Abstract
Prehypertension is associated with increased risk for hypertension and cardiovascular disease. Data are limited on the temporal changes in the prevalence of prehypertension and risk factors for hypertension and cardiovascular disease among United States adults with prehypertension. We analyzed data from 30,958 United States adults aged ≥20 years who participated in the National Health and Nutrition Examination Surveys between 1999 and 2012. Using the mean of three blood pressure measurements from a study examination, prehypertension was defined as systolic blood pressure of 120 to 139 mmHg and diastolic blood pressure <90 mmHg or diastolic blood pressure of 80 to 89 mmHg and systolic blood pressure <140 mmHg among participants not taking antihypertensive medication. Between 1999–2000 and 2011–2012, the percentage of United States adults with prehypertension decreased from 31.2% to 28.2% (p-trend=0.007). During this time period, the prevalence of several risk factors for cardiovascular disease and incident hypertension increased among United States adults with prehypertension including prediabetes (9.6% to 21.6%) and diabetes (6.0% to 8.5%) and overweight (33.5% to 37.3%) and obesity (30.6% to 35.2%). There was a non-statistically significant increase in no weekly leisure-time physical activity (40.0% to 43.9%). Also, the prevalence of adhering to the Dietary Approaches to Stop Hypertension eating pattern decreased (18.4% to 11.9%). In contrast, there was a non-statistically significant decline in current smoking (25.9% to 23.2%). In conclusion, the prevalence of prehypertension has decreased modestly since 1999–2000. Population-level approaches directed at adults with prehypertension are needed to improve risk factors to prevent hypertension and cardiovascular disease.
Keywords: prehypertension, NHANES, trend, hypertension risk factors, risk for hypertension, prevention
Introduction
In 2003, the Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC7) characterized adults, not taking antihypertensive medication, with systolic blood pressure (SBP) between 120 and 139 mmHg with diastolic blood pressure (DBP) < 90 mm Hg or DBP between 80 and 89 mmHg with SBP < 140 mm Hg as having prehypertension.1 Adults with prehypertension have a high risk for developing hypertension, defined as SBP ≥140 mmHg or DBP ≥90 mmHg or the use of antihypertensive medication.2–5 The risk for hypertension among people with prehypertension can be reduced through lifestyle modification and antihypertensive medication use.1, 5–7 While one goal of the JNC7 guideline was to increase awareness of the high risk for incident hypertension associated with prehypertension,1, 7 studies conducted after its publication have been cross-sectional and there have been limited data published on the temporal changes in the prevalence of prehypertension and the risk factors for incident hypertension among those with prehypertension.8–11
In the current study, we determined temporal changes in the prevalence of prehypertension among US adults, overall, and within subgroups defined by age, race/ethnicity and sex. Also, since there is an opportunity to prevent the transition to hypertension and reduce cardiovascular disease (CVD) morbidity and mortality through lifestyle modification and pharmacologic antihypertensive treatment among adults with prehypertension, temporal changes in risk factors for incident hypertension, target-organ damage and CVD were determined among this population.12 Results from the current study may help to determine the need for interventions among adults with prehypertension and identify specific approaches that may lower blood pressure (BP) in adults at high risk for developing hypertension.
Methods
Study population
The National Health and Nutrition Examination Survey (NHANES) is a US-based cross-sectional survey of the non-institutionalized civilian population. NHANES applies a multistage stratified probability sampling approach to identify participants and allows the generation of nationally representative estimates. Additional information on the design and conduct of NHANES is available online.13 In brief, NHANES has been conducted in 2-year cycles since 1999. For the current analysis, we studied seven 2-year cycles from 1999–2000 through 2011–2012.14 During this time period, there were 30,958 participants with 3 valid clinic SBP and DBP measurements and complete information on antihypertensive medication use obtained during study visits (Figure S1). The National Center for Health Statistics Review Board governing human subjects’ research approved the NHANES protocol. All participants provided written informed consent.
Data collection
NHANES data were collected during an in-home interview and clinic examination. During the interview, trained staff administered questionnaires to collect self-reported information on socio-demographics, diet- and health-related behaviors and prior diagnosed co-morbid conditions and use of prescription antihypertensive medication. During the clinic examination, trained technicians measured height, weight and BP and collected blood and spot urine samples.
Risk factors for incident hypertension, CVD and target-organ damage
Age was categorized as <40, 40–59 and ≥60 years. Race/ethnicity was defined as non-Hispanic white, non-Hispanic black and Hispanic. Heart rate, quantified in beats per minutes, was measured by palpating the radial pulse after 3 minutes of rest. Total cholesterol was categorized as normal (<200 mg/dL), borderline-elevated (200–239 mg/dL) or elevated (≥240 mg/dL). Low high-density-lipoprotein cholesterol (HDL) was defined as <40 and <50 mg/dL in men and women, respectively. C-reactive protein was defined as normal (<1.0 mg/L), borderline-elevated (1.0 to <3.0 mg/L) or elevated (≥3.0 mg/L). Participants were categorized as not having pre-diabetes or diabetes if they did not self-report a prior diagnosis by a physician and were not taking hypoglycemic medication and they had a hemoglobin A1c <5.7%, pre-diabetes if they did not self-report a history of diabetes and were not taking hypoglycemic medication and had hemoglobin A1c of 5.7% to 6.4% or diabetes if they self-reported a history of diagnosis and/or were taking hypoglycemic medication and/or had hemoglobin A1c ≥6.5%. Estimated glomerular filtration rate (eGFR) was calculated using the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equation with calibrated serum creatinine.15, 16 Reduced eGFR was defined as <60 ml/min/1.73m2. Elevated urinary albumin-to-creatinine ratio (ACR) was defined as ≥30 mg/g. High 10-year predicted atherosclerotic cardiovascular disease (ASCVD) risk was defined as ≥7.5% using the Pooled Cohort risk equations.17
Modifiable lifestyle risk factors
Body mass index (BMI), calculated as weight in kilograms divided by height in meters squared, was categorized as <25, 25 to <30 and ≥30 kg/m2. Current cigarette smoking was defined by self-reporting smoking >100 cigarettes in their lifetime and currently smoking or having quit <1 year ago. Leisure-time physical activity was calculated in minutes per week following similar methods as described by Ladabaum.18 Briefly, the total minutes of physical activity per week were calculated from participants’ self-reported information on the frequency, duration and level of exertion for leisure-time activities. The ideal physical activity category included participants who self-reported at least 75 minutes of vigorous activity or at least 150 minutes of moderate or vigorous activity per week. The category for intermediate physical activity included those who had 1 to 74 minutes of vigorous activity or 1 to 149 minutes of moderate or vigorous activity per week. Poor physical activity was defined as 0 minutes of moderate or vigorous activity per week. Weekly alcohol consumption, determined by the self-reported number of drinks per week during the previous 12 months, was defined as none, moderate (men: 1–14 drinks; women: 1–7 drinks) or heavy (men: >14 drinks; women: >7 drinks). Interviewer-administered questionnaires were used to record dietary intake over two 24-hour periods. A Dietary Approaches to Stop Hypertension (DASH) adherence score was estimated similar to Fung and Günther.19, 20 This dietary pattern is low in sodium and cholesterol, high in dietary fiber, potassium, calcium and magnesium and moderately high in protein content. Quintiles of the eight DASH diet components (increased intake of fruits, vegetables, low-fat dairy products, whole grains, and nuts/seeds/legumes; reduced intake of fats/oils, sugar-sweetened beverages, meat/poultry/fish) and reduced sodium consumption were created among all NHANES participants between 1999 and 2012. The rank scores were summed to obtain an overall DASH diet score (range: 9 [least healthy] to 45 [healthiest]). Participants were grouped into quartiles based on the distribution of DASH diet scores among all US adults ≥20 years old (cut-points [quartile 1 to quartile 4]: < 25 [least healthy], 25 to < 28, 28 to < 31 and ≥ 31 [healthiest]).
