Abstract
Objectives:
To describe marijuana use by Canadians and their perceptions of risk and harm.
Design:
A cross-sectional, structured, online and telephone survey.
Participants:
A nationally representative sample of Canadians.
Methods:
This survey used random probability sampling and targeted respondents based on age, sex, region and their expected response rate.
Results:
Of the 20% of respondents reporting marijuana use in the past 12 months, they were more likely to be younger and male. The most common form of use was smoking, 79%. When asked about harmfulness, 42% and 41% responded that they considered marijuana more harmful than helpful to mental health and to physical health, respectively. When asked about driving under the influence, 71% responded that it was the same as alcohol.
Conclusion:
This research is important for health providers and policy makers seeking to maximize public health through clinical and legislative reform of non-medical use of marijuana.
Abstract
Objectifs:
Décrire l'usage de la marijuana chez les Canadiens ainsi que leurs perceptions des risques et dommages.
Conception:
Sondage transversal structuré, en ligne et téléphonique.
Participants:
Échantillon national représentatif des Canadiens.
Méthodes:
Ce sondage a eu recours à un échantillonnage probabiliste aléatoire et à des répondants ciblés selon l'âge, le sexe, la région et le taux de réponse escompté.
Résultats:
Les 20 % de répondants qui ont indiqué avoir fait usage de la marijuana au cours des 12 derniers mois sont plus susceptibles d'être des jeunes hommes. La forme d'usage la plus courante est par l'inhalation de fumée, 79 %. Au sujet de la nocivité, 42 % et 41 % ont répondu qu'ils considéraient la marijuana plus dommageable que salutaire pour la santé mentale et la santé physique, respectivement. Au sujet de la conduite sous influence, 71 % ont répondu que c'était comme pour l'alcool.
Conclusion:
Cette recherche est importante pour les fournisseurs de services de santé et les responsables de politiques qui veulent maximiser la santé publique par une réforme clinique et législative de l'usage non médical de la marijuana.
Introduction
Marijuana is currently an illicit substance in Canada. However, there have been long standing debates over policy reforms to decriminalize or legalize its use (Fischer et al. 2003, 2009; Hall 2009), and discussion on the merits of shifting from a model of criminalized prohibition to a public health approach. Currently, legal use is restricted to medical purposes, as outlined and governed by the Federal Government and as specified in Access to Cannabis for Medical Purposes Regulations (ACMPR).
Self-reported marijuana use is lower than alcohol or tobacco use. Nationally, 78% report using alcohol, 17% report using tobacco, 10% report using marijuana and 3% report using other substances in 2012 (Health Canada). Although the harms and health risks associated with problematic drinking and smoking tobacco have been widely studied and broadly disseminated, the health risks associated with marijuana use have received less attention (Nutt et al. 2007, 2010). Recent syntheses conclude that the health harms associated with marijuana may include increased risk of psychosis, but the causal relationship is still unclear (Large et al. 2011; Le Bec et al. 2009; Marconi et al. 2016; Minozzi et al. 2010; Moore et al. 2007; Myles et al. 2012, 2016; Semple et al. 2005; Szoke et al. 2014), mania (Gibbs et al. 2015), suicide (Borges et al. 2016; Calabria et al. 2010; Lev-Ran et al. 2014), depression (Lev-Ran et al. 2014; Rey et al. 2004), neurological soft signs (Ruiz-Veguilla et al. 2012), neurocognitive changes, some cancers (Gurney et al. 2015; Huang et al. 2015), stroke (Hackam 2015) and low birth weight complications (English et al. 1997; Gunn et al. 2016).
In 2015, the Federal Government of Canada announced plans to legalize marijuana for recreational use (medical use has been legal across Canada since 2001). In June of 2016, a nine-member Federal Task Force on marijuana legalization and regulation was announced. In November of 2016, the Federal Task Force published “A Framework for the Legalization and Regulation of Cannabis in Canada.” Guided in part by recommendations from this Task Force, legislation (Bills C-45 and C-46) was tabled in Canada's Parliament in April 2017 and is expected to be finalized by July 2018, albeit, individual provinces must then align with and implement this Federal legislation (Canada 2016). With this national policy direction, it is likely that the public discourse surrounding marijuana and health will shift. There is a need for physicians, care providers and policy makers to understand how the Canadian public perceives the harms of marijuana (Canada 2016; CMA 2016), particularly if these perceptions contradict the best available evidence. This will better equip policy makers to develop public health messages, approaches tailored to subpopulations of users and evidence-informed, coordinated policy efforts to reduce the risks of marijuana use. In addition, in the clinical setting, the educator role of physician and other healthcare providers may become increasingly important in helping patients to understand the benefits, risks, health harms and effects of marijuana use. Accordingly, the objective of this study is to describe the attributes of users, patterns of use and perceptions of risk and health harms of marijuana among Canadians.
