Abstract
Background:
Spinal anesthesia is used commonly intraoperatively. However, local anesthetics are associated with relatively short duration of action. A number of adjuvants have been used to prolong the postoperative analgesia.
Objectives:
To compare efficacy of dexmedetomidine and fentanyl when given intrathecally as an adjuvant to 2.5 ml of 0.75% isobaric ropivacaine.
Materials and Methods:
Sixty selected patients were randomized to receive 2.5 ml of 0.75% isobaric ropivacaine with dexmedetomidine 5 mcg (Group RD) or 20 mcg of fentanyl (Group RF) intrathecally for lower limb surgeries, block characteristics, hemodynamic changes, and adverse effects were compared.
Results:
Efficacy of both the drugs when given intrathecally was studied. Mean time needed for sensory blockade at T10 was 156.4667 ± 33.78 s in Group RD and 185.2000 ± 35.17 s in Group RF. The results are clinically and statistically significant (P - 0.002). The mean of total duration of sensory block in Group RD was 194.400 min while it was 139.9000 min in Group RF which was clinically and statistically significant (P - 0.0001). Time taken for onset of motor block was almost same in both groups. The mean of total duration of motor block in Group RD was 136.7333 min while it was 94.8667 min in Group RF which was clinically and statistically significant (P - 0.000).
Conclusion:
Dexmedetomidine at a dose of 5 μg added to 2.5 ml of ropivacaine provided earlier sensory blockade, prolonged duration of sensory and motor blockade for patients under intrathecal anesthesia for lower limb surgeries with no sedation.
Keywords: Dexmedetomidine, duration of block, fentanyl, isobaric ropivacaine, spinal anesthesi
INTRODUCTION
Ropivacaine an amide local anesthetic which was approved by the Food and Drug Administration (FDA) in 1997 but used extensively in India since 2009 which is with a high pKa and low lipid solubility has gained popularity as an intrathecal agent. It may be a suitable alternative as long-acting local anesthetic because it is considered to be less cardiotoxic and has a significantly higher threshold for central nervous system (CNS) toxicity on a milligram basis than bupivacaine.[1]
Intrathecal use of ropivacaine has been reported relatively sparingly.[2,3] It has been reported that intrathecal injection of plain (glucose-free) ropivacaine in the dose of 15 and 22.5 mg produced a sensory block of very variable extent with a proportion of patients requiring general anesthesia because of inadequate distribution of block.[4,5] Therefore, studies were conducted to elucidate the efficacy of isobaric ropivacaine,[6,7] using adjuvants such as clonidine,[8,9] fentanyl,[10] or dexmedetomidine.[11]
Dexmedetomidine is a highly selective α2-adrenergic agonist which was FDA approved in 1999 and used in India since 2012 and has been used for premedication and as an adjunct to general anesthesia. It reduces opioid and inhalational anesthetic requirements.[12] Intrathecal α2-receptor agonists are found to have antinociceptive action for both somatic and visceral pain.[13]
Fentanyl is an opioid that has shown to enhance the analgesic potency of ropivacaine for spinal anesthesia. The addition of fentanyl to ropivacaine for spinal anesthesia has been shown to prolong the duration of analgesia in the early postoperative period. Thus, it is improving the quality of anesthesia. However, there are limited studies on intrathecal isobaric ropivacaine-fentanyl combination for postoperative analgesia in lower abdominal and lower limb surgeries.
This study was undertaken to compare the safety, quality, efficacy of intrathecal dexmedetomidine 5 μg and isobaric ropivacaine 2.5 ml of 0.75% combination as compared to the isobaric ropivacaine 2.5 ml of 0.75% and fentanyl 20 μg for lower limb surgeries.
MATERIALS AND METHODS
This is a randomized, prospective study performed over the period from January 2015 to June 2016. The study was carried out in sixty patients between the age group of 18 and 60 years.
After the Institutional Ethical Committee approval and informed consent from each patient, the study was conducted at Narayana Medical College and Hospital, Nellore.
