Abstract
Objectives:
The aim of this study was to identify the type and frequency of incidental findings (IFs) in the maxillofacial region of CBCT scans with different sizes of field of view (FOV), and the clinical relevance of the findings was classified as requirement or not of monitoring, treatment or referral to a specialist.
Methods:
We analyzed 150 CBCT examinations, divided according to the size of the FOV into 3 groups: 6-cm maxilla, 6-cm mandible and 13-cm maxilla/mandible. The IFs were categorized into six areas: airway, temporomandibular joint (TMJ), bone, lesions of the jaws, teeth and soft-tissue calcifications.
Results:
The results showed 560 IFs that were found in 92% of the samples studied. A total of 225 IFs were found in examinations of the maxilla group, 99 findings in the mandible group and 236 findings in the maxilla/mandible group. The IFs were most frequent in the tooth zone (27.32%), followed by airways, soft-tissue calcifications, TMJ, bone, lesions of the jaw and other findings. We also found that 43.46% of the IFs did not need treatment or referral to another professional, 28.97% findings required the acquisition of new images for monitoring and 27.55% findings needed treatment or referral.
Conclusions:
The present study confirmed the high frequency of IFs in CBCT scans. It was concluded that it is necessary to interpret and report the total volume obtained in CBCT examinations and not only the purpose of the examination region.
Keywords: incidental finding, CBCT, diagnostic imaging
Introduction
CBCT, used to capture images in the maxillofacial region, was developed in the 1990s and since then, it has evolved. This scan imaging is used in dentistry because it can provide excellent images with high contrast of the bone and tooth structures with lower radiation dose and low cost for the patient compared with examinations obtained by helical CT. Obtaining the image for CBCT still has advantages when compared with conventional X-rays, because it eliminates most of the problems related to image distortion and superimposition of structures.1
During the acquisition of a CBCT image, the field of view (FOV) can be modified and determined as the region of interest. The images obtained on a CBCT scanner with a small FOV are used for interpreting limited areas of the maxillofacial region, while the images obtained with a large FOV include the paranasal sinuses, airways and intracranial and cranial base structures.2
With the growing indication of CBCT in various dental specialities, much has been asked about the role of the dentist in evaluating the image obtained in the examination. Although often overlooked, the evaluation of all structures included in the examination is required according to the guidelines of the American and European Academies of Dentomaxillofacial Radiology. Therefore, knowledge is needed of not only the dentomaxillary complex, but also the adjacent structures.3,4
As imaging techniques evolve, the ability to identify incidental findings (IFs) increases. An IF can be defined as a radiographic or tomographic image with any discovery that is unrelated to the original purpose of the examination, which can range from anatomical variations to benign and malignant lesions.2
The inability to identify, inform or provide follow-up and care related to the IFs may have negative consequences for the patient and result in dentists neglecting their legal responsibility.2 The recognition of IFs in CBCT images allows the identification of occult lesions, thereby improving the accuracy of the diagnosis and enabling the most appropriate therapeutic approach.
Research shows that when two-dimensional images are interpreted, IFs are identified in 6–43% of patients.5–7 CBCT examinations contain more information than images in two dimensions, so it is to be expected that in these examinations, the radiologist will find higher occurrence of IFs.
Although there are some studies that have already found many IFs in the maxillofacial region,1,8–13 there are no studies with Brazilian samples yet. In addition, these studies did not use examinations showing different sizes of FOV in their samples. Therefore, it would be a great contribution to carry out more studies aimed at recognizing the types and frequency of IFs in each type of FOV in order to avoid underestimation or overestimation of substantial abnormalities.
The objectives of our study were to identify the type, frequency and location of IFs in the maxillofacial region of CBCT scans with different sizes of FOV and classify the findings into the requirement or not of monitoring, treatment or referral to another professional.
Methods and materials
This study was approved by the Ethics Committee of the Bauru School of Dentistry, University of São Paulo. A total of 150 CBCT examinations were selected from the image files of the Department of Stomatology of this institution.
The inclusion criteria for sample selection were: (1) images with an FOV 6-cm high involving only the maxilla; (2) images with an FOV 6-cm high involving only the mandible; and (3) images with an FOV 13-cm high involving both the maxilla and mandible. The exclusion criteria were: examinations without reasons for their requests and examinations with bad picture quality.
The sample was divided into 3 groups: (1) 50 examinations covering the maxilla; (2) 50 examinations covering the mandible; and (3) 50 examinations covering the maxilla and mandible. The examinations showed varying voxels (0.2, 0.25, 0.3 and 0.4) and the diameter of the FOV was 16 cm.
The equipment used in this research was an i-CAT Classic® (Imaging Science International, Hatfield, PA) and for the interpretation of the examinations, i-Cat Vision® software (Imaging Sciences International, Hatfield, PA) was used on a multiplanar reformatting screen.
2 researcher radiologists performed the analysis of the examinations in 2 stages: 21 examinations (15% of the sample) were observed first and after 15 days, a new assessment was performed. Thus, an intracalibration and an intercalibration were performed through the kappa test. Thereafter, a single dentist radiologist examiner, followed the study and evaluated all the CBCT examinations and reported the possible IFs, which were not associated with the reason. Findings directly related to the preliminary indications of the CBCT were excluded. A list containing the most common IFs in CBCT examinations based on the literature1,8–13 was developed for a better classification of images. In the few cases of doubt about the image, other experienced radiologists were consulted.
Data about the patients (gender and age) and the indication of each CBCT examination were also collected. All diagnoses were based on CBCT findings. Comparisons and associations with conventional radiography and histopathological examinations were not performed.
The IFs were divided into six zones: (1) airway, (2) temporomandibular joint (TMJ), (3) bone, (4) lesions of the jaw, (5) teeth and (6) soft-tissue calcifications.
The TMJ and the airways were not analyzed in Group 2 (mandible) because they were not visible in this FOV. When the IF did not fit in any of the six zones shown, it was included in the “Other” group. Findings such as missing teeth, dental caries and bone loss were excluded. An IF that was observed more than once in the examination was recorded to be observed.
