Abstract
Background:
Hypobaric spinal anesthesia is advantageous for unilateral lower extremity fractures as it obviates pain of lying on fractured limb for performing subarachnoid block.
Aims:
This study compares block characteristics and complications of three different baricities of constant dose intrathecal hypobaric levobupivacaine to determine an optimum baricity.
Settings and Design:
One-twenty American Society of Anesthesiologists Physical Status 1 and 2 patients aged 18–65 years undergoing unilateral lower limb surgeries were divided into three equal groups for this prospective cohort study.
Materials and Methods:
To 2 mL intrathecal 0.5% isobaric levobupivacaine (10 mg), 0.4 mL, 0.6 mL, and 0.8 mL of distilled water were added in Groups A, B, and C, respectively. Baricities of Groups A, B, and C are 0.999294, 0.998945, and 0.998806, respectively. Development of sensory and motor block was assessed by the pinprick method and Bromage scale, respectively. The total duration of analgesia and complications were noted.
Statistical Analysis Used:
Mean, standard error, one-way ANOVA, and Bonferroni were used to analyze quantitative variables; proportions and Chi-square tests for qualitative variables.
Results:
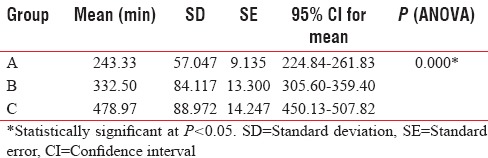
Demographic parameters, motor block of operated limb, and complications were comparable. Group C had the fastest onset of sensory block (10.10 min) and maximum duration of analgesia (478.97 min; P < 0.001); but high sensory levels in 48.7%. Group B had T10 sensory level in 92.5%; onset comparable to Group C (P = 0.248), and reasonable duration of analgesia (332.50 min). Group A had inadequate sensory levels, slow onset, and early regression.
Conclusions:
Group B (baricity - 0.998945) has better block characteristics among three groups compared.
Keywords: Anesthesia, comparative study, levobupivacaine, lower extremity/surgery, spinal
INTRODUCTION
Subarachnoid block (SAB) is a widely used regional anesthetic technique for lower limb surgeries. Hyperbaric, isobaric, and hypobaric local anesthetic (LA) preparations have been used for performing SAB of which hyperbaric is most common.
Compared to hyperbaric technique, hypobaric spinal anesthesia is especially useful for surgical procedures involving hip or any lower extremity fracture because patients need not lay on the fractured limb for performing SAB.[1] The fractured limb is nondependent during the performance of hypobaric spinal which is more comfortable to the patient. This is because hypobaric solutions tend to rise in cerebrospinal fluid (CSF), unlike hyperbaric solutions which concentrate in the most dependent regions of spinal column.
However, this technique is seldom used nowadays, mainly because hypobaric LA preparations for intrathecal administration is scarce in the market, and these have to be prepared at bedside by mixing isobaric solutions with distilled water.[2] It is impossible to measure the density of these preparations at the bedside before each spinal anesthetic. However, at the same time, even a small change in density as low as 6 kg/m3 can influence the spread of LA.[3] Unintentional rise of block height has been considered a complication of hypobaric spinal, main reason of which could be accidental alterations in baricity. Thus, for safe conduct of hypobaric spinal, it is important to have an assessment of an optimum baricity which can produce desirable block with minimum complications. This is the purpose of the present study. For practical purposes, solutions with a baricity <0.9990 are hypobaric in all patients and solutions with a baricity of ≥1.0015 are hyperbaric.[4]
Theoretically, the injection of a nonisobaric LA should induce a unilateral spinal anesthesia in patients in a lateral decubitus position. The increased interest of unilateral spinal anesthesia is mainly because of hemodynamic benefits.[5] Compared to hyperbaric spinal, difficulties related to frequent changing of patient positions can also be decreased because many of the surgeries are done with fracture site in same nondependent position that we use for hypobaric spinal. The hypobaric spinal anesthetic technique also has advantage of decrease in complications such as urinary retention and moreover better patient satisfaction.
