Abstract
Objectives. To demonstrate how inclusion of the Centers for Disease Control and Prevention’s Community Assessment for Public Health Emergency Response (CASPER) as a tool in Public Health Preparedness Capabilities: National Standards for State and Local Planning can increase public health capacity for emergency response.
Methods. We reviewed all domestic CASPER activities (i.e., trainings and assessments) between fiscal years 2012 and 2016. Data from these CASPER activities were compared with respect to differences in geographic distribution, type, actions, efficacy, and usefulness of training.
Results. During the study period, the Centers for Disease Control and Prevention conducted 24 domestic in-person CASPER trainings for 1057 staff in 38 states. On average, there was a marked increase in knowledge of CASPER. Ninety-nine CASPERs were conducted in the United States, approximately half of which (53.5%) assessed preparedness; the others were categorized as response or recovery (27.2%) or were unrelated to a disaster (19.2%).
Conclusions. CASPER trainings are successful in increasing disaster epidemiology skills. CASPER can be used by Public Health Emergency Preparedness program awardees to help build and sustain preparedness and response capabilities.
No US state or territory is exempt from the devastation of a natural or human-induced disaster (e.g., tornado, hurricane, oil spill, water contamination). Responding appropriately and effectively to the public health consequences of environmental disasters, whether natural or human induced, requires timely access to accurate information. Public health data are especially important to provide vital situational awareness and increase public health decision support, which may significantly influence resource allocation strategies and approaches for implementing public health response priorities, including preventive and protective measures for affected populations. Epidemiological methods, including rapid needs assessments, can provide reliable and actionable data for emergency management throughout the disaster life cycle (preparedness, response, recovery, and mitigation).1
To assist states in capturing critical epidemiological data throughout the disaster life cycle, the Health Studies Branch (HSB), part of the National Center for Environmental Health of the Centers for Disease Control and Prevention (CDC), developed the Community Assessment for Public Health Emergency Response (CASPER) methodology.2 CASPER is a rapid needs assessment designed to quickly gather household-based information on the health status and basic requirements of communities.
CASPER is modeled on the World Health Organization’s Expanded Programme on Immunization survey technique for estimating vaccine coverage.3,4 The design is a cluster sampling methodology wherein a set number (e.g., 30) of clusters (i.e., mutually exclusive groups in a population) are selected in the first stage and a set number (e.g., 7) of individuals or households are interviewed from each selected cluster in the second stage. Although there are variations in the methodology, the CASPER toolkit recommends the 30 × 7 sampling design to gain 210 interviews in the sampling frame. Results of data obtained with the 30 × 7 sampling design are weighted during analyses to provide population estimates with a precision of plus or minus 10 percentage points.3,4
CASPER is an important tool in public health disaster response. When a CASPER is conducted, the information it generates can be used by emergency managers to make informed decisions, allocate scarce resources, provide valid information to the news media to dispel rumors, support funding needs for recovery efforts, and plan for future disasters.5 For example, during the 2009 ice storms in Kentucky, CDC and the Kentucky Department for Public Health conducted a CASPER and identified the community’s need for additional supplies of supplemental oxygen.5,6 The Kentucky Department for Public Health also used CASPER data to determine the need to disseminate targeted public health messages on the dangers of carbon monoxide, educate the community on safe use of generators, and modify future emergency plans to account for gaps such as pet-friendly shelters and early communication messaging.7
Although CASPER was originally designed to provide information during disaster responses, it is also used throughout the disaster life cycle to obtain population-representative data. CASPER is also useful for collecting community public health information unrelated to a disaster. For example, public health departments used CASPERs to identify household-level information about chronic respiratory conditions, ascertain knowledge about emerging infectious diseases such as Zika virus and H1N1, and assess community awareness, opinions, and concerns on subjects such as coal gasification plants, healthy homes, community health, and radiation emergency preparedness.8–12
HSB developed the CASPER toolkit to provide standard criteria for implementation among public health practitioners and emergency management personnel.2 The first edition was released in 2009 and the second in 2012. To supplement the toolkit, HSB developed an interactive CASPER Web site and provides in-person trainings, by request, for state, tribal, local, and territorial (STLT) health department staff; emergency managers; and others. HSB staff educate participants about when to conduct a CASPER, the local capabilities required for conducting an assessment, and how to appropriately implement the assessment in the field. Each 1-day CASPER training is provided by HSB subject matter experts and tailored toward the specific requesting audience. Participant evaluations are often collected at the end of the training to gauge the usefulness and efficacy of the training and to help improve future trainings. HSB also provides technical assistance to support conducting CASPERs nationwide.
