Abstract
Background:
Effective pain relief therapy after caesarean section is essential for the parturient's comfort and early ambulation. Paracetamol has an excellent safety profile when compared to opioids.
Aim:
To assess and evaluate the effect of oral, rectal, and intravenous infusion of paracetamol for post-operative analgesia in women undergoing caesarean section under spinal anaesthesia.
Settings and Design:
We conducted a prospective, randomized controlled study (18-35 years of age) of the ASA- I and II parturient scheduled for lower segment caesarean section were included.
Methods and Materials:
They were randomly allocated to 3 groups of 50 each. Group A received oral paracetamol tablet 650mg (1 tablet) 20min before shifting to operation room, group B received rectal paracetamol suppository 35-45 mg/kg immediately after spinal anaesthesia and group C received i.v. paracetamol infusion of 10-15mg/kg over 15min duration 20min before finishing the operation. Duration of analgesia was evaluated as primary outcome and other parameters as secondary outcome.
Statistical Tests:
All statistical analyses were performed using the SPSS statistical package 17.0 version. Results were analyzed using Chi Square test for non-parametric data and ANOVA for parametric data. P value of less than 0.05 was considered significant and less than 0.001 as highly significant.
Results:
Duration of analgesia was significantly longer in group B as compared to group A and C. The requirement of supplemental rescue analgesia was also lower in group B compared to group A and C. No significant haemodynamic derangements and adverse effects were noted among all the three groups.
Conclusion:
Paracetamol when given rectally improves the quality and duration of postoperative analgesia to a greater extent as compared to oral and intravenous route of paracetamol without any side effects.
Keywords: Cesarean section, paracetamol, postoperative pain
INTRODUCTION
Cesarean delivery is one of the most commonly performed surgical procedures in women.[1] Effective postoperative pain relief is an important concern as it promotes faster recovery and shortens hospital stay.[2]
Systemic and neuraxial opioids are commonly used modalities for postcesarean pain relief. Paracetamol also known as acetaminophen or N-acetyl-p-aminophenol is a widely used nonopioid analgesic that is devoid of risks related to opioids such as nausea, vomiting, constipation, pruritus, urinary retention, respiratory depression, and sedation. Paracetamol is considered as first-line treatment for pain as per the World Health Organization (WHO) guidelines of pain management with few drug interactions. The postoperative use of paracetamol has been shown to decrease acute pain after various surgical procedures.
We have planned this study to compare the effectiveness of oral, rectal, and intravenous (IV) paracetamol for postoperative analgesia in cesarean section, the analgesic requirement in the first 24 h in postoperative period among all the three groups.
MATERIALS AND METHODS
A prospective, randomized controlled study was proposed to be conducted on 150 parturients with ASA physical Status I or II undergoing lower segment cesarean section under subarachnoid block in a tertiary care hospital after obtaining approval from the hospital ethics committee; prior written informed consent was taken from all the parturients.
One-hundred and fifty parturients were randomized and included into three groups of 50 each and given oral paracetamol tablet 650 mg (1 tablet) as premedication 20 min before shifting to operation room in Group A, rectal paracetamol suppository 35–45 mg/kg immediately after spinal anesthesia in Group B, and IV paracetamol infusion of 10–15 mg/kg over 15 min duration 20 min before the end of surgery in Group C [Figure 1].
Figure 1.

Consort diagram
Parturients in the age group of 18–35 years belonging to ASA Class I and II were included in the study. The exclusion criteria taken for the study were any known hypersensitivity to paracetamol, history of alcoholism or drug abuse, bleeding diathesis or coagulation disorders, unable to rate their pain on scales used due to psychiatric or other reasons, severe allergic, hepatic, renal, cardiovascular, or pulmonary disease, with central or peripheral nervous system disease, chronic abdominal pain or on the treatment with analgesics and anticoagulants.
Data were collected in pro forma meeting the objectives of the study. Details pertaining to patient's clinical history, general physical and systemic examination, and basic routine investigations such as hemoglobin, bleeding time, clotting time, urine for albumin, and sugar were noted. All patients were premedicated on the night before surgery and 6 am in the morning with tablet ranitidine 150 mg. IV line was started with 18-gauge cannula, and coloading with Ringer's lactate 500 ml was done. All patients were taken to operation theater in left lateral position.
Monitoring was done using multi-parameter monitor having electrocardiography (ECG), noninvasive blood pressure (NIBP), and arterial pulse saturation (SpO2). Patients were placed in left lateral position. Under aseptic precautions, lumbar puncture was performed at the level of L2–L3/L3–L4 through a midline approach using 25-gauge Quincke's spinal needle and 0.5% bupivacaine 2.2 ml was injected after the confirmation of needle tip in the subarachnoid space by clear and free flow of cerebrospinal fluid. After delivery of baby, injection oxytocin was given as slow 0.3–1 IU bolus over 1 min followed by an infusion of 5–10 IU for 4 h. All the three groups of patients received oxygen 4 L/min via a facemask. Fetal parameters were noted.
