Abstract
Objectives:
To find the differences between treatment decisions of lower impacted third molars among experts of oral and maxillofacial surgery according to panoramic radiographic and CBCT findings.
Methods:
A retrospective analysis of 62 panoramic radiographs and CBCT of lower third molars evaluated for treatment decisions by 9 independent experts of oral and maxillofacial surgery.
Results:
Differences in interpretation of the panoramic radiography were found between surgeons. The absence of radiological signs suspected for risk to the inferior alveolar nerve lead to the decision of extraction according to panoramic radiography without CBCT (p < 0.01). The presence of those signs lead to referral to CBCT by surgeons before treatment but did not change their decision.
Conclusions:
Treatment decision for surgical treatment of the lower third molar can be accepted without CBCT findings. The use of CBCT is popular before extraction of lower third molars. We found that it has a little effect on the treatment decision of the surgical intervention in comparison to panoramic radiography.
Keywords: lower third molar extractions, imaging methods, treatment decision, CBCT
Introduction
Mandibular third molar extraction is a common procedure. Indications to perform the operation are mainly due to the presence of tooth decay, tooth impaction-related pathologies and preventing future problems such as tooth-related pericoronitis, cysts, tumours and periodontal problems.1
Risks and complications of surgical procedures include bleeding, infection, jaw fracture, nerve damage of the lingual nerve and of the inferior alveolar nerve (IAN).
The incidence of risks is associated with the following factors: age, gender and health status according to the American Society of Anesthesiologists, bone density, tooth position, the degree of impaction and the degree of surgeon experience.2
Sensory injury of the IAN is a complication that most of the dentists and oral surgeons would like to prevent; the incidence of IAN injury is 0.4–0.7%.1,2 The rate of temporary damage to the IAN is between 4% and 8%1,2 when the procedure is performed by an expert surgeon;2 the damage is the result of direct trauma to the nerve itself (tearing or damaging the nerve by drills or by pushing the root to the canal) or of later complications such as oedema or haemorrhage.1
Imaging methods are used to provide information regarding the number and location of the roots of teeth and their proximity to the mandibular canal. The common means used today are panoramic radiography and CBCT.
Panoramic radiography gives a complete picture of the jaw structures, vital structures, the temporomandibular joints, adjacent important structures of the jaws and possible pathologies. Panoramic radiographs give information in the anteroposterior relation but not the buccolingual relation between the tooth and vital structures, and it has lower picture sharpness3 and distortion of the dimensions in 20–35% of the cases.4,5
Nowadays the use of CBCT as a routine imaging technique before oral surgery procedures is very popular, whereas in the past, CT was used instead. CBCT has the advantages of lower price and less radiation dose without degradation of image quality.6
It is claimed that in cases where there is proximity or overlap between the root canal, we need more information.3–5
CBCT gives a three-dimensional image with high quality and accuracy and a lesser amount of radiation than medical CT. It is available and its use is easier and cheaper.3 The distortion created by CBCT is negligible and ranges from 0.05 to 0.04 mm. The percentage of distortion is close to 0%,7,8 therefore theoretically, it is more precise than panoramic radiography and may change the treatment decision of the oral surgeon.
An alternative treatment modality for surgical extraction of the lower third molar (in special occasions) is partial odontectomy or coronectomy. The technique of coronectomy, partial odontectomy or deliberate root retention is used to protect the IAN.9 The technique of coronectomy is worth considering in cases in which panoramic radiography and CBCT scanning show an intimate relationship between the roots of the mandibular third molar and the IAN.
This study examined the additional value of CBCT information to the therapeutic decision of impacted lower third molar (full extraction/coronectomy/partial odontectomy) among experts of oral and maxillofacial surgery.
The purpose of the study
To check if the information obtained from CBCT of the impacted third molar in comparison to data obtained from panoramic radiography has an effect on treatment decision of lower third molars among experts of oral and maxillofacial surgery.
Methods and materials
65 panoramic radiographs and CBCTs of patients treated in the Department of Oral and Maxillofacial Surgery in 2 medical centres were evaluated retrospectively by 9 independent experts of oral and maxillofacial surgery.
Ethical approval and Helsinki approval were obtained from the ethical committee and Helsinki committees of the medical centres as required (No. 121/11).