Inclusion criteria
Patients aged between 18 and 60 years, American Society of Anesthesiologists (ASA) Classes I–II, scheduled for lower limb surgeries were included in the study.
Exclusion criteria
Patients using α2-adrenergic receptors antagonists, calcium channel blockers, and angiotensin-converting enzyme inhibitors, patients with dysrhythmia, history of allergy to study drugs, patients with coagulopathy, and patients with neurological disorders were excluded from the study.
Sixty patients aged between 18 and 60 years of physical status ASA Classes I and II undergoing lower limb surgeries were included in the study after ethical clearance from the college Ethical Committee. Each patient was visited preoperatively, and the procedure explained, and written and informed consent obtained. All the routine investigations required for preoperative evaluation and the proposed surgery were done. All the patients were premedicated with tablet alprazolam 0.5 mg overnight. Patients were allowed for a period of absolute fasting of 8 h.
On arrival in the operating room, intravenous line was secured with 18-gauge intravenous cannula, and patients were preloaded with lactated ringer's solution at 15 ml/kg. Patients were randomized to two groups of thirty each. It is a double blinded as the patient and the anesthesiologist administering the drug do not know what drug it is. On the basis of a sealed envelope technique, the third person loads the drug to give one of the followings for the intrathecal injection to the patient:
Group RD (n = 30): 15 mg of 0.75% isobaric ropivacaine plus 5 μg dexmedetomidine
Group RF (n = 30): 15 mg of 0.75% isobaric ropivacaine plus 20 μg fentanyl.
Monitoring was done using automated multiparameter monitor. Vital parameters such as heart rate, noninvasive blood pressure, and SpO2 were recorded every 5 min till the end of 1 h and then every 15 min till the end of surgery.
Patients were placed in sitting position. Under all aseptic precautions, L3–L4 space was pierced with 25-gauge Quincke spinal needle by midline approach, and the study drug was deposited intrathecally. After completion of the block, patients were made to lie in the supine position. Oxygen was administrated through a mask if the pulse oximetry reading decreased below 90%. Hypotension defined as a decrease in systolic blood pressure by more than 30% from baseline or <80 mmHg was treated with incremental intravenous doses of ephedrine 6 mg and further intravenous fluid as required. Bradycardia defined as heart rate <50 beats/min was treated with intravenous atropine 0.6 mg. Sensory testing was assessed by loss of temperature discrimination to alcohol solution for onset and dermatomal levels tested every 2 min until the highest level had stabilized for four consecutive tests. Data regarding the time to reach highest dermatomal level of sensory blockade from the time of injection were collected.
After the surgery, patients will be shifted to the Postanesthesia Care Unit where they remained until there is complete recovery of sensory and motor blockade. Postoperatively, there was monitoring for any adverse event such as nausea, vomiting, pruritus, and shivering and was noted. Time to gain back the motor function of lower limb defined as time to reach Bromage 0 was noted. Even the time to recover from sensory block as regression to S1 level was noted. All durations were calculated in relation to the time of spinal injection.
Statistical analysis observations are expressed as mean ± one standard deviation (SD). Student's t-test (two-tailed, independent) has been used to find the significance of study parameters on continuous scale between two groups. The values of P < 0.05 were considered statistically significant. The statistical software, namely, SAS 9.2, SPSS 15.0, Stata 10.1, MedCalc 9.0.1, and Systat 12.0 was used for the analysis of the data, and Microsoft Word and Excel have been used to generate graphs, tables, etc.
Statistical analysis
All recorded data were entered using MS Excel software and analyzed using SPSS 20 version.
Results were expressed as mean ± SD.
Proportions were compared using Chi-square test.
P > 0.05 was considered not to be statistically significant, P < 0.05 was considered to be statistically significant, a value of P < 0.01 was highly statistically significant, and a P < 0.001 was considered as extremely statistically significant.
