Abstract
BACKGROUND AND OBJECTIVES
To date, no studies have examined vocabulary outcomes of children meeting all 3 components of the Early Hearing Detection and Intervention (EHDI) guidelines (hearing screening by 1 month, diagnosis of hearing loss by 3 months, and intervention by 6 months of age). The primary purpose of the current study was to examine the impact of the current EHDI 1-3-6 policy on vocabulary outcomes across a wide geographic area. A secondary goal was to confirm the impact of other demographic variables previously reported to be related to language outcomes.
METHODS
This was a cross-sectional study of 448 children with bilateral hearing loss between 8 and 39 months of age (mean = 25.3 months, SD = 7.5 months). The children lived in 12 different states and were participating in the National Early Childhood Assessment Project.
RESULTS
The combination of 6 factors in a regression analysis accounted for 41% of the variance in vocabulary outcomes. Vocabulary quotients were significantly higher for children who met the EHDI guidelines, were younger, had no additional disabilities, had mild to moderate hearing loss, had parents who were deaf or hard of hearing, and had mothers with higher levels of education.
CONCLUSIONS
Vocabulary learning may be enhanced with system improvements that increase the number of children meeting the current early identification and intervention guidelines. In addition, intervention efforts need to focus on preventing widening delays with chronological age, assisting mothers with lower levels of education, and incorporating adults who are deaf/hard-of-hearing in the intervention process.
Significant delays in language acquisition are consistently reported for children who are deaf or hard of hearing.1–3 Universal newborn hearing screening (UNHS) and programs based on the Early Hearing Detection and Intervention (EHDI) guidelines were established in the United States to expedite diagnosis and treatment of hearing loss with the hope of mitigating these delays. The Joint Committee on Infant Hearing has recommended universal hearing screening by 1 month of age, diagnosis of hearing loss by 3 months of age, and enrollment in early intervention by 6 months of age.4 These recommendations are commonly referred to as the EHDI 1-3-6 guidelines.
Recent epidemiologic cohort studies conducted in England and Australia have reported better language outcomes for children born in areas of the country or during years in which UNHS had been implemented compared with cohorts of children born before UNHS, 5, 6 with long-term benefits in reading ability also reported.7 Comparing a group screened at birth with those who received a behavioral screen at 9 months of age, researchers in the Netherlands reported better scores on a quality-of-life measure for the UNHS group but no significant group differences in language outcomes.8 This may be because the UNHS group received amplification at the relatively late mean age of 15.7 months. In the United States, researchers have reported more favorable language outcomes for children whose hearing loss was identified earlier, 9 who received hearing aids earlier, 3 or who began intervention services at an earlier age.10, 11 Collectively, the majority of previous research has supported the beneficial effects of early identification and intervention. However, many of these studies were conducted within a restricted geographic area and/or included an age of confirmation of hearing loss within the “early” group that was relatively late by today’s standards, and in all studies, grouping was based on only a single component of the EHDI program (screening, identification, or intervention).
To date, no studies have reported vocabulary or other language outcomes of children meeting all 3 components of the EHDI guidelines. The primary purpose of this study was to examine the impact of the current EHDI 1-3-6 guidelines on vocabulary outcomes across a wide geographic area. A secondary goal was to confirm the impact of other demographic variables (chronological age, additional disabilities, degree of hearing loss, presence of an adult who is deaf or hard of hearing in the home, and mother’s level of education) previously reported to be related to language outcomes.
METHODS
Participants
This was a cross-sectional study of 448 children with bilateral, prelingual hearing loss between 8 and 39 months of age (mean = 25.3 months, SD = 7.5 months). All of the children were participating in the National Early Childhood Assessment Project (NECAP). This project, supported by the Centers for Disease Control and Prevention, is a multistate effort to examine developmental outcomes of young children with hearing loss. Participants lived in 12 different states (see Table 1).
TABLE 1.
N umber of Participants From Each NECAP State
| State of Residence | No. of Participants |
|---|---|
| Arizona | 78 |
| California | 37 |
| Florida | 8 |
| Idaho | 88 |
| Indiana | 41 |
| Maine | 14 |
| North Dakota | 8 |
| Oregon | 1 |
| Texas | 66 |
| Utah | 55 |
| Wisconsin | 32 |
| Wyoming | 20 |
Participants included children with (18%) and without (82%) additional disabilities judged by their parents and/or early interventionists to interfere with speech and/or language development. Cognitive impairment was reported in 58% of those who had additional disabilities (see Table 2). The primary written language used in the home was English (88%) or Spanish (12%). The communication modes used with the children and additional demographic characteristics are summarized in Table 3.
TABLE 2.