Methods
Survey design
The survey was designed to ask Canadians about their usage and perceptions of the harms of marijuana compared to other substances (i.e., alcohol and tobacco). Broadly, the questions were developed to understand personal use patterns and the extent to which Canadians perceive marijuana to be harmful to mental and physical health. If respondents indicated a perception of harm, this harm was compared to other common substances. Survey development was informed and refined by expert opinion and a pilot was completed with 10 respondents (McIsaac 1995) to verify the clarity of the questions and 15 respondents as an online pre-test. Participants were selected using a convenience sample and snowball technique. The survey was implemented by a private survey firm (EKOS). The sampling frame and respondent profile was designed to be representative of the Canadian population as well as British Columbia, Alberta, Ontario and Quebec, using the 2011 Canadian Census. Questions were administered in both English and French online and via telephone.
Sampling
Respondents were contacted from a panel of 90,000 members selected using random probability sampling. Participants were contacted online or by telephone (land-line or cell-line). To ensure a representative final sample, members were targeted based on age, sex, region and their expected response rates. The random probability sample avoids the self-selection bias of opt-in convenience samples. It also allows for calculation of confidence intervals and error testing. Online participants were e-mailed up to two times and telephone participants were called up to five times.
Survey questions
The survey included demographic questions as used on the Canadian Census (age category, sex, province of residence, income category and educational attainment). Marijuana use was established using the validated questions from the Canadian Alcohol and Other Drug Use Monitoring Survey (CADUMS) used by Statistics Canada. Mode of use, age of first use and patterns of use were also ascertained. Respondents were asked “What best describes the impact of recreational marijuana on physical health?” with four responses possible: (1) more harmful than helpful, (2) more helpful than harmful, (3) no impact and (4) unsure. The same question was used to assess perceived mental health harm. When respondents indicated that marijuana was harmful, they were then asked if it was more, less or similarly harmful compared to cigarettes, alcohol, prescription drugs and other illicit drugs (cocaine, crack, speed, ecstasy). Respondents were asked whether driving under the influence is (1) as harmful as driving while intoxicated because of alcohol, (2) not as harmful as driving while intoxicated because of alcohol or (3) more harmful than driving while intoxicated because of alcohol. Respondents were asked if they think marijuana is addictive and how its addictiveness compares to cigarettes, alcohol, prescription drugs and other illicit drugs. Lastly, respondents were asked whether they believe the use of marijuana leads to other illicit drug use.
Analysis
Data were weighted to match regional, sex and age proportions nationally. For categorical data, simple proportions were calculated. Multinomial regression analysis was used to understand and control for the relationship between respondents' personal characteristics and their responses. Personal characteristics used in the model were age, sex, highest level of education, income, region and reported marijuana use.
Results
Respondents
Contact was attempted with 11,272 panel members (6,437 online and 4,835 by phone). There were 2,088 completed surveys, 1,788 online and 300 by telephone, resulting in a response rate of 18.5%. Respondents ranged in age from 19 to 95 years old. Responses were weighted to be representative of the Canadian population.
Characteristics of users
Twenty per cent of Canadians reported having used marijuana in the past 12 months, with no difference in the proportions across provinces: 20% in Alberta, 20% in British Columbia, 18% in Ontario, 19% in Quebec. The proportion of respondents reporting marijuana use is higher in males and those younger than 35 years of age (Figure 1). Respondents with an income of less than $50,000 were also more likely to report marijuana use in the last 12 months compared to other higher income categories (p < 0.05).
Figure 1.
