Abstract
Healthcare systems must be responsive to the healthcare needs of the populations they serve. However, typically neither health services nor health workforce planning account for populations' needs for care, resulting in substantial and unnecessary unmet needs. These are further exacerbated during unexpected surges in need, such as pandemics or natural disasters. To illustrate the potential of improved methods to help planning for these types of events, we applied an integrated, needs-based approach to health service and workforce planning in the context of a potential influenza pandemic at the provincial level in Canada. This application provides evidence on the province's capacity to respond to surges in need for healthcare and identifies specific services which may be in short supply in such scenarios. This type of approach can be implemented by planners to address a variety of health issues in different contexts.
Abstract
Les systèmes de santé doivent se montrer réactifs aux besoins de santé des populations qu'ils desservent. Cependant, habituellement ni les services de santé ni la planification de la main-d'œuvre en santé tiennent compte des besoins des populations en termes de soins, ce qui donne lieu à d'importants besoins inutilement non comblés. La situation s'exacerbe davantage quand il y a une intensification imprévue en matière de soins, tels que les pandémies ou les désastres naturels. Afin d'illustrer le potentiel des méthodes améliorées pour faire face à ce type de situation, nous avons appliqué une démarche intégrée axée sur les soins aux services de santé et à la planification de la main-d'œuvre en santé dans le contexte d'une éventuelle pandémie d'influenza au niveau provincial, au Canada. Cette application permet de dégager des données sur la capacité de la province à réagir à l'intensification des besoins en santé et permet de repérer les services précis qui pourraient présenter une carence dans ce type de scénario. Ce genre de démarche peut être utilisé par les planificateurs pour traiter une variété d'enjeux de santé dans divers contextes.
Introduction
Because the effectiveness of healthcare services is directly contingent on the health human resources (HHR) who provide them, HHR planning must be integrated with health service planning. Further, in order for healthcare systems to effectively address the needs of the populations they serve, the planned levels of services and, by extension, the HHR to provide them, must be derived from the needs for care in the population. In practice, however, HHR planning is typically conducted in isolation from health service planning, and population health needs are seldom accounted for by either process (Birch 1985; Birch et al. 2007; Eyles et al. 1993; Mejía and Fülöp 1978; Ono et al. 2013). The results of this failure in planning are apparent in healthcare systems worldwide where healthcare needs frequently go unmet because the services required to address them and/or the HHR necessary to deliver those services have not been planned in accordance with needs for care in the population. These failures have even more unfortunate consequences during surges in need such as natural disasters or pandemics.
In recent years, progress has been made in addressing these planning failures. More comprehensive planning approaches in which (a) estimates of the required number and type of HHR are calculated as a function of estimates of the number and type of healthcare services required and (b) estimates of the number and type of healthcare services required are calculated as a function of measures of population health – have been applied to a range of health conditions and planning contexts. Examples include:
caring for older adults in Canada (Tomblin Murphy et al. 2013b) and New Zealand (New Zealand Department of Health 2011a);
dental services for schoolchildren in Thailand (Tianviwat et al. 2009) and for adults over age 65 in England (Gallagher et al. 2013);
diabetes care in Australia (Segal and Leach 2011) and New Zealand (New Zealand Department of Health 2011b); and
maternal health services in Guinea (Jansen et al. 2014).
Several studies have applied similarly comprehensive approaches to plan for HIV/AIDS services in various countries. These include analyses in, for example, Chad and Tanzania (Kurowski et al. 2004, 2007), sub-Saharan and low- and middle-income non-sub-Saharan Africa (Bärnighausen et al. 2007), Zimbabwe (Hallett et al. 2011), Zambia (Goma et al. 2014) and South Africa (Bärnighausen et al. 2007, 2016).
Such approaches represent important advances to more traditional planning methods which typically (1) do not consider population health needs, (2) consider population health needs but only one type of HHR such as physicians or (3) consider population health needs but do not derive HHR requirements from service requirements. Many studies have used these more common types of approaches over the past few decades, such as those by Crettenden et al. (2014), Tomblin Murphy et al. (2014) and Bruckner et al. (2011), respectively.
Building on this evidence base, the objectives of this paper are to:
demonstrate the application of an integrated, needs-based approach to healthcare service and HHR planning in the context of an influenza pandemic; and
demonstrate methodological advancements in the practical application of such an approach.
This research was conducted as part of a study funded by the Canadian Institutes of Health Research and the Nova Scotia Health Research Foundation in two Canadian jurisdictions. For the purposes of this paper, only the findings from one jurisdiction are reported.