After analyzing the CBCT examinations, the IFs were classified in relation to their clinical management into three groups: (1) does not need treatment/referral to another professional; (2) monitoring is suggested; and (3) needs treatment/referral to another professional.
The descriptive and inferential analyses of the data were performed using the Statistica v. 5.1 program (Stat Soft Inc, Tulsa, OK) and by adopting a significance level of 5%.
Results
Intraexaminer and interexaminer calibration
Kappa test was performed and the agreement was almost perfect, with a 0.87 intraexaminer calibration and 0.81 interexaminer calibration.
Sample profile
Patients in the sample were aged between 8 and 91 years (mean 37 ± 18.3 years). The females were predominant in the sample (n = 82) with 54.7% while 45.3% were males.
Reason for requesting CBCT examination
The prevailing indication of CBCT examinations was planning implants (n = 61) with a frequency of 40.67% of the sample (Table 1).
Table 1.
Indications of CBCT examinations in the sample
| Indications of CBCT examination | Amount |
|
|---|---|---|
| n | % | |
| Planning for implant | 61 | 40.67 |
| Evaluation/control of cysts/tumours | 21 | 14.00 |
| Pre-operative assessment of third molar | 12 | 8.00 |
| Unerupted tooth assessment | 14 | 9.33 |
| Supernumerary tooth location | 6 | 4.00 |
| Others | 36 | 24.00 |
| Total | 150 | 100.00 |
Incidental findings
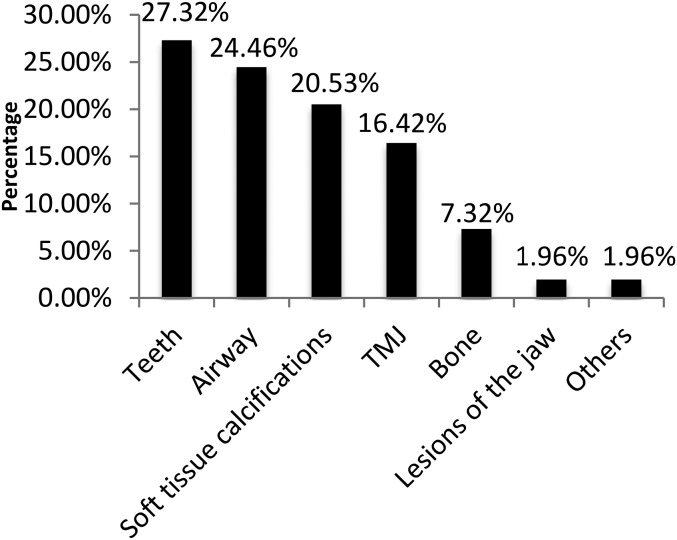
A total of 560 IFs were obtained; the maxilla/mandible group had the largest number of IFs, followed by the maxilla group and the mandible group. The distribution of the number of IFs between sample groups is shown in Table 2. The zone with the highest number of IFs was the teeth, with 27.32%, and the most common IF in the sample was thickening of the maxillary sinus mucosa (n = 70), with 12.5%. The frequency of IFs among the six zones evaluated in the sample is illustrated in Figure 2. The IFs of each group evaluated can be seen in Tables 3–5.
Table 2.
Distribution of the number of incidental findings (IFs) in accordance with the field of view (FOV) used
| FOV | Total number of IFs | Average of findings per examination | Number of examinations with findings |
|---|---|---|---|
| Maxilla | 225 | 4.50 | 49 |
| Mandible | 99 | 1.98 | 42 |
| Maxilla/mandible | 236 | 4.72 | 47 |
| Total | 560 | 3.73 | 138 |
Figure 2.
Frequency of distribution of incidental findings by zone evaluated in the total sample.
Table 3.
Descriptive analysis and frequency of incidental findings (IFs) of CBCT examinations with the field of view encompassing the maxilla
| Zone | IFs | Number (%) of IF | Number of patients with IF | Clinical managementa |
|---|---|---|---|---|
| Airway | Thickening maxillary sinus mucosa | 41 (18.22) | 30 | >2 mm: Y |
| Alveolar extension of the maxillary sinus | 17 (7.55%) | 17 | N | |
| Deviated septum | 8 (3.55%) | 8 | Y | |
| Cyst retention/pseudocyst/polyp | 6 (2.66%) | 6 | N | |
| Turbinate hypertrophy | 4 (1.77%) | 4 | Y | |
| Antrolith | 3 (1.33%) | 3 | N | |
| Thickening sphenoid sinus mucosa | 3 (1.33%) | 3 | Y | |
| Tuber extension of the maxillary sinus | 3 (1.33%) | 3 | N | |
| Bucosinusal communication | 2 (0.89%) | 2 | Y | |
| Total opacification of the maxillary sinus | 1 (0.44%) | 1 | Y | |
| Total opacification of the sphenoid sinus | 1 (0.44%) | 1 | Y | |
| Concha bullosa | 1 (0.44%) | 1 | Y | |
| Nasal polyposis | 1 (0.44%) | 1 | N | |
| Total | 91 (40.44%) | 80 | ||
| TMJ | Osteophytes | 25 (11.11%) | 17 | F |
| Flattening condyle | 24 (10.67%) | 17 | F | |
| Away zoneb | 12 | |||
| Total | 49 (21.78%) | 34 | ||
| Bone | Palatal torus | 9 (4.00%) | 9 | N |
| Bone sclerosis | 2 (0.89%) | 2 | N | |
| Total | 11 (4.89%) | 11 | ||
| Lesions of the jaw | Periapical cyst | 4 (1.78%) | 4 | Y |
| Odontoma | 1 (0.44%) | 1 | Y | |
| Total | 5 (2.22%) | 5 | ||
| Teeth | Root dilaceration | 16 (7.11%) | 10 | N |
| Apical lesion | 9 (4.00%) | 9 | Y | |
| Impacted tooth | 3 (1.33%) | 2 | F | |
| Pulp calcification | 1 (0.44%) | 1 | N | |
| Endoperio lesion | 1 (0.44%) | 1 | Y | |
| Condensing osteitis | 1 (0.44%) | 1 | Y | |
| External resorption | 1 (0.44%) | 1 | Y | |
| Total | 32 (14.22%) | 25 | ||
| Soft-tissue calcifications | Calcification of the style–hyoid complex | 33 (14.67%) | 18 | N |
| Tonsillolith | 1 (0.43%) | 1 | N | |
| Total | 34 (15.11%) | 19 | ||
| Others | Residual root | 2 (0.89%) | 2 | Y |
| Amalgam fragment | 1 (0.44%) | 1 | N | |
| Total | 3 (1.33%) | 3 |
F, need follow-up; N, do not require treatment/referral; TMJ, temporomandibular joint; Y, need treatment/referral to another professional.