In 2011 CDC, in consultation with the Association of State and Territorial Health Officials and the National Association of County and City Health Officials, developed and published standards to aid STLT health departments in prioritizing use of federal funding received under the Public Health Emergency Preparedness (PHEP) program.13 These standards drew from directives in national public health preparedness legislation,14–16 the Pandemic and All-Hazards Preparedness Act,17 and the National Health Security Strategy.18 The CDC PHEP program provides funding for STLT public health departments across the nation to upgrade their ability to effectively respond to a range of public health threats including natural disasters, infectious diseases, and biological, chemical, nuclear, and radiological events. Since 2002, the PHEP program has provided 62 STLT awardees with more than $11 billion in funding to prepare for and respond to public health emergencies.
Public Health Preparedness Capabilities: National Standards for State and Local Planning (hereafter Public Health Preparedness Capabilities) identifies 15 public health preparedness and response capabilities that serve as national standards for planning and response to public health emergencies.13 CASPER is referenced within the community recovery (capability 2) and mass care (capability 7) capability standards as a resource to identify and monitor the care and recovery needs of public health, medical, and mental–behavioral health in the community after a disaster or public health emergency.
The community recovery capability highlights specific recommendations and guidance that can help communities recover, including identifying and monitoring public health, medical, and mental–behavioral health system recovery needs. The mass care capability provides recommendations and guidance to PHEP awardees about “working with partner agencies to address the public health, medical, and mental/behavioral health needs of those impacted, and includes conducting ongoing active surveillance and community assessment.”13 Here we demonstrate how the use of CASPER as a tool for community recovery and mass care, as described in Public Health Preparedness Capabilities, can increase state and local public health capacity for emergency response.
METHODS
We reviewed all domestic CASPER activities (i.e., trainings and assessments) occurring between fiscal year (FY) 2012 and FY2016. FY2012 was selected because Public Health Preparedness Capabilities, which contained the CASPER recommendations, was published in spring 2011. These standards clarified that public health programs could invest FY2012 PHEP funds to operationalize CASPER-related activities, including training activities and conducting CASPER assessments.
Information about CASPER training led by HSB subject matter experts, including evaluation results, is stored in an internal database. Training evaluations are self-administered by attendees, who are asked to rate statements about the instruction, design, usefulness, and content of the training as well as their skill levels in conducting various aspects of CASPER before and after the training. Additional information captured in the database includes geographic location, number of individuals trained, and evaluations of the efficacy and usefulness of the training. Information on all CASPERs in which HSB provided any type of assistance to state or local health departments is also routinely collected and maintained. Captured data includes date, purpose of the CASPER, sampling frame, and event stage (e.g., preparedness, response, recovery).
We obtained information on CASPERs not originally captured within the HSB database via a request form on the CDC CASPER Web site interactive map (https://www.cdc.gov/nceh/hsb/disaster/casper/casper_map.htm)9 and reviews of ProQuest, PubMed, Google Scholar, and the National Institutes of Health Disaster Research Response database; we used the keywords “Community Assessment for Public Health Emergency Response” as a single search term in our search of these databases. Two CASPER subject matter experts reviewed the information obtained from these sources for the terms “CASPER” and “training,” as well as other information about CASPER type and location. The information was then added to the database.
We compared data on all CASPERs and trainings conducted from FY2012 through FY2016 with respect to differences in geographic distribution, type of activity, and results or actions taken by decision-makers. We only included in-person, domestic CASPER training sessions that were not a part of a CASPER assessment; international, Webinar, and “just-in-time” trainings were excluded. Evaluations varied slightly depending on training, and therefore we included only responses from questions common to at least 4 evaluations. Self-efficacy response scales ranged from not at all confident (score of 0) to very confident (score of 5). The percentages reported are percentages among those who responded to the individual questions. We used Microsoft Excel 2010 software (Microsoft Corp, Redmond, WA) in conducting our data analyses.
RESULTS
We found the following results for CASPER training and CASPER assessments.