Additional Disabilities and Percentage of Occurrence (Based on the 81 Children Who Were Reported to Have One or More Additional Disabilities Thought to Impact Speech and/or Language Development)
| Disability | Percentage of Participants |
|---|---|
| Cognitive | 58 |
| Motor | 44 |
| Vision | 40 |
| Brain damage | 12 |
| Cleft lip and/or palate | 12 |
| Seizures | 12 |
| Cerebral palsy | 11 |
| Sensorimotor integration | 9 |
| Balance | 7 |
| Emotional and/or behavioral | 6 |
| Autism spectrum disorder | 4 |
| Other | 23 |
Percentages total to more than 100% because some participants had more than 1 additional disability.
TABLE 3.
Participant and Family Characteristics
| Characteristic | Percentage of Participants |
|---|---|
| Sex | |
| Male | 53 |
| Female | 47 |
| Ethnicity | |
| Non-Hispanic | 68 |
| Hispanic | 32 |
| Race | |
| White | 87 |
| African American | 5 |
| Asian | 3 |
| Native American | 2 |
| Other | 3 |
| Communication mode used with the child | |
| Primarily spoken language | 74 |
| Spoken language only | 30 |
| Spoken language with occasional use of sign language | 44 |
| Sign language and spoken language | 22 |
| Sign language only | 4 |
| Hearing status of the parent | |
| Both parents hearing | 83 |
| One or both parents deaf and/or hard of hearinga | 17 |
| Mother’s highest educational degree | |
| Less than bachelor’s degree | 71 |
| Less than high school | 13 |
| High school | 38 |
| Vocational | 8 |
| Associate’s | 12 |
| Bachelor’s degree or higher | 29 |
| Bachelor’s | 22 |
| Graduate | 7 |
Of the parents who were deaf or hard of hearing, approximately half used sign language when communicating with their child.
Information regarding hearing loss (onset, degree, and amplification) is presented in Table 4. Preliminary analyses found that independent variable effects were significantly different for children with auditory neuropathy spectrum disorder (ANSD) compared with those without ANSD. The small number of children with ANSD (n = 26) prevented adequately exploring or controlling for these differences, so these children were not included in this study.
TABLE 4.
Characteristics of the Participants’ Hearing Loss
| Characteristic | Percentage of Participants |
|---|---|
| Age of onset of hearing loss | |
| Congenital | 90 |
| Late onset (before 2 y of age) | 6 |
| Unknown | 4 |
| Degree of hearing loss | |
| Mild to moderate | 57 |
| Mild (26–40 dB HL) | 35 |
| Moderate (41–55 dB HL) | 22 |
| Moderately severe to profound | 43 |
| Moderately severe (56–70 dB HL) | 15 |
| Severe (71–90 dB HL) | 8 |
| Profound (>90 dB HL) | 20 |
| Type of amplification | |
| None | 11 |
| Hearing aids | 68 |
| Cochlear implant | 13 |
| Bone conduction hearing aid | 5 |
| Hearing aid and cochlear implant | 3 |
The degree of hearing loss was determined by using the better-ear pure tone average, that is, the average of hearing thresholds at 500, 1000, and 2000 Hz. HL, hearing level.
The participants’ hearing loss was confirmed through diagnostic audiologic testing at a mean age of 4.1 months. All children were enrolled in an early intervention program (mean age of enrollment = 7.0 months). Slightly over half of the participants (58%) met the 1-3-6 guidelines. Of the 258 children who met the 1-3-6 guidelines, 58% also met a stricter 1-2-3 criteria (screening by 1 month of age, identification by 2 months of age, and intervention by 3 months of age).
All of the children participating in the NECAP who met the participant criteria are included in the study. Although it is unknown to what extent the eligible population of each participating intervention program were invited and agreed to participate in the NECAP, the demographics of this sample are consistent with the Gallaudet Research Institute national survey of 37 828 students who are deaf or hard of hearing in terms of sex, ethnicity, primary language at home, degree of hearing loss, type of amplification, and communication mode used by the family.12 Compared with the Gallaudet results, this sample included a smaller percentage of children who were African American (5% vs 16%), a higher percentage of children who had a parent who was deaf and/or hard of hearing (17% vs 9%), and a smaller percentage of children with additional disabilities (18% vs 39%). This is not surprising because, initially, only children without additional disabilities were included in the current study. Additionally, the Gallaudet national survey included students through 12th grade, allowing more time for additional special needs to be identified.
This project was approved by the Institutional Review Board at the University of Colorado Boulder. All families provided written informed consent.