Methods
The methods build on an integrated needs-based planning approach that was pilot-tested by Tomblin Murphy and colleagues (2013a) in the context of pandemic planning in one District Health Authority (DHA) in Nova Scotia, Canada. Under this approach, two quantities are estimated and compared under different scenarios: (1) how many people in a particular population would be expected to need a particular healthcare service (requirements) and (2) how many people can be provided with that service by the existing health workforce (supply). Having identified pandemic influenza as the particular condition to be addressed, the process to estimate service needs requires knowledge of the size of the population, the expected incidence and severity of influenza within that population (i.e., levels and distribution of health), the range of healthcare services required for persons in each level of health and the frequency with which each service is required by persons in different levels of severity. Estimating the supply of services requires information on the supply of licensed HHR of different professions, their levels of direct care participation and activity, the prevalence of the competencies to provide each of the services under consideration, and the rates at which they can be expected to perform those services (Tomblin Murphy et al. 2013a, 2013b). The relationships between these various planning parameters are shown in Figure 1, which illustrates the study's underlying analytical framework.
Figure 1.
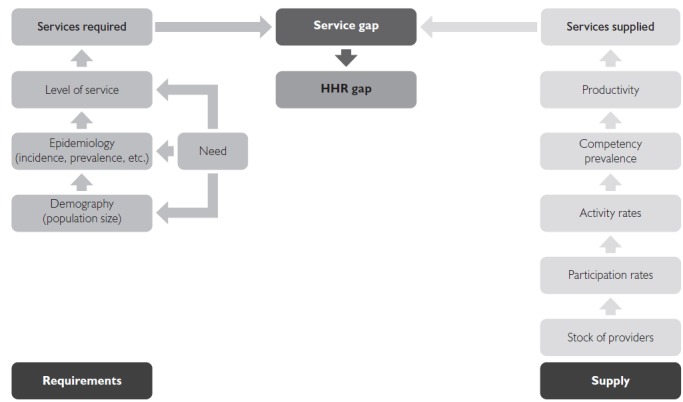
Integrated needs-based HHR planning framework (Tomblin Murphy et al. 2013b)
HHR = health human resources.
In the present study, the approach was expanded to the entire province of Nova Scotia (population 943,000). The range of potentially required healthcare services identified in the pilot study served as the first “draft” for this study, and was specific to clinical services and did not include other important but non-clinical services that would be required during a pandemic, such as mass media communications. These were then reviewed and updated by an infectious disease specialist before being validated by a Steering Committee made up of local healthcare policy makers and clinicians available at (Appendix 1).
Because the timing and nature of pandemics are uncertain, this approach is designed to accommodate different assumptions – including age-specific incidence or “attack” rates and distributions of severity – so that planners can assess system capacity to respond to a range of potential pandemic scenarios. To illustrate this capacity, historical data from past influenza pandemics in 2009 (Nova Scotia Department of Health 2010; Smetanin et al. 2010) and 1918 (Pike 2011) were applied to the most recent data on Nova Scotia's population and health workforce. Although Nova Scotia-specific data on the 2009 pandemic are available, the data on the other pandemic are global in scope. These data are summarized in Appendix 2.
The proportions of people who could be expected to require each service were estimated at each of four levels of severity: those without influenza, those with influenza but only mildly ill (i.e., who may need some out-patient care), those acutely ill with influenza (i.e., requiring in-patient care) and those critically ill with influenza (i.e., requiring intensive in-patient care). Estimates reported by Tomblin Murphy et al. (2013a), were adjusted for the current application by an infectious disease specialist on the research team. Importantly, these estimates were based on the question of what services these individuals would require given their health status as opposed to, for example, what services may already be available given specific resource constraints. These measures are referred to as “level of service” estimates.
Data on population size and demographics (Statistics Canada 2015), when combined with the data on pandemic incidence and severity, yielded estimates of the number of people in the province who would have influenza with different degrees of severity. These were multiplied by severity-specific level of service values to produce estimates of the number of people in the province likely to require each service in the event of an influenza pandemic with a particular epidemiological profile.
Data to estimate the supply of each service were obtained from multiple sources. For regulated professions, headcounts of those holding licenses to practice were provided by their respective regulatory colleges, whereas headcounts for unregulated professions were taken from administrative records of each of the province's DHAs. Participation levels for each regulated profession were calculated by dividing the numbers used by DHAs by the numbers holding licences to practice in the province. In the absence of a reliable source of data on participation levels among non-regulated professions in the province, their supplies were modelled as if their participation level was 100%. Profession-specific activity levels were estimated based on data from administrative records, using 40 hours worked per week as a benchmark (e.g., someone who worked an average of 36 hours per week would have an activity level of 90%).