Inclusion criteria
Patients who had undergone extractions of lower third molars.
Patients who have had both panoramic radiography and CBCT before the operation.
Radiography and the CBCT were performed for treatment itself as regular medical records before the operation.
The radiographic images were evaluated independently and separately by experts of oral and maxillofacial surgery in different sessions for panoramic radiography and CBCT.
The radiographic images of the same patient were not evaluated during the same session by the same surgeon.
Exclusion criteria
Patients who did not have both panoramic radiography and CBCT of lower third molars
Poor resolution or poor quality images not enabling identification of anatomical landmarks.
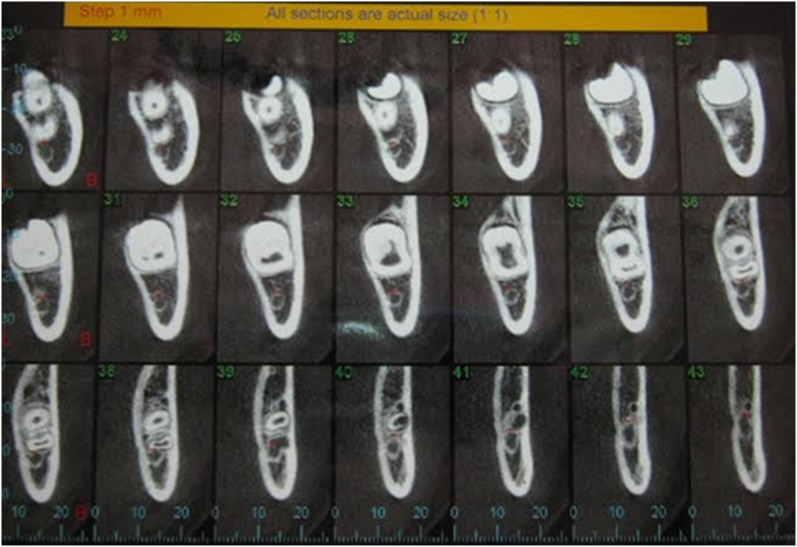
All the images were coded randomly and arranged in two files. A total of three cases were excluded because of poor quality of panoramic radiography (Figures 1 and 2). Consequently a total of 62 cases were examined in this study.
Figure 1.
Panoramic radiographs of poor quality.
Figure 2.
Panoramic radiograph of good quality.
The images were presented to the surgeons continuously on a computer screen enabling changing the degree of contrast and brightness. The images of the same patients were evaluated separately by each individual surgeon, first viewing the panoramic radiographs and after 1 month, the CBCTs.
The surgeons were asked to consider the following criteria: are there indicating risks of the tooth extraction, whether to perform a full extraction or to perform coronectomy (full extraction yes/no, coronectomy yes/no). The same questions were asked both for CT and for panoramic radiography.
Statistical analysis was performed on the results to find out if there was a difference between the treatment decisions according to panoramic radiography and CBCT.
The statistical analysis included:
(1) Analysis of variance with repeated observations: distribution test—to find out the differences between the surgeons and the interpretation of the images with different modalities; differences in treatment decisions among different surgeons regarding the same patient according to the different radiological modalities and the distribution of decisions of the same surgeon regarding the same patient.
(2) Non-parametric correlation analysis: Spearman Rho test regarding the radiological findings and treatment decisions. Correlations were performed between the radiological findings and treatment decisions.
(3) Kappa for interrater and intrarater agreement.
Results
The treatment decision of the surgeons according to panoramic radiography and CBCT is demonstrated in Table 1. In most of the cases, the treatment decision was total extraction according to both imaging modalities. In several cases (26), the treatment decision following CBCT findings was changed to coronectomy (Table 2).
Table 1.
Treatment decision of each surgeon according to panoramic radiography and CBCT and kappa interrater and internal coherence
| Doctor | Seniority (years) | Treatment decision according to panorex | Treatment decision according to CBCT | Kappa | Significance |
|---|---|---|---|---|---|
| 1 | 10 | 17 | 45 | 0.023 | NS |
| 2 | 5 | 20 | 42 | 0.000 | NS |
| 3 | 35 | 50 | 12 | 0.000 | NS |
| 4 | 15 | 31 | 31 | 0.033 | NS |
| 5 | 13 | 33 | 29 | 0.012 | NS |
| 6 | 40 | 50 | 12 | 0.000 | NS |
| 7 | 10 | 24 | 38 | 0.000 | NS |
| 8 | 10 | 33 | 29 | 0.000 | NS |
| 9 | 15 | 33 | 29 | 0.052 | NS |
| All | 291 | 267 | 0.038 | 0.045 |
NS, not significant.
