Abstract
Objective:
This study aims to assess the role of herpesviruses in chronic periodontitis and their association with clinical parameters and in increasing severity.
Materials and Methods:
This was a prospective case–control study. Ethical approval and prior consent were taken. A subgingival plaque sample was collected from a total of 300 patients and 300 controls and processed for DNA extraction and multiplex polymerase chain reaction for detection of herpesviruses.
Results:
The most predominant age group affected was 41–50 followed by 31–40 years and male patients outnumbered the female patients. Herpes simplex virus (HSV)-1 (46.6%) was the most common Herpesvirus followed by HSV-2 (34.6%), Epstein–Barr viruses (EBV) (30.6%), and cytomegalovirus (CMV) (19.3%) in chronic periodontitis. Herpesviruses were significantly associated with increasing severity of the disease and had shown differences in their association with clinical parameters. Multiple herpesvirus infection was seen in patients with severe chronic periodontitis. The most common combination was HSV-1 + HSV-2 and HSV-1 + HSV-2 + EBV.
Conclusions:
HSV-1 was the most common herpesviruses implicated in the etiology of the chronic periodontitis followed by HSV-2, EBV and CMV. A herpesvirus differs in association with clinical parameters and plays an important role in increasing severity of the disease.
Keywords: Chronic periodontitis, clinical parameters, herpesviruses, multiplex polymerase chain reaction, severity
INTRODUCTION
Periodontal diseases are the most common oro-dental conditions in India.[1] Chronic periodontitis is an infectious disease which leads to inflammation of gingiva and unless treated appropriately leads to loss of the tooth. The most commonly reported etiological agents from this condition are anaerobes.[2] Bacterial etiology alone cannot explain the clinic-pathological features observed in the disease. Thus, efforts to find out additional etiological agents for chronic periodontitis are necessary. A new concept has emerged during the past decade concerning the contribution of herpesviruses in etiopathogenesis of the chronic periodontitis. There are several studies showing the evidence of herpesviruses and chronic periodontitis on the basis of their presence in the diseased sites and absence in the healthy controls.[3,4]
However, in India, very few studies have been undertaken to know the role of herpesviruses in chronic periodontitis. The currently available studies have been conducted with a small sample size and from limited areas.[5,6] The present study was undertaken to assess the role of herpesviruses including herpes simplex virus Type 1 and 2 (HSV-1 and 2), cytomegalovirus (CMV), and Epstein–Barr viruses (EBV) in chronic periodontitis and to see their effects on clinical parameters used to monitor chronic periodontitis such as oral hygiene, plaque index, gingival index, bleeding on probing, clinical attachment loss, and pocket depth and to assess their role in increasing severity of the disease.
MATERIALS AND METHODS
A prospective case–control study was undertaken after ethical approval from the Institutional Ethical Committee of B. J. Government Medical College and the no is D-1210169-71. Informed consent was obtained before enrolling patients in the study. The selection criteria for enrolling patients with chronic periodontitis in the study were as per those of the American Academy of Periodontology. The study period was from June 2011 to December 2014 in Sinhgad Dental College and Hospital and B. J. Government Medical College Pune India. A total of 300 cases (100 each from mild, moderate, and severe chronic periodontitis) and 300 age- and sex-matched healthy controls were included in the present study. An inclusion criterion for the patient was generalized chronic periodontitis with different grades of severity, free from systemic diseases including diabetes, no smoking history as well as HIV infection. While exclusion criteria include patients with treated within 3 months, systemic diseases, smoking, and HIV infections. Before collecting the specimen, patients were instructed not to brush their teeth for at least 2 h before collection of specimen. A dedicated periodontologist collected subgingival plaque specimen with the help of sterile curette and paper points from the affected tooth which was then transferred to Tris-ethylenediaminetetraacetic acid (EDTA) buffer for DNA extraction and multiplex polymerase chain reaction (MPCR). DNA Extraction was performed as per the procedure described earlier.[7] MPCR was also done as discussed by Shin et al.[7] in their study. The primers (Bioserve India Pvt. Ltd. India) used in the study were as follows:[7] HSV-1 (Forward: 5’-CGTACCTGCGGCTCGTGAAGT-3’ and Reverse: 5’-AGCAGGGTGCTCGTGTATGGGC-3’), HSV-2: Forward: 5’-TGGTATCGCATGGGAGACAAT-3’ and Reverse: 5’CTCCGTCCAGTCGTTTATCTTG-3’), CMV: Forward: 5’-ACGTGTTACTGGCGGAGTCG-3’ and Reverse: 5’-TTGAGTGTGGCCAGACTGAG-3’), EBV: Forward: 5’-AGCACTGGCCAGCTCATATC-3’ and Reverse: 5’-TTGACGTCATGCCAAGGCAA-3’). MPCR cyclic conditions were as follows: Initial denaturation at 95°C for 5 min, 45 cycles of denaturation at 95°C for 30 s, Annealing at 54°C for 30 s and extension at 72°C for 30 s, Final extension was given at 72°C for 5 min. PCR product was detected by gel electrophoresis. Detection of amplified products was done by electrophoresis on 2% agarose gel (HiMedia) containing 1× Tris-acetate-EDTA. A 100 bp DNA ladder was loaded with the sample DNA. The amplicon size of 271, 231, 368, and 326 bp for HSV-1, HSV-2, CMV, and EBV were compared with 100 bp ladder [Figures 1–4]. Excel sheet was prepared, and demographic data of the patient with results were entered. The analysis of data was done using SSPS software version. 21.0 (IBM). Chi-square test was applied. P < 0.001 was taken as statistically significant.