An attempt was made to estimate the final two parameters of the analytical framework – competency prevalence and productivity – using survey methods similar to those described in the pilot study (Tomblin Murphy et al. 2013a). The survey asked respondents to self-assess their competency to provide each pandemic service on a five-point scale with the following values: 1 = I have never been trained to provide this service; 2 = I have been trained to provide this service but do not currently feel competent to provide it; 3 = I could provide this service with some supervision; 4 = I feel competent to provide this service; and 5 = I feel competent to provide this service and could train others to provide it. These response categories were developed to allow planners to consider the feasibility of, among other strategies, “skilling up” HHR currently working in administrative roles to provide some direct patient care in the event of a pandemic. Because of a low (10%) response rate, alternative methods of estimating these parameters were developed.
To estimate the prevalence of the competencies required to deliver each service in the province, the list of potentially required services was compared with descriptions of the core competencies of each profession specified by their respective regulatory colleges. Based on this comparison, a “map” showing whether each service was deemed to be within the competencies expected of each profession – and if so, at what level of training, from entry-to-practice through various additional certifications – was developed. This map was cross-referenced with relevant provincial legislative and regulatory frameworks. An initial draft map was revised based according to feedback from professional colleges (Appendix 3). Once complete, the map identified which of the required services could, under existing professional regulatory structures, be performed by licensed members of each profession in the province.
To estimate productivity at the team level, multi-professional panels were convened with participants from 12 different health professions. Separate panels were convened to discuss influenza care at the different levels of severity identified above. These panels were presented with the list of potentially needed services for those levels of illness and asked to answer the following questions:
What team configurations would be appropriate to provide this “basket” of services to people with influenza of this severity?
How many patients could such a team, providing quality care, be reasonably expected to care for, over a single eight-hour shift?
The panels collectively identified 30 different potential team configurations across the four levels of patient severity. These ranged in complexity from solo physician or nurse practitioner (NP) practices vaccinating 100 healthy patients per shift to, for example, a team of four care assistants, one dietitian, three licensed practical nurses (LPNs), one physician, one NP, one pharmacist, one physiotherapist, two physiotherapy assistants, two registered nurses (RNs) and one respiratory therapist (RT) caring for 25 acutely ill patients per shift. In several configurations pertaining to vaccinating healthy people, it was noted that an additional team member, with some level of healthcare training but not necessarily pertaining to influenza, could administer screening questionnaires or monitor patients following their vaccinations. These could include professionals such as occupational therapists or dental hygienists who might otherwise not play a major role in an influenza pandemic response.
Using these data, analyses were performed to identify potential shortages at two levels: specific types of HHR and specific services. In the latter case, the information from the competency maps, in combination with the other measures of the existing supply of each type of HHR in each jurisdiction, allowed for the estimation of the numbers of full-time equivalent (FTE) personnel available and competent to provide each potentially required service. These were compared with the estimates of the number of people likely to require each service in the event of a pandemic, allowing for the identification of the services required most often relative to the availability of personnel to provide them. In this way, specific services for which the capacity to provide is the most “scarce” were identified. Lacking adequate data to allow for service-specific estimates of productivity (e.g., the average amount of time required to perform each service per patient), it was not possible to calculate the number of times each service could be provided and thus estimate service-specific gaps.
To identify potential shortages of specific types of HHR (as opposed to specific services) in the event of a future influenza pandemic, each of the suggested teams' productivity was applied to the numbers of patients expected to have each level of illness to estimate FTE numbers of each type of HHR required under that configuration. These estimates were then compared with existing FTE supplies in the province to identify gaps.
The study's methods and findings were discussed with provincial healthcare stakeholders at a day-long workshop with a view toward facilitating its broader application to health service and HHR planning in the province. These stakeholders included members of the Steering Committee as well as representatives of the DHAs, regulatory colleges and professional associations.
Results
There are many possible combinations of the different teams suggested by the panels. The results of the gap analysis for three such configurations based on the profiles of the 1918 and 2009 influenza pandemics in terms of the overall attack rate and distribution of severity are provided in Figure 2.
Figure 2.