The present study aims to compare the maximum cephalic level of sensory block achieved and its onset, motor block, total duration of analgesia, and hemodynamic as well as respiratory complications of three different baricities of constant dose intrathecal hypobaric levobupivacaine so that an optimum baricity, which produces preferred block characteristics with minimum complications, can be made out for use in hypobaric spinal anaesthesia.
MATERIALS AND METHODS
This study was conducted as a prospective cohort study at our institution after obtaining approval of the Institutional Technical Committee and Human Ethical Committee. The study period was 9 months – from January 2013 to September 2013.
The inclusion criteria were:
Patients posted for elective or emergency unilateral lower limb surgeries under SAB
The American Society of Anesthesiologists Physical Status (ASA PS) 1 and 2
Age between 18 and 65 years
Height between 150 and 180 cm.
The exclusion criteria were:
Patient refusal
Contraindications to spinal anesthesia
Expected duration of surgery more than 3 h.
A total of 120 patients who received hypobaric spinal for unilateral lower limb surgeries were observed during this study period.
After preanesthetic checkup, written informed consent in local language was obtained from the patient and relative. On arrival in the operation theater, monitors including noninvasive blood pressure, electrocardiogram and pulse oximeter were attached; baseline readings recorded and monitoring continued throughout intraoperative period. Intravenous access was secured in the nondependent forearm, and coloading started with 500 mL of lactated ringer. 1 mg of midazolam was given intravenously as premedication. Oxygen was supplemented through face mask at 5 L/min. Under asepsis, SAB was performed by a qualified anesthesiologist at L3/4 or L4/5 interspaces using 25-gauge Quincke needle with patient in the lateral position and limb to be operated as nondependent. Once the free flow of CSF was confirmed, 15° Trendelenburg tilt was given to table and drug injected slowly at a rate of 0.1 mL/s with bevel of spinal needle facing nondependent hip. Total dose of intrathecal levobupivacaine given to all patients was 10 mg, but baricities and total volume administered were different.
Patients who received 2.4 mL (2 mL of 0.5% isobaric levobupivacaine with 0.4 mL of distilled water) with baricity of 0.999294 were termed Group A.
Patients who received 2.6 mL (2 mL of 0.5% isobaric levobupivacaine with 0.6 mL of distilled water) with baricity of 0.998945 were termed Group B.
Patients who received 2.8 mL (2 mL of 0.5% isobaric levobupivacaine with 0.8 mL of distilled water) with baricity of 0.998806 were termed Group C.
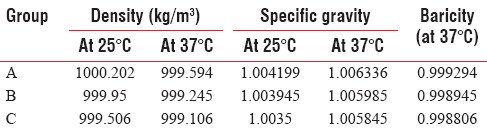
Hence, Group A is near to isobaricity whereas other two groups are reliably hypobaric. The densities of three study solutions were measured in the laboratory before conducting study by finding out mass of unit volume of solution. The density of parent solution is 1.00024 [Table 1].
Table 1.
Densities, specific gravities, and baricities of study solutions
Patients were kept in the same position (lateral decubitus with Trendelenburg) for 10 min before turning supine (if the surgery was planned in the supine position). The lateral position was maintained if surgery was planned in that position itself. Upper sensory block level of T10 and motor block of Bromage 3 on operated limb are taken as preferred block characteristics in this study. T10 was considered the target block height since we had included hip surgeries also.[6] If block height ascended above T8, Trendelenburg tilt was increased so as to restrict the level to T8. Otherwise, initial degree of Trendelenburg tilt was continued for 20 min.
Pinprick test performed with blunted tip of 24-gauge needle in midclavicular line every 2 min for the first 20 min after SAB, and every 5 min, thereafter till time of skin incision. Maximal upper sensory block level and its onset time were noted.
Evolution of motor block assessed using Bromage scale every 5 min for 30 min or till time of skin incision whichever occurred early.[7]
Full flexion of knees and feet
Just able to flex knees, full flexion of feet
Unable to flex knees, but some flexion of feet possible
Unable to move legs or feet.
Surgeons were allowed to operate once adequate level of block was achieved.
Systolic, diastolic and mean arterial blood pressures, heart rate, respiratory rate, and oxygen saturation were recorded every two min for 20 min, then every five min during surgery, and every 15 min in recovery room.
