Abstract
Purpose
The aim of this study was to evaluate an intervention designed to assist after school programs (ASPs) in meeting snack nutrition policies that specify that a fruit or vegetable (FV) be served daily, and sugar-sweetened beverages/foods and artificially flavored foods eliminated.
Design
One-year group randomized controlled trial
Setting
Afterschool programs operating in South Carolina, US.
Subjects
Twenty ASPs serving over 1,700 children were recruited, match-paired post-baseline on enrollment size and days FV were served/week (days/wk), and randomized to either an intervention (n=10) or control (n=10) groups.
Intervention
Strategies To Enhance Practice for Healthy Eating (STEPs-HE), a multi-step adaptive intervention framework, which assists ASP leaders and staff to serve snacks that meet nutrition policies while maintaining cost.
Measures
Direct observation of snacks served and consumed, and monthly snack expenditures via receipts.
Analysis
Nonparametric and mixed-model repeated-measures
Results
By post-assessment, intervention ASPs increased serving FV to 3.9±2.1 vs. 0.7±1.7days/wk and decreased serving sugar-sweetened beverages to 0.1±0.7 vs. 1.8±2.4days/wk and foods to 0.3±1.1 vs. 2.7±2.5days/wk compared to controls, respectively. Cost of snacks increased by $0.02/snack in the intervention ASPs ($0.36 to $0.38) compared to a $0.01/snack decrease in the control ($0.39 to $0.38). Across both assessments and groups 80–100% of children consumed FV.
Conclusions
The STEPs-HE intervention can assist ASPs in meeting nationally endorsed nutrition policies with marginal increases in cost.
Keywords: Nutrition, Community-based Programs, Children, School, Food
Introduction
Across the nation, afterschool programs (Mon–Fri 3–6pm, ASPs) have been called upon to improve the nutritional quality of the snacks served to the millions of children (5–12yrs) attending each day of the school year.1,2 Over the past several years, the largest providers of ASPs in the nation have adopted policies/standards for the types of foods and beverages ASP providers should serve to children enrolled in their programs.1,2 These policies/standards, called the Healthy Eating Standards, call for ASPs to serve a fruit or vegetable every day, eliminate sugar-based foods and beverages, as well as, eliminate foods that are artificially flavored (see naaweb.org). While these standards represent important public health guidelines that can lead to marked improvements in children’s daily consumption of fruits and vegetables, ASPs struggle to achieve them.3–7
Snacks typically served in ASPs are high in sugar (e.g., cookies, powdered drink mixes), salt and artificial flavoring (e.g., nacho cheese flavored tortilla chips), with little to no fruits or vegetables.4–6,8,9 Such snacks often are lower in cost,7 have longer shelf-life, and therefore meet the limited snack budget (<$0.40 per snack/child/day) many ASPs allocated for snack expenditures.10 Interventions addressing snack quality through policy changes have resulted in improvements in the number of days per week fruits/vegetables are served and have reduced the serving of less healthful snacks and beverages.4,5,9 Policy-level approaches, however, have failed to address snack expenses, which is noted as a primary barrier to serving snacks that meet the Healthy Eating Standards.3,10–12
One promising approach may be with assisting ASPs to identify low cost outlets to purchase foods for snack that meet the Healthy Eating Standards, such as grocery stores or bulk warehouse chains.3,12 In addition, many ASPs do not formally plan weekly or monthly snack menus and are often unaware of the amount they currently spend on snacks, which creates difficulties in knowing what snacks will be served and how much a program can allocate for snack expenditures for each child and whether more costly snacks,7 such as fruits or vegetables, are within budget.7,10,11 Thus, working with ASPs to build capacity to establish a snack budget, menu, and identifying outlets to purchase foods that meet the Healthy Eating Standards at a price within their proposed budget, can assist ASPs leaders and staff in meeting these important public health goals. The purpose of this study was to evaluate the effectiveness of a multi-step adaptive intervention framework called Strategies To Enhance Practice for Healthy Eating (STEPs-HE)13 that assists ASP leaders and staff to serve snacks that meet the HE Standards. The primary outcomes were changes in the types of snacks served and the associated cost of these snacks. A secondary outcome was whether children consumed the snacks served. The information presented represents only the healthy eating outcomes from a healthy eating and physical activity focused intervention in afterschool programs.14
Methods
Participants, Setting, and Design
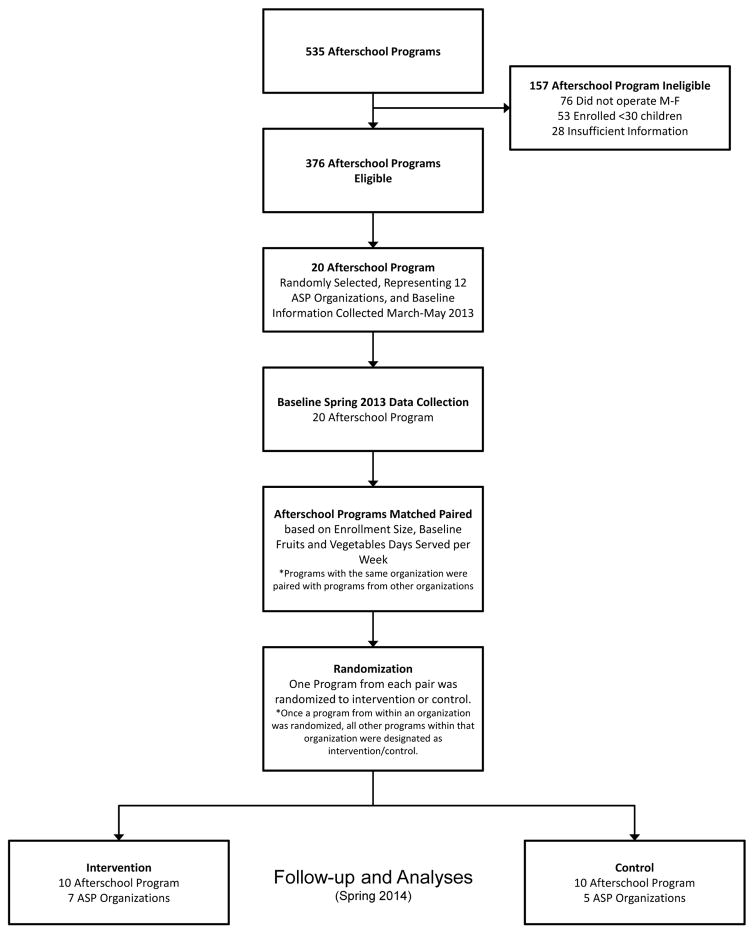
For this study, ASPs were defined as child care programs operating immediately after the school day, every day of the school year for a minimum of 2 hours. Programs had to serve a minimum of 30 children of elementary age (6–12yrs) and could operate in a school, community, or faith setting. Programs had to provide a snack, homework assistance/completion time, enrichment, and opportunities for physical activity to participate in this study.15 Programs that were singularly focused (e.g., dance, tutoring) and/or physical activity focused (e.g., sports, activity clubs), were not eligible for participation. All children enrolled, staff, and ASP leaders in the ASPs were eligible to participate in the study. A total of twenty afterschool programs, representing 13 different organizations were randomly selected from programs meeting eligibility criteria from an existing registry of 535 ASPs in South Carolina and invited to participate in an intervention targeting healthy eating and physical activity – Making Healthy Eating and Physical Activity Policy Practice.14 Of the 535 programs, 376 met the eligibility criteria – 76 did not operate Mon–Fri, 53 enrolled fewer than 30 children, and 28 did not have sufficient information to evaluate eligibility. Program eligibility consisted of operating within 1.5hr drive from the university and classification as an ASP as defined above. Across the 20 ASPs, mean enrollment was 88 children (range 30 to 162). Five programs received federal or state reimbursement for snacks. All study procedures were approved by the Institutional Review Board of the lead author at the University of South Carolina.