Many findings were classified as being asymptomatic. Treatment may be changed according to the symptoms and complaints of patients.
It was not possible to analyze the zone because the region was not visible in the examination.
Table 5.
Descriptive analysis and frequency of incidental findings (IFs) of CBCT examinations with the field of view encompassing the maxilla/mandible
| Zone | IFs | Number (%) of IF | Number of patients with IF | Clinical managementa |
|---|---|---|---|---|
| Airway | Thickening maxillary sinus mucosa | 29 (12.28%) | 20 | >2 mm: Y |
| Alveolar extension of the maxillary sinus | 5 (2.11%) | 5 | N | |
| Cyst retention/pseudocyst/polyp | 4 (1.69%) | 4 | N | |
| Turbinate hypertrophy | 3 (1.27%) | 3 | Y | |
| Deviated septum | 2 (0.84%) | 2 | Y | |
| Antrolith | 1 (0.42%) | 1 | N | |
| Total opacification of the maxillary sinus | 1 (0.42%) | 1 | Y | |
| Concha bullosa | 1 (0.42%) | 1 | N | |
| Total | 46 (19.49%) | 37 | ||
| TMJ | Flattening condyle | 22 (9.32%) | 15 | F |
| Osteophytes | 20 (8.47%) | 16 | F | |
| Bifid condyle | 1 (0.43%) | 1 | N | |
| Total | 43 (18.22%) | 32 | ||
| Bone | Bone sclerosis | 10 (4.23%) | 10 | N |
| Palatal torus | 5 (2.11%) | 5 | N | |
| Mandibular torus | 1 (0.43%) | 1 | N | |
| Exostosis | 1 (0.43%) | 1 | N | |
| Total | 17 (7.20%) | 17 | ||
| Lesions of the jaw | Periapical cyst | 2 (0.84%) | 2 | Y |
| Bone dysplasia | 1 (0.43%) | 1 | F | |
| Total | 3 (1.27%) | 3 | ||
| Teeth | Impacted tooth | 40 (16.94%) | 16 | F |
| Root dilaceration | 13 (5.50%) | 9 | N | |
| Giroversion | 11 (4.66%) | 6 | N | |
| Apical lesion | 8 (3.38%) | 6 | Y | |
| Supernumerary tooth | 4 (1.69%) | 2 | F | |
| Endoperio lesion | 3 (1.27%) | 3 | Y | |
| Agenesis | 2 (0.89%) | 1 | N | |
| Dens in dente | 1 (0.42%) | 1 | Y | |
| Enamel pearl | 1 (0.42%) | 1 | N | |
| External resorption | 1 (0.42%) | 1 | Y | |
| Total | 84 (35.59%) | 46 | ||
| Soft-tissue calcifications | Calcification of the style–hyoid complex | 31 (13.13%) | 17 | N |
| Calcification of triticeous cartilage | 5 (2.11%) | 5 | N | |
| Tonsillolith | 2 (0.89%) | 2 | N | |
| Atheroma | 2 (0.89%) | 2 | Y | |
| Total | 40 (35.59%) | 26 | ||
| Others | Residual root | 2 (0.89%) | 2 | Y |
| Increased pericoronal space | 1 (0.42%) | 1 | F | |
| Total | 3 (1.27%) | 3 |
F, need follow-up; N, do not require treatment/referral; TMJ, temporomandibular joint; Y, need treatment/referral to another professional.
Many findings were classified as being asymptomatic. Treatment may be changed according to the symptoms and complaints of patients.
Table 4.
Descriptive analysis and frequency of incidental findings (IFs) of CBCT examinations with the field of view encompassing the mandible
| Zone | IFs | Number (%) of IF | Number of patients with IF | Clinical managementa |
|---|---|---|---|---|
| Bone | Bone sclerosis | 12 (12.12%) | 9 | N |
| Mandibular torus | 1 (1.01%) | 1 | N | |
| Total | 13 (13.13%) | 10 | ||
| Lesions of the jaw | Osteoma | 1 (1.01%) | 1 | F |
| Dentigerous cyst | 1 (1.01%) | 1 | Y | |
| Odontoma | 1 (1.01%) | 1 | Y | |
| Total | 3 (3.03%) | 3 | ||
| Teeth | Apical lesion | 10 (10.10%) | 8 | Y |
| Endoperio lesion | 5 (5.05%) | 3 | Y | |
| Impacted tooth | 5 (5.05%) | 5 | F | |
| Giroversion | 4 (4.04%) | 4 | N | |
| Root dilaceration | 3 (3.03%) | 3 | N | |
| Furcation lesion | 3 (3.03%) | 3 | Y | |
| Pulp calcification | 2 (2.02%) | 2 | N | |
| Condensing osteitis | 2 (2.02%) | 2 | Y | |
| External resorption | 1 (1.01%) | 1 | Y | |
| Taurodontism | 1 (1.01%) | 1 | N | |
| Supernumerary tooth | 1 (1.01%) | 1 | N | |
| Total | 37 (37.37%) | 33 | ||
| Soft-tissue calcifications | Calcification of the style–hyoid complex | 18 (18.18%) | 16 | N |
| Tonsillolith | 14 (14.14%) | 14 | N | |
| Calcification of triticeous cartilage | 7 (7.07%) | 7 | N | |
| Greater horn thyroid calcification | 2 (2.02%) | 2 | N | |
| Total | 41 (41.41%) | 39 | ||
| Others | Residual root | 4 (4.04%) | 3 | Y |
| Increased pericoronal space | 1 (1.01%) | 1 | F | |
| Total | 5 (5.05%) | 4 |
F, need follow-up; N, do not require treatment/referral; Y, need treatment/referral to another professional.
