Abstract
Background:
Gabapentinoids have been used as preemptive analgesics for pain management following laparoscopic cholecystectomy. Recently, multimodal analgesic techniques have been found superior to preemptive analgesia alone.
Aim:
The aim of this study is to evaluate and compare a single preoperative dose of pregabalin 150 mg and gabapentin 300 mg for pain relief following laparoscopic cholecystectomy as a part of multimodal drug regime.
Settings and Design:
This randomized, single-blind study was conducted after Ethical Committee approval and written informed consent from the patients.
Materials and Methods:
Fifty patients undergoing laparoscopic cholecystectomy under general anesthesia were randomly allocated to receive either 150 mg pregabalin (Group PG), or 300 mg gabapentin (Group GB) orally, 2 h before surgery. Standard anesthesia induction and maintenance were done. For intraoperative pain management, injection fentanyl 2 μg.kg-1 intravenous (IV) along with injection voveran 75 mg IV and port site infiltration was used. Postoperatively, injection diclofenac 75 mg intramuscular TDS was continued. Severity of postoperative pain (visual analog scale [VAS]), postoperative fentanyl requirement and incidence, and severity of side effects were assessed. When VAS >40 mm or on patient's request, a Fentanyl bolus at an increment of 25–50 μg IV was given as rescue analgesia.
Results:
Intraoperative fentanyl requirement was 135 ± 14 μg in Group PG and 140 ± 14 μg in Group GB (P = 0.21). Postoperative, fentanyl requirement was 123 ± 18 μg in Group PG and 131 ± 23 μg in Group GB (P = 0.17) There was no statistically significant difference in the VAS score for static and dynamic pain. Time to the first requirement of analgesic was 5.4 ± 1.1 h in Group PG and 4.6 ± 1.6 h in Group GB (P = 0.015). No side effects were observed.
Conclusion:
We conclude that a single preoperative dose of pregabalin (150 mg) or gabapentin (300 mg) are equally efficacious in providing pain relief following laparoscopic cholecystectomy as a part of multimodal regime without any side effects.
Keywords: Gabapentin, laparoscopic cholecystectomy, multi-modal analgesia, pregabalin
INTRODUCTION
Multimodal analgesic techniques have gained popularity for postoperative pain management. The major advantage being superior pain control with reduced side effects as opioids consumption is decreased. Drugs used include nonsteroidal anti-inflammatory drugs, selective cyclooxygenase-2 inhibitors, N-methyl-D-aspartate antagonists, alpha-2 adrenergic agonists, gabapentinoids, and local anesthetic injection at the surgical site.[1]
Gabapentinoids drugs (gabapentin and pregabalin) were developed originally as anticonvulsants and subsequently found to be effective in neuropathic and postoperative pain management.[2,3,4,5]
Pregabalin compared to gabapentin has better pharmacokinetic profile with rapid absorption, higher bioavailability, and less intersubject variability.[6] Animal studies show that pregabalin is 3–10-folds more potent than gabapentin as an epileptic and 2–4-fold more potent as an analgesic in the treatment of chronic neuropathic pain.[7,8]
Various studies separately evaluating the role of these drugs for pain relief following laparoscopic cholecystectomy show that a single preoperative dose of pregabalin (150 mg) or gabapentin (300 mg) is effective in reducing pain scores and opioid consumption.[9,10,11]
Recently studies have been done comparing the effectiveness of these drugs as preemptive analgesics in prolonging the duration of spinal anesthesia. Both the drugs prolong the duration of postoperative analgesia compared to placebo. Pregabalin (300 mg) was found to be superior to gabapentin (900–1200 mg).[12,13,14]
Mishra et al. compared pregabalin (150 mg) and gabapentin (900 mg) for pain relief following laparoscopic cholecystectomy. Both the drugs were found to be effective in reducing pain as compared to placebo. Side effects including sedation, nausea vomiting, respiratory depression, and vertigo were observed in all the groups.[15]
Recent research shows that preventive analgesia using multimodal techniques in the perioperative period is more effective than using drugs preincision (preemptive analgesia).[16] None of these studies show the effects of these drugs when a multimodal approach to pain management is used.
Hence, we planned a study to evaluate and compare a single preoperative dose of pregabalin 150 mg and gabapentin 300 mg for pain relief following laparoscopic cholecystectomy as a part of multimodal drug regime.
