Abstract
Objectives. To evaluate trends in funding over the past 16 years for key federal public health preparedness and response programs at the US Department of Health and Human Services, to improve understanding of federal funding history in this area, and to provide context for future resource allocation decisions for public health preparedness.
Methods. In this 2017 analysis, we examined the funding history of key federal programs critical to public health preparedness by reviewing program budget data collected for our annual examination of federal funding for biodefense and health security programs since fiscal year (FY) 2001.
Results. State and local preparedness at the Centers for Disease Control and Prevention initially received $940 million in FY2002 and resulted in significant preparedness gains, but funding levels have since decreased by 31%. Similarly, the Hospital Preparedness Program within the Office of the Assistant Secretary for Preparedness and Response was funded at a high of $515 million in FY2003, but funding was reduced by 50%. Investments in medical countermeasure development and stockpiling remained relatively stable.
Conclusions. The United States has made significant progress in preparing for disasters and advancing public health infrastructure. To enable continued advancement, federal funding commitments must be sustained.
Since 2001, the US federal government dedicated significant funding and focus toward local, state, federal, and international preparedness for public health emergencies and disasters.1,2 In the years immediately following the September 11, 2001, terrorist attacks and subsequent anthrax attacks, much of that focus was targeted at addressing terrorism—specifically, bioterrorism.3 Over time, priorities, policies, funding, and focus shifted away from terrorism and toward improving public health preparedness for many types of emergencies, as well as toward reinforcing the spectrum of preparedness activities from prevention through response and recovery.4
Overall, the increased availability of preparedness funds since 2001 strengthened public health systems, which before that time were underdeveloped.3 Public health preparedness was tested many times in the intervening years, including but not limited to the Severe Acute Respiratory Syndrome (SARS) coronavirus epidemic; Hurricanes Katrina and Sandy; the 2009 H1N1 influenza pandemic; the 2011 Joplin tornado; the 2013 Boston Marathon bombing; the 2014 West Virginia Elk River chemical spill; the Ebola epidemic and isolated cases in the United States; and the ongoing Zika virus pandemic. Today, some preparedness gains are in jeopardy because of budget reductions at both the state and the federal levels.4 Public health staff positions are being eliminated, and the United States is in danger of reversing significant progress in public health preparedness.4,5
We evaluated trends in funding over the past 16 years for key federal public health preparedness and response programs at the US Department of Health and Human Services (DHHS). The aim of this analysis is to improve understanding of federal funding history in this area and provide context for future resource allocation decisions for public health preparedness.
METHODS
To conduct this 2017 analysis, we reviewed data on program funding levels collected for our annual examination of federal funding for biodefense and health security programs.1,2 We then compared funding levels for each program for each fiscal year (FY) and reviewed changes since FY2001.
Information for this analysis was derived from our Federal Funding for Health Security and Federal Agency Biodefense Funding series, which rely on publicly available DHHS and other federal department and agency budget materials, including “Budgets in Brief” and “Congressional Justifications,” as well as personal contacts with agency representatives.1,2
RESULTS
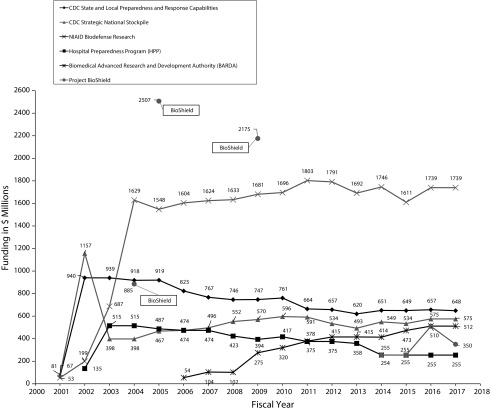
The programs discussed in this section are funded by DHHS and are critical to strengthening public health and health care infrastructure and improving US readiness to handle major public health emergencies.6 Figure 1 shows funding changes over time for these programs.