Many findings were classified as being asymptomatic. Treatment may be changed according to the symptoms and complaints of patients.
Number of incidental findings and gender of patients
There was no statistically significant result for any zone and gender using the Mann–Whitney U-test to correlate the number of IFs with male and female gender.
Number of incidental findings and age of patients
Using Spearman correlation to correlate the age of patients with the number of findings by zone, it was found to be a statistically significant result that older patients had a larger number of IFs in the soft-tissue calcification zone (p = 0.001).
Clinical relevance of incidental findings
Most of the findings with a 43.46% frequency do not require treatment or referral to another professional. A total of 28.97% of the findings need monitoring by the dentist and 27.97% of them need treatment or referral to another professional. In Tables 3–5, the classification of each IF is established.
Discussion
In the present study, we evaluated 150 CBCT examinations performed as a complementary examination for diagnosis in dentistry. Planning for implant placement was the most frequent reason for the request for examinations, with 40.07% of the total sample (Table 1). This result was also reported by other authors with 52.7–73% of frequency.1,10,14 The current criteria for the prescription of images obtained by CBCT were established by SEDENTEXCT in 2011, an evidence-based guidelines on use of CBCT in Dentistry, including referral criteria, quality assurance guidelines and optimisation strategies.
The sample was divided into three groups according to the size of the FOV in this study. This division was aimed at differentiating the type and frequency of findings between the dental arches. Most of the studies of IFs in the literature are performed with a large FOV.10,15 Some authors do not describe the size of the FOV,11–13 as shown in Table 6.
Table 6.
Previous studies of prevalence of incidental findings (IFs) in CBCT examinations
| Study | CBCT scanner | Mean age (range) (years) | FOV | Number of examinations with IF (%) Number of IFa |
Zone with the highest number of findings |
|---|---|---|---|---|---|
| Price et al 20111 | NewTom 3G Sirona Galileos 3D Comfort |
49.3 (9–80) | 6 or 9 cm | 272 examinations (90.7%) 881 findings |
Airway |
| Pette et al 201215 | i-CAT | Males 64.7; females 62.4 (16–91) | 13 cm | 789 findings | Paranasal sinuses |
| Allareddy et al 201210 | i-CAT | 5–87 (not reported) | 13 cm | 943 examinations (94.3%) | Teeth |
| Çağlayan; Tozoğlu 201211 | NewTom 3G | 30.3 (9–74) | Not reported | 192 examinations (92.8%) | Airway |
| Drage et al 20139 | i-CAT Classic® (Imaging Science International, Hatfield, PA) | 14.5 (not reported) | 4 cm | 66% examinations 370 findings |
Teeth |
| Edwards et al 201412 | i-CAT Next Generation | 6.3 (5–46) | Large: size not reported | 356 examinations (83.4%) 842 findings |
Airway |
| Rheem et al 201313 | Hitachi CB MercuRay Care stream 9300 |
Mean age not reported (8–80) | Not reported | 59 examinations (40.1%) | Paranasal sinuses |
| Present study | i-CAT Classic | 37 (8–91) | 6-cm: maxilla 6-cm: mandible 13-cm: maxilla and mandible |
138 examinations (92%) 560 findings |
Teeth |
FOV, field of view.
Some authors describe their results only with the total number of examinations with IFs or with only the total number of IFs; NewTom 3G (Quantitative Radiology, Verona, Italy); Sirona Galileos 3D Comfort (Sirona Dental Systems, Charlotte, NC); i-CAT (Imaging Sciences, Hatfield, Pennsylvania, PA); i-CAT Classic® (Imaging Sciences, Hatfield, Pennsylvania, PA); i-CAT Next Generation (Imaging Sciences, Hatfield, Pennsylvania, PA); Hitachi CB MercuRay (Hitachi Medical Corporation, Tokyo, Japan); Care stream 9300 (Carestream Health Inc, Rochester, NY).
With regard to the profile of the sample of this research, the majority of patients were female, with 54.7%, which corroborates with findings in the literature.1,8–13
With regard to age, we had a very large age range in the sample (8–91 years). In the literature, there are similar results, since in these studies there were no criteria for inclusion or exclusion in relation to age (Table 6).1,10–13,15
The frequency of the IFs depends on the sample, age group, criteria and categories of IFs that are considered by each researcher. In this study, a high frequency of IFs was obtained, i.e. findings not related to the purpose of the examination, similar to results found in the literature (Table 6).1,10–12
A total of 560 IFs were found in 138 of the 150 examinations. Therefore, 92% of the examinations showed at least one IF and 8% examinations did not present any findings. The average number of IFs per examination was 3.73. We observed that the maxilla/mandible group (n = 236) had a higher number of IFs than the maxilla group (n = 225) and the mandible group (n = 99) (Table 2). This can be explained by the fact that the maxilla/mandible group has FOV of the largest size (13 cm), thereby providing more visible structures and a greater likelihood of IFs. The maxilla group showed the greatest number of findings in relation to the mandible, and this can be attributed to the absence of airway zone and TMJ in the mandible group.