Figure 1.
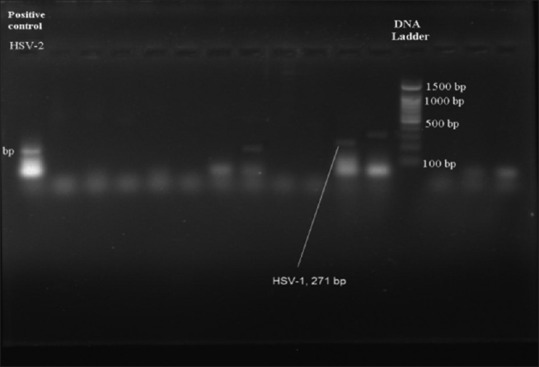
Multiplex PCR showing positive band for Herpes simplex virus - 1
Figure 4.
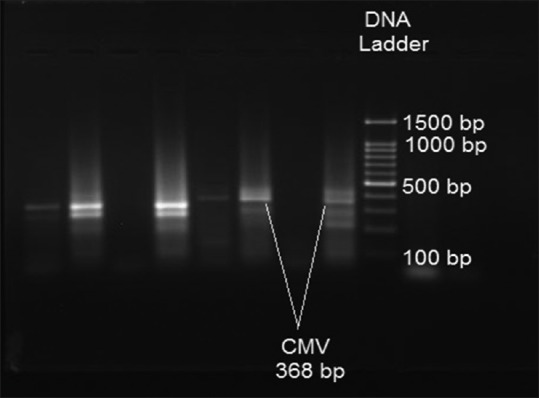
Multiplex PCR showing positive band for cytomegalovirus
Figure 2.
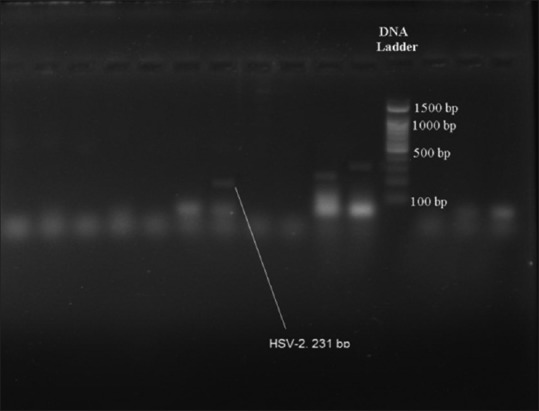
Multiplex PCR showing positive band for Herpes simplex virus - 2
Figure 3.