Procedures
The participants’ expressive vocabulary was measured by using the MacArthur-Bates Communicative Development Inventories.13 This norm-referenced assessment has been extensively validated with typically developing children14, 15 as well as those with a variety of different disabilities, 16, 17 including hearing loss.18, 19 Families in which the language of the home was Spanish completed the Spanish version of this instrument.20 Expressive vocabulary ability was selected as the dependent variable because vocabulary size and rate of word learning are important predictors of later language and academic skills.21, 22
In keeping with the administration instructions in the test manual for populations with language delays, the level of the inventory administered (Words and Gestures versus Words and Sentences) was determined on the basis of the interventionists’ and/or caregivers’ estimate of the child’s vocabulary size rather than chronological age.13 For the participants in all but 1 state, the appropriate MacArthur-Bates inventory was given to the family by their early interventionist. In the remaining state, the inventory was mailed to the family’s home. The MacArthur-Bates Communicative Development Inventories list a variety of early-developing words arranged in different semantic categories. The child’s primary caregiver was instructed to mark all of the words that his or her child produced spontaneously in spoken and/or sign language. The form was then reviewed by the child’s early interventionist for completeness and accuracy and sent to the NECAP staff for scoring.
Scoring of all assessments was completed by 1 person and checked by a second person. Disagreements in scoring were corrected by consensus. Total raw scores were calculated by counting the number of words a child produced regardless of modality (spoken or signed). Raw scores were converted to vocabulary age scores by using the procedure described in the test manual. To examine each participant’s expressive vocabulary age score relative to his or her chronological age, vocabulary quotients (VQs) were calculated by dividing the child’s vocabulary age by his or her chronological age and multiplying by 100. A VQ of 100 indicated that a child’s vocabulary age was commensurate with his or her chronological age.
All families and/or their interventionist completed a demographic form, which included information such as the caregivers’ level of education. Audiologic records were used to determine the degree of hearing loss. For data analysis, the participants’ demographic characteristics were categorized as detailed in Table 5.
TABLE 5.
Description of the Coding of the Independent Variables Included in the Regression Model
| Independent Variable | Coding of Variable |
|---|---|
| Chronological age | Treated as a continuous variable in 1 mo increments |
| Disability status | 0 = no additional disabilities 1 = additional disabilities |
| Adherence to the 1-3-6 EHDI guidelines | 0 = does not meet 1 = meets |
| Adult who is deaf or hard of hearing in the home | 0 = not present 1 = present |
| Maternal level of education | 0 = less than a bachelor’s degree 1 = bachelor’s degree and higher |
| Degree of hearing loss | 0 = mild to moderate 1 = moderately severe to profound |
RESULTS
The mean VQ for the 448 children was 74.4 (SD = 20.3). When considering the 367 children with no additional disabilities, the mean VQ was 77.6 (SD = 19.7). For the 81 participants with additional disabilities, the mean was 59.8 (SD = 15.6).
To explore the relationships between vocabulary ability and the demographic variables, Pearson product-moment correlations were computed. As detailed in Table 6, there was no significant relationship between VQ and sex or between VQ and language of the home (Spanish versus English). Significant correlations were obtained between VQs and the remaining demographic variables.
TABLE 6.
Correlations Between VQ and Demographic Variables
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | |
|---|---|---|---|---|---|---|---|---|---|
| 1. VQ | — | — | — | — | — | — | — | — | — |
| 2. Chronological age | −0.50 ** | — | — | — | — | — | — | — | — |
| 3. Disability status | −0.34 ** | 0.05 | — | — | — | — | — | — | — |
| 4. Meets EHDI | 0.27 ** | −0.17 ** | −0.10 * | — | — | — | — | — | — |
| 5. Adult who is deaf or hard of hearing | 0.21 ** | −0.11 * | −0.15 ** | 0.09 | — | — | — | — | — |
| 6. Level of educationa | 0.14 ** | 0.01 | −0.02 | 0.08 | 0.02 | — | — | — | — |
| 7. Degree of hearing lossb | −0.11 * | 0.03 | −0.02 | 0.04 | 0.06 | 0.05 | — | — | — |
| 8. Sex | 0.02 | −0.02 | −0.05 | −0.02 | −0.09 | 0.003 | −0.07 | — | — |
| 9. Language of homec | 0.01 | 0.07 | −0.02 | 0.17 ** | 0.13 ** | 0.17 ** | 0.01 | −0.04 | — |
Level of education: below bachelor’s degree versus bachelor’s degree or higher.
Degree of hearing loss: mild to moderate versus moderately severe to profound.
Language of the home: English versus Spanish.
P < .05, 2-tailed.
P < .01, 2-tailed.
Multiple linear regression analysis was used to identify predictors of variance in the participants’ VQs. Sex and language of the home were initially included in the model to confirm that they were not significantly related to VQs when controlling for other demographic factors. These variables remained nonsignificant and were removed from the final model. The primary independent variable was whether the child met all 3 components of the EHDI 1-3-6 guidelines. Five additional independent variables were entered into the regression equation to explore and control for other factors known from previous research to be related to vocabulary outcomes. The overall model was significant (F6, 441 = 51.0, P < .0005) and explained 41% of the variance in the children’s expressive vocabulary abilities (see Table 7). All 6 predictor variables made a significant, independent contribution to the model.