Table 2.
Panoramic radiography and CBCT cross-tabulation among all doctors regarding treatment decisions
| Treatment Decision | Panoramic extraction | Panoramic CBCT referral | Total |
|---|---|---|---|
| CT extraction | 291 | 241 | 532 |
| CT coronectomy | 9 | 17 | 26 |
| Total | 300 | 258 | 558 |
The interrater agreement was low between the physicians (kappa = 0.038 p < 0.05).
Table 1 demonstrates that the interrater agreement was low and non-significant.
Table 3 demonstrates the included cases with the risk for IDN injury according to panoramic radiography and CBCT as interpreted by different surgeons. The interpretation of panoramic radiography regarding the signs of risk to IAN injury during extraction in provided in Table 3.
Table 3.
Descriptive data for included cases (number of patients)
| Surgeon | Risk for IDN injury/panorex | Multirooted teeth/panorex | Multirooted teeth/CBCT | Risk for IDN injury/CBCT |
|---|---|---|---|---|
| 1 | 38 | 11 | 13 | 17 |
| 2 | 31 | 10 | 0 | 4 |
| 3 | 33 | 5 | 0 | 30 |
| 4 | 33 | 5 | 0 | 4 |
| 5 | 33 | 1 | 6 | 12 |
| 6 | 35 | 7 | 2 | 7 |
| 7 | 31 | 17 | 0 | 22 |
| 8 | 49 | 10 | 8 | 36 |
| 9 | 23 | 3 | 0 | 3 |
IDN, inferior dental nerve.
A re-evaluation of the cases to establish kappa of each evaluator, with their own opinion according to panoramic radiography and CBCT is provided in Table 1. CBCT provided additional information for treatment decision of extraction in most of the cases and for coronectomy in several cases. Panoramic radiography did not enable treatment decision of coronectomy in any of the cases.
The interpretation of the panoramic radiography was different between surgeons—there was no consensus on any of the radiological findings that could lead to potential damage to the IAN according to Rood and Shehab4 (Table 3).
Correlation tests found that the treatment suggested according to panoramic radiography (referral to CBCT) is inversely proportional to the findings: root darkening (p < 0.01) and root split (p < 0.06) discontinuity of canal upper border (p < 0.15). Absence of this signs enabled the surgeons to get their treatment decision according to panoramic radiographs. Presence of this signs enabled the surgeons to get their treatment decision only after CBCT findings.
There was no difference between the surgeons according to their seniority and their treatment decision following the findings in panoramic radiographs (Table 1).
Discussion
The surgical approach of total extraction of impacted third molar can be accepted according to panoramic radiography if the tooth is far enough from the IDN canal.