Blood pressure
BP was measured following a standardized protocol using the American Heart Association’s recommendations.13, 21–23 After participants were seated for at least 5 minutes in an upright position with their back and arms supported, feet flat on the floor and legs uncrossed, trained staff conducted three BP measurements in the right arm using a mercury sphygmomanometer and appropriate cuff size determined from an arm circumference measurement. At least 30 seconds elapsed between the measurements. Quality control included quarterly re-certification with retraining as needed, annually retraining of all physicians and monitoring/repairing equipment. Certification required video test recognition of Korotkoff sounds and performing measurements on volunteers. Normal BP was defined as SBP < 120 mmHg and DBP < 80 mmHg without antihypertensive medication use. Prehypertension was defined by SBP of 120 to 139 mm Hg with DBP < 90 mmHg or DBP of 80 to 89 mm Hg with SBP < 140 mmHg without antihypertensive medication use. The lower range of prehypertension was defined as SBP 120–129 mmHg with DBP < 85 mm Hg and/or DBP 80–84 mmHg with SBP < 130 mm Hg and the upper range of prehypertension was defined as SBP 130–139 mmHg and/or DBP 85–89 mmHg. Hypertension was defined as SBP≥140 mmHg or DBP≥90 mmHg and/or antihypertensive medication use.
Statistical Analysis
The age-adjusted percentage of US adults aged ≥20 years with normal BP, prehypertension and hypertension was calculated for each 2-year cycle of NHANES overall and in subgroups defined by age, race/ethnicity and sex. Age was adjusted using 2010 US Census data. Using logistic regression, the statistical significance of the linear trend in the age-adjusted prevalence of prehypertension was calculated by modeling an ordinal variable for each NHANES cycle as a continuous predictor variable of prehypertension status. Differences in linear trends in the prevalence of prehypertension over NHANES cycles across age, race/ethnicity and sex sub-groups was determined by modeling interaction terms (e.g., sex*NHANES cycle). Analyses were repeated to calculate the age-adjusted prevalence of prehypertension among adults without normal BP (i.e., among adults with prehypertension or hypertension) and without hypertension (i.e., among adults with normal BP and prehypertension), separately. Also, multivariable adjusted prevalence ratios for prehypertension associated with NHANES cycles were calculated among adults without normal BP and without hypertension, separately, using Poisson regression. An initial model with adjustment for age, race/ethnicity and sex was further adjusted for incident hypertension, CVD and target-organ damage and modifiable lifestyle risk factors in three subsequent regression models. Pooling 2009–2012 NHANES data to provide stable estimates, we calculated prevalence ratios for prehypertension or hypertension comparing participants <40 and 40 to 59 versus ≥60 years of age, non-Hispanic blacks and Hispanics versus non-Hispanic whites and females versus males using log-binomial models. Prevalence ratios for prehypertension associated with age, race/ethnicity and sex were also calculated among US adults without hypertension.
The mean or prevalence of risk factors (i.e., heart rate, total cholesterol, high density lipoprotein cholesterol, diabetes, estimated glomerular filtration rate, urinary albumin to creatinine ratio and 10-year predicted atherosclerotic cardiovascular disease risk) and modifiable lifestyle factors (i.e., BMI, smoking status, physical activity level, alcohol consumption and DASH diet adherence) was calculated in adults with prehypertension by NHANES cycle. The statistical significance of trends in the change in risk factors over NHANES cycles were calculated using linear regression or logistic regression, as appropriate. All analyses were performed accounting for the complex survey design of NHANES and results were weighted to the non-institutionalized civilian US adult population using SAS 9.4 (SAS Institute, Cary NC). Two-sided p-values <0.05 were considered statistically significant.
RESULTS
Trends in prevalent normal blood pressure, prehypertension and hypertension
From 1999–2000 to 2011–2012, there was a non-statistically significant increase in the age-adjusted percentage of US adults with normal BP and hypertension and a statistically significant decrease in prevalent prehypertension from 31.2% to 28.2% (Figure 1, top panel). The number of US adults with normal BP and hypertension increased from 1999–2000 to 2011–2012 while the number with prehypertension was stable (Figure 1, bottom panel). The prevalence of normal BP increased (Figure 2, left column and Table S1, top panel) and prehypertension decreased in those aged ≥60 years between 1999–2000 and 2011–2012. A decrease in the age-adjusted prevalence of prehypertension occurred among males (Figure 2, middle column and Table S1, middle panel). The prevalence of hypertension remained stable in all subgroups (Figure 2, right column and Table S1, bottom panel).
Figure 1.
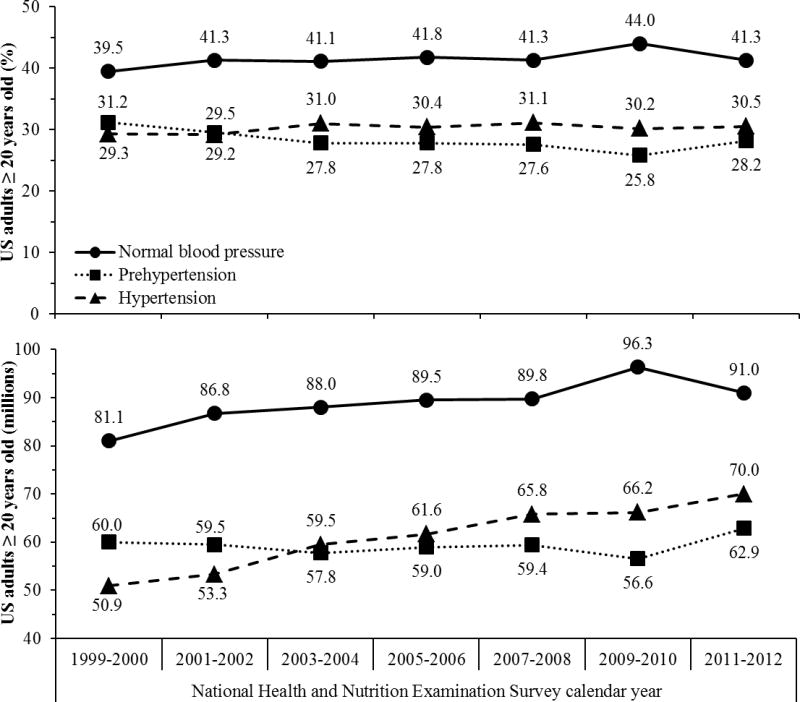
Age-adjusted percentage (top panel) and unadjusted number (bottom panel) of United States adults aged ≥ 20 years with normal blood pressure, prehypertension and hypertension by National Health and Nutrition Examination Survey (NHANES) by calendar year.
Normal blood pressure: systolic blood pressure < 120 mmHg and diastolic blood pressure < 80 mmHg without antihypertensive medication use.
Prehypertension: systolic blood pressure 120–139 mmHg with diastolic blood pressure < 90 mmHg or diastolic blood pressure 80–89 mmHg with systolic blood pressure < 140 mmHg without antihypertensive medication use.
Hypertension: systolic blood pressure ≥ 140 mmHg or diastolic blood pressure ≥ 90 mmHg and/or antihypertensive medication use.
Figure 2.