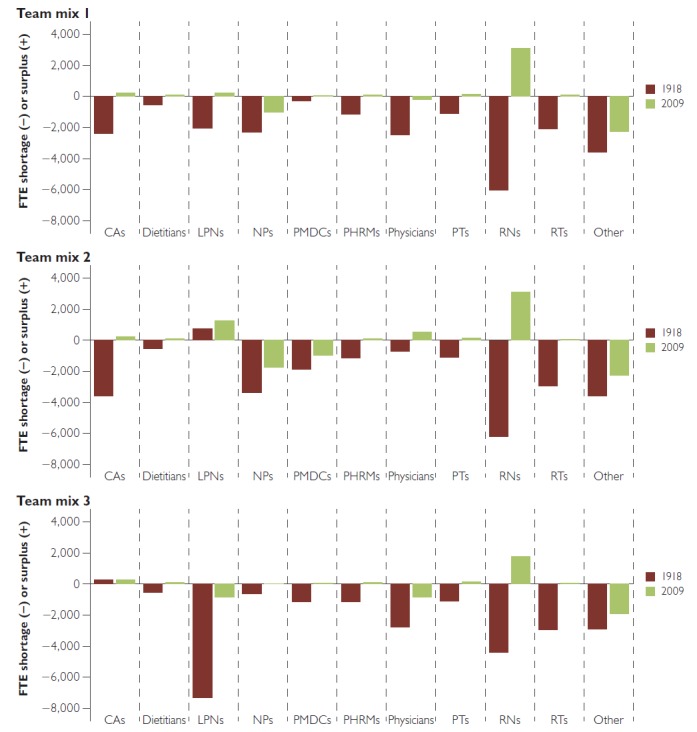
Simulated Nova Scotia HHR gaps based on 1918 and 2009 pandemic profiles
CAs = care aides; HHR = health human resources; LPNs = licensed practical nurses; NPs = nurse practitioners; PHRMs = pharmacists; PMDCs = paramedics; PTs = physiotherapists; RNs = registered nurses; RTs = respiratory therapists.
In each of these scenarios, there are enough of some types of HHR but not enough of others to respond to the simulated pandemic. The simulated shortages are more prevalent across types of HHR and larger in magnitude under the more severe pandemic, to the point that the sizes of the simulated shortages are greater than the entire existing provincial supplies of some of these professions.
The results shown in Figure 2 are based on the assumption that current levels of participation in direct patient care and hours worked would apply in the event of another influenza pandemic. These levels may be different during a pandemic. As an example of such a scenario, the same analysis was undertaken using two different assumptions: all those licensed to provide direct patient care do so, and all those providing direct patient care work full-time (an “all hands on deck” scenario). In this scenario, Nova Scotia would have enough FTEs of most types of HHR to respond to a pandemic similar to that of 2009, but not enough to respond to one similar to the 1918 pandemic.
Results of service-specific analysis for the scenarios based on the 1918 and 2009 pandemic profiles are provided in Table 1, which shows estimates of: (1) the 10 services that, in each scenario, would be required most in the population, (2) the numbers of FTE providers who are competent to provide these services, and (3) based on these two values, the number of times each competent FTE would be required to provide each service over the four-week peak of the pandemic.
Table 1.
Most-needed services in Nova Scotia under simulated influenza pandemic by scenario (1918 vs. 2009 pandemic profiles)
| Service | Number of patients requiring | Number of FTEs competent | Required productivity (services/FTE/month) | ||
|---|---|---|---|---|---|
| 1918 | 2009 | 1918 | 2009 | ||
| Recommend supports in the home for personal care/activities of daily living as required | 583,827 | 834,852 | 6,760 | 58 | 87 |
| Administer vaccine | 512,295 | 664,087 | 6,466 | 53 | 73 |
| Document vaccination according to policy and regulations | 512,295 | 664,087 | 6,466 | 53 | 73 |
| Take a medical history relevant to immunization, noting contraindications, allergies, etc. | 512,295 | 664,087 | 6,586 | 52 | 71 |
| Recognize initial adverse events (e.g., anaphylaxis) occurring in community immunization clinics | 512,295 | 664,087 | 6,586 | 52 | 71 |
| Monitor for adverse events associated with immunization among members of the public (surveillance) | 512,295 | 664,087 | 6,586 | 52 | 71 |
| Obtain informed consent for immunization | 512,295 | 664,087 | 6,762 | 51 | 69 |
| Screen for eligibility for immunization | 512,295 | 664,087 | 7,109 | 48 | 66 |
| Interpret the results of history, physical exam, chest X-ray and laboratory tests, leading to a diagnosis | 71,532 | 170,765 | 608 | 78 | 198 |
| Assess nutritional and hydration needs of patient | 71,532 | 170,765 | 6,466 | 7 | 19 |
FTE = full-time equivalent.
The services required most often are the same in each pandemic scenario, but they are required by more people for the more severe pandemic. In both scenarios, making diagnoses based on histories, exam and test results is most “scarce” in terms of the ratio of numbers of patients requiring that service to the number of FTE providers with the competency to provide it. Eight of these 10 services pertain mainly to providing mass vaccinations and as such would be required by large numbers of people. However, there are over 6,000 FTE providers competent to provide these services. In contrast, the “most scarce” service in both scenarios – making a diagnosis – would only be required by those patients who are (or suspected to be) ill, yet there are far fewer (about 600) FTE providers competent to provide this service.