MATERIALS AND METHODS
This randomized, single-blind study was conducted in the Department of Anaesthesiology, Hamdard Institute of Medical Sciences and Research after taking approval of the Institutional Ethical Committee and written informed consent from the patients.
Adult patients of either sex, age (18–60 years), with physical status American Society of Anesthesiologists (ASA) Classes I and II, undergoing laparoscopic cholecystectomy under general anesthesia were included in the study. Patients having history of chronic pain, drug abuse, pregnancy, and altered kidney or liver function were excluded from the study.
Patients meeting the inclusion criteria during the preanesthetic evaluation were randomly assigned into two groups of 25 each with the help of a computer-generated table of random numbers, to receive either 150 mg pregabalin (Group PG) or 300 mg gabapentin (Group GB). All the medications were provided by hospital pharmacy and were administered orally, 2 h before the induction of anesthesia with sips of water by a staff nurse who was not involved in the study.
Anesthesia technique was standardized in both the groups. Patients were induced with fentanyl 2 μg.kg-1 intravenous (IV) and propofol 2 mg.kg-1 IV; orotracheal intubation was facilitated by vecuronium 0.08mg.kg-1 IV. Anesthesia was maintained using isoflurane and 66% nitrous oxide in oxygen. Supplemental fentanyl bolus and vecuronium were given as per anesthesiologist's discretion. All patients were given a single IV dose of prophylactic antiemetic, ondansetron 4 mg. Injection voveran 75 mg IV and port site infiltration with 0.25% bupivacaine were given for postoperative analgesia as a part of multimodal analgesic technique. At the end of surgery, residual neuromuscular paralysis was antagonized with neostigmine 0.05 mg.kg-1 IV and glycopyrrolate 0.01 mg.kg-1 IV. After satisfactory recovery, the patients were extubated and shifted to the postanesthesia Care Unit (PACU).
When visual analog scale (VAS) >40 mm or patient's request, a fentanyl bolus at an increment of 25–50 μg IV was titrated with the standard protocol in the PACU. Injection diclofenac 75 mg intramuscular TDS was continued postoperatively.
Severity of postoperative pain, postoperative fentanyl requirement, incidence, and severity of side effects such as postoperative nausea and vomiting, shivering headache, sedation, vision abnormalities (blurring of vision, double vision), and respiratory depression, if any were recorded.
The primary outcome was severity of postoperative pain and postoperative analgesic requirement and secondary outcome the incidence and severity of side effects. Both these outcomes were assessed by an independent anesthesiologist blinded to group allocation. Assessment of pain both at rest (static) and during coughing (dynamic) was done by a 100 mm VAS; 0, no pain; 100, worst imaginable pain. Assessment of pain was done on arrival of the patient to the PACU (0) and then every 2 h till the end of the study, that is, 24 h after operation. Sedation was assessed by Ramsay sedation score. Patients having sedation score >2 were considered sedated.
Statistical analysis
A reduction of VAS score to 30 mm was considered effective. With an α error of 0.05 and power of 80%, a sample size of 25 patients in each group was taken. Maximum pain scores at different time intervals (0, 0–4, 4–8, 8–12, and 12–24 h) for each patient were considered for statistical analysis. Student's t-test was used for calculating fentanyl consumption.
RESULTS
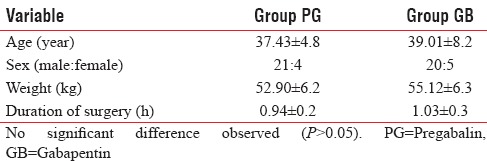
A total of fifty patients were enrolled, all the patients were ASA Grade I. There were no dropouts. There was no significant difference in demographic profile and duration of surgery [Table 1].
Table 1.
Demographic data and duration of surgery (mean±standard deviation)
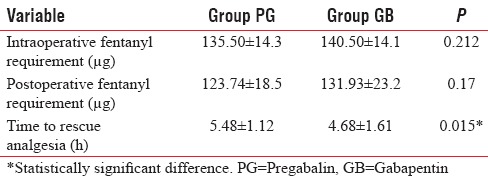
Intraoperative fentanyl requirement was 135 ± 14 μg in Group PG and 140 ± 14 μg in Group GB (P = 0.21) [Table 2].