FIGURE 1—
Federal Public Health Preparedness Funding in Millions of Dollars, by Program: United States, Fiscal Years 2001–2017
Note. CDC = Centers for Disease Control and Prevention; NIAID = National Institute of Allergy and Infectious Diseases. CDC state and local public health preparedness funding includes the Public Health Preparedness and Response Program cooperative agreement grants and other state and local preparedness initiatives such as Cities Readiness Initiative. Funding for NIAID Biodefense Research in FY2010 is an estimate only. All other funding amounts for FY2001–FY2015 are actual, amounts for FY2016 are estimated, and amounts for FY2017 are budget only.
The Centers for Disease Control and Prevention (CDC) has provided significant funding to support preparedness work by health departments since FY2002.1,2 The major support for state and local program work is the Public Health Emergency Preparedness (PHEP) cooperative agreement program, which enables health departments to build and sustain information and communication systems, establish routine surveillance for infectious diseases, build knowledge and expertise in risk communication and community engagement,7 establish and exercise plans for mass dispensing, address vulnerable populations in preparedness and response, and many other gains.4 These federally funded capabilities and capacities are used regularly by health departments to respond to disasters large and small. For instance, PHEP funding enabled public health laboratories to quickly respond to testing needs for emerging infectious disease threats such as Middle East Respiratory Syndrome.8 State and local preparedness and response programs at CDC were funded initially at a high of $940 million in FY2002.2
In parallel with the PHEP program, the Hospital Preparedness Program, Office of the Assistant Secretary for Preparedness and Response, was initiated by DHHS in FY2002 and was funded at a high of $515 million in FY2003.2 Gains from that program since its inception include routinized planning, training, and exercises at hospitals; planning for health care system surge; hiring of hospital preparedness coordinators; and establishing health care coalitions around the United States, which bring together public health and health care to enable coordinated response, among other gains.4,9 Health care preparedness funding also supported the response to several crises, including evacuation planning for hurricanes and establishing high-containment isolation units used to treat highly infectious or lethal diseases such as pandemic influenza or Ebola.4
Yet, although funding for public health and health care preparedness enabled the progress mentioned earlier, funding for these programs has not been level over time.1,2 Since the funding highs in FY2002 and FY2003 for the PHEP and Hospital Preparedness Program, these programs have experienced cumulatively decreased budgets by 31% and 50%, respectively.1,2
Important investments in research, development, and stockpiling of medical countermeasures for use in chemical, biological, radiological, and nuclear emergencies and other disasters are also noteworthy. Since FY2004, the National Institute of Allergy and Infectious Diseases provided between $1.6 and $1.8 billion per year in basic and applied research, which supports development of medical countermeasures.1,2 In addition, Project BioShield and the related Biomedical Advanced Research and Development Authority, Office of the Assistant Secretary for Preparedness and Response, bridged the gap from basic and applied research to drug development and procurement.10 Finally, funding for CDC’s Strategic National Stockpile resulted in stocks of drugs, vaccines, and medical supplies that can quickly be deployed around the United States in response to many types of emergencies.8 Investment in the medical countermeasures enterprise in the United States has realized benefits beyond stockpiling. For example, it enabled the rapid testing and scale up of drugs and vaccines for Ebola, which would not have been developed without prolonged federal commitment to preparedness.11
Funding for the National Institute of Allergy and Infectious Diseases, Biomedical Advanced Research and Development Authority, and Strategic National Stockpile remained relatively steady over time, but funding and responsibility for Project BioShield changed dramatically since its establishment.1,2 The original Project BioShield appropriation was made to the US Department of Homeland Security in the form of a 10-year Special Reserve Fund of $5.6 billion.2 The Department of Homeland Security was then responsible for making funds from the Special Reserve Fund available to the Secretary of Health and Human Services for medical countermeasures procurement following approval by the federal interagency and the White House. This fund was intended to provide a guaranteed market for companies in the final research and development, regulatory, and manufacturing phases over multiple years.10 However, in FY2014, Project BioShield responsibility was shifted from the Department of Homeland Security to the Biomedical Advanced Research and Development Authority within DHHS, and appropriations were moved to an annual cycle at a reduced level.1 With these changes, Project BioShield funding over multiple years is no longer a guarantee for biotechnology and pharmaceutical industry partners and may result in reduced interest and investment.
