Abstract
Background:
Although the advantages of ventilation with i-gel™ and laryngeal mask airway Supreme (LMA-Supreme™) has been well documented, they are still under debate for surgeries requiring flexion and extension of neck such as thyroid surgery, tonsillectomy, and neck exploration. Hence, we conducted a study to demonstrate the effect of neck flexion and extension in spontaneously breathing anesthetized pediatric patients utilizing i-gel™ and LMA-Supreme™.
Methods:
A prospective, randomized comparative study was conducted on sixty children, thirty each in i-gel™ and LMA-Supreme™ group. Oropharyngeal leak pressure (OPLP), fiberoptic view of vocal cords, and exhaled tidal volume were evaluated in neutral, flexion, and extension neck positions in spontaneously breathing children.
Results:
OPLP for i-gel™ was found to be significantly higher in flexion (29.00 ± 1.95 cmH2O, P < 0.001) and lower in extension (21.07 ± 2.08 cmH2O, P < 0.001) as compared to neutral (24.67 ± 2.08 cmH2O). Similar results were observed for LMA-Supreme™ which showed significantly higher OPLP in flexion (24.73 ± 2.26, P < 0.001 respectively) and lower in extension (18.67 ± 1.42 cmH2O, P < 0.001) as compared to neutral (20.87 ± 1.80 cmH2O). Worsening of fiberoptic view occurs for i-gel™ and LMA-Supreme™ in flexion (10/12/5/3/0 and 11/14/2/2/1, P < 0.05) as compared to neutral position (17/10/2/1/0 and 15/12/1/1/1), respectively. Significant change did not occur in extension. Ventilation worsening occurred in flexion as compared to neutral position evidenced by significant decrease in exhaled tidal volume (92.90 ± 11.42 and 94.13 ± 7.75 ml, P < 0.05) as compared to neutral (100.23 ± 12.31 and 101.50 ± 8.26 ml) for i-gel™ and LMA-Supreme™, respectively.
Conclusion:
Neck flexion caused a significant increase in leak pressure in both i-gel™ and LMA-Supreme™. With deterioration of fiberoptic view and ventilation, both devices should be used cautiously in pediatric patients in extreme flexion.
Keywords: i-gel™, LMA-Supreme™, oropharyngeal leak pressure
INTRODUCTION
Since 1983, when Dr. Archie Brain invented first supraglottic airway device (SAD) and revolutionized the field of airway devices, multiple devices have come into market ranging from laryngeal mask Classic™, laryngeal mask ProSeal™, and laryngeal mask Ambu™.[1] Laryngeal mask airway Supreme (LMA-Supreme™) and i-gel™ are two new additions in the list of supraglottic devices introduced since 2007. The cuff of i-gel™ is made of medical grade thermoplastic elastomer. The part of i-gel™ incorporates epiglottic rest to prevent downfolding, an integral drain tube parallel to airway tube to prevent regurgitation and aspiration. It comes in multiple sizes: 1.5, 2, and 2.5 in pediatrics.[2,3,4] On the other hand, LMA-Supreme™ is made of polyvinyl chloride with combined features of ProSeal LMA (presence of gastric drain tube and high airway sealing pressure), LMA Fastrach (curved, rigid manifold for easy insertion), and LMA Unique™.[5]
I-gel™ has shown a high success insertion rates in multiple studies.[3,4] Many randomized control trials have compared i-gel™ with other LMAs and measured oropharyngeal leak pressure (OPLP).[6,7] Evaluation of OPLP was done in different head and neck positions in some studies among adults, but similar studies in pediatric patients with spontaneous breathing are rare.[8,9] Although the advantages of ventilation with i-gel™ have been well documented, it is still under debate for surgeries requiring flexion and extension of neck such as thyroid surgery, tonsillectomy, and neck exploration.[10,11] Hence, we conducted a study to demonstrate effect of neck flexion and extension in pediatric patients with spontaneous breathing utilizing i-gel™ and LMA-Supreme™.
Aims/objectives
The primary aim of our study was to evaluate OPLP in spontaneously breathing children for i-gel™ and LMA-Supreme™ in neutral, flexion, and extension position of head and neck. The secondary aim was to evaluate fiberoptic view and quality of ventilation by measuring exhaled tidal volume under these positions for both i-gel™ and LMA-Supreme™.