Continuous intraoperative monitoring was done, and heart rate, NIBP, respiratory rate, SpO2, and ECG were recorded every 5 min for the first 20 min, then at an interval of 10 min till the end of the surgery. Readings were noted in the recovery room for every 15 min for 2 h and in the postoperative ward every 2 hourly for the next 10 h, then at 16, 20, and 24 h (except for SpO2 and ECG which were noted only up to recovery room). Neonatal APGAR scores at 1, 5, and 10 min after birth were recorded.
Duration of analgesia is defined as the time interval between administration of the study drug and visual analog scale (VAS) ≥4, i.e., time to administer first top up. Pain intensity was measured using VAS immediately in recovery room then 2 hourly till 24 h postoperative in the ward; VAS (0–10 point scale), 0 - No pain, 1–3 - Mild pain, 4–7 - Moderate pain, and 8–10 - Severe pain.
Rescue analgesia was given for pain score ≥4 in the form of intramuscular diclofenac sodium 75 mg. Duration of analgesia, time to first rescue analgesia, total dosage, and number of doses of rescue analgesia consumed in 24 h in an individual patient were noted. Hemodynamics were monitored both intraoperatively and postoperatively. In the postoperative period, patients were also monitored for adverse effects, including nausea, vomiting and abdominal pain, bleed or ooze.
RESULTS
After completion of the study, the results were compiled and statistically analyzed using Chi-square test for non-parametric data and ANOVA for parametric data. Post-hoc students paired t-test was applied wherever indicated using SSPS I or III software (IBM SPSS version 17.0, IBM, Armonk, New York, United States). We have used mean and standard deviation to represent the average and typical spread of value of variables. We have chosen the precision of our estimates of outcome statistics as 95% confidence interval. P < 0.05 was considered statistically significant and P < 0.001 as highly significant. The power of our study was 100% taking primary outcome which was duration of analgesia into consideration. Time to first rescue analgesia, total dosage and number of doses of rescue analgesia consumed in 24 h, hemodynamics, and adverse effects were studied as the secondary outcomes.
Demographics including parturient age and class distribution were comparable in all the three groups [Table 1]. Postoperatively, the duration of analgesia had been significantly longer in Group B as compared to Groups A and C which were comparable [Table 2].
Table 1.
Demographic data
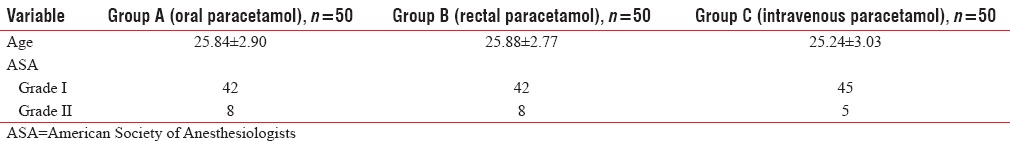
Table 2.
Perioperative outcome
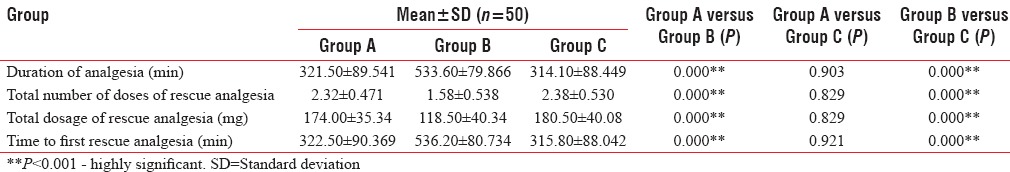
At 4 h postoperatively, VAS scores were lowest in Group B as compared to Group A and Group C whereas VAS scores were statistically significant in Groups A and B, and comparable in Groups A and C and B and C. At 8 h postoperatively, VAS score was lowest in Group C and Group A due to the effect of rescue analgesia and more in Group B. In other words, in Group B, duration of postoperative analgesia was prolonged as the requirement of rescue analgesia was after 8 h in this group. The intergroup analysis was significant between Groups A and C and highly significant between Groups A and B and B and C [Figure 2]. Total dose of rescue analgesia, number of dosages, and time to first rescue analgesia were longer in Group B. The effectivity of Groups A and C was much lower compared to Group B but statistically comparable between the two Groups A and C [Table 2].
Figure 2.

Visual analog scale scoring in three groups postoperatively
The Kaplan–Meier survival analysis showed a significantly better survival and longer time to rescue analgesia in Group B [Figure 3].