Table 2.
Fentanyl requirement and time to first analgesic request (mean±standard deviation)
Patients who received pregabalin 150 mg (Group PG) had comparatively lower VAS scores for static pain at all time intervals compared those who received gabapentin (Group GB). The difference was not statistically significant [Figure 1].
Figure 1.
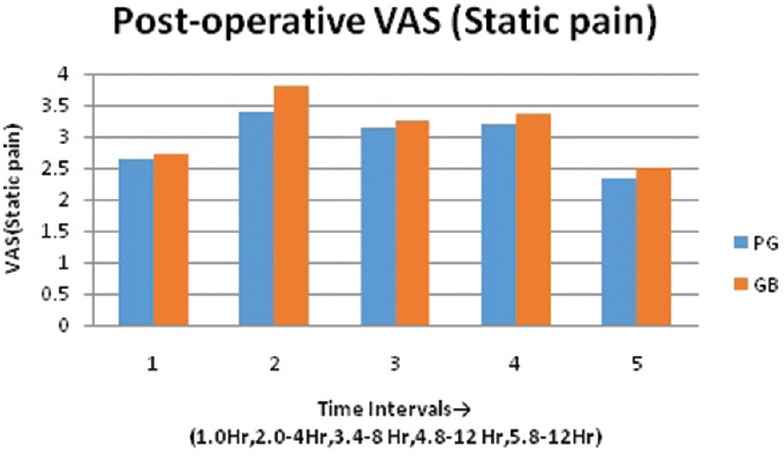
Postoperative visual analog scale (static pain). No statistically significant difference in visual analog scale (static pain) at all intervals
Dynamic pain scores (VAS) were lower in Group PG as compared to Group GB at all intervals. The difference was not statistically significant [Figure 2].
Figure 2.
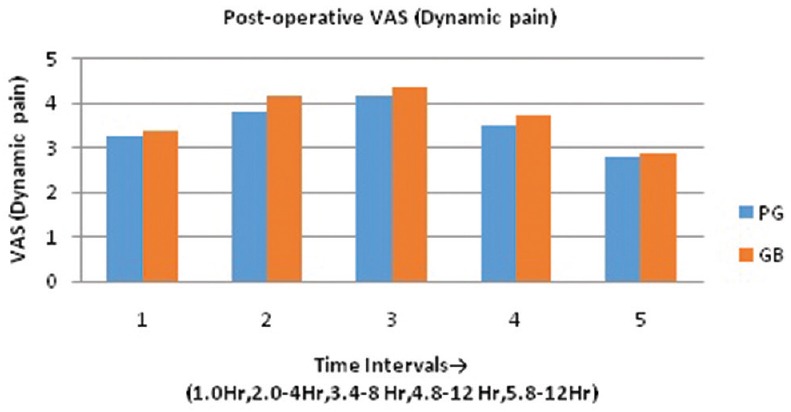
Postoperative visual analog scale (dynamic pain). No statistically significant difference in visual analog scale (dynamic pain) at all intervals
Time to first requirement of analgesic was 5.4 ± 1.1 h in Group PG and 4.6 ± 1.6 h in Group GB. The difference was found to be statistically significant (P = 0.015) [Figure 3].
Figure 3.
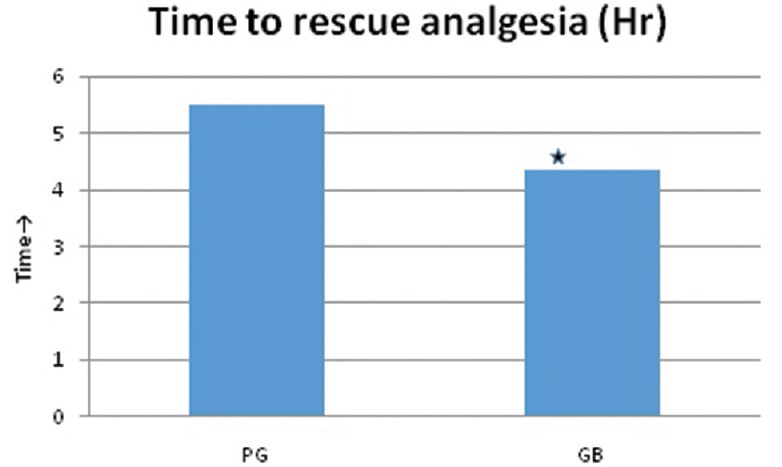
Time to rescue analgesia. The difference was statistically significant (P = 0.015)
Postoperative fentanyl requirement was 123 ± 18 μg in Group PG and 131 ± 23 μg in Group GB. The difference was found to be statistically nonsignificant (P = 0.17) [Table 2].