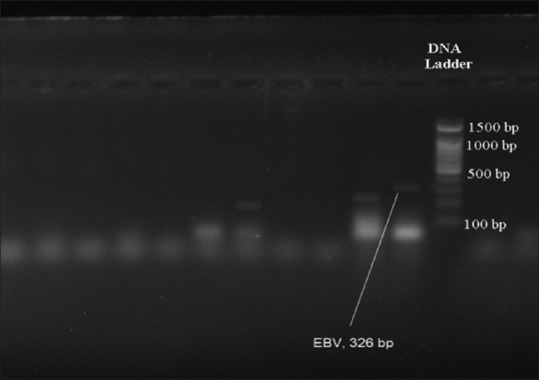
Multiplex PCR showing positive band for Epstein–Barr viruses
RESULTS
The most predominant age group affected was 41–50 followed by 31–40 years (43.49 + 8.48) and male patients were outnumbered the female patients in ratio of 1:1.2, but the difference was not statistically significant (P > 0.05). Herpesviruses were detected in 73.3% of patients with chronic periodontitis vis-a-vis 8.0% from the controls. The difference was statistically significant indicating that herpesviruses could be one of the important etiological agents in chronic periodontitis. All the four herpesviruses were significantly associated with chronic periodontitis (P < 0.001). HSV-1 (46.6%) virus was the virus most commonly detected followed by HSV-2 (34.6%), EBV (30.6%), and CMV (19.3%) from patients with chronic periodontitis and 7.0%, 0.6%, 0.0%, and 0.3% from healthy controls, respectively [Table 1]. All the four herpesviruses were significantly associated with severity of the disease so they could be playing a crucial role in increasing severity of the chronic periodontitis [Table 2]. Individual herpesviruses have shown differences in their association with different clinical parameters evaluated in the present study [Table 3]. Multiple herpesvirus infection was more commonly seen in patients with severe chronic periodontitis, which was statistically significant as compared to mild and moderate chronic periodontitis [Table 4]. The most common combination was HSV-1 + HSV-2 followed by HSV-1 + HSV-2 + EBV [Table 4].
Table 1.
Prevalence of individual Herpes viruses in patients with chronic periodontitis and controls
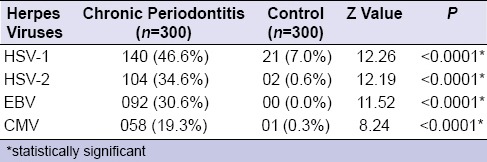
Table 2.
Correlation of Herpes viruses with severity of chronic periodontitis
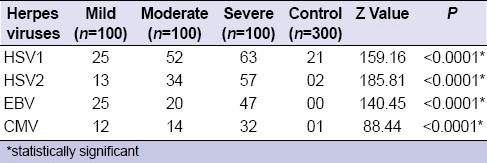
Table 3.
Association between Herpesviruses and clinical parameters in patients with chronic periodontitis
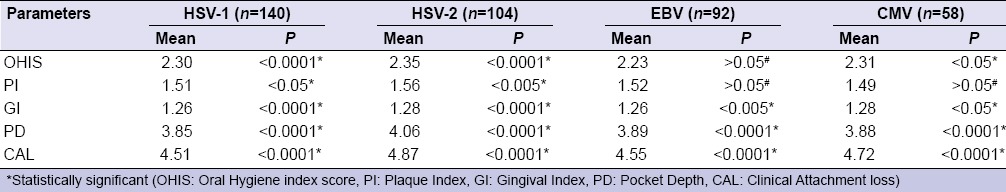
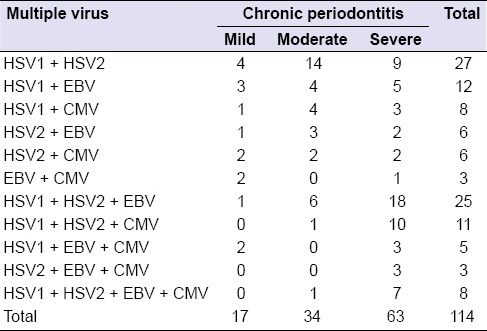
Table 4.
Combination of Herpes virus as per the severity of chronic periodontitis
DISCUSSION
Chronic periodontitis is a complex oro-dental disease induced by periodontopathic microbiota and aggravated by the predominant appearance of some of them. The present study was a prospective case–control study to find out the role of herpesviruses in etiopathogenesis of chronic periodontitis. Patients with systemic diseases, HIV infection, and smoking were not included as they could have acted as confounding factors in the disease process. The significant detection of herpesviruses from cases of chronic periodontitis as compared to healthy controls indicates that herpesviruses does play an important role in the etiology of the disease and are not a mere bystanders.