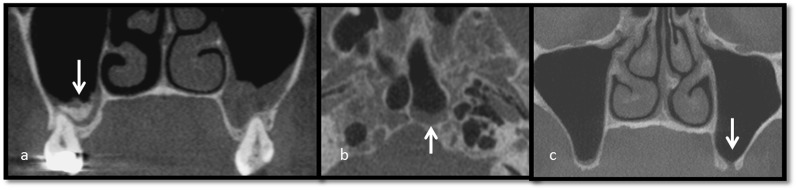
Airway findings
In this study, the airway was the zone with the second highest number of findings and represented 24.46% of the IFs (n = 137). In the literature, there is a high frequency of IFs in the airways, commonly the zone with the first or second highest incidence of findings in research (Table 6). In previous studies, frequencies of findings in the airways of 35, 51.8, 18.8 and 73.2, respectively, were reported.1,8,11,12
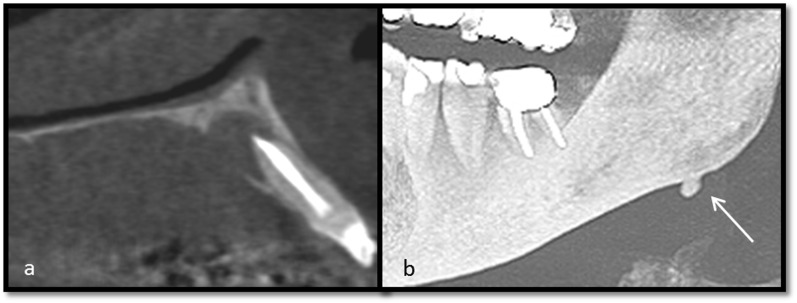
The most frequent finding in this area was the thickening of the maxillary sinus mucosa (n = 70) (Figure 1), similar to studies in the literature.1,11,15 In a previous study, the majority of cases of sinusitis presented thickenings of the sinus mucosa bigger than 2 mm, so this value can be considered an important indicator of maxillary sinusitis.16
Figure 1.
An antrolith (arrow) associated with mucosal thickening of the right maxillary sinus and mucosal thickening of the left maxillary sinus in coronal reformatting (a); the arrow is indicating mucosal thickening of the sphenoid sinus in the axial reformatting (b); nasal septum deviation, alveolar extension of the maxillary sinus bilateral and bucosinusal communication in the left maxillary sinus in coronal reformatting are indicated by the arrow (c).
The large number and variety of findings in the airways zone in this study shows how important it is for dentists (Figure 1), especially radiologists, to understand the nature of sinus changes. According to a systematic review of the use of CBCT in airways, there has been a significant increase in the number of publications on this subject in the past 5 years and the results indicate that CBCT can be used to accurately and reliably assess the airways.17
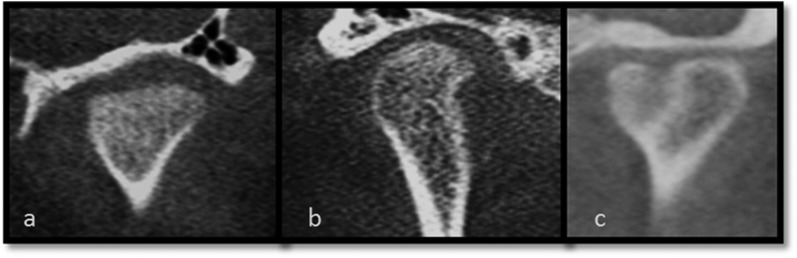
Temporomandibular joint findings
The TMJ was the fourth most frequent zone of IFs in this sample (n = 92) with a frequency of 16.42% (Figure 2), which is similar to previous studies with a frequency of 15.41 and 11.1%2 and less than that in another study, with a frequency 39.31%.15
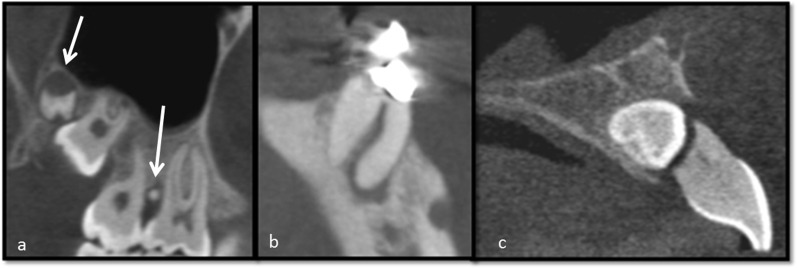
44 cases of flattening condyle and 47 cases of osteophytes were observed in this study (Figure 3). Flattening is represented by the loss of convexity of the condyle and is a signal of a remodelling bone or a physiological response to the increase of load in the region. An osteophyte is a marginal excrescence on the surface of the condyle that appears in the later stage of degenerative changes in the TMJ, when the body is adapting to repair the joint (Figure 3).18 Degenerative diseases of the TMJ detected on CBCT can be an IF, and patient history, clinical findings and symptoms are important in determining disease activity. Patients with symptoms such as pain and limited mouth opening need referral or intervention, while those without such symptoms do not need treatment, only monitoring.1
Figure 3.
Coronal reformatting: flattening condyle (a); osteophytes (b); and bifid condyle (c).
One case of unilateral bifid condyle (Figure 3), in a 23-year-old patient, was also found. A bifid condyle is a rare anomaly and may be unilateral or bilateral and anteroposterior or mediolateral. Although the aetiology is not fully understood, evidence suggests development change or traumatic aetiology. No treatment was indicated for that patient.1
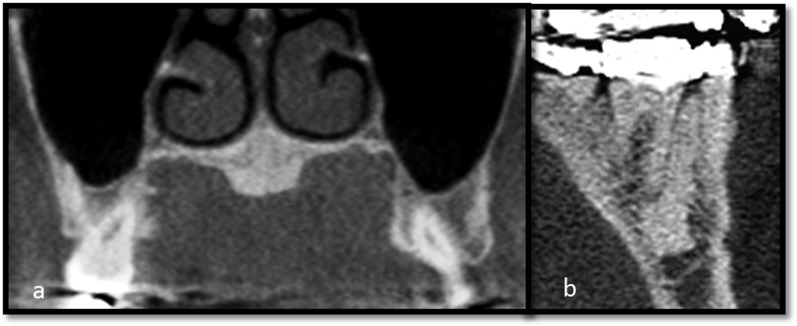
Bone findings
This zone corresponds to 7.32% (n = 42) of the IFs in this study and was the zone with the fifth highest incidence of findings (Figure 2). In the literature, we observed a greater number of findings in this zone with a frequency of 15–17%.1,13
24 cases of bone sclerosis were observed in this study (Figure 4). This condition is considered asymptomatic and does not cause expansion of the cortical bone. Bone sclerosis consists of hyperdense intraosseous lesions that do not result from infection or systemic disease and have an unknown aetiology. Ignorance of the frequency and location of these images can result in erroneous diagnosis suggestions. No treatment is required in cases of bone sclerosis.1
Figure 4.