Discussion
The results suggest that Nova Scotia likely has sufficient HHR necessary – in terms of numbers and competencies – to respond to an influenza pandemic similar to that which occurred in 2009 provided that available qualified personnel are fully deployed to this purpose. Although the profession-level results included shortages of at least one profession in every team combination for each type of pandemic simulated, the service-level results suggest that the provincial health workforce as a whole would have the capacity to respond to even a severe pandemic. The highest simulated productivity level required is just under 200 diagnoses per FTE per month; this seems achievable given that the Nova Scotia physicians provided an average of 218 consultations per physician per month in 2014 (CIHI 2015). The results suggest that Nova Scotia would not have sufficient HHR to respond to a more severe pandemic similar to that which occurred in 1918.
Participants in the stakeholder workshop reported that the results were plausible given their recent experiences, and agreed that the approach was useful for informing pandemic planning specifically and for workforce and health service planning more broadly. The conceptual complexity of this HHR approach was perceived as a potential barrier to uptake. This perception is understandable given that the participants were unfamiliar with this innovative approach and would need time to become familiar with its use. Furthermore, traditional approaches to HHR planning, such as the use of provider:population ratios, may be simpler but are not adapted for the particular setting to which they are applied, and thus may be inaccurate. Despite the fundamental flaws of such simple approaches being articulated by key stakeholders such as the WHO since at least the 1970s (WHO 1971), their use remains prevalent among governments and healthcare organizations worldwide (Ono et al. 2013; Tomblin Murphy et al. 2016). Collaborative, long-term partnerships between researchers, clinicians and policy- and decision-makers are critical to ensuring that governments and healthcare organizations develop the political and technical capacity to undertake planning to meet the needs of the populations they serve. Toward this broader aim, in the present study the research team included both clinicians and policy- and decision-makers, and the broader communities of researchers, policy- and decision-makers and clinicians were invited to review and provide input on the study methods and findings at multiple points during and after its implementation.
Assessing the provincial health workforce's overall capacity to respond to a pandemic is central to pandemic planning. Three other crucial HHR policy issues which will affect Nova Scotia's pandemic response to a pandemic but which are outside the scope of this study are: (a) the way in which provincial resources are managed and deployed within the province; (b) the degree to which Nova Scotia's HHR could be relieved of their existing responsibilities to respond to a pandemic and (c) the availability of other, non-human resources, such as ventilators, vaccines and hospital beds. The Nova Scotia Department of Health (2010)'s report on its response to the 2009 H1N1 pandemic addresses these issues indirectly via three points:
Purchasing 90 additional ventilators, developing a protocol to prioritize the use of intensive care beds and working with the federal government to have more involvement in the process of approving and acquiring vaccines.
The establishment of a provincial “good neighbour” protocol to allow the workforce to more easily provide care through different DHAs and other organizations in the event of staff shortages during emergency situations.
The establishment of two alternate means for members of the public to obtaining influenza information and care – a telephone consultation service and 15 dedicated influenza assessment centres separate from existing healthcare facilities – is thought to have significantly reduced requirements for influenza care from doctor's offices, clinics and emergency departments.
The degree to which existing HHR could potentially be “diverted” from their existing duties to respond to a pandemic could be analyzed through the model's participation (e.g., by reserving some percentage of the available workforce for pre-existing, non-pandemic-related care) and/or activity (e.g., by reserving some percentage of the available workforce's working hours for pre-existing care) parameters. Because of space constraints, such analyses have not been included here. Other examples of analyses not included here – but which are possible through the model – include estimating the impacts of policies aimed at improving healthcare productivity, such as training to promote and support more collaborative care between different types of HHR.
More broadly, the scope of the study was specific to human resources as opposed to non-human resources. Although the capacity of health systems to respond to pandemics (or any other health issue) will depend on the adequacy of available human and non-human resources, we know of no integrated, needs-based service planning model that includes both human and non-human resources. A recent systematic review of HHR and health labour market analyses identified this as a gap across high-income Organisation for Economic Co-operation and Development countries (Tomblin Murphy et al. 2016).
The analyses were affected by some important data limitations which must be considered when interpreting the results. The model can accommodate any updated or improved input data as they become available, at which time the analyses can be re-run.
The epidemiological profile of a future influenza pandemic cannot be accurately predicted. The data used to create these results, because they are based on responses to actual influenza pandemics, are biased by the availability of workforce and other healthcare resources such as vaccines, and may therefore underestimate the potential severity of a similar future pandemic.
The level of service estimates, although informed by clinical experience, knowledge of current evidence and established best practices, may still be subject to professional bias.