The different mechanism of herpesviruses in the pathogenesis was proposed in the literature. These incudes direct cytopathic effects on fibroblasts, keratinocytes, endothelial cells, inflammatory cells and possibly bone cells, viral proteins expressed on eukaryotic cell membranes can act as bacterial receptors and generate new bacterial binding sites, alter functions of monocytes, macrophages, and lymphocytes in periodontitis lesions, induce a proinflammatory response including expression of cytokines and chemokines and possibly through producing tissue injury as a result of immunopathologic responses.[8,9,10,11]
The different herpesviruses vary in their association with chronic periodontitis [Table 1]. In the present study, HSV-1 was detected in 46.7% of patients with chronic periodontitis and 7% from healthy controls suggesting as a principal etiological agent. Various authors have reported HSV-1 as principal etiological agent in their respective studies (100% HSV-1 by Bilichodmath et al.,[5] 81.2% by Kolliyavar et al.,[6] 40.0% by Imbronito et al.[12]). However, few studies did not report HSV-1 from patients with chronic periodontitis.[13,14]
HSV-2 was detected in 34.6% of patients with chronic periodontitis and 0.6% of healthy controls in the present study [Table 1]. In literature, its prevalence in chronic periodontitis has been reported to range from 0% to 20.0%. Various studies have reported various prevalence rates (20.0% HSV-2 by Singh et al.,[15] 12.0% by Das et al.[16]) from the cases of chronic periodontitis. While no HSV-2 was reported by other studies.[13,14]
EBV was detected in 30.6% from patients with chronic periodontitis and none from healthy controls in the present study [Table 2]. Various studies have reported various prevalence rates (78.9% EBV by Bilichodmath et al.,[5] 32.0% by Das et al.,[16] 79.0% by Contreras and Slots[17] 32.0% by Mauricio et al.[18]) from patients with chronic periodontitis. The detection rates of the present study and Mauricio et al.[18] are in accordance.
CMV was detected in 19.33% from patients with chronic periodontitis in the present study [Table 1]. Various studies have shown varying rates of detection of CMV in their respective studies (Bilichodmath et al.[5] in 26.3%, Das et al.[16] in 12.0%, Chalabi et al.[13] in 59.0%) from the cases of chronic periodontitis.
There is difference found in the prevalence of individual herpesviruses in the present study and various other studies published so far in the literature. There are various reasons for these differences in the prevalence of herpesviruses. One of the important reasons could be the different prevalence in general population which varies in different geographical areas. Furthermore, the sample size, nature of specimen collected is another possible reason for different detection rates. Many studies did not look for HSV-2 as an additional etiological agent because of its chief involvement in causing sexually transmitted diseases. A herpesvirus differs in reactivation rate in different individuals, which might have affected the prevalence rates also. It is concluded that the herpesviruses differs in their prevalence rates in the present study as well as other published studies. As per the results obtained from patients with chronic periodontitis, HSV-1 seems to play a major role in current population followed by HSV-2, EBV, and CMV, respectively.
Herpesviruses are involved in increasing the severity of the disease. They were predominantly detected from severe chronic periodontitis as compared to mild and moderate chronic periodontitis [Table 2]. Contreras et al.[19] have shown high detection rates of herpes viruses from severe chronic periodontitis than moderate and slight (Mild) periodontitis in their study. Parra and Slots[4] have also reported a positive association between subgingival herpesvirus infections and severity of the periodontal disease. However, Mauricio et al.[18] have reported dubious role of herpesviruses in the severity of the chronic periodontitis as they have reported a very less prevalence rates in their study population.
Knowledge of the association of herpesviruses with chronic periodontitis may not only be significant for understanding the pathogenesis of the disease but will also help in diagnosis, monitoring and treatment of the disease. So to conclude, a significant association was seen in detection rates of herpesviruses and increasing severity of the disease in the present study.
A very strong statistical significance (<0.0001) was found between overall detection of herpesviruses and clinical parameters such as oral hygiene, plaque index, gingival inflammation, pocket depth and attachment loss and bleeding on probing in the present study.
However, when compared these clinical parameters with individual herpesvirus detection from patients with chronic periodontitis, it shows varying results. HSV-1 and HSV-2 were found to be significantly associated with poor oral hygiene, increased plaque index and gingival index, attachment loss and pocket depth in the present study [Table 3]. However, EBV and CMV have shown significant association with increased pocket depth and clinical attachment loss, but differ with poor oral hygiene index, gingival index, plaque index in the present study [Table 3].
Various studies have reported various observations in terms of herpesviruses and clinical parameters.[3,20,21] The observations from the present study revealed the significant association with loss of clinical attachment and increased pocket depth suggesting the role of herpesviruses in increasing the severity of the disease.