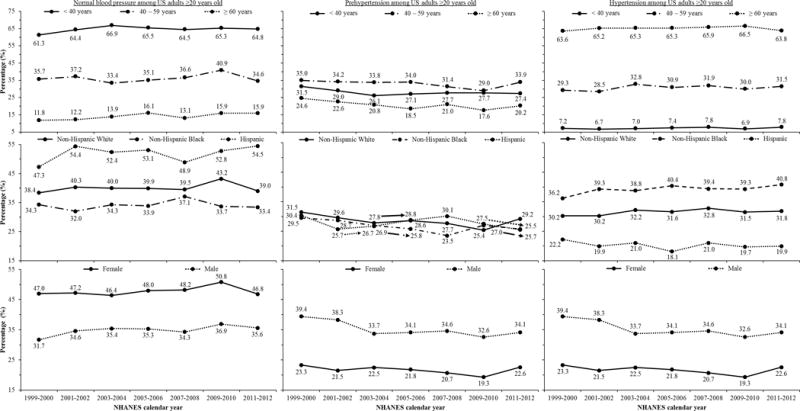
Age-adjusted percentage of United States adults aged ≥ 20 years with normal blood pressure (left column), prehypertension (middle column) and hypertension (right column) from 1999–2000 through 2011–2012 by age, race/ethnicity and sex.
US: United States.
Arrows indicate the prevalence corresponding with Non-Hispanic Whites, Non-Hispanic Blacks or Hispanics where the plotted values for these race/ethnic groups are difficult to distinguish.
The age-adjusted percentage of United States adults aged ≥ 20 years with normal blood pressure, prehypertension and hypertension from 1999–2000 through 2011–2012 overall is reported in Table S1. Also, the 95% confidence interval corresponding with each point estimate in the current figure, p-trend representing the change in the prevalence over calendar period and the p-interaction representing differences in the change in the prevalence over calendar period across age, race/ethnicity and sex sub-groups is reported in Table S1.
Trends in prevalent prehypertension among adults without normal BP and without hypertension
Among US adults without normal BP, the age-adjusted prevalence of prehypertension decreased between 1999–2000 and 2011–2012. There was no change in prehypertension in any of the age categories investigated, but the prevalence of prehypertension declined in non-Hispanic whites, non-Hispanic blacks and males (Figure 3, left column and Table S2, top panel). The change in the prevalence of prehypertension from 1999–2000 through 2011–2012 was similar across age, race/ethnicity and sex groups. In adults without hypertension, there was a decrease in the prevalence of prehypertension overall and among US adults aged ≥60 years and males, but no statistically significant change was present for any of the race/ethnicity groups (Figure 3, right column and Table S2, bottom panel).
Figure 3.
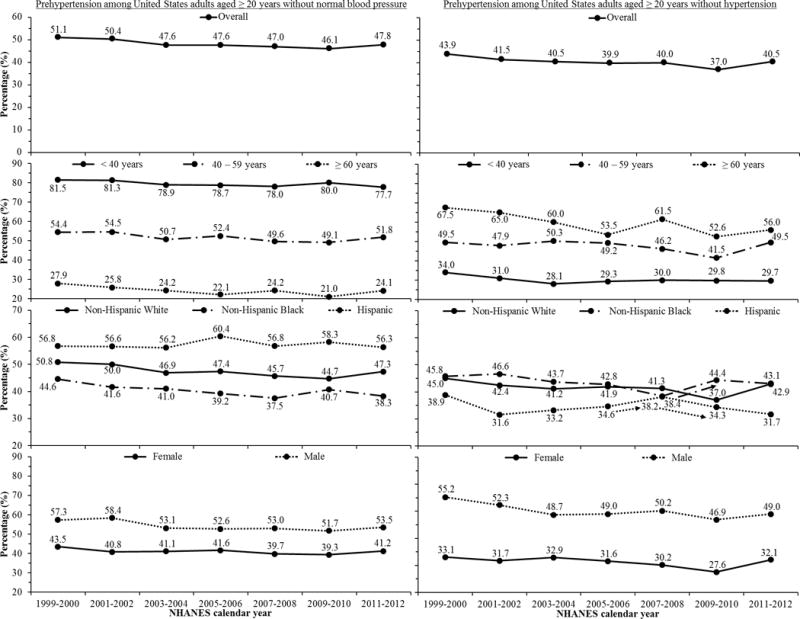
Age-adjusted percentage of United States adults aged ≥ 20 years with prehypertension in US adults without normal blood pressure (left column) and without hypertension (right column) by National Health and Nutrition Examination Survey (NHANES) calendar year overall and by age, race/ethnicity and sex.
Arrows indicate the prevalence corresponding with Non-Hispanic Whites, Non-Hispanic Blacks or Hispanics where the plotted values for these race/ethnic groups are difficult to distinguish.
The 95% confidence interval corresponding with each point estimate, p-trend representing the change in the prevalence over calendar period and the p-interaction representing differences in the change in the prevalence over calendar period across age, race/ethnicity and sex sub-groups is reported in Table S2.
Among US adults without normal BP, there was a non-statistically significant decrease in the prevalence ratio of prehypertension between 1999–2000 and 2011–2012 after adjustment for age, race/ethnicity and sex (Table 1, top panel). There was no trend in the prevalence ratios for prehypertension after further adjustment for risk factors for incident hypertension, CVD and target-organ damage and modifiable lifestyle risk factors. The prevalence ratio for prehypertension decreased over calendar time among US adults without hypertension (Table 1, bottom panel).
Table 1.
Multivariable adjusted prevalence ratio for prehypertension among United States Adults aged ≥ 20 years without normal blood pressure (top panel) and without hypertension (bottom panel) by National Health and Nutrition Examination Survey (NHANES) calendar year.
| Model | National Health and Nutrition Examination Survey calendar year | |||||||
|---|---|---|---|---|---|---|---|---|
| 1999–2000 | 2001–2002 | 2003–2004 | 2005–2006 | 2007–2008 | 2009–2010 | 2011–2012 | p–trend* | |
| Prevalence ratio (95% confidence interval) | ||||||||
| Prehypertension among United States adults aged ≥ 20 years without normal blood pressure | ||||||||
| Model 1 | 1 (reference) |
0.99 (0.91,1.09) |
0.95 (0.86,1.04) |
0.95 (0.86,1.04) |
0.93 (0.85,1.01) |
0.92 (0.83,1.01) |
0.95 (0.87,1.05) |
0.052 |
| Model 2 | 1 (reference) |
1.00 (0.91,1.09) |
0.94 (0.86,1.02) |
0.95 (0.87,1.03) |
0.94 (0.87,1.01) |
0.92 (0.84,1.00) |
0.96 (0.88,1.05) |
0.087 |
| Model 3 | 1 (reference) |
1.01 (0.93,1.10) |
0.94 (0.87,1.03) |
0.97 (0.89,1.06) |
0.95 (0.88,1.03) |
0.96 (0.87,1.06) |
0.99 (0.91,1.08) |
0.474 |
| Model 4 | 1 (reference) |
1.02 (0.93,1.10) |
0.95 (0.88,1.03) |
0.98 (0.90,1.07) |
0.95 (0.88,1.03) |
0.98 (0.89,1.07) |
1.00 (0.91,1.10) |
0.678 |
| Prehypertension among United States adults aged ≥ 20 years without hypertension | ||||||||
| Model 1 | 1 (reference) |
0.94 (0.84,1.05) |
0.91 (0.82,1.03) |
0.91 (0.80,1.03) |
0.91 (0.81,1.02) |
0.84 (0.75,0.94) |
0.92 (0.82,1.03) |
0.032 |
| Model 2 | 1 (reference) |
0.92 (0.83,1.02) |
0.89 (0.79,1.00) |
0.90 (0.80,1.03) |
0.89 (0.80,0.99) |
0.84 (0.75,0.94) |
0.92 (0.82,1.04) |
0.072 |
| Model 3 | 1 (reference) |
0.93 (0.84,1.03) |
0.88 (0.78,0.99) |
0.88 (0.77,1.00) |
0.85 (0.76,0.95) |
0.80 (0.71,0.90) |
0.90 (0.80,1.01) |
0.005 |
| Model 4 | 1 (reference) |
0.91 (0.82,1.01) |
0.84 (0.74,0.96) |
0.86 (0.75,0.99) |
0.83 (0.75,0.93) |
0.79 (0.70,0.88) |
0.89 (0.78,1.01) |
0.009 |
Numbers in the table are prevalence ratio (95% confidence interval).