Twelve percent of patients in Group PG and 8% in Group GB were observed to have sedation levels >2 in the immediate postoperative period. None of the other side effects were observed.
DISCUSSION
Gabapentinoids have been recommended for perioperative administration to improve acute pain after surgery and are being used as a part of multimodal approach to postoperative pain control.[1] These drugs reduce the hyperexcitability of dorsal horn neurons induced by tissue damage rather than affecting afferent input from the site of injury.[17]
We used a single preoperative dose of pregabalin 150 mg and gabapentin 300 mg. Dose selection was based on pharmacokinetic, pharmacodynamics, and side effects of both the drugs reported in literature. The relative potency of pregabalin is 2–4-fold higher with favorable pharmacokinetic profile.[7,8]
Various studies show that 150 mg of pregabalin administered 1 h before surgery is effective with minimal side effects where as lower dose of pregabalin (50–75 mg) does not reduce opioid consumption following laparoscopic cholecystectomy.[9,10,18]
Optimal dose of gabapentin for laparoscopic cholecystectomy has not been identified. Pandey et al. evaluated optimal dose of gabapentin for lumbar discectomy. Optimal dose was identified to be 600 mg. Laparoscopic cholecystectomy comparative less painful procedure than lumbar discectomy. In addition, gabapentin 300 mg has been shown to be effective in reducing postoperative pain and opioid consumption following laparoscopic cholecystectomy and lower limb orthopedic surgery.[11,19,20]
Studies show that higher doses of pregabalin (300–600 mg) and gabapentin (600–1200 mg) can produce side effects such as sedation, dizziness, and blurred vision.[21,22,23,24]
The results of our study show no statistically significant difference in the static and dynamic pain scores in both the groups.
Our results are in contrast with those reported by Mishra et al., who compared pregabalin (150 mg) with gabapentin (900 mg) and placebo, in patients undergoing laparoscopic cholecystectomy. All the drugs were given 1 h preoperatively. Postoperative pain management was done using injection tramadol. The results of their study show lower VAS score in the Groups PG and GB than placebo. Among gabapentinoids, Group PG had lower VAS scores.[15]
Major reasons for these differences might be due to use of drugs 2 h before surgery and multimodal approach of pain management in our study. Pharmacokinetic properties of gabapentin show that its bioavailability varies inversely with dose (single dose of 300 mg and 600 mg has bioavailability of 60% and 40% respectively) and peak effect occurs in 2–3 h. Preventive analgesia using multimodal approach helps in reducing postoperative pain and analgesic requirement. The dose of individual drug is reduced. Mechanism of preventive analgesia being decrease in hyperalgesia, peripheral, and central sensitization.[16]
The requirement of supplemental doses of fentanyl in the postoperative period was similar in both the groups. Ghai et al. compared the effects of gabapentin (900 mg) and pregabalin (300 mg) in patients undergoing hysterectomy. The consumption of diclofenac was similar in Group PG and GB.[25]
In our study, time to rescue analgesia was found to be longer in Group PG. Similar findings were observed in the study was conducted by Saraswat and Arora comparing the analgesic efficacy of gabapentin (1200 mg) and pregabalin (300 mg) in surgery under spinal anesthesia. The duration of analgesia was 8.9 h in Group GB and 14.17 h in Group PG.[26]
Three of the patients in pregabalin were observed to be sedated compared to two in gabapentin. None of our patients had any other adverse effects.
Side effects reported by Ghai et al. include high incidence of somnolence (40% and 33.3% with pregabalin 300 mg and gabapentin 900 mg respectively). Saraswat and Arora observed sedation and dizziness in both the groups (1200 mg of gabapentin vs. 300 mg of pregabalin).