RESULTS
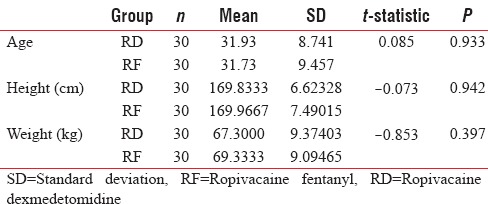
The groups were comparable with respect to their age, sex, and weight because there was no statistically significant difference among the two groups (P > 0.05) [Table 1].
Table 1.
Age, height, and weight
Mean time needed for sensory blockade at T10 was 156.4667 ± 33.78 s in Group RD and 185.2000 ± 35.17 s in Group RF. The results are clinically and statistically significant (P - 0.002) [Figure 1 and Table 2].
Figure 1.
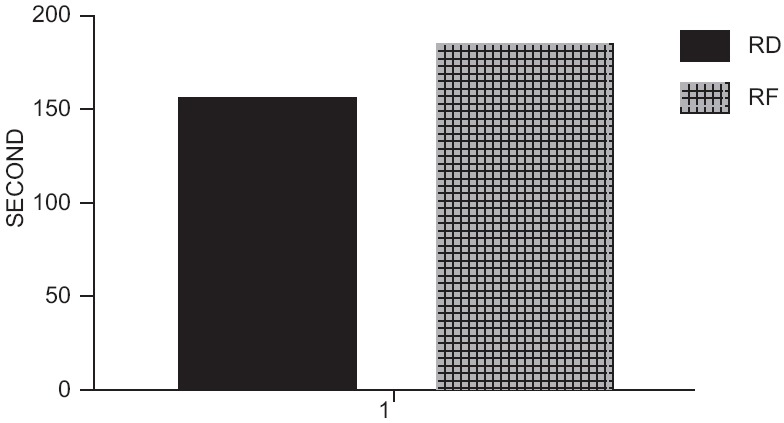
Onset of sensory block.
Table 2.
Time of onset of sensory block (s)
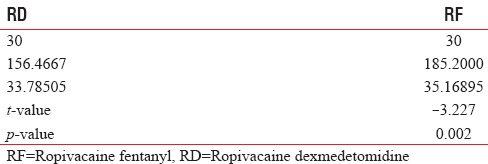
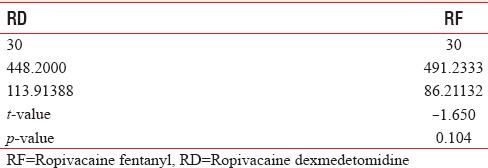
The mean time of onset of motor block in Group RD was 448.2000 s while it was 491.2333 s in Group RF which was statistically insignificant (P - 0.104) [Figure 2 and Table 3].
Figure 2.
Onset of motor block.
Table 3.
Time of onset of motor block (s)
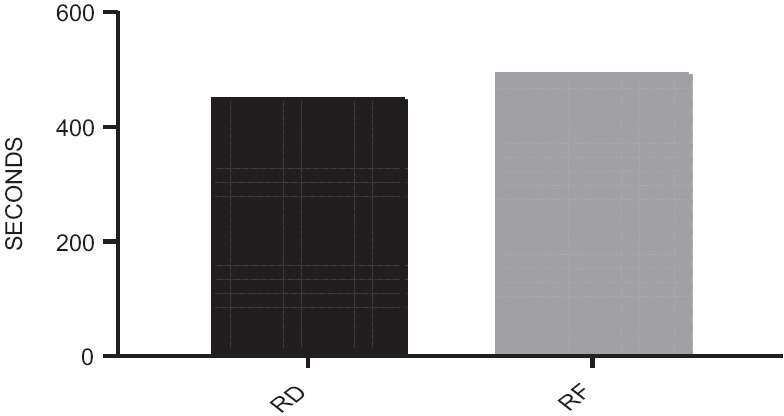
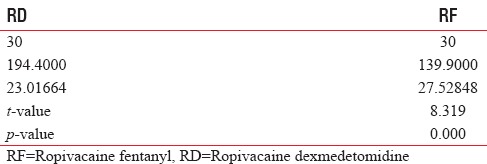
The mean of total duration of sensory block in Group RD was 194.400 min while it was 139.9000 min in Group RF which was clinically and statistically significant (P - 0.000) [Figure 3 and Table 4].