The different team configurations and their associated estimated productivity values were based on the professional opinions and experiences of panel participants as opposed to empirical analysis or other evidence that may have been more rigorous and less subject to potential bias.
The estimated participation and activity levels for different types of HHR were based on data from only one DHA and only some of the included types of HHR – care aides, dietitians, the nursing professions, pharmacists and physiotherapists – and thus may not accurately represent the values of these levels at the provincial level.
For the service-specific analysis, the mapping of influenza care services to the respective competencies of different types of HHR is an imperfect means of estimating the prevalence of these competencies among the members of these professions. This is because, despite their being required as a condition of entry to practice, not all members of a given profession may possess each of these competencies at a given time. By the same token, clinicians may have gained competency in performing other services beyond those required for entry to practice without having been formally certified as such.
These limitations notwithstanding, the results illustrate the application of a healthcare planning approach in which planning for healthcare services and planning for HHR are interdependent, and in which both processes are directly contingent on measures of population health. Although a wide range of simulation tools exist to guide influenza pandemic resource planning, most of which incorporate consideration of different epidemiological parameters (Van Kerkhove and Ferguson 2012), we are not aware of any that also integrate planning for specific influenza services with planning for the HHR required to provide them. For example, the AsiaFluCap simulator (Stein et al. 2012) calculates HHR requirements based on specific staffing:bed ratios.
Moreover, the demonstration of the competency mapping process as an objective and systematic means of estimating the prevalence of particular competencies across a health workforce has applicability across health system and HHR planning. It is considerably less burdensome on practicing HHR than a lengthy survey, and less subject to the low response rates and selection biases that may accompany such instruments. In contrast to other methods of assessing the prevalence of specific competencies within a health workforce, competency mapping lends itself well to application across multiple health issues and on a regular basis, providing planners with a means of more comprehensively, regularly and systematically assessing the degree to which the capacities of their respective health workforces are aligned with the needs of the populations they serve.
In the present study, analyses were specific to a single population health issue – pandemic influenza. Other applications of similar planning approaches provide examples of how these can be broadened to apply to multiple conditions or to entire populations. For example, in the present study, pandemic influenza was chosen as the issue of interest from the outset. One alternative approach would be to begin the study by selecting the specific health issue(s) to be addressed; this approach was used by Goma and colleagues (2014) in planning for malaria and HIV/AIDS in Zambia. Another application of such an approach in Canada began by planning for the top five health issues facing the populations being studied and eventually expanded to eight; the authors noted that with each added condition, the number of unique services (and associated competencies) to be included in the model was smaller (Tomblin Murphy et al. 2013b). This finding suggests that the vast majority of healthcare services required by a population could be feasibly incorporated into a planning approach such as the one used in the present study without the underlying model becoming unwieldy.
Conclusions
The results of these analyses suggest that the publicly funded healthcare system in Nova Scotia has the overall capacity to cope with a mild influenza epidemic. The degree to which the province is able to respond to such an event is directly contingent not only on this overall capacity, but also on how it is deployed and managed across different parts of the province.
More broadly, this study demonstrated the application of an integrated, needs-based approach to healthcare service and HHR planning in the context of a potential future influenza pandemic at the provincial level in Canada. The results provide insight into this jurisdiction's capacity to respond to such surges in its population's need for healthcare, and identified specific services which may be in short supply during such an event. Although the included data and analyses are specific to influenza, the general approach can also be applied to other diseases which result in surges in health needs, such as Ebola.
Finally, this paper described the application of competency mapping as an advancement in the practical application of such approaches to planning. This method increases the ease with which these types of needs-based, integrated approaches to health service and HHR planning can be systematically implemented by planners to address a variety of health issues in different contexts.
Acknowledgements
This research received funding from the Canadian Institutes of Health Research, Partnerships for Health System Improvement program (PHE-104197) and the Nova Scotia Health Research Foundation (PSO-MAT-2010-6404-RPP). The funders had no involvement in the study design; in the collection, analysis and interpretation of data; in the writing of the report and in the decision to submit the article for publication.
The project was supported by and included involvement from our project partners – the Nova Scotia Department of Health and Wellness, the Island Health Authority (BC) and the British Columbia Ministry of Health.
Contributor Information
Gail Tomblin Murphy, Professor and Director, WHO/PAHO Collaborating Centre on Health Workforce Planning & Research, School of Nursing, Dalhousie University, Halifax, NS.
Stephen Birch, Professor, Centre for Health Economics and Policy Analysis, McMaster University, Hamilton, ON.
Adrian Mackenzie, Doctoral Trainee, WHO/PAHO Collaborating Centre on Health Workforce Planning & Research, School of Nursing, Dalhousie University, Halifax, NS.