TABLE 7.
Multiple Regression Predicting MacArthur Expressive VQ
| Participant Characteristics | Standardized Coefficient | Unstandardized Coefficient | t test Value | P |
|---|---|---|---|---|
| Chronological age | −0.44 | −1.19 | −11.80 | <.0005 |
| Disability status | −0.29 | −14.97 | −7.65 | <.0005 |
| Meets EHDI guidelines | 0.16 | 6.42 | 4.19 | <.0005 |
| Mother’s level of education | 0.12 | 5.50 | 3.37 | .001 |
| Degree of loss | −0.12 | −4.79 | −3.19 | .002 |
| Adult who is deaf/hard of hearing | 0.11 | 5.74 | 2.86 | .004 |
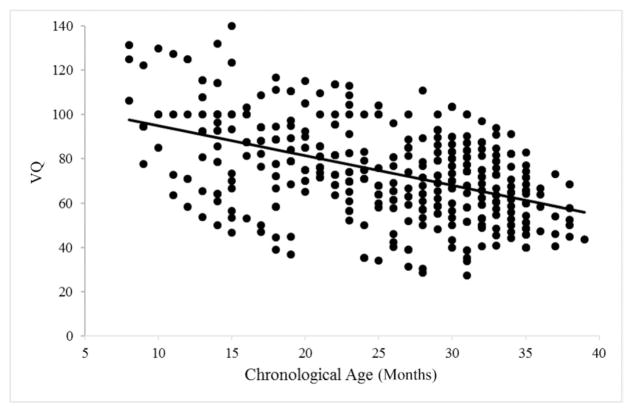
On the basis of the results of the regression, and as shown in Fig 1, mean VQs were shown to decrease as chronological age increased. Although absolute vocabulary size increased with participant age, the gap between chronological and vocabulary age was greater for older children, resulting in lower VQs.
FIGURE 1.
VQs for participants as a function of chronological age.
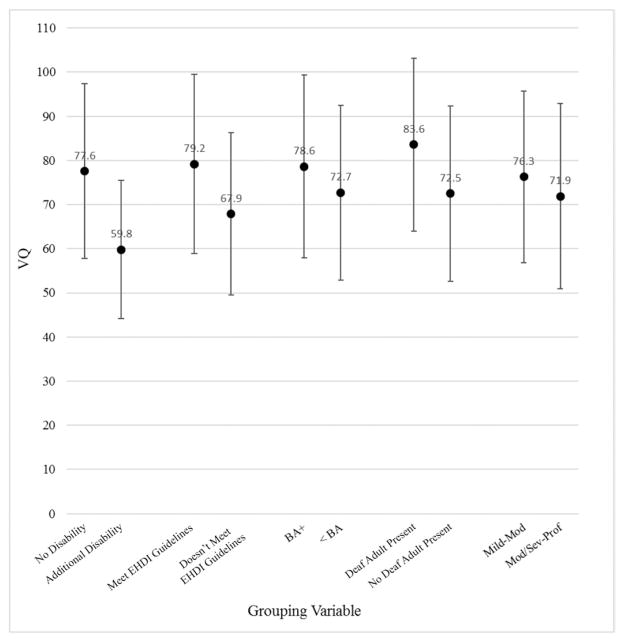
Higher VQs were predicted by the absence of additional disabilities, higher maternal level of education, lesser degrees of hearing loss, and the presence of a parent who was deaf and/or hard of hearing in the home. Even when controlling for these factors, meeting EHDI 1-3-6 guidelines was a significant predictor of vocabulary outcomes. The standardized β weight of .16 indicates that meeting EHDI guidelines had a meaningful impact on vocabulary outcomes in addition to being statistically significant. In comparing the children who met the EHDI guidelines to those who did not, there was a 12-point difference in mean VQ. Mean VQ comparisons across all of the independent predictors are presented in Fig 2.
FIGURE 2.
Mean VQs and SD bars of subgroups on the basis of significant independent variables from the regression analysis (all participants included). BA +, Bachelor’s degree or higher; Mild-Mod, mild to moderate hearing loss; Mod/Sev-Prof, moderately severe to profound hearing loss; < BA, less than a Bachelor’s degree.