Model 1: Adjustment for age, race/ethnicity and sex.
Model 2: Adjustment for the variables in Model 1 plus risk factors for incident hypertension, cardiovascular disease and target-organ damage (i.e., heart rate, total cholesterol, high density lipoprotein cholesterol, diabetes, estimated glomerular filtration rate, urinary albumin to creatinine ratio and 10-year predicted atherosclerotic cardiovascular disease risk).
Model 3: Adjustment for the variables in Model 1 plus modifiable lifestyle risk factors (i.e., body mass index, smoking status, physical activity level, alcohol consumption and Dietary Approaches to Stop Hypertension adherence).
Model 4: Adjustment for the variables in Model 1, Model 2 and Model 3.
Normal blood pressure: systolic blood pressure < 120 mmHg and diastolic blood pressure < 80 mmHg without antihypertensive medication use.
Prehypertension: systolic blood pressure 120–139 mmHg with diastolic blood pressure < 90 mmHg or diastolic blood pressure 80–89 mmHg with systolic blood pressure < 140 mmHg without antihypertensive medication use.
Hypertension: systolic blood pressure ≥ 140 mmHg or diastolic blood pressure ≥ 90 mmHg and/or antihypertensive medication use.
P-trend: statistical significance of the trend in the change of the prevalence ratio over calendar period.
Prevalence of prehypertension and hypertension in subgroups of US adults
In 2009–2012, after race-ethnicity and sex adjustment, US adults <40 and 40–59 versus ≥60 years old were less likely to have prehypertension or hypertension versus normal BP (Table S3, middle column). After age and sex adjustment, the prevalence ratio for prehypertension or hypertension versus normal BP was higher for non-Hispanic blacks versus non-Hispanic whites. After age and race-ethnicity adjustment, females were less likely to have prehypertension or hypertension compared with males. Among adults without hypertension and after race/ethnicity and sex adjustment, US adults 40 to 59 and ≥ 60 years of age were less likely than their counterparts < 40 years of age to have prehypertension (Table S3, right column). Also, non-Hispanic blacks were more likely than non-Hispanic whites and females were less likely than males to have prehypertension.
Modifiable risk factors among adults with prehypertension
Among US adults with prehypertension, mean heart rate and the prevalence of prediabetes and diabetes increased and elevated total cholesterol decreased between 1999–2000 and 2011–2012 (Table 2). Also, while the proportion of adults who were overweight or obese increased, DASH diet adherence decreased during the study period (Table 3). There was also a non-statistically significant increase in poor levels of leisure-time physical activity among adults with prehypertension. In contrast, the prevalence of current smoking declined from 25.9% to 23.2% (p-trend=0.097). Heavy alcohol intake did not change over time.
Table 2.
Risk factors for incident hypertension, cardiovascular disease and target organ damage among United States adults aged ≥ 20 years with prehypertension by calendar year.
| Risk factor | Risk factors for incident hypertension, cardiovascular disease and target organ damage | |||||||
|---|---|---|---|---|---|---|---|---|
| National Health and Nutrition Examination Survey calendar year | ||||||||
| 1999–2000 | 2001–2002 | 2003–2004 | 2005–2006 | 2007–2008 | 2009–2010 | 2011–2012 | p-trend* | |
| Mean heart rate, beats per minute | 71.3 (70.5, 72.1) | 72.9 (71.8, 74.0) | 73.2 (71.8, 74.6) | 72.6 (71.5, 73.6) | 74.2 (73.0, 75.4) | 73.0 (72.1, 73.9) | 73.5 (72.3, 74.7) | 0.003 |
| Systolic blood pressure, mm Hg | ||||||||
| 120 – 129 | 70.0 (64.2, 75.8) | 66.2 (62.9, 69.4) | 66.7 (62.8, 70.7) | 66.3 (63.1, 69.5) | 71.8 (69.2, 74.5) | 71.2 (68.2, 74.3) | 68.7 (64.5, 72.8) | 0.219 |
| 130 – 139 | 30.0 (24.2, 35.8) | 33.8 (30.6, 37.1) | 33.3 (29.3, 37.2) | 33.7 (30.5, 36.9) | 28.2 (25.5, 30.8) | 28.8 (25.7, 31.8) | 31.3 (27.2, 35.5) | |
| Diastolic blood pressure, mm Hg | ||||||||
| 80 – 84 | 73.3 (66.9, 79.7) | 70.2 (65.5, 75.0) | 67.9 (57.8, 78.0) | 70.4 (63.8, 77.0) | 78.9 (75.3, 82.6) | 71.0 (64.9, 77.2) | 67.6 (60.6, 74.5) | 0.715 |
| 85 – 89 | 26.7 (20.3, 33.1) | 29.8 (25.0, 34.5) | 32.1 (22.0, 42.2) | 29.6 (23.0, 36.2) | 21.1 (17.4, 24.7) | 29.0 (22.8, 35.1) | 32.4 (25.5, 39.4) | |
| Total cholesterol | ||||||||
| Normal (< 200 mg/dL) | 44.7 (40.4, 49.0) | 47.1 (44.9, 49.4) | 47.7 (44.0, 51.3) | 49.6 (46.0, 53.2) | 49.0 (44.3, 53.8) | 50.2 (46.5, 53.8) | 48.9 (44.7, 53.0) | 0.018 |
| Borderline elevated (200 – 239 mg/dL) | 37.0 (32.0, 41.9) | 34.2 (30.8, 37.5) | 32.3 (28.4, 36.1) | 32.7 (29.1, 36.4) | 32.0 (27.1, 36.9) | 34.2 (31.7, 36.7) | 36.4 (33.2, 39.7) | |
| Elevated (≥ 240 mg/dL) | 18.4 (13.7, 23.0) | 18.7 (15.0, 22.4) | 20.0 (15.5, 24.6) | 17.7 (14.6, 20.7) | 19.0 (14.6, 23.4) | 15.6 (12.9, 18.4) | 14.7 (11.2, 18.3) | |
| High-density lipoprotein cholesterol | ||||||||
| Normal (men: ≥ 40; women: ≥ 50, mg/dL) | 63.8 (60.0, 67.7) | 69.5 (65.8, 73.3) | 70.1 (64.7, 75.5) | 72.8 (69.7, 75.9) | 65.2 (59.5, 70.9) | 68.6 (65.6, 71.5) | 71.7 (65.4, 78.1) | 0.220 |
| Low (men: < 40; women: < 50, mg/dL) | 36.2 (32.3, 40.0) | 30.5 (26.7, 34.2) | 29.9 (24.5, 35.3) | 27.2 (24.1, 30.3) | 34.8 (29.1, 40.5) | 31.4 (28.5, 34.4) | 28.3 (21.9, 34.6) | |
| C-reactive protein | ||||||||
| Normal (< 1.0 mg/L) | 90.2 (87.4, 93.1) | 91.8 (89.4, 94.2) | 91.6 (89.1, 94.2) | 90.0 (87.6, 92.4) | 91.9 (90.0, 93.7) | 92.9 (91.2, 94.5) | NR | |