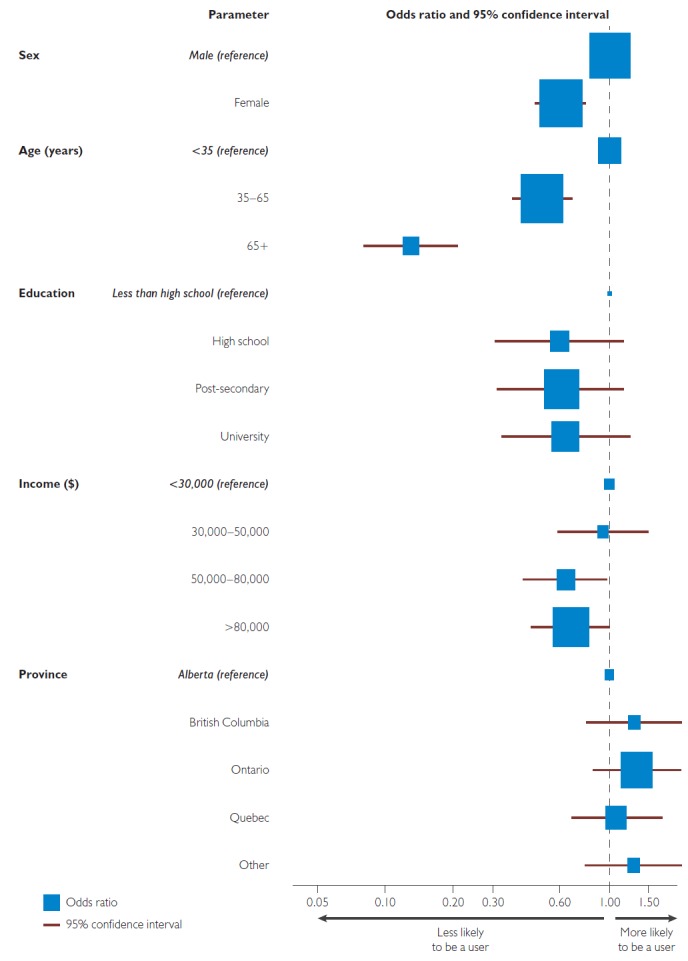
Respondents' personal characteristics and marijuana use in the past 12 months
Note: Variables controlled for in the model: sex, age, education, income and province.
Patterns of use
Those reporting marijuana use reported a median age of first use of 17 (interquartile range = 5) ranging from 9 to 78 years old. Age of first use was less than 16 years old for 48% of respondents and 10% reported age of first use as 25 years or older (Table 1). Forty-three per cent of respondents reported that they used marijuana yearly while 17% reported daily use. The most common method of use was smoking dried marijuana, with 79% of users indicating this as their preferred method of consumption. Other methods included smoking marijuana mixed with tobacco (co-use) (24%), using a vaporizer (25%) or bong (23%); or consuming edibles (31%), oil (13%) and hashish (15%). Differences in methods of use and products used were observed by sex, age and province. Respondents from Quebec were more likely to smoke, use a vaporizer or edibles (p < 0.04) and less likely to roll with tobacco than respondents in the rest of Canada (p < 0.01). Females reported being more likely to use a vaporizer than males (p = 0.01) and respondents less than 35 years of age were more likely to use a bong (p < 0.03).
Table 1.
Practice of marijuana users
| Factors of marijuana use | % |
|---|---|
| Age of first use | |
| <16 | 48 |
| 16–18 | 21 |
| 19–21 | 15 |
| 22–24 | 5 |
| ≥25 | 10 |
| Frequency of use | |
| Daily | 17 |
| Weekly | 18 |
| Monthly | 19 |
| Yearly | 43 |
| Methods of use | |
| Smoked | 79 |
| Rolled with a cigarette | 24 |
| Vaporizer | 25 |
| Bong | 23 |
| Edibles | 31 |
| Oil | 13 |
| Hashish | 15 |
Perception of social effects
Seventy-one per cent responded that driving under the influence of marijuana is similarly harmful as driving under the influence of alcohol. However, 21% responded that they did not believe driving under the influence of marijuana was as harmful as alcohol and 4% responded they were unsure. Females and those 65 years and older were significantly more likely to say that driving under the influence of marijuana is as harmful as alcohol (p < 0.04).