Figure 3.

Kaplan–Meyer analysis
On statistical analysis, the comparison between the three groups showed no significant change in APGAR scores at 1, 5, and 10 min. Thus, paracetamol through any route does not affect neonatal outcome.
Hemodynamics parameters both intraoperatively and postoperatively were comparable among all the three groups. No significant adverse effects were noted in either of the three groups [Table 3].
Table 3.
Adverse effects

DISCUSSION
Although pain is a predictable component of the postoperative period, inadequate management of pain has generally been observed that may lead to altered physiological and psychological changes which increases morbidity and mortality in patients.[3] A well-improvised postoperative analgesia regime helps in early mobilization and discharge from the hospital. This is especially important in parturients as they have to feed and take care of baby, which affects the bonding between baby and mother.
Paracetamol has been widely used for over a century as an effective analgesic and an antipyretic agent with an established efficacy and tolerability. Indeed, paracetamol is currently the most commonly prescribed drug for the treatment of postoperative pain as monotherapy as well as multimodal therapy.[4]
Paracetamol is widely used to relieve pain due to its efficacy and wide safety profile. It is a safe, cheap, and effective analgesic drug. The WHO has recommended that it can be used as starting point for all analgesic regimes. It is routinely used in the perioperative period to improve analgesia and reduce the need of opioids postsurgery. It can be administered parenterally, orally, and rectally to provide perioperative analgesia.[5]
The rectal route has been preferred for administration for various reasons such as need to bypass the first-pass metabolism, in unconscious or uncooperative patients or in children, where the oral route is not convenient; to avoid using parenteral route; and to avoid gastric irritation. The extensive vascular supply in rectum allows for good absorption. If medicine is absorbed in upper part of rectum, it is carried into portal circulation via the superior hemorrhoidal vein, whereas if absorbed from lower part of rectum, it enters systemic circulation directly.
The difference between duration of analgesia in IV and rectal forms of acetaminophen in controlling postoperative pain could be due to slower absorption of rectal acetaminophen (that lasts about 35–45 min), despite the first hepatic passage, causes this form of drug to reach its peak plasma concentration after about 2–3 h. In contrast, IV acetaminophen reaches its maximum concentration after 15–20 min. As a result, analgesic effects of rectal acetaminophen last longer.[6,7,8] The oral and rectal routes have been preferred over IV due to lack of pain during administration. The studies that have compared rectal route to IV or parenteral route have confirmed that suppository gives longer duration of analgesia.
A study in concordance with above results was conducted by Marzban et al. in 2014 comparing the duration of the analgesic effect of IV and rectal acetaminophen following tonsillectomy in children, concluding that postoperative pain in rectal acetaminophen group was less than that in IV acetaminophen. VAS score at 4th and 6th h postoperatively in rectal group (1.97 ± 0.48 and 1.7 ± 0.79, respectively) was lower than IV group (2.68 ± 1.5 and 2.33 ± 1.61, respectively), and the time requirement of first rescue analgesia in rectal group (7.63 ± 7.9 h) was more as compared to IV group (2.63 ± 2.2 h).[6]
Kulkarni et al. in 2007 compared rectal paracetamol with parenteral paracetamol in children undergoing minor surgery showed prolonged analgesia in rectal group (7 h postoperative) as compared to parenteral group. Time taken to attain the maximum concentration when given by rectal route was longer than that by parenteral route (2.5 ± 0.89 h vs. 1.47 ± 0.65 h). There was delay in the need for rescue analgesia in rectal group as compared to parenteral group, indicating more prolonged duration of action of paracetamol when given rectally. This is attributed to the fact regarding the formulation of suppositories, lipophilic bases provide greater bioavailability than hydrophilic bases, and particle size (smaller dose suppositories dissolve more rapidly than larger sizes). Hence, rectal paracetamol can be used as a safe, effective, and more acceptable analgesic. Because the rectal route leads to slower absorption and a longer time for the drug to achieve peak levels, it is recommended when a delayed and sustained effect is required, especially in view of its safety and opioid-sparing effect.
