablish or strengthen health systems, or monitoring long-term sequelae such as mental or behavioral health issues in affected populations following a significant public health emergency or disaster.
STANDARDS
We define standards as codified expectations for practice, typically in the form of guidelines or requirements for functions, processes, resources, or performance in an organization or system.15,16 Standards serve multiple purposes.17 For example, they can drive improvement in an organization or program by serving as the desired end state or outcome of a certain activity (e.g., be able to activate an EOC within 60 minutes of notification). Gaps in capacity or capability can be assessed against the standards and strategies put into place for addressing those gaps. Standards also serve an important accountability function; meeting standards assures funding authorities and governance bodies that organizations and programs are directing their efforts and activities in preferred or even required ways or that their level of performance meets minimally acceptable requirements.
Related to this, standards can also act to enhance trust and credibility in an organization or program. In some disciplines and industries, meeting standards can even convey excellence or elite status. Another key benefit of standards is that they can be recognized and accepted across entire communities of practice, irrespective of geography, type of organization, or individual background. Finally, adherence to standards is verifiable through empirical observation, often through second (i.e., purchaser or funder) or third (independent, outside) party review, which reduces the need to rely exclusively on self-assessment.
The field of PHEM is currently coalescing around several sets of standards and guidelines (Table 1). Public health and health care–related standards are relatively new: most, if not all, have been published within the past 10 years. Standards developed in the field of emergency management have a longer history, with early roots in fire safety and building codes and later developments in a theory of practice linked to the emergency management cycle with significant emphasis on planning, training, exercising, and evaluation.
TABLE 1—
Standards and Related Guidelines That Inform the Field of Public Health Emergency Management
| Standard | Description |
| Center for Medicare and Medicaid Services—emergency preparedness rule18 | Requires a wide range of health care organizations to develop an emergency plan, an emergency communications plan, a training plan, policies and procedures, and implementation of exercises to receive Medicare or Medicaid reimbursement |
| Emergency Management Accreditation Program19 | A voluntary standards, assessment, and accreditation process for disaster preparedness programs throughout the country |
| Health care preparedness and response capabilities12 | Four capabilities, composed of multiple objectives and activities, describing what entities in the health care delivery system should do to effectively prepare for and respond to emergencies |
| International Organization for Standardization 22300—societal security20 | Establishes common understanding on the protection of society from, and response to, incidents, emergencies, and disasters caused by intentional and unintentional human acts, natural hazards, and technical failures |
| National Association of City and County Health Officials—Project Public Health Ready21 | Criteria-based emergency preparedness program developed for local health departments with an emphasis on documentation of an all-hazards preparedness plan, workforce capacity development, and a comprehensive exercise plan |
| National Fire Protection Association 1561: standard on emergency services incident management system and command safety22 | Contains requirements for emergency services on the principles, structure, and operations of an incident management system to ensure the safety of emergency responders and others during an incident |
| National Fire Protection Association 1600: Standard on disaster, emergency management, and business continuity and continuity of operations programs23 | Contains requirements for the development, implementation, assessment, and maintenance of programs for prevention, mitigation, preparedness, response, continuity, and recovery |
| National public health performance standards24 | Forty standards also linked to the 10 essential public health services, whose purpose is to drive improvement at a public health system level in a jurisdiction; emergency management content similar to PHAB standards, with additional content related to legal authority in emergencies |
| PHAB—multiple standards25 | Thirty-two standards linked to the 10 essential public health services for use by agencies seeking public health accreditation; standards related to emergency management include requirements for emergency plans, policies, and procedures; training; exercises; 24/7 operations if needed; surge staffing; emergency risk communications; incident management; continuity of operations; and workforce development |
| Public health preparedness capabilities: national standards for state and local planning11 | Fifteen capabilities composed of functions and tasks that state and local health departments are expected to be able to do on the basis of resources they are expected to have or have access to |
| WHO—Framework for a public health emergency operations center26 | Recently published guidance by WHO for use by ministries of health and other health authorities outlining “key concepts and essential requirements for developing and managing a PHEOC” for the purpose of enabling “a goal-oriented response to public health emergencies” |
Note. PHAB = public health accreditation board; PHEOC = public health emergency operation center; WHO = World Health Organization.
Multiple sets of emergency management standards exist in US and global contexts. These standards tend to include some or all of the following functional areas:
hazard and risk assessment,
planning,
prevention and mitigation,
incident management,
resource management,
communications,
operations, and
training, exercising, evaluation, and corrective action and continuous quality improvement.