Fifty-eight per cent of Canadians perceive marijuana to be an addictive substance. Broadly, 37% of Canadians think that cigarettes are more addictive than marijuana, 23% think alcohol is more addictive, 44% that prescription drugs are more addictive and 65% think other illicit drugs are more addictive than marijuana (Figure 2a). Those not indicated in the figure responded that they believe marijuana is equally as addictive.
Figure 2.
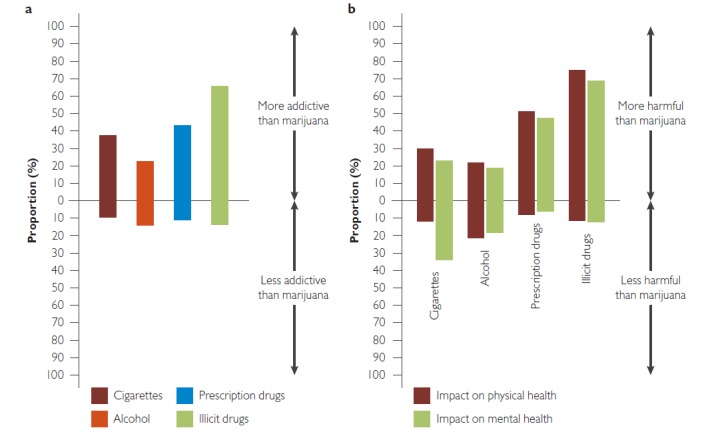
Canadian perceptions of the harm (a) and addictiveness (b) of marijuana
Fifty-five per cent of Canadians believe that consumption of marijuana does not lead to the use of other illicit drugs. Non-users and those over 65 years of age are more likely to perceive that marijuana use leads to the use of other illicit drugs (p < 0.01).
Perceptions of physical and mental harms
Twenty-one per cent responded they were unsure if marijuana caused physical harm. Forty-one per cent responded that marijuana is more harmful than helpful to physical health, 21% responded that it is more helpful than harmful and 14% responded that it had no impact on physical health. Of those that stated that marijuana is physically more harmful than helpful, 22% responded that alcohol is more harmful than marijuana and 75% responded that other illicit drugs are more harmful to physical health (Figure 2b). Respondents reporting that they had not used marijuana in the last 12 months were more likely to say that marijuana is more harmful than helpful to physical health compared to those who have reported marijuana use in the past 12 months (p < 0.01).
Twenty-three per cent responded they were unsure if marijuana caused mental health harm. Forty-two per cent responded that marijuana is more harmful than helpful to mental health, while 22% reported that marijuana is less harmful than helpful and 10% reported that it has no impact. Of those that stated that marijuana is mentally more harmful than helpful, 19% responded that alcohol is more harmful than marijuana and 69% responded that other illicit drugs are more harmful to mental health (Figure 2b). As with physical harms, non-users were more likely to respond that marijuana is more harmful than helpful than marijuana users (p < 0.01). Eighty-one per cent of respondents who said marijuana was harmful to physical health also replied that marijuana was harmful to mental health.
Discussion
This study reports on current marijuana usage in Canada and Canadians' perceptions of risk and harm. Twenty per cent of Canadians report marijuana use in the past 12 months. Similar rates of use are reported across provinces. Forty-eight per cent of marijuana users report their age of first use as less than 16 years of age. A similar per cent perceives that marijuana is more harmful than helpful to physical health (41%) and mental health (42%). Notably, the majority of Canadians perceive driving under the influence of marijuana to be as harmful as driving under the influence of alcohol (71%) and that marijuana is addictive (58%).
It is important for physicians and health providers to be aware that use is occurring in all populations. Although use is higher in younger men, there is use across all age groups, education levels and incomes. This finding challenges the stigma generally associated with people who use illicit substances. Awareness that marijuana use occurs across all demographics should encourage physicians and health providers to assess marijuana consumption as part of a routine visit with all of their patients.
When asked about the harmfulness of marijuana, 42% and 41% responded that they considered it more harmful than helpful to mental health and to physical health, respectively. Given the evidence that marijuana use is associated with harms, such as increased stroke, inflammation of lungs, anxiety, psychosis, depression, mania, low birthweight complications and behavioural issues, there is a clear need to initiate public health campaigns to begin a dialogue with Canadians about the health consequences of use. There may be lessons that can be learned from tobacco and alcohol public health campaigns aimed at denormalizing smoking and reducing problematic drinking, recognizing that health education campaigns must be paired with tight regulation under the goal of reducing the harms of substance use (Kolar et al. 2015). In the context of legalization, a “single substance” approach to prevention is unlikely to be sufficient, but may require efforts to address cannabis co-use. For example, the risks to respiratory health from smoking cannabis mixed with tobacco – the chosen route of administration for many of our survey respondents – and the increased intoxication risks of combining alcohol and cannabis co-use.