Figure 3.
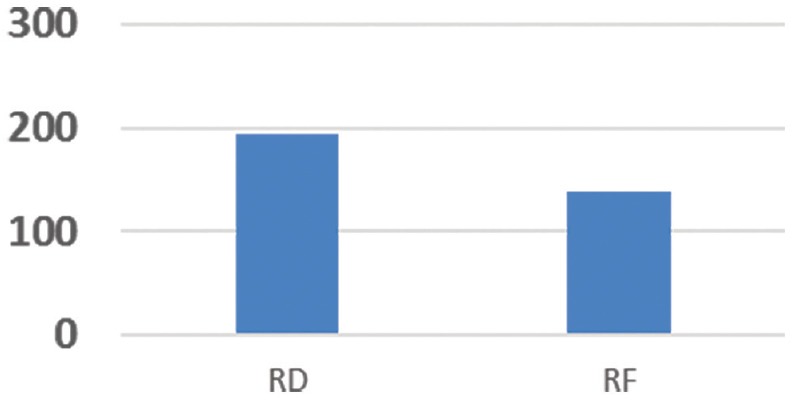
Total duration of sensory block.
Table 4.
Total duration of sensory block (min)
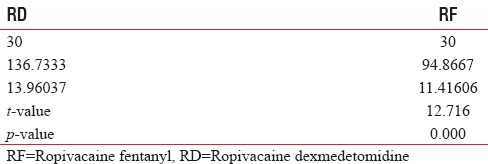
The mean of total duration of motor block in Group RD was 136.7333 min while it was 94.8667 min in Group RF which was clinically and statistically significant (P - 0.000) [Figure 4 and Table 5].
Figure 4.
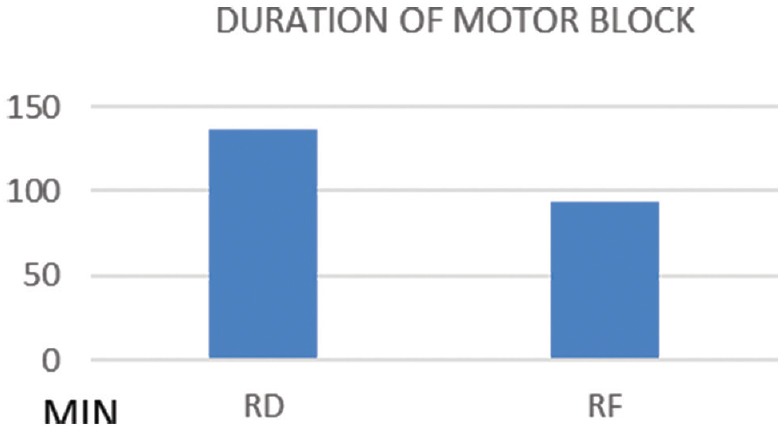
Total duration of motor block.
Table 5.
Total duration of motor block (min)
All patients in each group achieved sensory blockade at T10 for surgery. The highest level of block reached in both groups was T5 [Figure 5].
Figure 5.
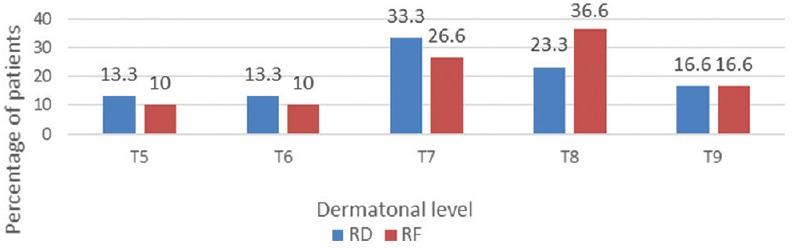
Maximum height of sensory block.