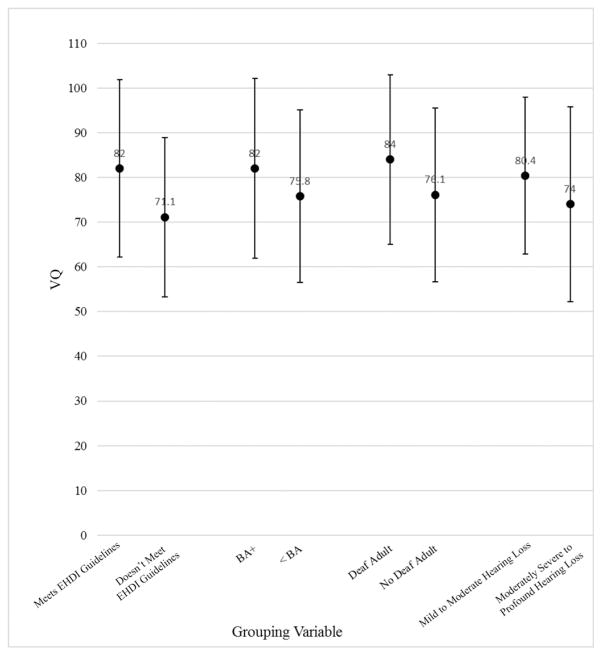
To determine if the impact of meeting EHDI guidelines had a differential effect across various demographic subgroups, 5 interaction terms (meets EHDI × each of the remaining 5 independent variables) were created and evaluated within separate regression models that retained all 6 of the main effect variables. In all cases, the main effects remained significant, and the interaction term was not significant (P > .05). Thus, it appears that the benefits of meeting EHDI guidelines in terms of vocabulary outcomes are consistent across children with a wide range of demographic characteristics. Although there was no significant interaction between EHDI and disability status, to examine vocabulary performance in children with hearing loss without additional disabilities, mean comparisons across the different independent variables are presented for this no-additional-disabilities subgroup in Fig 3.
FIGURE 3.
Mean VQs and SD bars of subgroups on the basis of significant independent variables from the regression analysis (only children without additional disabilities included). BA +, Bachelor’s degree or higher; Mild-Mod, mild to moderate hearing loss; Mod/Sev-Prof, moderately severe to profound hearing loss; < BA, less than a Bachelor’s degree.
To examine possible differences among children who did not meet the EHDI guidelines, participants were divided into 4 groups: (1) meets both the identification and intervention criteria, (2) meets identification by 3 months but not intervention by 6 months, (3) meets intervention by 6 months but not identification by 3 months, and (4) does not meet either criteria. A one-way analysis of variance was conducted with VQ as the dependent variable and EHDI category as the independent and/or grouping variable. The main effect was significant (F3, 437 = 11.26, P < .0005). The results of Scheffe post hoc tests revealed the group that met all EHDI criteria performed significantly better than the other 3 groups (P < .05 across all comparisons). There was no significant difference in any of the post hoc pairwise comparisons among the remaining 3 groups (P = .94 to .99). See Table 8 for means and SDs of the 4 groups.
TABLE 8.
Mean VQs and SDs for 4 EHDI Groups
| EHDI Group | Mean | SD |
|---|---|---|
| Identified by 3 mo; intervention by 6 mo | 79.2 | 20.3 |
| Identified by 3 mo; intervention after 6 mo | 66.7 | 16.7 |
| Identified after 3 mo; intervention by 6 mo | 68.7 | 20.3 |
| Identified after 3 mo; intervention after 6 mo | 68.9 | 18.8 |
DISCUSSION
This large, multistate study is the first to explore the benefits of meeting all 3 components of the EHDI 1-3-6 guidelines on the vocabulary outcomes of children with bilateral hearing loss. Higher VQs were associated with meeting EHDI guidelines even when controlling for a variety of other factors previously reported to impact language development. The lack of significant interactions indicated that the benefits of meeting the guidelines were consistent across a variety of demographic subgroups.
Despite the benefits for children who met the EHDI guidelines, the mean VQ of children without additional disabilities who met EHDI guidelines was 82, considerably less than the expected mean of 100. Particularly concerning is that 37% of this subgroup had VQs <75 (ie, below the 10th percentile). Although this percentage is substantially better than for those who did not meet EHDI guidelines (64% without additional disabilities had VQs <75), it points to the importance of identifying additional factors that may lead to improved vocabulary outcomes.