In the United States, the gold standard of emergency management standards is part of the Emergency Management Accreditation Program, a voluntary standards, assessment, and accreditation process for disaster preparedness programs throughout the country.19 The Emergency Management Accreditation Program addresses a range of elements and functions expected to be in place for an emergency management program, from administration and finance to communication and warning systems. In 2013, the CDC became the first civilian agency of the US government to receive accreditation by the Emergency Management Accreditation Program in recognition of meeting all necessary standards for its emergency management program.
Related standards include (1) the National Fire Protection Association 1561 and 1600 standards, long embraced by first responder organizations and professional associations as foundational emergency management standards in the United States, and (2) international standards such as the International Organization for Standardization 22300 series, which covers topics such as continuity of operations, incident response, organizational resilience, emergency management capability assessment, and guidelines for exercises.20,22,23
Highlighting these standards is not meant to suggest that these have been adopted evenly, or in some cases at all, across the landscape of public health preparedness and response programs or the nascent field of PHEM. Although many public health preparedness capabilities have, for example, been comprehensively adopted by health departments funded to build or sustain the public health emergency preparedness programs (CDC, unpublished data), emergency management standards such as the Emergency Management Accreditation Program and the National Fire Protection Association 1600 have not. PHEM as a field of practice has begun to take shape in areas where these standards intersect: hazard and risk identification; planning, training, and exercising; use of the IMS; and emergency communication to the public.
INCIDENT MANAGEMENT SYSTEMS
Another fundamental component of PHEM is the IMS. The IMS is a scalable, flexible system for organizing emergency response functions and resources characterized by principles such as standardized roles, modular organization, and unity of command.7 Although it embraces management by objective at the level of an overall response, IMS is in essence a modified command-and-control system.27 An effective IMS hinges on the integration and coordination of staff, systems, and infrastructure under a standardized organizational structure, which is typically managed from an EOC, joint field office, or similar entity. In the United States, recipients of preparedness funding are required to develop an incident management framework that complies with the National Incident Management System.
The National Response Framework describes key contributions of an IMS in a response context, including
(1) developing a single set of objectives, (2) using a collective, strategic approach, (3) improving information flow and coordination, (4) creating a common understanding of joint priorities and limitations, (5) ensuring that no agency’s legal authorities are compromised or neglected, and (6) optimizing the combined efforts of all participants under a single plan.8
Drawing from, and adapting, foundational scholarship in the field, we suggest that the main work of an IMS in a PHEM context includes coordination between functional units or groups of expertise within and across organizations; information collection, integration, and sharing internal to the IMS but also external to response partners and other stakeholders; developing and disseminating public information and warning and crisis and emergency risk communication messages to target audiences and the general public; and providing access to and deployment of resources such as staff and equipment to an EOC or the field (including the management and logistical support of surge staff).28 A fifth purpose, more prominent in certain response contexts, relates to the IMS’s role in informing policy or engaging with elected and other political or senior officials (e.g., to address multifaceted challenges such as mandatory evacuation orders, the quarantine of well individuals, closure of schools or businesses, and recommending travel restrictions to avoid exposure to harmful pathogens).
IMSs are rooted in the concept of the incident command system, a typically on-scene command-and-control organizational structure characterized by standardized functions and terminology initially developed to facilitate interagency coordination and integration of resources for combating wildfires.29 There is significant and ongoing debate about the implementation and effectiveness of the incident command system and IMS. Whether these systems are being implemented appropriately or consistently and whether they are equally effective in managing emergency responses across different hazard and threat contexts are of concern.27,30,31
Despite this, documented examples of IMS use in public health contexts notably increased over the past several years. For example, health departments in the United States have highlighted the successful use of incident command system or IMS principles in various response contexts, including pandemic influenza exercises,32 natural disasters such as floods,33 and vector-borne disease outbreaks.34 Similarly, the use of IMS principles has been noted globally,35–37 and the momentum it has gained internationally has led the World Health Organization to advocate its use in the context of broader emergency management capacity–building efforts.26
In the United States, the CDC has activated its IMS 62 times between 2003 and 2016, including during recent responses to outbreaks of Ebola (2014–2016) and Zika (2016 to the present). However, the CDC has not been immune to IMS implementation challenges. Early efforts to adopt the IMS within the agency were met with variable success. Public health scientists were not clear on how to work effectively in a relatively structured command-and-control model for response activity, and emergency managers were hard pressed to implement the IMS with a public health workforce that was used to handling major infectious disease outbreaks without integration into an emergency management program.38 Related to this were warning signs of a broader clash of professional cultures.