Evidence suggests that marijuana use in some individuals may be associated with serious mental illness, such as psychosis, mania, suicide and major depression (Borges et al. 2016; Gibbs et al. 2015; Lev-Ran et al. 2014; Ruiz-Veguilla et al. 2012). Close to 50% of Canadians may be underestimating the mental health harms associated with frequent or heavy marijuana use. Within the current climate of public efforts around “destigmatizing” mental health, legalization may provoke a context for more open conversations between users and their healthcare providers about the possible role of marijuana in their mental health.
Approximately 50% of users reported their age of first use as less than 16 years of age. This is particularly concerning given the growing evidence that suggests the neurocognitive and developmental effects of marijuana use for those under 25 years of age. Based on the developing neuroscience, the Canadian Centre on Substance Abuse recommended avoidance below the age of 24 or 25 years and the Canadian Medical Association set the age restriction at 21 years of age. The recommendation of the Task Force is that the minimum age of purchase be 18 years old, although provinces will set their own age limits and may or may not choose to harmonize age restrictions with alcohol and tobacco. There is a push towards older age restrictions to reduce youth access, albeit tempered with the sense that youth may continue to access through a parallel illegal market. While the risk of a parallel illegal market is an important consideration in formulating regulation, it should not deter from setting policy to improve public health.
Of note, respondents in our survey were more likely than respondents in previous surveys to indicate use of marijuana in the last 12 months, 20% compared to 11% in the 2013 CADUMS, completed by Statistics Canada. These differences may be real or may be because of differences in survey methods. CADUMS conducted telephone interviews with 1,008 respondents aged 15 and older per province, that is, 10,080 interviews annually. The response rate was 39.8%. The high number of interviews and response rates is important since they used random sampling rather than probability sampling. As in this study, results were weighted to match the Canadian Census. Differences in marijuana use may be due to Canadians being more willing to self-report marijuana use on a non-governmental survey or because the survey was online. Equally, it may be due to a higher willingness to identify as a marijuana user knowing that it is likely to be legalized. Regardless of the reason, this survey indicates that the self-report use of marijuana is higher than has been previously shown.
Despite attempts to achieve representativeness in the sample, through probability sampling and weighting, we have only weighted the sample using a limited number of variables. Moreover, the low response rate may introduce a non-response bias that could influence our assessment of use and perceptions of risk and harm, although probability sampling was undertaken to mitigate this bias. This survey relies on self-report which is known to underestimate substance use. Thus, our estimates of use may be low and we may have misclassification bias between users and non-users. However, given that our reported rates of use are higher than other national estimates, we anticipate the impact of under-reporting to be lower than in other data sources. Lastly, this work was carried out at a specific point in time which may not reflect the steady state rates and patterns of use that may eventually occur following legalization.
Conclusion
In conclusion, this study provides a better understanding of public use and perceptions of marijuana risks and harms. The findings of this survey are informative content to developing public policy. These results will likely change with time, and repeating this survey pursuant to legalization will be particularly informative as the prevalence and frequency of use will shape public opinion. Moreover, given the widespread acceptability of use and the correspondingly high proportion who believe that marijuana is neither harmful nor addictive, this will challenge health messaging and will require serious consideration in the regulatory regime which accompanies legalization.
Contributor Information
Eldon Spackman, O'Brien Institute for Public Health, Health Technology Assessment Unit, Department of Community Health Sciences, University of Calgary, Calgary, AB.
Rebecca Haines-Saah, O'Brien Institute for Public Health, Department of Community Health Sciences, University of Calgary, Calgary, AB.
Vishva M. Danthurebandara, O'Brien Institute for Public Health, Health Technology Assessment Unit, Department of Community Health Sciences, University of Calgary, Calgary, AB.
Laura E. Dowsett, O'Brien Institute for Public Health, Health Technology Assessment Unit, Department of Community Health Sciences, University of Calgary, Calgary, AB.