Crystalloids were administered intraoperatively and allowable blood loss replaced with a crystalloid solution on a 3:1 basis (3 mL of crystalloid for 1 mL of blood). Injection mephentermine was given in three-milligram increments intravenously if systolic BP decreased >20% from baseline value despite adequate crystalloid infusion. Injection atropine 0.6 mg was given intravenously if heart rate decreased to <50/min.
Total duration of analgesia was taken as time between spinal injection and the first analgesic requirement for a pain score of more than three on numeric rating scale (ranging from 0 to 10) at operated site.
Calculation of sample size was based on a previous study by Kaya et al. that compared low-dose hyperbaric levobupivacaine and hypobaric levobupivacaine in unilateral spinal anesthesia for elective ambulatory arthroscopic surgery of the knee.[8] Considering alpha error 5% (zα = 1.96: 95% confidence desired) and beta error (zβ = 0.842; 80% power desired), sample size was calculated using the formula (zα + zβ)2 × pq × 1.5/d2. The difference in redistribution of spinal block toward operated side which significantly affected the total duration of analgesia between hyperbaric and hypobaric groups of parent study was considered for calculation of sample size. “P” was 46.5 (60 + 33/2), “q” 53.5 (100-p) and d was 27 (60–33). Calculated sample size was 40 in each group.
Data were analyzed using software - Statistical Package for Social Sciences for Windows version 16.0 (SPSS Inc, Chicago, USA). Mean, standard error, one-way ANOVA, and Bonferroni were used to compare quantitative variables. Qualitative variables were compared using proportions and Chi-square tests. Data were expressed as mean ± standard deviation/confidence interval and number (percentage), and it was normally distributed.
RESULTS
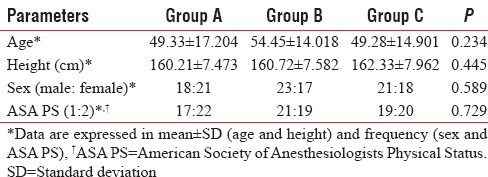
Two patients – one each from Group A and Group C required conversion to general anesthesia due to inadequate block and were excluded from the study. Patients in three groups were comparable with respect to age, sex, ASA PS, and height [Table 2].
Table 2.
Demographic data
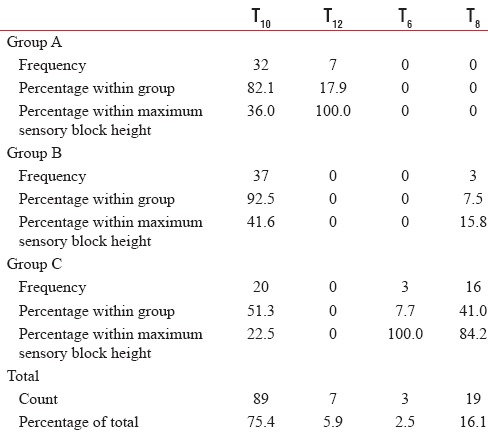
Maximum cephalic level of sensory block achieved ranged between T12 and T6. The majority of patients had T10 sensory level (89), followed by T8 (19), and T12 (7). Comparison of maximum attained sensory block height was found to be statistically significant among groups. Group B had more consistent T10 blockade [Table 3].
Table 3.
Maximum sensory block height
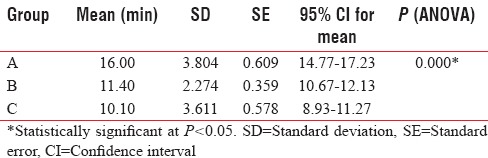
Time taken for attaining maximum cephalic level of sensory block was fastest in Group C and slowest in Group A. Onset of maximum sensory block height was statistically insignificant between Groups B and C (P = 0.248), whereas it was significant when comparing Group A with other two groups (P < 0.001) [Table 4].
Table 4.
Onset of maximum sensory block height
All 118 patients had Bromage 3 on operated limb.
The mean of total duration of analgesia was maximum in Group C followed by Group B [Table 5].
Table 5.