CASPER Trainings
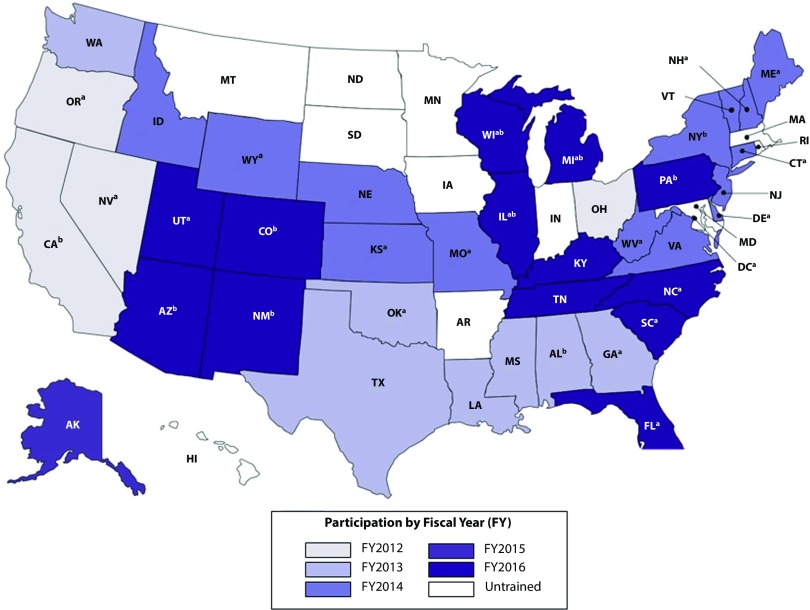
From October 1, 2012, through September 30, 2016, HSB conducted 24 domestic in-person CASPER trainings for 1057 public health and emergency management staff in 38 states (Figure 1). We recorded evaluations from 457 staff (43.2%) involved in 16 trainings (66.6%).
FIGURE 1—
Community Assessment for Public Health Emergency Response (CASPER) Trainings: United States, Fiscal Year 2012 to Fiscal Year 2016
aIndicates states with fewer than 10 participants.
bIndicates states that hosted > 1 training.
The majority of people trained considered themselves epidemiologists (42.0%) or preparedness staff (23.0%). Other job categories included, but were not limited to, environmental staff (8.3%), nurses (7.4%), and students (2.8%). Evaluations were obtained from 6 (1.3%) emergency managers who attended the trainings. The majority of these individuals (89.2%) strongly agreed or agreed that the CASPER training was useful for their job, and 97.4% found that the training helped them understand the uses of CASPER for public health. The trainings were generally well received, with 90.6% of participants strongly agreeing or agreeing that the material was presented at the correct level, that the instructors were clear (91.6%), and that activities were helpful in understanding the material (93.4%; Table 1).
TABLE 1—
Evaluation of Community Assessment for Public Health Emergency Response (CASPER) Trainings: United States, Fiscal Year 2012 to Fiscal Year 2016
| Component | Strongly Disagree, No. (%) | Disagree, No. (%) | Neutral, No. (%) | Agree, No. (%) | Strongly Agree, No. (%) |
| Training helpful in understanding use of CASPER (n = 392) | 0 (0.0) | 1 (0.2) | 9 (2.0) | 99 (21.7) | 283 (61.9) |
| Instructors presented clearly (n = 455) | 0 (0.0) | 2 (0.4) | 36 (7.9) | 135 (29.6) | 282 (62.0) |
| Material presented at correct level (n = 454) | 1 (0.2) | 6 (1.3) | 33 (7.3) | 144 (31.7) | 270 (59.4) |
| Activities helpful in understanding material (n = 454) | 0 (0.0) | 1 (0.2) | 29 (6.4) | 170 (37.4) | 254 (55.9) |
| Training useful for job (n = 455) | 0 (0.0) | 6 (1.3) | 43 (9.5) | 164 (36.0) | 242 (53.2) |
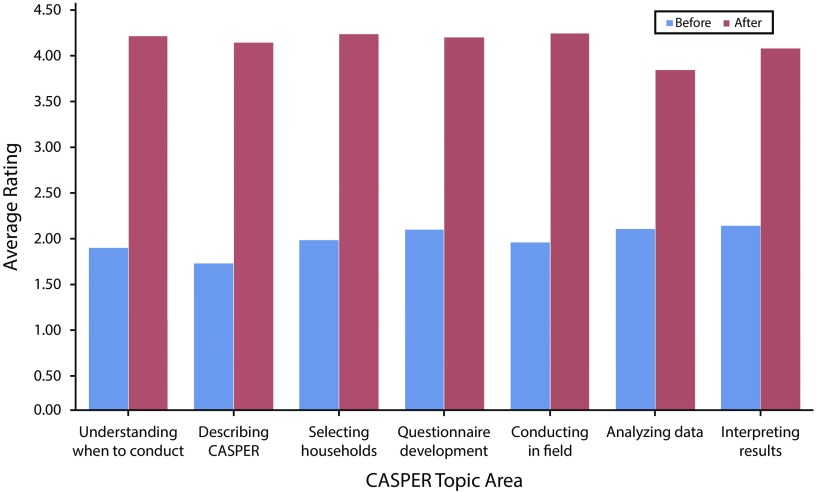
Attendees were asked to rate their skills in each CASPER topic area before and after the training. On average, there were marked posttraining increases in knowledge about when to conduct a CASPER, how to conduct a CASPER, selecting households to interview, conducting CASPERs in the field, developing CASPER questionnaires, and interpreting CASPER results (Figure 2).