Mostly, studies conducted are on children due to better acceptability of rectal route versus parenteral or IV route.[5,6,9]
Capici et al. in 2008 conducted a randomized controlled trial for comparing the duration of analgesia following IV versus rectal acetaminophen after adenotonsillectomy in children concluded that rectal acetaminophen provides longer analgesia as compared to IV route.[10]
A study conducted by Bhandari et al. in 2015 concluded that time to first rescue analgesia was significantly longer in children receiving rectal acetaminophen (8.96 ± 3.46 h) compared with those receiving IV acetaminophen (6.00 ± 1.63 h).[9]
A similar study by Moller et al. in 2005 compared IV with oral route of paracetamol showed that oral paracetamol is similar to IV for postoperative analgesia after the third molar extraction in adults. This is due to the fact that plasma concentrations became very similar following both oral and IV from 1 to 24 h postadministration.[11]
Aleagha et al. in 2015 compared oral with rectal route of paracetamol in children undergoing adenotonsillectomy surgery concluded that total postoperative syrup consumption (mg) in oral group (150 ± 51.22 mg) was more as compared to rectal group (125 ± 75.49 mg), the difference was not statistically significant, but clinically rectal is better than oral group.[12]
Our study showed that duration of analgesia was prolonged with rectal route of paracetamol as compared to oral and IV route of paracetamol, because in case of rectal administration, effect-site concentration is maintained for a longer period with larger rectal dose in spite of lower bioavailability.
CONCLUSION
We concluded that rectal route of paracetamol improves the quality of postoperative analgesia after lower segment cesarean section to greater extent as compared to oral and IV routes of paracetamol without any side effect.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Chandon M, Bonnet A, Burg Y, Barnichon C, DesMesnards-Smaja V, Sitbon B, et al. Ultrasound-guided transversus abdominis plane block versus continuous wound infusion for post-caesarean analgesia: A randomized trial. PLoS One. 2014;9:e103971. doi: 10.1371/journal.pone.0103971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Doniz M, Illodo G, Vazquez-Martinez A, Vazquez-Barreiro L, Diz JC, Rey F, et al. Analysis of the efficacy and safety of the administration of epidural morphine chloride for postoperative pain after cesarean section. Rev Soc Esp Dolor. 2011;18:6–11. [Google Scholar]
- 3.Prakash M, Yachendra V, Manohar P. Comparison of efficacy of intravenous paracetamol and intravenous tramadol for post operative pain in patients undergoing infraumbilical surgeries. J Dent Med Sci. 2016;15:24–9. [Google Scholar]
- 4.Pasero C, Stannard D. The role of intravenous acetaminophen in acute pain management: A case-illustrated review. Pain Manag Nurs. 2012;13:107–24. doi: 10.1016/j.pmn.2012.03.002. [DOI] [PubMed] [Google Scholar]
- 5.Kulkarni R, Dave N, Bartakke A, Nair A, Kadam PP, Thatte UM, et al. Pharmacokinetics of rectal compared to intravenous paracetamol in children undergoing minor surgery. Indian J Pharmacol. 2007;39:187–91. [Google Scholar]
- 6.Marzban S, Haddadi S, Karami MS, Heidarzadeh A, Parvizi A, Nabi BN. Comparing the duration of the analgesic effects of intravenous and rectal acetaminophen following tonsillectomy in children. Anesth Pain Med. 2014;3:1–7. doi: 10.5812/aapm.13175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Viitanen H, Tuominen N, Vääräniemi H, Nikanne E, Annila P. Analgesic efficacy of rectal acetaminophen and ibuprofen alone or in combination for paediatric day-case adenoidectomy. Br J Anaesth. 2003;91:363–7. doi: 10.1093/bja/aeg196. [DOI] [PubMed] [Google Scholar]
- 8.Paseron C, Standard D. The role of intravenous acetaminophen in pain management. Am Soc Pain Manage. 2012;13:107–24. doi: 10.1016/j.pmn.2012.03.002. [DOI] [PubMed] [Google Scholar]
- 9.Bhandari G, Mitra S, Shahi KS, Rani A, Chauhan R, Satrunjay Analgesic efficacy of intravenous versus rectal acetaminophen after adenotonsillectomy in children. J Med Dent Sci. 2015;4:3933–9. [Google Scholar]
- 10.Capici F, Ingelmo PM, Davidson A, Sacchi CA, Milan B, Sperti LR, et al. Randomized controlled trial of duration of analgesia following intravenous or rectal acetaminophen after adenotonsillectomy in children. Br J Anaesth. 2008;100:251–5. doi: 10.1093/bja/aem377. [DOI] [PubMed] [Google Scholar]
- 11.Moller PL, Sindet-Pedersen S, Petersen CT, Juhl GI, Dillenschneider A, Skoglund LA. Onset of acetaminophen analgesia: Comparison of oral and intravenous routes after third molar surgery. Br J Anaesth. 2005;94:642–8. doi: 10.1093/bja/aei109. [DOI] [PubMed] [Google Scholar]
- 12.Aleagha AE, Behzadi M, Jafarich A, Hajimohamadi F. Effects of prophylactic rectal versus oral acetaminophen on postoperative conditions in pediatric adeno tonsillectomy patients: A randomized clinical trial. Arch Anesthesiol Crit Care. 2015;1:39–41. [Google Scholar]