| Borderline elevated (1.0 – 2.9 mg/L) | 8.8 (5.4, 12.3) | 7.0 (4.5, 9.4) | 6.7 (4.2, 9.2) | 8.2 (5.9, 10.5) | 7.3 (5.8, 8.7) | 6.2 (4.8, 7.6) | NR | 0.162 |
| Elevated (≥ 3.0 mg/L) | 0.9 (0.0, 1.8) | 1.2 (0.5, 2.0) | 1.7 (0.6, 2.8) | 1.8 (0.7, 2.8) | 0.9 (0.3, 1.4) | 0.9 (0.4, 1.5) | NR | |
| Diabetes status | ||||||||
| No diabetes | 84.4 (80.4, 88.4) | 82.1 (79.0, 85.1) | 81.9 (78.9, 84.9) | 79.3 (74.4, 84.1) | 70.5 (65.7, 75.3) | 69.4 (66.0, 72.8) | 69.9 (67.8, 72) | <0.001 |
| Pre-diabetes | 9.6 (7.1, 12.1) | 11.2 (8.4, 14.0) | 12.9 (10.3, 15.6) | 13.8 (9.9, 17.7) | 21.3 (17.0, 25.5) | 24.1 (21.1, 27.0) | 21.6 (19.6, 23.5) | |
| Diabetes | 6.0 (4.0, 7.9) | 6.7 (4.8, 8.7) | 5.2 (3.9, 6.4) | 7.0 (4.7, 9.2) | 8.3 (6.6, 9.9) | 6.5 (5.2, 7.8) | 8.5 (7.0, 10.0) | |
| Estimated glomerular filtration rate | ||||||||
| Normal (≥ 60 ml/min/1.73m2) | 97.2 (96.2, 98.2) | 97.5 (96.3, 98.6) | 96.9 (95.7, 98.0) | 96.4 (94.9, 97.8) | 96.8 (95.4, 98.2) | 97.4 (96.2, 98.6) | 97.5 (96.5, 98.5) | 0.525 |
| Reduced (< 60 ml/min/1.73m2) | 2.8 (1.8, 3.8) | 2.5 (1.4, 3.7) | 3.1 (2.0, 4.3) | 3.6 (2.2, 5.1) | 3.2 (1.8, 4.6) | 2.6 (1.4, 3.8) | 2.5 (1.5, 3.5) | |
| Urinary albumin to creatinine ratio | ||||||||
| Normal (≤ 30 mg/g) | 92.6 (90.4, 94.8) | 92.7 (90.7, 94.7) | 93.3 (91.1, 95.5) | 93.9 (92.0, 95.7) | 91.6 (89.2, 94) | 95.0 (93.5, 96.4) | 91.9 (89.5, 94.4) | 0.938 |
| Elevated (> 30 mg/g) | 7.4 (5.2, 9.6) | 7.3 (5.3, 9.3) | 6.7 (4.5, 8.9) | 6.1 (4.3, 8.0) | 8.4 (6.0, 10.8) | 5.0 (3.6, 6.5) | 8.1 (5.6, 10.5) | |
| 10-year predicted ASCVD risk | ||||||||
| < 7.5% | 64.9 (59.7, 70.1) | 63.1 (58.2, 68.1) | 64.2 (60.8, 67.6) | 65.5 (59.3, 71.7) | 61.6 (58.2, 65) | 66.7 (64.5, 68.9) | 66.2 (60.3, 72.1) | 0.343 |
| ≥ 7.5% | 35.1 (29.9, 40.3) | 36.9 (31.9, 41.8) | 35.8 (32.4, 39.2) | 34.5 (28.3, 40.7) | 38.4 (35.0, 41.8) | 33.3 (31.1, 35.5) | 33.8 (27.9, 39.7) | |
Numbers in the table are mean (95% confidence interval) or percentage (95% confidence interval).
ASCVD: atherosclerotic cardiovascular disease.
NR: Not reported due to data not being available at the time of analyses.
Standard International System conversion factors: To convert mg/dL to mmol/L, multiply values by 0.0259. To convert mg/L to mmol/L, multiply values by 5.581.
P-trend: statistical significance of the trend in the change of the prevalence over calendar period.
Table 3.
Modifiable lifestyle risk factors for incident hypertension among United States adults aged ≥ 20 years with prehypertension by calendar year.
| Modifiable lifestyle risk factor | Modifiable lifestyle risk factors for incident hypertension | |||||||
|---|---|---|---|---|---|---|---|---|
| National Health and Nutrition Examination Survey calendar year | p-trend† | |||||||
| 1999–2000 | 2001–2002 | 2003–2004 | 2005–2006 | 2007–2008 | 2009–2010 | 2011–2012 | ||
| Body mass index categories | ||||||||
| Normal (< 25 kg/m2) | 35.8 (32.2, 39.5) | 31.7 (28.8, 34.6) | 27.6 (23.2, 32.0) | 28.8 (23.5, 31.7) | 28.4 (24.1, 32.8) | 26.2 (21.4, 31.0) | 27.5 (22.9, 32.2) | <0.001 |
| Overweight (25 – 30 kg/m2) | 33.5 (29.4, 37.7) | 37.9 (34.3, 41.5) | 39.3 (34.2, 44.4) | 32.7 (30.3, 35.1) | 37.4 (34.4, 40.4) | 34.3 (29.9, 38.7) | 37.3 (31.2, 43.4) | |
| Obese (≥ 30 kg/m2) | 30.6 (26.4, 34.8) | 30.3 (25.7, 35.0) | 33.1 (29.2, 37.0) | 38.4 (34.4, 42.5) | 34.2 (30.2, 38.2) | 39.5 (35.5, 43.4) | 35.2 (31.7, 38.7) | |
| Smoking status | ||||||||
| Current | 25.9 (22.5, 29.3) | 26.8 (23.6, 29.9) | 27.5 (24.6, 30.5) | 24.7 (21.2, 28.3) | 25.7 (21.7, 29.8) | 21.4 (19.1, 23.6) | 23.2 (20.1, 26.2) | 0.097 |
| Former / never | 74.1 (70.7, 77.5) | 73.2 (70.1, 76.4) | 72.5 (69.5, 75.4) | 75.3 (71.7, 78.8) | 74.3 (70.2, 78.3) | 78.6 (76.4, 80.9) | 76.8 (73.8, 79.9) | |
| Physical activity (leisure-time) | ||||||||
| Ideal | 38.1 (33.5, 42.7) | 44.8 (41.3, 48.4) | 39.8 (37.1, 42.4) | 41.4 (38.0, 44.8) | 35.7 (30.5, 40.9) | 37.9 (33.7, 42.1) | 39.6 (34.6, 44.6) | 0.127 |
| Intermediate | 21.9 (17.0, 26.9) | 24.1 (21.6, 26.7) | 30.6 (27.6, 33.6) | 26.5 (22.3, 30.8) | 20.0 (17.0, 23.0) | 16.3 (14.3, 18.2) | 16.5 (14.1, 18.8) | |
| Poor | 40.0 (35.9, 44.1) | 31.0 (27.1, 34.9) | 29.6 (26.3, 33.9) | 32.0 (27.0, 37.1) | 44.3 (38.1, 50.5) | 45.8 (41.1, 50.5) | 43.9 (38.7, 49.1) | |
| Alcohol consumption* | ||||||||
| None | 11.8 (8.2, 15.4) | 14.6 (7.8, 21.4) | 11.5 (9.0, 14.0) | 10.7 (5.8, 15.7) | 11.6 (9.4, 13.8) | 11.1 (8.5, 13.6) | 10.6 (7.8, 13.4) | 0.393 |
| Moderate | 76.6 (73.3, 80.0) | 72.9 (66.4, 79.3) | 77.5 (74.8, 80.2) | 76.9 (71.5, 82.2) | 75.2 (72.5, 77.8) | 77.1 (73.3, 80.8) | 77.0 (73.1, 80.9) | |
| Heavy | 11.6 (9.2, 14.0) | 12.5 (10.9, 14.1) | 11.0 (8.3, 13.7) | 12.4 (9.8, 15.0) | 13.2 (10.9, 15.6) | 11.9 (9.8, 14.0) | 12.4 (8.8, 16.0) | |
| DASH diet adherence categories | ||||||||
| Quartile 1 (low, less healthy) | 38.2 (33.7, 42.8) | 37.7 (32.8, 42.6) | 31.7 (27.8, 35.5) | 43.6 (38.0, 49.1) | 39.0 (34.0, 44.0) | 43.7 (39.8, 47.7) | 41.6 (35.1, 48.1) | 0.007 |
| Quartile 2 | 25.3 (21.6, 29.0) | 23.3 (20.4, 26.2) | 24.2 (21.1, 27.4) | 28.2 (24.6, 31.8) | 28.5 (25.0, 31.8) | 25.8 (22.0, 29.5) | 26.5 (22.2, 30.8) | |
| Quartile 3 | 18.1 (15.0, 21.1) | 19.8 (16.6, 23.0) | 24.9 (21.5, 28.3) | 17.1 (14.8, 19.4) | 18.7 (16.1, 21.2) | 19.5 (17.3, 21.8) | 20.0 (16.8, 23.1) | |
| Quartile 4 (high, healthier) | 18.4 (16.2, 20.5) | 19.3 (16.9, 21.6) | 19.2 (17.0, 21.3) | 11.1 (7.9, 14.4) | 13.9 (10.9, 16.8) | 10.9 (8.9, 13.0) | 11.9 (8.5, 15.4) | |
Numbers in the table are percentage (95% confidence interval).