Janet Rigby, Research Officer, WHO/PAHO Collaborating Centre on Health Workforce Planning & Research, School of Nursing, Dalhousie University, Halifax, NS.
Joanne Langley, Professor, Departments of Pediatrics and Community Health and Epidemiology, Dalhousie University and IWK Health Centre, Halifax, NS.
References
- Bärnighausen T., Bloom D.E., Humair S. 2007. “Human Resources for Treating HIV/AIDS: Needs, Capacities, and Gaps.” AIDS Patient Care and STDs 21(11): 799–812. [DOI] [PubMed] [Google Scholar]
- Bärnighausen T., Bloom D.E., Humair S. 2016. “Human Resources for Treating HIV/AIDS: Are the Preventive Effects of Antiretroviral Treatment a Game Changer?” PLoS ONE 11(10): e0163960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birch S. 1985. “Equity and Efficiency in Medical Manpower Planning: Defining Objectives and Looking Towards the Future.” Health Policy 4(4): 341–46. [DOI] [PubMed] [Google Scholar]
- Birch S., Kephart G., Murphy Tomblin, O'Brien-Pallas L., Alder R., MacKenzie A. 2007. “Human Resources Planning and the Production of Health: A Needs-Based Analytical Framework.” Canadian Public Policy 33(Suppl.): S1–S16. [DOI] [PubMed] [Google Scholar]
- Bruckner T.A., Scheffler R.M., Shen G., Yoon J., Chisholm D., Morris J. et al. 2011. “The Mental Health Workforce Gap in Low- and Middle-Income Countries: A Needs-Based Approach.” Bulletin of the World Health Organization 89(3): 184–94. 10.2471/BLT.10.082784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Canadian Institute for Health Information (CIHI). 2015. Physicians in Canada, 2014. Ottawa, ON: Author; Retrieved October 27, 2015. <https://secure.cihi.ca/estore/productFamily.htm?locale=en&pf=PFC2960>. [Google Scholar]
- Crettenden I.F., McCarty M.V., Fenech B.J., Heywood T., Taitz M.C., Tudman S. 2014. “How Evidence-Based Workforce Planning in Australia is Informing Policy Development in the Retention and Distribution of the Health Workforce.” Human Resources for Health 12: 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eyles J., Birch S., Newbold K.B. 1993. “Equitable Access to Health Care: Methodological Extensions to the Analysis of Physician Utilization in Canada.” Health Economics 2(2): 87–101. [DOI] [PubMed] [Google Scholar]
- Gallagher J.E., Lim Z., Harper P.R. 2013. “Workforce Skill Mix: Modelling the Potential for Dental Therapists in State-Funded Primary Dental Care.” International Dental Journal 63(2): 57–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goma F.M., Tomblin Murphy G., Libetwa M., MacKenzie A., Nzala S.H., Mbwili-Muleya C. 2014. “Pilot-Testing Service-Based Planning for Health Care In Rural Zambia.” BMC Health Services Research 14(Suppl. 1): S7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hallett T.B., Gregson S., Dube S., Mapfeka E.S., Mugurungi O., Garnett G.P. 2011. “Estimating the Resources Required in the Roll-Out of Universal Access to Antiretroviral Treatment in Zimbabwe.” Sexually Transmitted Infections 87(7): 621–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jansen C., Codjia L., Cometto G., Yansané M.L., Dieleman M. 2014. “Realizing Universal Health Coverage for Maternal Health Services in the Republic of Guinea: The Use of Workforce Projections to Design Health Labor Market Interventions.” Risk Management and Health Care Policy 7: 219–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kurowski C., Wyss K., Abdulla S., Mills A. 2007. “Scaling up Priority Health Interventions in Tanzania: The Human Resources Challenge.” Health Policy and Planning 22(3): 113–27. [DOI] [PubMed] [Google Scholar]
- Kurowski C., Wyss K., Abdulla S., Yémadji S., Mills A. 2004. Human Resources for Health: Requirements and Availability in the Context of Scaling-Up Priority Interventions in Low-Income Countries Case Studies from Tanzania and Chad. Washington, DC: The World Bank; Retrieved October 15, 2014. <http://www.who.int/workforcealliance/knowledge/resources/priority_interventions_tanzaniachad/en/>. [Google Scholar]
- Mejía A., Fülöp T. 1978. “Health Manpower Planning: An Overview.” In Hall T.L., Mejía A., eds. Health Manpower Planning: Principles, Methods, Issues. Geneva, CH: WHO; Retrieved May 5, 2015. <http://apps.who.int/iris/handle/10665/40341>. [Google Scholar]