Randomization
The design was group randomized controlled trial. The twenty ASPs were randomized into one of two conditions: 1) intervention or 2) control group. Randomization to intervention vs. control groups was performed after baseline data collection, during June 2013 (see Figure 1). Programs were match-paired based on enrollment size, and average number of days per week a fruit or vegetable was served. In order to minimize contamination, ASPs within the same organization were matched with ASPs from other organizations and were all randomized to the same condition. Once an ASP from within an organization was randomized to the intervention or control group, all other ASPs from this organization were also designated to this group. Enrollment size was selected as a matching variable to assure comparable group composition on a marker of organizational complexity (e.g., an ASP of 30 children is less complex than an ASP serving >150 children/day). Fruit and vegetable servings were identified as pertinent matching variables because they were the primary outcomes of interest. Randomization was conducted by study staff using a random number generator. Baseline characteristics for intervention and control ASPs are presented in Table 1. The control group was asked to continue with current ASP practices and received no technical assistance or support from the intervention staff.
Figure 1.
Participant flow chart for recruitment, data collection, and analyses.
Table 1.
Baseline (spring 2013) characteristics of afterschool programs and children enrolled by treatment condition
| Control (n = 10) | Intervention (n = 10) | P difference b | |
|---|---|---|---|
|
|
|
|
|
| Afterschool Program Characteristics | |||
| Total Kids Enrolled | 870 | 895 | |
| Average Enrollment (M, SD) | 87.0 ±47.8 | 89.5 ±52.0 | .961 |
| Daily Program Length (minutes per day, M, SD) | 205.5 ±134.3 | 190.5 ±128.7 | .303 |
| Reimbursement for Snack (n) | 1 | 4 | |
| Percentage of Population in Poverty, Census 2010 | 17.5 ±10.2% | 13.3 ±15.6% | .089 |
| Location (n) | |||
| School | 6 | 3 | |
| Faith/church | 1 | 3 | |
| Community (e.g., recreation center) | 3 | 4 | |
| Food Preparation and Storage (n) | |||
| Refrigerator and freezer combination unit | 7 | 10 | 0.210 |
| Standalone freezer | 3 | 2 | 0.900 |
| Pantry or storage closet for dry goods | 9 | 9 | 1.000 |
| Portable cooler/ice chest | 7 | 6 | 0.900 |
| Kitchen | 5 | 6 | 0.900 |
| Food preparation sink that is not in a bathroom | 4 | 9 | 0.029 |
| Stove/oven | 4 | 5 | 0.900 |
| Microwave | 9 | 10 | 0.900 |
| Serving plates or bowls | 9 | 10 | 0.900 |
| Child Characteristics | |||
| Boys (%) | 52.4 | 53.3 | |
| Age (years, M, SD) | 8.1 ±1.8 | 7.9 ±1.8 | .394 |
| Race/Ethnicity (%) | <.001 | ||
| White non-Hispanic | 48.4 | 64.6 | |
| African American | 44.7 | 29.7 | |
| Other | 6.9 | 5.7 | |
P-value for comparison between intervention and control at baseline.
Continuous variables at the ASP-level compared using two-sample t-tests; categorical variables compared using χ2 tests or Fisher Exact Test for small sample size (N = 20)
Intervention - Strategies To Enhance Practice for Healthy Eating (STEPs-HE)
A detailed description of the STEPs-HE can be found elsewhere.13 In brief, the STEPs-HE conceptual framework involves a multi-step, adaptive approach to incorporating healthy eating strategies into daily routine practice. The approach consists of identifying essential ASP characteristics that represent fundamental building blocks that function as necessary programmatic components to achieving full integration of healthy eating strategies and eventual achievement of the Healthy Eating Standards. The Standards indicate that, on a daily basis the ASP: 1) serves a fruit or vegetable; 2) offers water at the table and has water accessible at all times; 3) serves no candy or other foods that are primarily sugar-based; 4) serves no beverages that are primarily sugar-based; and 5) avoids foods and beverages made with artificial ingredients (sweeteners, flavors, or colors).
The STEPs-HE approach departs from traditional intervention models that are based on a pre-defined package of intervention components all provided identically to those individuals or settings allocated to a treatment condition.16 The STEPs-HE recognizes that each ASP is unique and, therefore, will require some similar and some different resources/strategies to achieve the Healthy Eating Standards (i.e., there is no “one size fits all” intervention). The approach taken in STEPs-HE is one where some degree of local site-level tailoring will occur that is both responsive and adaptive to the characteristics of each ASP.17 This assists with the local relevancy of the healthy eating strategies, and subsequent uptake/integration of them within daily practice. STEPs-HE is designed so that any one ASP can enter anywhere along the continuum, with the understanding that some ASPs will enter at a lower level indicating the need for greater technical assistance to achieve the Healthy Eating Standards versus those programs that enter at a higher level. STEPs-HE was informed from a systems framework for translating childhood obesity policies into practice in ASPs,18 the principles of community-based participatory research,19 the theory of human motivation,20 nonspecific hypothesis in psychotherapy,21,22 and adaptive interventions.23
The STEPs-HE13 begins by focusing on the program leader as the primary target of the process of integrating the Healthy Eating Standards into routine practice. The first steps of the healthy eating strategies begin with (1) the identification and/or development of a schedule/menu of daily/weekly snack offerings and following the menu, and (2) the budgeted amount for snacks (either daily cost per snack per child per day or annual budget) and the location(s) where snacks are purchased. These items are consistent with requirements outlined by the USDA to receive federal reimbursement for snacks.24 For ASPs without these items, technical assistance provided by research staff focused on developing a 2 or 4 week rotating snack menu that clearly defines the snacks to be served and their respective serving size, as well as, working with ASP leaders to determine challenges associated with serving the menu-specified snacks. For ASPs without knowledge of snack expenditures, monthly snack purchase receipts were collected and subsequent computation of monthly and per snack/child/day costs were performed. Where ASPs were identified as having a limited budget and/or were purchasing snacks from retailers where the retail cost of snacks that meet the Healthy Eating Standards was prohibitive, support was provided to identify grocery stores located conveniently to the ASPs where snack purchases could be made that fit within existing budgets. Alternative locations were first identified via Google Maps based on the ASPs address and/or based on what the ASP leader indicated was conveniently located near the program. Secondly, the locations were visited, either by the investigative team or ASP leader, to determine if the prices met the ASPs designated snack budget. Based on this information, an ASP could have selected one or more alternative outlets, at their discretion, to begin purchasing snacks.
Trainings, conducted by research staff, occurred at the beginning of the school year (August 2013) and lasted approximately 3 hours with the site leaders. Additionally, 4 booster sessions per intervention ASP, that include site leaders and staff, were provided. Booster sessions included a walkthrough with the program site leader to review opportunities to meet the Healthy Eating Standards. For the boosters, research personnel, site leaders and staff convened a 20 to 30 minute meeting immediately after the end of the ASP to discuss areas that were consistent and inconsistent with meeting the Healthy Eating Standards. Strategies to address challenges were agreed upon and implemented in subsequent days.