FIGURE 2—
Reported Community Assessment for Public Health Emergency Response (CASPER) Knowledge From Trainings: United States, Fiscal Year 2012 to Fiscal Year 2016
CASPER Assessments
During the 5-year study period, 99 CASPERs were conducted in the United States (Table 2). CDC personnel were deployed for 11 CASPERs (11.1%) and provided remote technical assistance for 48 others (48.5%); CDC personnel were not actively involved (e.g., no assistance provided, no technical assistance beyond initial conversations) in the remaining 40 CASPERs (40.4%). The majority of CASPERs (86.9%) took place in states where in-person training had previously been conducted.
TABLE 2—
Attributes of Community Assessments for Public Health Emergency Response (CASPERs) Conducted: United States, Fiscal Year 2012 to Fiscal Year 2016
| Variable | Preparedness, No. (%) | Response/Recovery, No. (%) | Other, No. (%) | Total, No. (%) |
| Fiscal year | ||||
| 2012 | 13 (61.9) | 6 (28.6) | 2 (9.5) | 21 (21.2) |
| 2013 | 8 (50.0) | 5 (31.3) | 3 (18.7) | 16 (16.2) |
| 2014 | 12 (60.0) | 5 (25.0) | 3 (15.0) | 20 (18.2) |
| 2015 | 8 (38.1) | 5 (23.8) | 8 (38.1) | 21 (21.2) |
| 2016 | 12 (57.1) | 6 (28.6) | 3 (14.3) | 21 (21.2) |
| Type of CASPER assistance | ||||
| In field | 3 (27.3) | 8 (72.7) | NA | 11 (11.1) |
| Remote technical assistance | 26 (54.2) | 14 (29.2) | 8 (16.7) | 48 (48.5) |
| Limited/none | 24 (60.0) | 5 (12.5) | 11 (27.5) | 40 (40.4) |
| Training completed in state | ||||
| Yes | 49 (52.1) | 27 (28.7) | 18 (19.1) | 94 (94.9) |
| Training received before CASPERa | 45 (52.3) | 24 (27.9) | 17 (19.8) | 86 (91.5) |
| Training received after CASPER | 4 (50.0) | 3 (37.5) | 1 (12.5) | 8 (8.5) |
| No | 4 (80.0) | NA | 1 (20.0) | 5 (5.1) |
| Publication type | ||||
| Unpublished report | 14 (36.8) | 13 (34.2) | 11 (28.9) | 38 (38.4) |
| Peer-reviewed journal/MMWR | 7 (50.0) | 5 (35.7) | 2 (14.3) | 14 (14.1) |
| Other (e.g., news article) | 7 (58.3) | 4 (33.3) | 1 (8.3) | 12 (12.1) |
| Unknown/none | 26 (74.3) | 4 (11.4) | 5 (14.3) | 35 (35.4) |
| Recommendation (n = 59) | ||||
| Educate community/engage in outreach | 13 (35.1) | 18 (48.6) | 6 (16.2) | 37 (62.7) |
| Revise/improve plans | 18 (48.6) | 17 (45.9) | 2 (5.4) | 37 (62.7) |
| Prioritize response or action items | 10 (31.3) | 11 (34.4) | 11 (34.4) | 32 (54.2) |
| Provide services (mental health, utilities) | NA | 13 (100) | NA | 13 (22.0) |
| Compare results with baseline data | 5 (41.7) | 3 (25.0) | 4 (33.3) | 12 (20.3) |
| Allocate additional resources/funding | NA | 7 (77.8) | 2 (22.2) | 9 (15.3) |
| Conduct follow-up CASPER/research | 1 (14.3) | 5 (71.4) | 2 (28.6) | 8 (13.6) |
| Otherb | 19 (52.8) | 6 (16.6) | 11 (30.6) | 36 (61.0) |
| Actions by decision-makers | ||||
| Yes, documented | 3 (15.8) | 13 (68.4) | 3 (15.8) | 19 (19.2) |
| Unknown | 50 (62.5) | 14 (17.5) | 16 (20.0) | 80 (80.8) |
Note. MMWR = Morbidity and Mortality Weekly Report; NA = not applicable. The sample size was n = 99.
