Abstract
Objectives:
To (1) compare pathological findings related to the mandibular third molar in panoramic images (PAN) and CBCT; (2) estimate the frequency of removals if pathological findings were indicative; and (3) assess factors in PAN associated with resorption and marginal bone loss at the second molar as observed in CBCT.
Methods:
379 mandibular third molars were examined with PAN and CBCT. Four observers registered resorption and marginal bone loss at the second molar and increased periodontal space at the third molar in both imaging modalities. Agreement between PAN and CBCT, frequency of removals based on pathological findings in either of the two modalities and interobserver reproducibility was calculated. Logistic regression analyses assessed factors in PAN, which could predict marginal bone loss and resorption observed in CBCT.
Results:
Agreement between PAN and CBCT: resorption 54–74%; marginal bone loss 66–85%; and increased periodontal space 92–97%. Removals based on CBCT and PAN: 58–71% and 36–65%. Interobserver percentage accordance and kappa values ranged from 57 to 98% and 0.10–0.91 for PAN and 61–97% and 0.22–0.78 for CBCT, respectively. Mesioangulated/horizontally positioned third molars were associated with marginal bone loss [odds ratio (OR) = 7.0–31.3; p < 0.001] and resorption (OR = 2.9–35.6; p < 0.001) in CBCT. Overprojection between the third and the second molars in PAN predicted resorption observed in CBCT (OR = 5.6–21.2; p < 0.001).
Conclusions:
Pathology associated with the third molar is more often observed in CBCT than in PAN. More third molars would be removed if pathological findings are based on CBCT. Mesioangulated/horizontally positioned third molars overprojecting the cervical/root part of the second molar in PAN are strongly associated with pathology observed in CBCT.
Keywords: molar, third; CBCT; patient management; resorption
Introduction
Surgical removal of mandibular third molars is one of the most frequently performed surgical procedures in dentistry. There is no evidence to support prophylactic removal of mandibular third molars;1 in contrast, in case of pathological conditions related to the mandibular third molar, removal may be considered.2,3 Pathological changes can be either symptomatic or asymptomatic. In the absence of subjective symptoms, at least three radiographic factors usually determine the decision to remove an impacted/semi-impacted mandibular third molar: resorption in the distal surface of the second molar, marginal bone loss at the distal root surface of the second molar and an increased periodontal space or cyst around the crown of the third molar.2 Thus, if at least one of these pathologies is present in the radiograph, the third molar should be removed. According to the literature,4 panoramic imaging may be the first-choice method for examination of mandibular third molars, since it provides an overview of the teeth and jaws. Intraoral imaging is an alternative, but it has been shown that in around 25–36% of the cases, the full third molar and adjacent anatomical structures are not imaged by this method.5,6
The debate on when to perform CBCT prior to surgical removal of mandibular third molars continues. Recently, is has been shown in a prospective clinical study that CBCT changed the treatment of the patients only in a minority of cases.7 Further, it has been shown in randomized controlled clinical trials that CBCT before removal did not decrease the number of sensory disturbances to the inferior alveolar nerve compared with panoramic imaging.8–10 On the other hand, it was speculated that CBCT could be indicated in cases of doubt after interpreting the panoramic image (PAN) with regard to the presence of root resorption in the distal surface of the second molar, if this was indicative for removal of the tooth.11
The aim of this study was to compare pathological findings observed in a PAN and CBCT taken prior to removal of a mandibular third molar, in the assessment of resorption in the distal surface of the second molar, marginal bone loss at the distal root surface of the second molar and the presence of an increased periodontal space around the crown of the third molar. Further, we aimed to estimate the frequency of removals if the presence of at least one of these pathological findings would be indicative for removal of the third molar, also taking into account observer variation in assessing PAN and CBCT. The third aim was to assess factors in PAN, which may predict the presence of resorption and marginal bone loss in/at the distal surface of the second molar as observed in CBCT.
Methods and materials
Radiographic examination
This was a retrospective study including 379 mandibular third molars (180 in the left side and 199 in the right side; 168 male and 211 female patients; mean age 26 years, range 17–73 years) that had undergone both a panoramic examination and a CBCT prior to removal of the tooth. All patients were referred between 2008 and 2013 to the Section of Oral and Maxillofacial Surgery and Pathology, Department of Dentistry, Aarhus University, for mandibular third molar removal. The radiographic examinations were performed in the Section of Oral Radiology, Department of Dentistry, Aarhus University.