METHODS
Our study was a prospective, randomized comparative study. A total of sixty children between age group of 2 and 5 years of the American Society of Anesthesiologists Class I–II, weighing 10–20 kg, and posted for elective surgeries were taken into study, thirty each into i-gel™ and LMA-Supreme™ group. The study was conducted in the Department of Anaesthesiology, SMS Medical College and Attached Group of Hospitals, Jaipur, with due permission. Well-informed written consent was obtained from parents/guardians of all children. Clearance was obtained from the ethical clearance committee. All the children were randomly allocated into Group A (i-gel™) and Group B (LMA-Supreme™). The children with upper respiratory tract infection, at risk of gastroesophageal regurgitation, with airway related conditions such as trismus, limited mouth opening pharyngo–perilaryngeal abscess, trauma or mass were excluded from study. All children were examined on the day before surgery and had a preanesthetic checkup which included any significant present/history, physical examination, and vital parameters such as respiratory rate/blood pressure/pulse rate. All patients were kept nil per oral according to the standard guidelines before elective surgery.
After the patient had been brought to operating table with intravenous line in situ according to hospital protocols, monitors for SpO2, noninvasive blood pressure, pulse rate, and capnography were attached. Injection fentanyl was given at dose of 2 μg/kg followed by injection glycopyrrolate 5 μg/kg and injection midazolam 0.05 mg/kg. Patients were preoxygenated with 100% oxygen. Induction was performed with injection propofol 2.5–3 mg/kg and maintained with nitrous oxide with oxygen inhalation given in 60:40 ratio with sevoflurane 2%. Device insertion was done by an experienced anesthetist, according to the manufacturer's recommendations.[2] Success of insertion was described as bilateral chest expansion and a square-shaped capnography. In case of partial or complete airway obstruction or significant air leak, device was removed and reinsertion was tried. If failure occurred on third attempt, then endotracheal intubation was done instead. None of children required intubation and there was no device insertion failure documented in our study. I-gel™ and LMA-Supreme™ both were used in size 2 as per the recommendations. LMA-Supreme™ was inflated with air so as to maintain cuff pressure of 60 cmH2O. I-gel™ did not have inflatable cuff. The device was fixed to chin with taping.
The head and neck was placed in neutral position which was maintained with the external ear canal and the top of the shoulder forming an imaginary line which should be perpendicular to the ear eye line (from the external ear canal to the superior orbital margin). Then, the patient was repositioned in the following positions: maximal extension, maximal flexion, and measurement started after 30–60 s. Maximal flexion was obtained by flexing the neck at point when chin touches sternum. Maximal extension was achieved by extending neck till resistance was felt. In each position, OPLP was measured and fiberoptic view grading was obtained. OPLP was measured by the detection of audible leak after closing adjustable pressure limiting valve and maintaining fresh gas flow fixed at 3 L/min. Pressure was measured by manometer at the time of leak. Maximum airway pressure limit was 40 cmH2O. Fiberoptic view was obtained by passing a flexible fiberoptic scope (size 4.5 mm), 1 cm proximal to the airway orifice. Fiberoptic view was graded as Grade 1 - when only larynx seen, Grade 2 - larynx and epiglottis posterior surface seen, Grade 3 - larynx and epiglottis tip of anterior surface seen, <50% visual obstruction of epiglottis to larynx, Grade 4 - epiglottis downfolded and its anterior surface seen, >50% visual obstruction of epiglottis to larynx, and Grade 5 - epiglottis downfolded and larynx not seen. Exhaled tidal volume was measured in neutral, flexion, and extension position with flow sensor analyzer applied to device and reading noted from the anesthesia machine.
Statistical analysis
All data were entered into Microsoft Excel Spreadsheet and OPLP and exhaled tidal volume were evaluated in three different head positions and mean and standard deviation was calculated. Fiberoptic view was also evaluated and calculated according to the predetermined grading system and analyzed with Kruskal–Wallis rank test and Mann–Whitney U-test. Test of significance was performed with IBM SPSS 20 software (Statistical Package for the Social Sciences, Amonk, New York, USA), and P < 0.05 was considered statistically significant, considering confidence interval of 95%.