Measures
All measurements occurred during the spring 2013 (March–April), Fall (September–November 2013), and post-intervention spring 2013 (March–April). Data were collected at mid-point to identify the length of time required to alter snacks to meet the Health Eating Standards. Consistent with previously established protocols, each ASP was visited for data collection on 4 non-consecutive, unannounced days Monday through Thursday at each measurement occasion.25–28 Evaluation of the Health Eating Standards (see above) was operationalized as the following: fruit or vegetable served every day; 2) water served to children during snack; no sugar-sweetened candy, desserts (e.g., cookies, pop tarts) or beverages (e.g., chocolate milk, powdered drink mixes) served; and 3) no foods made with artificial flavors (e.g., sour cream and onion potato chips) or colors (e.g., Trix cereal). At the beginning and end of each measurement wave, the food preparation and storage amenities were collected via self-report from the ASP site leaders. Each site leader was asked to indicate access to locations to store foods and beverages (e.g., refrigerator, pantry) and wash and prepare foods (e.g., sinks not located in bathrooms, kitchens).
Snack Classification
The types of foods and beverages served as snack were recorded via direct observation by trained research personnel. Each ASP was visited on 4 non-consecutive unannounced days between March and April 2013. Immediately at the start of snack, the trained observer recorded the brand name(s), size, and packaging, where appropriate, of the foods and beverages served as snack for that day. Foods and beverage items served as snacks were classified according to existing categories for snacks and beverages:1,29 sugar-sweetened beverages (e.g., soda, powered drink mixed, sport drinks), dairy food unsweetened (e.g., string cheese); dairy food sweetened (e.g., Trix yogurt); milk unsweetened (non-fat, 1%, 2%, and whole); milk sweetened (e.g., chocolate, strawberry); 100% fruit juice; salty flavored snacks (e.g., Doritos, Chex Mix), salty unflavored snacks (e.g., pretzels, plain corn tortilla chips); desserts (e.g., cookies, pop tarts); candy (e.g., chocolate, frozen treats); non-fruit fruit (e.g., fruit roll ups; fruit leather); prepackaged fruit (e.g., applesauce, fruit in syrup); cereal sugar-sweetened (e.g., Fruit Loops); cereal unsweetened (e.g., Cheerios); and fruits and vegetables (e.g., fresh, frozen, dried) recorded separately. Water was recorded if programs provided water in cups or bottles during snack time. Inter-rater agreement on the snacks served was 98.4% (kappa 0.98) across 133 reliability observations of snacks.
Consumption of Snacks
Consumption of snacks was collected using a modified direct observation protocol during baseline and post-assessment.30,31 At the beginning of snack, a trained research staff member positioned themselves next to the point of snack distribution. Subsequently, the observer waited for the first group of 5 or more children with a mixture of boys and girls to form at the designated seating areas (e.g., cafeteria tables, sitting on ground outside). Within this group, the observer selected 5 children and observed them for the entire duration of the snack time (approximately 15mins). No more than five children were selected due to the inability to directly observe more than this. During snack time, a single observer recorded what the children were served for snack and indicated whether each child consumed the snack. Consumption was operationalized as observing a child eating 50% or more of an offered snack item.12 For instance, if children were provided a whole piece of fruit, a child would be classified as consuming the fruit if researchers observed that the child had eaten at least half of the fruit. Where children did not eat any of the snack or only took several bites, consumption was recorded as zero (i.e., not consumed). Inter-rater agreement for consumption was 97% (κ= 0.88) based on 835 reliability observations of snack consumption.
Costs of Snacks
Costs of the snacks were estimated based on weekly receipts provided by ASPs from March 1st to June 1st 2013 (baseline) and during 4 weeks each for October 2013, and February and April 2014. For each individual food and beverage item, cost per serving was determined using standard serving sizes.1
Analysis
For the comparison of the number of days snacks and beverages were served in a week between the treatment and control ASPs, a series of nonparametric intent-to-treat models were estimated. This modeling approach was used to account for non-normal distributions in the snack and beverage categories at either baseline or post-assessment. At baseline and post-assessments, separately, comparisons between intervention and control ASPs across snack and beverage categories were evaluated using the Wilcoxon signed-rank test. Within group changes from baseline (spring 2013) to final post-assessment (spring 2014) across snack and beverage categories for intervention and control ASPs, separately, were evaluated using the Wilcoxon matched-pair test. Additionally, mixed effects logistic regression models, with observation days nested within ASPs, were estimated to evaluate the odds of observing a snack or beverage category being served on a given day. These models included the following covariates: Census 2010 zip code poverty level, enrollment size, and operating location of the program (community and faith vs. school). For child consumption of snacks, descriptive means of the percentage of children observed consuming 50% or more of fruits and vegetables are reported. The cost of snacks and beverages were computed for each snack/beverage category for treatment and control ASPs at baseline and post-assessment. Finally, the number of ASPs meeting the Healthy Eating Standards was evaluated by classifying whether ASPs met the standards every day. The matched-pairs were not included in the analyses given the small number of pairs.32,33 The criteria for a statistically significant difference between groups was set a priori at P < .05. All analyses were performed using Stata (v.13.0., College Station, TX).
Results
Comparison between control and intervention ASPs characteristics at baseline are presented in Table 1. Apart from race/ethnicity, with control ASPs serving a greater percentage of African Americans, and receipt of federal reimbursement for snack in the intervention ASPs, the two groups were equivalent. The number of days foods and beverages were served per week are presented in Table 2. At baseline, intervention ASPs served more salty unflavored snacks per week compared to control ASPs. The two groups were comparable on all other foods and beverages served at baseline. There were no changes in the controls ASPs in the snacks or beverages served at baseline to post-assessment. Conversely, intervention ASPs increased the number of days/wk fruits, vegetables, and fruits/vegetables were served and decreased the number of days/wk desserts and sugar-sweetened cereal were served. Additionally, all interventions ASPs eliminated non-dairy sugar-sweetened beverages by post-assessment. At post-assessment, intervention ASPs were serving more fruits, vegetables, and salty-unflavored snacks, and fewer desserts, sugar-sweetened cereals and beverages, and less 100% fruit juice compared to control ASPs. Results from the logit models indicated fruit was 12 times more likely and water 10 times more likely to be observed in intervention compared to control ASPs (see Table 2). Conversely, desserts and total sugar-sweetened beverages were less likely to be observed in intervention versus control ASPs. None of the covariates significantly impacted the model estimates.
Table 2.