The percentage of children in the “meets EHDI” group who fell below the 10th percentile is similar to that reported by Vohr et al, 10 who also used the MacArthur-Bates Communicative Development Inventory (43% of their early-identified 18- to 24-montholds fell below the 10th percentile). Several studies have used the Child Development Inventory to measure the language skills of children with hearing loss.8, 9, 23 Direct comparisons with these studies cannot be drawn given that the Child Development Inventory yields substantially higher scores in children who are deaf or hard of hearing than the MacArthur-Bates Communicative Development Inventory (on average by 11 quotient points).24
The variables in this study associated with higher VQs are consistent with previous reports that found better vocabulary and other language outcomes to be related to the absence of additional disabilities, 25 lesser degrees of hearing loss, 3, 10, 26 the presence of a parent who is deaf or hard of hearing, 26, 27 and higher maternal education.28 The association of lower VQs with increasing chronological age complements previous findings that, even when early-identified, children with hearing loss fail to match the vocabulary acquisition trajectory of children who are hearing.10, 29, 30 This suggests that many children with hearing loss fail to keep pace with the exponentially increasing vocabulary growth demonstrated by hearing children as they move beyond 18 months of age (ie, from producing an average of 9 new words per month to 40 words per month).13
Comparing children without additional disabilities who were younger than and older than 24 months of age revealed a 19-point difference in their mean VQs (younger group = 88.9; older group = 69.9). This significant drop is important to consider when describing the vocabulary abilities of children between birth and 3 years of age. Specifically, mean scores may be misleading because they are likely to underrepresent the abilities of younger children and overrepresent the abilities of older children. The low mean VQ of older children is concerning. This mean is well below the 10th percentile, indicating a significant risk for continued, substantial language delays. Awareness of the magnitude of typical growth is critical when setting early intervention goals for young children with hearing loss, and studies exploring strategies to increase the effectiveness of early intervention are needed.
One such strategy that warrants further investigation is how to most effectively include adults who are deaf or hard of hearing in the intervention process. This strategy is supported by the finding that better vocabulary outcomes were apparent in children for whom one or both parents were deaf or hard of hearing. Although this finding may be due in part to a quicker emotional adjustment to having a child with hearing loss and, for those parents who used sign language, to a fluent command of the language, it is also likely that these parents (who included both those who did and did not use sign language) have firsthand knowledge of effective communication strategies that can maximize vocabulary acquisition.
Examining the contribution of parental communication mode to expressive vocabulary acquisition is an additional area that warrants future exploration. Given that families may change their communication approach over time and, if they choose to use sign language, are likely to vary in the extent and fluency with which sign language is used over time, this question is best explored in future research through a longitudinal design.
A limitation of this study is that only a single aspect of language was examined: expressive vocabulary. Future studies should consider additional components of language, including comprehension, syntax, and pragmatics. A second limitation is that disability status was determined by parent and/or interventionist report. It is likely that some children in the “no disability” group actually had an additional disability that was not yet apparent to their parent and/or interventionist. A further limitation is the potential for selection bias. Because of the nature of the data collection process, it was not possible to compare children and/or families who chose to participate in the study with those who declined. However, given the close correspondence between the characteristics of the present sample and the results of the Gallaudet Research Institute survey,12 this sample appears to be representative of the population of children living in the United States who are deaf or hard of hearing.
CONCLUSIONS
The results of this study underscore the importance of current efforts to decrease the age at which children are identified with hearing loss and enrolled in early intervention. Given that, across the participating states, only one-half to two-thirds of children met the EHDI 1-3-6 guidelines, much work still needs to be done to ensure that all children are screened by 1 month of age, diagnosed with hearing loss by 3 months of age, and enrolled in intervention by 6 months of age. This requires a team approach that includes newborn screening personnel, audiologists, early interventionists, and state-based EHDI surveillance programs that monitor and facilitate timely transition from screening to diagnosis to intervention. Pediatricians and other pediatric medical professionals are critical members of this team. Parents look to their child’s primary care providers for advice, and these professionals have the ability to motivate families whose children have not passed a hearing screen to seek timely assessment of their child’s hearing and prompt enrollment in intervention when hearing loss is confirmed.
The independent variables in the current study explained only 41% of the variance in vocabulary outcomes. Given that a substantial proportion of the children performed below the average range, understanding additional factors that influence vocabulary development is critical. Future studies should examine variables such as family involvement, parent–child interaction, compliance with amplification use, intensity of intervention services, and characteristics of early intervention providers and programs. In addition, examining factors that influence vocabulary acquisition rates within a longitudinal design may provide additional information that can support improved outcomes for children who are deaf or hard of hearing.
WHAT’S KNOWN ON THIS SUBJECT
Previous research has supported the beneficial effects, within a restricted geographic area, of a single component of the Early Hearing Detection and Intervention system (ie, hearing screening, early identification, or early intervention).
WHAT THIS STUDY ADDS
This multistate study demonstrates the significant, positive impact on vocabulary outcomes of meeting all 3 criteria of the Early Hearing Detection and Intervention guidelines (screening by 1 month, identification by 3 months, and early intervention by 6 months of age).
Acknowledgments
We express our appreciation to the families, early interventionists, and agencies that participated in this project. We also gratefully acknowledge Dr Craig Mason for his guidance on and review of the statistical methods used in this study.
FUNDING: This study was funded by the Disability Research and Dissemination Center through its grant 5U01DD001007, FAIN U01DD001007 from the Centers for Disease Control and Prevention.