RESULTS
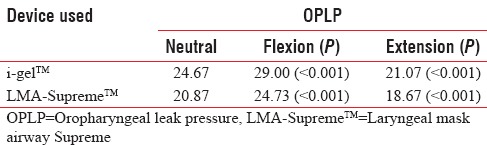
A total of sixty patients were considered into study, thirty each in i-gel™ and LMA-Supreme™ group. All children were within the age group of 2–5 years with mean age of 3.91 years. Mean weight of all children was 15.30 kg (11–20 kg). OPLP and exhaled tidal volume were measured in neutral position first and then in flexion or extension position and evaluated for both devices. OPLP for i-gel™ was 24.67 ± 2.06 versus 29.00 ± 1.95 cmH2O for neutral and flexion position (P < 0.001) and 24.67 ± 2.06 versus 21.07 ± 2.08 cmH2O for neutral and extension position (P < 0.001), respectively. These results clearly indicates higher sealing pressure in flexion position and lower sealing pressure in extension as compared to neutral position for i-gel™. Similar results were observed for LMA-Supreme™, which showed OPLP of 20.87 ± 1.80 versus 24.73 ± 2.26 cmH2O for neutral and flexion position (P < 0.001) and 20.87 ± 1.80 versus 18.67 ± 1.42 cmH2O for neutral and extension position (P < 0.001), respectively [Table 1].
Table 1.
Oropharyngeal leak pressure in various positions for i-gel™ and LMA-Supreme™
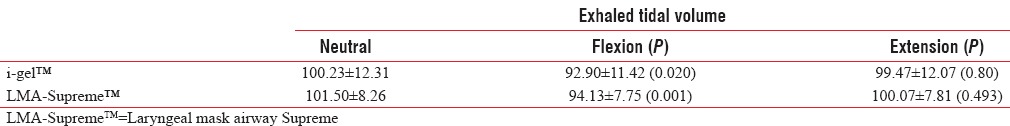
Exhaled tidal volume was significantly decreased in flexion (92.90 ± 11.42 and 94.13 ± 7.75 ml, P < 0.05) for i-gel™ and LMA-Supreme™, respectively. A significant change did not occur during extension [Table 2].
Table 2.
Exhaled tidal volume in different neck positions in i-gel™ and LMA-Supreme™
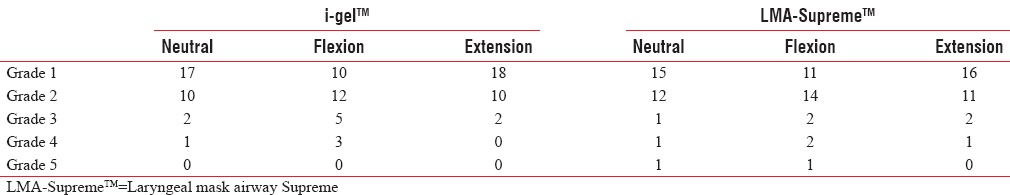
Fiberoptic grading was also compared for both devices in flexion and extension to neutral position. For i-gel™, fiberoptic view in neutral position for grade 1/2/3/4/5 was 17/10/2/1/0, respectively, which decreased significantly in flexion position to 10/12/5/3/0 (P < 0.05) but was similar to view in extension position 18/10/2/0/0 and no significant difference was found (P > 0.05). Similar results were obtained for LMA-Supreme™ where fiberoptic view in neutral position was 15/12/1/1/1 for grade 1/2/3/4/5, respectively, and it changed to 11/14/2/2/1 in flexion (P < 0.05) and 16/11/2/1/0 in extension (P > 0.05) [Table 3].
Table 3.
Fiberoptic view grading in various positions for i-gel™ and LMA-Supreme™
DISCUSSION
Pediatric patients have specific airway characteristics that are quite different from those of adults, and their intubation therefore has a number of unique features. This age group is likely to be associated with higher rates of complications of laryngoscopy and intubation. Supraglottic airways (SGAs) have an important place in pediatric use because a large number of day care surgeries may be performed in this age group without the use of endotracheal intubation; hence, SADs have been increasingly used in recent years in suitable cases.
I-gel™ and LMA-Supreme™ are newly devised second-generation supraglottic devices which are recent introduction in long line of supraglottic devices. Many SGAs are available in single-use and reusable versions. The i-gel™ and the LMA-Supreme™ are used for maintaining airway in children during controlled and spontaneous ventilation under general anesthesia; the esophageal drainage tubes in these devices may reduce the risk of airway contamination. Furthermore, noninfatable cuff of i-gel™ avoids the need for cuff pressure monitoring and possibility of mucosal injury from over inflation. Ideal supraglottic device should have OPLP sufficient for positive pressure ventilation even with various neck positions.