The panoramic examinations were performed with either a Cranex Tome unit (Soredex, Helsinki, Finland) with a phosphor plate image receptor (Digora image plate and PCT scanner; Soredex, Helsinki, Finland) or a ProMax unit (Planmeca, Helsinki, Finland) with a CCD-based image receptor. Two CBCT units were used for the CBCT examinations, either the NewTom 3G (QR SRL, Verona, Italy) (n = 67) or the Scanora 3D (Soredex, Helsinki, Finland) (n = 312). In the NewTom scanner, the patients were examined with a 6 × 8-cm field of view (FOV) and voxel resolution of 0.3 and in the Scanora 3D with a 6 × 6-cm FOV and voxel resolution of 0.13. The FOV was centred at the mandibular third molar region.
Radiographic assessment
The radiographic assessments were performed by four observers. An initial observer, not part of the assessments of pathology, assessed 665 PAN where the patient in addition had a CBCT examination. The inclusion criteria were that (1) the third molar overprojected the second molar in the PAN and (2) there was a period of maximum 3 months between the two radiographic examinations. 401 cases fulfilled these criteria; however, in 22 cases, the CBCT examination was judged to be inadequate for sufficient diagnosis owing to artefacts; thus, the final sample included 379 mandibular third molars.
Four oral radiologists (Observers 1, 2, 3 and 4) assessed the PAN and the CBCT volumes on two separate occasions; the PAN were all assessed at least 3 months before the CBCT volumes. The following variables in relation to the third molar were assessed in both the PAN and in CBCT: (1) angulation (vertical/mesioangulated/distoangulated/horizontal/inverted/transversal); (2) location of contact (for PAN: overprojection) to the second molar (crown/cervical part/root); (3) resorption >0.5 mm into the distal surface of the second molar (yes/no); (4) marginal bone loss >3 mm at the distal surface of the second molar (yes/no); and (5) the presence of an increased periodontal space >4 mm (defined as a cyst) around the crown of the third molar (yes/no).
Data treatment
Data were registered in Microsoft Office Excel® 2010 (Microsoft Corp., Redmond, WA) and imported to SPSS® (IBM Corp., New York, NY; formerly SPSS Inc., Chicago, IL) for statistical treatment. For the statistical analyses, angulation was dichotomized (mesioangulated or horizontal vs others), since the distribution revealed that other angulations were almost never associated with pathology. For each observer recordings in the PAN and CBCT, the percentage agreement/disagreement between findings in the PAN and CBCT was calculated. Moreover, if at least one of the three radiographic signs of pathology was an indication for removal, the frequency of third molars that were to be removed based on the PAN or CBCT, respectively, was calculated.
Interobserver reproducibility was estimated by two outcome variables: percentage of observer accordance and kappa statistics in a pairwise design, for all variables and for the two imaging modalities, respectively. Kappa values >0.75 were defined as “excellent” reproducibility, those between 0.40 and 0.75 as “fair to good” reproducibility and those <0.40 as “moderate to poor” reproducibility.
Initial logistic regression analyses were performed to assess whether angulation of the third molar registered in the PAN could predict the presence of a marginal bone loss >3 mm observed in CBCT (outcome variable), and whether tooth angulation, location of overprojection between the second and third molars or interpretation of resorption in the PAN could predict resorption as observed in CBCT (outcome variable). These analyses were performed for each observer separately, between his/her recordings in the PAN and CBCT of the same patient. Only variables with a significant association in the initial analyses were entered into the multivariate logistic regression analyses along with gender and age.
Results
Comparison between findings in PAN and CBCT
The agreement between pathological findings seen in the PAN and CBCT of the same patient varied among observers. For resorption of the second molar, agreement was lowest: range 54–74% (Table 1); for marginal bone loss >3 mm, agreement range was 66–85% (Table 2); and for cyst around the crown of the third molar, it was 92–97% (Table 3). For resorption of the second molar, approximately three-fourth of the disagreements were due to the fact that resorption was more often observed in CBCT than in the PAN; in few cases, resorption was recorded in the PAN, but not in CBCT. Observers 3 and 4 recorded more severe marginal bone loss >3 mm in CBCT than in PAN; on the other hand, Observers 1 and 2 recorded nearly the same number of cases with marginal bone loss in CBCT and PAN. For assessment of cyst, the few disagreements were equally distributed between the methods for Observer 4, while for Observers 1 and 2, more cysts were recorded in PAN than in CBCT; for Observer 3, it was the opposite.
Table 1.