ABBREVIATIONS
- ANSD
auditory neuropathy spectrum disorder
- EHDI
Early Hearing Detection and Intervention
- NECAP
National Early Childhood Assessment Project
- UNHS
universal newborn hearing screening
- VQ
vocabulary quotient
Footnotes
Dr Yoshinaga-Itano conceptualized and designed the study and drafted components of the initial and final manuscript; Dr Sedey participated in the conceptualization and design of the study, oversaw the collection of the data, conducted the statistical analysis, and had a major role in the written manuscript as submitted; Dr Wiggin participated in the review of the literature, assisted in data collection, drafted sections of the initial manuscript, and participated in editing of the final manuscript as submitted; Dr Chung conducted the initial literature review, supplied critical background material for the study, and critically reviewed the manuscript; and all authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
The views in this article are those of the authors and do not necessarily represent the official views of the Disability Research and Dissemination Center or the Centers for Disease Control and Prevention.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
References
- 1.American Speech-Language-Hearing Association (ASHA) [Accessed February 12, 2017];Effects of hearing loss on development. Available at: www.asha.org/public/hearing/effects-of-hearing-loss-on-development.
- 2.Nott P, Cowan R, Brown PM, Wigglesworth G. Early language development in children with profound hearing loss fitted with a device at a young age: part I–the time period taken to acquire first words and first word combinations. Ear Hear. 2009;30(5):526–540. doi: 10.1097/aud.0b013e3181a9ea14. [DOI] [PubMed] [Google Scholar]
- 3.Tomblin JB, Harrison M, Ambrose SE, Walker EA, Oleson JJ, Moeller MP. Language outcomes in young children with mild to severe hearing loss. Ear Hear. 2015;36(suppl 1):76S–91S. doi: 10.1097/AUD.0000000000000219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.American Academy of Pediatrics, Joint Committee on Infant Hearing. Year 2007 position statement: principles and guidelines for early hearing detection and intervention programs. Pediatrics. 2007;120(4):898–921. doi: 10.1542/peds.2007-2333. [DOI] [PubMed] [Google Scholar]
- 5.Wake M, Ching TYC, Wirth K, et al. Population outcomes of three approaches to detection of congenital hearing loss. Pediatrics. 2016;137(1):1–10. doi: 10.1542/peds.2015-1722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kennedy CR, McCann DC, Campbell MJ, et al. Language ability after early detection of permanent childhood hearing impairment. N Engl J Med. 2006;354(20):2131–2141. doi: 10.1056/NEJMoa054915. [DOI] [PubMed] [Google Scholar]
- 7.Pimperton H, Blythe H, Kreppner J, et al. The impact of universal newborn hearing screening on long-term literacy outcomes: a prospective cohort study. Arch Dis Child. 2016;101(1):9–15. doi: 10.1136/archdischild-2014-307516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Korver AMH, Konings S, Dekker FW, et al. DECIBEL Collaborative Study Group. Newborn hearing screening vs later hearing screening and developmental outcomes in children with permanent childhood hearing impairment. JAMA. 2010;304(15):1701–1708. doi: 10.1001/jama.2010.1501. [DOI] [PubMed] [Google Scholar]
- 9.Yoshinaga-Itano C, Sedey AL, Coulter DK, Mehl AL. Language of early- and later-identified children with hearing loss. Pediatrics. 1998;102(5):1161–1171. doi: 10.1542/peds.102.5.1161. [DOI] [PubMed] [Google Scholar]
- 10.Vohr B, Jodoin-Krauzyk J, Tucker R, et al. Expressive vocabulary of children with hearing loss in the first 2 years of life: impact of early intervention. J Perinatol. 2011;31(4):274–280. doi: 10.1038/jp.2010.110. [DOI] [PubMed] [Google Scholar]
- 11.Meinzen-Derr J, Wiley S, Choo DI. Impact of early intervention on expressive and receptive language development among young children with permanent hearing loss. Am Ann Deaf. 2011;155(5):580–591. doi: 10.1353/aad.2011.0010. [DOI] [PubMed] [Google Scholar]
- 12.Gallaudet Research Institute. Regional and National Summary Report of Data From the 2009–2010 Annual Survey of Deaf and Hard of Hearing Children and Youth. Washington, DC: GRI, Gallaudet University; 2011. [Google Scholar]
- 13.Fenson L, Marchman VA, Thal DJ, Dale PS, Reznick JS. MacArthur-Bates Communicative Development Inventories: User’s Guide and Technical Manual. Baltimore, MD: Brookes; 2007. [Google Scholar]