DASH: Dietary Approaches to Stop Hypertension. The cut-points for the DASH diet scores used to group participants into quartiles based on the distribution among US adults ≥ 20 years old were (quartile 1 [least healthy] to quartile 4 [healthiest]): < 25, 25 to < 28, 28 to < 31 and ≥ 31).
Alcohol consumption: None: 0 drinks per week; Moderate: > 0 to < 8 drinks per week for women and > 0 and < 15 drinks per week for men; Heavy: ≥ 8 drinks per week for women and ≥ 15 drinks per week for men.
P-trend: statistical significance of the trend in the change of the prevalence over calendar period.
DISCUSSION
Between 1999–2000 and 2011–2012, there was a statistically significant decrease in the age-adjusted prevalence of prehypertension and non-statistically significant increase in normal BP and hypertension. The number of US adults with prehypertension remained stable, whereas the number with normal BP and hypertension increased during this time period due to population growth. The prevalence of normal BP increased in those aged ≥60 years, prehypertension decreased in those aged ≥60 years, non-Hispanic whites, non-Hispanic blacks and males and hypertension increased in non-Hispanic whites, non-Hispanic blacks and males. Also, among adults with prehypertension, mean heart rate and the proportion with pre-diabetes and diabetes and were overweight and obese increased between 1999–2000 and 2011–2012. In contrast, adherence to the DASH diet eating pattern decreased over this time period. There was a non-statistically significant increase in poor levels of leisure-time physical activity and a non-statistically significant decrease in current smoking over time.
Temporal changes in the proportion of US adults with hypertension have been studied more often than prehypertension. NHANES data indicate the age-adjusted prevalence of hypertension increased from 23.9% (95% CI: 22.7%–25.2%) in 1988–1994 to 28.5% (95% CI: 25.9%–31.3%) in 1999–2000 and remained stable through 2007–2008 at 29.5% (95% CI: 27.6%–30.5%).24 The results reported herein also indicate that the prevalence of hypertension has not changed substantially since 1999–2000. As hypertension is a life-long condition, reducing the prevalence of hypertension will require interventions to prevent its development.
A study from 1939 described SBP levels between 120 mmHg and 139 mmHg as the “danger zone” for progressing to incident hypertension and CVD in younger individuals.25 The goal of the JNC7 for defining prehypertension was to increase awareness so that individuals with this condition can delay or prevent incident hypertension through early adoption of healthy lifestyle interventions that lower BP levels and reduce CVD risk.1 The range of BP levels used to define prehypertension was determined from accumulating evidence indicating that these levels were associated with traditional CVD risk factors (e.g., obesity, diabetes), incident hypertension and cardiovascular morbidity and mortality.1, 7, 26–30
While evidence from randomized controlled trials (RCTs) indicates prophylactic antihypertensive medication reduces BP and the incidence of hypertension, the JNC7 emphasized utilization of healthy lifestyles for individuals with prehypertension.1, 31, 32 The Trials of Hypertension Prevention (TOHP) reported that a mean 7.7 pounds difference in weight loss over 18 months in the active intervention (i.e., weight loss counseling) versus control group resulted in 5.8/3.2 mmHg lower SBP/DBP levels.33 A meta-analysis of 27 RCTs demonstrated that participants randomized to aerobic exercise had a 4.0 (95% CI: 2.75–5.32) mmHg reduction in SBP compared to their counterparts randomized to control groups, independent of the exercise intensity level.34 RCTs also provide evidence that a diet low in sodium, high in potassium and rich with fruits and vegetables and reduced saturated and total fat from dairy products can reduce SBP.35, 36 For example, randomization to the DASH with a low sodium level compared with a control diet with comparatively higher amounts of sodium reduced SBP by 7.1 mmHg in adults without hypertension.35 Furthermore, in a meta-analysis of 6 RCTs, reducing alcohol intake in adults without hypertension by 75% to 100% compared to baseline has been demonstrated to lower SBP by 3.6 (95% CI: 2.5–4.6) mmHg and DBP by 1.8 (95% CI: 0.6–3.0) mmHg.37 While each of these interventions is beneficial for reducing BP, the PREMIER and Multiple Risk Factor Intervention Trial (MRFIT) RCTs provided evidence of an additive effect of increasing the number of lifestyle interventions to lower BP levels.6, 38, 39 In the current analysis, many US adults with prehypertension had risk factors for incident hypertension, target-organ damage and CVD and were not using lifestyle interventions. Importantly, low-cost interventions for preventing hypertension are proven in all age groups, race/ethnicities and males and females.6 This indicates there is a substantial opportunity to lower the incidence of hypertension and CVD through lifestyle changes. However, novel approaches for maintaining lifestyle modification may be needed since BMI and diabetes increased and there was a decline in adherence to the DASH diet between 1999–2000 and 2011–2012.
Few studies have reported the number of US adults with normal BP, prehypertension and hypertension over time. In the current study, the percentage of US adults with normal BP and hypertension was stable and the proportion who had prehypertension increased between 1999–2000 and 2011–2012. However, the number of US adults with normal BP and hypertension increased and the number with prehypertension was stable during the time period. This suggests that the population growth has been primarily among US adults with normal BP and hypertension rather than with prehypertension.
The current study has several strengths. These include the complex sampling design of NHANES that permitted the calculation of prevalence estimates for the US population. The large sample size of NHANES facilitated subgroup analyses. Also, NHANES follows protocols which facilitate the rigorous collection of study data including BP. However, the results should be interpreted in the context of known and potential limitations. Mean BP levels were calculated from measurements at a single examination. Average BP measured at multiple exams would provide more accurate information to categorize participants by their BP level. Participants in NHANES were not followed longitudinally which prevented the assessment of within-person changes in BP levels, risk factors for incident hypertension, target-organ damage and CVD and modifiable lifestyle risk factors at the individual level. Data for Asian adults, separately from other race-ethnicity groups, were not available for the NHANES calendar years of 1999–2000 through 2009–2010 and temporal changes could not be reported for this sub-group.
PERSPECTIVES
The current serial cross-sectional analysis of NHANES data reports that the age-adjusted prevalence of prehypertension decreased among US adults between 1999–2000 and 2011–2012. During this time period, the age-adjusted proportion of US adults with normal BP and hypertension remained stable. Also, there has been limited improvement in risk factors for incident hypertension, target-organ damage and CVD and modifiable lifestyle risk factors in adults with prehypertension since the JNC7 characterized individuals with prehypertension as having an increased risk for transitioning to hypertension. Population-level approaches that improve CVD and lifestyle risk factors may help lower the risk for hypertension among US adults with prehypertension.