Multiple herpesviruses together contribute in increasing severity of the disease by synergistic mechanism. The periodontal sites with a particular herpesvirus coinfection may experience increased risk of infection which might lead to rapid destruction of tissue. Coinfection of herpesviruses was evaluated in the present study to know their association in increasing the severity in patients with chronic periodontitis [Table 4]. More than one herpesvirus was detected from patients with a severe type of chronic periodontitis than the mild and moderate type of chronic periodontitis.
Various studies have shown such coinfection does occur in the increasing severity of chronic periodontitis. Many studies have reported multiple herpesviruses in their respective studies.[3,5,17,22] These findings suggest that there is a strong association between multiple herpesviruses in increasing the severity of the disease. The possible mechanism might be one herpesvirus infection may activate other latent herpesvirus infection. Herpesvirus coinfection seen in the present study is suggesting a synergetic pathogenic interaction in severity of chronic periodontitis.
Various combinations of herpesviruses were seen in the present study [Table 4]. The most common combination of herpesviruses was HSV-1 + HSV-2 from patients with moderate and severe type of chronic periodontitis. The other most lethal combinations were HSV-1 + HSV-2 + EBV followed by HSV1 + HSV2 + CMV seen in patients with severe chronic periodontitis. Furthermore, all four herpesviruses were detected from severe chronic periodontitis in the present study. Various other studies also showed the different combinations of herpesviruses in cases of chronic periodontitis.[3,5,17]
Overall detection of multiple herpesviruses was more in severe chronic periodontitis as compared to mild and moderate chronic periodontitis cases. This suggests combined effect of the combination of herpesviruses in the pathogenesis of severe chronic periodontitis. This led to a conclusion that cohabitation of multiple herpesviruses plays an important role in the increasing severity of chronic periodontitis. All these observations led to an important conclusion that the multiple herpesviruses play an important role in increasing severity of chronic periodontitis.
CONCLUSION
The present study detected a very high prevalence rate of herpesviruses from chronic periodontitis cases than the healthy controls suggesting their strong association with the disease. HSV-1 was the most common herpesviruses implicated in the etiology of the chronic periodontitis followed by HSV-2, EBV, and CMV. HSV-2 was detected significantly in the present study as compared to other published studies which is one of the important findings. Herpesviruses differ in association with various clinical parameters. The combination of herpesviruses plays an important role in increasing severity of the disease.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We would like to thank Dr. Daisy Happy (MDS, periodontics) and Dr. Kishore Bhat MD Microbiology, Mr. Manoher, for their support during project.
REFERENCES
- 1.Kumar TS, Dagli RJ, Mathur A, Jain M, Balasubramanyam G, Prabu D, et al. Oral health status and practices of dentate Bhil adult tribes of southern Rajasthan, India. Int Dent J. 2009;59:133–40. [PubMed] [Google Scholar]
- 2.Newman MG, Socransky SS, Savitt ED, Propas DA, Crawford A. Studies of the microbiology of periodontosis. J Periodontol. 1976;47:373–9. doi: 10.1902/jop.1976.47.7.373. [DOI] [PubMed] [Google Scholar]
- 3.Ling LJ, Ho CC, Wu CY, Chen YT, Hung SL. Association between human herpesviruses and the severity of periodontitis. J Periodontol. 2004;75:1479–85. doi: 10.1902/jop.2004.75.11.1479. [DOI] [PubMed] [Google Scholar]
- 4.Parra B, Slots J. Detection of human viruses in periodontal pockets using polymerase chain reaction. Oral Microbiol Immunol. 1996;11:289–93. doi: 10.1111/j.1399-302x.1996.tb00183.x. [DOI] [PubMed] [Google Scholar]