Total duration of analgesia
The incidence of hemodynamic and respiratory complications was also compared among three groups and was found to be statistically insignificant. One patient from Group B had bradycardia which responded to injection atropine 0.6 mg intravenous. Two patients, one each from Group A and Group B had hypotension that promptly responded to treatment. There were no incidences of respiratory depression and desaturation.
DISCUSSION
The effects of altering baricity on onset, duration, and spread of LA blockade after intrathecal injection have been the subject of study for many decades. Baricity is defined as ratio of density of LA solution to density of CSF. Solutions that have the same density as CSF have a baricity of 1 and are called isobaric. Solutions that are denser than CSF are termed hyperbaric, whereas solutions that are less dense are termed hypobaric.[4]
The use of hypobaric LA preparation in the present day anesthesia practice is limited to perianal surgeries done in jack-knife position and lower limb surgeries. When comparing the same dose of hyperbaric bupivacaine with hypobaric bupivacaine, greater volume of hypobaric resulted in a greater dispersion of anesthetic. This may be the reason why many clinicians use and trust preferably in hyperbaric solutions.[5]
Levobupivacaine, drug used in the present study, is the S-enantiomer of Bupivacaine. Block characteristics regarding relative potency and duration of both differ among studies, but levobupivacaine has significantly less cardiotoxicity.[9] Levorotatory isomers tend to produce more vasoconstriction rather than vasodilatation. This might be useful in prolonging the duration of block and delaying the requirement of analgesics. However, in clinical situations, such as the spinal anesthetic, in which systemic toxicity is of minimal issue, the advantage of levobupivacaine over bupivacaine appears to be more theoretical than real.[9] Several studies have proved the safety and efficacy of intrathecal levobupivacaine.[10,11,12]
The present study compared block characteristics and complications of three different baricities of constant dose intrathecal hypobaric levobupivacaine. The maximum cephalic level of sensory block has been found to be highest in hypobaric groups compared to near isobaric group in the present study. There was no significant difference in maximum sensory block height between hypobaric and isobaric group in the study by Faust et al. using constant dose bupivacaine. In study by Faust et al., patients undergoing total hip arthroplasty randomly received, a spinal injection of 3.5 mL (17.5 mg) of plain bupivacaine mixed with either 1.5 mL of normal saline (isobaric group) or 1.5 mL of distilled water (hypobaric group) with operative side up.[13] The hypobaric solution spread one dermatome higher than the plain solution in another study comparing hypobaric and near isobaric bupivacaine for arthroscopic knee surgeries.[14] Similar maximum sensory block heights were also found in study comparing hyperbaric and hypobaric levobupivacaine in unilateral spinal anesthesia for elective ambulatory arthroscopic surgery of the knee by Kaya et al.[8]
Unlike hypobaric and hyperbaric solutions, patient position has no effect on distribution of isobaric solutions, and they tend not to spread far from site of injection. Inadequate upper sensory levels of patients in Group A may be due to this because the solution used was near isobaric.
The onset of maximum sensory block height is found to be statistically insignificant between hypobaric Groups (B and C), whereas it is significantly prolonged in near isobaric Group A. Time to reach maximum sensory level was comparable in study comparing hyperbaric and hypobaric levobupivacaine.[8] The onset of maximum sensory block height was delayed for isobaric group compared to hypobaric group but not statistically significant in the study by Faust et al.[13]
In the present study, the most hypobaric Group C has maximum duration of analgesia followed by Group B. Total duration of analgesia is found to be least in near isobaric Group A. Time taken for regression to L2 and total duration of analgesia were significantly prolonged in hypobaric group when compared to isobaric group in study by Faust et al.[13]
Block that spreads higher descends fast because of reduced drug concentration at nerve roots. However, in the present study, hypobaric groups had longer duration of analgesia than near isobaric group despite having higher sensory levels. This could be due to preferential redistribution of block to operated side in hypobaric spinal as evidenced by lower Bromage scores and dermatomal levels on nonoperated limb which we also observed during our study.