Snacks and beverages served at baseline (spring 2013) and post-assessment (spring 2014) for intervention and control ASPs.
| Snack Food/Beverage Category | Control (n = 10) | Intervention (n = 10) | Between Group Comparison | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|||||||||||||||||||
| Baseline Spring 2013 |
Fall 2013 |
Post-Assessment Spring 2014 |
Within group b |
Baseline Spring 2013 |
Fall 2013 |
Post-Assessment Spring 2014 |
Within group b |
Nonparametric | Logistic Regressionc | ||||||||||||
|
|
|
|
|
|
|
||||||||||||||||
| (n = 41)a | (n = 44)a | (n = 44)a | (n = 43) a | (n = 56) a | (n = 56) a | Baseline | Post Assessment c |
||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
||||||||||||
| M | (SD) | M | (SD) | M | (SD) | Δ | P | M | (SD) | M | (SD) | M | (SD) | Δ | P | P | P | OR | (95CI) | ||
| Foods (number of days served per week) | |||||||||||||||||||||
| Fruits (e.g., fresh, frozen, dried) | 0.6 | (1.7) | 0.7 | (1.7) | 0.5 | (1.5) | −0.2 | 0.487 | 0.6 | (1.6) | 3.8 | (2.1) | 3.6 | (2.3) | 3.0 | 0.006 | 0.720 | <0.001 | 12.05 | (2.05, | 71.00) |
|
| |||||||||||||||||||||
| Vegetables (e.g., baby carrots, celery) | 0.1 | (0.8) | 0.1 | (0.8) | 0.2 | (1.1) | 0.1 | 0.317 | 0.0 | (0.0) | 0.9 | (1.9) | 1.6 | (2.4) | 1.6 | 0.011 | 0.317 | 0.010 | 7.58 | (0.25, | 225.50) |
|
| |||||||||||||||||||||
| Total fruits and vegetables | 0.7 | (1.8) | 0.8 | (1.8) | 0.7 | (1.7) | 0.0 | 0.521 | 0.6 | (1.6) | 4.0 | (2.0) | 3.9 | (2.1) | 3.3 | 0.006 | 0.461 | <0.001 | 14.23 | (2.52, | 80.35) |
|
| |||||||||||||||||||||
| Dips (e.g., peanut butter, ranch dressing) | 0.2 | (1.1) | 0.2 | (1.1) | 0.0 | (0.0) | −0.2 | 0.157 | 0.7 | (1.8) | 1.2 | (2.1) | 2.2 | (2.5) | 1.5 | 0.007 | 0.260 | <0.001 | - - - | - - - | - - - |
|
| |||||||||||||||||||||
| Dairy - unsweetened (e.g., cheese) | 0.6 | (1.7) | 0.2 | (1.1) | 0.5 | (1.5) | −0.2 | 0.413 | 0.7 | (1.8) | 1.0 | (2.0) | 0.7 | (1.8) | 0.0 | 0.782 | 0.863 | 0.284 | 2.01 | (0.27, | 15.20) |
|
| |||||||||||||||||||||
| Dairy - sweetened (e.g., Trix yogurt) | 0.2 | (1.1) | 0.0 | (0.0) | 0.0 | (0.0) | −0.2 | 0.157 | 0.0 | (0.0) | 0.0 | (0.0) | 0.0 | (0.0) | 0.0 | - - - | 0.146 | - - - | - - - | - - - | - - - |
|
| |||||||||||||||||||||
| Salty snacks – flavored (e.g., Doritos, Chex Mix, Cheddar Goldfish) | 1.6 | (2.4) | 1.7 | (2.4) | 1.6 | (2.4) | 0.0 | 0.714 | 2.7 | (2.5) | 1.3 | (2.2) | 1.3 | (2.2) | −1.4 | 0.147 | 0.164 | 0.667 | 0.35 | (0.10, | 1.25) |
|
| |||||||||||||||||||||
| Salty snacks – unflavored (e.g., pretzels, crackers, tortilla chips) | 0.6 | (1.7) | 0.1 | (0.8) | 0.3 | (1.3) | −0.3 | 0.912 | 2.0 | (2.5) | 1.7 | (2.4) | 1.6 | (2.4) | −0.4 | 0.918 | 0.042 | 0.011 | 2.76 | (0.44, | 17.45) |
|
| |||||||||||||||||||||
| Desserts (e.g., cookies, muffins, snack cakes, cereal bars, pop tarts) | 2.6 | (2.5) | 2.6 | (2.5) | 2.7 | (2.5) | 0.2 | 0.529 | 2.9 | (2.5) | 0.2 | (0.9) | 0.3 | (1.1) | −2.6 | 0.013 | 0.293 | 0.002 | 0.03 | (0.01, | 0.16) |
|
| |||||||||||||||||||||
| Cereal – sugar-sweetened (e.g., Fruit Loops) | 0.9 | (1.9) | 0.3 | (1.3) | 0.8 | (1.8) | −0.1 | 0.654 | 0.9 | (2.0) | 0.0 | (0.0) | 0.0 | (0.0) | −0.9 | - - - | 0.738 | - - - | - - - | - - - | - - - |
|
| |||||||||||||||||||||
| Cereal – unsweetened (e.g., Cheerios) | 0.1 | (0.8) | 0.1 | (0.8) | 0.6 | (1.6) | 0.4 | 0.084 | 0.1 | (0.8) | 0.2 | (0.9) | 0.8 | (1.9) | 0.7 | 0.482 | 1.000 | 0.804 | 0.51 | (0.02, | 11.75) |
|
| |||||||||||||||||||||
| Beverages (number of days served per week) | |||||||||||||||||||||
| Sugar-sweetened non-dairy beverages (e.g., non-100% juices, powdered drink mixes, punch) | 1.2 | (2.2) | 1.7 | (2.4) | 1.4 | (2.3) | 0.2 | 1.000 | 3.2 | (2.4) | 0.3 | (1.1) | 0.0 | (0.0) | −3.2 | - - - | 0.107 | - - - | - - - | - - - | - - - |
|
| |||||||||||||||||||||
| Milk – sugar-sweetened (e.g., chocolate, strawberry) | 0.5 | (1.6) | 0.0 | (0.0) | 0.8 | (1.8) | 0.2 | 0.907 | 0.0 | (0.0) | 0.0 | (0.0) | 0.2 | (0.9) | 0.2 | --- | --- | 0.503 | - - - | - - - | - - - |
|
| |||||||||||||||||||||
| Non-100% Fruit Juice | 0.0 | (0.0) | 0.0 | (0.0) | 0.5 | (1.5) | 0.5 | - - - | 0.0 | (0.0) | 0.0 | (0.0) | 0.0 | (0.0) | 0.0 | - - - | - - - | - - - | - - - | - - - | - - - |
|
| |||||||||||||||||||||
| Total Sugar-sweetened Beverages | 1.5 | (2.3) | 1.6 | (2.4) | 1.8 | (2.4) | 0.4 | 0.221 | 2.4 | (2.5) | 0.2 | (0.9) | 0.1 | (0.7) | −2.4 | 0.017 | 0.230 | 0.005 | 0.01 | (0.00, | 0.11) |
|
| |||||||||||||||||||||
| 100% Fruit Juice | 1.6 | (2.4) | 1.8 | (2.4) | 2.0 | (2.5) | 0.4 | 0.395 | 0.3 | (1.2) | 0.0 | (0.0) | 0.2 | (0.9) | −0.1 | 0.317 | 0.112 | 0.018 | - - - | - - - | - - - |
|
| |||||||||||||||||||||
| Water | 2.1 | (2.5) | 2.1 | (2.5) | 2.3 | (2.5) | 0.2 | 1.000 | 2.0 | (2.5) | 5.0 | (0.0) | 3.8 | (2.2) | 1.9 | 0.257 | 0.612 | 0.969 | 10.90 | (1.27, | 93.56) |
|
| |||||||||||||||||||||
| Milk – unflavored (e.g., skim, 2%) | 0.7 | (1.7) | 0.4 | (1.3) | 0.3 | (1.2) | −0.4 | 0.158 | 0.9 | (2.0) | 0.1 | (0.8) | 1.5 | (2.3) | 0.6 | 0.620 | 0.687 | 0.425 | - - - | - - - | - - - |
Abbreviations: P = p-value, M = mean, SD = standard deviation;
Number of days snacks and beverages were observed – NOTE the difference in number of days observed was because of additional site visits due to inclement weather days where snack was served, yet other programming was substantially altered that precluded assessment of physical activity (outcomes not reported in this manuscript) ;
Within group change from spring 2013 to spring 2014 using nonparametric models;
comparison between baseline spring 2013 and final post assessment spring 2014 – models adjusted for covariates;
“- - - “ indicates models were unable to be estimated due to zero observations; BOLDED values are significant at p < .05
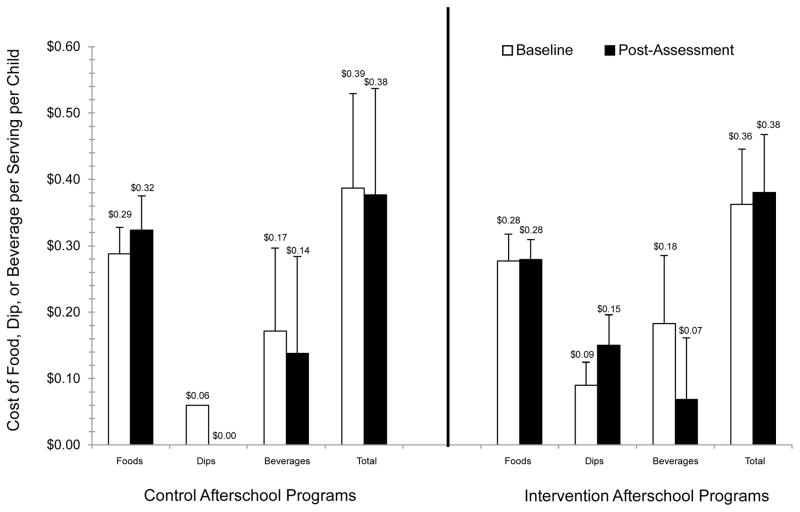