Tom Noseworthy, O'Brien Institute for Public Health, Health Technology Assessment Unit, Department of Community Health Sciences, University of Calgary, Calgary, AB.
Fiona M. Clement, Department Community Health Sciences, O'Brien Institute for Public Health, Cumming School of Medicine, University of Calgary, Calgary, AB.
References
- Borges G., Bagge C.L., Orozco R. 2016. “A Literature Review and Meta-Analyses of Cannabis use and Suicidality.” Journal of Affective Disorders 195: 63–74. [DOI] [PubMed] [Google Scholar]
- Calabria B., Degenhardt L., Hall W., Lynskey M. 2010. “Does Cannabis Use Increase the Risk of Death? Systematic Review of Epidemiological Evidence on Adverse Effects of Cannabis Use.” Drug and Alcohol Review 29(3): 318–30. 10.1111/j.1465-3362.2009.00149.x. [DOI] [PubMed] [Google Scholar]
- Canada G.O. 2016. A Framework for the Legalization and Regulation of Cannabis in Canada. Retrieved June 8, 2017. <http://healthycanadians.gc.ca/task-force-marijuana-groupe-etude/framework-cadre/index-eng.php>.
- Canadian Medical Association (CMA). 2016. (Sept. 9). CMA Statement – Legalization of Marijuana. Retrieved July 25, 2017. <https://www.cma.ca/Assets/assets-library/document/en/advocacy/submissions/2016-sep-09-cma-statement-legalization-of-marijuana-e.pdf>.
- English D.R., Hulse G.K., Milne E., Holman C.D., Bower C.I. 1997. “Maternal Cannabis Use and Birth Weight: A Meta-Analysis.” Addiction 92(11): 1553–60. [PubMed] [Google Scholar]
- Fischer B., Ala-Leppilampi K., Single E., Robins A. 2003. “Cannabis Law Reform in Canada: Is the ‘Saga of Promise, Hesitation and Retreat' Coming to an End?” Canadian Journal of Criminology and Criminal Justice 45(3): 265–98. [Google Scholar]
- Fischer B., Rehm J., Hall W. 2009. “Cannabis Use in Canada: The Need for a ‘Public Health’ Approach.” Canadian Journal of Public Health/Revue Canadienne de Sante Publique 100(2): 101–03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gibbs M., Winsper C., Marwaha S., Gilbert E., Broome M., Singh S.P. 2015. “Cannabis Use and Mania Symptoms: A Systematic Review and Meta-Analysis.” Journal of Affective Disorders 171: 39–47. [DOI] [PubMed] [Google Scholar]
- Gunn J.K., Rosales C.B., Center K.E., Nunez A., Gibson S.J., Christ C., Ehiri J.E. 2016. “Prenatal Exposure to Cannabis and Maternal and Child Health Outcomes: A Systematic Review and Meta-Analysis.” BMJ Open 6(4): e009986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gurney J., Shaw C., Stanley J., Signal V., Sarfati D. 2015. “Cannabis Exposure and Risk of Testicular Cancer: A Systematic Review and Meta-Analysis.” BMC Cancer 15: 897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hackam D.G. 2015. “Cannabis and Stroke.” Stroke 46(3): 852–56. [DOI] [PubMed] [Google Scholar]
- Hall W. 2009. “The Adverse Health Effects of Cannabis Use: What are They, and What are their Implications for Policy?” International Journal of Drug Policy 20(6): 458–66. [DOI] [PubMed] [Google Scholar]
- Health Canada. Canadian Alcohol and Drug Use Monitoring Survey (CADUMS). Retrieved June 18, 2017. <http://www.hc-sc.gc.ca/hc-ps/drugs-drogues/cadums-esccad-eng.php>.