Palatal torus in coronal reformatting (a) and bone sclerosis in sagittal reformatting (b).
14 cases of palatal torus (Figure 4), 1 case of mandibular torus and 1 exostosis were also found in this study. Torus and exostosis are anatomical variations characterized by hard bony prominences located on the hard palate (palatal torus), the lingual plate of the mandible (mandibular torus) or the buccal plate of the maxilla and mandible (exostosis).19 Because they are asymptomatic, they usually do not require treatment, but they may be removed for prosthetic reasons and for use as biomaterials in periodontics and implantology.1
Lesions of the jaw findings
We noted in this sample a low frequency of IFs in this zone (1.96%) (Figure 2), similar to the results found in the literature, with frequency ranging from 0.1 to 3.5%.1,20 It is important to emphasize that the findings were described only with tomographic characteristics and there was no clinical and histopathological examination of these. Therefore, the diagnosis is suggestive and not definitive.
One case of osteoma was found in this study at the lower border of the mandible (Figure 5). Osteomas are benign and asymptomatic tumours. However, they can increase in size causing cosmetic disfigurement and functional impairment and therefore require radiographic follow-up. It is important to evaluate their possible relationship with Gardner's syndrome.1,21
Figure 5.
A periapical cyst in sagittal reformatting (a); arrow is indicating osteoma in the panoramic reformatting (b).
Two cases of odontomas were found in this study. An odontoma is a tumour formed by the dental tissue that presents itself as a calcified mass, with a rounded or irregular shape.22 The treatment consists of surgical removal.23
Six cases of periapical cyst (Figure 5) and one dentigerous cyst were found in this study. These cysts can cause cortical expansion, root resorption and displacement of adjacent teeth. None of the cysts observed were large and the treatment normally recommended is enucleation. A diagnosis of the dentigerous cyst was considered in this study when the follicular space was >5 mm and the periapical cysts when the apical lesion was >10 mm.23
We also found one case of bone dysplasia in a 54-year-old female patient. This fibro-osseous lesion rarely produces symptoms and requires no treatment. However, regular monitoring with periodic radiographs is recommended to evaluate the development of the injury.1
Tooth findings
The largest number of IFs in this research was found in the tooth zone, with 27.32% of the findings (Figure 2), similar to a previous study.9 A total of 153 IFs were observed, involving dental anomalies and pulp, periapical and periodontal changes.
105 cases of dental anomalies were found. Teeth with taurodontism, supernumerary roots and root dilaceration do not require treatment. However, in cases of endodontic treatment or surgery, such teeth require better evaluation. Patients with agenesis require treatment only in cases of aesthetic or functional disability. In teeth with giroversion, orthodontic treatment may be indicated depending on their degree of rotation.23
A case of dens in dente of a maxillary central incisor was found. The invagination often communicates with the oral cavity, allowing the entry of irritants and microorganisms directly into the pulp tissues. In such cases, restorative treatment is necessary, or in more severe cases, endodontic treatment.23
Cases of supernumerary teeth and impacted teeth were also observed (Figure 6), and the treatment of these teeth depends on their position and their effects on the adjacent teeth. Diagnosis and early treatment are important to minimize the risk of complications.1
Figure 6.
The arrows are indicating supernumerary teeth in sagittal reformatting (a); an endoperio lesion in the sagittal reformatting (b); and a tooth retained causing external resorption in the adjacent tooth in the sagittal reformatting (c).
Furthermore, we also observed 48 cases of endodontic and periapical changes. Pulp calcifications are asymptomatic and do not need treatment, whereas apical lesions, endoperio lesions (Figure 6) and furcation lesions require treatment by a dentist.23
Soft-tissue calcification findings
The soft-tissue calcification zone is the third most prevalent finding in the sample, with 20.53% of the findings (Figure 2), which is similar to a previous study with 20%1 and above the amount found by another study13 with 12.92%.
With regard to age, it was found as a statistically significant difference that the older the patient, the greater the number of calcifications. This corroborates with a systematic review of research of IFs, in which the authors concluded that soft-tissue calcifications were much more common where there was a sample with older people.2 Patients in another CBCT study demonstrated that atheroma was 13.4 times more common in patients older than 65 years. In our study, 50% of the sample was patients more than 40 years.15
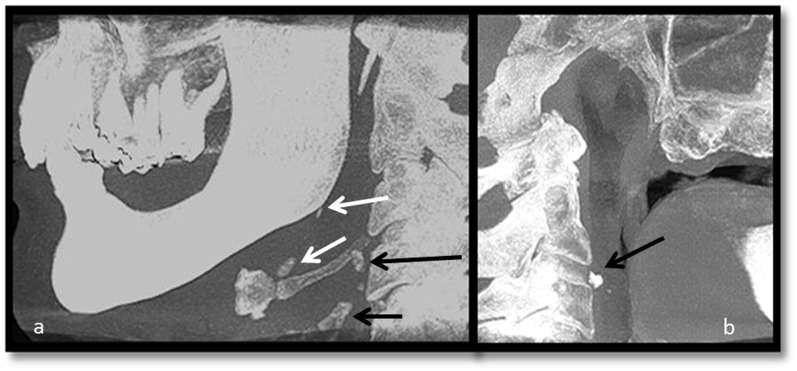
A diagnosis of ossification of the style–hyoid complex was made in 82 cases (Figure 7), which was considered in this study to be cases above 3-cm long.24,25 Usually, it shows no symptoms and no treatment is necessary. However, if there are any symptoms, they may be associated with Eagle's syndrome.25
Figure 7.