By post-assessment, intervention ASPs improved in each Healthy Eating Standard, with 4 ASPs serving FV daily, 9 offering water during snack, 8 serving no sugar-sweetened foods and 9 not serving sugar-sweetened beverages, and 3 not serving artificially flavored foods. This is in contrast to control ASPs where 0 served FV daily, 2 served water during snack, 1 serving no sugar-sweetened foods and 3 not serving sugar-sweetened beverages, and only 2 not serving artificially flavored foods. The costs of individual snack food and beverage categories based on the receipts provided by the ASPs are presented in Table 3 and Figure 2. Snack per child per day expenditures at baseline for the control ASPs were, on average, $0.39 (includes food, dip, beverage), with average food, dip, and beverage cost of $0.29, $0.06, and $0.17, respectively. Intervention ASPs, at baseline, were spending $0.36 per snack per child per day (includes food, dip, and beverage), with average food, dip, and beverage cost of $0.28, $0.09, and $0.18, respectively. At post-assessment, snack per child per day expenditures for control ASPs decreased to $0.38 ($0.32 for food, $0.00 for dips, and $0.14 for beverages), while intervention ASPs snack per child per day increased to $0.38 ($0.28 for food, $0.15 for dips, and $0.07 for beverage). For an ASP serving snack to an average of 88 children each day (average enrollment of the ASPs in this study), the $0.02 increase in snack cost translates into an additional $316.80 across a 180 day school year. Finally, across all snack categories at baseline for both intervention and control ASPs, children on average were observed consuming >90% of the snacks (range 66.7% salty-unflavored snacks to 100% fruits, vegetables, dairy, and cereal unsweetened). At post-assessment, similar consumption patterns were observed, with on average >88% of the children observed consuming the snacks served (range 66.7% dairy sugar-sweetened to 100% dairy unsweetened, cereal unsweetened, and salty-flavored snacks). Importantly, at both time points, >90% of intervention and control children were observed consuming the fruit served and >80% observed consuming the vegetables served.
Table 3.
Estimated cost of snacks and beverages based on monthly receipts provided by afterschool program leaders at baseline (spring 2013) and post-assessment (spring 2014)
| Snack Food/Beverage Category | Control ASPs | Intervention ASPs | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||||||
| Spring 2013 | Spring 2014 | Spring 2013 | Spring 2014 | |||||||||
|
|
|
|
|
|||||||||
| n | M | (SD) | n | M | (SD) | n | M | (SD) | n | M | (SD) | |
| Foods (price per serving per day) | ||||||||||||
| Fruits | 36 | $0.42 | ($0.23) | 11 | $0.39 | ($0.17) | 28 | $0.30 | ($0.16) | 96 | $0.32 | ($0.17) |
|
| ||||||||||||
| Apples | 10 | $0.56 | ($0.08) | 5 | $0.46 | ($0.10) | 11 | $0.45 | ($0.14) | 25 | $0.44 | ($0.12) |
|
| ||||||||||||
| Grapes | 2 | $0.46 | ($0.01) | 1 | $0.46 | 18 | $0.36 | ($0.14) | ||||
|
| ||||||||||||
| Bananas | 8 | $0.12 | ($0.00) | 2 | $0.16 | ($0.05) | 7 | $0.16 | ($0.03) | 11 | $0.11 | ($0.02) |
|
| ||||||||||||
| Vegetables | 13 | $0.37 | ($0.21) | 2 | $0.23 | ($0.10) | 14 | $0.24 | ($0.19) | 47 | $0.22 | ($0.09) |
|
| ||||||||||||
| Carrots | 7 | $0.26 | ($0.18) | 1 | $0.30 | 2 | $0.26 | ($0.03) | 14 | $0.25 | ($0.06) | |
|
| ||||||||||||
| Celery | 15 | $0.15 | ($0.08) | |||||||||
|
| ||||||||||||
| Cucumbers | 6 | $0.22 | ($0.07) | |||||||||
|
| ||||||||||||
| Dips | 9 | $0.06 | ($0.05) | 3 | $0.03 | ($0.01) | 14 | $0.09 | ($0.04) | 29 | $0.15 | ($0.07) |
|
| ||||||||||||
| Dairy - unsweetened | 7 | $0.13 | ($0.11) | 6 | $0.27 | ($0.12) | 13 | $0.25 | ($0.08) | 15 | $0.22 | ($0.08) |
|
| ||||||||||||
| Dairy - sweetened | 6 | $0.35 | ($0.04) | |||||||||
|
| ||||||||||||
| Salty snacks - flavored | 78 | $0.29 | ($0.12) | 52 | $0.29 | ($0.08) | 32 | $0.31 | ($0.16) | 11 | $0.26 | ($0.05) |
|
| ||||||||||||
| Chips | 26 | $0.27 | ($0.04) | 24 | $0.28 | ($0.04) | 13 | $0.34 | ($0.17) | 1 | $0.30 | |
|
| ||||||||||||
| Cheese Flavored Crackers | 24 | $0.33 | ($0.19) | 14 | $0.28 | ($0.13) | 13 | $0.29 | ($0.17) | 7 | $0.23 | ($0.05) |
|
| ||||||||||||
| Salty snacks - unflavored | 11 | $0.21 | ($0.12) | 7 | $0.62 | ($0.33) | 26 | $0.19 | ($0.11) | 28 | $0.25 | ($0.15) |
|
| ||||||||||||
| Pretzels | 5 | $0.31 | ($0.05) | 1 | $0.27 | 11 | $0.22 | ($0.10) | 14 | $0.29 | ($0.15) | |
|
| ||||||||||||
| Tortilla Chips | 1 | $0.16 | 8 | $0.17 | ($0.05) | 6 | $0.19 | ($0.09) | ||||
|
| ||||||||||||
| Whole Grain Crackers | 2 | $0.56 | ($0.04) | 3 | $0.02 | ($0.02) | 3 | $0.06 | ($0.01) | |||
|
| ||||||||||||
| Desserts | 100 | $0.28 | ($0.16) | 55 | $0.27 | ($0.12) | 65 | $0.25 | ($0.09) | 6 | $0.32 | ($0.09) |
|
| ||||||||||||
| Animal Crackers | 19 | $0.28 | ($0.20) | 8 | $0.14 | ($0.03) | 8 | $0.21 | ($0.08) | 3 | $0.33 | ($0.08) |
|
| ||||||||||||
| Snack Bars | 19 | $0.38 | ($0.10) | 7 | $0.33 | ($0.09) | 15 | $0.31 | ($0.09) | 1 | $0.30 | |
|
| ||||||||||||
| Cookies | 25 | $0.25 | ($0.18) | 17 | $0.26 | ($0.14) | 7 | $0.27 | ($0.09) | |||
|
| ||||||||||||
| Cereal - sugar-sweetened | 25 | $0.31 | ($0.16) | 20 | $0.37 | ($0.20) | 12 | $0.46 | ($0.16) | 2 | $0.24 | |
|
| ||||||||||||
| Cereal - unsweetened | 2 | $0.38 | ($0.03) | 6 | $0.52 | ($0.23) | 2 | $0.25 | 3 | $0.32 | ($0.16) | |
| Beverages (price per serving per day) | ||||||||||||
| Sugar-sweetened non-dairy beverages | 20 | $0.17 | ($0.18) | 12 | $0.08 | ($0.06) | 14 | $0.27 | ($0.11) | 1 | $0.33 | |
|
| ||||||||||||
| Milk - sugar-sweetened | 1 | $0.37 | 1 | $0.37 | ||||||||
|
| ||||||||||||
| Non-100% Fruit Juice | 1 | $0.50 | 4 | $0.37 | ($0.02) | |||||||
|
| ||||||||||||
| 100% Fruit Juice | 7 | $0.30 | ($0.11) | 12 | $0.37 | ($0.06) | ||||||
|
| ||||||||||||
| Milk - unflavored | 4 | $0.16 | ($0.07) | 4 | $0.25 | ($0.02) | 15 | $0.22 | ($0.09) | 5 | $0.24 | ($0.05) |
Figure 2.