Agreement between findings of resorption in the distal surface of the second molar in panoramic images (PAN) and CBCT for each observer
| PAN | CBCT |
||||||||
|---|---|---|---|---|---|---|---|---|---|
| Observer 1 |
Observer 2 |
Observer 3 |
Observer 4 |
||||||
| Yes | No | Yes | No | Yes | No | Yes | No | ||
| Observer 1 | Yes | 36 | 25 | ||||||
| No | 148 | 170 | |||||||
| Observer 2 | Yes | 25 | 38 | ||||||
| No | 60 | 256 | |||||||
| Observer 3 | Yes | 59 | 13 | ||||||
| No | 114 | 193 | |||||||
| Observer 4 | Yes | 61 | 13 | ||||||
| No | 147 | 158 | |||||||
Table 2.
Agreement between findings of marginal bone loss >3 mm at the distal surface on the second molar in panoramic images (PAN) and CBCT for each observer
| PAN | CBCT |
||||||||
|---|---|---|---|---|---|---|---|---|---|
| Observer 1 |
Observer 2 |
Observer 3 |
Observer 4 |
||||||
| Yes | No | Yes | No | Yes | No | Yes | No | ||
| Observer 1 | Yes | 58 | 32 | ||||||
| No | 24 | 265 | |||||||
| Observer 2 | Yes | 174 | 37 | ||||||
| No | 44 | 124 | |||||||
| Observer 3 | Yes | 93 | 3 | ||||||
| No | 126 | 157 | |||||||
| Observer 4 | Yes | 69 | 14 | ||||||
| No | 60 | 236 | |||||||
Table 3.
Agreement between findings of a cyst around the crown of the third molar in panoramic images (PAN) and CBCT for each observer
| PAN | CBCT |
||||||||
|---|---|---|---|---|---|---|---|---|---|
| Observer 1 |
Observer 2 |
Observer 3 |
Observer 4 |
||||||
| Yes | No | Yes | No | Yes | No | Yes | No | ||
| Observer 1 | Yes | 0 | 10 | ||||||
| No | 2 | 367 | |||||||
| Observer 2 | Yes | 7 | 28 | ||||||
| No | 3 | 341 | |||||||
| Observer 3 | Yes | 6 | 6 | ||||||
| No | 25 | 342 | |||||||
| Observer 4 | Yes | 2 | 7 | ||||||
| No | 7 | 363 | |||||||
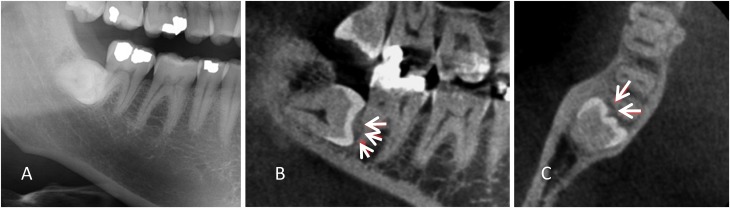
If the presence of at least one of the three radiographic signs of pathology is indicative for removal of the tooth, the frequency of removals would range from 35.5 to 65.2% depending on the observer (mean 47%) when findings are based on the PAN, while it would increase by approximately 20%, range 57.8–70.5% (mean 65%), when findings are based on CBCT (Table 4). Conclusively, more third molars may be removed when one or more of the radiographic signs of pathology observed in CBCT is indicative for removal. Only Observer 2 did not increase the overall number of pathological findings in CBCT compared with the PAN. Figure 1 shows an example of a right mandibular third molar with resorption observed in CBCT by all observers, but not all observers registered pathology in the PAN.
Table 4.
Number of removed third molars based on either the panoramic image (PAN) or CBCT, if the presence of at least one pathological finding would be indicative for removal
| Observers | PAN | CBCT |
|---|---|---|
| Observer 1 | 146 (35.5%) | 219 (57.8%) |
| Observer 2 | 247 (65.2%) | 243 (64.1%) |
| Observer 3 | 164 (43.3%) | 267 (70.5%) |
| Observer 4 | 150 (39.6%) | 250 (66.0%) |
Figure 1.
An impacted right mandibular third molar: in the (a) panoramic image; (b) CBCT image in the sagittal plane; and (c) CBCT image in the axial plane, white arrows are showing resorption of the second molar interpreted in the CBCT image sections.
Interobserver reproducibility in panoramic images and CBCT
Tables 5 and 6 show the pairwise percentage of observer accordance and kappa values among the observers for the two methods. The percentage of accordance among the observer pairs varied from 28.1 to 99.7% for assessment of the PAN and from 61.0 to 97.4% for assessment of CBCT. The results from the kappa statistics ranged from “poor” to “excellent” reproducibility for both modalities.
Table 5.