Ossification of the styloid complex (white arrows), calcification of the triticeous cartilage (long black arrow) and calcification of the greater horn of the thyroid (short black arrow) in sagittal reformatting (a); the arrow is indicating atheroma in sagittal reformatting (b).
17 cases of tonsilloliths were diagnosed in this study. These calcifications are present in the tonsils and can be single or multiple. They are usually asymptomatic and no treatment is usually necessary. Larger ones can cause bad breath, a sore throat, dysphagia or foreign body sensation, thereby requiring medical treatment.1,24
Two cases of atheroma were observed in this study (Figure 7). Atheromas present as single or multiple rice grains, with homogeneous density, and lateral cervical vertebrae in positions ranging between C3 and C4.2 Referral of these patients to a specialist to confirm the diagnosis contributes significantly to reducing stroke and its sequelae.26
The calcification of the triticeous cartilage and greater horn thyroid calcification was observed in 14 patients (Figure 7). Thyroid cartilage is part of the skeleton of the upper larynx and triticeous cartilage is located in the thyrohyoid ligament. They are bilateral ovoid structures that have a tendency to calcify with increasing age and are IFs without clinical symptoms. No treatment is necessary.1
Clinical management of incidental findings
In this study, most of the IFs do not require treatment or referral to another professional. This shows that not all IFs in CBCT examinations have a great impact on the health of the patient and only a minority need medical or dental work. In the literature, we observed similar results. In a previous study, 43.46% of IFs did not require treatment, 28.97% findings required monitoring and a minority of findings, with 22.57%, needed treatment or referral to another professional.1 In another study, only two results were significant enough to cause changes in orthodontic treatment in the sample.9 In another previous study, only 1 IF of high importance was reported, with the other 97 findings being of intermediate importance and 242 findings of low importance.20
We observed a large variety and quantity of IFs in this sample, which shows the importance of a dentist/radiologist evaluating the entire volume of the CBCT examination. In addition, the results reinforce the need for dentists to study and recognize the entire anatomy and anatomical variations of the maxillofacial region. In the literature, there are some researches with the same approach, but none with a Brazilian sample. There is a variation in the frequency and type of IFs between different samples. For example, in a study that used an Indian sample, the most frequent IFs were malignant lesions.14
Conclusions
– A total of 560 IFs were found in 92% of the samples studied, with the maxilla/mandible group presenting more findings, followed by the maxilla and finally the mandible group.
– The most frequent zone of IFs was the teeth zone, followed by airways, soft-tissue calcification, TMJ, bone and lesions of the jaws.
– Most of the IFs of this sample do not require treatment or referral to another professional.
– A statistically significant difference in the soft-tissue calcification zone was found, where there were a greater number of IFs with increasing age.
– This study showed a high frequency of IFs in CBCT examinations for dental purposes. The findings showed the importance for dentists/radiologists to examine the entire volume of the CBCT examination, in the three reformations, not only the purpose of the examination region.
Contributor Information
Ivna A Lopes, Email: ivnalbano@hotmail.com.
Rosana M A Tucunduva, Email: ivnalbano@hotmail.com.
Roberta H Handem, Email: ivnalbano@hotmail.com.
Ana Lucia A Capelozza, Email: ivnalbano@hotmail.com.
References
- 1.Price JB, Thaw KL, Tyndall DA, Ludlow JB, Padilla RJ. Incidental findings from cone beam computed tomography of the maxillofacial region: a descriptive retrospective study. Clin Oral Implants Res 2012; 23: 1261–8. doi: https://doi.org/10.1111/j.1600-0501.2011.02299.x [DOI] [PubMed] [Google Scholar]
- 2.Edwards R, Altalibi M, Flores-Mir C. The frequency and nature of incidental findings in cone-beam computed tomographic scans of the head and neck region: a systematic review. J Am Dent Assoc 2013; 144: 161–70. doi: https://doi.org/10.14219/jada.archive.2013.0095 [DOI] [PubMed] [Google Scholar]
- 3.Carter L, Farman AG, Geist J, Scarfe WC, Angelopoulos C, Nair MK, et al. ; American Academy of Oral and Maxillofacial Radiology. American academy of oral and maxillofacial radiology executive opinion statement on performing and interpreting diagnostic cone beam computed tomography. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2008; 106: 561–2. doi: https://doi.org/10.1016/j.tripleo.2008.07.007 [DOI] [PubMed] [Google Scholar]
- 4.Horner K, Islam M, Flygare L, Tsiklakis K, Whaites E. Basic principles for use of dental cone beam computed tomography: consensus guidelines of the European Academy of Dental and Maxillofacial Radiology. Dentomaxillofac Radiol 2009; 38: 187–95. doi: https://doi.org/10.1259/dmfr/74941012 [DOI] [PubMed] [Google Scholar]
- 5.Bondemark L, Jeppsson M, Lindh-Ingildsen L, Rangne K. Incidental findings of pathology and abnormality in pretreatment orthodontic panoramic radiographs. Angle Orthod 2006; 76: 98–102. [DOI] [PubMed] [Google Scholar]