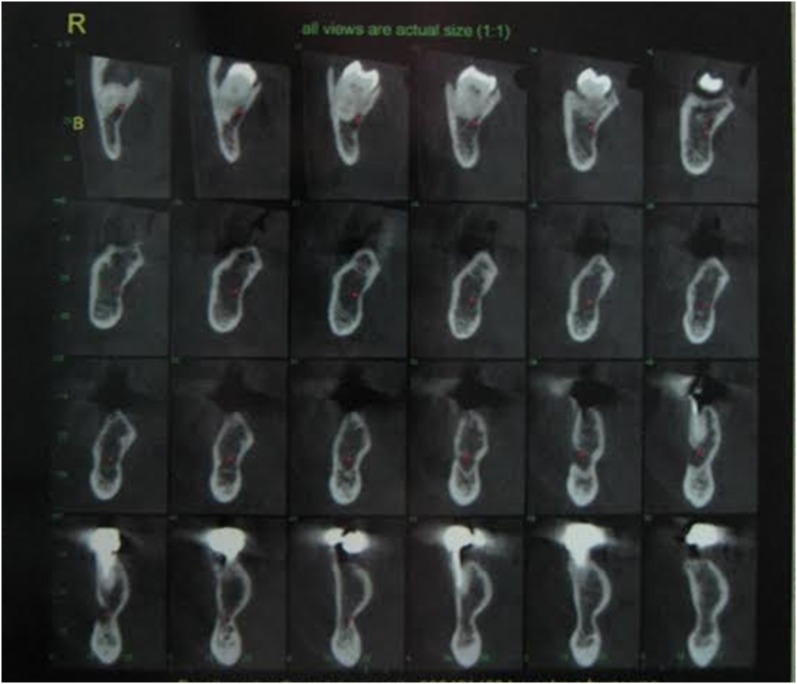
The radiological risk factors for IAN damage may be revealed in panoramic radiography. If the relationship of the tooth roots and the inferior alveolar canal is not clear, the surgeon would recommend to decide after CBCT imaging. However, Petersen et al10 found that CBCT was not superior to panoramic imaging in avoiding neurosensoric disturbances and concluded that the use of CBCT before removal of the mandibular third molar does not seem to reduce the number of neurosensoric disturbances. Guerrero et al11,12 concluded that CBCT was not better than panoramic radiography in predicting post-operative complications for moderate-risk cases of impacted lower third molars. Nonetheless, a CBCT buccolingual view can accurately confirm the number of roots and root morphology of the third molar better than panoramic radiography (Figure 3).
Figure 3.
Good-quality CBCT.
The use of CBCT is widespread nowadays due to availabilty and medicolegal environment but is does not have actual contribution. The author agrees with Roeder et al13 and considers that CBCT scans should only be performed in high-risk wisdom tooth removals or for determination of the surgical approach and/or for coping with intraoperative complications. An effort to reduce the use of CBCT should be carried out when not necessary, in order to reduce radiation exposure and damage to the patient (Figure 4).
Figure 4.
Poor-quality CBCT.
According to the literature,6,8 61% of the surgeons (among 72) needed CBCT to understand the relationship between the roots and canal. In our study, there was a difference between interpretation of panoramic radiographs between the surgeons. Suspicious signs of root proximity to the IAN lead to CBCT referral before the treatment. The CBCT findings gave the surgeons the confidence for total extraction in most of the cases and for coronectomy in few of the cases.
Rood and Shehab5 tested the predictive ability of IAN injury according to panoramic radiography with seven radiological parameters. Four of them related to the roots: (a) root darkening, (B) root diversion, (C) root narrowing and (D) root splitting. Additional parameters associated with the canal were (a) loss of continuity of the upper border of the IAN canal, (b) canal deflection and (c) narrowing of the canal. Significant correlation was found between canal deflection, root darkening and loss of continuity of canal borders and the possibility of nerve damage following surgical treatment in lower third molars. All other parameters were not significant. In our study, it was found that the existence of the signs regarding the root in panoramic radiography lead to CBCT referral before accepting the treatment decision. Although the treatment decision did not change, most of the physicians preferred to examine CBCT scans before treatment in order to plan the way of tooth removal and to handle intraoperative complications.
According to the literature,6 a recommendation of CBCT examination for pre-operative radiographic evaluation of complicated impacted lower third molars is necessary because CBCT revealed the number of roots of teeth more reliably than panoramic radiographs. Also in our study, although the risks of IAN damage were known to the surgeon according to panoramic radiography, additional information from CBCT was necessary to the surgeon for treatment of suspicious patients having too many questions regarding the risks. This contributed to the CBCT referral without a definite contribution to the treatment decision due to medicolegal reasons.
CT and CBCT imaging are more accurate to determine the ratio between the impacted tooth to the IAN canal and the exact location and relationship between them.4,6,14 It was found that the lingual location of the canal is associated with IAN damage.14 This increases the predictability of preventing possible IAN injury and helps the surgeon to plan the surgical procedure reducing the risks. However, the amount of radiation and high cost limit their use.