Percentage of accordance (%) for observers pairwise for assessment of tooth angulation; location of overprojection (in CBCT contact area); and pathology in panoramic images (PAN) and CBCT
| Variable | Observer 1 vs Observer 2 | Observer 1 vs Observer 3 | Observer 1 vs Observer 4 | Observer 2 vs Observer 3 | Observer 2 vs Observer 4 | Observer 3 vs Observer 4 |
|---|---|---|---|---|---|---|
| Angulation | ||||||
| PAN | 95.3% | 98.4% | 98.7% | 94.7% | 95.0% | 97.6% |
| CBCT | 93.7% | 95.0% | 94.5% | 97.1% | 95.5% | 97.4% |
| Location of overprojection | ||||||
| PAN | 81.5% | 89.2% | 81.2% | 82.1% | 84.7% | 82.1% |
| CBCT | 79.4% | 71.8% | 71.8% | 74.4% | 82.9% | 72.6% |
| Resorption | ||||||
| PAN | 80.5% | 90.2% | 82.3% | 81.8% | 79.7% | 81.5% |
| CBCT | 65.4% | 74.9% | 72.0% | 70.5% | 64.9% | 81.4% |
| Marginal bone loss >3 mm | ||||||
| PAN | 28.1% | 92.6% | 85.5% | 60.2% | 57.3% | 88.1% |
| CBCT | 61.0% | 61.2% | 80.7% | 83.9% | 74.4% | 73.6% |
| Cyst | ||||||
| PAN | 89.7% | 99.7% | 97.6% | 89.7% | 92.1% | 97.6% |
| CBCT | 96.8% | 91.3% | 97.1% | 92.4% | 96.6% | 92.1% |
Table 6.
Interobserver reproducibility expressed by kappa values for observers pairwise for assessment of tooth angulation; location of overprojection (in CBCT contact area); and pathology in the panoramic images (PAN) and CBCT
| Variable | Observer 1 vs Observer 2 | Observer 1 vs Observer 3 | Observer 1 vs Observer 4 | Observer 2 vs Observer 3 | Observer 2 vs Observer 4 | Observer 3 vs Observer 4 |
|---|---|---|---|---|---|---|
| Angulation | ||||||
| PAN | 0.88 | 0.96 | 0.97 | 0.86 | 0.87 | 0.94 |
| CBCT | 0.83 | 0.86 | 0.84 | 0.92 | 0.88 | 0.93 |
| Location of overprojection | ||||||
| PAN | 0.68 | 0.81 | 0.67 | 0.69 | 0.74 | 0.69 |
| CBCT | 0.63 | 0.52 | 0.52 | 0.57 | 0.69 | 0.49 |
| Resorption | ||||||
| PAN | 0.29 | 0.66 | 0.40 | 0.38 | 0.32 | 0.41 |
| CBCT | 0.30 | 0.50 | 0.44 | 0.38 | 0.33 | 0.62 |
| Marginal bone loss >3 mm | ||||||
| PAN | 0.21 | 0.80 | 0.59 | 0.25 | 0.20 | 0.66 |
| CBCT | 0.28 | 0.29 | 0.53 | 0.67 | 0.51 | 0.62 |
| Cyst | ||||||
| PAN | 0.10 | 0.91 | 0.51 | 0.13 | 0.29 | 0.56 |
| CBCT | – | – | – | 0.26 | 0.30 | 0.22 |
In general, the interobserver reproducibility varied little between PAN and CBCT, although there was a tendency of lower values for CBCT. The percentage accordance and kappa values were highest among observers for tooth angulation (excellent reproducibility) and the presence of a cyst around the crown of the third molar for both methods. In addition, the highest interobserver reproducibility was seen between Observer 1 and Observer 3 for assessing PAN.
Panoramic prediction of pathological findings observed in CBCT
All observers found that mesioangulated and horizontally positioned third molars as assessed in the PAN were strongly associated with the presence of marginal bone loss >3 mm observed in CBCT [odds ratio (OR) 7.0–31.3; p < 0.001]. For each observer assessments, tooth angulation, location of overprojection between the second and third molar and resorption of the second molar seen in the PAN were entered into a multivariate logistic regression analysis with resorption in the distal surface of the second molar observed in CBCT as the outcome (Table 7). Increased periodontal space or cyst at the third molar was the only variable, which was non-significant in the initial analysis and therefore not entered into the multivariate analyses.
Table 7.