All 118 patients had Bromage of 3 on operated limb. Maximal degree of motor blockade achieved and its onset was comparable statistically between two groups in study by Faust et al. although onset was slightly delayed in isobaric group.[13]
Theoretically, the injection of a nonisobaric LA should induce a unilateral spinal anesthesia in patients in a lateral decubitus position. The increased interest of unilateral spinal anesthesia is mainly because of hemodynamic benefits.[5] When hemodynamic changes are compared between bilateral and unilateral spinal anesthesia with the same dose of hyperbaric bupivacaine (8 mg), the frequencies of hypotension were 22.4% and 5%, respectively.[15]
Hemodynamic and respiratory complications in the present study are found to be statistically insignificant. Hemodynamic changes, observed during the first 45 min after spinal injection, were comparable between the two groups in the study by Faust et al.[13]
Low-dose hypobaric spinal has excellent hemodynamic stability compared to conventional hyperbaric spinal. Preferential redistribution of block to operated side in hypobaric spinal could be main reason for this also. This entity requires further research because by avoiding unnecessary motor block of nonoperated side, we can improve hemodynamic stability, decrease chances of venous thrombosis and can promote early ambulation.
Ali Hassan compared low-dose lidocaine and fentanyl as bilateral, hypobaric spinal anesthesia with unilateral hyperbaric bupivacaine and found that both techniques were suitable for ambulatory knee arthroscopy. The total discharge time or the time to home-readiness was 184.6 ± 14.2 min versus 153 ± 10.9 min in bupivacaine and lidocaine groups, respectively. Thus, lidocaine hypobaric spinal was found to be more eligible for the concept of fast-tracking anesthesia.[16]
Unilateral block saves the experience of healthy patient undergoing a reversible drug-induced paraplegia and possibly the feeling of helplessness. For most patients, a unilateral spinal anesthesia may be at least a psychological advantage.[5]
Nevertheless, few limitations of study need to be considered. The total volume of drug injected is different in three groups. However, it is not possible to keep dose and volume constant while changing baricities. Hence, we decided to keep dose constant considering the fact that three most important factors for determining spread of local anesthesia in subarachnoid space are baricity of LA solution, position of the patient during and just after injection, and dose of anesthetic injected.[2,17,18]
There exist flaws in design of this study as well. Randomized controlled study with blinding would have been done to allay bias. Further clinical trials need to be done in this field because hypobaric spinal has a definite potential to enter into the clinical arena.
CONCLUSIONS
Hypobaric spinal is indeed a good choice for unilateral lower limb fracture surgeries. It produces reliable sensory as well as motor blockade with excellent hemodynamic stability and postoperative analgesia. It is more comfortable to the patient compared to hyperbaric spinal.
However, even a small change in baricity produces a significant change in block characteristics. Compared to near isobaric drug group in our study, hypobaric solutions spread more in CSF with faster onset and higher upper sensory levels. Among the baricities that we compared, Group B (2.6 mL, i.e., 2 mL of 0.5% isobaric levobupivacaine with 0.6 mL of distilled water; baricity - 0.998945) appears better choice.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Butterworth JF, Mackey DC, Wasnick JD, editors. Morgan and Mikhail's Clinical Anesthesiology. 5th ed. United States of America: McGraw-Hill Education; 2013. p. 958. [Google Scholar]
- 2.Brull R, Macfarlane AJ, Chan VW. Spinal, epidural, and caudal anesthesia. In: Miller RD, editor. Miller's Anesthesia. 8th ed. Philadelphia: Elsevier Saunders; 2015. p. 1694. [Google Scholar]