Baseline and post-assessment expenditures for foods, dips, and beverages served for snack in control and intervention afterschool programs
Note: Error bars represent one standard deviation.
Discussion
Across the nation, ASPs are working to serve more healthful snacks that meet state and national guidelines that call on programs to serve fruits and vegetables on a regular basis, while eliminating foods and beverages that are high in sugar, salt, and artificial flavors. However, ASPs struggle to achieve these goals, with price being one of the primary barriers. This study evaluated an intervention that works with ASPs to identify current snack expenditures, develop menus that meet the Healthy Eating Standards, and to identify low-cost outlets for programs to purchase these snacks. Overall, increases in the foods and beverages that meet the Healthy Eating Standards were observed in the intervention ASPs, children consumed the more healthful snacks, and the overall cost of the snacks increased marginally. These findings hold considerable relevance for thousands of ASPs across the nation looking for simple ways to improve the quality of the snacks without substantially increasing cost.
Consistent with the findings presented herein, previous policy-focused studies4,5 have resulted in improvements in the types of snack served in ASPs. These studies focused on adopting policy standards for the types of foods and beverages served and found that changes made by program leaders led to improvements in the types of snacks served. These studies,4,5 however, did not address the cost associated with purchasing more healthful snacks, such as fruits and vegetables, which have been shown to be more expensive than less healthful snacks, such as flavored chips and cookies.7,34 The current study addressed this gap by integrating within the intervention approach strategies for ASPs to identify and subsequently purchase snacks at food outlets with prices that met their snack budget. However, this resulted in a marginal increase of $0.02 per snack (i.e., $317 across 180 day school year for 88 children/day). Whether this increase is prohibitive would be largely left to individual providers to determine, given that some are likely unable to adjust their snack budget, regardless of the amount increased, whereas other programs may be able to absorb this increase in snack cost. Despite this, this study demonstrated that working with ASPs to serve snacks more aligned with national recommendations and identifying outlets that help providers meet their snack budget does not result in programs having to substantially increase the amount they allocate to purchasing snacks.
Several of the intervention ASPs were conveniently located (e.g., within 2 to 3 blocks) near a grocery store and began purchasing snacks from them. Four ASPs were within <10 minute drive of a large bulk warehouse chain and were directed to this food outlet to save money on purchasing snacks. The remaining ASPs were directed towards food outlets within their vicinity where snacks could be purchase at a reduced cost compared to where they were currently purchasing snacks. This component of the intervention was critical, particularly since the ASPs were unaware of the amount of money they could save by changing the location from which they purchased snacks. As illustrated in Table 3 and Figure 2, redirecting ASPs to lower cost outlets resulted in a modest reduction in the cost of fruits and vegetables. As indicated in Table 2, intervention ASPs also substantially reduced the number of days they served a purchased beverage (e.g., non-100% fruit juice). Reducing cost associated with serving a beverage, other than water, helped in reducing the overall expenditures on snacks. Interestingly, the increase in fruits and vegetables served corresponded to an increase the purchases of dips which largely offset the cost savings not purchasing a beverage. While dips have received attention as an important component to getting children to each vegetables,35,36 their introduction into an ASPs’ snack presents another item that providers have to purchase that, as demonstrated in this study, contributes to overall snack cost. Thus, as ASPs look for ways to save on snack expenses, offsetting costs associated with purchasing fruits and vegetables can be done through eliminating costs associated with serving a purchased beverage, yet programs need to be mindful of added expenses associated with providing a dip with a fruit or vegetable.
The direct observation of children consuming the snack indicated that across the measurement periods, when children were served a fruit or vegetable, they ate the snack. This is important information for program providers who may hesitate serving more healthful snacks for fear of increased waste due to children not wanting to eat the snack. There are several reasons for the high level of consumption. First, the standards evaluated herein indicated that less healthful snacks (e.g., cookies, chips) cannot be served alongside a more healthful option (i.e., fruits or vegetables) with children given a choice of selecting one or the other. A recent study37 found that a greater percentage of children ate fruit when served as the only option, compared to when fruit was served alongside other, less healthful items (e.g., cookies and chips). Secondly, a component of the intervention was a specific focus on staff role modeling healthy eating behaviors, such as sitting and eating the snack with the children or refraining from eating outside foods/beverages in front of the children during the program. These are important socialization behaviors that policy and standards documents ask staff to exhibit to create a healthy eating environment.1,38,39 In total, we believe these are important for ASPs to consider when they look for way to adopt and subsequently meet snack nutritional standards.