- 14.Bennetts SK, Mensah FK, Westrupp EM, Hackworth NJ, Reilly S. The agreement between parent-reported and directly measured child language and parenting behaviors. Front Psychol. 2016;7:1710. doi: 10.3389/fpsyg.2016.01710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bornstein MH, Haynes OM. Vocabulary competence in early childhood: measurement, latent construct, and predictive validity. Child Dev. 1998;69(3):654–671. [PubMed] [Google Scholar]
- 16.Heilmann J, Ellis Weismer S, Evans J, Hollar C. Utility of the MacArthur-Bates communicative development inventory in identifying language abilities of late-talking and typically developing toddlers. Am J Speech Lang Pathol. 2005;14(1):40–51. doi: 10.1044/1058-0360(2005/006). [DOI] [PubMed] [Google Scholar]
- 17.Thal DJ, O’Hanlon L, Clemmons M, Fralin L. Validity of a parent report measure of vocabulary and syntax for preschool children with language impairment. J Speech Lang Hear Res. 1999;42(2):482–496. doi: 10.1044/jslhr.4202.482. [DOI] [PubMed] [Google Scholar]
- 18.Castellanos I, Pisoni DB, Kronenberger WG, Beer J. Early expressive language skills predict long-term neurocognitive outcomes in cochlear implant users: evidence from the MacArthur–Bates Communicative Development Inventories. Am J Speech Lang Pathol. 2016;25(3):381–392. doi: 10.1044/2016_AJSLP-15-0023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Thal D, Desjardin JL, Eisenberg LS. Validity of the MacArthur-Bates Communicative Development Inventories for measuring language abilities in children with cochlear implants. Am J Speech Lang Pathol. 2007;16(1):54–64. doi: 10.1044/1058-0360(2007/007). [DOI] [PubMed] [Google Scholar]
- 20.Jackson-Maldonado D, Thal D, Fenson L, Marchman VA, Newton T, Conboy BT. MacArthur Inventarios Del Desarrollo de Habilidades Comunicativas (Inventarios): User’s Guide and Technical Manual. Baltimore, MD: Brookes; 2003. [Google Scholar]
- 21.Can DD, Ginsburg-Block M, Golinkoff RM, Hirsh-Pasek K. A long-term predictive validity study: can the CDI Short Form be used to predict language and early literacy skills four years later? J Child Lang. 2013;40(4):821–835. doi: 10.1017/S030500091200030X. [DOI] [PubMed] [Google Scholar]
- 22.Rowe ML, Raudenbush SW, Goldin-Meadow S. The pace of vocabulary growth helps predict later vocabulary skill. Child Dev. 2012;83(2):508–525. doi: 10.1111/j.1467-8624.2011.01710.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tomblin JB, Barker BA, Spencer LJ, Zhang X, Gantz BJ. The effect of age at cochlear implant initial stimulation on expressive language growth in infants and toddlers. J Speech Lang Hear Res. 2005;48(4):853–867. doi: 10.1044/1092-4388(2005/059). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sedey AL, Yoshinaga-Itano C, Wiggin M. Language outcomes across 12 states: strengths, limitations, and predictors of success. Early Hearing Detection and Intervention Conference; April 14, 2014; Jacksonville, FL. [Google Scholar]
- 25.Verhaert N, Willems M, Van Kerschaver E, Desloovere C. Impact of early hearing screening and treatment on language development and education level: evaluation of 6 years of universal newborn hearing screening (ALGO) in Flanders, Belgium. Int J Pediatr Otorhinolaryngol. 2008;72(5):599–608. doi: 10.1016/j.ijporl.2008.01.012. [DOI] [PubMed] [Google Scholar]
- 26.Vohr B, Jodoin-Krauzyk J, Tucker R, Johnson MJ, Topol D, Ahlgren M. Early language outcomes of early-identified infants with permanent hearing loss at 12 to 16 months of age. Pediatrics. 2008;122(3):535–544. doi: 10.1542/peds.2007-2028. [DOI] [PubMed] [Google Scholar]
- 27.Hassanzadeh S. Outcomes of cochlear implantation in deaf children of deaf parents: comparative study. J Laryngol Otol. 2012;126(10):989–994. doi: 10.1017/S0022215112001909. [DOI] [PubMed] [Google Scholar]
- 28.Niparko JK, Tobey EA, Thal DJ, et al. CDaCI Investigative Team. Spoken language development in children following cochlear implantation. JAMA. 2010;303(15):1498–1506. doi: 10.1001/jama.2010.451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Moeller MP, Hoover B, Putman C, et al. Vocalizations of infants with hearing loss compared with infants with normal hearing: part II–transition to words. Ear Hear. 2007;28(5):628–642. doi: 10.1097/AUD.0b013e31812564c9. [DOI] [PubMed] [Google Scholar]
- 30.Moeller MP. Early intervention and language development in children who are deaf and hard of hearing. Pediatrics. 2000;106(3) doi: 10.1542/peds.106.3.e43. Available at: www.pediatrics.org/cgi/content/full/106/3/e43. [DOI] [PubMed] [Google Scholar]