Commentators have noted that a strict application of the IMS to public health may run counter to the “collaborative cultures and decision-making styles found in public health environments.”39(p416) Finally, despite relatively recent contributions to the literature describing beneficial process outcomes of an IMS structure, especially in global contexts,36 the scarcity of evidence illustrating the effectiveness and impact of an IMS prompts important questions about its advantages and why emergency responses should be organized around it.27
Drawing lessons from past experience, the CDC maintains a highly flexible IMS structure able to integrate subject matter expertise and operational capability from traditional public health functions—such as epidemiology and laboratory testing—and from specialized functions—such as community mitigation (e.g., social distancing and school closures), medical countermeasures (e.g., vaccines, prophylactics, respirators, and personal protective equipment), vector control, and birth defects—which can be activated as needed. The CDC organizes these functions under a “scientific response section,” which has been part of all major IMS activations since the agency’s response to H1N1.38
DOMAINS OF PUBLIC HEALTH EMERGENCY MANAGEMENT
Although no definitive list of PHEM domains exists, we have drawn from the literature to suggest some of its principal domains. The domains listed in Table 2 describe specific sets of discrete functional activities that draw on resources or capacities, such as staff with competencies or expertise in specified areas; systems that, using a broad definition, include policies, plans, and procedures as well as processes, protocols, and partnerships; and infrastructure entailing facilities, communication, and information technology and equipment, supplies, and other material goods.
TABLE 2—
Select Key Domains of Public Health Emergency Management
| PHEM Domains | Scope |
| Facilities, management, and operations | Encompasses the EOC facility and related resources as well as the personnel and processes necessary to ensure the effectiveness of day-to-day operations and activation procedures. Examples include the physical structure and supporting infrastructure for an EOC facility and permanent or on-call staff able to activate an IMS quickly. |
| Policies, plans, procedures, and partnerships | Primary reference documents, examples of which include emergency operations plans and continuity of operations plans, as well as policies, standard operating procedures, and protocols that provide guidance and indicate specific PHEM-related management and operational tasks. Also includes personnel with expertise in planning and policy development to develop and update these documents. |
| Internal communications and information technology | Staff, systems, and infrastructure to support internal communications. Examples include teleconferencing equipment, computers, servers, and trained staff who are able to operate available resources and technology to facilitate communication and information exchange between organizations, partners, and other responders. |
| Crisis and emergency risk communication and public information and warning | Staff, systems, and infrastructure for the synthesis and dissemination of accurate and timely information, guidance, warnings, or recommendations aimed at specific target audiences or at-risk populations to enhance knowledge or promote health protective behaviors or other actions. Examples of relevant capacities include public information officers and health communicators, communication plans that address triggers for issuing warnings to the public, procedures to disseminate risk communication messages to targeted or at-risk groups, Web and social media platforms, and media contact information. |
| Surveillance and control | Staff, systems, and infrastructure that facilitate timely, accurate receipt, management, and dissemination of information related to cases of infection, disease, or exposure, clinical management, broader measures of burden of disease or health status, and protocols and procedures to initiate appropriate and timely control measures. Examples include existing and ad hoc surveillance systems, trained epidemiologists and related staff, informatics capacity, and processes to develop guidelines and recommendations for control measures and health protective behaviors. |
| Information collection, integration, and sharing | Staff, systems, and infrastructure to support collection, analysis, integration, visualization, and sharing of public health data and other information generated as part of response operations. Example capacities include data analysts and information management specialists, data use and sharing agreements, standardized data sets, and analytic, data visualization and mapping software. |
| Incident management and response | Staff, systems, and infrastructure that facilitate effective incident management of a public health emergency response using accepted emergency management principles. Example capacities include preidentified staff to fill IMS roles, preestablished decision-making processes, and processes to track and account for the use of resources. |
| Coordination and logistical support of field operations | Staff, systems, and infrastructure that support emergency response field operations, including coordination and logistical support for deployed responders and dispensing of countermeasures. Examples include trained logisticians; infrastructure to support storage, shipping, and dispensing of medical countermeasures; and processes and procedures to prepare and safely deploy responders for field operations. |
| Training, exercising, and evaluation | Staff, systems, and infrastructure that support a training, exercising, and evaluation program on the basis of accepted emergency management and quality improvement principles. Example capacities include a process or program to ensure that responders receive required training, an exercise design and implementation program, and a system of performance monitoring and evaluation to assess capability and performance. |
Note. EOC = emergency operations center; IMS = incident management system; PHEM = public health emergency management.