From the site visits not all intervention ASPs readily adopted all the elements identified in the STEPs-HE framework. Specifically, by post-assessment, several intervention ASPs still did not have a regular snack menu, were not posting this for parents/staff to view, were not following the posted snack menu consistently, or were unaware of the amount of money allocated for snack purchases. Despite this, substantial changes in the quality of snacks served still occurred. This suggests that ASPs were making changes to the types of snacks they served, yet were not integrating or formalizing these changes into routine practice. This is concerning, particularly if the changes observed were largely driven by the ASP leader. For instance, in several cases the ASP leader indicated no snack menu was necessary because they “knew” what they were going to serve on a regular basis – fruits and vegetables. However, if this knowledge is confined to one specific individual, question concerning the practices’ (i.e., serving fruits and vegetables daily) longevity are raised, especially given the high rates of turnover at the site leader position.40 Conversely, having a formalized process and policies is not a guarantee for serving more healthful snacks. For example, a control ASP had adopted snack quality standards during the spring 2014 and also had a detailed weekly menu and budgeted amount. In conversations with the ASP leader, they indicated they were to serve a fruit or vegetable every day and the program leader indicated this was being achieved. Upon review of the snack menu (and based on direct observation), no fruit or vegetables were listed on the menu or were observed being served. These inconsistencies indicate a sizable disconnect between what policies and standards call for programs to do, what program leaders perceive they are doing, and what is actually delivered during routine practice. Given this, additional effort is required to assist ASP leaders in formalizing healthy eating practices so that any person within the ASP organization can continue the practice and that each individual is fully aware of what the standards call for programs to do and that this is carried out daily.
There are numerous strengths to this study. These include the large number of ASPs, direct observation of snacks served and consumed, and the use of actual food receipts to calculate cost. Previous studies have relied on menus provided by ASP leaders and cost estimated from national databases.5,7 Based on the findings here, with the substantial amount of inconsistency of what was served versus what was on the menu, reliance upon menus as an indicator of the snack served may lead to inaccurate estimates of what was actually served. There are also several limitations. First, the findings presented represent only a single year of intervention. Given the complexity of changing organizational structures, additional time may be necessary to formalize all the STEPs-HE components into routine practice. Secondly, several of the snack items’ costs were based on 10 or fewer occurrences. This was due to the limited times these items occurred on the receipts provided by the ASP leaders. Despite this these prices reflect a more accurate cost estimate than what can be found in national databases where costs are averaged across region and may not reflect current market prices.7 Additionally, the consumption measured used herein does not calculate the amount of waste via weight remaining of the snacks. This was not performed because of the complexity of the snack environment, with many children coming in to receive snack at one time and the inability to determine how many snacks were distributed by program staff. Further, the limited time allocated to snack (~15min) necessitated a measure that could quickly capture what children were eating. Despite these limitations, the substantial number of observations of children during snack provide a reasonable estimate of child consumption.
Conclusion
In conclusion, the STEPs-HE framework can assist ASPs in working towards meeting the Healthy Eating Standards with minimal increases in overall snack cost. Additional work is needed to assist ASPs in formalizing these practices through organizational adoption and formalization to ensure they are sustainable.
So What? Implications for Health Promotion Practitioners and Researchers.
What is already known on this topic?
The adoption of snack nutrition policies can lead to improvements in the types of foods and beverages afterschool programs serve. However, previous efforts have failed to address cost as a barrier to serving more healthful snacks, like fruits and vegetables.
What does this article add?
This study demonstrated that working with program providers to build capacity for developing menus, understanding snack budgets, and identification of outlets to purchase snack at an affordable rate leads to more providers achieving snack nutrition policies. Importantly, the findings demonstrate that programs can achieve nutrition policies without substantially increasing cost associated with purchasing more healthful snacks.
What are the implications for health promotion practice or research?
These findings provide evidence that afterschool program providers can achieve nationally endorsed snack nutrition policies with marginal increases in snack cost. Providers, however, should be mindful that the introduction of new food items, primarily dips, will have an associated cost and may eliminate cost savings with not serving a beverage.
Acknowledgments
Funding:
Research reported in this publication was supported by the National Heart, Lung, And Blood Institute of the National Institutes of Health under Award Number R01HL112787. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Potential conflicts of interest:
None
Clinical Trials.gov
References
- 1.Beets MW, Tilley F, Kim Y, Webster C. Nutritional policies and standards for snacks served in after-school programmes: a review. Public Health Nutr. 2011;14(10):1882–90. doi: 10.1017/S1368980011001145. [DOI] [PubMed] [Google Scholar]
- 2.Peterson E. First lady announces two new commitments to healthy eating and physical activity afterschool: Afterschool Alliance. 2014 [cited 2014 March 1]. Available from: http://www.afterschoolalliance.org/afterschoolsnack/printPage.cfm?idBlog=6FD1B2AD-215A-A6B3-02AAB84B1F59DA3F; http://ahealthieramerica.org/media/news-releases/#5482,news.
- 3.Beets MW, Tilley F, Turner-McGrievy G, Weaver RG, Jones SJ. Community partnership to address snack quality and cost in afterschool programs. J Sch Health. doi: 10.1111/josh.12175. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cassady D, Vogt R, Oto-Kent D, Mosley R, Lincoln R. The power of policy: a case study of healthy eating among children. Am J Public Health. 2006;96(9):1570–1. doi: 10.2105/AJPH.2005.072124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mozaffarian RS, Wiecha JL, Roth BA, Nelson TF, Lee RM, Gortmaker SL. Impact of an Organizational Intervention Designed to Improve Snack and Beverage Quality in YMCA After-School Programs. American Journal of Public Health. 2010;100(5):925–32. doi: 10.2105/AJPH.2008.158907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Coleman KJ, Geller KS, Rosenkranz RR, Dzewaltowski DA. Physical activity and healthy eating in the after-school environment. J Sch Health. 2008;78(12):633–40. doi: 10.1111/j.1746-1561.2008.00359.x. [DOI] [PubMed] [Google Scholar]
- 7.Mozaffarian RS, Andry A, Lee RM, Wiecha JL, Gortmaker SL. Price and Healthfulness of Snacks in 32 YMCA After-School Programs in 4 US Metropolitan Areas, 2006–2008. Preventing Chronic Disease. 2012:9. doi: 10.5888/pcd9.110097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dzewaltowski DA, Rosenkranz RR, Geller KS, Coleman KJ, Welk GJ, Hastmann TJ, et al. HOP’N after-school project: an obesity prevention randomized controlled trial. Int J Behav Nutr Phys Act. 2010;7(1):90. doi: 10.1186/1479-5868-7-90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nanney MS, Olaleye TM, Wang Q. Incorporating a Healthy Reimbursable Snack in an Afterschool Homework Program for Middle School Students: A Case Study. Health Educ Behav. 2011 doi: 10.1177/1090198111404066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hastmann TJ, Bopp M, Fallon EA, Rosenkranz RR, Dzewaltowski DA. Factors Influencing the Implementation of Organized Physical Activity and Fruit and Vegetable Snacks in the HOP’N After-School Obesity Prevention Program. J Nutr Educ Behav. 2013;45(1):60–8. doi: 10.1016/j.jneb.2012.06.005. [DOI] [PubMed] [Google Scholar]