- 3.McLeod G. Spinal anaesthesia – Intradural and extradural. In: Davies NJ, Cashman JN, editors. Lee's Synopsis of Anaesthesia. 13th ed. London: Butterworth-Heinemann Elsevier; 2006. p. 486. [Google Scholar]
- 4.Bernards CM, Hostetter LS. Epidural and spinal anesthesia. In: Barash PG, Cullen BF, Stoelting RK, Cahalan MK, Stock MC, Ortega R, editors. Clinical Anesthesia. 7th ed. Philadelphia: Lippincott Williams and Wilkins; 2013. p. 916. [Google Scholar]
- 5.Imbelloni LE. Spinal hemianesthesia: Unilateral and posterior. Anesth Essays Res. 2014;8:270–6. doi: 10.4103/0259-1162.143108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Brull R, Macfarlane AJ, Chan VW. Spinal, epidural, and caudal anesthesia. In: Miller RD, editor. Miller's Anesthesia. 8th ed. Philadelphia: Elsevier Saunders; 2015. p. 1693. [Google Scholar]
- 7.Veering BT, Cousins MJ. Epidural neural blockade. In: Cousins MJ, Carr DB, Horlocker TT, Bridenbaugh PO, editors. Cousins and Bridenbaugh's Neural Blockade in Clinical Anaesthesia and Pain. 4th ed. Philadelphia: Lippincott Williams and Wilkins; 2009. p. 257. [Google Scholar]
- 8.Kaya M, Oztürk I, Tuncel G, Senel GO, Eskiçirak H, Kadiogullari N. A comparison of low dose hyperbaric levobupivacaine and hypobaric levobupivacaine in unilateral spinal anaesthesia. Anaesth Intensive Care. 2010;38:1002–7. doi: 10.1177/0310057X1003800606. [DOI] [PubMed] [Google Scholar]
- 9.Berde CB, Strichartz GR. Local anesthetics. In: Miller RD, editor. Miller's Anesthesia. 8th ed. Philadelphia: Elsevier Saunders; 2015. p. 1049. [Google Scholar]
- 10.Goyal A, Shankaranarayan P, Ganapathi P. A randomized clinical study comparing spinal anesthesia with isobaric levobupivacaine with fentanyl and hyperbaric bupivacaine with fentanyl in elective cesarean sections. Anesth Essays Res. 2015;9:57–62. doi: 10.4103/0259-1162.150169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lee YY, Muchhal K, Chan CK, Cheung AS. Levobupivacaine and fentanyl for spinal anaesthesia: A randomized trial. Eur J Anaesthesiol. 2005;22:899–903. doi: 10.1017/S0265021505001523. [DOI] [PubMed] [Google Scholar]
- 12.Attri JP, Kaur G, Kaur S, Kaur R, Mohan B, Kashyap K. Comparison of levobupivacaine and levobupivacaine with fentanyl in infraumbilical surgeries under spinal anaesthesia. Anesth Essays Res. 2015;9:178–84. doi: 10.4103/0259-1162.152148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Faust A, Fournier R, Van Gessel E, Weber A, Hoffmeyer P, Gamulin Z. Isobaric versus hypobaric spinal bupivacaine for total hip arthroplasty in the lateral position. Anesth Analg. 2003;97:589–94. doi: 10.1213/01.ANE.0000070228.13782.ED. [DOI] [PubMed] [Google Scholar]
- 14.Kuusniemi KS, Pihlajamäki KK, Pitkänen MT, Korkeila JE. Low-dose bupivacaine: A comparison of hypobaric and near isobaric solutions for arthroscopic surgery of the knee. Anaesthesia. 1999;54:540–5. doi: 10.1046/j.1365-2044.1999.00855.x. [DOI] [PubMed] [Google Scholar]
- 15.Casati A, Fanelli G, Aldegheri G, Colnaghi E, Casaletti E, Cedrati V, et al. Frequency of hypotension during conventional or asymmetric hyperbaric spinal block. Reg Anesth Pain Med. 1999;24:214–9. doi: 10.1016/s1098-7339(99)90130-x. [DOI] [PubMed] [Google Scholar]
- 16.Ali Hassan HI. Comparison between two different selective spinal anesthesia techniques in ambulatory knee arthroscopy as fast-track anesthesia. Anesth Essays Res. 2015;9:21–7. doi: 10.4103/0259-1162.150157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tsai T, Greengrass R. Spinal anesthesia. In: Hadzik A, editor. Textbook of Regional Anesthesia and Acute Pain Management. 1st ed. United States: McGraw-Hill Companies; 2007. p. 200. [Google Scholar]
- 18.Butterworth JF, Mackey DC, Wasnick JD, editors. Morgan and Mikhail's Clinical Anesthesiology. 5th ed. United States of America: McGraw-Hill Education; 2013. p. 956. [Google Scholar]