Lesser incidence of side effects observed in our study may be due to lower doses of pregabalin and gabapentin used and use of multimodal regime to reduce the requirement of opioids.
Major limitation of our study was not observing pain scores and opioid requirement without premedication with gabapentinoids (no control group).
CONCLUSION
A single pre-operative dose of pregabalin (150 mg) or gabapentin (300 mg) are equally efficacious in providing pain relief following laproscopic cholecystectomy as a part of multi-modal regime without any side effects.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
Authors would like to thank the Department of Surgery, Hamdard Institute of Medical Sciences and Research, Jamia Hamdard, New Delhi, India.
REFERENCES
- 1.Buvanendran A, Kroin JS. Multimodal analgesia for controlling acute postoperative pain. Curr Opin Anaesthesiol. 2009;22:588–93. doi: 10.1097/ACO.0b013e328330373a. [DOI] [PubMed] [Google Scholar]
- 2.Ho KY, Gan TJ, Habib AS. Gabapentin and postoperative pain – A systematic review of randomized controlled trials. Pain. 2006;126:91–101. doi: 10.1016/j.pain.2006.06.018. [DOI] [PubMed] [Google Scholar]
- 3.Kong VK, Irwin MG. Gabapentin: A multimodal perioperative drug? Br J Anaesth. 2007;99:775–86. doi: 10.1093/bja/aem316. [DOI] [PubMed] [Google Scholar]
- 4.Tiippana EM, Hamunen K, Kontinen VK, Kalso E. Do surgical patients benefit from perioperative gabapentin/pregabalin? A systematic review of efficacy and safety. Anesth Analg. 2007;104:1545–56. doi: 10.1213/01.ane.0000261517.27532.80. [DOI] [PubMed] [Google Scholar]
- 5.Zhang J, Ho KY, Wang Y. Efficacy of pregabalin in acute postoperative pain: A meta-analysis. Br J Anaesth. 2011;106:454–62. doi: 10.1093/bja/aer027. [DOI] [PubMed] [Google Scholar]
- 6.Gajraj NM. Pregabalin: Its pharmacology and use in pain management. Anesth Analg. 2007;105:1805–15. doi: 10.1213/01.ane.0000287643.13410.5e. [DOI] [PubMed] [Google Scholar]
- 7.Bryans JS, Wustrow DJ. 3-substituted GABA analogs with central nervous system activity: A review. Med Res Rev. 1999;19:149–77. doi: 10.1002/(sici)1098-1128(199903)19:2<149::aid-med3>3.0.co;2-b. [DOI] [PubMed] [Google Scholar]
- 8.Lauria-Horner BA, Pohl RB. Pregabalin: A new anxiolytic. Expert Opin Investig Drugs. 2003;12:663–72. doi: 10.1517/13543784.12.4.663. [DOI] [PubMed] [Google Scholar]
- 9.Agarwal A, Gautam S, Gupta D, Agarwal S, Singh PK, Singh U. Evaluation of a single preoperative dose of pregabalin for attenuation of postoperative pain after laparoscopic cholecystectomy. Br J Anaesth. 2008;101:700–4. doi: 10.1093/bja/aen244. [DOI] [PubMed] [Google Scholar]
- 10.Balaban F, Yagar S, Özgök A, Koç M, Güllapoglu H. A randomized, placebo-controlled study of pregabalin for postoperative pain intensity after laparoscopic cholecystectomy. J Clin Anesth. 2012;24:175–8. doi: 10.1016/j.jclinane.2011.06.027. [DOI] [PubMed] [Google Scholar]
- 11.Pandey CK, Priye S, Singh S, Singh U, Singh RB, Singh PK. Preemptive use of gabapentin significantly decreases postoperative pain and rescue analgesic requirements in laparoscopic cholecystectomy. Can J Anaesth. 2004;51:358–63. doi: 10.1007/BF03018240. [DOI] [PubMed] [Google Scholar]
- 12.Rajendran I, Basavareddy A, Meher BR, Srinivasan S. Prospective, randomised, double blinded controlled trial of gabapentin and pregabalin as pre emptive analgesia in patients undergoing lower abdominal and limb surgery under spinal anaesthesia. Indian J Pain. 2014;28:155–9. [Google Scholar]