The magnitude of fall in mean arterial pressure (MAP) was similar in both groups, and it was not clinically or statistically significant [Figure 6].
Figure 6.
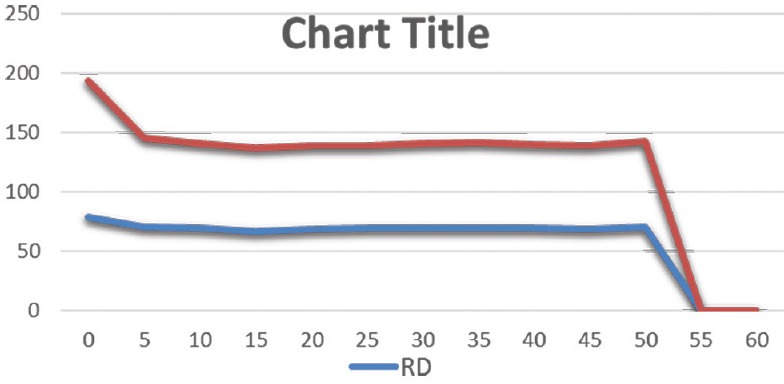
Effect on mean arterial pressure.
The heart rates were comparable in both groups without any clinically or statistically significance [Figure 7].
Figure 7.
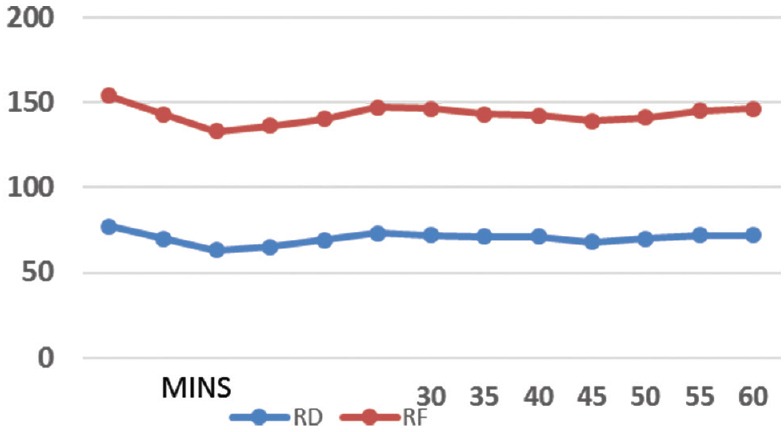
Effect on heart rate.
Hypotension was noted in 8 (26.67%) patients in Group RD and in 4 (13.33%) patients in Group RF. This was statistically not significant (P - 0.196) [Table 6].
Table 6.
Side effects
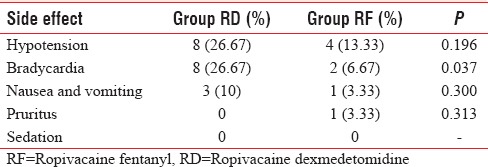
Bradycardia was noted in 8 (26.67%) patients in Group RD and 2 (6.67%) patients in Group RF. This was statistically significant (P - 0.037).
Nausea and vomiting were observed in 3 (10%) and 1 (3.33%) patient in Group RD and Group RF, respectively. This was statistically not significant (P - 0.300).
Pruritus was observed in 1 (3.33%) patient in Group RD and none in Group RF. This was statistically not significant (P - 0.313).
Sedation was not observed in either of the groups.
DISCUSSION
Ropivacaine is an amide local anesthetic, which is less toxic to the CNS and cardiovascular system and shows rapid recovery of motor function, which is now heralded as an alternative to bupivacaine. In the previous studies,[4,5] intrathecal injection of plain ropivacaine produced a sensory block of variable extent and considerable number of patients required general anesthesia to accomplish surgery.