Results from the multivariate logistic regression analysis for each observer with resorption yes/no in the CBCT as the outcome variable. Variable in square brackets is the reference group
| Findings in the PAN | p-value | OR | CI |
|---|---|---|---|
| Observer 1 | |||
| Angulation [other] (n = 94) | |||
| Mesioangulated/horizontal (n = 285) | 0.001 | 2.9 | 1.6–5.4 |
| Localization of overprojection [crown] (n = 51) | |||
| Cervical part (n = 212) | <0.001 | 5.8 | 2.3–14.6 |
| Root (n = 116) | <0.001 | 9.7 | 3.8–25.2 |
| Resorption [no] (n = 318) | |||
| Yes (61) | 0.521 | 1.2 | 0.7–2.2 |
| Gender [male] | |||
| Female | 0.476 | 1.2 | 0.8–1.8 |
| Age [ascending] | 0.707 | 1.0 | 1.0–1.0 |
| Observer 2 | |||
| Angulation [other] (n = 106) | |||
| Mesioangulated/horizontal (n = 273) | <0.001 | 8.5 | 2.9–24.5 |
| Localization of overprojection [crown] (n = 53) | |||
| Cervical part (n = 203) | 0.075 | 3.1 | 0.9–11.0 |
| Root (n = 123) | 0.066 | 3.4 | 0.9–12.4 |
| Resorption [no] (n = 316) | |||
| Yes (n = 63) | 0.006 | 2.5 | 1.3–4.8 |
| Gender [male] | |||
| Female | 0.786 | 1.1 | 0.6–1.8 |
| Age [ascending] | 0.297 | 1.0 | 1.0–1.0 |
| Observer 3 | |||
| Angulation [other] (n = 92) | |||
| Mesioangulated/horizontal (n = 287) | <0.001 | 35.5 | 8.2–154.1 |
| Localization of overprojection [crown] (n = 59) | |||
| Cervical part (n = 214) | <0.001 | 18.9 | 4.3–83.1 |
| Root (n = 106) | 0.001 | 13.3 | 2.9–61.0 |
| Resorption [no] (n = 307) | |||
| Yes (n = 72) | 0.001 | 3.2 | 1.6–6.5 |
| Gender [male] | |||
| Female | 0.634 | 0.9 | 0.5–1.5 |
| Age [ascending] | 0.016 | 1.0 | 1.0–1.0 |
| Observer 4 | |||
| Angulation [other] (n = 93) | |||
| Mesioangulated/horizontal (n = 286) | <0.001 | 10.9 | 5.2–23.0 |
| Localization of overprojection [crown] (n = 54) | |||
| Cervical part (n = 215) | <0.001 | 10.8 | 4.1–28.3 |
| Root (n = 110) | <0.001 | 6.6 | 2.4–18.0 |
| Resorption [no] (n = 305) | |||
| Yes (n = 74) | 0.045 | 2.0 | 1.0–4.1 |
| Gender [male] | |||
| Female | 0.390 | 0.8 | 0.5–1.3 |
| Age [ascending] | 0.572 | 1.0 | 1.0–1.0 |
CI, confidence interval; OR, odds ratio; PAN, panoramic image.
For all four observers, a third molar positioned either mesioangulated or horizontally in the PAN predicted resorption in the distal surface of the second molar as observed in CBCT (OR 2.9–35.5; p < 0.001). For three observers, overprojection in the cervical part of the second molar seen in the PAN was highly predictive for resorption observed in CBCT (OR 5.8–18.9; p < 0.001) and so was overprojection located at the root of the second molar (OR 6.6–13.3; p < 0.001). Resorption seen in the PAN was less able to predict resorption observed in CBCT (as also accounted for in Table 1), since the ORs were low for all observers (OR 2.0–3.2; p < 0.045; non-significant for one observer). Resorption was not related to gender and only for one observer increasing age was a significant factor predicting resorption observed in CBCT.