The risk of lingual plate fracture during an extraction and a displaced residual root into the submandibular space exists in an extraction of impacted root and proximity of the roots to the thin lingual plate, the information regarding this proximity and the width of the lingual plate can be achieved only from CBCT. The contribution of the CBCT information is important during an intraoperative complication; for example, in case of root fracture and residual root tip stacked in a thin lingual plate, the surgeon should decide intraoperatively to extract it or to leave it. Having the information provided by CBCT can help the surgeon prevent other complications by trying to handle a stacked root tip in a thin lingual plate.
On the other hand, the decision to leave a residual root tip can be accepted according to panoramic radiography. During the follow-up period, a CBCT should be considered only when necessary.
In our study, the main reason for CBCT referral was suspicious radiological signs of root–canal direct relationship, but it did not affect the treatment decision in most of the cases. In most of the cases, CBCT helped the surgeons to perform total extractions and plan it according to the CBCT findings.
Whenever a treatment is needed, the physician should consider the risks of treatment according to imaging. The type of image selected is according to the principle of radiation imaging, as low as reasonably achievable; it is necessary to perform the most basic imaging that will provide the necessary information.14 The image provides the necessary information when it affects the treatment decision and the surgical approach.
It was found in the present study that oral surgeons do not need CBCT to decide the treatment for impacted lower third molar. It was also stated that CBCT does not give a precise risk for perforation of the inferior alveolar nerve canal in comparison to panoramic radiography.14 The present study agrees with Matzen et al15 who found that CT did not change treatment decision accepted according to panoramic radiography in 88% of the cases. All the surgeons decided, in most of the cases, for extraction of the tooth without additional radiological information (CBCT).
Among the patients included in the study there were also CBCT and panoramic radiographs that were taken as a result of medicolegal reasons and for accepting an assistance for the surgical approach. The surgeons who checked the findings agreed that in some cases, CBCT gave additional information in comparison to the panoramic radiography, but this information did not affect the treatment decision.
One of the treatment modalities of lower third molars is partial odontectomy or coronectomy. It can be performed in particular cases and lowers the risk for IAN damage. This procedure is known to all the surgeons who participated in the study. We found that in most of the cases, the additional information from CBCT did not change the treatment decision from total extraction to coronectomy. The decision for coronectomy was accepted in <30% of the cases. The decision for coronectomy can be accepted according to panoramic radiography. Since the side effects and quality of life of the patients undergoing coronectomy is not different from patients undergoing total extraction of impacted lower third molar, it can also be recommended in cases with increased risk for IAN injury.16
Conclusion
The CBCT provides negligible information regarding the treatment decision but may help to plan the surgical approach by the surgeon and may provide a backup to inexperienced surgeons.
Treatment decision regarding third molar extraction or coronectomy can be accepted according to information provided from panoramic radiography thus saving unnecessary radiation to the patient.
Despite the contribution of CBCT imaging to the understanding of the relationship between the tooth root and the inferior dental canal, only in several cases there was a change in treatment decisions according to it.
Contributor Information
Yifat Manor, Email: yifatmanor@gmail.com.
Refael Abir, Email: rafiabir@gmail.com.
Alex Manor, Email: manoriphone@gmail.com.
Israel Kaffe, Email: Kaffed@post.tau.ac.il.