Many times, different neck positions are required depending on the type of surgery such as neck extension is required for thyroid surgery, neck exploration, laser pharyngoplasty, and tonsillectomy, whereas neck flexion is required for tracheal resection and occiput surgeries. In our study, OPLP of i-gel™ was significantly higher than LMA-Supreme™ and provided better sealing pressure in all neck positions. The value of OPLP for i-gel™ was similar to previous study conducted by Goyal et al.[12] Previous studies conducted have shown higher OPLP for i-gel™ as compared to LMA ProSeal™ and LMA-Classic™.[13] Higher leak pressure provides particular advantage during lithotomy, pneumoperitoneum, obese, and restrictive lung disease.[14]
Our study has shown that OPLP or sealing pressure was significantly higher for flexion position as compared to neutral position for both i-gel™ and LMA-Supreme™. In addition, OPLP for neck extension was significantly lower to neutral position among both devices. All these findings can be explained by anatomy of pediatric upper airway. Mishra et al. showed similar results of increase in OPLP in flexion and fall in extension for i-gel™ in adult population.[15] They found OPLP of neutral position at 22 cm, at flexion 25 cm, and at extension 19 cmH2O, which was lower than our findings. Xue et al. also showed a significant increase in OPLP with improvement in ventilation with neck flexion but study restricted itself to adult population.[16] Isserles and Rozenberg suggested that neck flexion removes the longitudinal tension in anterior pharyngeal muscles, allowing them to settle down onto the mask to form a better seal and provide higher leak pressure. Neck flexion causes reduction in anteroposterior diameter of pharynx and neck extension causes increase in anteroposterior diameter by raising the hyoid and the laryngeal inlet.[17] It also gives us scope to flex neck maneuvers to improve sealing pressure.
Fiberoptic scoring system is generally used to assess proper positioning and airway seal function of the LMAs. No major studies have evaluated and compared i-gel™ and LMA-Supreme™ for fiberoptic view in different neck positions among spontaneously breathing pediatric patients. Unlike adults, epiglottis of children is large, floppy, and more horizontally placed and hence different criteria were needed to evaluate fiberoptic view in children to assess optimal placement of device. Fiberoptic view is said to be best in extension position and worst in flexion due to decreased deflection of epiglottis in extension and increased deflection in flexion position as proposed by Okuda et al.[18] Our study confirmed the fall in quality of vocal cords view on flexion of neck which was statistically significant, but we failed to document better view on extension as compared to neutral position. The observation made by us cannot be used in neonates and infants. Further, the change in neck positions was done at maximal flexion and extension and changes in parameters with lesser degree of movement was not documented.
CONCLUSION
Neck flexion causes increase in leak pressure in both i-gel™ and LMA-Supreme™, whereas extension causes fall in leak pressure in spontaneously breathing pediatric patients.
Vocal cords view worsened severely with neck flexion although there was no significant change in extension.