Hyperbaric ropivacaine produces more predictable and reliable sensory and motor block, with faster onset than a plain solution.[6,7] Since commercial preparations of hyperbaric ropivacaine are not yet available, therefore adjuvants added to isobaric solution are being investigated to overcome the disadvantage of plain ropivacaine. Addition of fentanyl,[10] clonidine,[8,9] and dexmedetomidine[11] has been studied to see the effect on sensory and motor block characteristics of plain ropivacaine.
In our study, all patients receiving either drugs achieved adequate level of anesthesia. Mean time needed for sensory blockade at T10 was 156.4667 ± 33.78 s in Group RD and 185.2000 ± 35.17 s in Group RF. The results are clinically and statistically significant.
Our results are consistent with El-Attar et al.[14] study where he compared intrathecal dexmedetomidine and fentanyl as additives to bupivacaine and concluded that dexmedetomidine has faster sensory onset compared with fentanyl and local anesthetic when injected intrathecally.
Our study results were contrary to that of Mahendru et al.[15] who conducted a study on intrathecal dexmedetomidine, clonidine, and fentanyl as adjuvants to hyperbaric bupivacaine for lower limb surgery. They observed that the time of onset of sensory block was not significant in the groups receiving dexmedetomidine and fentanyl as adjuvants to intrathecal local anesthetic.
Total duration of sensory block (min) in Group RD was greater than in Group RF. The mean of total duration of sensory block in Group RD was 194.400 min while it was 139.9000 min in Group RF, which was clinically and statistically significant (P - 0.000).
Our results were similar to the studies done by Mahendru et al.,[15] Gupta et al.,[16] El-Attar et al.,[14] and Safari et al.[17] who observed that intrathecal dexmedetomidine is associated with prolonged sensory block when compared to other adjuvants added to local anesthetic.
The mean time of onset of motor block in Group RD was 448.2000 s while it was 491.2333 s in Group RF, which was statistically insignificant (P - 0.104).
Our results were similar to the study done by Mahendru et al.[15] who compared intrathecal dexmedetomidine, clonidine, and fentanyl as adjuvants to hyperbaric bupivacaine for lower limb surgery. They observed that intrathecal dexmedetomidine and fentanyl had no statistically significance with regard to the onset of motor blockade.
Our results were contrary to the studies done by El-Attar et al.[14] and Safari et al.[17] who compared intrathecal dexmedetomidine and fentanyl as additives to bupivacaine. They observed that intrathecal dexmedetomidine and fentanyl had statistically significance with regard to the onset of motor blockade. Their observation was that intrathecal dexmedetomidine has a faster onset of motor block than fentanyl.
Total duration of motor block in Group RD was greater than in Group RF. The mean of total duration of motor block in Group RD was 136.7333 min while it was 94.8667 min in Group RF, which was clinically and statistically significant (P - 0.000).
Our results were similar to the studies done by Mahendru et al.,[15] Gupta et al.,[16] El-Attar et al.,[14] and Safari et al.[17] who observed that intrathecal dexmedetomidine is associated with prolonged motor block when compared to other adjuvants added to local anesthetic.
All patients in each group achieved sensory blockade at T10 for surgery. The highest level of block reached in both groups was T5.
Mahendru et al.[15] compared intrathecal dexmedetomidine, clonidine, and fentanyl as adjuvants to hyperbaric bupivacaine for lower limb surgery. They observed that when dexmedetomidine and fentanyl were added as adjuvants, maximum height of sensory block achieved was T6 in both groups.
Gupta et al.[16] compared intrathecal dexmedetomidine and fentanyl as adjuvants to bupivacaine. They observed that the maximum height of sensory block achieved was T5 with dexmedetomidine and T6 with fentanyl as adjuvant to local anesthetic.
The fall in systolic blood pressure, diastolic blood pressure, and MAP was comparable between both RD and RF groups. The magnitude of fall was similar in both groups, and it was not clinically or statistically significant.