- 6.Granlund CM, Lith A, Molander B, Gröndahl K, Hansen K, Ekestubbe A. Frequency of errors and pathology in panoramic images of young orthodontic patients. Eur J Orthod 2012; 34: 452–7. doi: https://doi.org/10.1093/ejo/cjr035 [DOI] [PubMed] [Google Scholar]
- 7.Kuhlberg AJ, Norton LA. Pathologic findings in orthodontic radiographic images. Am J Orthod Dentofacial Orthop 2003; 123: 182–4. doi: https://doi.org/10.1067/mod.2003.4 [DOI] [PubMed] [Google Scholar]
- 8.Cha JY, Mah J, Sinclair P. Incidental findings in the maxillofacial area with 3-dimensional cone-beam imaging. Am J Orthod Dentofacial Orthop 2007; 132: 7–14. doi: https://doi.org/10.1016/j.ajodo.2005.08.041 [DOI] [PubMed] [Google Scholar]
- 9.Drage N, Rogers S, Greenall C, Playle R. Incidental findings on cone beam computed tomography in orthodontic patients. J Orthod 2013; 40: 29–37. doi: https://doi.org/10.1179/1465313312Y.0000000027 [DOI] [PubMed] [Google Scholar]
- 10.Allareddy V, Vincent SD, Hellstein JW, Qian F, Smoker WR, Ruprecht A. Incidental findings on cone beam computed tomography images. Int J Dent 2012; 9: 871532. doi: https://doi.org/10.1155/2012/871532 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Çağlayan F, Tozoğlu U. Incidental findings in the maxillofacial region detected by cone beam CT. Diagn Interv Radiol 2012; 18: 159–63. doi: https://doi.org/10.4261/1305-3825.DIR.4341-11.2 [DOI] [PubMed] [Google Scholar]
- 12.Edwards R, Alsufyani N, Heo G, Flores-Mir C. The frequency and nature of incidental findings in large-field cone beam computed tomography scans of an orthodontic sample. Prog Orthod 2014; 15: 37. doi: https://doi.org/10.1186/s40510-014-0037-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rheem S, Nielsen IB, Oberoi S. Incidental findings in the maxillofacial region identified on cone-beam computed tomography scans. J Orthod Res 2013; 1: 33–9. doi: https://doi.org/10.4103/2321-3825.112254 [Google Scholar]
- 14.Warhekar S, Nagarajappa S, Dasar PL, Warhekar AM, Parihar A, Phulambrikar T, et al. Incidental findings on cone beam computed tomography and reasons for referral by dental practitioners in indore city (M.P). J Clin Diagn Res 2015; 9: ZC21–4. doi: https://doi.org/10.7860/JCDR/2015/11705.5555 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pette GA, Norkin FJ, Ganeles J, Hardigan P, Lask E, Zfaz S, et al. Incidental findings from a retrospective study of 318 cone beam computed tomography consultation reports. Int J Oral Maxillofac Implants 2012; 27: 595–603. [PubMed] [Google Scholar]
- 16.Vallo J, Suominen-Taipale L, Huumonen S, Soikkonen K, Norblad A. Prevalence of mucosal abnormalities of the maxillary sinus and their relationship to dental disease in panoramic radiography: results from the Health 2000 Health Examination Survey. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2010; 109: e80–7. doi: https://doi.org/10.1016/j.tripleo.2009.10.031 [DOI] [PubMed] [Google Scholar]
- 17.Guijarro-Martínez R, Swennen GR. Cone-beam computerized tomography imaging and analysis of the upper airway: a systematic review of the literature. Int J Oral Maxillofac Surg 2011; 40: 1227–37. doi: https://doi.org/10.1016/j.ijom.2011.06.017 [DOI] [PubMed] [Google Scholar]
- 18.dos Anjos Pontual ML, Freire JS, Barbosa JM, Frazão MA, dos Anjos Pontual A. Evaluation of bone changes in the temporomandibular joint using cone beam CT. Dentomaxillofac Radiol 2012; 41: 24–9. doi: https://doi.org/10.1259/dmfr/17815139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nogueira AS, Gonçales ES, Santos PS, Damante JH, Alencar PN, Sampaio FA, et al. Clinical, tomographic aspects and relevance of torus palatinus: case report of two sisters. Surg Radiol Anat 2013; 35: 867–7. doi: https://doi.org/10.1007/s00276-013-1114-4 [DOI] [PubMed] [Google Scholar]
- 20.Doğramacı EJ, Rossi-Fedele G, McDonald F. Clinical importance of incidental findings reported on small-volume dental cone beam computed tomography scans focused on impacted maxillary canine teeth. Oral Surg Oral Med Oral Pathol Oral Radiol 2014; 118: e205–9. doi: https://doi.org/10.1016/j.oooo.2014.09.006 [DOI] [PubMed] [Google Scholar]
- 21.Manjunatha BS, Das N, Sutariya R, Ahmed T. Peripheral osteoma of the body of mandible. BMJ Case Rep 2013; 2013. doi: https://doi.org/10.1136/bcr-2013-009857 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bereket C, Çakır-Özkan N, Şener İ, Bulut E, Tek M. Complex and compound odontomas: analysis of 69 cases and a rare case of erupted compound odontoma. Niger J Clin Pract 2015; 18: 726–30. doi: https://doi.org/10.4103/1119-3077.154209 [DOI] [PubMed] [Google Scholar]
- 23.White SC, Pharoah MJ. Oral radiology: principles and interpretation. 7th edn. St. Louis, Missouri: Elsevier; 2014. p. 679. [Google Scholar]
- 24.Centurion BS, Imada TS, Pagin O, Capelozza AL, Lauris JR, Rubira-Bullen IR. How to assess tonsilloliths and styloid chain ossifications on cone beam computed tomography images. Oral Dis 2013; 19: 473–8. doi: https://doi.org/10.1111/odi.12026 [DOI] [PubMed] [Google Scholar]
- 25.Chaves H, Costa F, Cavalcante D, Ribeiro T, Gondim D. Asymptomatic bilateral elongated and mineralized stylohyoid complex: report of one case. Rev Med Chil 2013; 141: 793–6. doi: https://doi.org/10.4067/S0034-98872013000600015 [DOI] [PubMed] [Google Scholar]
- 26.Angelopoulos C. Anatomy of the maxillofacial region in the three planes of section. Dent Clin North Am 2014; 58: 497–521. doi: https://doi.org/10.1016/j.cden.2014.03.001 [DOI] [PubMed] [Google Scholar]