DISCUSSION
The events of 2001 catalyzed a surge of federal funding and programs focused on preparing public health at the state, territorial, tribal, and local levels to prevent, respond to, and recover from manmade and natural disasters.1,3,5 Prior to this funding and focused prioritization on emergency preparedness, health departments were underdeveloped and had a limited role in this area.3 Health departments had few plans in place to respond to epidemics and disasters, very little capability to vaccinate or dispense medical countermeasures emergently, little in the way of health system surge capacity or planning for mass casualties, and limited research and development to develop new medical countermeasures and stockpile them for the United States.3 In addition, many health departments in 2001 lacked even basic organizational capacities, including information systems to enable routine health data collection.12
With current targeted investment in building public health preparedness for more than a decade, the United States has made enormous progress not only in preparing for disasters but also in shoring up and advancing public health infrastructure more generally.5
PUBLIC HEALTH IMPLICATIONS
Without public health preparedness funding, many public health gains would not be realized.4,5 To enable continued advancement in the future, it is critical that federal funding commitments to public health preparedness programs are sustained.
HUMAN PARTICIPANT PROTECTION
Human participant protection was not required because no human subjects were involved in this budget review.
REFERENCES
- 1.Boddie C, Watson M, Sell TK. Federal funding for health security in FY2017. Health Secur. 2016;14(5):284–304. doi: 10.1089/hs.2016.0063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Franco C, Sell TK. Federal agency biodefense funding, FY2010-FY2011. Biosecur Bioterror. 2010;8(2):129–149. doi: 10.1089/bsp.2010.0013. [DOI] [PubMed] [Google Scholar]
- 3.Trust for America’s Health. Ready or Not? Protecting the Public’s Health in the Age of Bioterrorism. December 2003. Available at: http://healthyamericans.org/reports/bioterror03. Accessed February 1, 2017. [DOI] [PubMed]
- 4.Trust for America’s Health. Ready or Not? Protecting the Public From Diseases, Disasters, and Bioterrorism. December 2016. Available at: http://healthyamericans.org/reports/readyornot2016. Accessed February 1, 2017. [DOI] [PubMed]
- 5.Marquez M, Patel P, Raphael M, Morgenthau BM. The danger of declining funds: public health preparedness in NYC. Biosecur Bioterror. 2009;7(3):337–345. doi: 10.1089/bsp.2009.0048. [DOI] [PubMed] [Google Scholar]
- 6.Khan AS. Public health preparedness and response in the USA since 9/11: a national health security imperative. Lancet. 2011;378(9794):953–956. doi: 10.1016/S0140-6736(11)61263-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Schoch-Spana M, Selck FW, Goldberg LA. A national survey on health department capacity for community engagement in emergency preparedness. J Public Health Manag Pract. 2015;21(2):196–207. doi: 10.1097/PHH.0000000000000110. [DOI] [PubMed] [Google Scholar]
- 8.Centers for Disease Control and Prevention. Public Health Preparedness: 2016 National Snapshot. 2016. Available at: https://www.cdc.gov/phpr/pubs-links/2016/documents/2016_Preparedness_Report.pdf. Accessed February 1, 2017.
- 9.Toner E, Waldhorn R, Franco C Hospitals Rising to the Challenge: The First Five Years of the U.S. Hospital Preparedness Program and Priorities Going Forward. March 2009. Available at: http://www.upmchealthsecurity.org/our-work/pubs_archive/pubs-pdfs/2009/2009-04-16-hppreport.pdf. Accessed February 1, 2017.
- 10.Russell PK. Project BioShield: what it is, why it is needed, and its accomplishments so far. Clin Infect Dis. 2007;45(suppl 1):S68–S72. doi: 10.1086/518151. [DOI] [PubMed] [Google Scholar]
- 11.Boddie C. Federal funding in support of Ebola medical countermeasures R&D. Health Secur. 2015;13(1):3–8. doi: 10.1089/hs.2015.0001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Marmagas SW, King LR, Chuk MG. Public health’s response to a changed world: September 11, biological terrorism, and the development of an environmental health tracking network. Am J Public Health. 2003;93(8):1226–1230. doi: 10.2105/ajph.93.8.1226. [DOI] [PMC free article] [PubMed] [Google Scholar]