Discussion
No exact protocol for the radiographic examination of mandibular third molars exists,11 but there is rather strong evidence from studies with various designs that performing CBCT routinely to clarify the relationship between the tooth and the mandibular canal may not decrease the number of nerve injuries to the inferior alveolar nerve.6,8–13 Another reason to perform CBCT may be to clarify the presence of pathology in relation to the third molar, which could be decisive for removal, even in lack of patient symptoms. This study has focused on the association between findings in PAN and CBCT in terms of resorption and marginal bone loss in/at the distal surface on the second molar and increased periodontal space around the crown of the third molar. The presence of these pathological findings has been stated as indicative for removal of a third molar by the National Institute for Health and Care Excellence guidelines.2
Comparison between findings in panoramic images and CBCT
In general, there was little agreement between the observers' interpretation of resorption in PAN and CBCT, since much more resorption was observed in CBCT. This tendency was also reported in a previous study where 9 of 97 mandibular third molars were interpreted to resorb the second molar from assessment of the PAN, while 30 second molars were observed with resorption in the CBCT in a consensus between two observers.14 A reason for this may be that in CBCT, there is the possibility to section the volume in all three planes without distortion due to magnification to view small details. On the contrary, in the PAN, it may be difficult to assess the presence of resorption owing to overprojection between the second and third molar and/or because of some degree of magnification and distortion in the PAN.15 Two observers found more severe marginal bone loss in CBCT than in the PAN, while the other two observers found almost the same number of cases with bone loss. It might be speculated that the marginal bone condition may also appear worse in CBCT than that in a PAN, since it is possible to follow the bone level in all three planes in CBCT in contrast to an overprojection of structures as in panoramic imaging. In opposition, the observers mostly agreed on the presence of an increased periodontal space around the crown of the third molar in PAN and CBCT, which may not be surprising, because distally to the crown, there is no overprojection of tooth structures. In the present study, the majority of cases were examined with a Scanora 3D unit with a 6 × 6-cm FOV and voxel resolution of 0.13 and a minor fraction was examined with a NewTom3G unit with a 6 × 8-cm FOV and voxel resolution of 0.3. It could be speculated that smaller details like resorption would be displayed differently by the two units, but in the present study, we believe that this would not change the results significantly.
This study can be considered a Level 3 study in Fryback and Thornbury16 six-tiered hierarchical model of efficacy of a diagnostic imaging method, since it assessed whether the diagnosis was changed when CBCT was interpreted compared with a PAN in addition with the frequency of removals to be, based on the findings in the two modalities, respectively. It was found that between 22 and 27% additional third molars would be removed if a CBCT was the basis for the decision compared with a PAN of the same patient, when the presence of at least one radiographic sign of pathology was the indication for surgery. Moreover, as can be seen from the Tables 1–3, some third molars, scheduled for removal based on the PAN, would avoid treatment if CBCT was the decisive method.
Interobserver reproducibility in panoramic images and CBCT
Besides the differences seen between the two radiographic modalities, the results showed that the interpretation of the three types of pathology (resorption and marginal bone loss in/at the distal surface of the second molar and the presence of a cyst around the crown of the third molar) also differed among observers with both modalities. In two out of five parameters, there were higher percentages of accordance and kappa values among observers for assessing PAN than that for CBCT, although the differences were not large. For angulation and presence of a cyst around the crown of the third molar, the interobserver reproducibility was approximately the same for the two radiographic modalities. In contrast, for marginal bone loss >3 mm at the distal surface of the second molar, it varied among observer pairs whether the interobserver reproducibility was higher for CBCT or PAN.
In the present study, all observers were trained oral radiologists; nevertheless, the kappa statistics showed merely poor to good interobserver reproducibility. Only for assessing angulation of the third molar, there was excellent interobserver reproducibility among all observer pairs. Although we have previously claimed that CBCT may serve as a surrogate “gold standard” method for validation of bony separation between the roots of the third molar and the mandibular canal, since there was an extremely high reproducibility among oral radiologists in assessing this variable,17 this cannot be the case for the variables assessed in the present study. For a method to be a solid gold standard, three criteria have to be fulfilled:18 (1) it should be established by a method that is itself precise, i.e. reproducible; (2) it should reflect the pathoanatomical appearance of the condition in question; and (3) it should be established independently of the diagnostic method under evaluation. Applying these criteria to CBCT for assessment of pathology in relation to the mandibular third molar, CBCT seems to be no more reproducible in assessing pathological findings than panoramic imaging. Second, no study exists that has inspected an extracted second molar with regard to the true state of resorption or which has measured either bone loss at the distal surface of the second molar or around the crown of the third molar during surgery. Since there was no validation for the true state of the pathological findings in our study, we cannot claim that CBCT is more accurate than panoramic imaging. Conclusively, interpretation of CBCT is as observer dependent as interpretation of a PAN, and CBCT is to be seen as an individual diagnostic method in line with other radiographic methods.