Supplementary Material
Novelty and Significance.
1) What Is New?
-
-
Between 1999–2000 and 2011–2012, the age-adjusted prevalence of prehypertension decreased.
-
-
In 2011–2012, after adjustment for age, 28.2% of US adults had prehypertension.
-
-
Among adults with prehypertension, prediabetes, diabetes, overweight and obesity increased and Dietary Approaches to Stop Hypertension adherence decreased.
-
-
Also, there was a non-statistically significant increase in no physical activity each week, non-statistically significant decrease in current smoking and alcohol consumption did not change among adults with prehypertension.
2) What is Relevant?
-
-
Population-level approaches directed at adults with prehypertension should focus on improving risk factors to prevent hypertension and cardiovascular disease.
3) Summary
-
-
The prevalence of prehypertension is high among US adults and many adults with prehypertension have poor levels of many modifiable risk factors for incident hypertension and cardiovascular disease.
Acknowledgments
Study conception and design: JNBIII, PM, BE; Acquisition, analysis or interpretation of data: JNBIII, JL, LZ, LC, PM, BE; Statistical analysis: JL, LZ, LC, BE; Drafting of the manuscript: JNBIII, PM; Critical revision of the manuscript: JNBIII, JL, LZ, LC, PM, BE. JL, JC and BE had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Funding Sources: This work was partially supported by F31 HL129701 from the National Heart Lung and Blood Institute (PI: JNBIII) at the National Institutes of Health (NIH). The contents are solely the responsibility of the authors and do not necessarily represent the official view of NIH. PM was supported by grant 15SFRN2390002 from the American Heart Association.
Footnotes
Conflicts of Interest / Disclosures: JNBIII: None; JL: None; LZ: None; LC: None; PM: receives an institutional grant from Amgen Inc that is not related to the current project; BE has received income as a consultant from AstraZeneca, Inside Edge, Medtronic and Valencia and as a speaker from Merck Sorono, research support from Boehringer, and royalties from UpToDate, all of which are unrelated to the current project.
References
- 1.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jr, Jones DW, Materson BJ, Oparil S, Wright JT, Jr, Roccella EJ, National Heart L, Blood Institute Joint National Committee on Prevention DE, Treatment of High Blood P, National High Blood Pressure Education Program Coordinating C The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure: The jnc 7 report. JAMA: The Journal of the American Medical Association. 2003;289:2560–2572. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- 2.Vasan RS, Larson MG, Leip EP, Evans JC, O’Donnell CJ, Kannel WB, Levy D. Impact of high-normal blood pressure on the risk of cardiovascular disease. The New England Journal of Medicine. 2001;345:1291–1297. doi: 10.1056/NEJMoa003417. [DOI] [PubMed] [Google Scholar]
- 3.Muntner P, Woodward M, Mann DM, Shimbo D, Michos ED, Blumenthal RS, Carson AP, Chen H, Arnett DK. Comparison of the framingham heart study hypertension model with blood pressure alone in the prediction of risk of hypertension: The multi-ethnic study of atherosclerosis. Hypertension. 2010;55:1339–1345. doi: 10.1161/HYPERTENSIONAHA.109.149609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Selassie A, Wagner CS, Laken ML, Ferguson ML, Ferdinand KC, Egan BM. Progression is accelerated from prehypertension to hypertension in blacks. Hypertension. 2011;58:579–587. doi: 10.1161/HYPERTENSIONAHA.111.177410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Egan BM, Stevens-Fabry S. Prehypertension–prevalence, health risks, and management strategies. Nature Reviews Cardiology. 2015;12:289–300. doi: 10.1038/nrcardio.2015.17. [DOI] [PubMed] [Google Scholar]
- 6.Whelton PK, He J, Appel LJ, Cutler JA, Havas S, Kotchen TA, Roccella EJ, Stout R, Vallbona C, Winston MC, Karimbakas J, National High Blood Pressure Education Program Coordinating C Primary prevention of hypertension: Clinical and public health advisory from the national high blood pressure education program. JAMA: The Journal of the American Medical Association. 2002;288:1882–1888. doi: 10.1001/jama.288.15.1882. [DOI] [PubMed] [Google Scholar]
- 7.Pimenta E, Oparil S. Prehypertension: Epidemiology, consequences and treatment. Nature Reviews Nephrology. 2010;6:21–30. doi: 10.1038/nrneph.2009.191. [DOI] [PubMed] [Google Scholar]
- 8.Ostchega Y, Yoon SS, Hughes J, Louis T. Hypertension awareness, treatment, and control–continued disparities in adults: United states, 2005–2006. NCHS Data Brief. 2008:1–8. [PubMed] [Google Scholar]
- 9.Wang Y, Wang QJ. The prevalence of prehypertension and hypertension among us adults according to the new joint national committee guidelines: New challenges of the old problem. Archives of Internal Medicine. 2004;164:2126–2134. doi: 10.1001/archinte.164.19.2126. [DOI] [PubMed] [Google Scholar]
- 10.Gupta AK, McGlone M, Greenway FL, Johnson WD. Prehypertension in disease-free adults: A marker for an adverse cardiometabolic risk profile. Hypertension Research: Official Journal of the Japanese Society of Hypertension. 2010;33:905–910. doi: 10.1038/hr.2010.91. [DOI] [PubMed] [Google Scholar]
- 11.Mozaffarian D, Benjamin EJ, Go AS, et al. Heart disease and stroke statistics–2015 update: A report from the american heart association. Circulation. 2015;131:e29–322. doi: 10.1161/CIR.0000000000000152. [DOI] [PubMed] [Google Scholar]
- 12.Echouffo-Tcheugui JB, Batty GD, Kivimaki M, Kengne AP. Risk models to predict hypertension: A systematic review. PloS One. 2013;8:e67370. doi: 10.1371/journal.pone.0067370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Centers for disease control and prevention (cdc) National center for health statistics (nchs) National health and nutrition examination survey questionnaire, examination protocol and laboratory protocol. 1999–2012 [Google Scholar]
- 14.Centers for disease control and prevention (cdc) National center for health statistics (nchs) National health and nutrition examination survey data. 1999–2012 [Google Scholar]
- 15.Selvin E, Manzi J, Stevens LA, Van Lente F, Lacher DA, Levey AS, Coresh J. Calibration of serum creatinine in the national health and nutrition examination surveys (nhanes) 1988–1994, 1999–2004. American Journal of Kidney Diseases: The Official Journal of the National Kidney Foundation. 2007;50:918–926. doi: 10.1053/j.ajkd.2007.08.020. [DOI] [PubMed] [Google Scholar]
- 16.Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF, 3rd, Feldman HI, Kusek JW, Eggers P, Van Lente F, Greene T, Coresh J, Ckd EPI. A new equation to estimate glomerular filtration rate. Annals of Internal Medicine. 2009;150:604–612. doi: 10.7326/0003-4819-150-9-200905050-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Goff DC, Jr, Lloyd-Jones DM, Bennett G, et al. 2013 acc/aha guideline on the assessment of cardiovascular risk: A report of the american college of cardiology/american heart association task force on practice guidelines. Circulation. 2014;129:S49–73. doi: 10.1161/01.cir.0000437741.48606.98. [DOI] [PubMed] [Google Scholar]