- 5.Bilichodmath S, Mangalekar SB, Sharma DC, Prabhakar AK, Reddy SB, Kalburgi NB, et al. Herpesviruses in chronic and aggressive periodontitis patients in an Indian population. J Oral Sci. 2009;51:79–86. doi: 10.2334/josnusd.51.79. [DOI] [PubMed] [Google Scholar]
- 6.Kolliyavar B, Setty S, Patil A, Thakur SL. Association of viruses in chronic periodontitis – Fact or hype. Int J Oral Hyg Dent Res. 2013;1:1–5. [Google Scholar]
- 7.Shin CH, Park GS, Hong KM, Paik MK. Detection and typing of HSV-1, HSV-2, CMV and EBV by quadruplex PCR. Yonsei Med J. 2003;44:1001–7. doi: 10.3349/ymj.2003.44.6.1001. [DOI] [PubMed] [Google Scholar]
- 8.Contreras A, Slots J. Herpesviruses in human periodontal disease. J Periodontal Res. 2000;35:3–16. doi: 10.1034/j.1600-0765.2000.035001003.x. [DOI] [PubMed] [Google Scholar]
- 9.Contreras A, Zadeh HH, Nowzari H, Slots J. Herpesvirus infection of inflammatory cells in human periodontitis. Oral Microbiol Immunol. 1999;14:206–12. doi: 10.1034/j.1399-302x.1999.140402.x. [DOI] [PubMed] [Google Scholar]
- 10.Michelson S. Human cytomegalovirus escape from immune detection. Intervirology. 1999;42:301–7. doi: 10.1159/000053964. [DOI] [PubMed] [Google Scholar]
- 11.Mogensen TH, Paludan SR. Molecular pathways in virus-induced cytokine production. Microbiol Mol Biol Rev. 2001;65:131–50. doi: 10.1128/MMBR.65.1.131-150.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Imbronito AV, Okuda OS, Maria de Freitas N, Moreira Lotufo RF, Nunes FD. Detection of herpesviruses and periodontal pathogens in subgingival plaque of patients with chronic periodontitis, generalized aggressive periodontitis, or gingivitis. J Periodontol. 2008;79:2313–21. doi: 10.1902/jop.2008.070388. [DOI] [PubMed] [Google Scholar]
- 13.Chalabi M, Moghim S, Mogharehabed A, Najafi F, Rezaie F. EBV and CMV in chronic periodontitis: A prevalence study. Arch Virol. 2008;153:1917–9. doi: 10.1007/s00705-008-0186-7. [DOI] [PubMed] [Google Scholar]
- 14.Nibali L, Atkinson C, Griffiths P, Darbar U, Rakmanee T, Suvan J, et al. Low prevalence of subgingival viruses in periodontitis patients. J Clin Periodontol. 2009;36:928–32. doi: 10.1111/j.1600-051X.2009.01476.x. [DOI] [PubMed] [Google Scholar]
- 15.Singh A, Khuller N, Singh P, Rathore S, Bhatia J. Detection of herpes simplex virus (Hsv-1 & 2) in gingival tissue of chronic periodontitis patients using Polymerase Chain Reaction (PCR) technique. J Periodontal Med Clin Pract. 2014;1:13–8. [Google Scholar]
- 16.Das S, Krithiga GS, Gopalakrishnan S. Detection of human herpes viruses in patients with chronic and aggressive periodontitis and relationship between viruses and clinical parameters. J Oral Maxillofac Pathol. 2012;16:203–9. doi: 10.4103/0973-029X.98502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Contreras A, Slots J. Mammalian viruses in human periodontitis. Oral Microbiol Immunol. 1996;11:381–6. doi: 10.1111/j.1399-302x.1996.tb00199.x. [DOI] [PubMed] [Google Scholar]
- 18.Mauricio GR, Marianela GE, Ernesto TL, Rosa Velia RR, Claudio CR, Myriam GR. Identification of herpes virus in patients with chronic periodontitis from Northeastern Mexico. Afr J Microbiol Res. 2013;7:5582–6. [Google Scholar]
- 19.Contreras A, Nowzari H, Slots J. Herpesviruses in periodontal pocket and gingival tissue specimens. Oral Microbiol Immunol. 2000;15:15–8. doi: 10.1034/j.1399-302x.2000.150103.x. [DOI] [PubMed] [Google Scholar]
- 20.Joshi VM, Bhat KG, Katti SS, Kugaji MS, Ingalgi PS. Prevalence of herpesvirus and correlation with clinical parameters in Indian subjects with chronic periodontitis. J Contemp Dent Pract. 2015;16:915–20. doi: 10.5005/jp-journals-10024-1781. [DOI] [PubMed] [Google Scholar]
- 21.Saygun I, Sahin S, Ozdemir A, Kurtis B, Yapar M, Kubar A, et al. Detection of human viruses in patients with chronic periodontitis and the relationship between viruses and clinical parameters. J Periodontol. 2002;73:1437–43. doi: 10.1902/jop.2002.73.12.1437. [DOI] [PubMed] [Google Scholar]
- 22.Kamma JJ, Contreras A, Slots J. Herpes viruses and periodontopathic bacteria in early-onset periodontitis. J Clin Periodontol. 2001;28:879–85. doi: 10.1034/j.1600-051x.2001.028009879.x. [DOI] [PubMed] [Google Scholar]