Includes states where training was conducted before fiscal year 2012.
Includes recommendations such as improve future assessment planning, improve use of technology, and work with partners.
Approximately half of CASPERs (n = 53; 53.5%) were preparedness CASPERs designed to help advance jurisdictional disaster planning through assessing household emergency preparedness, evacuation plans, and other activities. The remaining were response or recovery CASPERs (n = 27; 27.2%) or were not related to a disaster (n = 19; 19.2%). These CASPERs focused on topics such as Zika virus knowledge, obesity and household nutrition, and housing. Use of CASPERs was proportionally similar among the categories over each of the 5 years with the exception of 2015.
The results of approximately two thirds of CASPERs (64.6%) were shared in a searchable manner (e.g., unpublished report, conference presentation posted online, peer-reviewed journal). Only 14.1% of results were published in peer-reviewed journals or the Morbidity and Mortality Weekly Report. Of the 59 (59.6%) CASPERs with documented recommendations, the most common recommendations were related to community education or outreach (62.7%) and revising or improving plans (62.7%), followed by prioritizing responses or actions on the basis of CASPER results (54.2%). Among response or recovery CASPERs, 22.0% recommended providing some type of service (e.g., mental health services, restoration of utilities, medication refills).
Overall, demonstrated use of CASPER findings to support specific public health actions taken by health authorities or emergency management officials was documented for 19 (19.2%) assessments, most often (68.4%) among response or recovery CASPERs.
For example, Napa County, California, conducted a CASPER in response to the 2014 South Napa earthquake that showed that many injuries occurred during cleanup activities.19 On the basis of these results, the county engaged in a public outreach campaign to communicate the importance of having earthquake-specific emergency supplies (e.g., heavy gloves) and of seeking medical evaluations for injuries. In addition, to address the psychological trauma associated with the disaster, Napa County Mental Health used CASPER information to reallocate mental health resources and conduct public training sessions and education campaigns to support those with mental health risks. Finally, Napa County Public Health conducted community social events on the 1-year anniversary of the earthquake and psychological first-aid training for outreach workers to promote community resilience and future earthquake preparedness.19
Unfortunately, the majority (80.0%) of CASPERs did not document implementation of recommendations based on CASPER findings.
DISCUSSION
Here we have shown that CASPER is an effective and frequently employed tool for public health emergency management and demonstrated how use of CASPER as a public health emergency preparedness and response tool can increase state and local public health emergency response capacities. CASPER trainings demonstrate increased disaster epidemiology skills among participants. Participant comments indicate that a key benefit of in-person CASPER training is its mixed audience of epidemiologists, emergency managers, disease surveillance staff, and others who do not regularly interact with each other owing to the diversity of their missions and separate physical locations.
Therefore, in-person training not only provides instruction on the implementation of an important disaster epidemiology tool, but it also offers opportunities to form common understandings among stakeholders and identify the value of each of their roles throughout the disaster life cycle. For example, CASPER training provides the opportunity to increase emergency managers’ awareness that epidemiologists can provide specific, relevant, and useful planning data about the needs of a community as a whole or the needs of vulnerable populations.
Although originally designed for disaster response, CASPERs can be used throughout the disaster life cycle and in nondisaster situations, and they can contribute to informing jurisdictional risk assessments as required by the CDC PHEP Program. Since the inclusion of CASPERs in the Public Health Preparedness Capabilities community recovery and mass care standards, they have been used increasingly for nonresponse purposes.5
The majority of CASPERs conducted each year are now used to guide preparedness planning. Not only can a preparedness CASPER provide essential data for planning, such as educating the community, targeting outreach campaigns, revising public health preparedness and response plans, and prioritizing action items, but it also allows public health and emergency management staff to use the tool in a less pressing environment. A preparedness CASPER readies the workforce for conducting a response CASPER, affording workforce members the opportunity to receive feedback and incorporate lessons learned from after-action reports, discussions, and evaluations of performance.