Our results were similar to the study, comparison of intrathecal dexmedetomidine, clonidine, and fentanyl as adjuvants to hyperbaric bupivacaine for lower limb surgery, conducted by Mahendru et al.[15] They observed that the mean values of MAP were comparable between the four groups throughout the intraoperative and postoperative periods.
Our results were also similar to the studies done by Gupta et al.[16] and Nayagam et al.[18]
There was no significant change in heart rate following subarachnoid block in both RD and RF groups. The heart rates were comparable in both groups without any clinically or statistically significance.
Our results were also similar to the studies done by Mahendru et al.,[15] Gupta et al.,[16] and Nayagam et al.[18]
In our study, hypotension was observed in eight patients in Group RD which is 26.67% in that group. Four patients in Group RF had hypotension which was 13.33%. This was statistically not significant (P - 0.196).
Our results were also similar to the studies done by Gupta et al.[16] and El-Attar et al.[14]
In our study, bradycardia was observed in eight patients in Group RD which is 26.67% in that group. Two patients in Group RF had bradycardia which was 6.67%. This was statistically significant (P - 0.037).
Our result was in contrary with the study conducted by Gupta et al.[16] and contrary to the study done by El-Attar et al.[14]
In our study, nausea and vomiting were observed in three patients in Group RD which is 10% in that group. One patient in Group RF had bradycardia which was 3.33%. This was not statistically significant (P - 0.300).
Our result was consistent with the studies conducted by Gupta et al.[16] and El-Attar et al.[14]
In our study, pruritus was observed in no patients in Group RD. One patients in Group RF had pruritus which was 3.33%. This was not statistically significant (P - 0.313).
Our result was consistent with the studies conducted by Gupta et al.[16] and El-Attar et al.[14]
CONCLUSION
Dexmedetomidine at a dose of 5 μg added to 2.5 ml of ropivacaine provided earlier sensory blockade, prolonged duration of sensory and motor blockade for patients under intrathecal anesthesia for lower limb surgeries with no sedation.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.David JS, Ferreti C, Amour J, Vivien B, Eve O, Petit P, et al. Effects of bupivacaine, levobupivacaine and ropivacaine on myocardial relaxation. Can J Anaesth. 2007;54:208–17. doi: 10.1007/BF03022642. [DOI] [PubMed] [Google Scholar]
- 2.Chung CJ, Choi SR, Yeo KH, Park HS, Lee SI, Chin YJ. Hyperbaric spinal ropivacaine for cesarean delivery: A comparison to hyperbaric bupivacaine. Anesth Analg. 2001;93:157–61. doi: 10.1097/00000539-200107000-00031. [DOI] [PubMed] [Google Scholar]
- 3.Gautier P, De Kock M, Huberty L, Demir T, Izydorczic M, Vanderick B. Comparison of the effects of intrathecal ropivacaine, levobupivacaine, and bupivacaine for Caesarean section. Br J Anaesth. 2003;91:684–9. doi: 10.1093/bja/aeg251. [DOI] [PubMed] [Google Scholar]
- 4.van Kleef JW, Veering BT, Burm AG. Spinal anesthesia with ropivacaine: A double-blind study on the efficacy and safety of 0.5% and 0.75% solutions in patients undergoing minor lower limb surgery. Anesth Analg. 1994;78:1125–30. [PubMed] [Google Scholar]
- 5.Wahedi W, Nolte H, Klein P. Ropivacaine for spinal anesthesia. A dose-finding study. Anaesthesist. 1996;45:737–44. doi: 10.1007/s001010050306. [DOI] [PubMed] [Google Scholar]