EMERGENCY MANAGEMENT IN A GLOBAL CONTEXT
Internationally, PHEM is becoming a more prominent fixture in global health initiatives. In 2005 the revised International Health Regulations provided a framework for member countries to better protect their populations from public health threats and emphasized the need for emergency preparedness and response activities to meet their obligations. Despite the International Health Regulations being a binding legal instrument for all member states of the World Health Organization, enforcing obligations under them remains challenging. The Global Health Security Agenda launched in 2014 expanded on International Health Regulations (2005) by strengthening national public health EOCs among other elements of PHEM.2 Aligned with this initiative, the CDC hosts a Public Health Emergency Management Fellowship program to train leaders and practitioners in the global public health community in PHEM concepts and principles.40 Through 2016, this fellowship has graduated 39 health officials from 25 countries. Graduates are versed in the principles of emergency management and trained to implement an emergency management program in a public health context.
Challenges persist in determining how to best maximize limited available resources in public health infrastructure; in some cases, governments’ political will to invest in PHEM systems and capacities is lacking, and money or expertise is instead diverted to other health or economic priorities. In some nations, civil conflict and instability discourage the implementation of national-level strategies to improve public health. The Ebola outbreak in West Africa and Zika virus outbreak in the Americas and elsewhere have underscored the importance of strengthening the PHEM capacities required to prevent, respond to, and recover from public health events. The public health EOC framework developed by the World Health Organization in 2015 attempts to present scalable aspects of PHEM capacities, so national governments can make investments to achieve basic requirements addressing the country’s particular health vulnerabilities and tailor strategies to do so in their specific geopolitical and socioeconomic contexts.26
WHERE DO WE GO FROM HERE?
A spate of recent global disease outbreaks serves as a reminder of the importance of developing and maintaining capacities to effectively manage responses to public health emergencies. We have attempted to sketch some features and pillars of a fluid yet gradually cohering field of PHEM. The future of PHEM as a field of practice is difficult to predict, but its maturation may hinge in part on at least 2 factors. The first factor relates to the need for evidence. Prominent public health programs in areas such as infectious and chronic disease surveillance and prevention depend on high-quality data and evidence of effectiveness.
Similar scientific rigor to evaluate effectiveness or identify best practices does not yet exist across the board for PHEM. Although techniques of evaluation in the form of hotwashes and after-action reviews are key components of emergency management, the field has been slow to adopt scientific evaluation of practice, leaving open questions regarding the effectiveness and impact of PHEM-related activities across the emergency management cycle. Fortunately, public health practitioners and researchers trained in the sciences and evaluation are well positioned to remedy this deficit and yield extensive insights about what—at present—we take to be self-evident.
The second factor relates to instruction and pedagogy. Whether and to what extent PHEM will further cohere as a field of practice will depend on how its core precepts and practices are imparted to entering practitioner cohorts. Will the next generation of public health emergency management practitioners learn from professionals, scholars, and instructors who have extensive experience in PHEM practice, research, or both? Will curricula draw on rigorously evaluated and identified best practices? Will PHEM be taught widely across schools of public health and elsewhere? Will future cohorts of public health professionals embrace precepts of emergency management as tools to help respond to complex public health emergencies? The answers are not yet clear, but the viability of PHEM as a sustainable field of practice in years to come might depend on the results. The CDC has made strides in this area with its Public Health Emergency Management Fellowship program and other efforts to train public health emergency responders and leaders, yet the field has immense room to grow both domestically and internationally. Where will PHEM go from here?
ACKNOWLEDGMENTS
The authors would like to gratefully acknowledge the members of the Division of Emergency Operations, Centers for Disease Control and Prevention (CDC) for their specific contributions to public health emergency management at the CDC.
Note. The findings and conclusions in this article are those of the authors and do not necessarily represent the official position of the CDC.
REFERENCES
- 1.Nelson C, Lurie N, Wasserman J, Zakowski S. Conceptualizing and defining public health emergency preparedness. Am J Public Health. 2007;97(suppl 1):S9–S11. doi: 10.2105/AJPH.2007.114496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Katz R, Sorrell EM, Kornblet SA, Fischer JE. Global health security agenda and the international health regulations: moving forward. Biosecur Bioterror. 2014;12(5):231–238. doi: 10.1089/bsp.2014.0038. [DOI] [PubMed] [Google Scholar]
- 3.Federal Emergency Management Agency. Principles of emergency management supplement. 2007. Available at: https://www.fema.gov/media-library-data/20130726-1822-25045-7625/principles_of_emergency_management.pdf. Accessed March 15, 2017.