In addition to highlighting the benefits of CASPER trainings and assessments in the context of Public Health Preparedness Capabilities, we have identified areas for improvement, in particular publicizing the results of CASPERs. We included only those CASPERs reported to CDC or published. Therefore, CASPERs conducted without the knowledge of the CDC were excluded. Very few CASPERs (14%) were described and published in peer-reviewed journals. Also, more than a third 35.4%) of the CASPERs we included could not be found by searching the literature or the Internet. These CASPERs were included only because information about them was tracked in HSB’s internal database.
These findings emphasize the need to increase publication and reporting of CASPERs. Disseminating CASPER findings and sharing lessons learned with the wider public health community are important to highlight common problems and opportunities for improvement that exist across many communities.5,20,21 Publishing findings in peer-reviewed journals, adding information to the CDC CASPER interactive map, and presenting data at conferences are important ways to disseminate CASPER results, lessons learned, and the application of this methodology to the field of emergency preparedness, response, and recovery.
In addition, there is a need to increase follow-up on actions taken on the basis of CASPER results. Reports from less than one quarter of CASPERs described specific actions taken by decision-makers to implement recommendations. It is likely that this low number is the result of lack of follow-up or publication. However, even when results are published, they are often published before implementation of recommendations. The PHEP program awardees could play a valuable role in filling this information gap by disseminating actions taken as a result of CASPER findings.
Finally, although the timing of the publication of Public Health Preparedness Capabilities corresponded with an increase in CASPER trainings and implementations,5 we cannot make a direct causal link to the increasing numbers of CASPER trainings and CASPERs conducted. Also, we cannot determine whether the people who attended the in-person CASPER trainings were those who eventually organized CASPERs within their state.
PUBLIC HEALTH IMPLICATIONS
There are many opportunities for CASPERs to influence public health. CASPERs can be used as an evidence-based practice for meeting some of the standards published in Public Health Preparedness Capabilities. PHEP awardees can build and sustain capability through CASPER trainings and assessments. To further advance CASPER as a resource for public health emergency management, we encourage continued CDC reviews of PHEP-funded jurisdictions to identify current CASPER knowledge, interest in training, and assessments conducted. As jurisdictions become trained in the CASPER methodology and comfortable in implementing CASPERs, they rely less on CDC assistance and thus build their internal capacity to prepare for, respond to, and recover from disasters. We also encourage publication and reporting of CASPERs on the CDC CASPER interactive map.
CASPER has been shown to be a useful tool for assessing community needs throughout the disaster life cycle and in nondisaster situations. Through PHEP investments, STLT public health departments are able to use CASPERs to improve their capabilities in all disaster phases and to provide emergency management staff with community-level preparedness information. Continued prioritization of PHEP funding for ongoing training is necessary to ensure that CASPER knowledge is institutionalized within state, local, and territorial public health systems. As jurisdictions are increasingly able to implement CASPERs, it is important that they share lessons learned and disseminate information to promote the usefulness of the tool.
HUMAN PARTICIPANT PROTECTION
No protocol approval was needed for this study because no human participants were involved.
REFERENCES
- 1.Malilay J, Heumann M, Perrotta D et al. The role of applied epidemiology methods in the disaster management cycle. Am J Public Health. 2014;104(11):2092–2102. doi: 10.2105/AJPH.2014.302010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Community Assessment for Public Health Emergency Response (CASPER) 2nd ed. Atlanta, GA: Centers for Disease Control and Prevention; 2012. [Google Scholar]
- 3.Malilay J, Flanders WD, Brogan D. A modified cluster-sampling method for post-disaster rapid assessment of needs. Bull World Health Organ. 1996;74(4):399–405. [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization. Immunization coverage cluster survey reference manual. Available at: http://apps.who.int/iris/bitstream/10665/69087/1/WHO_IVB_04.23.pdf. Accessed July 10, 2017.