References
- 1.Blondeau F, Daniel NG. Extraction of impacted mandibular third molar: postoperative complication and their risk factors. J Can Dent Assoc 2007; 73: 325–7. [PubMed] [Google Scholar]
- 2.Jerjes W, Swinson B, Moles DR, El-Maaytah M, Banu B, Upile T, et al. Permanent sensory nerve impairment following third molar surgery: a prospective study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2006; 102: e1–7. doi: https://doi.org/10.1016/j.tripleo.2006.01.016 [DOI] [PubMed] [Google Scholar]
- 3.Lindh C, Petersson A, Klinge B. Visualization of the mandibular canal by different radiographic techniques. Clin Oral Implants Res 1992; 3: 90–7. doi: https://doi.org/10.1034/j.1600-0501.1992.030207.x [DOI] [PubMed] [Google Scholar]
- 4.Rood JP, Shehab BA. The radiological prediction of inferior alveolar nerve injury during third molar surgery. Br J Oral Maxillofac Surg 1990; 28: 20–5. doi: https://doi.org/10.1016/0266-4356(90)90005-6 [DOI] [PubMed] [Google Scholar]
- 5.Suomalainen A, Ventä I, Mattila M, Turtola L, Vehmas T, Peltola JS. Reliability of CBCT and other radiographic methods in preoperative evaluation of lower third molars. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2010; 109: 276–84. doi: https://doi.org/10.1016/j.tripleo.2009.10.021 [DOI] [PubMed] [Google Scholar]
- 6.White SC, Pharoah MJ. Oral radiology principles and interpretation. 5th edn. St Louis, MO: Elsevier/Mosby; 2004. pp. 247–55. [Google Scholar]
- 7.Damstra J, Fourie Z, Huddleston Slater JJ, Ren Y. Accuracy of linear measurements from cone-beam computed tomography-derived surface models of different voxel sizes. Am J Orthod Dentofacial Orthop 2010; 137: e1–6; discussion 16–17. doi: https://doi.org/10.1016/j.ajodo.2009.06.016 [DOI] [PubMed] [Google Scholar]
- 8.Koong B, Pharoah MJ, Bulsara M, Tennant M. Methods of determining the relationship of the mandibular canal and third molars: a survey of Australian oral and maxillofacial surgeons. Aust Dent J 2006; 51: 64–8. doi: https://doi.org/10.1111/j.1834-7819.2006.tb00403.x [DOI] [PubMed] [Google Scholar]
- 9.Pogrel MA. Partial odontectomy. Oral Maxillofac Surg Clin North Am 2007; 19: 85–91. doi: https://doi.org/10.1016/j.coms.2006.11.006 [DOI] [PubMed] [Google Scholar]
- 10.Petersen LB, Vaeth M, Wenzel A. Neurosensoric disturbances after surgical removal of the mandibular third molar based on either panoramic imaging or cone beam CT scanning: a randomized controlled trial (RCT). Dentomaxillofac Radiol 2016; 45: 20150224. doi: https://doi.org/10.1259/dmfr.20150224 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Guerrero ME, Botetano R, Beltran J, Horner K, Jacobs R. Can preoperative imaging help to predict postoperative outcome after wisdom tooth removal? A randomized controlled trial using panoramic radiography versus cone-beam CT. Clin Oral Investig 2014; 18: 335–42. doi: https://doi.org/10.1007/s00784-013-0971-x [DOI] [PubMed] [Google Scholar]
- 12.Guerrero ME, Nackaerts O, Beinsberger J, Horner K, Schoenaers J, Jacobs R; SEDENTEXCT Project Consortium. Inferior alveolar nerve sensory disturbance after impacted mandibular third molar evaluation using cone beam computed tomography and panoramic radiography: a pilot study. J Oral Maxillofac Surg 2012; 70: 2264–70. doi: https://doi.org/10.1016/j.joms.2012.04.015 [DOI] [PubMed] [Google Scholar]
- 13.Roeder F, Wachtlin D, Schulze R. Necessity of 3D visualization for the removal of lower wisdom teeth: required sample size to prove non-inferiority of panoramic radiography compared to CBCT. Clin Oral Investig 2012; 16: 699–706. doi: https://doi.org/10.1007/s00784-011-0553-8 [DOI] [PubMed] [Google Scholar]
- 14.Ghaeminia H, Meijer GJ, Soehardi A, Borstlap WA, Mulder J, Bergé SJ. Position of the impacted third molar in relation to the mandibular canal. Diagnostic accuracy of cone beam computed tomography compared with panoramic radiography. Int J Oral Maxillofac Surg 2009; 38: 964–71. doi: https://doi.org/10.1016/j.ijom.2009.06.007 [DOI] [PubMed] [Google Scholar]
- 15.Matzen LH, Christensen J, Hintze H, Schou S, Wenzel A. Influence of cone beam CT on treatment plan before surgical intervention of mandibular third molars and impact of radiographic factors on deciding on coronectomy vs surgical removal. Dentomaxillofac Radiol 2013; 42: 98870341. doi: https://doi.org/10.1259/dmfr/98870341 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Manor Y, Bader A, Chaushu G, Haim D, Manor A, Gultekin A, et al. How patients percept their recovery following impacted mandibular third molar coronectomy. J Craniofac Surg 2016; 27: 671–4. doi: https://doi.org/10.1097/SCS.0000000000002565 [DOI] [PubMed] [Google Scholar]