Panoramic prediction of pathological findings observed in CBCT
According to guidelines, CBCT should be preceded by a two-dimensional radiographic examination.4,19 If the PAN can predict the findings that will be observed in a CBCT by the same observer, the CBCT examination may not be needed. If a mandibular third molar was positioned either mesioangulated or horizontally as seen in the PAN, there was 7–31 times the risk that there was marginal bone loss >3 mm at the distal surface of the second molar observed in CBCT. It seems logical that marginal bone loss is associated with third molars positioned mesioangulated or horizontally, since the eruption pattern of these teeth has a direction towards the second molar with destruction of bone, in contrast to, for e.g., a vertically positioned or distoangulated third molar. Mesioangulated and horizontally positioned third molars in PAN were also associated with the presence of resorption in the distal surface of the second molar observed in CBCT, since there was between 3 and 36 times the risk that resorption was present if the third molar was positioned in either of these angulations in the PAN. This was also found in other studies including both impacted maxillary and mandibular third molars.14,20,21 In the present study, we also found that third molars overprojecting the second molar at the cervical part (OR = 6–19) or at the root (OR = 7–13) area in the PAN were more likely to be associated with resorption as observed in CBCT. In an older study on periapical images, it was found that resorption mostly occurred in the upper half of the root of the second molar;22 in contrast, another study also on periapical images found that resorption most frequently occurred in the apical part of the root.21 In the present study, tooth angulation was a reproducible parameter among observers; thus, mesioangulated and horizontally positioned mandibular third molars seen in a PAN may be trusted to be related to both marginal bone loss and resorption of the second molar. On the other hand, the interpretation of resorption in the second molar in the PAN had a relatively low association with the presence of resorption observed in CBCT. Therefore, resorption assessed in the PAN is not a reliable indicator for resorption observed in CBCT by the same observer.
Guidelines for removal of mandibular third molars2 state that in case of pathological conditions related to the tooth, removal may be considered. One could speculate that asymptomatic mandibular third molars positioned either mesioangulated or horizontally could be removed based on the PAN. All observers found an increased risk of pathology observed in CBCT for mandibular third molars positioned in either of these angulations and moreover, there was an excellent reproducibility among the observers assessing exactly this parameter.
In conclusion, more third molars are to be removed when the decision for removal is based on radiographic findings of pathology observed in CBCT than if based on a PAN. Interobserver reproducibility of these findings is on the same level in CBCT and PAN. Third molars positioned mesioangulated or horizontally, and those that are overprojecting the second molar in the PAN, are highly predictive for pathology (marginal bone loss and resorption in the second molar) observed in CBCT.
Contributor Information
Louise H Matzen, Email: louise.hauge.matzen@odontologi.au.dk.
Lars Schropp, Email: lars.schropp@dent.au.dk.
Rubens Spin-Neto, Email: rsn@dent.au.dk.
Ann Wenzel, Email: awenzel@dent.au.dk.
References
- 1.Mettes TD, Ghaeminia H, Nienhuijs ME, Perry J, van der Sanden WJ, Plasschaert A. Surgical removal versus retention for the management of asymptomatic impacted wisdom teeth. Cochrane Database Syst Rev 2012; 6: CD003879. doi: https://doi.org/10.1002/14651858.CD003879.pub3 [DOI] [PubMed] [Google Scholar]
- 2.National Institute for Clinical Excellence. Guidance on the extraction of wisdoms teeth. London, UK: NICE; 2000. [Google Scholar]
- 3.Marciani RD. Is there pathology associated with asymptomatic third molars? J Oral Maxillofac Surg 2012; 70: 15–19. doi: https://doi.org/10.1016/j.joms.2012.04.025 [DOI] [PubMed] [Google Scholar]
- 4.Radiation Protection. European guidelines on radiation protection in dental radiology: the safe use radiographs dental practice. European Commission. Vol. 136; 2004. [Google Scholar]
- 5.Matzen LH, Christensen J, Wenzel A. Patient discomfort and retakes in periapical examination of mandibular third molars using digital receptors and film. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2009; 107: 566–72. doi: https://doi.org/10.1016/j.tripleo.2008.10.002 [DOI] [PubMed] [Google Scholar]