Deterioration of ventilation occurs during flexion of head and neck; hence, both devices should be used cautiously in pediatric patients in extreme flexion.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.van Zundert TC, Brimacombe JR, Ferson DZ, Bacon DR, Wilkinson DJ. Archie Brain: Celebrating 30 years of development in laryngeal mask airways. Anaesthesia. 2012;67:1375–85. doi: 10.1111/anae.12003.x. [DOI] [PubMed] [Google Scholar]
- 2.I-gel user guide; I-gel Instruction manual. Intersurgical. 2016 [Google Scholar]
- 3.Beylacq L, Bordes M, Semjen F, Cros AM. The i-gel, a single-use supraglottic airway device with a non-inflatable cuff and an esophageal vent: An observational study in children. Acta Anaesthesiol Scand. 2009;53:376–9. doi: 10.1111/j.1399-6576.2008.01869.x. [DOI] [PubMed] [Google Scholar]
- 4.Beringer RM, Kelly F, Cook TM, Nolan J, Hardy R, Simpson T, et al. A cohort evaluation of the paediatric i-gel™ airway during anaesthesia in 120 children. Anaesthesia. 2011;66:1121–6. doi: 10.1111/j.1365-2044.2011.06884.x. [DOI] [PubMed] [Google Scholar]
- 5.Verghese C, Ramaswamy B. LMA-Supreme – A new single-use LMA with gastric access: A report on its clinical efficacy. Br J Anaesth. 2008;101:405–10. doi: 10.1093/bja/aen174. [DOI] [PubMed] [Google Scholar]
- 6.Das B, Mitra S, Jamil SN, Varshney RK. Comparison of three supraglottic devices in anesthetised paralyzed children undergoing elective surgery. Saudi J Anaesth. 2012;6:224–8. doi: 10.4103/1658-354X.101212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mitra S, Das B, Jamil SN. Comparison of size 2.5 i-gel™ with proseal LMA™ in anaesthetised, paralyzed children undergoing elective surgery. N Am J Med Sci. 2012;4:453–7. doi: 10.4103/1947-2714.101983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Keller C, Brimacombe J. The influence of head and neck position on oropharyngeal leak pressure and cuff position with the flexible and the standard laryngeal mask airway. Anesth Analg. 1999;88:913–6. doi: 10.1097/00000539-199904000-00042. [DOI] [PubMed] [Google Scholar]
- 9.Buckham M, Brooker M, Brimacombe J, Keller C. A comparison of the reinforced and standard laryngeal mask airway: Ease of insertion and the influence of head and neck position on oropharyngeal leak pressure and intracuff pressure. Anaesth Intensive Care. 1999;27:628–31. doi: 10.1177/0310057X9902700612. [DOI] [PubMed] [Google Scholar]
- 10.Chauhan G, Nayar P, Seth A, Gupta K, Panwar M, Agrawal N. Comparison of clinical performance of the i-gel with LMA proseal. J Anaesthesiol Clin Pharmacol. 2013;29:56–60. doi: 10.4103/0970-9185.105798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fukuhara A, Okutani R, Oda Y. A randomized comparison of the i-gel and the ProSeal laryngeal mask airway in pediatric patients: Performance and fiberoptic findings. J Anesth. 2013;27:1–6. doi: 10.1007/s00540-012-1477-4. [DOI] [PubMed] [Google Scholar]
- 12.Goyal R, Shukla RN, Kumar G. Comparison of size 2 i-gel supraglottic airway with LMA-ProSeal™ and LMA-Classic™ in spontaneously breathing children undergoing elective surgery. Paediatr Anaesth. 2012;22:355–9. doi: 10.1111/j.1460-9592.2011.03757.x. [DOI] [PubMed] [Google Scholar]
- 13.Maitra S, Baidya DK, Bhattacharjee S, Khanna P. Evaluation of i-gel™ airway in children: A meta-analysis. Paediatr Anaesth. 2014;24:1072–9. doi: 10.1111/pan.12483. [DOI] [PubMed] [Google Scholar]
- 14.Lopez-Gil M, Brimacombe J. The ProSeal laryngeal mask airway in children. Paediatr Anaesth. 2005;15:229–34. doi: 10.1111/j.1460-9592.2005.01427.x. [DOI] [PubMed] [Google Scholar]
- 15.Mishra SK, Nawaz M, Satyapraksh MV, Parida S, Bidkar PU, Hemavathy B, et al. Influence of head and neck position on oropharyngeal leak pressure and cuff position with the ProSeal laryngeal mask airway and the i-gel: A randomized clinical trial. Anesthesiol Res Pract 2015. 2015 doi: 10.1155/2015/705869. 705869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Xue FS, Mao P, Liu HP, Yang QY, Li CW, He N, et al. The effects of head flexion on airway seal, quality of ventilation and orogastric tube placement using the ProSeal laryngeal mask airway. Anaesthesia. 2008;63:979–85. doi: 10.1111/j.1365-2044.2008.05490.x. [DOI] [PubMed] [Google Scholar]
- 17.Isserles SA, Rosenberg B. LMA: Reduction of gas leak. Can J Anaesth. 1995;42:449. doi: 10.1007/BF03015498. [DOI] [PubMed] [Google Scholar]
- 18.Okuda K, Inagawa G, Miwa T, Hiroki K. Influence of head and neck position on cuff position and oropharyngeal sealing pressure with the laryngeal mask airway in children. Br J Anaesth. 2001;86:122–4. doi: 10.1093/bja/86.1.122. [DOI] [PubMed] [Google Scholar]