- Huang Y.H., Zhang Z.F., Tashkin D.P., Feng B., Straif K., Hashibe M. 2015. “An Epidemiologic Review of Marijuana and Cancer: An Update.” Cancer Epidemiology Biomarkers and Prevention 24(1): 15–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kolar K., Hyshka E., Jesseman R., Lucas; P., Robert Solomon LLB L., 2015. “A Common Public Health-Oriented Policy Framework for Cannabis, Alcohol and Tobacco in Canada?”’ Canadian Journal of Public Health 106(8): E474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Large M., Sharma S., Compton M.T., Slade T., Nielssen O. 2011. “Cannabis Use and Earlier Onset of Psychosis: A Systematic Meta-Analysis.” Archives of General Psychiatry 68(6): 555–61. [DOI] [PubMed] [Google Scholar]
- Le Bec P.Y., Fatseas M., Denis C., Lavie E., Auriacombe M. 2009. “Cannabis and Psychosis: Search of a Causal Link Through a Critical and Systematic Review.” Encephale 35(4): 377–85. [DOI] [PubMed] [Google Scholar]
- Lev-Ran S., Roerecke M., Le F.B., George T.P., McKenzie K., Rehm J. 2014. “The Association between Cannabis Use and Depression: A Systematic Review and Meta-Analysis of Longitudinal Studies.” Psychological Medicine 44(4): 797–810. [DOI] [PubMed] [Google Scholar]
- Marconi A., Di F.M., Lewis C.M., Murray R.M., Vassos E. 2016. “Meta-Analysis of the Association Between the Level of Cannabis Use and Risk of Psychosis.” Schizophrenia Bulletin 42(5): 1262–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McIsaac S. 1995. Handbook in Research and Evaluation. San Diego, CA: Edits Publishers. [Google Scholar]
- Minozzi S., Davoli M., Bargagli A.M., Amato L., Vecchi S., Perucci C.A. 2010. “An Overview of Systematic Reviews on Cannabis and Psychosis: Discussing Apparently Conflicting Results.” Drug & Alcohol Review 29(3): 304–17. [DOI] [PubMed] [Google Scholar]
- Moore T.H., Zammit S., Lingford-Hughes A., Barnes T.R., Jones P.B., Burke M., Lewis G. 2007. “Cannabis Use and Risk of Psychotic or Affective Mental Health Outcomes: A Systematic Review.” Lancet 370(9584): 319–28. [DOI] [PubMed] [Google Scholar]
- Myles H., Myles N., Large M. 2016. “Cannabis Use in First Episode Psychosis: Meta-Analysis of Prevalence, and the Time Course of Initiation and Continued Use.” Australian & New Zealand Journal of Psychiatry 50(3): 208–19. [DOI] [PubMed] [Google Scholar]
- Myles N., Newall H., Nielssen O., Large M. 2012. “The Association between Cannabis Use and Earlier Age at Onset of Schizophrenia and Other Psychoses: Meta-Analysis of Possible Confounding Factors.” Current Pharmaceutical Design 18(32): 5055–69. [DOI] [PubMed] [Google Scholar]
- Nutt D.J., King L.A., Phillips L.D. 2010. “Drug Harms in the UK: A Multicriteria Decision Analysis.” Lancet 376(9752): 1558–65. [DOI] [PubMed] [Google Scholar]
- Nutt D., King L.A., Saulsbury W., Blakemore C. 2007. “Development of a Rational Scale to Assess the Harm of Drugs of Potential Misuse.” Lancet 369(9566): 1047–53. [DOI] [PubMed] [Google Scholar]
- Rey J.M., Martin A., Krabman P. 2004. “Is the Party Over? Cannabis and Juvenile Psychiatric Disorder: The Past 10 Years.” Journal of the American Academy of Child & Adolescent Psychiatry 43(10): 1194–205. [DOI] [PubMed] [Google Scholar]
- Ruiz-Veguilla M., Callado L.F., Ferrin M. 2012. “Neurological Soft Signs in Patients with Psychosis and Cannabis Abuse: A Systematic Review and Meta-Analysis of Paradox.” Current Pharmaceutical Design 18(32): 5156–64. [DOI] [PubMed] [Google Scholar]
- Semple D.M., McIntosh A.M., Lawrie S.M. 2005. “Cannabis as a Risk Factor for Psychosis: Systematic Review.” Journal of Psychopharmacology 19(2): 187–94. [DOI] [PubMed] [Google Scholar]
- Szoke A., Galliot A.M., Richard J.R., Ferchiou A., Baudin G., Leboyer M., Schurhoff F. 2014. “Association between Cannabis Use and Schizotypal Dimensions–A Meta-Analysis of Cross-Sectional Studies.” Psychiatry Research 219(1): 58–66. [DOI] [PubMed] [Google Scholar]