- 4.Rubin CB. Emergency Management: The American Experience 1900–2010. 2nd ed. Boca Raton, FL: CRC Press; 2012. [Google Scholar]
- 5.Knowles SG. The Disaster Experts: Mastering Risk in Modern America. Philadelphia, PA: University of Pennsylvania Press; 2011. [Google Scholar]
- 6.Lakoff A. Preparing for the next emergency. Public Culture. 2007;19(2):247–271. [Google Scholar]
- 7.Federal Emergency Management Agency. National Incident Management System. 2008. Available at: https://www.fema.gov/pdf/emergency/nims/NIMS_core.pdf. Accessed March 8, 2017.
- 8.US Department of Homeland Security. National Response Framework. 2016. Available at: https://www.fema.gov/media-library/assets/documents/117791. Accessed January 9, 2017.
- 9.US Department of Homeland Security. Emergency support function #8—public health and medical services annex. 2016. Available at: https://www.fema.gov/media-library-data/1470149644671-642ccad05d19449d2d13b1b0952328ed/ESF_8_Public_Health_Medical_20160705_508.pdf. Accessed March 10, 2017.
- 10.US Department of Homeland Security. Biological incident annex. 2008. Available at: https://www.fema.gov/media-library-data/20130726-1825-25045-1567/biological_incident_annex_2008.pdf. Accessed March 10, 2017.
- 11.Centers for Disease Control and Prevention. Public health preparedness capabilities: national standards for state and local planning. 2011. Available at: https://www.cdc.gov/phpr/readiness/capabilities.htm. Accessed December 21, 2016.
- 12.Office of the Assistant Secretary for Preparedness and Response. 2017–2022 Health care preparedness and response capabilities. 2016. Available at: https://www.phe.gov/Preparedness/planning/hpp/reports/Documents/2017-2022-healthcare-pr-capablities.pdf. Accessed January 6, 2017.
- 13.National Earthquake Hazards Reduction Program. Introduction to emergency management. Available at: http://training.fema.gov/EMIWeb/EarthQuake/NEH0101220.htm. Accessed January 9, 2017.
- 14.Fagel MJ. Principles of Emergency Management and Emergency Operations Centers (EOC) Boca Raton, FL: CRC Press; 2010. [Google Scholar]
- 15.Office of Management and Budget. OMB circular no. A-119: Federal participation in the development and use of voluntary consensus standards and in conformity assessment activities. 2016. Available at: https://www.nist.gov/sites/default/files/revised_circular_a-119_as_of_01-22-2016.pdf. Accessed January 9, 2017.
- 16.Bowker GC, Star SL. Sorting Things Out: Classification and Its Consequences. Cambridge, MA: MIT Press; 1999. [Google Scholar]
- 17.Lampland M, Star SL, editors. Standards and Their Stories: How Quantifying, Classifying, and Formalizing Practices Shape Everyday Life. Ithaca, NY: Cornell University Press; 2009. [Google Scholar]
- 18.Centers for Medicare & Medicaid Services. Emergency preparedness rule. 2016. Available at: https://www.cms.gov/Medicare/Provider-Enrollment-and-Certification/SurveyCertEmergPrep/Emergency-Prep-Rule.html. Accessed December 21, 2016.
- 19.Emergency Management Accreditation Program. Emergency management standard ANSI/EMAP 4-2016. 2016. Available at: https://www.emap.org/index.php/root/about-emap/96-emap-em-4-2016/file. Accessed August 7, 2017.
- 20.International Organization for Standardization. ISO 22300: Societal security—terminology. 2012. Available at: https://www.iso.org/obp/ui/#iso:std:iso:22300:ed-1:v1:en. Accessed December 21, 2016.
- 21.National Association of County and City Health Officials. Project public health ready criteria. 2015. Available at: http://www.naccho.org/uploads/downloadable-resources/PPHR-Criteria-Version-8-FINAL-2.pdf. Accessed December 21, 2016.
- 22.National Fire Protection Association. NFPA 1561: Standard on emergency services incident management system and command safety. Available at: http://www.nfpa.org/codes-and-standards/all-codes-and-standards/list-of-codes-and-standards/detail?code=1561. Accessed December 21, 2016.