- 6.Matzen LH, Petersen LB, Wenzel A. Radiographic methods used before removal of mandibular third molars among randomly selected general dental clinics. Dentomaxillofac Radiol 2016; 45: 20150226. doi: https://doi.org/10.1259/dmfr.20150226 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Matzen LH, Christensen J, Hintze H, Schou S, Wenzel A. Influence of cone beam CT on treatment plan before surgical intervention of mandibular third molars and impact of radiographic factors on deciding on coronectomy versus surgical removal. Dentomaxillofac Radiol 2013; 42: 98870341. doi: https://doi.org/10.1259/dmfr/98870341 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ghaeminia H, Gerlach NL, Hoppenreijs TJ, Kicken M, Dings JP, Borstlap WA, et al. Clinical relevance of cone beam computed tomography in mandibular third molar removal: a multicentre, randomized, controlled trial. J Craniomaxillofac Surg 2015; 43: 2158–67. doi: https://doi.org/10.1016/j.jcms.2015.10.009 [DOI] [PubMed] [Google Scholar]
- 9.Guerrero ME, Botetano R, Beltran J, Horner K, Jacobs R. Can preoperative imaging help to predict postoperative outcome after wisdom tooth removal? A randomized controlled trial using panoramic radiography versus cone-beam CT. Clin Oral Investig 2014; 18: 335–42. doi: https://doi.org/10.1007/s00784-013-0971-x [DOI] [PubMed] [Google Scholar]
- 10.Petersen LB, Vaeth M, Wenzel A. Neurosensoric disturbances after surgical removal of the mandibular third molar based on either panoramic imaging or cone beam CT scanning: a randomized controlled trial (RCT). Dentomaxillofac Radiol 2016; 45: 20150224. doi: https://doi.org/10.1259/dmfr.20150224 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Matzen LH, Wenzel A. Efficacy of cone beam computed tomography for assessment of impacted mandibular third molars: a review based on a hierarchical model of evidence. Dentomaxillofac Radiol 2015; 44: 20140189. doi: https://doi.org/10.1259/dmfr.20140189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Matzen LH, Schou S, Christensen J, Hintze H, Wenzel A. Audit of a 5-year radiographic protocol for assessment of mandibular third molars before surgical intervention. Dentomaxillofac Radiol 2014; 43: 2014172. doi: https://doi.org/10.1259/dmfr.20140172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Suomalainen A, Apajalahti S, Vehmas T, Ventä I. Availability of CBCT and iatrogenic nerve injuries. Acta Odontol Scand 2013; 71: 151–6. doi: https://doi.org/10.3109/00016357.2011.654254 [DOI] [PubMed] [Google Scholar]
- 14.Oenning AC, Neves FS, Alencar PN, Prado RF, Groppo FC, Haiter-Neto F. External root resorption of the second molar associated with third molar impaction: comparison of panoramic radiography and cone beam computed tomography. J Oral Maxillofac Surg 2014; 72: 1444–55. doi: https://doi.org/10.1016/j.joms.2014.03.023 [DOI] [PubMed] [Google Scholar]
- 15.Schropp L, Stavropoulos A, Gotfredsen E, Wenzel A. Calibration of radiographs by a reference metal ball affects preoperative selection of implant size. Clin Oral Investig 2009; 13: 375–81. doi: https://doi.org/10.1007/s00784-009-0257-5 [DOI] [PubMed] [Google Scholar]
- 16.Fryback DG, Thornbury JR. The efficacy of diagnostic imaging. Med Decis Making 1991; 11: 88–94. doi: https://doi.org/10.1177/0272989X9101100203 [DOI] [PubMed] [Google Scholar]
- 17.Matzen LH, Hintze H, Spin-Neto R, Wenzel A. Reproducibility of third molar assessment comparing two CBCT units in a matched pairs design. Dentomaxillofac Radiol 2013; 42: 20130228. doi: https://doi.org/10.1259/dmfr.20130228 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wenzel A, Hintze H. The choice of gold standard for evaluating tests for caries diagnosis. Dentomaxillofac Radiol 1999; 28: 132–6. doi: https://doi.org/10.1259/dmfr.28.3.10740465 [DOI] [PubMed] [Google Scholar]
- 19.SEDENTEXCT Project. Radiation protection no 172: cone beam CT for dental and maxillofacial radiology. Luxembourg: European Commission Directorate-General for Energy; 2012. [Google Scholar]
- 20.Oenning AC, Melo SL, Groppo FC, Haiter-Neto F. Mesial inclination of impacted third molars and its propensity to stimulate external root resorption in second molars—a cone-beam computed tomographic evaluation. J Oral Maxillofac Surg 2015; 73: 379–86. doi: https://doi.org/10.1016/j.joms.2014.10.008 [DOI] [PubMed] [Google Scholar]
- 21.Nemcovsky CE, Libfeld H, Zubery Y. Effect of non-eurpted 3rd molars on distal roots and supporting structures of approximal teeth. A radiographic survey of 202 cases. J Clin Periodontol 1996; 23: 810–15. doi: https://doi.org/10.1111/j.1600-051X.1996.tb00616.x [DOI] [PubMed] [Google Scholar]
- 22.Nitzan D, Keren T, Marmary Y. Does an impacted tooth cause root resorption of the adjacent one? Oral Surg Oral Med Oral Pathol 1981; 51: 221–4. doi: https://doi.org/10.1016/0030-4220(81)90047-5 [DOI] [PubMed] [Google Scholar]