- 5.Bayleyegn T, Schnall AH, Ballou SG et al. Use of Community Assessments for Public Health Emergency Response (CASPERs) to rapidly assess public health issues—United States, 2003–2012. Prehosp Disaster Med. 2015;30(4):374–381. doi: 10.1017/S1049023X15004938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Public Health Emergency Response to the Major Ice Storm in Kentucky—2009. Final Report. Atlanta, GA: Centers for Disease Control and Prevention; 2009. [Google Scholar]
- 7.Lutterloh EC, Iqbal S, Clower JH et al. Carbon monoxide poisoning after an ice storm in Kentucky, 2009. Public Health Rep. 2011;126(suppl 1):108–115. doi: 10.1177/00333549111260S114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Black E. County going door-to-door during CASPER next week. Available at: http://www.theleafchronicle.com/story/news/local/2016/07/19/county-going-door–door-during-casper-next-week/87287480. Accessed July 10, 2017.
- 9.Centers for Disease Control and Prevention. Interactive map of CASPERs. Available at: https://www.cdc.gov/nceh/hsb/disaster/casper/casper_map.htm. Accessed July 10, 2017.
- 10.St. Louis County Department of Public Health. Community respiratory health survey to compare residents near Bridgeton Landfill and matched populations in St. Louis County, Missouri. Available at: https://www.stlouisco.com/Portals/8/docs/health/Bridgeton%20Respiratory%20Health%20Survey/Bridgeton%20Respiratory%20Health%20Survey%20-%20Full%20Report.pdf. Accessed July 10, 2017.
- 11.Ylitalo KR, Umstattd M, Stone K, Doyle E, Curtis R. Using the Community Assessment for Public Health Emergency Response (CASPER) to assess barriers to healthy eating and active living in a low-income community. Eval Program Plann. 2016;59:41–46. doi: 10.1016/j.evalprogplan.2016.08.003. [DOI] [PubMed] [Google Scholar]
- 12.Nyaku MK, Wolkin AF, McFadden J et al. Assessing radiation emergency preparedness planning by using Community Assessment for Public Health Emergency Response (CASPER) methodology. Prehosp Disaster Med. 2014;29(3):262–269. doi: 10.1017/S1049023X14000491. [DOI] [PubMed] [Google Scholar]
- 13.Centers for Disease Control and Prevention. Public Health Preparedness Capabilities: National Standards for State and Local Planning. Available at: https://www.cdc.gov/phpr/readiness/00_docs/DSLR_capabilities_July.pdf. Accessed July 10, 2017.
- 14.US Department of Homeland Security. Homeland Security Presidential Directive 5. Available at: https://www.dhs.gov/sites/default/files/publications/Homeland%20Security%20Presidential%20Directive%205.pdf. Accessed July 10, 2017.
- 15.US Department of Homeland Security. Presidential Policy Directive/PPD-8: national preparedness. Available at: https://www.dhs.gov/presidential-policy-directive-8-national-preparedness. Accessed July 10, 2017.
- 16.White House Office of the Press Secretary. Presidential policy directive—critical infrastructure security and resilience. Available at: https://www.whitehouse.gov/the-press-office/2013/02/12/presidential-policy-directive-critical-infrastructure-security-and-resil. Accessed July 10, 2017.
- 17.US Government Publishing Office. Pandemic and All-Hazards Preparedness Act. Available at: https://www.gpo.gov/fdsys/pkg/PLAW-109publ417/pdf/PLAW-109publ417.pdf. Accessed July 10, 2017.
- 18.US Department of Health and Human Services. National Health Security Strategy (NHSS) of the United States. Available at: https://www.phe.gov/Preparedness/planning/authority/nhss/strategy/Documents/nhss-final.pdf. Accessed July 10, 2017.
- 19.Attfield KR, Dobson CB, Henn JB. Injuries and traumatic psychological exposures associated with the South Napa earthquake—California, 2014. MMWR Morb Mortal Wkly Rep. 2015;64(35):975–978. doi: 10.15585/mmwr.mm6435a4. [DOI] [PubMed] [Google Scholar]
- 20.Bayleyegn T, Wolkin A, Oberst K et al. Rapid assessment of the needs and health status in Santa Rosa and Escambia counties, Florida, after Hurricane Ivan, September 2004. Disaster Manag Response. 2006;4(1):12–18. doi: 10.1016/j.dmr.2005.10.001. [DOI] [PubMed] [Google Scholar]
- 21.World Health Organization. Effective media communication during public health emergencies: a World Health Organization handbook. Available at: http://www.who/int/csr/resources/publications/WHO%20MEDIA%20HANDBOOK.pdf. Accessed July 10, 2017.