- 18.Ladabaum U, Mannalithara A, Myer PA, Singh G. Obesity, abdominal obesity, physical activity, and caloric intake in us adults: 1988 to 2010. The American Journal of Medicine. 2014;127:717–727.e712. doi: 10.1016/j.amjmed.2014.02.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fung TT, Hu FB, Wu K, Chiuve SE, Fuchs CS, Giovannucci E. The mediterranean and dietary approaches to stop hypertension (dash) diets and colorectal cancer. The American Journal of Clinical Nutrition. 2010;92:1429–1435. doi: 10.3945/ajcn.2010.29242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gunther AL, Liese AD, Bell RA, Dabelea D, Lawrence JM, Rodriguez BL, Standiford DA, Mayer-Davis EJ. Association between the dietary approaches to hypertension diet and hypertension in youth with diabetes mellitus. Hypertension. 2009;53:6–12. doi: 10.1161/HYPERTENSIONAHA.108.116665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Perloff D, Grim C, Flack J, Frohlich ED, Hill M, McDonald M, Morgenstern BZ. Human blood pressure determination by sphygmomanometry. Circulation. 1993;88:2460–2470. doi: 10.1161/01.cir.88.5.2460. [DOI] [PubMed] [Google Scholar]
- 22.Pickering TG, Hall JE, Appel LJ, Falkner BE, Graves J, Hill MN, Jones DW, Kurtz T, Sheps SG, Roccella EJ, Subcommittee of P, Public Education of the American Heart Association Council on High Blood Pressure R Recommendations for blood pressure measurement in humans and experimental animals: Part 1: Blood pressure measurement in humans: A statement for professionals from the subcommittee of professional and public education of the american heart association council on high blood pressure research. Hypertension. 2005;45:142–161. doi: 10.1161/01.HYP.0000150859.47929.8e. [DOI] [PubMed] [Google Scholar]
- 23.Egan BM, Li J, Hutchison FN, Ferdinand KC. Hypertension in the united states, 1999 to 2012: Progress toward healthy people 2020 goals. Circulation. 2014;130:1692–1699. doi: 10.1161/CIRCULATIONAHA.114.010676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Egan BM, Zhao Y, Axon RN. Us trends in prevalence, awareness, treatment, and control of hypertension, 1988–2008. JAMA: The Journal of the American Medical Association. 2010;303:2043–2050. doi: 10.1001/jama.2010.650. [DOI] [PubMed] [Google Scholar]
- 25.Robinson SC, Brucer M. Range of normal blood pressure: A statistical and clinical study of 11,383 persons. Archives of Internal Medicine. 1939;64:409–444. [Google Scholar]
- 26.Vasan RS, Larson MG, Leip EP, Kannel WB, Levy D. Assessment of frequency of progression to hypertension in non-hypertensive participants in the framingham heart study: A cohort study. Lancet. 2001;358:1682–1686. doi: 10.1016/S0140-6736(01)06710-1. [DOI] [PubMed] [Google Scholar]
- 27.Vasan RS, Beiser A, Seshadri S, Larson MG, Kannel WB, D’Agostino RB, Levy D. Residual lifetime risk for developing hypertension in middle-aged women and men: The framingham heart study. JAMA: The Journal of the American Medical Association. 2002;287:1003–1010. doi: 10.1001/jama.287.8.1003. [DOI] [PubMed] [Google Scholar]
- 28.De Marco M, de Simone G, Roman MJ, Chinali M, Lee ET, Russell M, Howard BV, Devereux RB. Cardiovascular and metabolic predictors of progression of prehypertension into hypertension: The strong heart study. Hypertension. 2009;54:974–980. doi: 10.1161/HYPERTENSIONAHA.109.129031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lewington S, Clarke R, Qizilbash N, Peto R, Collins R, Prospective Studies C. Age-specific relevance of usual blood pressure to vascular mortality: A meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360:1903–1913. doi: 10.1016/s0140-6736(02)11911-8. [DOI] [PubMed] [Google Scholar]
- 30.Dyer AR, Liu K, Walsh M, Kiefe C, Jacobs DR, Jr, Bild DE. Ten-year incidence of elevated blood pressure and its predictors: The cardia study. Coronary artery risk development in (young) adults. Journal of Human Hypertension. 1999;13:13–21. doi: 10.1038/sj.jhh.1000740. [DOI] [PubMed] [Google Scholar]
- 31.Julius S, Kaciroti N, Egan BM, Nesbitt S, Michelson EL, Trial of Preventing Hypertension I Trophy study: Outcomes based on the seventh report of the joint national committee on hypertension definition of hypertension. Journal of the American Society of Hypertension: JASH. 2008;2:39–43. doi: 10.1016/j.jash.2007.07.005. [DOI] [PubMed] [Google Scholar]
- 32.Luders S, Schrader J, Berger J, Unger T, Zidek W, Bohm M, Middeke M, Motz W, Lubcke C, Gansz A, Brokamp L, Schmieder RE, Trenkwalder P, Haller H, Dominiak P, Group PS The pharao study: Prevention of hypertension with the angiotensin-converting enzyme inhibitor ramipril in patients with high-normal blood pressure: A prospective, randomized, controlled prevention trial of the german hypertension league. Journal of Hypertension. 2008;26:1487–1496. doi: 10.1097/HJH.0b013e3282ff8864. [DOI] [PubMed] [Google Scholar]
- 33.He J, Whelton PK, Appel LJ, Charleston J, Klag MJ. Long-term effects of weight loss and dietary sodium reduction on incidence of hypertension. Hypertension. 2000;35:544–549. doi: 10.1161/01.hyp.35.2.544. [DOI] [PubMed] [Google Scholar]
- 34.Whelton SP, Chin A, Xin X, He J. Effect of aerobic exercise on blood pressure: A meta-analysis of randomized, controlled trials. Annals of Internal Medicine. 2002;136:493–503. doi: 10.7326/0003-4819-136-7-200204020-00006. [DOI] [PubMed] [Google Scholar]
- 35.Sacks FM, Svetkey LP, Vollmer WM, Appel LJ, Bray GA, Harsha D, Obarzanek E, Conlin PR, Miller ER, 3rd, Simons-Morton DG, Karanja N, Lin PH, Group DA-SCR Effects on blood pressure of reduced dietary sodium and the dietary approaches to stop hypertension (dash) diet. Dash-sodium collaborative research group. The New England Journal of Medicine. 2001;344:3–10. doi: 10.1056/NEJM200101043440101. [DOI] [PubMed] [Google Scholar]
- 36.Appel LJ, Moore TJ, Obarzanek E, Vollmer WM, Svetkey LP, Sacks FM, Bray GA, Vogt TM, Cutler JA, Windhauser MM, Lin PH, Karanja N. A clinical trial of the effects of dietary patterns on blood pressure. Dash collaborative research group. The New England Journal of Medicine. 1997;336:1117–1124. doi: 10.1056/NEJM199704173361601. [DOI] [PubMed] [Google Scholar]
- 37.Xin X, He J, Frontini MG, Ogden LG, Motsamai OI, Whelton PK. Effects of alcohol reduction on blood pressure: A meta-analysis of randomized controlled trials. Hypertension. 2001;38:1112–1117. doi: 10.1161/hy1101.093424. [DOI] [PubMed] [Google Scholar]
- 38.Appel LJ, Champagne CM, Harsha DW, Cooper LS, Obarzanek E, Elmer PJ, Stevens VJ, Vollmer WM, Lin PH, Svetkey LP, Stedman SW, Young DR, Writing Group of the PCRG Effects of comprehensive lifestyle modification on blood pressure control: Main results of the premier clinical trial. JAMA: The Journal of the American Medical Association. 2003;289:2083–2093. doi: 10.1001/jama.289.16.2083. [DOI] [PubMed] [Google Scholar]
- 39.Grimm RH, Jr, Cohen JD, Smith WM, Falvo-Gerard L, Neaton JD. Hypertension management in the multiple risk factor intervention trial (mrfit). Six-year intervention results for men in special intervention and usual care groups. Archives of Internal Medicine. 1985;145:1191–1199. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