- 23.National Fire Protection Association. NFPA 1600: Standard on disaster/emergency management and business continuity/continuity of operations programs. Available at: http://www.nfpa.org/codes-and-standards/all-codes-and-standards/list-of-codes-and-standards/detail?code=1600. Accessed December 21, 2016.
- 24.Association of State and Territorial Health Officials. National public health performance standards. Available at: http://www.astho.org/Programs/Accreditation-and-Performance/National-Public-Health-Performance-Standards. Accessed December 21, 2016.
- 25.Public Health Accreditation Board. Standards: an overview. 2013. Available at: http://www.phaboard.org/wp-content/uploads/StandardsOverview1.5_Brochure.pdf. Accessed December 21, 2016.
- 26.World Health Organization. Framework for a public health emergency operations centre. 2015. Available at: http://apps.who.int/iris/bitstream/10665/196135/1/9789241565134_eng.pdf?ua=1. Accessed December 21, 2016.
- 27.Jensen J, Thompson S. The incident command system: a literature review. Disasters. 2016;40(1):158–182. doi: 10.1111/disa.12135. [DOI] [PubMed] [Google Scholar]
- 28.Quarantelli EL. Final Project Report No. 24: Studies in Disaster Response and Planning. Columbus, OH: The Ohio State University; 1979. [Google Scholar]
- 29.Stambler KS, Barbera JA. Engineering the Incident Command and Multiagency Coordination systems. J Homel Secur Emerg. 2011;8(1):43. [Google Scholar]
- 30.Jensen J, Waugh WL. The United States’ experience with the Incident Command System: what we think we know and what we need to know more about. J Contingencies Crisis Manage. 2014;22(1):5–17. [Google Scholar]
- 31.Rimstad R, Braut GS. Literature review on medical incident command. Prehosp Disaster Med. 2015;30(2):205–215. doi: 10.1017/S1049023X15000035. [DOI] [PubMed] [Google Scholar]
- 32.Branum A, Dietz JE, Black DR. An evaluation of local incident command system personnel in a pandemic influenza. J Emerg Manag. 2010;8(5):39–46. [Google Scholar]
- 33.Wiedrich TW, Sickler JL, Vossler BL, Pickard SP. Critical systems for public health management of floods, North Dakota. J Public Health Manag Pract. 2013;19(3):259–265. doi: 10.1097/PHH.0b013e3182641b39. [DOI] [PubMed] [Google Scholar]
- 34.Adams EH, Scanlon E, Callahan JJ, 3rd, Carney MT. Utilization of an incident command system for a public health threat: West Nile Virus in Nassau County, New York, 2008. J Public Health Manag Pract. 2010;16(4):309–315. doi: 10.1097/PHH.0b013e3181bb8392. [DOI] [PubMed] [Google Scholar]
- 35.Elachola H, Al-Tawfiq JA, Turkestani A, Memish ZA. Public health emergency operations center—a critical component of mass gatherings management infrastructure. J Infect Dev Ctries. 2016;10(8):785–790. doi: 10.3855/jidc.8332. [DOI] [PubMed] [Google Scholar]
- 36.Centers for Disease Control and Prevention. Incident management systems and building emergency management capacity during the 2014–2016 Ebola epidemic—Liberia, Sierra Leone, and Guinea. MMWR Suppl. 2016;65(3):28–34. doi: 10.15585/mmwr.su6503a5. [DOI] [PubMed] [Google Scholar]
- 37.Cruz MA, Hawk NM, Poulet C, Rovira J, Rouse EN. Public health incident management: logistical and operational aspects of the 2009 initial outbreak of H1N1 influenza in Mexico. J Emerg Manag. 2015;13(1):71–77. doi: 10.5055/jem.2015.0219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Papagiotas SS, Frank M, Bruce S, Posid JM. From SARS to 2009 H1N1 influenza: the evolution of a public health incident management system at CDC. Public Health Rep. 2012;127(3):267–274. doi: 10.1177/003335491212700306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bochenek R, Grant M, Schwartz B. Enhancing the relevance of incident management systems in public health emergency preparedness: a novel conceptual framework. Disaster Med Public Health Prep. 2015;9(4):415–422. doi: 10.1017/dmp.2015.62. [DOI] [PubMed] [Google Scholar]
- 40.Centers for Disease Control and Prevention. CDC emergency operations center: public health emergency management fellowship. Available at: https://www.cdc.gov/phpr/eoc/emergencymanagementfellowship.htm. Accessed January 6, 2017.