- 13.Kohli M, Murali T, Gupta R, Khan P, Bogra J. Optimization of subarachanoid block by oral pregabalin for hysterectomy. J Anaesthesiol Clin Pharmacol. 2011;27:101–5. [PMC free article] [PubMed] [Google Scholar]
- 14.Pal S, Dasgupta S, Mukhopadhyay S, Chaudhuri A. A comparative study between oral pregabalin and gabapentin in prolongation of postoperative pain relief after spinal anesthesia. Indian J Pain. 2016;30:7–12. [Google Scholar]
- 15.Mishra R, Tripathi M, Chandola HC. Comparative clinical study of gabapentin and pregabalin for postoperative analgesia in laparoscopic cholecystectomy. Anesth Essays Res. 2016;10:201–6. doi: 10.4103/0259-1162.176409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Vadivelu N, Mitra S, Schermer E, Kodumudi V, Kaye AD, Urman RD. Preventive analgesia for postoperative pain control: A broader concept. Local Reg Anesth. 2014;7:17–22. doi: 10.2147/LRA.S62160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gilron I. Gabapentin and pregabalin for chronic neuropathic and early postsurgical pain: Current evidence and future directions. Curr Opin Anaesthesiol. 2007;20:456–72. doi: 10.1097/ACO.0b013e3282effaa7. [DOI] [PubMed] [Google Scholar]
- 18.Peng PW, Li C, Farcas E, Haley A, Wong W, Bender J, et al. Use of low-dose pregabalin in patients undergoing laparoscopic cholecystectomy. Br J Anaesth. 2010;105:155–61. doi: 10.1093/bja/aeq116. [DOI] [PubMed] [Google Scholar]
- 19.Pandey CK, Navkar DV, Giri PJ, Raza M, Behari S, Singh RB, et al. Evaluation of the optimal preemptive dose of gabapentin for postoperative pain relief after lumbar diskectomy: A randomized, double-blind, placebo-controlled study. J Neurosurg Anesthesiol. 2005;17:65–8. doi: 10.1097/01.ana.0000151407.62650.51. [DOI] [PubMed] [Google Scholar]
- 20.Montazeri K, Kashefi P, Honarmand A. Pre-emptive gabapentin significantly reduces postoperative pain and morphine demand following lower extremity orthopaedic surgery. Singapore Med J. 2007;48:748–51. [PubMed] [Google Scholar]
- 21.Sarakatsianou C, Theodorou E, Georgopoulou S, Stamatiou G, Tzovaras G. Effect of pre-emptive pregabalin on pain intensity and postoperative morphine consumption after laparoscopic cholecystectomy. Surg Endosc. 2013;27:2504–11. doi: 10.1007/s00464-012-2769-3. [DOI] [PubMed] [Google Scholar]
- 22.Jokela R, Ahonen J, Tallgren M, Haanpää M, Korttila K. A randomized controlled trial of perioperative administration of pregabalin for pain after laparoscopic hysterectomy. Pain. 2008;134:106–12. doi: 10.1016/j.pain.2007.04.002. [DOI] [PubMed] [Google Scholar]
- 23.Kim SY, Jeong JJ, Chung WY, Kim HJ, Nam KH, Shim YH. Perioperative administration of pregabalin for pain after robot-assisted endoscopic thyroidectomy: A randomized clinical trial. Surg Endosc. 2010;24:2776–81. doi: 10.1007/s00464-010-1045-7. [DOI] [PubMed] [Google Scholar]
- 24.Turan A, Memis D, Karamanlioglu B, Yagiz R, Pamukçu Z, Yavuz E. The analgesic effects of gabapentin in monitored anesthesia care for ear-nose-throat surgery. Anesth Analg. 2004;99:375–8. doi: 10.1213/01.ANE.0000136646.11737.7B. [DOI] [PubMed] [Google Scholar]
- 25.Ghai A, Gupta M, Hooda S, Singla D, Wadhera R. A randomized controlled trial to compare pregabalin with gabapentin for postoperative pain in abdominal hysterectomy. Saudi J Anaesth. 2011;5:252–7. doi: 10.4103/1658-354X.84097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Saraswat V, Arora V. Preemptive gabapentin vs. pregabalin for acute post-operative pain after surgery under spinal anaesthesia. Indian J Anaesth. 2008;52:829–34. [Google Scholar]