- New Zealand Ministry of Health. 2011a. Aged Care Workforce Service Forecast. Wellington, NZ: Author; Retrieved September 20, 2015. <http://www.health.govt.nz/our-work/health-workforce/workforce-service-forecasts/aged-care-workforce-service-forecast>. [Google Scholar]
- New Zealand Ministry of Health. 2011b. Diabetes Workforce Service Forecast. Wellington, NZ: Author; Retrieved September 20, 2015. <http://www.health.govt.nz/our-work/health-workforce/workforce-service-forecasts/diabetes-workforce-service-forecast>. [Google Scholar]
- Nova Scotia Department of Health. 2010. Nova Scotia's Response to H1N1: Summary Report. Halifax, NS: Author; Retrieved November 15, 2013. <http://novascotia.ca/dhw/publications/H1N1-Summary-Report.pdf>. [Google Scholar]
- Ono T., Lafortune G., Schoenstein M. 2013. Health Workforce Planning in OECD Countries. Paris, FR: Organisation for Economic Co-operation and Development; Retrieved April 6, 2015. <http://www.oecd-ilibrary.org/social-issues-migration-health/health-workforce-planning-in-oecd-countries_5k44t787zcwb-en>. [Google Scholar]
- Pike J. 2011. Flu Pandemic Mortality/Morbidity. Retrieved February 10, 2012. <http://www.globalsecurity.org/security/ops/hsc-scen-3_flu-pandemic-deaths.htm>.
- Segal L., Leach M.J. 2011. “An Evidence-Based Health Workforce Model for Primary and Community Care.” Implementation Science 6(6): 93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smetanin P., Stiff D., Briante C. 2010. H1N1 2009 Pandemic Analysis: Evaluation and Scenarios for Post Pandemic Planning. Toronto, ON: RiskAnalytica; Retrieved November 15, 2013. <http://beta.riskanalytica.com/sites/riskanalytica.com/files/H1N1 2009 Pandemic Analysis Evaluation and Scenarios for Post-Pandemic Planning August 2010.pdf>. [Google Scholar]
- Statistics Canada. 2015. Estimates of Population, by Age Group and Sex for July 1, Canada, Provinces and Territories. CANSIM Table 051-0001. Ottawa, ON: Author; Retrieved October 27, 2015. <http://www5.statcan.gc.ca/cansim/a26?lang=eng&id=510001>. [Google Scholar]
- Stein M.L., Rudge J.W., Coker R., van der Weijden C., Krumkamp R., Hanvoravongchai P. et al. 2012. “Development of a Resource Modelling Tool to Support Decision Makers in Pandemic Influenza Preparedness: The Asiaflucap Simulator.” BMC Public Health 12: 870. 10.1186/1471-2458-12-870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tianviwat S., Chongsuvivatwong V., Birch S. 2009. “Optimizing the Mix of Basic Dental Services for Southern Thai Schoolchildren Based on Resource Consumption, Service Needs and Parental Preference.” Community Dentistry and Oral Epidemiology 37(4): 372–80. [DOI] [PubMed] [Google Scholar]
- Tomblin Murphy G., Birch S., MacKenzie A., Bradish S., Elliott Rose A. 2016. “A Synthesis of Recent Analyses of Human Resources for Health Requirements and Labour Market Dynamics in High-Income OECD Countries.” Human Resources for Health 14: 59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomblin Murphy G., MacKenzie A., Alder R., Langley J., Hickey M., Cook A. 2013a. “Pilot-Testing an Applied Competency-Based Approach to Health Human Resources Planning.” Health Policy and Planning 28(7): 739–49. 10.1093/heapol/czs115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomblin Murphy G., MacKenzie A., Rigby J., Rockwood K., Gough A., Greeley G. et al. 2013b. “Service-based Planning for Older Adults.” Journal of the American Medical Directors Association 14(8): 611–15. [DOI] [PubMed] [Google Scholar]
- Tomblin Murphy G., MacKenzie A., Walker C., Guy-Walker J. 2014. “Needs-Based Human Resources for Health Planning in Jamaica: Using Simulation Modelling to Inform Policy Options for Pharmacists in the Public Sector.” Human Resources for Health 12: 67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Kerkhove M.D., Ferguson N.M. 2012. “Epidemic and Intervention Modelling – A Scientific Rationale for Policy Decisions? Lessons from the 2009 Influenza Pandemic.” Bulletin of the World Health Organization 90(4): 306–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO. 1971. The Development of Studies in Health Manpower: Report of a WHO Scientific Group. Geneva, CH: Author; Retrieved May 15, 2015. <http://apps.who.int/iris/handle/10665/40928>. [PubMed] [Google Scholar]