- 6.Whiteside JB, Burke D, Wildsmith JA. Spinal anaesthesia with ropivacaine 5 mg ml(-1) in glucose 10 mg ml(-1) or 50 mg ml(-1) Br J Anaesth. 2001;86:241–4. doi: 10.1093/bja/86.2.241. [DOI] [PubMed] [Google Scholar]
- 7.Whiteside JB, Burke D, Wildsmith JA. Comparison of ropivacaine 0.5% (in glucose 5%) with bupivacaine 0.5% (in glucose 8%) for spinal anaesthesia for elective surgery. Br J Anaesth. 2003;90:304–8. doi: 10.1093/bja/aeg077. [DOI] [PubMed] [Google Scholar]
- 8.Öðün CO, Kirgiz EN, Duman A, Kara I, Ökesli S. The comparison of intrathecal isobaric ropivacaine and isobaric ropivacaine-clonidine for caesarean delivery. Internet J Anesthesiol. 2007;15:904–9. [Google Scholar]
- 9.Sagiroglu G, Sagiroglu T, Meydan B. The effects of adding various doses of clonidine to ropivacaine in spinal anesthesia. Eurasian J Med. 2009;41:149–53. [PMC free article] [PubMed] [Google Scholar]
- 10.Förster JG, Rosenberg PH. Small dose of clonidine mixed with low-dose ropivacaine and fentanyl for epidural analgesia after total knee arthroplasty. Br J Anaesth. 2004;93:670–7. doi: 10.1093/bja/aeh259. [DOI] [PubMed] [Google Scholar]
- 11.Gupta R, Bogra J, Verma R, Kohli M, Kushwaha JK, Kumar S. Dexmedetomidine as an intrathecal adjuvant for postoperative analgesia. Indian J Anaesth. 2011;55:347–51. doi: 10.4103/0019-5049.84841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Martin E, Ramsay G, Mantz J, Sum-Ping ST. The role of the alpha2-adrenoceptor agonist dexmedetomidine in postsurgical sedation in the intensive care unit. J Intensive Care Med. 2003;18:29–41. doi: 10.1177/0885066602239122. [DOI] [PubMed] [Google Scholar]
- 13.Kalso EA, Pöyhiä R, Rosenberg PH. Spinal antinociception by dexmedetomidine, a highly selective alpha 2-adrenergic agonist. Pharmacol Toxicol. 1991;68:140–3. doi: 10.1111/j.1600-0773.1991.tb02052.x. [DOI] [PubMed] [Google Scholar]
- 14.El-Attar A, Aleem MA, Beltagy R, Ahmed W. A comparative study of intrathecal dexmedetomidine and fentanyl as additives to bupivacaine. Res Opin Anesth Intensive Care. 2015;1:43–9. [Google Scholar]
- 15.Mahendru V, Tewari A, Katyal S, Grewal A, Singh MR, Katyal R. A comparison of intrathecal dexmedetomidine, clonidine, and fentanyl as adjuvants to hyperbaric bupivacaine for lower limb surgery: A double blind controlled study. J Anaesthesiol Clin Pharmacol. 2013;29:496–502. doi: 10.4103/0970-9185.119151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gupta R, Verma R, Bogra J, Kohli M, Raman R, Kushwaha JK. A Comparative study of intrathecal dexmedetomidine and fentanyl as adjuvants to Bupivacaine. J Anaesthesiol Clin Pharmacol. 2011;27:339–43. doi: 10.4103/0970-9185.83678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Safari F, Aminnejad R, Mohajerani SA, Farivar F, Mottaghi K, Safdari H. Intrathecal dexmedetomidine and fentanyl as adjuvant to bupivacaine on duration of spinal block in addicted patients. Anesth Pain Med. 2016;6:e26714. doi: 10.5812/aapm.26714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nayagam HA, Singh NR, Singh HS. A prospective randomised double blind study of intrathecal fentanyl and dexmedetomidine added to low dose bupivacaine for spinal anesthesia for lower abdominal surgeries. Indian J Anaesth. 2014;58:430–5. doi: 10.4103/0019-5049.138979. [DOI] [PMC free article] [PubMed] [Google Scholar]