- 11.Institute of Medicine. Child and Adult Care Food Program: Aligning Dietary Guidance for All. Washington, DC: 2010. [cited 2012 April 20]. Available from: Available at: http://www.iom.edu/Reports/2010/Child-and-Adult-Care-Food-Program-Aligning-Dietary-Guidance-for-All.aspx. [Google Scholar]
- 12.Beets MW, Tilley F, Weaver RG, Turner-McGrievy G, Moore JB, Webster C. From Policy to Practice: Addressing Snack Quality, Consumption, and Price in After-School Programs. J Nutr Educ Behav. 2013 doi: 10.1016/j.jneb.2013.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Beets MW, Weaver RG, Turner-McGrievy G, Huberty J, Ward D, Freedman DA, et al. Making Healthy Eating and Physical Activity Policy Practice: The Design and Overview of a Group Randomized Controlled Trial in Afterschool Programs. Contemporary Clinical Trials. doi: 10.1016/j.cct.2014.05.013. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Beets MW, Glenn Weaver R, Turner-McGrievy G, Huberty J, Ward DS, Freedman DA, et al. Making healthy eating and physical activity policy practice: The design and overview of a group randomized controlled trial in afterschool programs. Contemp Clin Trials. 2014;38(2):291–303. doi: 10.1016/j.cct.2014.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Beets MW. Enhancing the translation of physical activity interventions in afterschool programs. American Journal of Lifestyle Medicine. 2012;6(4):328–41. [Google Scholar]
- 16.Wandersman A, Duffy J, Flaspohler P, Noonan R, Lubell K, Stillman L, et al. Bridging the gap between prevention research and practice: the interactive systems framework for dissemination and implementation. Am J Community Psychol. 2008;41(3–4):171–81. doi: 10.1007/s10464-008-9174-z. [DOI] [PubMed] [Google Scholar]
- 17.Hawe P, Shiell A, Riley T. Complex interventions: how “out of control” can a randomised controlled trial be? BMJ. 2004;328(7455):1561–3. doi: 10.1136/bmj.328.7455.1561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Beets MW, Webster C, Saunders R, Huberty JL. Translating policies into practice: a framework for addressing childhood obesity in afterschool programs. Health Promotion Practice. 2013;14(2):228–37. doi: 10.1177/1524839912446320. [DOI] [PubMed] [Google Scholar]
- 19.Israel BA, Schulz AJ, Parker EA, Becker AB. Review of community-based research: assessing partnership approaches to improve public health. Annu Rev Public Health. 1998;19:173–202. doi: 10.1146/annurev.publhealth.19.1.173. [DOI] [PubMed] [Google Scholar]
- 20.Maslow AH. A theory of human motivation. Psychological Review. 1943;50:370–96. [Google Scholar]
- 21.Butler SF, Strupp HH. Specific and Nonspecific Factors in Psychotherapy - a Problematic Paradigm for Psychotherapy-Research. Psychotherapy. 1986;23(1):30–40. [Google Scholar]
- 22.Chatoor I, Krupnick J. The role of non-specific factors in treatment outcome of psychotherapy studies. Eur Child Adolesc Psychiatry. 2001;10(Suppl 1):I19–25. doi: 10.1007/s007870170004. [DOI] [PubMed] [Google Scholar]
- 23.Collins LM, Murphy SA, Bierman KL. A conceptual framework for adaptive preventive interventions. Prev Sci. 2004;5(3):185–96. doi: 10.1023/b:prev.0000037641.26017.00. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.U.S. Department of Agriculture Food and Nutrition Service. Monitoring Handbook for State Agencies: A Child and Adult Care Food Program Handbook. U.S. Department of Agriculture; 2013. [Google Scholar]
- 25.Beets MW, Rooney L, Tilley F, Beighle A, Webster C. Evaluation of policies to promote physical activity in afterschool programs: are we meeting current benchmarks? Prev Med. 2010;51(3–4):299–301. doi: 10.1016/j.ypmed.2010.07.006. [DOI] [PubMed] [Google Scholar]
- 26.Beets MW, Beighle A, Bottai M, Rooney L, Tilley F. Pedometer-determined step count guidelines for afterschool programs. Journal of Physical Activity and Health. 2012;9(1):71–7. doi: 10.1123/jpah.9.1.71. [DOI] [PubMed] [Google Scholar]
- 27.Beets MW, Huberty J, Beighle A. Physical Activity of Children Attending Afterschool Programs Research- and Practice-Based Implications. Am J Prev Med. 2012;42(2):180–4. doi: 10.1016/j.amepre.2011.10.007. [DOI] [PubMed] [Google Scholar]
- 28.Beets MW, Weaver RG, Moore JB, Turner-McGrievy G, Pate RR, Webster C, et al. From Policy to Practice: Strategies to Meet Physical Activity Standards in YMCA Afterschool Programs. Am J Prev Med. doi: 10.1016/j.amepre.2013.10.012. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mozaffarian RS, Wiecha JL, Roth BA, Nelson TF, Lee RM, Gortmaker SL. Impact of an Organizational Intervention Designed to Improve Snack and Beverage Quality in YMCA After-School Programs. Am J Public Health. 2009 doi: 10.2105/AJPH.2008.158907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sweitzer SJ, Briley ME, Robert-Gray C. Do Sack Lunches Provided by Parents Meet the Nutritional Needs of Young Children Who Attend Child Care? J Am Diet Assoc. 2009;109(1):141–4. doi: 10.1016/j.jada.2008.10.010. [DOI] [PubMed] [Google Scholar]
- 31.Simons-Morton BG, Forthofer R, Huang IW, Baranowski T, Reed DB, Fleishman R. Reliability of direct observation of schoolchildren’s consumption of bag lunches. J Am Diet Assoc. 1992;92(2):219–21. [PubMed] [Google Scholar]
- 32.Donner A, Taljaard M, Klar N. The merits of breaking the matches: a cautionary tale. Stat Med. 2007;26(9):2036–51. doi: 10.1002/sim.2662. [DOI] [PubMed] [Google Scholar]
- 33.Diehr P, Martin DC, Koepsell T, Cheadle A. Breaking the matches in a paired t-test for community interventions when the number of pairs is small. Stat Med. 1995;14(13):1491–504. doi: 10.1002/sim.4780141309. [DOI] [PubMed] [Google Scholar]
- 34.Beets MW, Weaver RG, Tiley F, Turner-McGrievy G, Huberty J, Ward DS, et al. Salty or Sweet? Nutritional quality, consumption, and cost of snacks served in afterschool programs. J Sch Health. doi: 10.1111/josh.12224. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Savage JS, Fisher JO, Marini M, Birch LL. Serving smaller age-appropriate entree portions to children aged 3–5 y increases fruit and vegetable intake and reduces energy density and energy intake at lunch. Am J Clin Nutr. 2012;95(2):335–41. doi: 10.3945/ajcn.111.017848. [DOI] [PubMed] [Google Scholar]
- 36.Fisher JO, Mennella JA, Hughes SO, Liu Y, Mendoza PM, Patrick H. Offering “Dip” Promotes Intake of a Moderately-Liked Raw Vegetable among Preschoolers with Genetic Sensitivity to Bitterness. J Acad Nutr Diet. 2012;112(2):235–45. doi: 10.1016/j.jada.2011.08.032. [DOI] [PubMed] [Google Scholar]
- 37.Beets MW, Tilley F, Kyryliuk R, Weaver RG, Moore JB, Turner-McGrievy G. Children select unhealthy choices when given a choice among snack offerings. Journal of the Academy of Nutrition and Dietetics. doi: 10.1016/j.jand.2014.04.022. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ajja R, Beets MW, Huberty J, Kaczynski AT, Ward DS. The Healthy Afterschool Activity and Nutrition Documentation Instrument. Am J Prev Med. 2012;43(3):263–71. doi: 10.1016/j.amepre.2012.05.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Weaver RG, Beets MW, Webster C, Huberty J. System for Observing Staff Promotion of Activity and Nutrition (SOSPAN) J Phys Act Health. 2014;11(1):173–85. doi: 10.1123/jpah.2012-0007. [DOI] [PubMed] [Google Scholar]
- 40.Beets MW, Weaver RG, Moore JB, Turner-McGrievy G, Pate RR, Webster C, et al. From Policy to Practice: Strategies to Meet Physical Activity Standards in YMCA Afterschool Programs. Am J Prev Med. 2014;46(3):281–8. doi: 10.1016/j.amepre.2013.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]